Amnio vs nipt
What Noninvasive Prenatal Testing Can Tell Expecting Parents | UNM Health Blog
By Vivek Katukuri, MD | March 24, 2021
NIPT is still a relatively new screening option for pregnant women.
During your first trimester of pregnancy, your Ob/Gyn or midwife may offer noninvasive prenatal testing (NIPT) prenatal testing to determine whether the baby might be at increased risk for birth defects.
NIPT primarily looks for signs that your pregnancy may be at increased risk of:
- Down syndrome (trisomy 21, caused by an extra chromosome 21)
- Edwards syndrome (trisomy 18, caused by an extra chromosome 18)
- Patau syndrome (trisomy 13, caused by an extra chromosome 13)
- Conditions caused by missing or extra X and Y chromosomes
NIPT can also tell you whether you’re having a boy or girl—often earlier than an ultrasound.
Unlike traditional tests such as amniocentesis or chorionic villus sampling (CVS), NIPT does not require disturbing the placenta or amniotic fluid, which can slightly increase the risk of miscarriage. NIPT requires just a small blood draw from your arm during a regular prenatal visit or at your home, if desired. Since fragments of the placental DNA circulate in your blood, all we need is a small blood draw that a lab can analyze.
While it might be scary to think about pregnancy abnormalities, some patients prefer to know so they can plan for the future. NIPT has only been available in the last decade and can be done as early as 9 weeks.
In summer 2020, the American College of Obstetricians and Gynecologists recommended that all pregnant women be offered prenatal screening for chromosomal disorders, which includes NIPT, and the decision to have it is personal.
Let’s talk about who might benefit from NIPT, as well as its accuracy. Our goal is to help you feel more empowered to make the best decision for you and your family.
It’s important to understand that NIPT is a screening tool, not a diagnostic test. This means it can’t diagnose a genetic condition; it can only predict whether your baby is at high or low risk of having one.
— Vivek Katukuri, MD
Who Might Want to Consider NIPT?If you have certain risk factors such as these, your health care provider might recommend NIPT:
- Being 35 or older.
- A personal or family history of chromosomal disorders
- If an abnormality is detected on an ultrasound
While many insurance companies cover NIPT, it's a good idea to check with yours to find out whether you’re covered and what your out-of-pocket costs might be.
It’s important to understand that NIPT is a screening tool, not a diagnostic test. This means it can’t diagnose a genetic condition; it can only predict whether your baby is at high or low risk of having one.
These tests are never 100% accurate. However, a 2016 study found that NIPT has a high sensitivity for detecting Down syndrome. While the sensitivity for detecting conditions such as Edwards and Patau syndromes is lower, it’s still strong.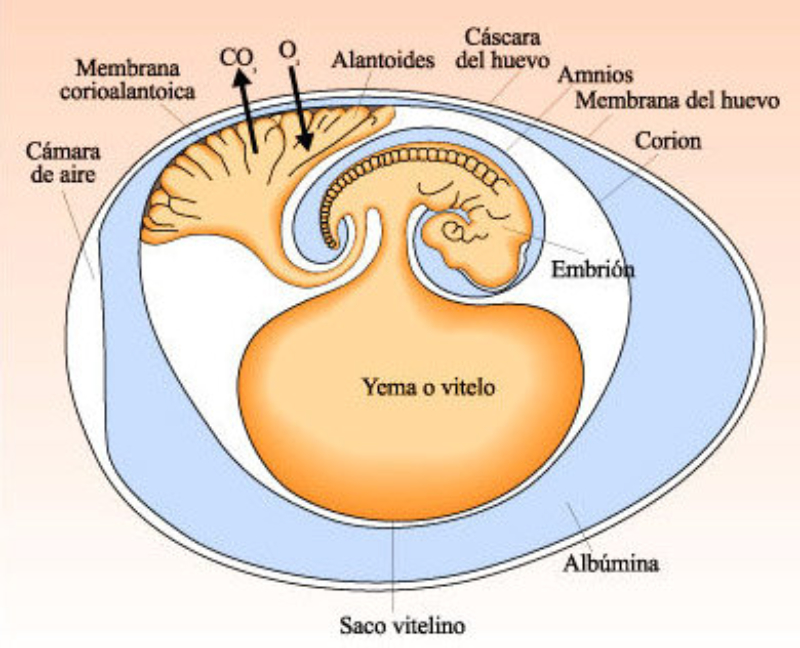 Depending on the results of the screening, your doctor may recommend further tests.
