What can i do to have a healthy pregnancy
12 Ways to Stay Healthy During Pregnancy
Audra Meadows, MD, MPH, an obstetrician at Brigham and Women’s Hospital, helps patients optimize their health before, during and after pregnancy. Here are 12 tips from Dr. Meadows to help you increase your chances of having a healthy pregnancy and a healthy baby.
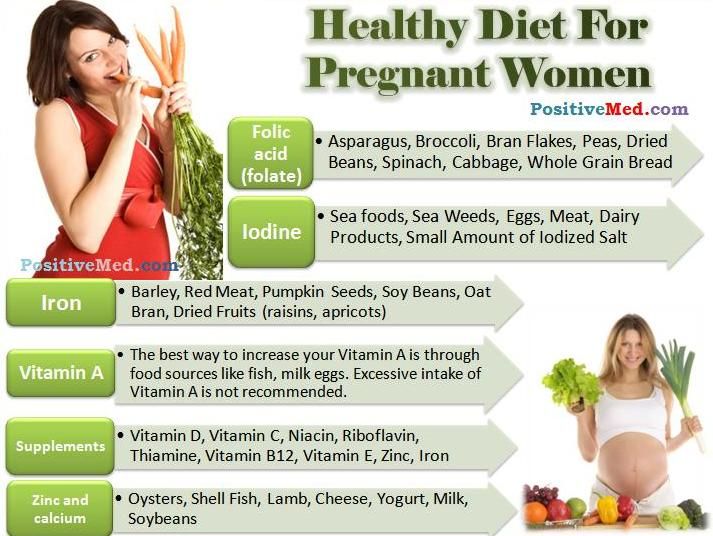
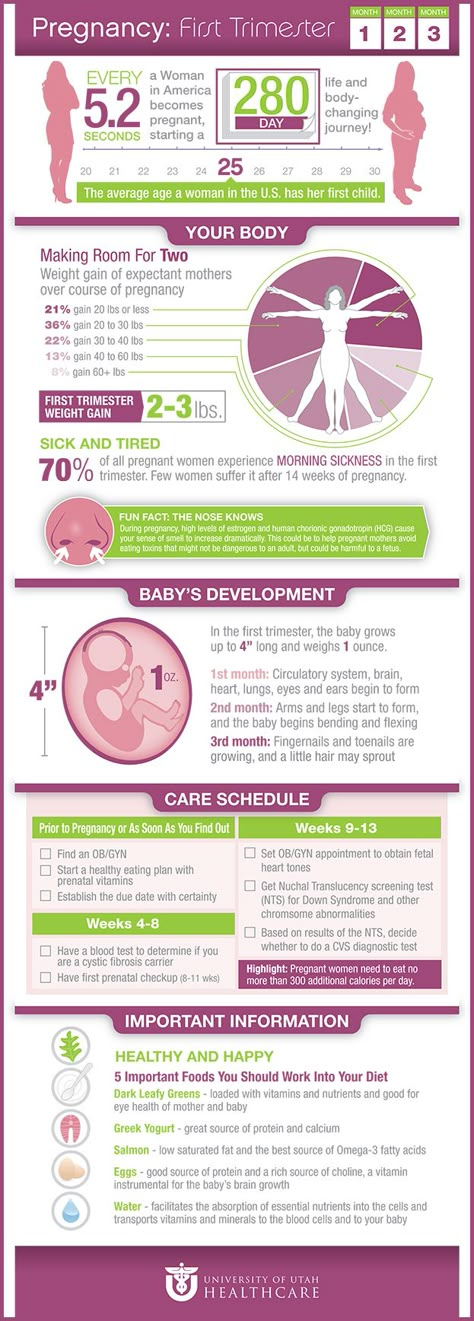
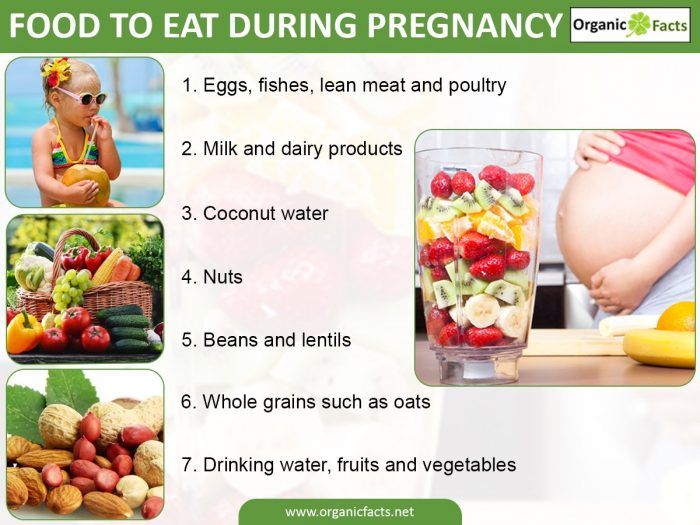
1. Eat healthy foods.
Eating healthy foods is especially important for pregnant women. Your baby needs nutrients to grow healthy and strong in the womb. Eat plenty of colorful fruits and vegetables, whole grains, calcium-rich foods and foods low in saturated fat.
2. Take a daily prenatal vitamin.
Taking a daily prenatal multivitamin can help ensure you get the right amount of the key nutrients you and your baby need during pregnancy. These include folic acid, iron and calcium.
