How to relieve stuffy nose in child
What Kind of Stuff Clears Up a Stuffy Nose?
AddictionAllergies & AsthmaAmbulatoryAudiologyAutismAwardsBC4TeensBehavioral HealthBehind the ScenesBurn CenterCancerCardiologyCenter for Healthy Weight and NutritionCenter for Injury Research and PolicyChild BehaviorChild DevelopmentColorectal and Pelvic ReconstructionCommunity EducationCommunity ResourcesCoronavirusDentistryDermatologyDiseases & ConditionsDiversity and InclusionEndocrinologyENTEpilepsyEverything MattersFertility and Reproductive Health ProgramFundraising EventsGastroenterologyGeneticsGynecologyHematologyHomecareHospiceHospital NewsInfants & NewbornsInfectious DiseaseKids & TeensLaboratory ServicesMake Safe HappenMarathonNeonatologyNephrologyNeurologyNeurosurgeryNew HospitalNICUNutrition & FitnessOccupational TherapyOphthalmologyOrthopedicsOur PatientsOur staffPalliative CareParentingPediatric NewsPharmacyPhysical Therapy - Sports and OrthopedicPlastic SurgeryPopulation HealthPregnancyPrimary CarePsychologyPulmonaryRadiologyReach Out and ReadRehabilitationResearchRheumatologySafety & PreventionSports MedicineSurgical ServicesThe Center for Family Safety and HealingTherapeutic RecreationTherapyTHRIVE ProgramToddlers & PreschoolersUrgent CareUrology
Aaron Barber, AT, ATC, PESAbbie Roth, MWCAdam Ostendorf, MDAdriane Baylis, PhD, CCC-SLPAdrienne M. Flood, CPNP-ACAdvanced Healthcare Provider CouncilAila Co, MDAlaina White, AT, ATCAlana Milton, MDAlana Milton, MDAlecia Jayne, AuDAlena SchuckmannAlessandra Gasior, DOAlex Kemper, MDAlexandra Funk, PharmD, DABATAlexandra Sankovic, MDAlexis Klenke, RD, LDAlice Bass, CPNP-PCAlison PeggAllie DePoyAllison Rowland, AT, ATCAllison Strouse, MS, AT, ATCAmanda E. Graf, MDAmanda GoetzAmanda Smith, RN, BSN, CPNAmanda Sonk, LMTAmanda Whitaker, MDAmber Patterson, MDAmberle Prater, PhD, LPCCAmy Coleman, LISWAmy Dunn, MDAmy E. Valasek, MD, MScAmy Fanning, PT, DPTAmy Garee, CPNP-PCAmy Hahn, PhDAmy HessAmy Leber, PhDAmy LeRoy, CCLSAmy Moffett, CPNP-PCAmy Randall-McSorley, MMC, EdD CandidateAmy Thomas, BSN, RN, IBCLCAmy Wahl, APNAnastasia Fischer, MD, FACSMAndala HardyAndrea Brun, CPNP-PCAndrea M. Boerger, MEd, CCC-SLPAndrea Sattler, MDAndrew AxelsonAndrew Kroger, MD, MPHAndrew SchwadererAndria Haynes, RNAngela AbenaimAngela Billingslea, LISW-SAnn Pakalnis, MDAnna Lillis, MD, PhDAnnette Haban-BartzAnnie Drapeau, MDAnnie Temple, MS, CCC-SLP, CLCAnnie Truelove, MPHAnthony Audino, MDAnup D.
 Patel, MDAri Rabkin, PhDAriana Hoet, PhDArielle Sheftall, PhDArleen KarczewskiAshlee HallAshleigh Kussman, MDAshley Debeljack, PsyDAshley Ebersole, MDAshley EcksteinAshley Kroon Van DiestAshley M. Davidson, AT, ATC, MSAshley Minnick, MSAH, AT, ATCAshley Overall, FNPAshley Parikh, CPNP-PCAshley Parker MSW, LISW-SAshley Parker, LISW-SAshley Tuisku, CTRSAsuncion Mejias, MD, PhDAurelia Wood, MDBailey Young, DOBecky Corbitt, RNBelinda Mills, MDBenjamin Fields, PhD, MEdBenjamin Kopp, MDBernadette Burke, AT, ATC, MSBeth Martin, RNBeth Villanueva, OTD, OTR/LBethany Uhl, MDBethany Walker, PhDBhuvana Setty, MDBill Kulju, MS, ATBlake SkinnerBonnie Gourley, MSW, LSWBrad Childers, RRT, BSBrandi Cogdill, RN, BSN, CFRN, EMT-PBrandon MorganBreanne L. Bowers, PT, DPT, CHT, CFSTBrendan Boyle, MD, MPHBrian Boe, MDBrian K. Kaspar, PhDBrian Kellogg, MDBriana Crowe, PT, DPT, OCSBrigid Pargeon, MS, MT-BCBrittney Hardin, MOT, OTR/LBrooke Sims, LPCC, ATRCagri Toruner, MDCaitlin Bauer, RD, LDCaitlin TullyCaleb MosleyCallista DammannCallista PoppCami Winkelspecht, PhDCamille Wilson, PhDCanice Crerand, PhDCara Inglis, PsyDCarl H.
Patel, MDAri Rabkin, PhDAriana Hoet, PhDArielle Sheftall, PhDArleen KarczewskiAshlee HallAshleigh Kussman, MDAshley Debeljack, PsyDAshley Ebersole, MDAshley EcksteinAshley Kroon Van DiestAshley M. Davidson, AT, ATC, MSAshley Minnick, MSAH, AT, ATCAshley Overall, FNPAshley Parikh, CPNP-PCAshley Parker MSW, LISW-SAshley Parker, LISW-SAshley Tuisku, CTRSAsuncion Mejias, MD, PhDAurelia Wood, MDBailey Young, DOBecky Corbitt, RNBelinda Mills, MDBenjamin Fields, PhD, MEdBenjamin Kopp, MDBernadette Burke, AT, ATC, MSBeth Martin, RNBeth Villanueva, OTD, OTR/LBethany Uhl, MDBethany Walker, PhDBhuvana Setty, MDBill Kulju, MS, ATBlake SkinnerBonnie Gourley, MSW, LSWBrad Childers, RRT, BSBrandi Cogdill, RN, BSN, CFRN, EMT-PBrandon MorganBreanne L. Bowers, PT, DPT, CHT, CFSTBrendan Boyle, MD, MPHBrian Boe, MDBrian K. Kaspar, PhDBrian Kellogg, MDBriana Crowe, PT, DPT, OCSBrigid Pargeon, MS, MT-BCBrittney Hardin, MOT, OTR/LBrooke Sims, LPCC, ATRCagri Toruner, MDCaitlin Bauer, RD, LDCaitlin TullyCaleb MosleyCallista DammannCallista PoppCami Winkelspecht, PhDCamille Wilson, PhDCanice Crerand, PhDCara Inglis, PsyDCarl H. Backes, MDCarlo Di Lorenzo, MDCarly FawcettCarol Baumhardt, LMTCarolyn FigiCarrie Rhodes, CPST-I, MTSA, CHESCasey Cottrill, MD, MPHCasey TrimbleCassandra McNabb, RN-BSNCatherine Earlenbaugh, RNCatherine Sinclair, MDCatherine Trimble, FNPCatrina Litzenburg, PhDCharae Keys, MSW, LISW-SCharles Elmaraghy, MDChelsea Britton, MS, RD, LD, CLC Chelsie Doster, BSCheryl Boop, MS, OTR/LCheryl G. Baxter, CPNPCheryl Gariepy, MDChet Kaczor, PharmD, MBAChris MarreroChris Smith, RNChristina Ching, MDChristina DayChristine Johnson, MA, CCC-SLPChristine Koterba, PhDChristine Mansfield, PT, DPT, OCS, ATCChristine PrusaChristopher Goettee, PT, DPT, OCSChristopher Iobst, MDChristopher Ouellette, MDChristy Lumpkins, LISW-SCindy IskeClaire Kopko PT, DPT, OCS, NASM-PESCody Hostutler, PhDConnor McDanel, MSW, LSWCorey Rood, MDCorinne Syfers, CCLSCourtney Bishop. PA-CCourtney Brown, MDCourtney Hall, CPNP-PCCourtney Porter, RN, MSCristina Tomatis Souverbielle, MDCrystal MilnerCurt Daniels, MDCynthia Holland-Hall, MD, MPHDana Lenobel, FNPDana Noffsinger, CPNP-ACDane Snyder, MDDaniel Coury, MDDaniel DaJusta, MDDanielle Peifer, PT, DPTDavid A Wessells, PT, MHADavid Axelson, MDDavid Stukus, MDDean Lee, MD, PhDDebbie Terry, NPDeborah Hill, LSWDeborah Zerkle, LMTDeena Chisolm, PhDDeipanjan Nandi, MD MScDenis King, MDDenise EllDennis Cunningham, MDDennis McTigue, DDSDiane LangDominique R.