Depending on the results of the screening, your doctor may recommend further tests.
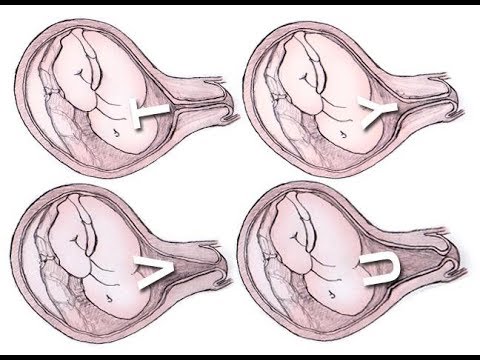
If the NIPT indicates a high risk of a chromosomal condition such as Down syndrome, your doctor may recommend you receive genetic counseling, a comprehensive ultrasound, and CVS or amniocentesis to verify the diagnosis.
Once a diagnosis is confirmed, you can discuss with your partner and health care provider what the results may mean for your family. Your UNM Health team will support you in your next steps, which will depend on your beliefs, values, and circumstances.
If you choose to proceed with the pregnancy, we can help you plan for the baby’s future health needs. If you choose to terminate the pregnancy, we offer judgment-free abortion care and counseling up to 23 weeks and 6 days of pregnancy.
Deciding to have NIPT is a personal decision. Talk with your health care provider or a genetic counselor about your questions and concerns. We are here to listen, provide information, and support you throughout the process.
We are here to listen, provide information, and support you throughout the process.
To find out whether you or a loved one might benefit from Ob/Gyn care
Call 505-272-2245.
Categories: Women's Health
Our concerns about non-invasive prenatal testing (NIPT) in the private healthcare sector
If you or your partner have been pregnant in the last five years, or you have seen news stories about pregnancy screening and Down’s syndrome, you will have probably heard of non-invasive prenatal testing (NIPT), or the ‘Harmony test’ as its often called (which is one of the test’s brand names).
This is a newish kind of screening test in which a blood sample from a pregnant woman is used to test for a range of genetic conditions in the fetus, with varying levels of certainty. NIPT has been shown in multiple studies to be very good at identifying the most common chromosomal conditions – Down’s syndrome, Edwards’ syndrome and Patau’s syndrome – particularly in women who have a higher chance[1] of having a fetus with one of these conditions. You still get some false positive results, but far fewer than with older screening tests. NIPT for these conditions has recently become available to pregnant women in the higher chance category in the NHS in Wales, and it has been promised to women in England and Scotland in the near future.
You still get some false positive results, but far fewer than with older screening tests. NIPT for these conditions has recently become available to pregnant women in the higher chance category in the NHS in Wales, and it has been promised to women in England and Scotland in the near future.
However, NIPT can already be accessed through numerous private clinics and hospitals across the UK for around £500. It is pretty accurate for Down’s, Edwards’ and Patau’s syndromes even if you are not in the higher chance category, and the test is available from around 9 weeks of pregnancy.
The Nuffield Council on Bioethics’ 2017 report on the ethical issues raised by NIPT discussed the offer of NIPT in the private sector. We highlighted some serious issues with how some (not all) clinics and NIPT test providers are marketing and offering NIPT in the UK. Disappointingly, despite our best efforts to raise these issues, little has changed.
Our main concerns are:
1. Misleading use of statistics
The websites of most private providers state that NIPT is ‘99% accurate’ or has ‘99% sensitivity’. I think most people would assume that this means their result will tell them pretty much for sure whether their fetus has one of the conditions or not. But as the conditions affect less than 1% of all children born, a dummy test that gave everybody a low chance result would be 99% accurate.
I think most people would assume that this means their result will tell them pretty much for sure whether their fetus has one of the conditions or not. But as the conditions affect less than 1% of all children born, a dummy test that gave everybody a low chance result would be 99% accurate.
A more helpful statistic is the positive predictive value. Sometimes NIPT gives a high chance result when the fetus does not actually have the condition. If you receive a high chance result for Down’s syndrome, there is a 1 in 5 (20%) chance that the result is wrong and your fetus does not have the condition. For Patau’s syndrome, there is a 1 in 2 (50%) chance the result is wrong, and for Edwards’ syndrome, it’s a 3 in 5 (60%) chance.[2] So, if you want to know for sure, you will also need to have a diagnostic test such as amniocentesis. Some companies give people’s results as being ‘positive’ or ‘negative’, which as you can see is highly misleading or, at best, confusing.
