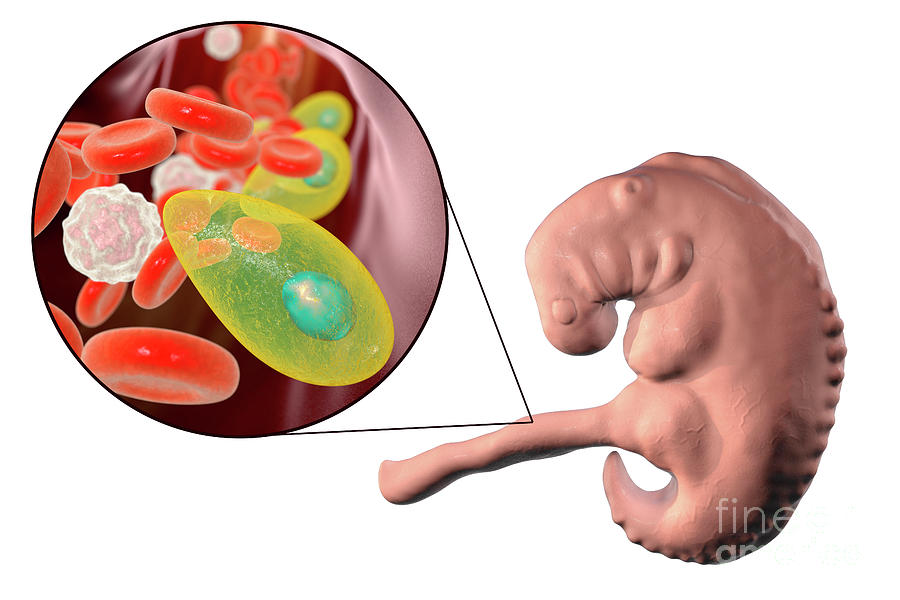
Toxoplasmosis in fetus
Toxoplasmosis
Topics
In This Topic
KEY POINTS
Toxoplasmosis is an infection you can get from eating undercooked meat or touching cat poop.
Most times, there are no symptoms so you may not know that you have toxoplasmosis.
If you get toxoplasmosis just before or during pregnancy, you may pass it to your baby.
Toxoplasmosis can cause problems during pregnancy, including miscarriage, preterm birth or stillbirth.
Most babies born with toxoplasmosis have no symptoms. Symptoms can include eye infections, swollen glands, liver or spleen, or jaundice.
Toxoplasmosis is an infection you can get from eating undercooked meat or touching cat poop or a litter box. It’s caused by a very common parasite called Toxoplasma gondii. The parasite is so tiny you can’t see it.
More than 40 million people in the United States may have the parasite. Very few people have symptoms because a healthy immune system usually keeps the parasite from causing an infection. However, toxoplasmosis can cause health problems for you and your baby during pregnancy.
How do you get infected with toxoplasmosis?
You can come in contact with the parasite that causes the infection through:
- Eating raw or undercooked meat or shellfish
- Eating unwashed fruits and vegetables
- Touching cat litter or poop
- Touching kitchen utensils and cutting boards used to prepare raw or undercooked meat and fruits and vegetables
- Touching dirt or sand
- Touching stray cats
What are the signs and symptoms of toxoplasmosis?
You may not know if you have the infection. Many times there are no symptoms. For some people, it feels like the flu.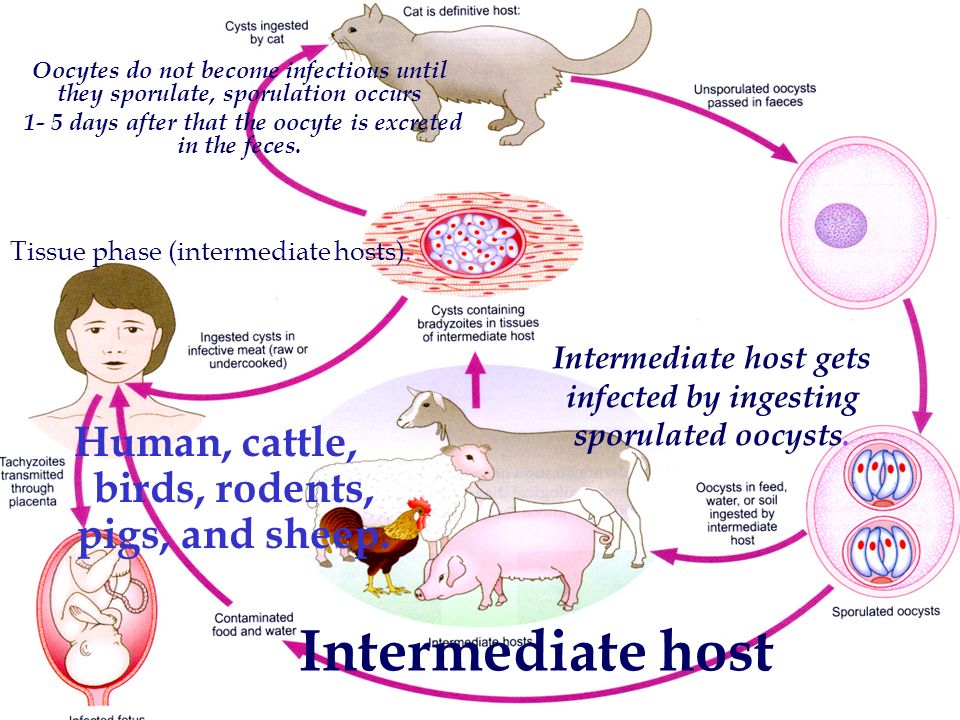 Symptoms can include:
Symptoms can include:
- Achy muscles
- Headache
- Fatigue (tiredness)
- Fever
- Swollen glands
- Blurry vision
- Eye redness
These symptoms can last for a month or longer. If you think you have toxoplasmosis, talk to your health care provider. Your provider can give you a blood test to find out if you have the infection. Even though blood tests are a regular part of prenatal care, you don’t usually get tested for toxoplasmosis. So be sure to talk to your provider if you think you have the infection.
Can toxoplasmosis cause problems before pregnancy?
If you have toxoplasmosis within 6 months of getting pregnant, you may be able to pass it to your baby during pregnancy. Talk to your health care provider about being tested. Wait 6 months after a toxoplasmosis infection before trying to get pregnant.
Can toxoplasmosis cause problems during pregnancy?
Yes. Pregnancy complications caused by toxoplasmosis include:
- Preterm birth – Birth that happens before 37 weeks of pregnancy
- Stillbirth – When a baby dies after 20 weeks of pregnancy
- Miscarriage – When a baby dies before 20 weeks of pregnancy
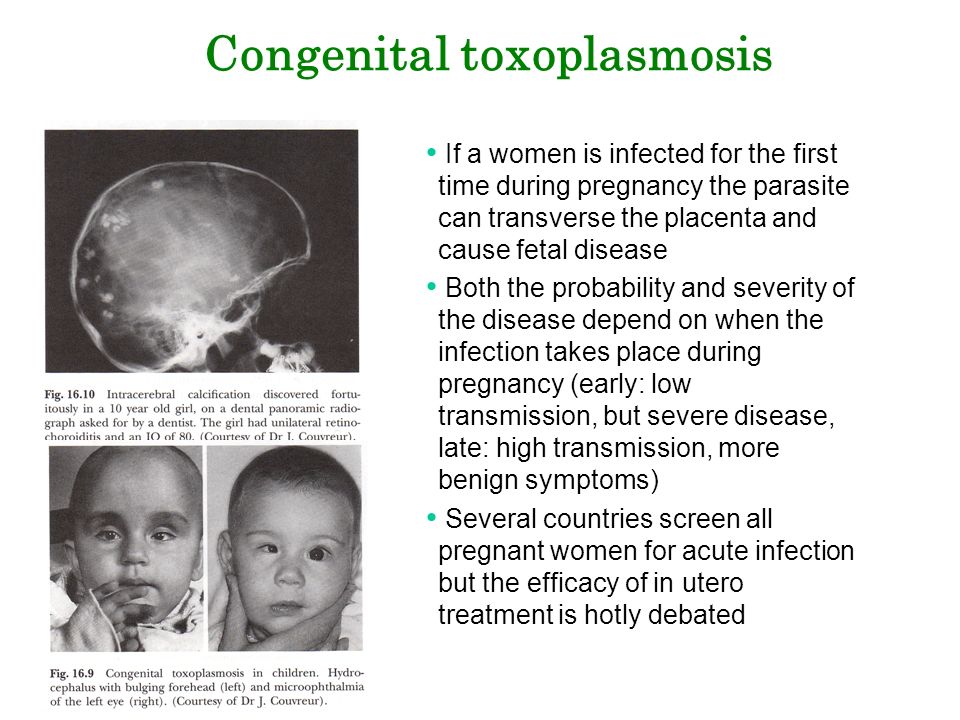
If you get toxoplasmosis just before or during pregnancy, you may pass the infection to your baby even if you don’t have any symptoms. The risk of passing the infection to your baby depends on how far along in your pregnancy you were when you were infected. The later in your pregnancy that you get infected (third trimester), the more likely it is that your baby will also get infected. But the earlier in pregnancy you get infected, the more serious the baby’s problems may be after birth. For example, your baby could have damage to the liver, brain and eyes. Up to 1 in 2 babies (50 percent) who are infected with toxoplasmosis during the pregnancy are born early (preterm). Some infected babies may die.
The risk of passing the infection to your baby depends on how far along in your pregnancy you were when you were infected. The later in your pregnancy that you get infected (third trimester), the more likely it is that your baby will also get infected. But the earlier in pregnancy you get infected, the more serious the baby’s problems may be after birth. For example, your baby could have damage to the liver, brain and eyes. Up to 1 in 2 babies (50 percent) who are infected with toxoplasmosis during the pregnancy are born early (preterm). Some infected babies may die.
If you have toxoplasmosis during pregnancy, there are several ways your health care provider can check to see if your baby is infected:
Amniocentesis. An amniocentesis (also called amnio) can test the fluid around your baby for infection. You can get this test at 15 to 20 weeks of pregnancy. It also can be tested for other problems with the baby, like birth defects or genetic problems.