Backes, MDCarlo Di Lorenzo, MDCarly FawcettCarol Baumhardt, LMTCarolyn FigiCarrie Rhodes, CPST-I, MTSA, CHESCasey Cottrill, MD, MPHCasey TrimbleCassandra McNabb, RN-BSNCatherine Earlenbaugh, RNCatherine Sinclair, MDCatherine Trimble, FNPCatrina Litzenburg, PhDCharae Keys, MSW, LISW-SCharles Elmaraghy, MDChelsea Britton, MS, RD, LD, CLC Chelsie Doster, BSCheryl Boop, MS, OTR/LCheryl G. Baxter, CPNPCheryl Gariepy, MDChet Kaczor, PharmD, MBAChris MarreroChris Smith, RNChristina Ching, MDChristina DayChristine Johnson, MA, CCC-SLPChristine Koterba, PhDChristine Mansfield, PT, DPT, OCS, ATCChristine PrusaChristopher Goettee, PT, DPT, OCSChristopher Iobst, MDChristopher Ouellette, MDChristy Lumpkins, LISW-SCindy IskeClaire Kopko PT, DPT, OCS, NASM-PESCody Hostutler, PhDConnor McDanel, MSW, LSWCorey Rood, MDCorinne Syfers, CCLSCourtney Bishop. PA-CCourtney Brown, MDCourtney Hall, CPNP-PCCourtney Porter, RN, MSCristina Tomatis Souverbielle, MDCrystal MilnerCurt Daniels, MDCynthia Holland-Hall, MD, MPHDana Lenobel, FNPDana Noffsinger, CPNP-ACDane Snyder, MDDaniel Coury, MDDaniel DaJusta, MDDanielle Peifer, PT, DPTDavid A Wessells, PT, MHADavid Axelson, MDDavid Stukus, MDDean Lee, MD, PhDDebbie Terry, NPDeborah Hill, LSWDeborah Zerkle, LMTDeena Chisolm, PhDDeipanjan Nandi, MD MScDenis King, MDDenise EllDennis Cunningham, MDDennis McTigue, DDSDiane LangDominique R.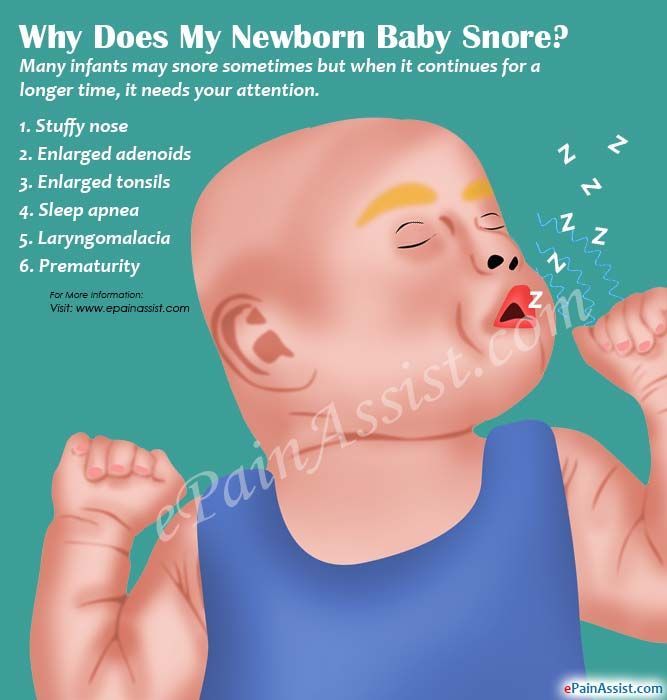 Williams, MD, MPH, FAAP, Dipl ABOMDonna M. Trentel, MSA, CCLSDonna Ruch, PhDDonna TeachDoug WolfDouglas McLaughlin, MDDrew Duerson, MDEd MinerEdward Oberle, MD, RhMSUSEdward Shepherd, MDEileen Chaves, PhDElena CamachoElise Berlan, MDElise DawkinsElizabeth A. Cannon, LPCCElizabeth Cipollone, LPCC-SElizabeth Zmuda, DOEllyn Hamm, MM, MT-BCEmily A. Stuart, MDEmily Decker, MDEmily GetschmanEmma Wysocki, PharmD, RDNEric Butter, PhDEric Leighton, AT, ATCEric Sribnick, MD, PhDErica Domrose, RD, LDEricca L Lovegrove, RD, LDErika RobertsErin Gates, PT, DPTErin Johnson, M.Ed., C.S.C.S.Erin Shann, BSN, RNErin TebbenFarah W. Brink, MDFatimah MasoodFrances Fei, MDGail Bagwell, DNP, APRN, CNSGail Besner, MDGail Swisher, ATGarey Noritz, MDGary A. Smith, MD, DrPHGeri Hewitt, MDGina Hounam, PhDGina McDowellGina MinotGrace Paul, MDGregory D. Pearson, MDGriffin Stout, MDGuliz Erdem, MDHailey Blosser, MA, CCC-SLPHanna MathessHeather Battles, MDHeather ClarkHeather L. Terry, MSN, RN, FNP-C, CUNPHeather Yardley, PhDHenry SpillerHenry Xiang, MD, MPH, PhDHerman Hundley, MS, AT, ATC, CSCSHilary Michel, MDHiren Patel, MDHolly Deckling, MSWHoma Amini, DDS, MPH, MSHoward Jacobs, MDHunter Wernick, DOIbrahim Khansa, MDIhuoma Eneli, MDIlana Moss, PhDIlene Crabtree, PTIrene Mikhail, MDIrina Buhimschi, MDIvor Hill, MDJackie Cronau, RN, CWOCNJacqueline Wynn, PhD, BCBA-DJacquelyn Doxie King, PhDJaime-Dawn Twanow, MDJaimie D.
Williams, MD, MPH, FAAP, Dipl ABOMDonna M. Trentel, MSA, CCLSDonna Ruch, PhDDonna TeachDoug WolfDouglas McLaughlin, MDDrew Duerson, MDEd MinerEdward Oberle, MD, RhMSUSEdward Shepherd, MDEileen Chaves, PhDElena CamachoElise Berlan, MDElise DawkinsElizabeth A. Cannon, LPCCElizabeth Cipollone, LPCC-SElizabeth Zmuda, DOEllyn Hamm, MM, MT-BCEmily A. Stuart, MDEmily Decker, MDEmily GetschmanEmma Wysocki, PharmD, RDNEric Butter, PhDEric Leighton, AT, ATCEric Sribnick, MD, PhDErica Domrose, RD, LDEricca L Lovegrove, RD, LDErika RobertsErin Gates, PT, DPTErin Johnson, M.Ed., C.S.C.S.Erin Shann, BSN, RNErin TebbenFarah W. Brink, MDFatimah MasoodFrances Fei, MDGail Bagwell, DNP, APRN, CNSGail Besner, MDGail Swisher, ATGarey Noritz, MDGary A. Smith, MD, DrPHGeri Hewitt, MDGina Hounam, PhDGina McDowellGina MinotGrace Paul, MDGregory D. Pearson, MDGriffin Stout, MDGuliz Erdem, MDHailey Blosser, MA, CCC-SLPHanna MathessHeather Battles, MDHeather ClarkHeather L. Terry, MSN, RN, FNP-C, CUNPHeather Yardley, PhDHenry SpillerHenry Xiang, MD, MPH, PhDHerman Hundley, MS, AT, ATC, CSCSHilary Michel, MDHiren Patel, MDHolly Deckling, MSWHoma Amini, DDS, MPH, MSHoward Jacobs, MDHunter Wernick, DOIbrahim Khansa, MDIhuoma Eneli, MDIlana Moss, PhDIlene Crabtree, PTIrene Mikhail, MDIrina Buhimschi, MDIvor Hill, MDJackie Cronau, RN, CWOCNJacqueline Wynn, PhD, BCBA-DJacquelyn Doxie King, PhDJaime-Dawn Twanow, MDJaimie D. Nathan, MD, FACSJames Murakami, MDJames Popp, MDJames Ruda, MDJameson Mattingly, MDJamie Macklin, MDJamie ReedyJane AbelJanelle Huefner, MA, CCC-SLPJanice M. Moreland, CPNP-PC, DNPJanice Townsend, DDS, MSJared SylvesterJason JacksonJason P. Garee, PhDJaysson EicholtzJean Hruschak, MA, CCC/SLPJeff Sydes, CSCSJeffery Auletta, MDJeffrey Bennett, MD, PhDJeffrey Hoffman, MDJeffrey Leonard, MDJen Campbell, PT, MSPTJena HeckJenn Gonya, PhDJennie Aldrink, MDJennifer Borda, PT, DPTJennifer HofherrJennifer LockerJennifer PrinzJennifer Reese, PsyDJennifer Smith, MS, RD, CSP, LD, LMTJennifer Walton, MD, MPH, FAAPJenny Worthington, PT, DPTJerry R. Mendell, MDJessalyn Mayer, MSOT, OTR/LJessica Bailey, PsyDJessica Bogacik, MS, MT-BCJessica Bowman, MDJessica BrockJessica Bullock, MA/CCC-SLPJessica Buschmann, RDJessica Scherr, PhDJim O’Shea OT, MOT, CHTJoan Fraser, MSW, LISW-SJohn Ackerman, PhDJohn Caballero, PT, DPT, CSCSJohn Kovalchin, MDJonathan D. Thackeray, MDJonathan Finlay, MB, ChB, FRCPJonathan M.
Nathan, MD, FACSJames Murakami, MDJames Popp, MDJames Ruda, MDJameson Mattingly, MDJamie Macklin, MDJamie ReedyJane AbelJanelle Huefner, MA, CCC-SLPJanice M. Moreland, CPNP-PC, DNPJanice Townsend, DDS, MSJared SylvesterJason JacksonJason P. Garee, PhDJaysson EicholtzJean Hruschak, MA, CCC/SLPJeff Sydes, CSCSJeffery Auletta, MDJeffrey Bennett, MD, PhDJeffrey Hoffman, MDJeffrey Leonard, MDJen Campbell, PT, MSPTJena HeckJenn Gonya, PhDJennie Aldrink, MDJennifer Borda, PT, DPTJennifer HofherrJennifer LockerJennifer PrinzJennifer Reese, PsyDJennifer Smith, MS, RD, CSP, LD, LMTJennifer Walton, MD, MPH, FAAPJenny Worthington, PT, DPTJerry R. Mendell, MDJessalyn Mayer, MSOT, OTR/LJessica Bailey, PsyDJessica Bogacik, MS, MT-BCJessica Bowman, MDJessica BrockJessica Bullock, MA/CCC-SLPJessica Buschmann, RDJessica Scherr, PhDJim O’Shea OT, MOT, CHTJoan Fraser, MSW, LISW-SJohn Ackerman, PhDJohn Caballero, PT, DPT, CSCSJohn Kovalchin, MDJonathan D. Thackeray, MDJonathan Finlay, MB, ChB, FRCPJonathan M. Grischkan, MDJonathan Napolitano, MDJoshua Prudent, MDJoshua Watson, MDJulee Eing, CRA, RT(R)Julia Colman, MOT, OTR/LJulie ApthorpeJulie Lange, MDJulie Leonard, MD, MPHJulie Racine, PhDJulie Samora, MDJustin Indyk, MD, PhDKady LacyKaitrin Kramer, DDS, MS, PhDKaleigh Hague, MA, MT-BCKaleigh MatesickKamilah Twymon, LPCC-SKara Malone, MDKara Miller, OTR/LKaren A. Diefenbach, MDKaren Allen, MDKaren Days, MBAKaren Rachuba, RD, LD, CLCKari A. Meeks, OTKari Cardiff, ODKari Dubro, MS, RD, LD, CWWSKari Phang, MDKarla Vaz, MDKaryn L. Kassis, MD, MPHKasey Strothman, MDKatherine Deans, MDKatherine McCracken, MD FACOGKathleen (Katie) RoushKathryn Blocher, CPNP-PCKathryn J. Junge, RN, BSNKathryn Obrynba, MDKatia Camille Halabi, MDKatie Brind'Amour, MSKatie DonovanKatie Thomas, APRKatrina Hall, MA, CCLSKatrina Ruege, LPCC-SKatya Harfmann, MDKayla Zimpfer, PCCKaylan Guzman Schauer, LPCC-SKeli YoungKelley SwopeKelli Dilver, PT, DPTKelly AbramsKelly BooneKelly HustonKelly J. Kelleher, MDKelly McNally, PhDKelly N.