2.
 Poor information about the tested-for conditions
Poor information about the tested-for conditionsVery fewprivate clinics or test providers include information about Down’s syndrome, Edwards’ syndrome and Patau’s syndrome in their marketing and information materials. In the NHS, the development of balanced and up-to-date information about the conditions has been central to the aim of ensuring women and couples make informed decisions about NIPT. Public Health England has spent a year consulting with support organisations and families of people with the conditions to help them describe, as neutrally as possible, what having a child with one of these conditions might mean.[3] Yet, in the private sector, you’re lucky if they have included the web address of a Down’s syndrome organisation.
At the Nuffield Council, we believe it's only ethical to offer NIPT within an environment that enables women and couples to make informed choices, and the provision of high quality information about the tested-for conditions is crucial to this.
3. Offering NIPT where the accuracy is low or unknown
Many clinics and NIPT test providers offer the option of testing for a range of other, often very rare, genetic conditions. These include those caused by unusual numbers ofthe sex (X and Y) chromosomes, such as Turner syndrome and Triple X syndrome,and those caused by small bits of DNA missing, called microdeletions, such as Prader-Willi syndrome and 5p deletion syndrome.
Information relating to the accuracy of NIPT for these conditions is often missing from websites and public materials. This is probably because the limited research that has taken place has shown that NIPT performs poorly for many of these conditions.[4]
This means that, if you chose to test for these other conditions (and I can understand why many women opt for this when NIPT is marketed as being 99% accurate) and you get a high chance result, there is a high probability that the result will turnout to be wrong. You’re left with a choice between having an amniocentesis, which carries a small risk of miscarriage, to get a definite result, or living withthe uncertainty. We have heard from women in this position that the anxiety this causes can be huge.
We have heard from women in this position that the anxiety this causes can be huge.
We believe that clinics and test providers should stop offering NIPT for conditions where it does not offer an accurate prediction, and that they should provide full information about the limitations of the tests they do offer.
4. Lack of follow-up support
Some private hospitals and clinics offer a full package of care that includes pre-test counselling, access to a healthcare professional to discuss high chance results, and follow-up diagnostic testing if requested. But many do not offer all this. This is particularly true for those companies offering NIPT on a direct-to-consumer basis, where you order online and the test kit is sent to you in the post.
In many cases, it is NHS staff who have to deal with the fall-out. We have heard that women with high chance NIPT results are going to the NHS for advice, support and diagnostic testing. How the NHS will meet demand for this as private provision escalates is a source of concern. [5]Although maternity care staff are receiving training in preparation for theroll-out of NIPT for Down’s, Edwards’ and Patau’s syndromes, they are less likely to know about the other conditions that private NIPT providers offer to test for.
[5]Although maternity care staff are receiving training in preparation for theroll-out of NIPT for Down’s, Edwards’ and Patau’s syndromes, they are less likely to know about the other conditions that private NIPT providers offer to test for.
What next?
I’ve highlighted four areas of practice that we are concerned about, but our list ismuch longer (e.g. lack of information about the possibility that NIPT might not produce a clear result either way, or that it might identify secondary findings about the mother’s health, using offensive language when referring to Down’ssyndrome and other conditions, and the offer of ‘baby gender’ tests). We think things could be much better.
We have already produced a guidance leaflet for manufacturers and healthcare providers on the information to include on their websites and leaflets about NIPT.
However, it seems unlikely that self-regulation will be enough. As such, we are delighted that the Care Quality Commission has recently changed its position and now considers NIPT to be within its remit, in line with a recommendation in our report. It has already started carrying out inspections of clinics in England that offer NIPT, so we hope to start seeing improvements in standards of care soon.
It has already started carrying out inspections of clinics in England that offer NIPT, so we hope to start seeing improvements in standards of care soon.
In addition, last week we urged the House of Commons Science and Technology Select Committee to investigate the regulation of private NIPT as part of an inquiry on commercial genetic testing. We are also seeking to raise public awareness of the issues (see today's BBC article and segment on BBC Radio 4's Today programme).
We will continue to work with these and other partners in a renewed effort to raise standards among private NIPT providers.