Ultrasound.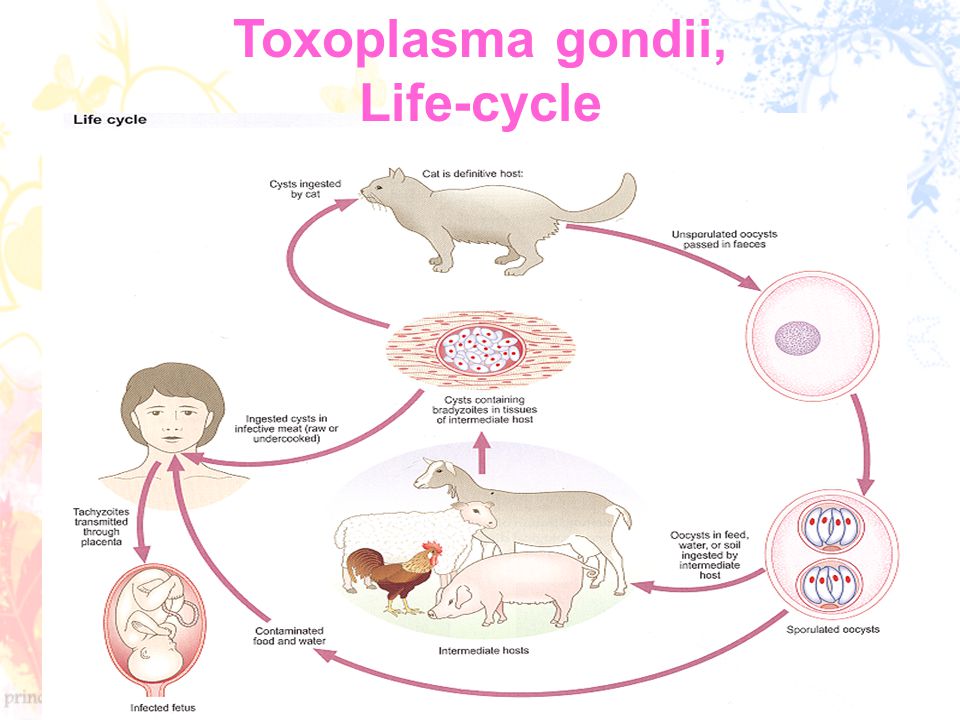 About 1 in 3 babies infected with toxoplasmosis have a problem that can be seen on an ultrasound. Ultrasound (also called sonogram) is a prenatal test that uses sound waves to show a picture of your baby before they are born. Ultrasound helps your provider check on your baby’s health and development. Most pregnant people get an ultrasound in their second trimester at 18 to 20 weeks of pregnancy.
About 1 in 3 babies infected with toxoplasmosis have a problem that can be seen on an ultrasound. Ultrasound (also called sonogram) is a prenatal test that uses sound waves to show a picture of your baby before they are born. Ultrasound helps your provider check on your baby’s health and development. Most pregnant people get an ultrasound in their second trimester at 18 to 20 weeks of pregnancy.
Blood test. Your baby’s blood can be tested for toxoplasmosis after birth.
How can toxoplasmosis during pregnancy harm your baby?
Most babies born with toxoplasmosis have no symptoms. But about 1 in 10 babies (10 percent) with the infection are born with problems, including:
- Eye infections or eye inflammation
- Swollen liver and spleen
- Jaundice (when a baby's eyes and skin look yellow.)
- Seizures or convulsions
- Fluid on the brain (hydrocephalus)
- Swollen lymph nodes
- Large head size (macrocephaly) or smaller-than-normal head size (microcephaly)
- Feeding problems
- Low birth weight
- Skin rash or bruising
Without treatment, newborns may develop problems later in life, even if they show no symptoms earlier. This can happen even 20 or 30 years later. These problems include:
This can happen even 20 or 30 years later. These problems include:
- Intellectual and developmental disabilities (problems with how the brain works that can cause your baby trouble or delays in physical development, learning, communicating, taking care of themselves or getting along with others).
- Eye infections and vision problems
- Pneumonia
- Cerebral palsy (a group of conditions that affects the parts of the brain that control the muscles. It can cause problems with movement, posture,standing up straight and balance).
- Seizures or convulsions
- Hearing loss
Each year, between 800 and 4,400 babies in the United States are born with toxoplasmosis. If you think you had toxoplasmosis during pregnancy, be sure your baby is tested.
How is toxoplasmosis treated during pregnancy?
If you are infected during pregnancy, both you and your baby should be closely monitored during your pregnancy and after the baby is born.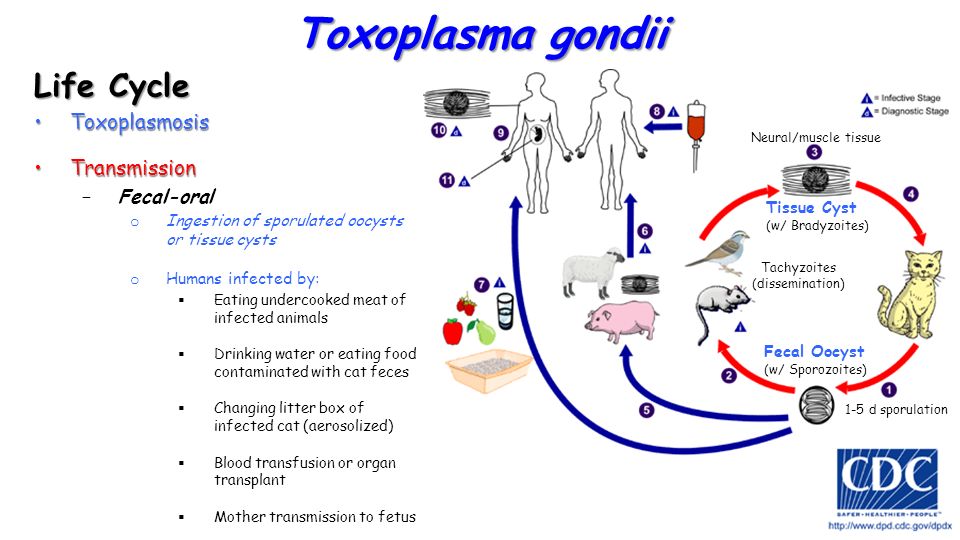 Getting treated with certain antibiotics helps reduce the chance of your baby getting toxoplasmosis. Antibiotics are medicines that treat certain types of infections. This treatment also helps reduce the seriousness of any symptoms your baby may have.
Getting treated with certain antibiotics helps reduce the chance of your baby getting toxoplasmosis. Antibiotics are medicines that treat certain types of infections. This treatment also helps reduce the seriousness of any symptoms your baby may have.
If you’re infected before 18 weeks of pregnancy, your provider may give you an antibiotic called spiramycin. This medicine helps reduce the chance of your baby getting the infection.
If you’re infected after 18 weeks of pregnancy, your provider may give you different antibiotics called pyrimethamine, sulfadiazine or leucovorin. These medicines are recommended for use after 18 weeks of pregnancy. If you take them before 18 weeks of pregnancy, they may cause birth defects in your baby.
How is toxoplasmosis treated in your baby after birth?
If your baby shows symptoms of toxoplasmosis, the provider may treat your baby with antibiotics. Your baby may continue these antibiotic treatments until their first birthday, sometimes even longer.
Should you nurse your baby if you had toxoplasmosis during pregnancy?
Yes. Your provider can give you a blood test to find out if you are still infected. If you are healthy and no longer infected, the chances of giving your baby toxoplasmosis while nursing is very small. Don’t nurse your baby if you have cracked and bleeding nipples or breast inflammation if you were infected recently.
How can you prevent toxoplasmosis?
Here’s how to protect yourself from toxoplasmosis:
- Don’t eat raw, undercooked or contaminated meat, especially lamb, pork or venison. Cooked meat should not look pink, and the juices should be clear. Use a meat thermometer to check the temperature of the meat before you eat it.
- Don’t eat raw, undercooked or contaminated shellfish, such as oysters, clams or mussels.
- Do not drink raw milk, especially goat’s milk.
- Wash your hands with soap and water after handling fruits, vegetables or raw meat, poultry (such as chicken or turkey) or shellfish.
- Don’t touch your eyes, nose or mouth when handling raw meat.
- Clean cutting boards, work surfaces and utensils with hot, soapy water after using them with fruits, vegetables or raw meat.
- Peel or thoroughly wash all raw fruits and vegetables before eating.
- Use work gloves when you’re gardening. Wash your hands afterward.
If you have a cat:
- Don’t let your cat go outside your home, where it may eat spoiled food or come in contact with the parasite.
- Change your cat’s litter box daily. Ask someone else to clean the litter box. If you have to do it yourself, wear gloves. Wash your hands thoroughly when you’re done emptying the litter.
- Only feed your cat canned or dried cat food from the store or well-cooked table food. Don’t feed your cat raw or uncooked meat.
- Stay away from children’s sandboxes. Cats like to use them as litter boxes.
- Don’t touch stray cats or kittens.