Grischkan, MDJonathan Napolitano, MDJoshua Prudent, MDJoshua Watson, MDJulee Eing, CRA, RT(R)Julia Colman, MOT, OTR/LJulie ApthorpeJulie Lange, MDJulie Leonard, MD, MPHJulie Racine, PhDJulie Samora, MDJustin Indyk, MD, PhDKady LacyKaitrin Kramer, DDS, MS, PhDKaleigh Hague, MA, MT-BCKaleigh MatesickKamilah Twymon, LPCC-SKara Malone, MDKara Miller, OTR/LKaren A. Diefenbach, MDKaren Allen, MDKaren Days, MBAKaren Rachuba, RD, LD, CLCKari A. Meeks, OTKari Cardiff, ODKari Dubro, MS, RD, LD, CWWSKari Phang, MDKarla Vaz, MDKaryn L. Kassis, MD, MPHKasey Strothman, MDKatherine Deans, MDKatherine McCracken, MD FACOGKathleen (Katie) RoushKathryn Blocher, CPNP-PCKathryn J. Junge, RN, BSNKathryn Obrynba, MDKatia Camille Halabi, MDKatie Brind'Amour, MSKatie DonovanKatie Thomas, APRKatrina Hall, MA, CCLSKatrina Ruege, LPCC-SKatya Harfmann, MDKayla Zimpfer, PCCKaylan Guzman Schauer, LPCC-SKeli YoungKelley SwopeKelli Dilver, PT, DPTKelly AbramsKelly BooneKelly HustonKelly J. Kelleher, MDKelly McNally, PhDKelly N.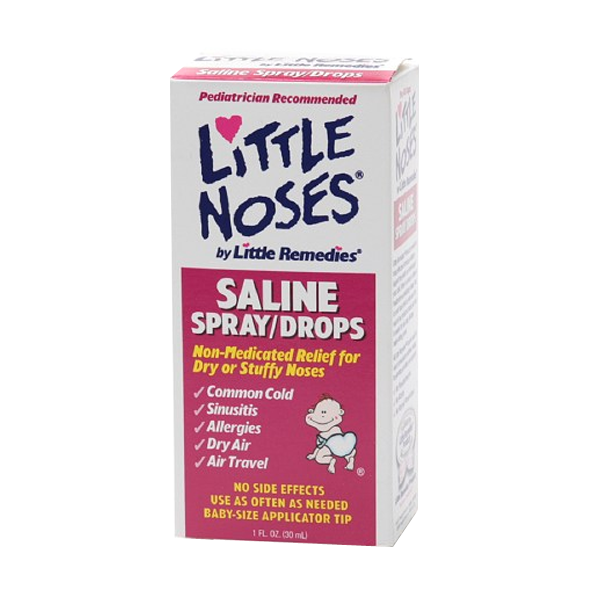 Day, CPNP-PCKelly Pack, LISW-SKelly Tanner,PhD, OTR/L, BCPKelly Wesolowski, PsyDKelly Wise, PharmDKent Williams, MDKevin Bosse, PhDKevin Klingele, MDKim Bjorklund, MDKim Hammersmith, DDS, MPH, MSKimberly Bates, MDKimberly Sisto, PT, DPT, SCSKimberly Van Camp, PT, DPT, SCSKirk SabalkaKris Jatana, MD, FAAPKrista Winner, AuD, CCC-AKristen Armbrust, LISW-SKristen Cannon, MDKristen E. Beck, MDKristen Martin, OTR/LKristi Roberts, MS MPHKristina Booth, MSN, CFNPKristina Reber, MDKristol Das, MDKyle DavisLance Governale, MDLara McKenzie, PhD, MALaura Brubaker, BSN, RNLaura Dattner, MALaura Martin, MDLaurel Biever, LPCLauren Durinka, AuDLauren Garbacz, PhDLauren Justice, OTR/L, MOTLauren Madhoun, MS, CCC-SLPLauryn Rozum, MS, CCLSLeah Middelberg, MDLee Hlad, DPMLeena Nahata, MDLelia Emery, MT-BCLeslie Appiah, MDLinda Stoverock, DNP, RN NEA-BCLindsay Kneen, MDLindsay Pietruszewski, PT, DPTLindsay SchwartzLindsey Vater, PsyDLisa GoldenLisa Halloran, CNPLisa M. Humphrey, MDLogan Blankemeyer, MA, CCC-SLPLori Grisez PT, DPTLorraine Kelley-QuonLouis Bezold, MDLourdes Hill, LPCC-S Lubna Mazin, PharmDLuke Tipple, MS, CSCSLynda Wolfe, PhDLyndsey MillerLynn RosenthalLynne Ruess, MDMaggy Rule, MS, AT, ATCMahmoud Kallash, MDManmohan K Kamboj, MDMarc P.
Day, CPNP-PCKelly Pack, LISW-SKelly Tanner,PhD, OTR/L, BCPKelly Wesolowski, PsyDKelly Wise, PharmDKent Williams, MDKevin Bosse, PhDKevin Klingele, MDKim Bjorklund, MDKim Hammersmith, DDS, MPH, MSKimberly Bates, MDKimberly Sisto, PT, DPT, SCSKimberly Van Camp, PT, DPT, SCSKirk SabalkaKris Jatana, MD, FAAPKrista Winner, AuD, CCC-AKristen Armbrust, LISW-SKristen Cannon, MDKristen E. Beck, MDKristen Martin, OTR/LKristi Roberts, MS MPHKristina Booth, MSN, CFNPKristina Reber, MDKristol Das, MDKyle DavisLance Governale, MDLara McKenzie, PhD, MALaura Brubaker, BSN, RNLaura Dattner, MALaura Martin, MDLaurel Biever, LPCLauren Durinka, AuDLauren Garbacz, PhDLauren Justice, OTR/L, MOTLauren Madhoun, MS, CCC-SLPLauryn Rozum, MS, CCLSLeah Middelberg, MDLee Hlad, DPMLeena Nahata, MDLelia Emery, MT-BCLeslie Appiah, MDLinda Stoverock, DNP, RN NEA-BCLindsay Kneen, MDLindsay Pietruszewski, PT, DPTLindsay SchwartzLindsey Vater, PsyDLisa GoldenLisa Halloran, CNPLisa M. Humphrey, MDLogan Blankemeyer, MA, CCC-SLPLori Grisez PT, DPTLorraine Kelley-QuonLouis Bezold, MDLourdes Hill, LPCC-S Lubna Mazin, PharmDLuke Tipple, MS, CSCSLynda Wolfe, PhDLyndsey MillerLynn RosenthalLynne Ruess, MDMaggy Rule, MS, AT, ATCMahmoud Kallash, MDManmohan K Kamboj, MDMarc P. Michalsky, MDMarcel J. Casavant, MDMarci Johnson, LISW-SMarcie RehmarMarco Corridore, MDMargaret Bassi, OTR/LMaria HaghnazariMaria Vegh, MSN, RN, CPNMarissa Condon, BSN, RNMarissa E. Larouere, MBA, BSN, RNMark E. Galantowicz, MDMark Smith, MS RT R (MR), ABMP PhysicistMarnie Wagner, MDMary Ann Abrams, MD, MPHMary Fristad, PhD, ABPPMary Kay SharrettMary Shull, MDMatthew Washam, MD, MPHMeagan Horn, MAMegan Brundrett, MDMegan Dominik, OTR/LMegan FrancisMegan Letson, MD, M.EdMeghan Cass, PT, DPTMeghan Fisher, BSN, RNMeika Eby, MDMelanie Fluellen, LPCCMelanie Luken, LISW-SMelissa and Mikael McLarenMelissa McMillen, CTRSMelissa Winterhalter, MDMeredith Merz Lind, MDMichael Flores, PhDMichael T. Brady, MDMichelle Ross, MHA, RD, LD, ALCMike Patrick, MDMindy Deno, PT, DPTMitch Ellinger, CPNP-PCMolly Dienhart, MDMolly Gardner, PhDMonica Ardura, DOMonica EllisMonique Goldschmidt, MDMotao Zhu, MD, MS, PhDMurugu Manickam, MDNancy AuerNancy Cunningham, PsyDNancy Wright, BS, RRT, RCP, AE-C Naomi Kertesz, MDNatalie DeBaccoNatalie I.
Michalsky, MDMarcel J. Casavant, MDMarci Johnson, LISW-SMarcie RehmarMarco Corridore, MDMargaret Bassi, OTR/LMaria HaghnazariMaria Vegh, MSN, RN, CPNMarissa Condon, BSN, RNMarissa E. Larouere, MBA, BSN, RNMark E. Galantowicz, MDMark Smith, MS RT R (MR), ABMP PhysicistMarnie Wagner, MDMary Ann Abrams, MD, MPHMary Fristad, PhD, ABPPMary Kay SharrettMary Shull, MDMatthew Washam, MD, MPHMeagan Horn, MAMegan Brundrett, MDMegan Dominik, OTR/LMegan FrancisMegan Letson, MD, M.EdMeghan Cass, PT, DPTMeghan Fisher, BSN, RNMeika Eby, MDMelanie Fluellen, LPCCMelanie Luken, LISW-SMelissa and Mikael McLarenMelissa McMillen, CTRSMelissa Winterhalter, MDMeredith Merz Lind, MDMichael Flores, PhDMichael T. Brady, MDMichelle Ross, MHA, RD, LD, ALCMike Patrick, MDMindy Deno, PT, DPTMitch Ellinger, CPNP-PCMolly Dienhart, MDMolly Gardner, PhDMonica Ardura, DOMonica EllisMonique Goldschmidt, MDMotao Zhu, MD, MS, PhDMurugu Manickam, MDNancy AuerNancy Cunningham, PsyDNancy Wright, BS, RRT, RCP, AE-C Naomi Kertesz, MDNatalie DeBaccoNatalie I. Rine, PharmD, BCPS, BCCCPNatalie Powell, LPCC-S, LICDC-CSNatalie Rose, BSN, RNNathalie Maitre, MD, PhDNationwide Children's HospitalNationwide Children's Hospital Behavioral Health ExpertsNeetu Bali, MD, MPHNehal Parikh, DO, MSNichole Mayer, OTR/L, MOTNicole Caldwell, MDNicole Dempster, PhDNicole Greenwood, MDNicole Parente, LSWNicole Powell, PsyD, BCBA-DNina WestNkeiruka Orajiaka, MBBSOctavio Ramilo, MDOliver Adunka, MD, FACSOlivia Stranges, CPNP-PCOlivia Thomas, MDOmar Khalid, MD, FAAP, FACCOnnalisa Nash, CPNP-PCOula KhouryPaige Duly, CTRSParker Huston, PhDPatrick C. Walz, MDPatrick Queen, BSN, RNPedro Weisleder, MDPeter Minneci, MDPeter White, PhDPitty JenningsPreeti Jaggi, MDRachael Morocco-Zanotti, DORachel D’Amico, MDRachel Schrader, CPNP-PCRachel Tyson, LSWRajan Thakkar, MDRaymond Troy, MDRebecca Fisher, PTRebecca Hicks, CCLSRebecca Lewis, AuD, CCC-ARebecca M. Romero, RD, LD, CLC Reggie Ash Jr.Reno Ravindran, MDRichard Kirschner, MDRichard Wood, MDRobert A. Kowatch, MD, Ph.D.Robert Hoffman, MDRochelle Krouse, CTRSRohan Henry, MD, MSRose Ayoob, MDRose Schroedl, PhDRosemary Martoma, MDRoss Maltz, MDRyan Ingley AT, ATCSamanta Boddapati, PhDSamantha MaloneSammy CygnorSandra C.