3. Stay hydrated.
A pregnant woman’s body needs more water than it did before pregnancy. Aim for eight or more cups each day.
4. Go to your prenatal care checkups.
Women should get regular prenatal care from a health care provider. Moms who don’t get regular prenatal care are much more likely to have a baby with low birth weight or other complications. If available, consider group prenatal care.
5. Avoid certain foods.
There are certain foods that women should avoid eating while pregnant. Don’t eat:
- Raw or rare meats
- Liver, sushi, raw eggs (also in mayonnaise)
- Soft cheeses (feta, brie)
- Unpasteurized milk
Raw and unpasteurized animal products can cause food poisoning. Some fish, even when cooked, can be harmful to a growing baby because they’re high in mercury.
6. Don’t drink alcohol.
Don’t drink alcohol before and during pregnancy and while breastfeeding. Drinking alcohol increases the risk of having a baby with fetal alcohol spectrum disorder (FASD). FASD can cause abnormal facial features, severe learning disabilities and behavioral issues.
Alcohol can impact a baby’s health in the earliest stages of pregnancy, before a woman may know she is pregnant. Therefore, women who may become pregnant also should not drink alcohol.
Therefore, women who may become pregnant also should not drink alcohol.
7. Don’t smoke.
Smoking is unhealthy for you and your unborn child. It increases the risk of sudden infant death syndrome (SIDS), premature birth, miscarriage and other poor outcomes.
8. Get moving.
Daily exercise or staying active in other ways can help you stay healthy during pregnancy. Check with your doctor to find out how much physical activity is right for you.
9. Get a flu shot.
The flu can make a pregnant woman very sick and increase risks of complications for your baby. The flu shot can protect you from serious illness and help protect your baby after birth, too. Ask your doctor about getting a flu shot.
10. Get plenty of sleep.
Ample sleep (7 to 9 hours) is important for you and your baby. Try to sleep on your left side to improve blood flow.
11. Reduce stress.
Reducing stress is crucial for improving birth outcomes. Pregnant women should avoid, as much as they can, stressful situations. Recruit your loved ones to help you manage stress in your life.
Recruit your loved ones to help you manage stress in your life.
12. Plan the right time to get pregnant.
“If you are choosing to become pregnant at a time when you know that you’re at your healthiest, that increases your chances of having a healthy pregnancy and a healthy birth,” says Dr. Meadows.
This not only means that women should make sure that they are healthy before they become pregnant, but they also should consider their age before getting pregnant. Mothers who have children early in life (earlier than 16-years-old), or late in life (older than 40) are at greater risk for having a premature birth. Also, women who become pregnant again too soon (less than 18 months in between births) are even more likely to have a premature baby.
Audra Meadows, MD, MPH
Audra Meadows, MD, MPH is an obstetrician at Brigham and Women’s Hospital (BWH).
Before you go,
If you’re thinking about pregnancy, managing a pregnancy complication or looking for tips on newborn care, our experts can help support you at every step in your journey.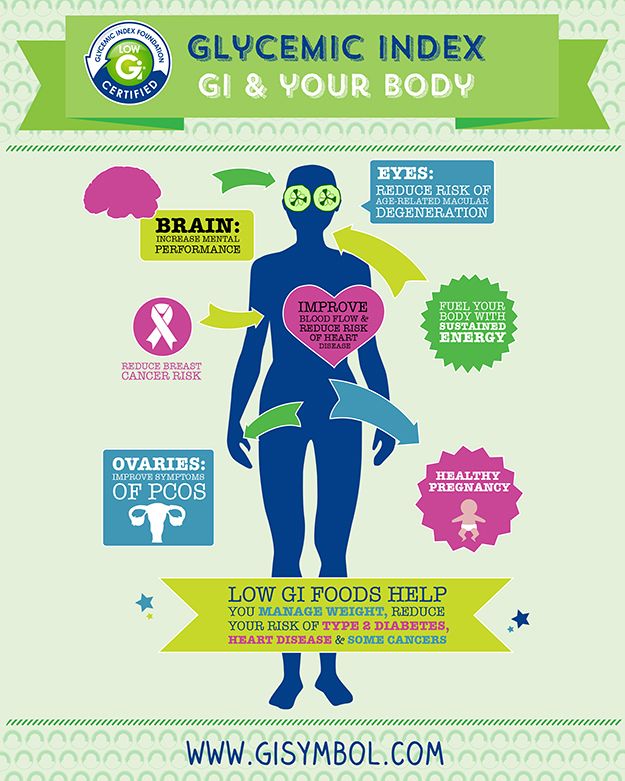 Read more pregnancy and childbirth articles.
Read more pregnancy and childbirth articles.
Learn more about the Department of Obstetrics and Gynecology
Request an Appointment
Have a Healthy Pregnancy - MyHealthfinder
- The Basics
- Take Action
The Basics
Overview
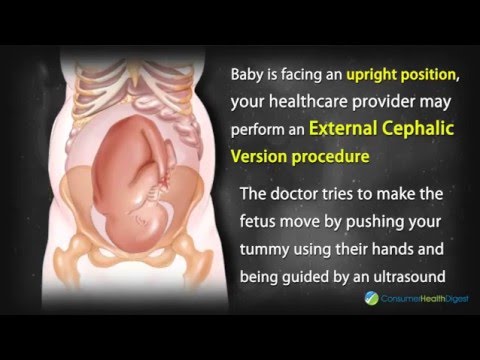
Health care during pregnancy is called prenatal care. Getting prenatal care can help you have a healthier baby. It also lowers the risk of your baby being born too early, which can lead to health problems for your baby.