[1]Pregnant women usually find out if they have a higher chance of having a fetus with Down’s syndrome, Edwards’ syndrome or Patau’s syndrome through early pregnancy screening tests, such as the combined test. These tests are offered to all pregnant women in England, Scotland and Wales. The results of an ultrasound scan and blood tests are taken together with the woman’s age to workout a probability score. If the score is at least 1 in 150, the woman is considered to be in a ‘higher chance’ category.
If the score is at least 1 in 150, the woman is considered to be in a ‘higher chance’ category.
[2]See the Warwick Evidence systematic review of the performance of NIPT across 41studies, which is summarised on p13 of the Nuffield Council on Bioethics’ reporton NIPT. For statistics geeks, in a general population of pregnant women, the positive predictive value of NIPT for Downs’ syndrome is 81.6%, for Edwards’ syndrome is 37%, and for Patau’s syndrome is 49%. The negative predictive value (NPV) tells you how likely it is that a low chance NIPT resultis correct. NIPT has a very high NPV for Down’s, Edwards’ and Patau’s syndromes(99.9%) so you can be pretty certain a low chance result means that you do not have a fetus with one of the conditions.
[3]See the Public Health England screening blog for updates, e.g. https://phescreening.blog.gov.uk/2017/03/24/introducing-non-invasive-prenatal-testing-to-antenatal-screening-progress-so-far/
[4] Cochrane,an independent research organisation, published a meta-analysisof the evidence on the accuracy of NIPT in 2017. They were unable to perform meta-analyses of NIPT for several sex aneuploidy conditions because there were very few or no studies. Other studies have considered the utility of NIPT for testing for microdeletions, e.g. this study, by some of the leading NIPT experts in the UK, concluded that NIPT for microdeletions is not ready for routine clinical implementation.
They were unable to perform meta-analyses of NIPT for several sex aneuploidy conditions because there were very few or no studies. Other studies have considered the utility of NIPT for testing for microdeletions, e.g. this study, by some of the leading NIPT experts in the UK, concluded that NIPT for microdeletions is not ready for routine clinical implementation.
[5]See paragraph 4.35-36 of the Nuffield Council on Bioethics’ reporton NIPT.
Legacy 1st trimester prenatal screening or NIPT test?
As you know, the IGR Medical Center (MC IGR) actively conducts not only practical activities, but also scientific ones. We carefully analyze the treatment cycles performed, the appointment of tests and their results. One of the areas that is constantly monitored is prenatal screening of pregnant women in order to detect fetal chromosomal pathology (for example, Down syndrome).
There are two types of non-invasive prenatal diagnosis analysis.
- Conventional non-invasive prenatal screening is performed during the first and second trimesters based on ultrasound and blood chemistry of the pregnant woman.
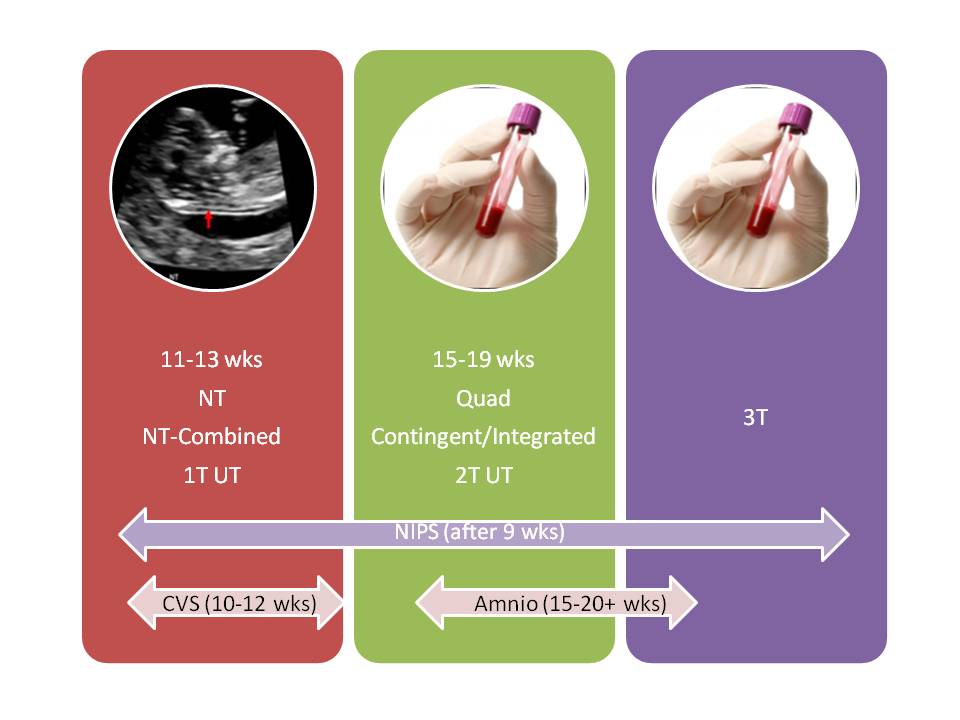 In combination with maternal age, the risk of the genetic condition of the fetus is assessed, but without fetal DNA testing.