Rine, PharmD, BCPS, BCCCPNatalie Powell, LPCC-S, LICDC-CSNatalie Rose, BSN, RNNathalie Maitre, MD, PhDNationwide Children's HospitalNationwide Children's Hospital Behavioral Health ExpertsNeetu Bali, MD, MPHNehal Parikh, DO, MSNichole Mayer, OTR/L, MOTNicole Caldwell, MDNicole Dempster, PhDNicole Greenwood, MDNicole Parente, LSWNicole Powell, PsyD, BCBA-DNina WestNkeiruka Orajiaka, MBBSOctavio Ramilo, MDOliver Adunka, MD, FACSOlivia Stranges, CPNP-PCOlivia Thomas, MDOmar Khalid, MD, FAAP, FACCOnnalisa Nash, CPNP-PCOula KhouryPaige Duly, CTRSParker Huston, PhDPatrick C. Walz, MDPatrick Queen, BSN, RNPedro Weisleder, MDPeter Minneci, MDPeter White, PhDPitty JenningsPreeti Jaggi, MDRachael Morocco-Zanotti, DORachel D’Amico, MDRachel Schrader, CPNP-PCRachel Tyson, LSWRajan Thakkar, MDRaymond Troy, MDRebecca Fisher, PTRebecca Hicks, CCLSRebecca Lewis, AuD, CCC-ARebecca M. Romero, RD, LD, CLC Reggie Ash Jr.Reno Ravindran, MDRichard Kirschner, MDRichard Wood, MDRobert A. Kowatch, MD, Ph.D.Robert Hoffman, MDRochelle Krouse, CTRSRohan Henry, MD, MSRose Ayoob, MDRose Schroedl, PhDRosemary Martoma, MDRoss Maltz, MDRyan Ingley AT, ATCSamanta Boddapati, PhDSamantha MaloneSammy CygnorSandra C. Kim, MDSara Bentley, MT-BCSara Bode, MDSara Breidigan, MS, AT, ATCSara N. Smith, MSN, APRNSara O'Rourke, MOT, OTR/L, Clinical LeadSara Schroder, MDSarah A. Denny, MDSarah Cline, CRA, RT(R)Sarah Driesbach, CPN, APNSarah GreenbergSarah Hastie, BSN, RNC-NIC Sarah Keim, PhDSarah MyersSarah O'Brien, MDSarah SaxbeSarah Schmidt, LISW-SSarah ScottSarah TraceySarah VerLee, PhDSasigarn Bowden, MDSatya Gedela, MD, MRCP(UK)Scott Coven, DO, MPHScott Hickey, MDSean EingSean Rose, MDSeth Alpert, MDShalini C. Reshmi, PhD, FACMGShana Moore, MA, CCC-AShannon Reinhart, LISW-SShari UncapherSharon Wrona, DNP, PNP, PMHSShaun Coffman PT, DPT, OCSShawn Pitcher, BS, RD, USAWShawNaye Scott-MillerShea SmoskeSheena PaceSheila GilesShelly BrackmanSimon Lee, MDStacy Ardoin, MDStacy Whiteside APRN, MS, CPNP-AC/PC, CPONStefanie Bester, MDStefanie Hirota, OTR/LStephanie Burkhardt, MPH, CCRCStephanie CannonStephanie Santoro, MDStephanie Vyrostek BSN, RNStephen Hersey, MDSteve Allen, MDSteven C. Matson, MDSteven Ciciora, MDSteven CuffSuellen Sharp, OTR/L, MOTSurlina AsamoaSusan Colace, MDSusan Creary, MDSwaroop Pinto, MDTabatha BallardTabbetha GrecoTabi Evans, PsyDTabitha Jones-McKnight, DOTahagod Mohamed, MDTamara MappTammi Young-Saleme, PhDTaylor Hartlaub, MD, MPHTerry Barber, MDTerry Bravender, MD, MPHTerry Laurila, MS, RPhTheresa Miller, BA, RRT, RCP, AE-C, CPFTThomas Pommering, DOTiasha Letostak, PhDTiffanie Ryan, BCBA Tim RobinsonTim Smith, MDTimothy Cripe, MD, PhDTimothy Landers PhD RN APRN-CNP CIC FAANTracey L.
Kim, MDSara Bentley, MT-BCSara Bode, MDSara Breidigan, MS, AT, ATCSara N. Smith, MSN, APRNSara O'Rourke, MOT, OTR/L, Clinical LeadSara Schroder, MDSarah A. Denny, MDSarah Cline, CRA, RT(R)Sarah Driesbach, CPN, APNSarah GreenbergSarah Hastie, BSN, RNC-NIC Sarah Keim, PhDSarah MyersSarah O'Brien, MDSarah SaxbeSarah Schmidt, LISW-SSarah ScottSarah TraceySarah VerLee, PhDSasigarn Bowden, MDSatya Gedela, MD, MRCP(UK)Scott Coven, DO, MPHScott Hickey, MDSean EingSean Rose, MDSeth Alpert, MDShalini C. Reshmi, PhD, FACMGShana Moore, MA, CCC-AShannon Reinhart, LISW-SShari UncapherSharon Wrona, DNP, PNP, PMHSShaun Coffman PT, DPT, OCSShawn Pitcher, BS, RD, USAWShawNaye Scott-MillerShea SmoskeSheena PaceSheila GilesShelly BrackmanSimon Lee, MDStacy Ardoin, MDStacy Whiteside APRN, MS, CPNP-AC/PC, CPONStefanie Bester, MDStefanie Hirota, OTR/LStephanie Burkhardt, MPH, CCRCStephanie CannonStephanie Santoro, MDStephanie Vyrostek BSN, RNStephen Hersey, MDSteve Allen, MDSteven C. Matson, MDSteven Ciciora, MDSteven CuffSuellen Sharp, OTR/L, MOTSurlina AsamoaSusan Colace, MDSusan Creary, MDSwaroop Pinto, MDTabatha BallardTabbetha GrecoTabi Evans, PsyDTabitha Jones-McKnight, DOTahagod Mohamed, MDTamara MappTammi Young-Saleme, PhDTaylor Hartlaub, MD, MPHTerry Barber, MDTerry Bravender, MD, MPHTerry Laurila, MS, RPhTheresa Miller, BA, RRT, RCP, AE-C, CPFTThomas Pommering, DOTiasha Letostak, PhDTiffanie Ryan, BCBA Tim RobinsonTim Smith, MDTimothy Cripe, MD, PhDTimothy Landers PhD RN APRN-CNP CIC FAANTracey L. Sisk, RN, BSN, MHATracie Rohal RD, LD, CDETracy Mehan, MATravis Gallagher, ATTrevor MillerTria Shadeed, NNPTyanna Snider, PsyDTyler Congrove, ATValencia Walker, MD, MPH, FAAPVanessa Shanks, MD, FAAPVenkata Rama Jayanthi, MDVidu Garg, MDVidya Raman, MDW. Garrett Hunt, MDWalter Samora, MDWarren D. Lo, MDWendy Anderson, MDWendy Cleveland, MA, LPCC-SWhitney McCormick, CTRSWhitney Raglin Bignall, PhDWilliam Cotton, MDWilliam J. Barson, MDWilliam Ray, PhDWilliam W. Long, MD
Sisk, RN, BSN, MHATracie Rohal RD, LD, CDETracy Mehan, MATravis Gallagher, ATTrevor MillerTria Shadeed, NNPTyanna Snider, PsyDTyler Congrove, ATValencia Walker, MD, MPH, FAAPVanessa Shanks, MD, FAAPVenkata Rama Jayanthi, MDVidu Garg, MDVidya Raman, MDW. Garrett Hunt, MDWalter Samora, MDWarren D. Lo, MDWendy Anderson, MDWendy Cleveland, MA, LPCC-SWhitney McCormick, CTRSWhitney Raglin Bignall, PhDWilliam Cotton, MDWilliam J. Barson, MDWilliam Ray, PhDWilliam W. Long, MD
How to Treat a Stuffy Nose in Babies and Toddlers
Written by Heidi Godman
Your little one is congested. What should you do?
In a child age 3 or under, this can be a challenge. For starters, it’s not always obvious what’s causing that stuffy nose. Infants and toddlers often catch colds because they are just starting to build up their immunity to common viruses. But there are many other potential causes of congestion.
You’re also limited by the treatments that are OK to use in children younger than 4. You shouldn’t turn to cold medicines for relief. They can be dangerous for infants and toddlers.
You shouldn’t turn to cold medicines for relief. They can be dangerous for infants and toddlers.
Fortunately, there are plenty of safe and effective treatments that you can try.
The First Step
Before you or your pediatrician can decide on a treatment plan, you need to know what’s causing that stuffy nose. And there are many possible causes.
Nasal congestion happens when blood vessels and tissue in the nasal cavity fill up with too much fluid. It can make it hard to sleep and lead to problems like a sinus infection (sinusitis). Your baby may also have trouble feeding if they are congested.
The color of mucus doesn't reveal whether it's a viral or bacterial infection.
The cause of congestion could instead be an allergy, which would require a doctor visit and possibly an allergy test. Congestion can even happen if a piece of food or another object gets lodged in your child’s nose. This, too, needs a visit to the emergency room or your pediatrician. Don’t try to remove anything but mucus from your baby’s nose on your own.
Sometimes, congestion may be a sign of a more serious problem. A stuffy nose due to a cold can often be treated with saline drops, time, and some TLC. If there are other symptoms, especially a fever and thick, yellow mucus, call your pediatrician as soon as possible.
Safe Treatments
One of the safest and most effective ways to help clear a baby’s congestion is with a saline (salt water) spray or nose drops. These products are available without a prescription.
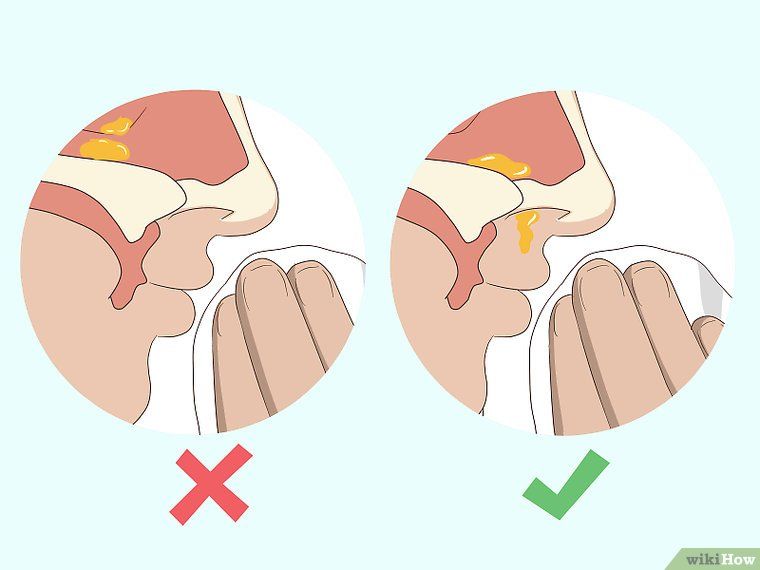
If you use drops, place two drops in each nostril to loosen the mucus inside. Then use a suction bulb immediately afterward to withdraw the saline and mucus. You can place a rolled up towel under your baby’s shoulders so you can gently tilt the head back a little to make sure the drops get up into the nose.
Squeeze the bulb before you place it in the nose. That way, when you release the bulb, it will pull out mucus from inside. If you squeeze when the bulb is already inside a nostril, it will give off a puff of air that could push the mucus farther into the nasal cavity.
Squeeze out any mucus inside the bulb onto a tissue.
Do this about 15 minutes or so before you feed your child and before bedtime. This will help your baby breathe more easily when they nurse, take a bottle, or go down to sleep.
Some saline solutions also contain medicine. Avoid these. Plain saline drops or sprays will work fine. Just make sure to wash and dry the suction bulb after each use.
Steamy Solutions
There are other ways to moisten the nasal passages.
A vaporizer or humidifier that releases a cool mist into the room is usually safe, as long as you keep it out of your baby’s reach. Place it close enough so that the mist reaches your baby while they sleep, or while you’re in the room together snuggling or playing.
To avoid mold and bacteria growth, change the water every day, and clean and dry the vaporizer, according to the machine’s instructions.
You may also try this tried-and-true solution: Take your baby into the shower. Let your shower and bathroom get nice and steamy while you hold your baby close for a few minutes. This can help to clear your baby’s head before bedtime.
This can help to clear your baby’s head before bedtime.
Don’t use hot water in a humidifier, since it can cause burns.
3 More Tips
Follow some of these other steps to help clear up your baby’s stuffy nose:
- Place a pillow under the mattress so there’s a slight angle with your child’s head higher than the feet. That may help drain mucus out of the sinuses. If your child is still a baby in a crib, don’t do this. You should keep pillows and other things out of their sleeping area to lower the risk of SIDS (sudden infant death syndrome). Most pediatricians recommend doing so until your child is 2 years old.
- Encourage your child to drink more water. Fluids help thin mucus, but don’t force it. Even if your child just sips some more water throughout the day, that will help.
- If your little one is old enough, teach them to blow their nose. To show them how, exhale through your own nose. Place a tissue by your nostrils so your baby can see the air move the tissue as you exhale.
 Ask them to blow into a tissue the same way.
Ask them to blow into a tissue the same way.