Last reviewed: August 2021
') document.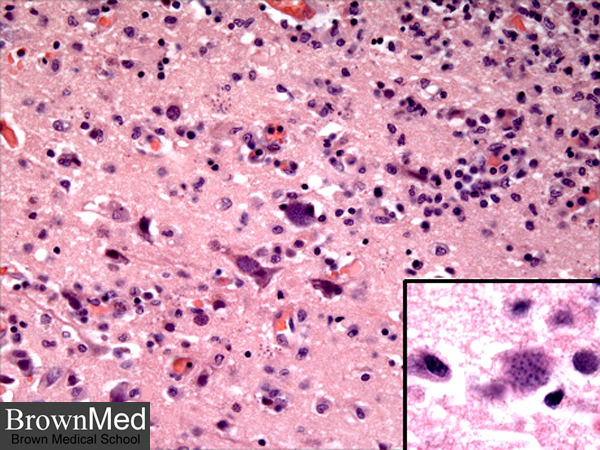 write('
write('
Preterm labor & premature birth
') document.write('') }
') document.write('') }
Toxoplasmosis and pregnancy - PMC
1. Yamada H, Nishikawa A, Yamamoto T, Mizue Y, Yamada T, Morizane M, et al. Prospective study of congenital toxoplasmosis screening with use of IgG avidity and multiplex nested PCR methods. J Clin Microbiol. 2011;49(7):2552–6. doi: 10.1128/JCM.02092-10. Epub 2011 May 4. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2. Jenum PA, Stray-Pedersen B, Melby KK, Kapperud G, Whitelaw A, Eskild A, et al. Incidence of Toxoplasma gondii infection in 35,940 pregnant women in Norway and pregnancy outcome for infected women. J Clin Microbiol. 1998;36(10):2900–6. [PMC free article] [PubMed] [Google Scholar]
3. Montoya JG, Liesenfeld O. Toxoplasmosis.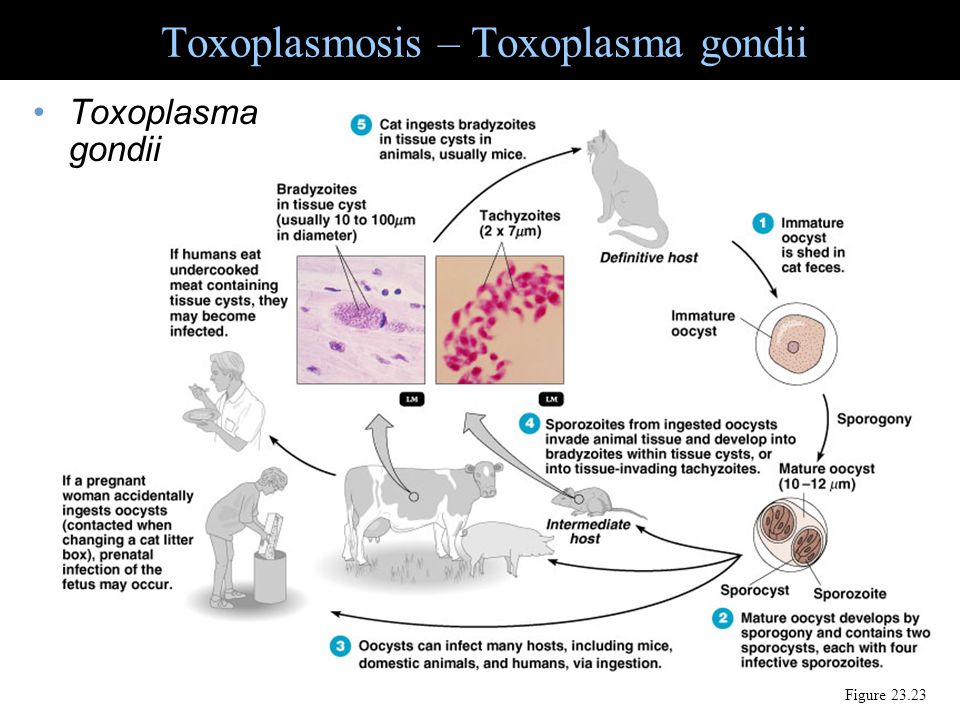 Lancet. 2004;363(9425):1965–76. doi: 10.1016/S0140-6736(04)16412-X. [PubMed] [CrossRef] [Google Scholar]
Lancet. 2004;363(9425):1965–76. doi: 10.1016/S0140-6736(04)16412-X. [PubMed] [CrossRef] [Google Scholar]
4. Saadatnia G, Golkar M. A review on human toxoplasmosis. Scand J Infect Dis. 2012;44(11):805–14. doi: 10.3109/00365548.2012.693197. Epub 2012 Jul 25. [PubMed] [CrossRef] [Google Scholar]
5. Bodaghi B, Touitou V, Fardeau C, Paris L, LeHoang P. Toxoplasmosis: new challenges for an old disease. Eye (Lond) 2012;26(2):241–4. doi: 10.1038/eye.2011.331. Epub 2012 Jan 6. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
6. Kieffer F, Wallon M. Congenital toxoplasmosis. Handb Clin Neurol. 2013;112:1099–101. doi: 10.1016/B978-0-444-52910-7.00028-3. [PubMed] [CrossRef] [Google Scholar]
7. Dubey JP. History of the discovery of the life cycle of Toxoplasma gondii. Int J Parasitol. 2009;39(8):877–82. [PubMed] [Google Scholar]
8. Lebech M, Andersen O, Christensen NC, Hertel J, Nielsen HE, Peitersen B, et al. Feasibility of neonatal screening for toxoplasma infection in the absence of prenatal treatment.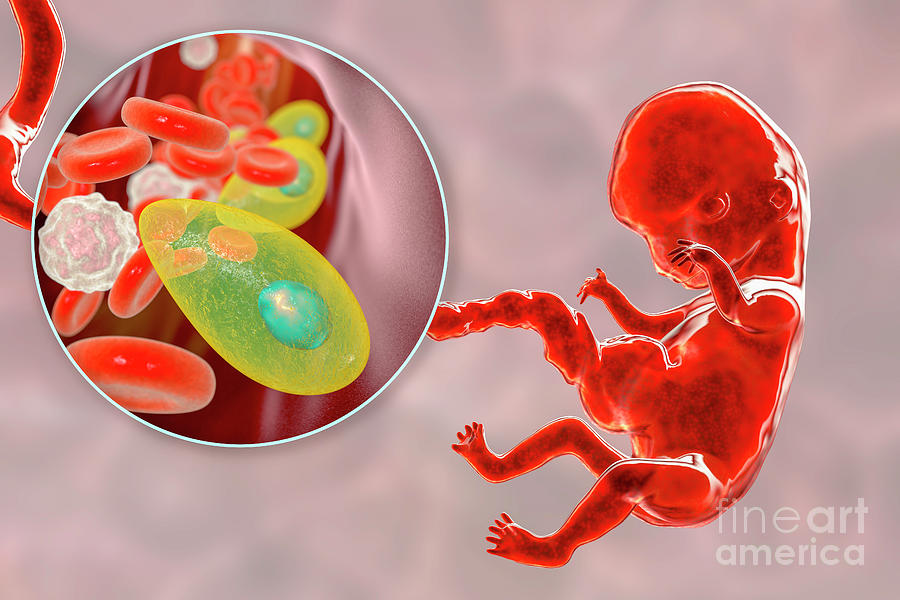 Danish Congenital Toxoplasmosis Study Group. Lancet. 1999;353(9167):1834–7. [PubMed] [Google Scholar]
Danish Congenital Toxoplasmosis Study Group. Lancet. 1999;353(9167):1834–7. [PubMed] [Google Scholar]
9. Vogel N, Kirisits M, Michael E, Bach H, Hostetter M, Boyer K, et al. Congenital toxoplasmosis transmitted from an immunologically competent mother infected before conception. Clin Infect Dis. 1996;23(5):1055–60. [PubMed] [Google Scholar]
10. Gavinet MF, Robert F, Firtion G, Delouvrier E, Hennequin C, Maurin JR, et al. Congenital toxoplasmosis due to maternal reinfection during pregnancy. J Clin Microbiol. 1997;35(5):1276–7. [PMC free article] [PubMed] [Google Scholar]
11. McAuley J, Boyer KM, Patel D, Mets M, Swisher C, Roizen N, et al. Early and longitudinal evaluations of treated infants and children and untreated historical patients with congenital toxoplasmosis: the Chicago Collaborative Treatment Trial. Clin Infect Dis. 1994;18(1):38–72. [PubMed] [Google Scholar]
12. Swisher CN, Boyer K, McLeod R. Congenital toxoplasmosis. The Toxoplasmosis Study Group. Semin Pediatr Neurol.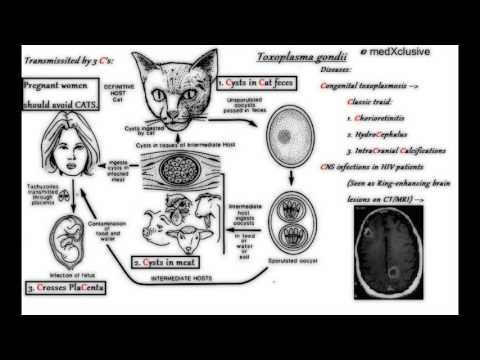 1994;1(1):4–25. [PubMed] [Google Scholar]
1994;1(1):4–25. [PubMed] [Google Scholar]
13. Dunn D, Wallon M, Peyron F, Petersen E, Peckham C, Gilbert R. Mother-to-child transmission of toxoplasmosis: risk estimates for clinical counselling. Lancet. 1999;353(9167):1829–33. doi: 10.1016/S0140-6736(98)08220-8. [PubMed] [CrossRef] [Google Scholar]
14. Berrébi A, Assouline C, Bessières MH, Lathière M, Cassaing S, Minville V, et al. Long-term outcome of children with congenital toxoplasmosis. Am J Obstet Gynecol. 2010;203(6):552.e1–6. doi: 10.1016/j.ajog.2010.06.002. Epub 2010 Jul 15. [PubMed] [CrossRef] [Google Scholar]
15. Wilson CB, Remington JS, Stagno S, Reynolds DW. Development of adverse sequelae in children born with subclinical congenital toxoplasma infection. Pediatrics. 1980;66(5):767–74. [PubMed] [Google Scholar]
16. Baquero-Artigao F, Del Castillo Martín F, Fuentes Corripio I, Goncé Mellgren A, Fortuny Guasch C, de la Calle Fernández-Miranda M, et al. The Spanish Society of Pediatric Infectious Diseases guidelines for the diagnosis and treatment of congenital toxoplasmosis [article in Spanish] An Pediatr (Barc) 2013;79(2):116.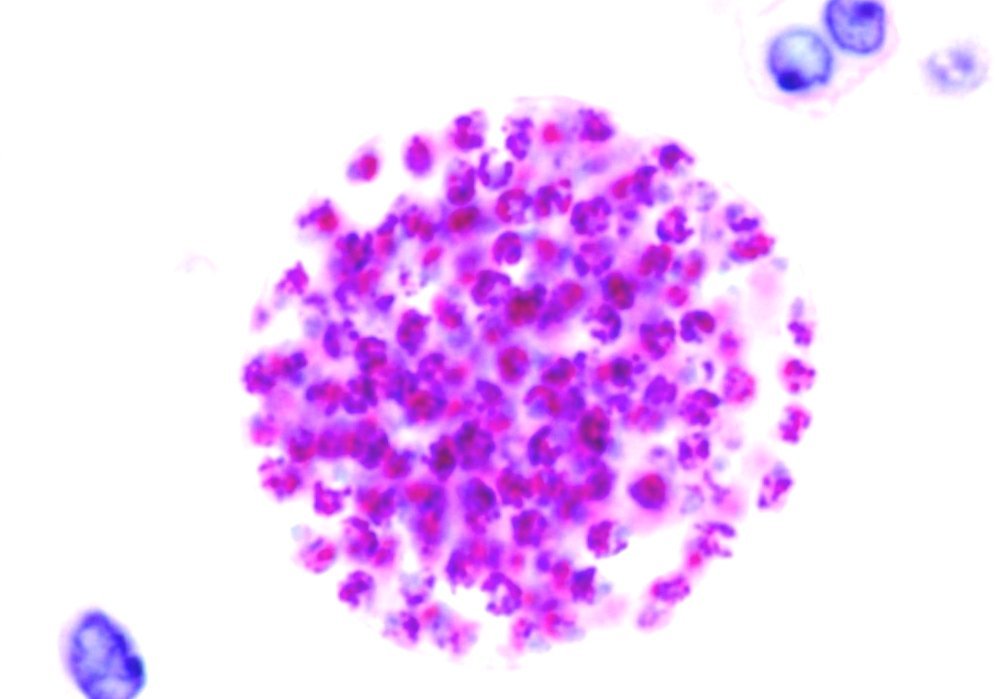 e1–16. doi: 10.1016/j.anpedi.2012.12.001. Epub 2013 Jan 23. [PubMed] [CrossRef] [Google Scholar]
e1–16. doi: 10.1016/j.anpedi.2012.12.001. Epub 2013 Jan 23. [PubMed] [CrossRef] [Google Scholar]