In combination with maternal age, the risk of the genetic condition of the fetus is assessed, but without fetal DNA testing. - Starting from the 10th week of pregnancy, it became possible to analyze the DNA of the fetus on the blood of a pregnant woman using NIPT-BT. After all, as you know, during pregnancy, fetal DNA travels from the placenta to the maternal bloodstream and circulates there with its own DNA. At the same time, the accuracy of such a study is much higher than that of classical biochemical screening.
Thus, after evaluating the results obtained over many years of practice at the MC IHR, we found that among 4,226 pregnant women who underwent biochemical screening at the MC IHR, 802 or 18.9% of women were referred for an invasive prenatal procedure (amniocentesis) . According to the results of the study of amniotic fluid cells, only 100 women out of 802 (12.5%) had a fetal chromosomal pathology confirmed (Down syndrome, Edwards syndrome, Patau syndrome, and others).
After analyzing data from 182 NIPT-VT studies, it was found that 4 out of 182 patients (or 2.2%) were referred for amniocentesis after a non-invasive test to confirm chromosomal abnormality in the fetus. At the same time, chromosomal pathology of the fetus was confirmed in 100% (in 4 women).
| Screen type | Examined women | Number of amniocentesis performed based on screening results | Number of cytogenetically confirmed cases of fetal chromosomal pathology |
| Classic biochemical screening | 4226 | 802 (18.9% of total) | 100 (12.5% of the number of amniocentesis performed ) |
| NIPT-VT | 182 | 4 (2.2% of total) | 4 (100% of the number of amniocentesis performed ) |
Thus, screening with NIPT-VT is much more accurate than classical biochemical screening and avoids an invasive prenatal procedure due to false positive results.
But it must be remembered that if a chromosomal pathology is detected according to the results of NIPT-VT, confirmation of this disease is required using an invasive procedure (amniocentesis) in order to study the complete chromosomal set of the fetus.
Amniocentesis has a very high accuracy (99.99%), and only 0.1% can lead to a violation of the course of pregnancy. If you have undergone NIPT-VT testing at the MC IGR, cytogenetic testing of amniotic fluid cells is performed for you free of charge.
By contacting the IGR Medical Center, with the help of NIPT-VT you have the opportunity to reduce the likelihood of the need for an invasive prenatal procedure, as well as with high accuracy (> 99%) determine the abnormal number of chromosomes 13, 18, 21, X, Y in the blood of a pregnant woman.
Our specialists are always ready to provide you with highly qualified advice and assistance even in the most difficult diagnostic cases.
Non-Invasive Prenatal Test (NIPT)
WHY NIPT?
The generally accepted methods of prenatal diagnosis of fetal pathology are "double" and "triple" tests - screening of the 1st and llth trimesters of pregnancy in combination with ultrasound. However, for all their merits, the accuracy of these studies in relation to frequent chromosomal abnormalities is ~80%. The accuracy of a non-invasive test is much higher than that of biochemical screening, since its results are not affected by the characteristics of the course of pregnancy, the drugs taken, and the woman's somatic diseases. For example, the most common symptoms can be recognized with maximum certainty:
Down syndrome >99%
Edwards syndrome >98%
Patau syndrome ~98%
Advanced NIPT recognizes all the pathology that is included in the standard plus five microdeletion syndromes: crying cat, 1p36, Prader-Willi, Angelman, DiGeorge.
SAFETY
An important advantage is that non-invasive diagnostics is also the safest way to diagnose fetal chromosomal disorders. Unlike various invasive methods such as cordocentesis, amniocentesis and chorionic villus aspiration, this test is done on the mother's blood and is absolutely safe for both her health and the health of the unborn child.