Nasal congestion in a child - City Hospital No. 12, Barnaul: articles
Nasal congestion in children is often accompanied by headaches, sleep disturbance, refusal to eat, irritability, tearfulness, irritability. The inability to breathe freely through the nose can negatively affect your child's mood and well-being.
Chronic conditions disrupt the functioning of the respiratory and circulatory systems and cause oxygen starvation of the brain.
Types of congestion
about the nature of this
Nasal congestion in children may be acute or chronic. The first is sudden nasal dyspnea, which is most often caused by viruses.
Stable or chronic runny nose may be caused by chronic otorhinolaryngological disease or allergies. Nasal congestion is observed continuously for more than 2 months, while there is a period of improvement and a period of exacerbation.
Time of onset
Rhinitis in children is morning and evening. The first type of appearance is most often associated with allergic reactions and conditions in which the air in the room is very dry.
The first type of appearance is most often associated with allergic reactions and conditions in which the air in the room is very dry.
Breathing is normal during the day and is a common symptom when nasal congestion occurs at night. This is due to the fact that the secretion of mucus is active during the day, and when the child sleeps, mucus secretions come out less frequently, resulting in increased swelling of the mucous membranes.
Nocturnal nasal congestion is also common in children with postnasal sinusitis and adenoiditis. In such cases, a large amount of secretions is formed, which flow down the back of the pharynx. When you lie on your side, mucus accumulates in your throat, which swells and inflames the lining of your throat, causing you to cough.
There are several types of nasal congestion in children:
- Infectious rhinitis. Infectious rhinitis. A feature of this type of rhinitis is the abundant distribution of SONO.
- Allergic rhinitis.
 Allergens cause inflammation of the mucous membranes. Allergic reactions can be caused by dust, mold, plant pollen, animal dander, food, and medicines.
Allergens cause inflammation of the mucous membranes. Allergic reactions can be caused by dust, mold, plant pollen, animal dander, food, and medicines. - Traumatic rhinitis. Swelling of the nasal mucosa is caused by a foreign object entering the nasal cavity.
- Vasomotor rhinitis. Accompanied by nasal congestion, runny nose, sneezing, reduced sense of smell, sleep disturbance, headache. It develops due to reduced blood supply to the vessels of the mucous membrane against the background of prolonged use of vasoconstrictive eye drops.
The normal nose of a child aged 10 to 12 weeks does not have nasal congestion. Only a large amount of clear mucus is excreted from the nasal cavity. Due to the large number of membranes, the baby will begin to breathe through the mouth, so it is necessary to remove them in a timely manner with a nasal aspirator.
Possible causes
A condition caused by swelling of the nasal mucosa. This is not an independent disease, but occurs as a result of inflammation caused by infection or exposure to irritants, such as allergens.
Nasal congestion in children is most commonly caused by acute respiratory infections or allergic reactions.
The inflammatory process causes dilation of blood vessels in the nasal passages and swelling of the mucous membranes, which leads to narrowing of the nasal passages. As a result, air becomes difficult to pass, causing nasal congestion.
The main causes of weak breathing
- Infectious diseases of the nasopharynx (nasopharyngitis, sinusitis, acute sinusitis).
- Inflammation and growth of adenoids.
- allergic disease
- Deviated septum.
- Penetration of a foreign object into the nasal cavity.
- Long-term use of vasoconstrictive eye drops.
Hypothermia, a weakened immune system, teething, dry or dusty air inhalation, and frequent antibiotic treatment can be serious contributing factors to nasal congestion.
Even if the cause of nasal congestion is known, a pediatrician should be consulted. Your doctor will select the right treatment that will help you quickly restore nasal breathing without developing side effects.
Your doctor will select the right treatment that will help you quickly restore nasal breathing without developing side effects.
Symptoms and possible complications
Stuffy nose is rarely the only complaint. As a rule, it is accompanied by the following symptoms:
- nasal catarrh
- Burning or itching in the nasal passages.
- sinus pain
- I often wake up at night.
- Increased lacrimation
- sneeze
- In the early stages of infection, in addition to the above symptoms, there are symptoms such as fever, sore throat, fatigue, drowsiness, ear congestion.
Late treatment of chronic rhinitis and acute inflammatory processes in the nose increases the likelihood of complications.
Acute or chronic sinusitis, including sinusitis.
- Acute or chronic otitis media Acute or chronic otitis media Acute or chronic otitis media Acute or chronic otitis media Acute or chronic otitis media
- Mastoiditis - inflammation of the mastoid process behind the ear.

- Hearing loss, acute or chronic hearing loss, acute or chronic hearing loss, hearing loss.
- Pharyngitis, laryngitis, tonsillitis
- bronchitis, pneumonia
- eyelid inflammation
- Meningitis?
- decreased sense of smell
- Chronic headache, drowsiness/loss of appetite, weakness, lethargy.
- diseases of the circulatory system
- If the state of not breathing through the nose continues for a long period of time, it will adversely affect the functioning of the whole organism, as well as the mind and emotions.
Danger of prolonged runny nose in a child
Permanent stagnation is dangerous in the long term in the form of cardiovascular diseases that develop in situations of oxygen starvation of tissues. Your nose can't breathe, you can't get enough sleep, you can't focus on your studies, you're distracted and restless, and you're at increased risk of chronic respiratory disease. The ongoing inflammation of the nose leads to an increase in the adenoids, children often develop acute respiratory viral infections, weakened local and systemic immunity.
Infants and young children are at risk of deviated septum, pathological changes in the orbit, etc.
Severe nasal congestion in children not only interferes with normal breathing, but also interferes with eating, sleeping and playing. There are ways to improve your child's condition, but you won't be able to get normal nasal breathing back unless the underlying cause is addressed first.
How to alleviate the condition of the child's body with a cold?
Tips for clearing a stuffy nose at home.
It is good to suckle your baby. If you have a runny nose, it should always be removed from the nasal passages. Failure to do so creates an environment conducive to the growth of pathogenic bacteria.
Children who cannot blow their nose may want to flush their nose with saline or saline and use a nasal aspirator to suck up the mucus. Some mothers take mucus with a pear, but this method is not sterile and therefore unsafe. If your child already blows his nose, flush his nasal passages first to loosen the mucus.
Treatment of nasal congestion in children depends on the cause, some treatments are effective for some types of rhinitis, others are contraindicated for others, so you cannot treat it yourself. If you don't know how to properly treat a runny nose, it's a good idea to talk to your pediatrician.
What should not be done in case of a cold in children?
If you have a stuffy nose, do not:
For bacterial rhinitis, heat treatments such as steam inhalation are given.
- Rinse the nasal cavity with a syringe or blower, you can use a special spray based on sea water and saline.
- At the same time, it can cause otitis media, so make sure both nostrils are tight or too much.
- To treat children under two years of age with nasal drops, nasal nasal treatment.
- Use antibiotic infusions and disinfectants without a doctor's prescription.
- Independently give solution for the treatment of baby's silly nose and use breast milk, garlic juice, onion, aloe and kalancho.

- Use blood vessels for 5 days or more.
- Vastring Agent eye drops effectively relieve stuffy nose, but are addictive to dry nasal mucosa. Prolonged use may cause rhinitis medications, so be careful. When choosing a medicine, think about the age of the child.
Treatment should begin with the identification and removal of the cause. To investigate the cause of the disease, tests such as nasal mucosal patterns, clinical blood tests, allergy tests, etc. may be ordered.
How to deal with the problem
Vastroctomy is the most effective treatment for a foolish nose. Use after rinsing the nasal cavity with seawater, saline, normal saline, etc.
In case of a goofy nose and due to a bacterial infection, antibiotics are used in addition to blood vessel eye drops. There are several types of external antibacterial drugs. System notebooks are only prescribed if there are complications such as sinusitis, otitis media, and tonsillitis.
Allergic nasal congestion is treated with antihistamines. Be sure to protect your child from contact with allergens. Otherwise, breathing disorders will not disappear anywhere.
Parents should not forget that healthy nasal breathing is the key to respiratory and cardiovascular health and a strong immune system. Inflammation of the nose is important to treat at an early stage, and it does not become a serious chronic disease. If you start having problems with your nose, see a doctor immediately.
Miracle Doctor clinic has a specialist with more than 30 years of experience. Registering a pediatrician is possible on any day. We work 7 days a week. Call the phone number listed on the homepage or apply online.
Today I will talk about the structure and functions of the child's nasal cavity, how to use nasal tablets correctly, in which cases it is necessary and in which cases it is not necessary to be drug therapy.
Therefore, great pediatricians at 19century knew it. " Children are not a copy for adults. "Childhood" is a special state of growing beings and has some characteristics. There is.
" Children are not a copy for adults. "Childhood" is a special state of growing beings and has some characteristics. There is.
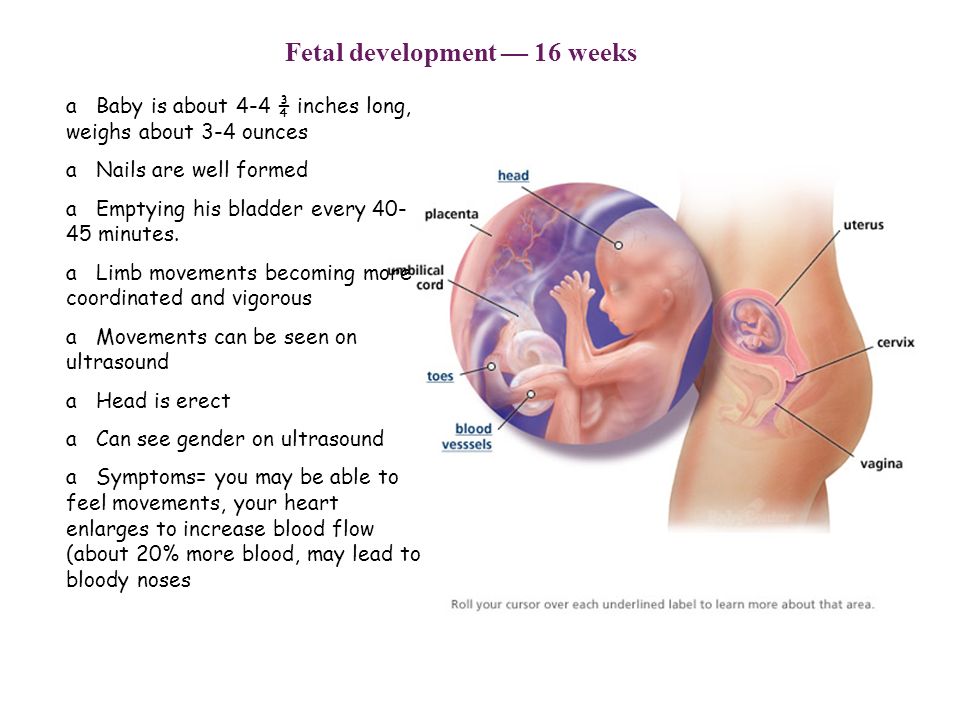
Thus, the mucous membrane of the nasal cavity is richer in blood vessels compared to the mucous membrane of adults, and it swells quickly when there is something uncomfortable. The width of the blood vessels is wider than adults, so you can quickly warm the air. The mucous glands that protect themselves from injury are small, soft, and easily damaged. The nasal cavity of the child has a narrow nasal cavity, which is also an air replacement disorder and due to inflammation of the nasal mucosa, accumulation of secretions and decrease in excretion. The child has two out of three out of three, compared to adults. Yes, and not only does the baby know how to bite his nose, but he also has no muscles.