17. Stray-Pedersen B. Toxoplasmosis in pregnancy. Baillieres Clin Obstet Gynaecol. 1993;7(1):107–37. [PubMed] [Google Scholar]
18. Liesenfeld O, Press C, Montoya JG, Gill R, Isaac-Renton JL, Hedman K, et al. False-positive results in immunoglobulin M (IgM) toxoplasma antibody tests and importance of confirmatory testing: the Platelia Toxo IgM test. J Clin Microbiol. 1997;35(1):174–8. [PMC free article] [PubMed] [Google Scholar]
19. Hedman K, Lappalainen M, Seppäiä I, Mäkelä O. Recent primary toxoplasma infection indicated by a low avidity of specific IgG. J Infect Dis. 1989;159(4):736–40. [PubMed] [Google Scholar]
20. Iqbal J, Khalid N. Detection of acute Toxoplasma gondii infection in early pregnancy by IgG avidity and PCR analysis. J Med Microbiol. 2007;56(Pt 11):1495–9. doi: 10.1099/jmm.0.47260-0. [PubMed] [CrossRef] [Google Scholar]
21. Montoya JG. Laboratory diagnosis of Toxoplasma gondii infection and toxoplasmosis. J Infect Dis. 2002;185(Suppl 1):S73–82. doi: 10.1086/338827. [PubMed] [CrossRef] [Google Scholar]
J Infect Dis. 2002;185(Suppl 1):S73–82. doi: 10.1086/338827. [PubMed] [CrossRef] [Google Scholar]
22. Petersen E, Borobio MV, Guy E, Liesenfeld O, Meroni V, Naessens A, et al. European multicenter study of the LIAISON automated diagnostic system for determination of Toxoplasma gondii-specific immunoglobulin G (IgG) and IgM and the IgG avidity index. J Clin Microbiol. 2005;43(4):1570–4. doi: 10.1128/JCM.43.4.1570-1574.2005. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
23. Pour Abolghasem S, Bonyadi MR, Babaloo Z, Porhasan A, Nagili B, Gardashkhani OA, et al. IgG avidity test for the diagnosis of acute Toxoplasma gondii infection in early pregnancy. Iran J Immunol. 2011;8(4):251–5.IJIv8i4A8 [PubMed] [Google Scholar]
24. Merz E. Ultrasound in obstetrics and gynecology. Vol. 1: obstetrics. 2nd ed. New York, NY: Thieme; 2004. [Google Scholar]
25. Paquet C, Yudin MH. Toxoplasmosis in pregnancy: prevention, screening, and treatment. J Obstet Gynaecol Can.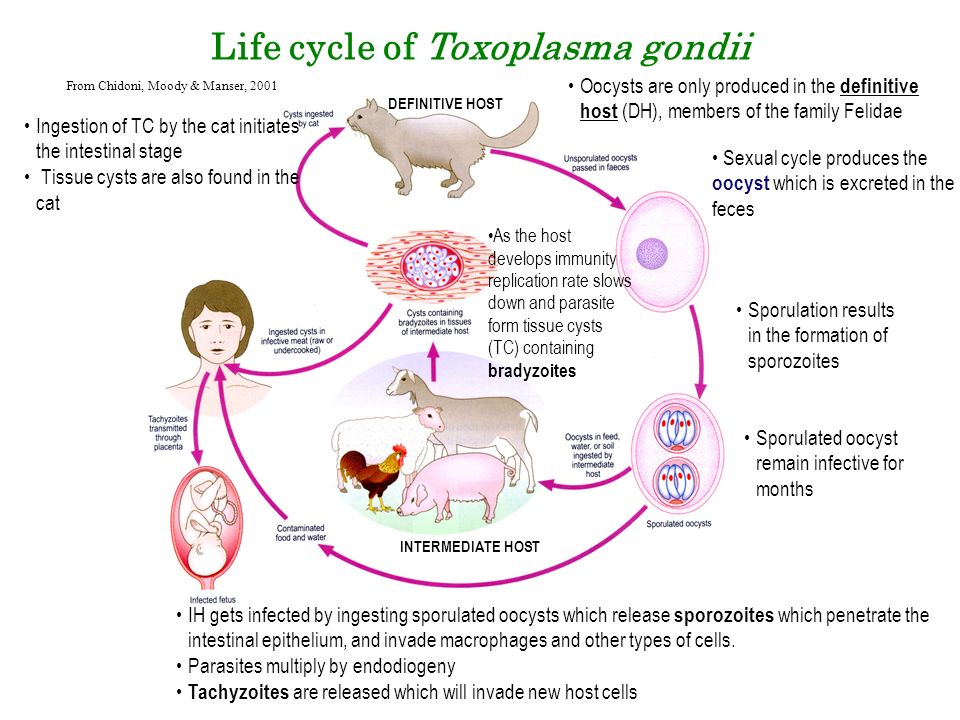 2013;35(1):78–9. [PubMed] [Google Scholar]
2013;35(1):78–9. [PubMed] [Google Scholar]
26. Wallon M, Liou C, Garner P, Peyron F. Congenital toxoplasmosis: systematic review of evidence of efficacy of treatment in pregnancy. BMJ. 1999;318(7197):1511–4. [PMC free article] [PubMed] [Google Scholar]
27. Peyron F, Wallon M, Liou C, Garner P. Treatments for toxoplasmosis in pregnancy. Cochrane Database Syst Rev. 2000;(2):CD001684. doi: 10.1002/14651858. CD001684. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
28. Montoya JG, Remington JS. Management of Toxoplasma gondii infection during pregnancy. Clin Infect Dis. 2008;47(4):554–66. doi: 10.1086/590149. [PubMed] [CrossRef] [Google Scholar]
29. McLeod R, Kieffer F, Sautter M, Hosten T, Pelloux H. Why prevent, diagnose and treat congenital toxoplasmosis? Mem Inst Oswaldo Cruz. 2009;104(2):320–44. [PMC free article] [PubMed] [Google Scholar]
30. Messier V, Lévesque B, Proulx JF, Rochette L, Libman MD, Ward BJ, et al. Seroprevalence of Toxoplasma gondii among Nunavik Inuit (Canada) Zoonoses Public Health.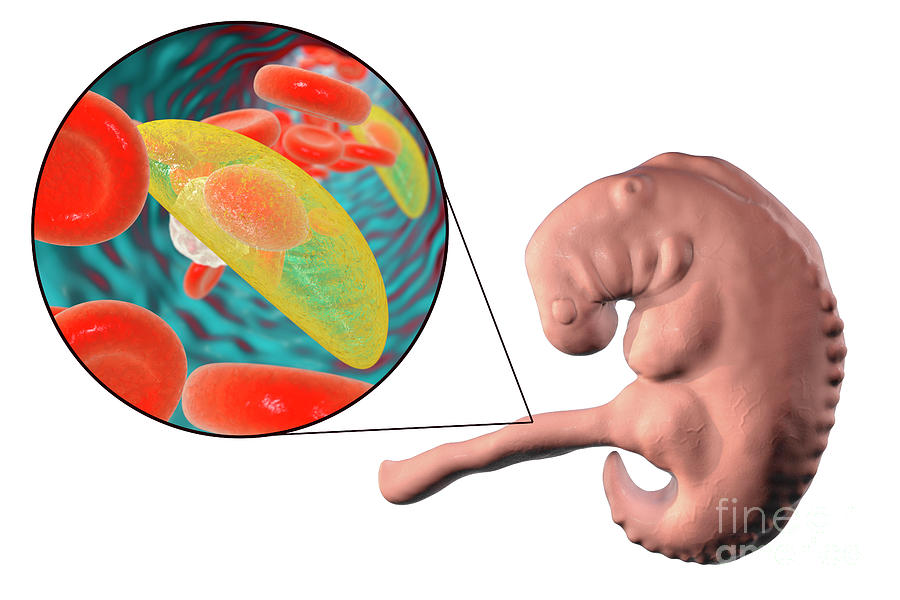 2009;56(4):188–97. doi: 10.1111/j.1863-2378.2008.01177.x. Epub 2008 Sep 22. [PubMed] [CrossRef] [Google Scholar]
2009;56(4):188–97. doi: 10.1111/j.1863-2378.2008.01177.x. Epub 2008 Sep 22. [PubMed] [CrossRef] [Google Scholar]
31. Cook AJ, Gilbert RE, Buffolano W, Zufferey J, Petersen E, Jenum PA, et al. Sources of toxoplasma infection in pregnant women: European multicentre case-control study. European Research Network on Congenital Toxoplasmosis. BMJ. 2000;321(7254):142–7. [PMC free article] [PubMed] [Google Scholar]
32. Elmore SA, Jones JL, Conrad PA, Patton S, Lindsay DS, Dubey JP. Toxoplasma gondii: epidemiology, feline clinical aspects, and prevention. Trends Parasitol. 2010;26(4):190–6. doi: 10.1016/j.pt.2010.01.009. Epub 2010 Mar 2. [PubMed] [CrossRef] [Google Scholar]
33. Jones JL, Krueger A, Schulkin J, Schantz PM. Toxoplasmosis prevention and testing in pregnancy, survey of obstetrician-gynaecologists. Zoonoses Public Health. 2010;57(1):27–33. doi: 10.1111/j.1863-2378.2009.01277.x. Epub 2009 Sep 10. [PubMed] [CrossRef] [Google Scholar]
Toxoplasmosis and pregnancy
Toxoplasmosis is one of the TORCH infections that is associated with one single sign - pathogens can be transmitted in utero: from mother to child. These infections are often the cause of problems with pregnancy and the culprits of congenital malformations in the baby.