During prenatal care, your doctor or midwife can find any health problems that may come up. A midwife is a health professional who provides health care during pregnancy and helps pregnant people during childbirth.
Get regular prenatal checkups.
Schedule a visit with your doctor or midwife as soon as you know you're pregnant — or if you think you might be. You'll need many checkups with your doctor or midwife during your pregnancy. Don't miss any of these appointments — they're all important.
Be sure to get all the medical tests that your doctor or midwife recommends. Early treatment can cure many problems and prevent others.
Take steps to have a healthy pregnancy.
To keep you and your baby healthy, it's important that you:
- Don’t smoke or drink alcohol
- Eat healthy and get enough folic acid
- Stay physically active
Get more tips for a healthy pregnancy:
- If you just learned that you're pregnant, find out what to do next
- Check out these tips for staying healthy and safe during pregnancy
Topics to Discuss
Make the most of each visit with the doctor or midwife.
Talk with your doctor or midwife about:
- Your personal and family health history, including any chronic (long-term) health problems or surgeries you've had
- When you need to get medical care for issues that can come up — like high blood pressure, dizziness, swelling, pain, bleeding, or contractions
- When and where to go for emergency care during your pregnancy
- Any prescription and over-the-counter medicines that you take — as well as vitamins, supplements, and herbs
- Healthy weight gain during pregnancy
These visits are also a great time to discuss:
- Questions you have about pregnancy, childbirth, and breastfeeding
- How to get help buying food if you need it — including how to get help from a program called WIC (Women, Infants, and Children)
- Anything that’s bothering or worrying you
If you're worried about your health during pregnancy, don't wait to ask for help.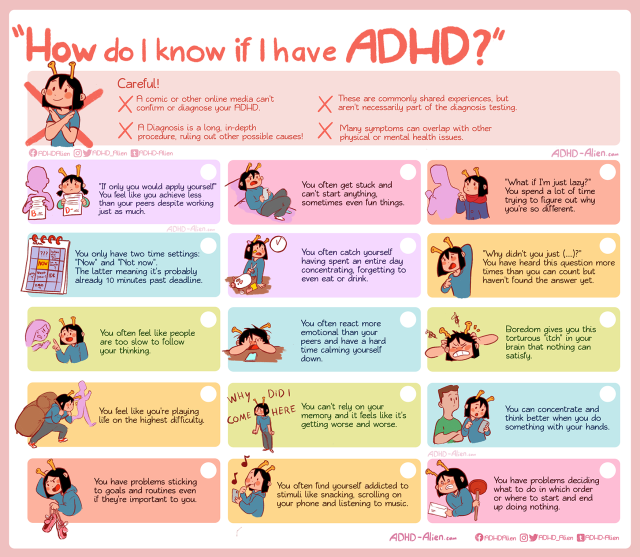 Learn more about pregnancy complications and when to call your doctor or midwife.
Learn more about pregnancy complications and when to call your doctor or midwife.
Make a birth plan.
A birth plan describes what you want to happen during childbirth and after your baby's birth. It can include:
- Where you'd like to give birth — for example, at a hospital or birthing center
- Who you want with you for support (like your partner, family member, or close friend) before, during, and after childbirth
- How you want to manage pain during childbirth
- Who you want to help you make important medical decisions during childbirth
- Your plan to breastfeed after your baby is born
Talk with your doctor about depression.
Many people experience depression during and after pregnancy. Talk with your doctor about your risk for depression and whether you need counseling to help prevent it.
Medical Tests
Get important medical tests.
During your pregnancy, your doctor or midwife will recommend medical tests that all people need as part of routine prenatal care. You’ll need to get some tests more than once.
You’ll need to get some tests more than once.
These tests give your doctor or midwife important information about you and your baby. The tests will check your blood or urine (pee) for:
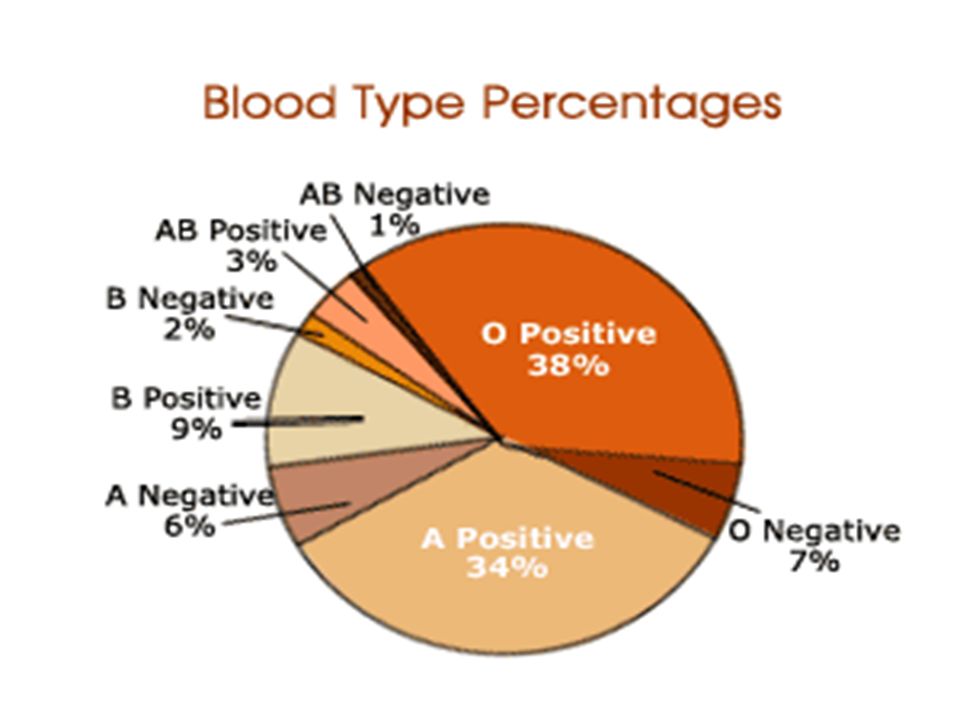
- Rh factor (a protein some people have in their blood)
- Hepatitis B [PDF - 859 KB]
- Urinary tract infection (UTI)
- Syphilis
- HIV
- Signs of past rubella infections (German measles)
- Group B strep
If you're younger than age 25 or have certain risk factors, your doctor or midwife may also check for other sexually transmitted diseases (STDs). Learn more about STDs during pregnancy.