The nasal cavity takes only four years to form. The volume of the nasal cavity is about 2.5 times with age. Children's upper respiratory tract often merges with inflammation of the middle ear.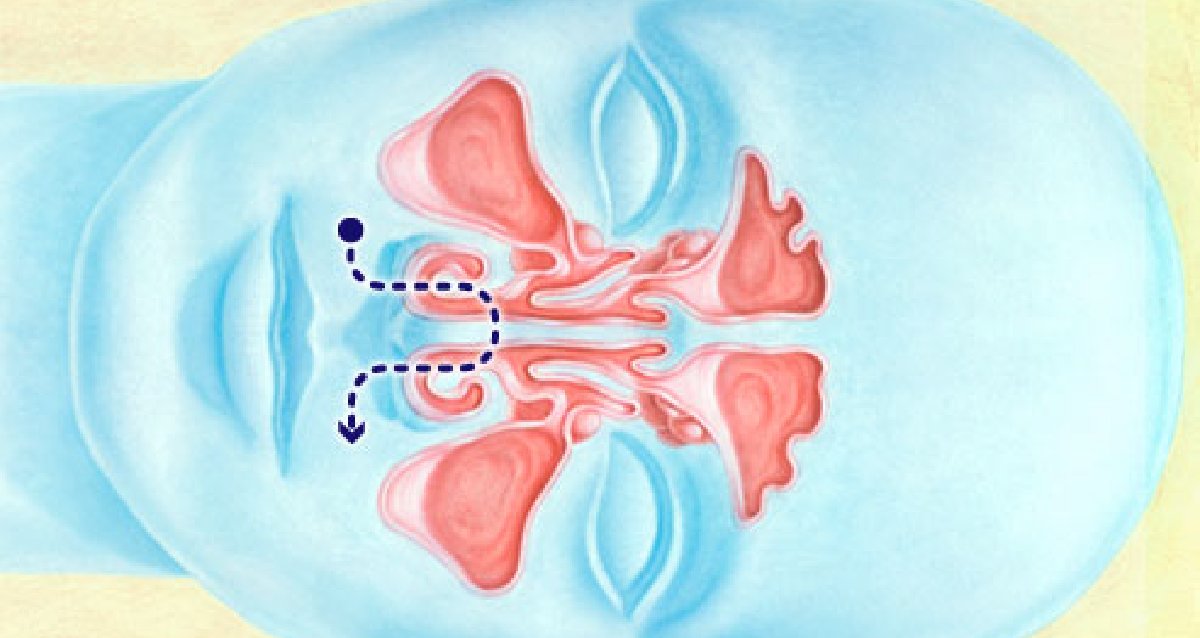 This is because it is easy to get infected into the wide and short tube called the Anop Tube that connects the nasopharynx and the middle ear. This is a negative point that adults do not have. However, there are advantages: small children are formed only after 5-7 years and 10 years after 5-7 years and 10 years, and not Tinaritis, pre-livedovitis and sinuses.
This is because it is easy to get infected into the wide and short tube called the Anop Tube that connects the nasopharynx and the middle ear. This is a negative point that adults do not have. However, there are advantages: small children are formed only after 5-7 years and 10 years after 5-7 years and 10 years, and not Tinaritis, pre-livedovitis and sinuses.
An otolaryngologist says that women who have children should teach their children how to breathe through the nose. Of course, the mouth is not meant for breathing. The air that passes through the nasal cavity is heated, watered and washed, and because of the special structure of the mucous membrane.
Air sucked from nasal pressure on the nasal mucosa stimulates respiratory reflex and expands the chest more than when sucking from the mouth.
Rohto Pharmaceutical Breath Causes
Oxygen starvation
- Phenomenon that catches in the box of the chest and skull.
- Chest deformity, hearing loss.

- Ethitis common, bronchitis.
- Mucus in the mouth dries up.
- Inappropriate (high) development of hard piles.
- Normal position of the nasal septum and the shape of the lower jaw.
- If you do not breathe through your nose, air will not enter your sinuses. Since nature does not allow a vacuum, there is a special thing called the adenoid organization. Even if it is removed, it often grows back because the nose has not yet breathed.
No mother wants their parents to hurt their children, but not everyone is willing to put in the time, effort and nerves and focus on it. Unfortunately, many parents hope for the wonderful treatment that doctors give, that is, special eye drops that will make your child's nose healthy in a few days. Unfortunately, such a drop has not yet come out, the nature of people has not changed much in the last century, and there are more and more factors that impair health, so it will not appear at the moment.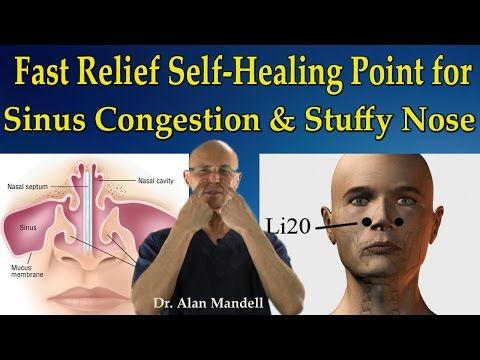 Correctly.
Correctly.
I know that acute viral diseases can be cured in seven days if treated within one week if treated. Why? Are our efforts and material costs useless? Never! ? In fact, you must go through any stages of inflammation, so you need time for your body to build up the power and overcome the infection. By using drugs that suddenly cut off the inflammation process, he brings in a nature that doesn't like violence, you know.
Blood Vessel Contractor Waterfall may be converted and may not function normally. In other words, oxygen and nutrients are not sent to the mucous membranes, and they cannot be protected from infections, which always linger, thicken and enter the nasal cavity regularly. Thus, our children have a recurrence of the upper respiratory tract or chronic diseases that perform the most important functions that represent a preliminary area and a barrier to further infection in the body.
Main conclusion derived from the above.
Children should breathe through their nose
- Although this does not apply in the natural world, attention must be paid to everything that happens in the body, including the inflammatory process that helps infectious diseases.

- Swelling of the baby's nasal mucosa is also due to causes that are not necessarily associated with infectious diseases (the same crying, rapid temperature change, allergic reaction, etc.), so the baby is simply with low resistance. You just have to walk around and start breathing with your mouth. What will happen in the future as mentioned above. Therefore, it is necessary to perform breathing exercises with children every day (!).
Let's explain the most effective and very popular nasal preparations.
The action of the drug of the pharmaceutical group is to shrink the blood vessels in the nasal cavity so that it can reduce nasal congestion and facilitate nasal breathing. It must be understood that if you inoculate a blood vessel controlled drug, this will not happen. Only temporarily relieves the symptoms of the disease.
In addition, the so-called "medicated rhinitis" stagnant discharge due to vasoconstriction and increased blood flow and renewal of the discharge, using nasal preparations in vascular contractors for a long period of time.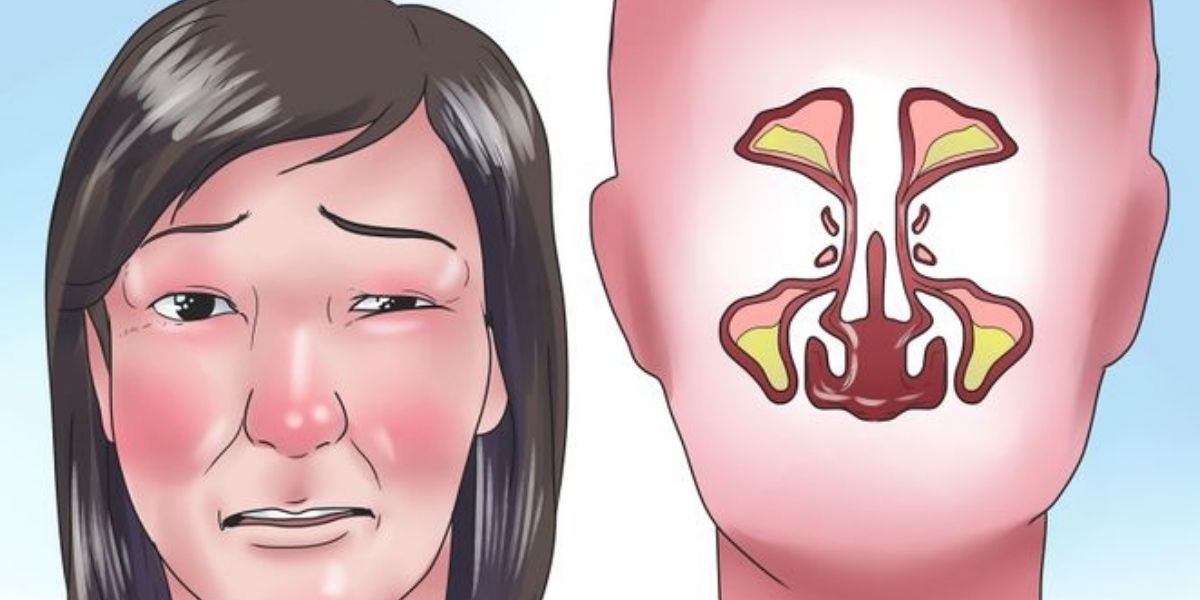 You must remember that this is a phenomenon. Relapse nasal stuffy nose treatment! In addition, prolonged use causes atrophy of the nasal mucosa.
You must remember that this is a phenomenon. Relapse nasal stuffy nose treatment! In addition, prolonged use causes atrophy of the nasal mucosa.
To understand the huge number of pharmaceuticals in the pharmaceutical network, we recommend that you pay attention not only to the name of the drug, but also what substances are based on. A similar name may be a completely different derivative of the substance.
Short-term action of medium-active agents B is a drug for 4-6 hours, with the main component of naphazoline (sanulin: from 0.05% to 0.1%, nafthadine: from 0.05% to 1 year). Naphazorin products can only be used four times a day in principle. The main disadvantages of Naphazoline are toxic to the epithelial body, which can often cause poisoning. Make sure you don't use it as much as possible in baby practice
Nasal vasoconstrictor drops are divided according to the duration of their action
- There are also short-term medicines (vibration drops from birth, nazol-2 years, nazor-2 months).
 Child care is more desirable to use phenylfrine. In addition to crossing the mucosa, it is also important to withdraw quickly. This can minimize the risk of poisoning by children.
Child care is more desirable to use phenylfrine. In addition to crossing the mucosa, it is also important to withdraw quickly. This can minimize the risk of poisoning by children. - Xylometazoline medium type drug (Galazolin: 0.05%-2 years, 0.1-6 years, olibin drip agent. 0.05%-6 years, from 0.1%-6 years, from farmeisolin with spray-6 years: 0.05%-6 months, 0.1%-6 years, Thaizinxiro, Rhino Stop, xylene eye spray: 0.05%-2 years, 0.1%-6 years Folk drops: 0.05 %-3 months to 6 years, 0.1–6 years). The effect of such a drug is from 8 to 10 hours, and its effect is much higher than that of drugs based on napazoline. A course of treatment with xylometazoline is not recommended for more than 7 days.
- Long-acting, twice a day - Oxymetazoline (Nazivin, Rinazolin - 0.01% from birth, 0.025% from 1 year to 6 years, 0.05% from 6 years, Nazol, Knoxspray - up to 6 years). Such funds are not recommended to be used more than twice a day, since a prolonged spasm of the vessels of the nasal mucosa will destroy their function.
 The duration of treatment with oxymetazoline is not more than 3-5 days. These drugs are prescribed with caution to pregnant women, patients with renal insufficiency and diabetes mellitus, as well as children under the age of 1 year.
The duration of treatment with oxymetazoline is not more than 3-5 days. These drugs are prescribed with caution to pregnant women, patients with renal insufficiency and diabetes mellitus, as well as children under the age of 1 year. - Andrianol (containing two vasoconstrictors, lerimazoline and phenylephrine): from 3 years of age, 1-2 drops 3-4 times a day. Rhinospray Plus (Tramazolin): sprayed from 6 years of age.