These infections are often the cause of problems with pregnancy and the culprits of congenital malformations in the baby.
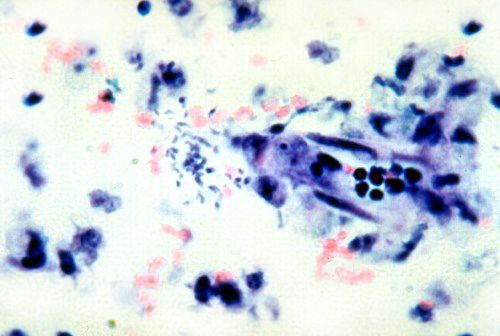
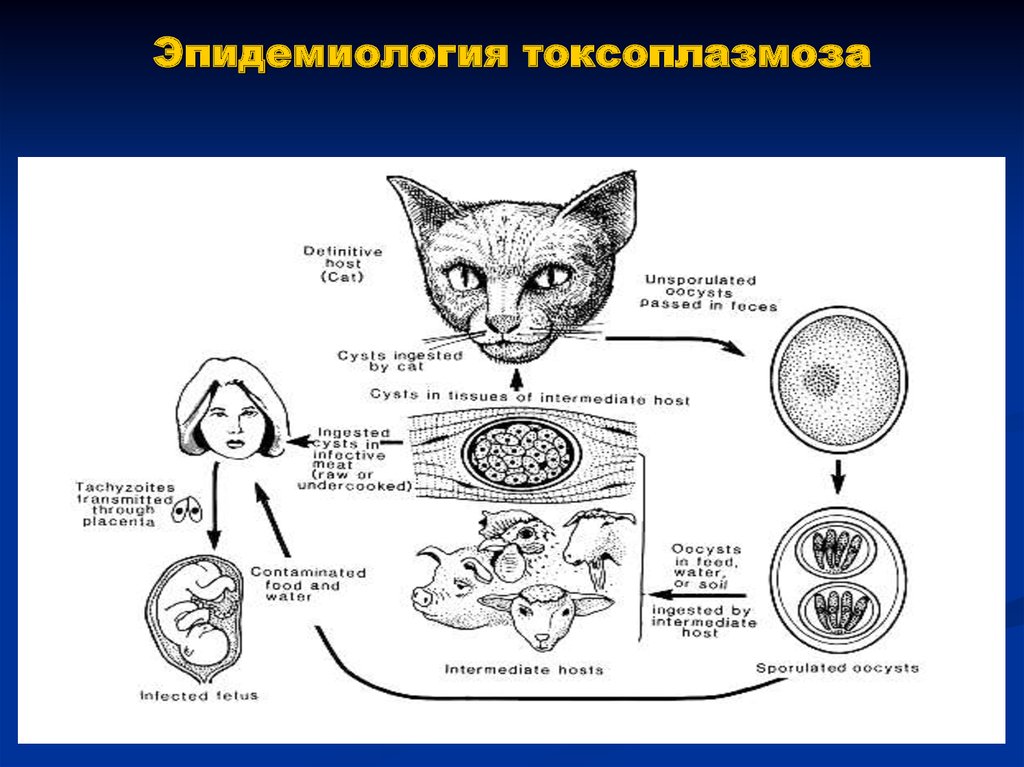
The causative agent of toxoplasmosis is a protozoan intracellular parasite - Toxoplasma gondii (Toxoplasma gondii) , the main source of which is domestic animals. The life cycle of Toxoplasma goes with the participation of the final and intermediate hosts. Toxoplasma gondii are definitive hosts of the feline family, while intermediate hosts are many species of mammals and birds. In cats, Toxoplasma parasites parasitize not only in organs and tissues (which is typical for diseased animals and humans), but also in the intestines. A sick cat pollutes the soil, lawns, fields and gardens with its feces. Toxoplasma with feces are excreted into the environment, where they retain their viability in the form of cysts for a year and a half and can cause disease if they enter the human body. Farm animals and birds become infected by eating grass contaminated with Toxoplasma cysts.
Accordingly, the following ways of infection of people are possible:
- consumption of undercooked or undercooked meat of animals and birds, unwashed vegetables, berries, herbs infected with toxoplasma;
- infection directly from a sick cat, but only if the pathogen, together with saliva, lacrimal fluid, cat urine, enters the human body through damaged skin and mucous membranes.
A sick person does not release the pathogen into the environment, therefore, no danger to others poses .
Toxoplasmosis is not sexually transmitted. In addition, not every person who has got Toxoplasma into the body needs to be treated. If the immune system of an infected person has built a reliable defense, he remains practically healthy. Transmission of the pathogen from person to person is possible only with organ transplantation (transplantation) from a donor with primary toxoplasmosis or congenital route (intrauterine infection of the fetus from the mother through the placenta).
Toxoplasmosis clinic
As mentioned above, in the vast majority of cases, the penetration of toxoplasma into the human body does not lead to the development of the disease, at least clinically expressed disease. Whether a person gets sick or not depends on the degree of pathogenicity of the pathogen itself, the amount of toxoplasma that has penetrated the body and on the state of the defenses of the human body itself.
Usually, if the disease develops, it is not severe, and very often it is so easy that it goes unnoticed, as a result of the fact that a person has been ill with toxoplasmosis, they learn by chance, according to the conclusion of a blood test.
As a rule, acute toxoplasmosis is disguised as SARS: the patient's temperature rises, sometimes up to 38 degrees and above, the cervical and occipital lymph nodes increase, headache and muscle pain appear, sweating, general weakness. After a week, the above symptoms disappear.
If the body is weakened, the likelihood of developing the disease increases. In this case, from the gastrointestinal tract, toxoplasma enters the lymph and blood, they are carried by their current throughout the body, affecting various organs and tissues, primarily the brain, eyes, heart, and muscles.
In this case, from the gastrointestinal tract, toxoplasma enters the lymph and blood, they are carried by their current throughout the body, affecting various organs and tissues, primarily the brain, eyes, heart, and muscles.
In a severe course of the disease, encephalitis, meningoencephalitis may develop, which are accompanied by a sharp headache, seizures, loss of consciousness. But this is extremely rare.
Thus, toxoplasmosis is one of those diseases that people get sick once in a lifetime and so easily that they often do not even notice it. After the illness, persistent immunity remains for life, respectively, there can be no consequences of the disease, nor secondary infection.
Clinical manifestations of toxoplasmosis in pregnant women and newborns
Despite the fact that infection with Toxoplasma is a trifle for most people, for a pregnant woman it is a real disaster.
Primary exposure to toxoplasmosis during pregnancy is the only situation in which toxoplasmosis poses a serious risk.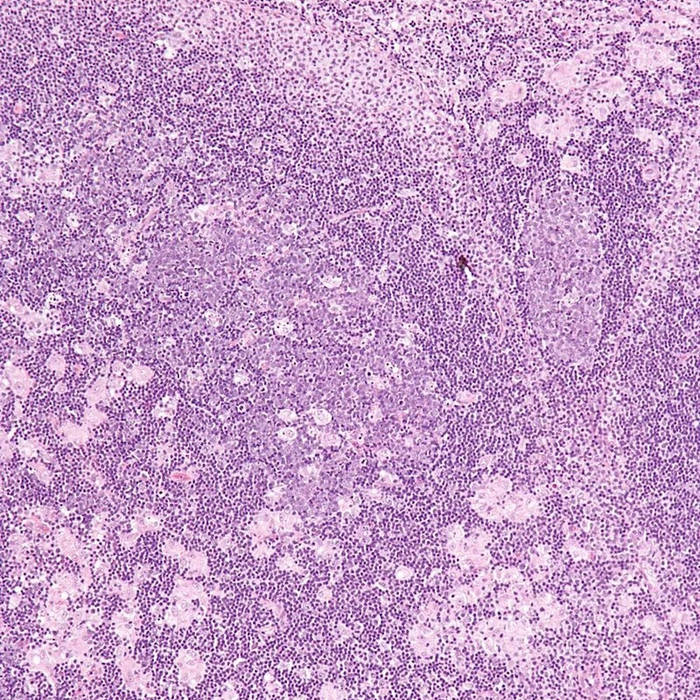 Frankly speaking, the probability of such an infection is not great - according to statistics, no more than 1% of women become infected with toxoplasmosis during pregnancy, in other words, this is one pregnant woman out of a hundred.
Frankly speaking, the probability of such an infection is not great - according to statistics, no more than 1% of women become infected with toxoplasmosis during pregnancy, in other words, this is one pregnant woman out of a hundred.
In addition, about 63% of women who have already developed immunity to toxoplasmosis in Belarus. Moreover, even if the mother is infected with toxoplasmosis, intrauterine infection does not always occur (!). The probability of infection of the baby depends on how long the pregnancy Toxoplasma entered the body of a pregnant woman.
There is a certain dependence:
- the earlier the gestational age, the greater the risk of severe consequences when the fetus is infected with toxoplasmosis and the less the likelihood of infection itself;
- The later in pregnancy infection occurs, the higher the rate of transmission of toxoplasmosis to the fetus and the lower the risk of severe fetal injury.
So if the infection of the mother occurred in the first trimester of pregnancy, the probability of overcoming the placental barrier by toxoplasma is small (about 15%), since the placenta is still not very permeable to pathogens. In this case, everything can end well (a healthy baby will be born), or a spontaneous abortion will occur due to the development of defects incompatible with the life of the baby.
In this case, everything can end well (a healthy baby will be born), or a spontaneous abortion will occur due to the development of defects incompatible with the life of the baby.
In the second trimester, toxoplasma enters the blood of the fetus more easily, as a result of which the likelihood of congenital toxoplasmosis increases to 20%. If infection of the fetus has occurred, the pathogens will accumulate and multiply in the brain, affecting the eyes and the central nervous system of the fetus. The immune system will soon cope with the disease and destroy all pathogens in the body, but some of the child's cells will be destroyed. As a result, increased intracranial pressure, mental retardation, epilepsy and blindness. That is why, when infected with toxoplasmosis at the initial stage of pregnancy, a pregnant woman is often offered to make an artificial termination of pregnancy.