Your doctor or midwife will also check your blood pressure regularly during your pregnancy. They may recommend that you check your own blood pressure at home using a monitor you can buy at a drug store. High blood pressure during pregnancy can be a sign of preeclampsia, a health problem that some pregnant people develop. Learn more about preventing preeclampsia.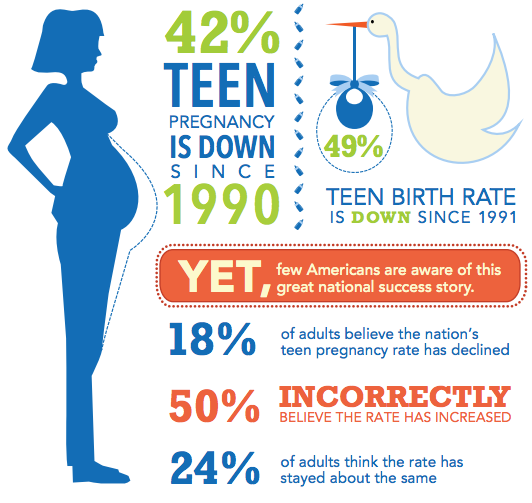
Talk about your family history.
Share your personal and family health history with your doctor or midwife. This will help you and your doctor or midwife decide whether you need any other tests, like genetic testing. Find out more about genetic testing.
Diabetes Testing
Get tested for gestational diabetes.
All pregnant people need to get tested for gestational diabetes between 24 and 28 weeks of pregnancy. Gestational diabetes is a type of diabetes that some people develop during pregnancy.
Pregnant people at high risk for type 2 diabetes may need to get tested earlier than people at normal risk. Find out about your risk for type 2 diabetes.
What do I need to know about gestational diabetes?
Gestational diabetes can lead to health problems for moms and babies — both during and after pregnancy. It’s important to get tested so that you and your doctor or midwife can take steps to protect you and your baby.
You're at higher risk for gestational diabetes if you:
- Are overweight or have obesity
- Have a family history of diabetes
- Are over age 25
- Are African American, Hispanic or Latino, American Indian, Alaska Native, Native Hawaiian, or Pacific Islander
- Had gestational diabetes during an earlier pregnancy
- Have had a baby weighing over 9 pounds
- Have polycystic ovary syndrome (PCOS)
You can reduce your risk for gestational diabetes by eating healthy and staying active during pregnancy.
- Learn more about gestational diabetes
- Ask your doctor about getting tested for gestational diabetes
Cost and Insurance
What about cost?
Under the Affordable Care Act, insurance plans must cover routine prenatal tests. Depending on your insurance plan, you may be able to get these tests at no cost to you. Check with your insurance company to find out more.
To learn more, check out these resources:
- Free preventive care for women covered by the Affordable Care Act
- How the Affordable Care Act protects you
- Understanding your health insurance and how to use it [PDF - 698 KB]
If you don’t have health insurance, you can still get help paying for medical care during pregnancy:
- Get connected with free or low-cost services in your state by calling 1-800-311-BABY (1-800-311-2229)
- Find a health center near you and ask about prenatal care
Learn more about health insurance options for pregnant people.
Take Action
Take Action
Get Prenatal Care
There are lots of things you can do today to help you have a healthy pregnancy and a healthy baby.
Get regular prenatal care.
Plan on getting a prenatal checkup at least once a month for the first 6 months (through week 28) — and more often during the last 3 months of your pregnancy (after week 28). Learn more about prenatal care.
Get important vaccines.
All pregnant people need whooping cough and flu vaccines (shots). Talk to your doctor or midwife about getting other vaccines to help protect you and your baby. Learn more about vaccines for adults.
Take charge of your health care.
Speak up and ask questions when you're with your doctor or midwife. When you play an active role in your health care, you help make sure that you and your growing family will get good care. Find out how to take charge of your health care.
Keep track of your baby’s movement.
Sometime between 16 and 28 weeks of pregnancy, you'll probably start to feel your baby move. Keep track of how often your baby moves. If you think your baby is moving less than usual, call your doctor or midwife.