HOW IT WORKS
For the test, venous blood is taken from the mother and the DNA of the fetus is analyzed, which enters the bloodstream of the pregnant woman from the placenta. The test detects the presence of a violation of the number of chromosomes (aneuploidy) of the fetus. Aneuploidies are the causes of congenital genetic diseases of the child, which can have a significant impact on his physical health and mental abilities.
- 10 days will be required for the study.
- The test was put into practice in 2012 and has since been successfully used worldwide.
Since 2013, more than 6,000 non-invasive genetic tests have already been performed at Mother and Child clinics.
HISTORY IN DETAILS
WHO NEEDS THIS TEST?
Since the non-invasive genetic test is an absolutely safe diagnostic method, any pregnant woman who wants to get the most complete information about the health of her unborn child and dispel unnecessary doubts and fears can do it.
INDICATION FOR NON-INVASIVE TEST:
1. The age of the pregnant woman is over 35 years.
2. High risk on biochemical screening.
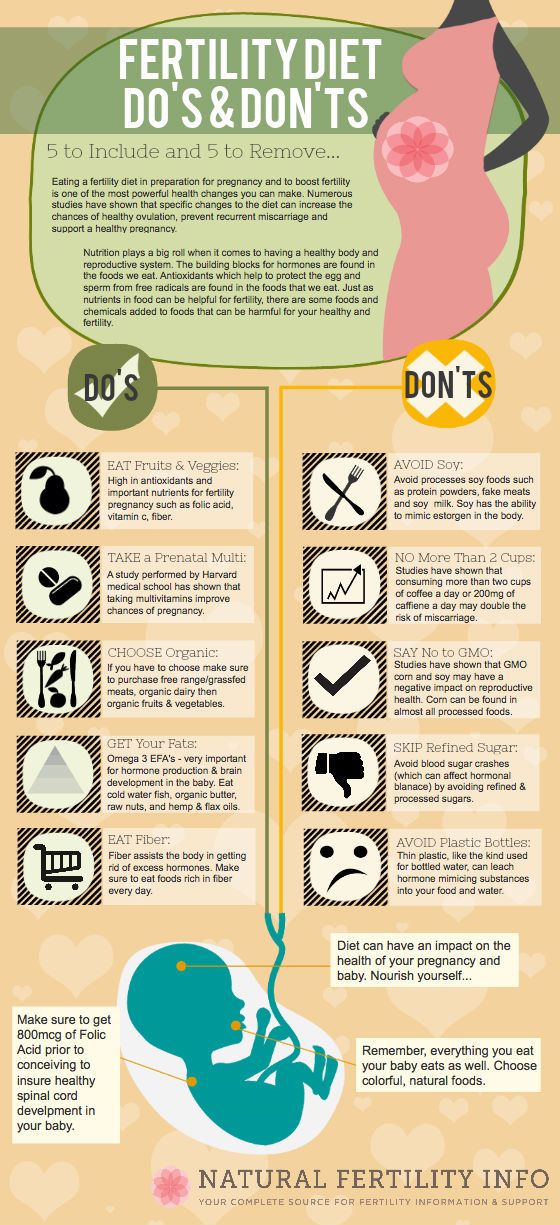
The test can be taken from 10 weeks of pregnancy, but leading geneticists recommend that you first undergo an ultrasound screening of the first trimester at 11 weeks and, if the result is good, do not go for blood biochemistry, but do NIPT instead.
PLEASE NOTE!
Blood for testing is not taken on an empty stomach. It is advisable to eat something sweet before donating blood for the study. The analysis is not affected by drugs, medicines or vitamins taken during pregnancy.
BLOOD COLLECTION
When giving blood for a test, the fetal DNA fraction (the amount of fetal DNA circulating in maternal blood) must be at least 4%. In the case of a reduced amount (less than 4%), a blood sample may be required. Also, the second attempt is likely with increased body weight of the pregnant woman.
CONTRAINDICATIONS FOR NIPT:
1. The presence of ultrasound markers of chromosomal pathology (such as expansion of the thickness of the collar space, non-immune dropsy, hypoplasia of the nasal bone, shortening of the length of tubular bones) or malformations.
2. Carrying a balanced chromosomal rearrangement by one of the parents.
3. The presence in the family of a child with a genetic pathology. In all these cases, consultation with a geneticist and karyotyping of the fetus is necessary.