By the third trimester, the probability of infection increases to 50-60%, but the fetus is already more resistant to the destructive effects of Toxoplasma - the baby can be born without any visible abnormalities, and the consequences of the infection may appear months or even years later.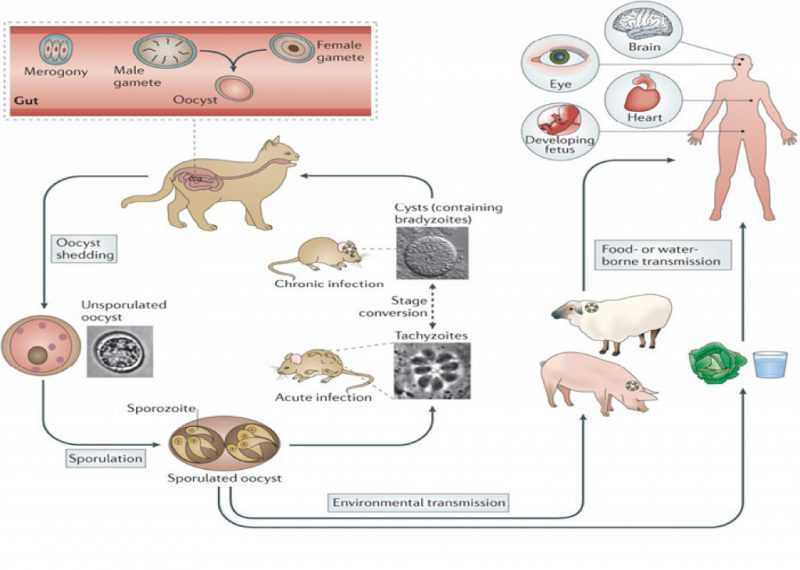
Signs of congenital toxoplasmosis at birth may include fever, rash, enlargement of the liver and spleen, microcephaly, seizures, jaundice, changes in blood tests. The so-called classical triad of congenital toxoplasmosis includes chorioretinitis, hydrocephalus, and the presence of intracranial calcifications.
With timely treatment, the risk of infection of the baby is only 1-5%. It is important to emphasize once again that the danger is only toxoplasmosis, which the woman contracted during the current pregnancy. Accordingly, if a woman has already had toxoplasmosis before pregnancy (at least three months before her), her unborn child is not threatened by toxoplasmosis. In a situation where a woman loses a child due to toxoplasmosis during pregnancy, after six months she can become pregnant again, no longer fearing toxoplasmosis (!).
Prophylactic treatment to prevent congenital toxoplasmosis not available ! If a proven infection of a pregnant woman occurred in the 1st trimester of pregnancy, as a rule, it is recommended to terminate the pregnancy, and if there is a threat of miscarriage, it is not saved.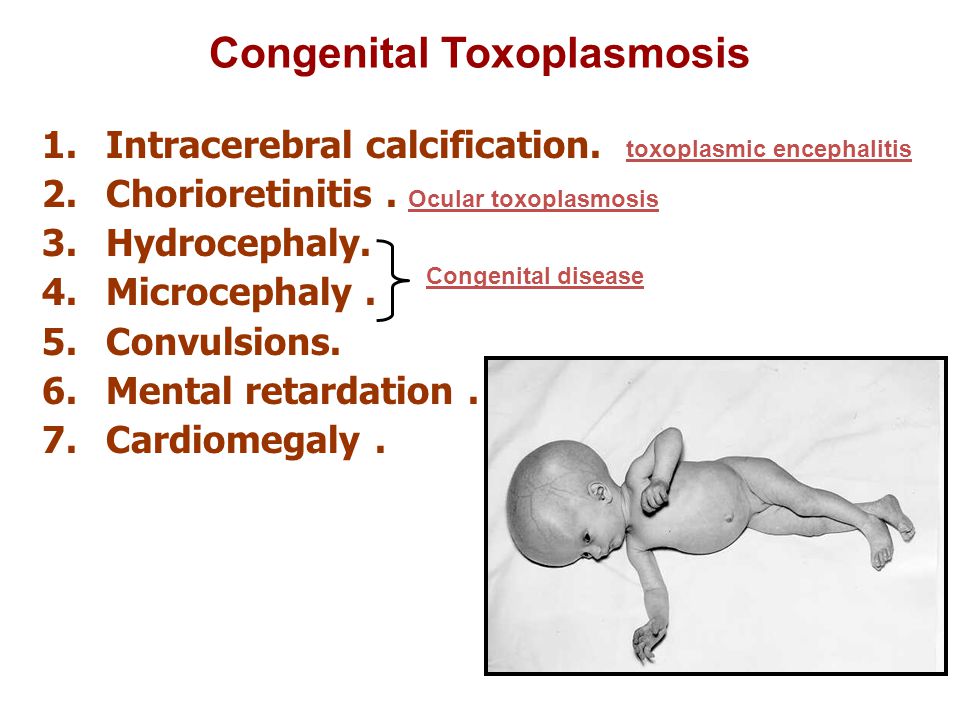 In case of infection in the second trimester, which is reliably diagnosed, an additional examination of the fetus is indicated. It includes: Ultrasound, detection of Toxoplasma in the amniotic fluid (amniocentesis + culture analysis or PCR).
In case of infection in the second trimester, which is reliably diagnosed, an additional examination of the fetus is indicated. It includes: Ultrasound, detection of Toxoplasma in the amniotic fluid (amniocentesis + culture analysis or PCR).
If the fetus is proven to be infected, abortion is also recommended.
In case of refusal to interrupt, specific therapy is carried out with drugs that are detrimental to toxoplasma.
Pregnant women should not be treated before 12-16 weeks of pregnancy. At the same time, correction of violations of various organs is carried out, which requires an individual approach to each patient. When infected in the third trimester, abortion is not carried out, specific therapy is used. As mentioned above, timely therapy significantly increases the likelihood of having a healthy baby. If the trouble, nevertheless, came, the treatment of newborns with confirmed toxoplasmosis is mandatory, as well as observation during the year. In the case of a primary infection of a pregnant woman with toxoplasmosis, regardless of the outcome of the pregnancy, one can be sure that at least the next child will not be afraid of congenital toxoplasmosis, thanks to the immunity acquired by the mother.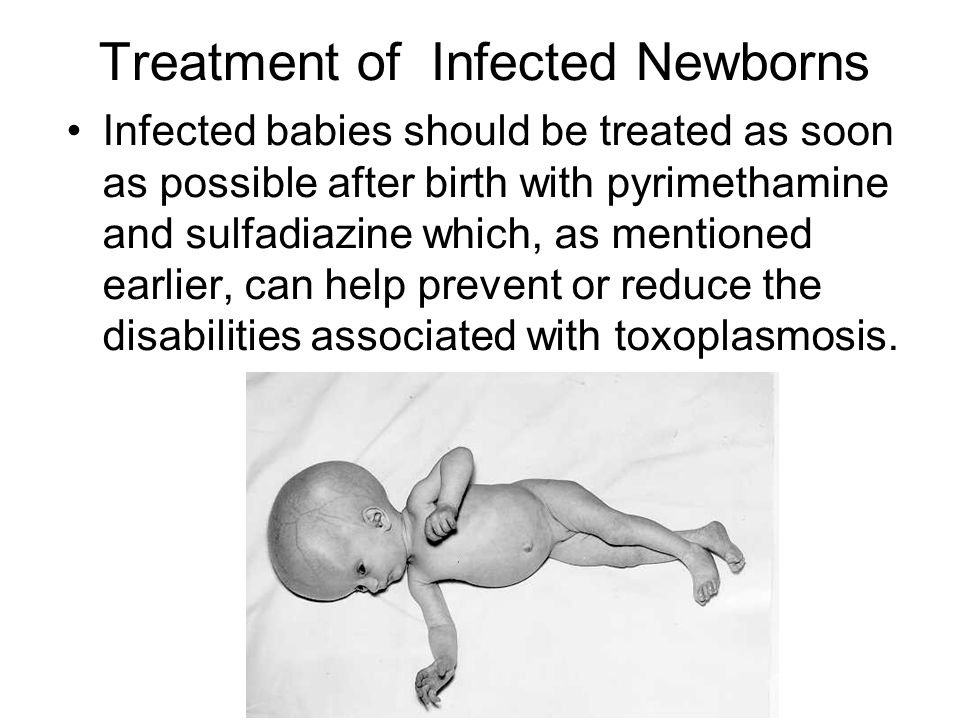
Memo for seronegative infection T . Gondii pregnant woman
- Avoid tasting raw minced meat.
- Do not taste meat during cooking.
- Wear gloves when handling soil. Wash your hands with soap and water after any contact with soil, sand, raw meat of any animal, and unwashed vegetables.
- Prepare your meat fully cooked: there should be no pink color and no bloody meat juice! Frozen meat for several days significantly reduces the risk of infection.
- Do not drink unpasteurized milk.
- Wash all cutting boards and knives thoroughly after each use.
- Wash or peel all fruits and vegetables before eating.
- Do not drink water from an unverified source.
- Do not let domestic cats outside and do not stroke stray cats, kittens and dogs. Feed cats only canned or dry food or well-cooked food.
- Avoid contact with cat litter, if this is not possible, use gloves, wash your hands thoroughly.
- Remove cat feces from the litter box daily.
Thus, if you are planning a pregnancy - diagnose toxoplasmosis, and then get pregnant, wear it calmly, give birth easily and raise a healthy baby! Good luck to you!
Obstetrician-gynecologist
Elena Viktorovna Borovskaya
Toxoplasmosis during pregnancy - Yunona
Toxoplasmosis during pregnancy - Yunona -->home
Articles
Toxoplasmosis during pregnancy
Toxoplasmosis during pregnancy is dangerous. Its pathogen belongs to the group TORCH infections that can penetrate the fetus through the placenta and cause Problems. From the article you will learn more about toxoplasmosis - how to identify and when to treat.