Keep track of how often your baby moves. If you think your baby is moving less than usual, call your doctor or midwife.
Don't Smoke, Drink Alcohol, or Use Drugs
Don’t smoke, drink alcohol, or use drugs.
One of the best ways to protect you and your baby is to stop smoking, drinking alcohol, and using drugs before you become pregnant — or as soon as possible during your pregnancy.
There's no safe amount to drink or smoke while you're pregnant. Both can harm your baby’s health. Talk with your doctor or midwife about ways to help you quit.
Quitting all forms of tobacco products, including e-cigarettes (vapes), is best for you and your baby. Secondhand smoke (smoke from other people’s cigarettes) can also put you and your baby at risk for health problems. Stay away from cigarette smoke during your pregnancy.
Using drugs during pregnancy — including opioid pain medicines and marijuana — can also put your baby’s health at risk. If you’re pregnant and using drugs, talk with your doctor right away.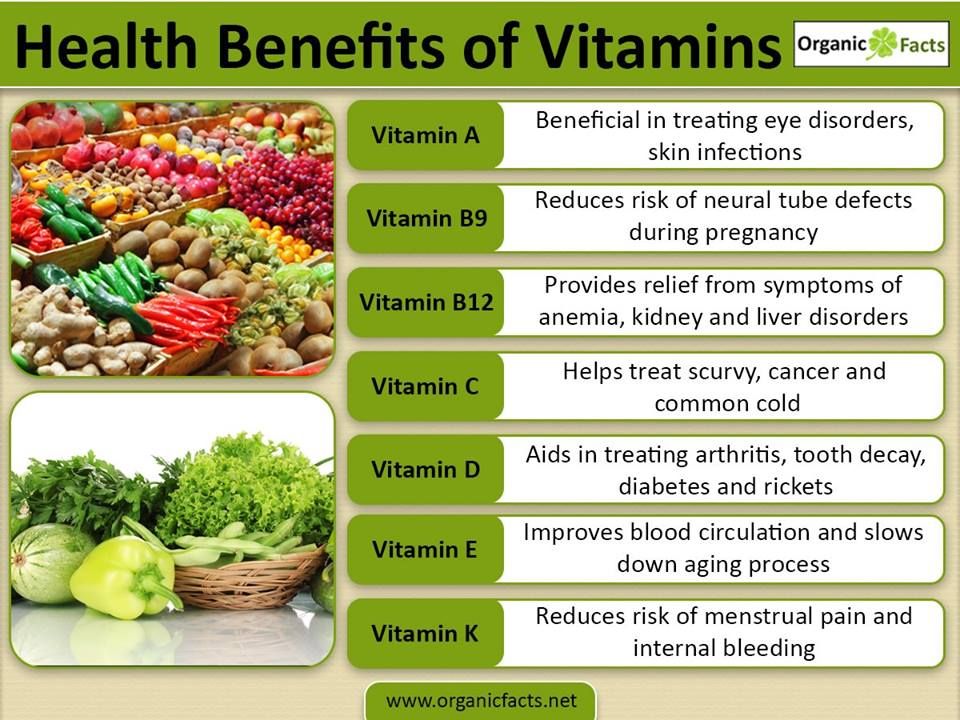
Learn more:
- Pregnant? Don’t Smoke!
- Quit Smoking
- Alcohol Use in Pregnancy
- What You Need to Know About Marijuana Use and Pregnancy
- Pregnancy and Opioid Pain Medications [PDF — 0.99 MB]
Eat Healthy and Stay Active
Get the nutrients you need.
Making healthy food choices and taking supplements as needed can help you gain weight in a healthy way, feel good while you're pregnant, and have a healthy baby.
- Check out these tips on healthy eating during pregnancy
- Ask your doctor or midwife if you need to take a daily prenatal supplement during pregnancy
- Take a daily supplement with 400 to 800 micrograms (mcg) of folic acid — folic acid is a vitamin that can prevent birth defects
Gain weight in a healthy way.
Gaining a certain amount of weight during pregnancy is important for both you and your baby. Learn how much weight is healthy for you to gain during pregnancy.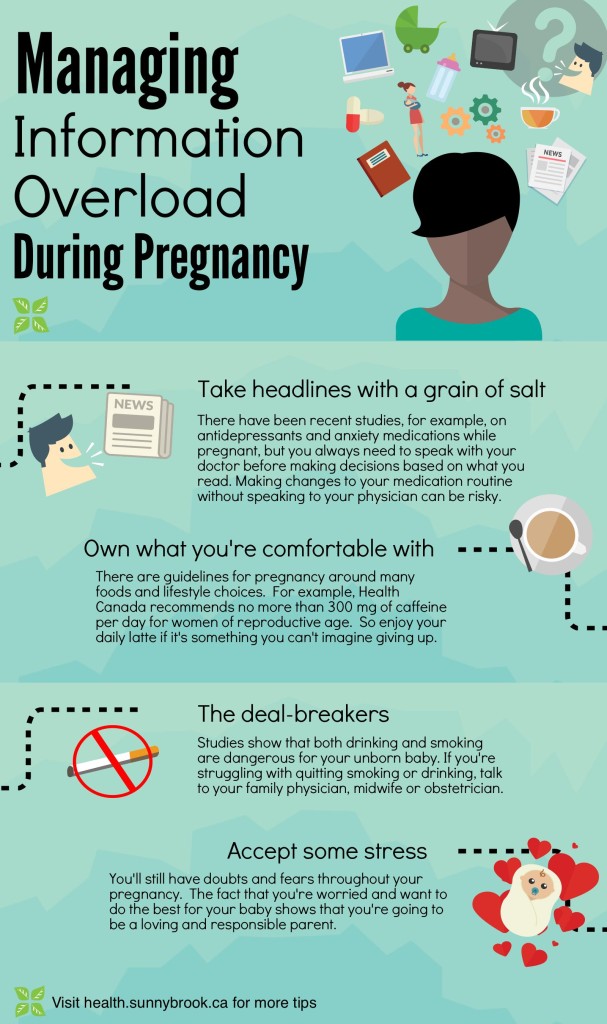
Even if you're overweight, you still need to gain some weight for your baby to grow. Ask your doctor or midwife how much weight is healthy for you to gain.