- Many cold remedies containing essential oils have vasoconstrictive, antispasmodic, mild antiseptic and anti-inflammatory properties. The main advantage of such drugs is that, as a rule, they are not habitogenic and do not aggravate the condition of the nasal mucosa, but contribute to its restoration. Also, drugs in this group are able to neutralize most viruses and bacteria. These drugs are not approved for use in young children.
Preparations for the common cold with essential oils
Specifically:
Pinosol (oil of mountain pine, mint, eucalyptus, vitamin E) from 3 years.
- Eucacept (spruce oil, mint, eucalyptus, vitamin E) from 2 years.
- Nazol Advance (oxymetazoline hydrochloride, camphor, menthol, eucalyptol) - from 6 years of age, no more than 3 days.
- Otrivin Menthol, Eucalyptus nasal spray 0.1% - from 6 years.
- Vita On Karabaeva (based on soy oil), Vita On Lux (based on olive oil, for sensitive skin): Medicinal plants (mint, chamomile, wormwood, St. John's wort, wild rose, thyme, straw, calendula, cumin, fennel, ferrandina, pine, buds) oil extract.
- Tuina oil. In the 16th century, the French kings called it the "tree of life". In the treatment of bronchitis, colds, otitis media, stomatitis and arthritis, tree ear oil was used to increase overall tone, reduce fatigue and quickly restore strength. Instead of 100% pure essential oils, you should use 15% homeopathic, Tsuyaedas-801 or Tsuya DN oil, which can be bought at a pharmacy. Contraindication is acute rhinitis. These drugs are indicated for subacute, chronic rhinitis, adenoids.

- Recently, not only vasoconstrictor, but also combined preparations with antiallergic action, thinning action, antibacterial action, etc. have become popular. Let's consider some of them.
Antihistamines are often added to enhance the vasoconstrictor action. Perfectly relieves swelling and symptoms of allergic rhinitis. What are combined agents?
Antihistamine nasal drops
Vibrosil
- Sanorin Analergin (naphazoline nitrate - 2.5 mg, anthrazoline mesylate - 50 mg - from 16 years of age and older).
- It is not recommended to use such preparations for more than 1 week. An overdose may cause drowsiness and lethargy. In this regard, such funds are recommended to be planted at night.
Some cold medicines have antibacterial and antiseptic properties.
Antibacterial, antimicrobial nasal drops
Polydex (neomycin, polymyxin B - antibiotic, dexamethasone - hormonal, phenylephrine - vasoconstrictor) - from 2. 5 years.
5 years.
- Isofura nasal drops - contains AB aminoglycosides.
- Nasal medicine that dilutes mucus
Synfort (European extract of cyclamen) causes reflective secretions throughout the nasal mucosa and sinuses. The stimulated reflective reaction is immediately expressed and lasts about 30-60 minutes. After stimulating the formation of the nasal cavity, this remedy has a local redeeming effect by a remarkable dehydration of the mucous membrane. The fistula between the nasal cavity and the sinus cavity expands, and the sinuses and pus are discharged into the nasopharynx. From the age of 12, once a day, every day.
- Rinoflum chyl (100 ml acetylocysteine-salasal, chymin heptane sulfate with vascular contraction) is recommended for use on the third day of rhinitis. There is no age limit in the instructions.
- Salt Salt Water has a therapeutic effect by flushing out foreign matter such as mucus, allergens and microorganisms in the nasal cavity.
 The mucous membrane is gently rinsed and the nasalharingology is washed with a special solution based on salt and sea water. It contains many chemical elements, preventing further progress in the processes of inflammation and reduces the strength of the allergic reaction.
The mucous membrane is gently rinsed and the nasalharingology is washed with a special solution based on salt and sea water. It contains many chemical elements, preventing further progress in the processes of inflammation and reduces the strength of the allergic reaction.
Moisturizing drops
Characteristic moisturizers are without any preparations and their effects can be observed at least after a few days. In case of severe diseases, this is not the main drug, but only in combination with other drugs.
The components of the moisturizing solution are almost the same, and it is pure sea water or classic saline. Physiomeric nasal sprays (from 2 weeks), physiomeric nasal sprays (from 2 years) are well known on the Russian market. 0.9%-tagium, 13-18-23%, different from sodium chloride to high thang.
Aqua Roll Forte (2 years), Aquamaris Strong (1 year) - the effect of these drugs is based on the law of osmotic pressure: high salt water, which is useful for suppressing swelling of the mucous membrane. Questionnaire
Questionnaire
I really like the classic cast of a-2.6% sodium chloride, which has been proven in the treatment of allergic rhinitis, nasal sinusitis, the first sign of an obsessive nose, especially when it manifests itself as an inflammation of the mucous membrane of the ar and nasopharynx. It can be used by children 3 months old. If you have had an allergic reaction in the past, you should be careful about using eucalyptus quickly.
Currently, Dead Sea and Adriatic Sea salts are on the market in various concentrations and contain, combining coarse medicines and oils. I have a group of young patients and each child must consider candidates from risk groups for allergic pathology, so I do not like to think about IBD, but I can be effective and efficient. I prescribe a group of drugs.
Below is a compound ophthalmos based on saline.
Aquamaris Plus (Deku Span Ten All) is recommended for drying mucous membranes. Dry rustling of the nose has the effect of normalizing the function of the epithelium for the body of the hair.

Rinomaris nasal preparation: Adriatic water and xylometazoline (blood vessel contractor) -0.05% from 2 years and from 0.1% to 6 years.
Snup Spray Nasal Pharmaceutical Water + Xylometazoline (blood vessel contractor) -0.05% (2 years later), 0.1% (6 years later)
Oral preparation intended for the treatment of the nose.
RINOSTOP P-SYRUP LINOSTOP T-RINOSTOP T-SYRU P-RINOSTOP T-SYROP is used for patients aged 2 to 12 years. Use per day: 5-5 years - 5 ml / 2 times, 6-10 years - 10 ml / 2 times. There are up to 5 days of courses.
Tablets 0.5 tablets are prescribed for patients aged 6 to 12 years. Up to four times a day, 12 years and older 1 table, up to four times a day.
Sinuptate-Herb (from 2 years of fall, 6 years after Drage or Table).
Dzhinnabsin - a homeopathic remedy three years ago.
Euforbium Compositum is a homeopathic spray. It is effective for the treatment of prolonged rhinitis and adenoids.
Office for the elimination of March-homeopathy in the treatment of adenoid germination
Miscellaneous drugs
Protal cel-Colloid silver solution (2% aqueous solution of silver protein).
 No age restrictions. It is recommended when a large amount of body fluid is discharged and has a "drying" effect.
No age restrictions. It is recommended when a large amount of body fluid is discharged and has a "drying" effect. - Medical care moves forward, not pharmaceutical. Recently, new brands have been released such as "Aphrin", Aphrinkle (Contains Eucalyptus/Menthol), "Moisturizing Aphrin (Allergic)" and "Esology (Infectious/Inflammatory Rhinitis Treatment)".
And, of course, the king of nasal drops can be called a group of synthetic external corticosteroids with strong anti-inflationary effects. Momesazon active ingredient: Nazonex, Decon, Erotic, etc.
From 2 year old, 1-2 s.
On the other hand, in the nerve prevention clinic in the work of setting up high-quality treatment and diagnosis based on clinical, organizational, laboratory, biochemical and serum scientific tests, forklifts have a variety of high-quality clinicians. Dressing, persistent complications, persistent complications, persistent complications, persistent complications.
A bumpy nose is a problem that everyone faces. Such diseases are always uncomfortable, causing headaches, difficulty breathing through the nose and interfering with sleep and greatly degrading the quality of life.
Such diseases are always uncomfortable, causing headaches, difficulty breathing through the nose and interfering with sleep and greatly degrading the quality of life.
And because of breathing disorders, symptoms such as rapid body fatigue, daily weakness and productivity have decreased, indicating that the brain is insufficient. Currently, there are various treatments for such diseases, but before starting treatment, it is necessary to find out the cause of the foolish nose.
Causes of a stuffy nose
There are various causes of nasal breathing difficulties, and both the common cold (SARS) and malignant exercise. In some cases, congenital characteristics may contribute to bloody blood.
Children who suffer from a labored nose have difficulty breathing and due to colds, low body temperature, upper respiratory inflammation and allergic reactions as half of regenosis.
Nasal congestion in children
Violation of air pressure in both nostrils.
- Breathing is rough.
- General temperature increase.
- Childish whimsical state, irritability.
- Squeeze or chew your nose.
- Sleeping disorder
- Children often rub their nose.
- Other cold symptoms: sore throat, cough.
- According to world literature, the problem of nasal congestion in children has increased several times over the past century, from 10% to 30%, which significantly reduces the quality of life, and in severe cases, nasal dyspnea, which makes it difficult for children to learn, is also considered an obstacle.
The main causes of nasal congestion in children are deviated septum and inflammation of the mucous membranes. In addition, the initiator of the manifestation of symptoms may be an allergy or a viral or bacterial infection. Constant nasal congestion not only causes discomfort, but can also lead to various complications, such as impaired hearing. Causes of chronic nasal congestion in children are adenoid pleural effusions, acute and chronic inflammation of the paranasal sinuses (sinusitis).
There are many possible causes of nasal dyspnea in children, but in each individual case it is necessary to identify the factors that cause persistent or intermittent nasal congestion in children. First, it makes sense to eliminate the most likely and important causes of nasal congestion in children: allergic rhinitis, rhinitis, sinusitis, adenoid hypertrophy.
The most common cause of nasal congestion without a runny nose is a complication of rhinitis (sinusitis - inflammation of the mucous membrane of the paranasal sinuses), usually due to various modifications of rhinitis in children.
Stuffy nose but no runny nose?
Chronic allergic rhinitis occurs all year round. Such reactions are caused by household allergens (dust, wool, lint). When walking in the city, the physical condition of the child noticeably improves, breathing becomes freer. This type of nasal congestion without a runny nose can be easily treated by an allergist by simply identifying and identifying the offending allergen.
Infectious rhinitis lasting 1 year is a complication of acute viral rhinitis. In this case, the immunologist will identify the pathogen and select the necessary combination of drugs.
Seasonal allergic rhinitis can cause nasal congestion without a runny nose. This is due to the flowering of some plants and occurs at the same time. This type of rhinitis is treated in the same way as allergic rhinitis all year round.
For the successful treatment of nasal congestion, first of all, it is necessary to determine the very cause of the occurrence, and for this it is necessary to conduct examinations using oropharyngoscopy, an examination of the anterior nasal cavity, and otoscopy. An x-ray (CT) of the sinuses may also be needed to check for inflammation.
Nasal congestion treatment
Our ENT and ASP Center uses a unique and effective method for the treatment of nasal congestion, providing complete hygiene and restoration of the mucous membrane of the upper respiratory tract. The cause of nasal shortness of breath can be eliminated quickly without resorting to surgical methods.
The cause of nasal shortness of breath can be eliminated quickly without resorting to surgical methods.
With the exception of anatomical abnormalities, almost all diseases are the same disease, differing only in the stage of onset. Most of the activation mechanisms of these diseases are manifested by symptoms of nasal congestion, and an infection that penetrates the mucous membrane of the respiratory tract causes degeneration and transformation of the mucous membrane, and, in addition, is involved in a decrease in local immunity.
The most effective treatment, besides surgery and obsessive nose, is drainage and mucosal rehabilitation, which contributes to the normalization of nasal breathing, and for many years at the center. We achieve results.
Apply for consultation on stupid nose
Questions from users on the home page regarding stupid nose
This is a temple, but here I read in your article that he was an adenoid, we don't have a good doctor here, he has oxygen starvation.