Contents of the article
How you can get toxoplasmosis
The causative agent is Toxoplasma (the simplest intracellular parasite). Its carriers are mostly domestic animals.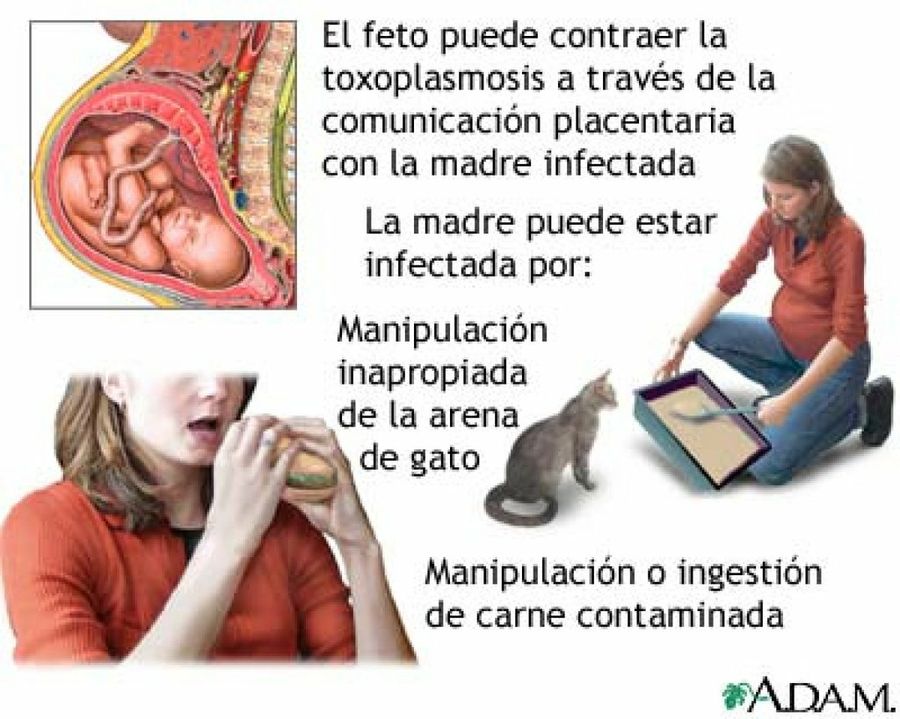 Toxoplasma finally settles in the body of cats, but can choose birds and mammals as an intermediate place of residence. Sick animals infect the soil, grass, vegetable gardens.
Toxoplasma finally settles in the body of cats, but can choose birds and mammals as an intermediate place of residence. Sick animals infect the soil, grass, vegetable gardens.
The main ways of infection with toxoplasmosis during pregnancy:
- eating poorly cooked or raw meat, as well as unwashed vegetables, herbs;
- work with the earth, for example in a vegetable garden;
- interaction with cat waste products;
- organ transplant, blood transfusion;
- in utero - from mother to fetus.
The causative agent is not transmitted from a sick person through sexual or airborne droplets. During pregnancy, 1% of women become infected with toxoplasmosis, while 20% pass the infection to the fetus.
Causes of toxoplasmosis during pregnancy
If a woman had an infection long before pregnancy - in childhood or adolescence, then the disease is not dangerous for her. After suffering toxoplasmosis, antibodies are formed that protect the mother and baby.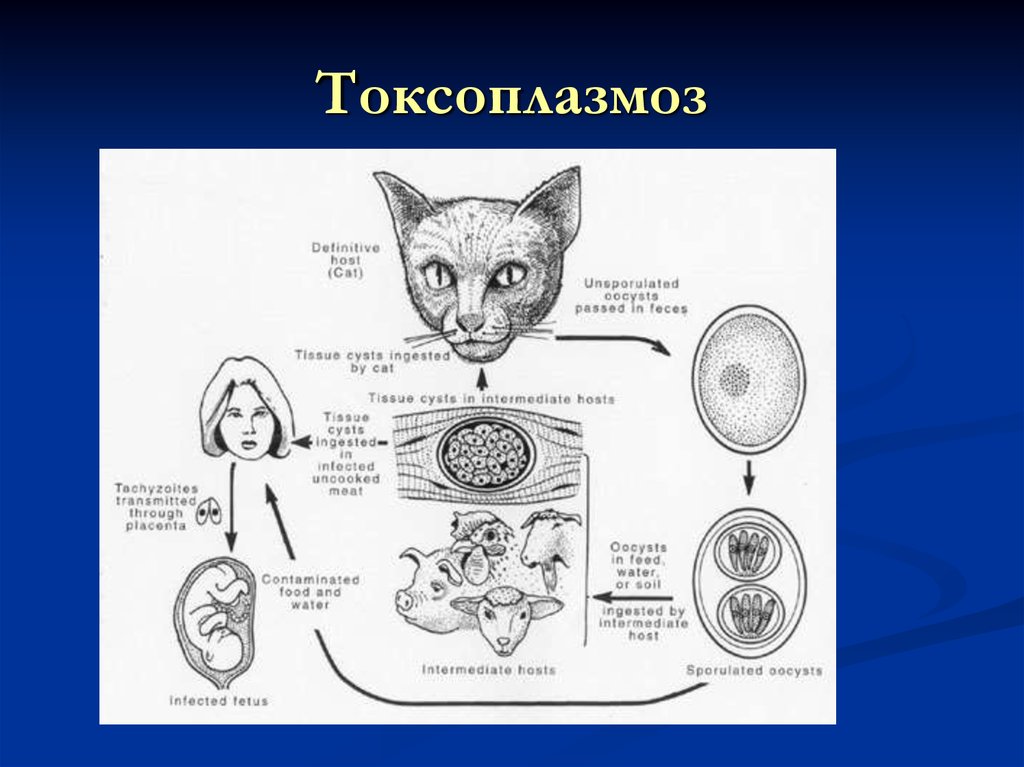
However, if the infection occurred within six months before conception, the health of the mother and child may be at risk. It takes time for the formation of antibodies - at least 6 months after the disease. Accordingly, when they are not there yet, the pathogen can re-penetrate and harm the fetus.
There are also cases of chronic toxoplasmosis - when the infection proceeds in a latent form and is activated when immunity is reduced in pregnant women.
During pregnancy, contact with animals should be avoided, and, if possible, visiting regions with a high prevalence of toxoplasma: Africa, the Middle East and Latin America should be excluded.
Symptoms of toxoplasmosis in pregnant women
The infection has no pronounced manifestations. The most severe signs of toxoplasmosis in pregnant women appear in case of reduced immunity. In the acute course of the disease, the symptoms are similar to a viral disease (flu, SARS): the temperature rises to 38‒39degrees, the lymph nodes are enlarged, the woman feels weak and weak.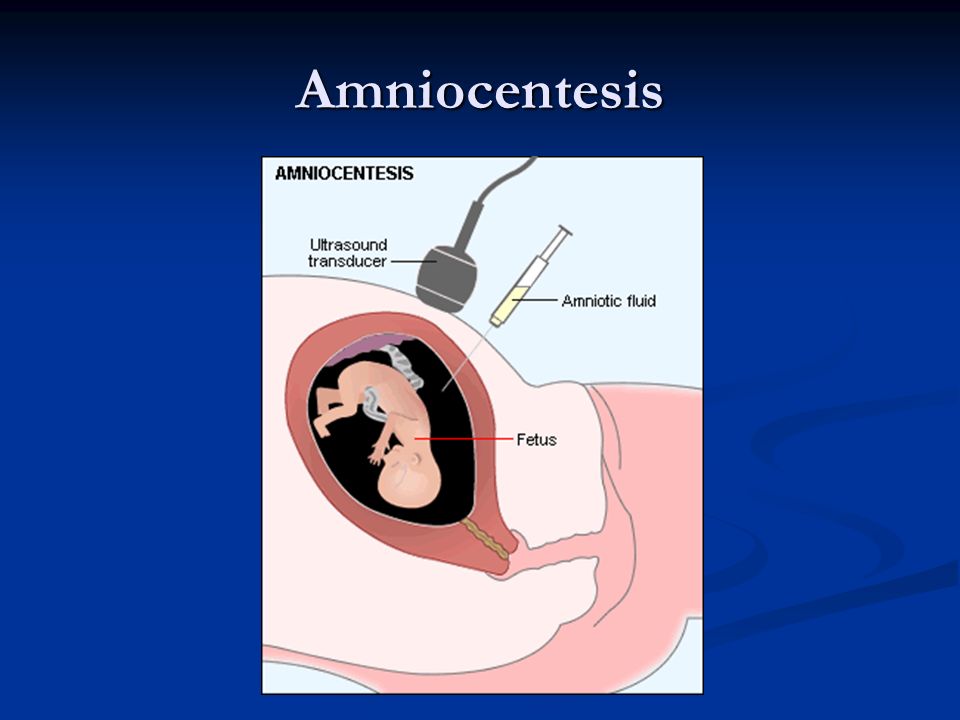 Headaches and muscle pain may also join.
Headaches and muscle pain may also join.
In most cases, the entry of the pathogen into the body does not cause the development of the disease. Toxoplasmosis manifests itself in a mild form, sometimes goes unnoticed, and a person learns about the disease from tests.
The likelihood of a more severe course increases if the body is weakened. Therefore, with toxoplasmosis in pregnant women, the likelihood of clinical complications is higher.
Fetal effects
In the first trimester, the greatest risk of severe consequences is when the fetus is infected, since the laying of organs and systems in the baby occurs. However, the risk of infection is lower. And at a later date, toxoplasmosis is less dangerous for the fetus, but it is easier for a woman to get infected with it.
The severity of the consequences depends on the gestational age:
- Up to 8-9 weeks, the risk is no more than 20%, but leads to severe malformations and even intrauterine death.
 Among the frequent consequences: stillbirth, absence of a brain in a child, hydrocephalus, liver enlargement, severe organic pathologies.
Among the frequent consequences: stillbirth, absence of a brain in a child, hydrocephalus, liver enlargement, severe organic pathologies. - At 9-18 weeks, the risk of infection is approximately 25%. The danger is in severe damage to the brain, liver, eyes, as well as the appearance of convulsive syndrome and fever in an infant.
- At 18–25 weeks, the risk is approximately 65%. Infection leads to dysfunction of organs in a child. Jaundice, anemia, enlargement of the liver, spleen are possible.
- At 26-40 weeks, the risk of infection of the fetus from the mother is high - up to 80%. Subsequently, the child may develop deafness, epileptic seizures, mental retardation.
If a child had an acute infection in the 2nd trimester, then more often at birth, chronic or overt (with severe clinical symptoms) toxoplasmosis is diagnosed. In the first case, complications may appear a few months after birth or already in adolescence.