Stay active.
Being physically active can help you have a healthier pregnancy. Aim for at least 150 minutes a week of moderate-intensity aerobic activity — like walking, dancing, or swimming.
If you haven’t been active before, start slow and do what you can! Even a 5-minute walk has real health benefits, and you can add more activity over time.
Get more information about physical activity during pregnancy from these resources:
- Stay Active During Pregnancy: Quick Tips
- Move Your Way: Pregnancy
Prevent Infections
Take steps to prevent infections.
Follow these tips to prevent infections and help keep your baby safe:
- Wash your hands often with soap and water
- Make safe food choices and prepare food safely
- If you have a cat, learn how to protect yourself from toxoplasmosis (a disease spread by dirty cat litter)
- Get vaccines to protect you from whooping cough and the flu
- Avoid traveling to an area with Zika virus — and if you have to travel to an area with Zika, learn how to protect yourself from Zika virus
Learn more about preventing infections during pregnancy.
Get Support and Plan Ahead
Ask for help if you need it.
Being pregnant may be tiring or stressful at times. Extra support from loved ones can help. For example, family members or friends can:
- Provide emotional support so you feel less stressed
- Visit the doctor or midwife with you
- Go with you to a breastfeeding or birthing class
- Change the litter box if you have a cat
- Help prepare for the baby’s arrival by setting up furniture
Think about what you need, and don’t be afraid to ask for help.
Plan ahead for the first year with your new baby.
Having a new baby is exciting, but it can be stressful. Take steps to help you prepare for your new baby:
- Create a safe sleeping area for your baby, without soft objects in the crib.
- Talk with your doctor or midwife about newborn screening tests.
- Learn how to breastfeed your baby.
- Know the signs and symptoms of postpartum depression.
 About 1 in 8 women experience depression after they have a baby. Talk to your doctor or midwife if you have any questions or concerns.
About 1 in 8 women experience depression after they have a baby. Talk to your doctor or midwife if you have any questions or concerns. - Make sure to keep up with postpartum visits to your doctor or midwife.
- Talk to friends and family about helping out after the baby arrives. If you don't want visitors, people can support you in other ways, like dropping off food.
Read more about preparing for your baby.
Before You Get Pregnant
Not pregnant yet? Plan ahead.
Planning ahead can help you have a healthier pregnancy. For example:
- Take a daily supplement with 400 to 800 micrograms (mcg) of folic acid. Taking folic acid before and during early pregnancy can help prevent certain birth defects. Most multivitamins have 400 mcg of folic acid — check the label to be sure.
- Stop drinking alcohol when you start trying to get pregnant.
- If you smoke, quit smoking when you start trying to get pregnant.
Read about more things you can do to plan ahead.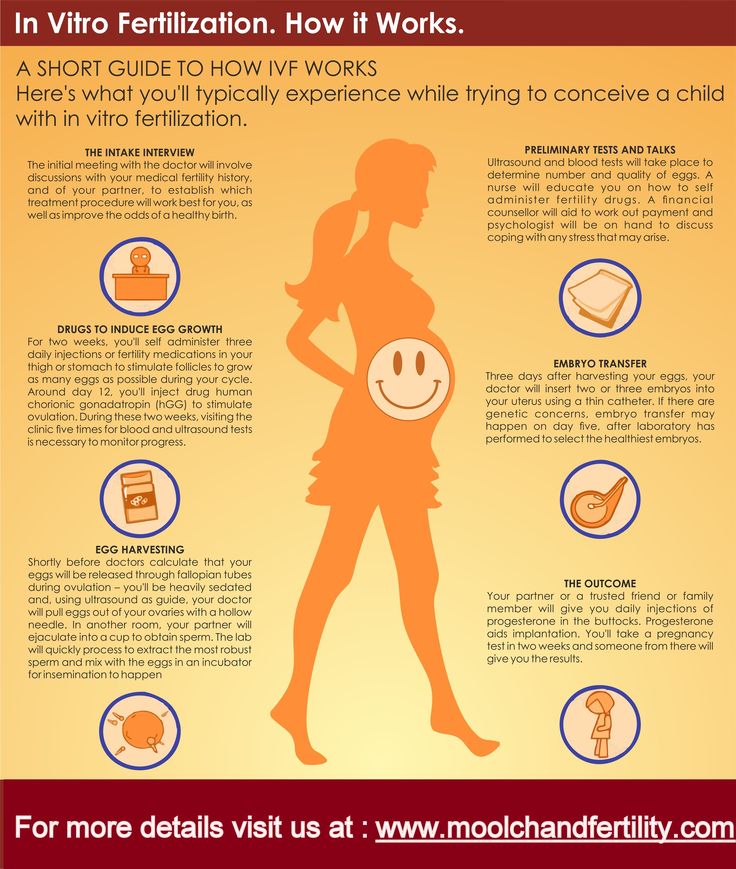
Schedule an appointment with a doctor or midwife.