 As directed, but heavy drops may be prescribed.
As directed, but heavy drops may be prescribed. Alexander Priacef (Doctor of Medicine, director of the clinic): children who snore, of course, also because of Mindirina adenoma. In this process, as a result of prolonged inflammation of the lymphatic tissue, I was wisely called adenoids, because the adenoids not only became inflamed, but also blocked as immune organs and were not invalidated from the struggle for recovery. The work is not only to eliminate swelling and inflammation, but also to restore immunity. And it's not easy. Therefore, "a few drops" is not useful here! In fact, there is no such drop in the pharmacy. You need to work to improve your daily routines and immunity. This is something that can only be achieved after visiting our hospital. And this is not a matter of life (in my understanding). Many people who need treatment come from other cities and countries. We are waiting for you without worry.
Alexander Polisef, MD and chief doctor of the clinic. Dark green secretion - pus. There may be fins for seeding, there may be aggressive infections.
There may be fins for seeding, there may be aggressive infections.
What are they allergic to, most likely milk, remove milk from meals? Thanks for your reply.
Alexander Polisef, MD and chief doctor of the clinic. Green nostrils - pus and infectious diseases. Give a smear for shading. This is blood. You can immediately see shoguns, tucks and allergies.
Alexander Priacef, MD, director. Clinic. Requires adenoids, catalytic catalog pharynx, and x-slab sinus check.
Alexander Priacef, MD, director. Clinic. The teeth show it. Please rest assured that only the nasal toilet is ok.
This is a hired nose (separation) that often occurs as a symptom of existing diseases in otolaryngology. It is recognized only without other symptoms, no other symptoms, no secretions from the nasal cavity, no nasal congestion on nasal feeding), but these phenomena are more serious and combined. The onset of the disease cannot be ignored.
When an otolaryngology infection or most other diseases develop, the two processes begin simultaneously.
Main causes
This indicates that the mucous membrane is swollen and the tissue is inflamed.
- It generates abundant mucus (snot) and removes the pathogen (microorganisms) and its decomposition from the passage.
- The cause of congestion is both. And because of the edema in the internal cavity of motion, there is a mechanical stenosis. Due to copious obstruction of mucus.
In the early stages of acute respiratory infections, a runny nose (separate nose) is allowed. Mucus at this time has not yet begun to form, but after 2-3 days the clinical image is a mythical headache, an obsessive nose and a classic. Nedosya (a separate type) has always indicated another disease and requires early diagnosis and accurate treatment.
Many causes of nasal congestion without a nose have been found (project). The most common is
Deviated septum, which caused some causes (after trauma, congenital, disease). Patterns can always be and sometimes.
- Dry mucous membrane and due to excessive air drying. Allergic infectious rhinitis causes the typical swelling of the mucous membranes, but the mucus itself (snot) dries quickly and the classic clinical image is washed away. Similar phenomena are often observed at the onset of sinusitis, such as sinusitis and a feeling of obstruction.
- There are foreign substances in the injury and internal cavity. EEDEMA develops as a response to a stimulus when the mucosa is affected by foreign matter or the compartment is compromised.
- Medicinal nasoli t-response to abuse of blood vessels (eye drops, ointments).
- Changes in hormones common in pregnant and lactating women. If a pregnant woman has such a complaint, it can be considered a symptom of steroid metabolism. In rare cases, mucous membranes can lead to the appearance of endocrine diseases such as diabetes, not only the balance of hormones, but also metabolic disorders.
- The onset of rhinitis is limited to the internal pharynx after underwear formed departure.
- Polypi s is a benign new creature that mechanically restricts the nasal cavity.
- Adenoids and other pathological processes in the throat.
- The cause of the obsessive nose is possible if it is not a full nose (separate type). The patient will immediately be tested by an otolaryngologist to establish a definite diagnosis and prescribe targeted treatment.
Stuffy nose without hereditary nose (separation) cannot be treated with appropriate treatment if the cause is not determined. In some cases, the cause, such as the curvature of the nasal septum, may be obvious, or a clinical and instrumental accurate test that is only performed in our hospital.
Treatment
At the Kolenenko clinic, the doctor collects the mixture, examines the condition and characteristics of the problem and conducts the first consultation. Among them, organic methods are often used.
Internal and Posterior Nasal Speculum Test: Examine the internal oral and mucous membranes using a special device, the nasal speculum.
- Endoscopy - outside of tests, it may be possible to simultaneously perform medical practices such as polyp screening and removal of foreign matter at the same time.
- Our doctor can be appointed in other diagnostic methods.
Mucous Membrane Patch
- X-ray, Ct.
- Allergy testing
- Physicians choose the method of tumor testing and diagnosis based on patient complaints, general clinical images, and data at the first consultation.
Treatment for runny nose (separate nose) without goofy nose varies depending on the condition. During pregnancy, a difficult nose, unlike the normal one, is temporary and is considered temporary, and there is no need for special treatment. For allergic rhinitis, the treatment is an anti-allergic and antihistamine prescription and the allergy department should be consulted. Foreign substances are subject to compulsory exclusion. Approaches and treatment for patients are prescribed individually.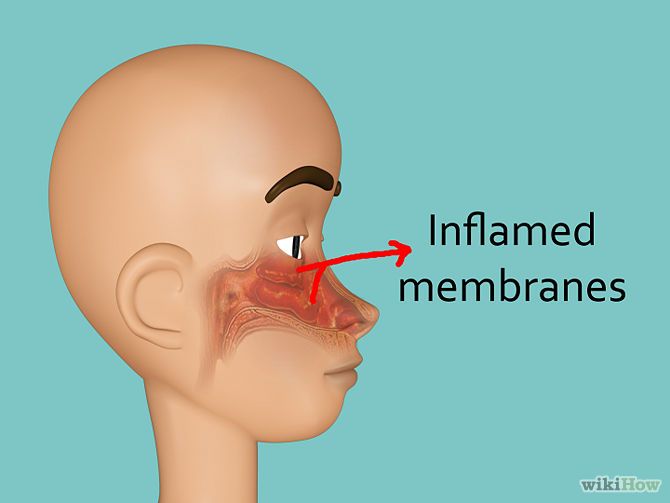 Only an otolaryngologist can make a diagnosis on the basis of a diagnostic test carried out in the clinic and prescribe the appropriate treatment in a timely manner.
Only an otolaryngologist can make a diagnosis on the basis of a diagnostic test carried out in the clinic and prescribe the appropriate treatment in a timely manner.
If you do not treat the contracted nose for a long time, you will experience unpleasant results such as atrophy of the mucous membrane, elimination of odor and complete absence of mucus. Allergic rhinitis can cause bronchial asthma, polyps can cause sinusitis, pre-list, for meningitis, otitis media and hearing loss.
Why visit our clinic?
If you are not a doctor, you will not be able to perform targeted treatment, fully restore nasal breathing and eliminate the possibility of complications. I can't afford to be late. The sooner you consult with your doctor, the more likely you are to complete your treatment without complications.
Nasal medicine for children
Persistent nasal congestion in a child: what to give for a runny nose if the nose is stuffy
Co-author, editor and medical expert - Maximov Alexander Alekseevich.
Last updated: 09/28/2022
Number of views: 340,297.
Average reading time: 5 minutes.
Contents:
Causes of the disease
How to relieve nasal congestion in a child
Parents often face the problem of difficulty in nasal breathing in babies 3.4 due to mucosal edema 4 . Nasal congestion in a child may also occur without signs of a runny nose 5 . Such a state not only leads to a deterioration in well-being and a bad mood, but also causes various consequences 3,4,7 . When the nose does not breathe, the child's sleep is disturbed 3.7 and appetite 3.4 , there is a threat of inflammation of the pharynx and bronchi due to inhalation of cold air through the mouth 4 . Infants may develop life-threatening sleep apnea 9 . Therefore, it is necessary to remove nasal congestion in a child, including for safety reasons.
Up to content
Causes of the disease
At present, acute respiratory infections 2 and allergic reactions 8 are considered the most common causes of a runny nose with nasal congestion in a child. Enlarged adenoids and anomalies in the structure of the nose can also prevent the child from breathing normally 1 .
Predisposing factors for the appearance of nasal congestion are:
 7 in the first 3 years of life 3 ;
7 in the first 3 years of life 3 ; Up to content
How to relieve nasal congestion in a child
Even if nasal congestion has not occurred for the first time, before starting treatment, it is necessary to consult a doctor to find out the cause of the disease 4.8 . Allergic rhinitis and viral infection require different treatment regimens, and only a specialist will be able to quickly recognize the nature of the existing disorders 4.7 .
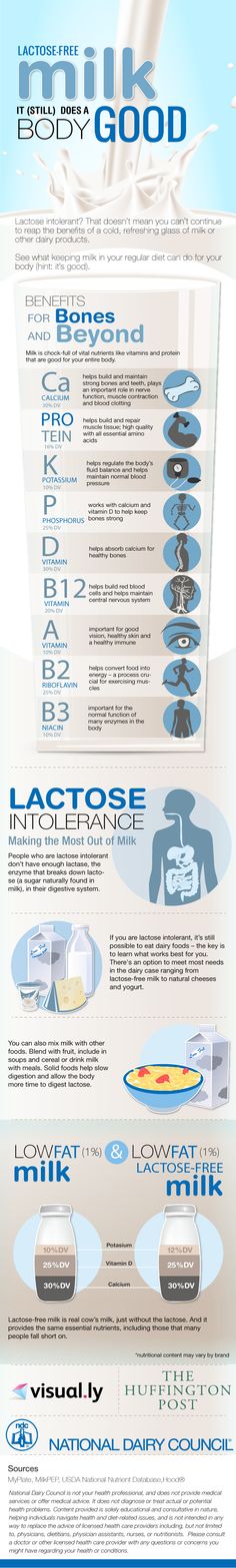
Nasal wash 3,4,12 . Can be used for any kind of runny nose 12 . This simple and affordable procedure helps to clear the mucous membrane from the accumulated inflammatory secretion and microorganisms, reduce its swelling 3,4,12 . For washing use saline solutions 3 , sterile sea water 4 , antiseptic and anti-inflammatory agents 12 .
For washing use saline solutions 3 , sterile sea water 4 , antiseptic and anti-inflammatory agents 12 .
Inhalation 14 . For the treatment of nasal congestion in a child, warm inhalations are allowed 14.15 . You can breathe over hot decoctions of medicinal plants 14 or use essential oils added to the water 15 . Even ordinary steam often helps to cope with nasal congestion with a runny nose in a child 14 . During inhalation, inflamed tissues are gently warmed up, mucus is liquefied, swelling is reduced, some pathogens are destroyed 14.15 . After this treatment, empty the nose by using an aspirator or by asking the child to blow his nose 3 .
Warming ointments 17 . In addition to other products, warming ointments with essential oils can be used. They are smeared on the feet, temples, bridge of the nose and wings of the nose 17 .
They are smeared on the feet, temples, bridge of the nose and wings of the nose 17 .
Acupressure 18.19 . This method is based on the acupuncture effect on certain points on the human body 18 . It is used to relieve nasal congestion in children and adults 19 . Essential oils are used to enhance the effect of acupressure. 22
Nasal drops and sprays. For viral respiratory diseases and allergic rhinitis, the treatment regimen includes the use of the latest generation of antihistamines 8 in the form of nasal drops and sprays 20 . They have a local effect and have a small number of contraindications 8 . Special products for children of the TIZIN ® line help to cope with congestion, facilitating nasal breathing and improving well-being. TIZIN ® Allergy contains antihistamines and is used in the treatment of hay fever and allergic rhinitis 11 .