If infected in the last weeks of pregnancy, a child is likely to be born with signs of acute congenital toxoplasmosis, accompanied by fever, rash, jaundice, pneumonia, and gastrointestinal upset.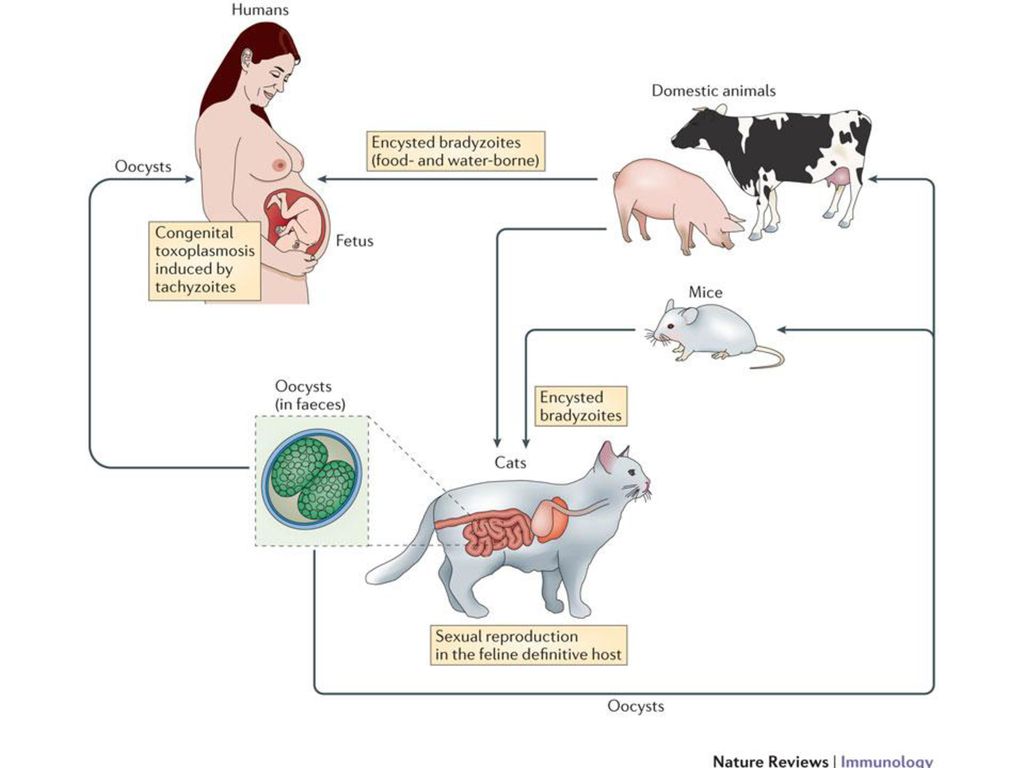
Diagnosis of toxoplasmosis during pregnancy
To reliably determine the infection, it is necessary to take tests. Laboratory diagnosis of toxoplasmosis is carried out by the methods of RNIF and ELISA. In the blood of a pregnant woman, the presence or absence of antibodies of class M and G is determined:
- If no antibodies are found, then the woman was not infected at all. This means that there is a risk of infection entering the body during pregnancy.
- If class G antibodies less than 40 U / ml are detected, it is possible to speak about the carriage of Toxoplasma without the risk of infection of the fetus.
- With G values over 200 U/ml and absence of M antibodies, the diagnosis is chronic acquired toxoplasmosis. In this case, specific treatment is not required.
- If both types of antibodies increase, the situation indicates an acute infection.
If there is no suspicion of pathology, the examination is carried out 1-2 times during pregnancy.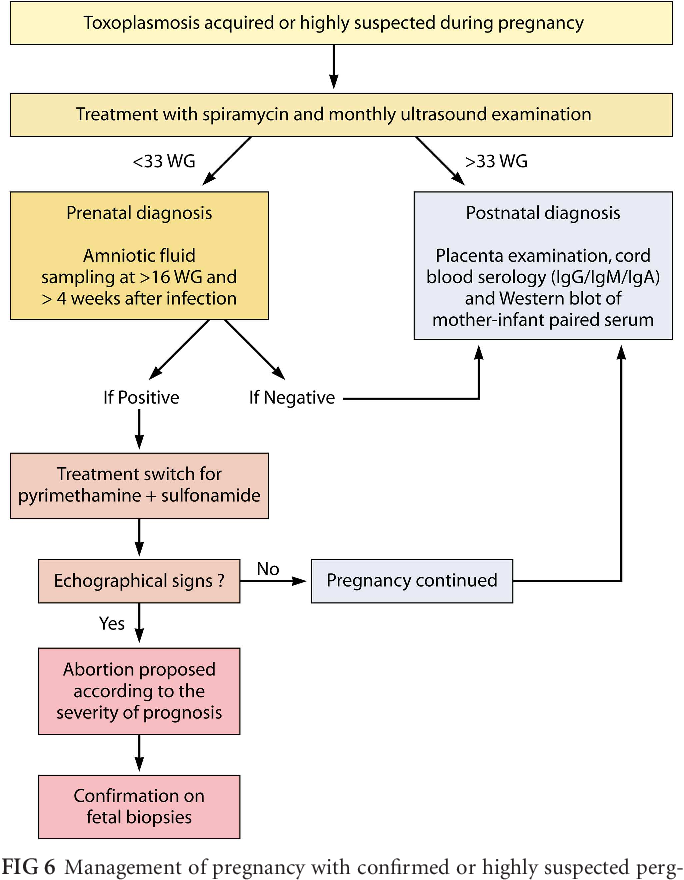 If there are warning signs, the doctor may prescribe to donate blood regularly. To detect intrauterine toxoplasmosis in children, amniocentesis (analysis of amniotic fluid), as well as cordocentesis (examination of umbilical cord blood), assess the likely signs of pathology on ultrasound. If an infection is detected in the fetus in combination with signs of damage on ultrasound, it is recommended to terminate the pregnancy.
If there are warning signs, the doctor may prescribe to donate blood regularly. To detect intrauterine toxoplasmosis in children, amniocentesis (analysis of amniotic fluid), as well as cordocentesis (examination of umbilical cord blood), assess the likely signs of pathology on ultrasound. If an infection is detected in the fetus in combination with signs of damage on ultrasound, it is recommended to terminate the pregnancy.
Treatment of toxoplasmosis in pregnant women
Treatment of pregnant women for the prevention of congenital toxoplasmosis in the fetus is not carried out. With proven infection of the expectant mother in the first trimester, it is recommended to terminate the pregnancy, and if there is a threat of miscarriage, preservation therapy is not carried out.
Starting from the second trimester, the question is whether to treat the pregnant woman:
- After 12 weeks, with a reliably accurate test result, an additional examination is carried out.
 In this case, interruption according to indications is also possible. But at such times, if a woman refuses to interrupt, the disease can be treated with specific drugs against Toxoplasma.
In this case, interruption according to indications is also possible. But at such times, if a woman refuses to interrupt, the disease can be treated with specific drugs against Toxoplasma. - A gynecologist and an infectious disease specialist are involved in the treatment. Therapy involves taking strong antibacterial drugs, in some cases, antimalarial and antiparasitic drugs are used. You can start drinking such medicines no earlier than 12-16 weeks.
- The treatment has side effects, so the doctor individually determines the dosage, correlates the risk and benefit, and makes important recommendations. Therapy has been shown to reduce the risk of infant mortality and neurological damage from congenital toxoplasmosis.
- Chronic toxoplasmosis is treated before or after pregnancy. In the absence of complaints and clinical manifestations in the mother and fetus, the woman is observed, but specific therapy is not prescribed.
Toxoplasmosis in pregnant women is not an indication for caesarean section.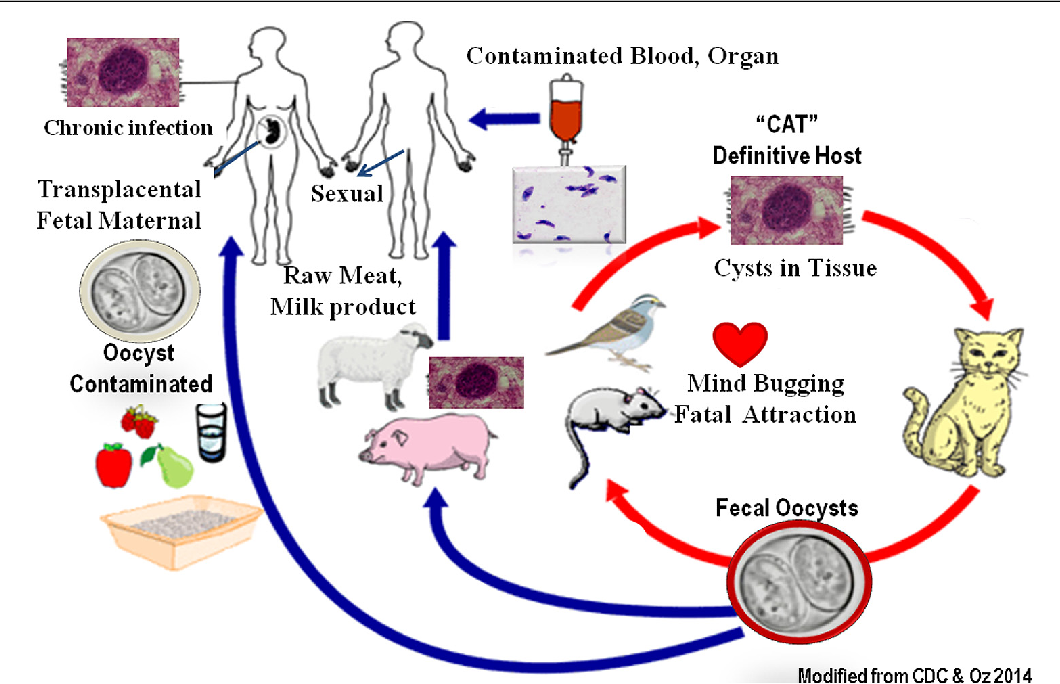 A woman can give birth naturally.
A woman can give birth naturally.
Prophylaxis
Tips to help reduce the chance of infection during pregnancy:
- Maintain good personal hygiene. Wash your hands before and after eating, and especially after interacting with any pets and visiting public places.
- Eat only well-done or long-cooked meat, wash vegetables and fruits thoroughly with boiled water.
- Avoid close contact with cats, especially outdoor cats, do not litter box.
- Regularly undergo examinations: screenings, tests, ultrasound.
- Wear gloves when working on the ground or in sand.
The danger of infection is not so great, but if you are planning a pregnancy or are already in happy expectation, keep your finger on the pulse. It is much easier to take the proper steps to avoid contracting a dangerous infection than to try to treat it during pregnancy. Take care of yourself and your future baby!
Other articles
08/17/2022
Perinatal screening of the 1st trimester of pregnancy
Perinatal screening of the 1st trimester of pregnancy - what are the features? What is important for a future mother to know? We tell you all the important details in our article!
08/05/2022
Insomnia during pregnancy
The need for proper sleep is a natural desire of the body.