- Get your blood pressure checked. If you have high blood pressure, ask your doctor how you can control it before and during your pregnancy.
- If you have a chronic (long-term) health condition, like diabetes, ask your doctor how you can control it before and during your pregnancy.
- Ask about getting vaccines before you get pregnant.
- Talk with your doctor about your family health history, including any medical conditions you have that could affect a pregnancy.
- Talk with your doctor about your risk for depression during pregnancy and whether you need counseling to help prevent it. Learn about depression during and after pregnancy.
- Talk with your doctor about any medicines you’re taking — both prescription drugs and over-the-counter medicines. Some medicines may not be safe to take while you’re pregnant.
- If you take opioid pain medicine, talk with your doctor about how to protect yourself and your baby.
 Learn more about opioids and pregnancy.
Learn more about opioids and pregnancy.
The Basics
How to prepare for conception?
Pregnancy planning is really necessary, especially in our time, when a healthy woman is the exception rather than the rule. Not to mention the fact that pregnancy is a serious test for the body of even a perfectly healthy woman.
It can be said that entering into a pregnancy without prior preparation for it is the same as flying on an airplane that has not been checked in advance: maybe it will cost, or maybe not. Of course, aircraft are tested before each flight. So why does a woman, ready to give birth to a new human being, not always conduct a similar check of her body? After all, the price of her neglect of herself and her health can be the life of the unborn child.
The process of preparing for pregnancy is quite complex and includes several stages. It is worth starting planning a few months (at least three) before the time when the couple intends to conceive a baby.
And at the stage of pregnancy planning , it is necessary to understand that the bearing and birth of a baby is not a woman's business, but a married couple's. Therefore, the active participation of the father in planning pregnancy is extremely necessary and important for himself, and for his wife, and for the unborn baby.
Without the help of doctors, it will not be possible to manage even at this stage. A visit to the gynecologist will allow you to identify possible diseases and treat them in a timely manner. After the first appeal, future parents undergo several examinations and pass certain tests in order to find out how ready their bodies are for conceiving a baby, as well as to prevent possible problems when carrying a child. The gynecologist will tell you what to do if, before planning a pregnancy, a woman was protected with hormonal contraceptives. It is necessary to stop taking hormonal contraceptives 3 months before the planned pregnancy.
It is important for a future mother to understand that only a healthy woman can bear and give birth to a healthy baby.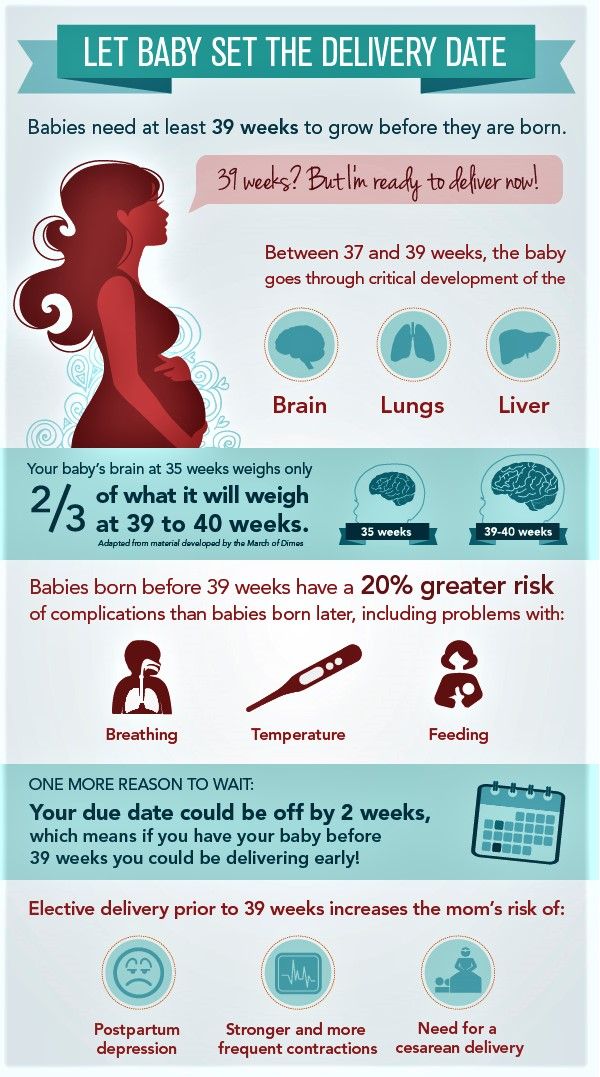 In this regard, you need to start taking care of your own health long before conception. Good physical shape, the absence of diseases, proper nutrition and the rejection of bad habits, hygiene and a measured lifestyle - all this has a beneficial effect on the female body and subsequently makes it easier to endure pregnancy. However, not all vitamins can be obtained from food. For example, the body can only obtain folic acid in an artificial form, since its counterpart (folate), found in green vegetables, beans, asparagus, and citrus fruits, is much less absorbed. Folic acid is very important for the development of the baby to take place correctly, and the need for its intake exists throughout pregnancy. If the mother's body during the bearing of the child receives a sufficient amount of this substance, then the risk of pathology from the nervous system is minimized.
In this regard, you need to start taking care of your own health long before conception. Good physical shape, the absence of diseases, proper nutrition and the rejection of bad habits, hygiene and a measured lifestyle - all this has a beneficial effect on the female body and subsequently makes it easier to endure pregnancy. However, not all vitamins can be obtained from food. For example, the body can only obtain folic acid in an artificial form, since its counterpart (folate), found in green vegetables, beans, asparagus, and citrus fruits, is much less absorbed. Folic acid is very important for the development of the baby to take place correctly, and the need for its intake exists throughout pregnancy. If the mother's body during the bearing of the child receives a sufficient amount of this substance, then the risk of pathology from the nervous system is minimized.
What tests should a married couple undergo
before planning a pregnancy?
- Gynecological examination, colposcopy for women.
- Blood type, Rh factor for both spouses. If a woman has a positive Rh factor, there is no problem. If a woman has a negative Rh factor - antibodies to the Rh factor (even if a man is also negative). If they are positive, pregnancy is not currently possible and needs to be corrected. If negative - repeat this analysis once a month, starting from 8 weeks of pregnancy. If a woman has 1 group, and a man has any other group, incompatibility by blood types is possible. An analysis for group antibodies, as well as an analysis for antibodies to the Rh factor, is carried out once a month, starting from 8 weeks of pregnancy.
- Tests for infections: routine smear, PCR for latent infections - both spouses.
- Blood test for TORCH-complex. Antibodies to rubella, toxoplasma, herpes, CMV, chlamydia - quantitative analysis (with titer). The presence of IgG antibodies means immunity to these infections, and is not an obstacle to pregnancy. The presence of IgM means an acute stage, planning in this case must be postponed until recovery.
 If there are no IgG antibodies to rubella, it is necessary to be vaccinated and protected for another 3 months after it.
If there are no IgG antibodies to rubella, it is necessary to be vaccinated and protected for another 3 months after it. - A trip to the dentist, a therapist, chest x-ray is a must for both spouses. By appointment of the therapist - consultation of narrow specialists (ENT doctor, urologist, endocrinologist, cardiologist, gastroenterologist).
- Spermogram. Desirable, but not required. It is done to determine the quality of spermatozoa and identify a hidden inflammatory process (a much more informative analysis than any smears and PCR).
- Ultrasound of the pelvic organs - at least 2 times per cycle: after menstruation and before menstruation. For the first time, the general condition of the pelvic organs is assessed, in the second, the presence of a corpus luteum and endometrial transformation, indicating that ovulation has occurred. Ideally, an intermediate third ultrasound on the eve of the expected ovulation is to detect the dominant follicle.
- Blood test for hormones of the reproductive system, thyroid gland, adrenal glands - according to indications.
- Ultrasound of the thyroid gland, mammary glands - according to indications.
- Hemostasiogram, coagulogram. - according to indications.
- General clinical blood test (hemoglobin, erythrocytes, leukocytes, platelets, ESR, color index, leukocyte formula). Finger blood. General urinalysis (morning portion of urine - completely collected, it is important that the analysis does not include discharge from neighboring organs).
- Blood tests for syphilis, HIV, hepatitis B and C - for both spouses.
- If there was a case of hereditary diseases in the family, miscarriages, spontaneous miscarriages, seek advice from a medical genetic consultation (Krasnoyarsk Regional Consultative and Diagnostic Center for Medical Genetics, Krasnoyarsk, Molokova St. 7, t. 55-99-20).
Fomin's clinic — a network of multidisciplinary clinics
If pregnancy does not occur within six months of active sexual life, then this is one of the signs of infertility. But don't panic. This does not mean at all that you have infertility, perhaps it is enough for you, for example, to adjust your diet. Second, infertility is treated. Well, you should not immediately cheat yourself on the subject of IVF. Remember, infertility is not the same as IVF.
But don't panic. This does not mean at all that you have infertility, perhaps it is enough for you, for example, to adjust your diet. Second, infertility is treated. Well, you should not immediately cheat yourself on the subject of IVF. Remember, infertility is not the same as IVF.
Infertility is a diagnosis that 10% of women worldwide have to live with: according to statistics, every fourth married couple is infertile. In this article we will talk about what female infertility is, how to live with it and whether it can be overcome.
Female infertility is a diagnosis that is made after a year of unsuccessful attempts to have children, subject to regular sex with a partner without contraception. If a woman is older than 35 years, the diagnosis is made faster - after 6 months. After 35 years, the ability to conceive gradually decreases, so older women should not delay treatment.
However, one should not rush to sad conclusions either. According to statistics, even completely healthy couples under the age of 30 manage to conceive a child in the first three months only in 20-37% of cases. At the same time, after six months, pregnancy occurs already in 80% of couples. Until a year has passed from the first attempt, there is no need to worry, be examined, and even more so, to be treated.
At the same time, after six months, pregnancy occurs already in 80% of couples. Until a year has passed from the first attempt, there is no need to worry, be examined, and even more so, to be treated.
Pregnancy depends on many reasons - in order for the "stars to converge" and all the factors to coincide, sometimes some time must pass.
For example, it is known that the easiest way to get pregnant is to make love 3-4 times a week. But a break of more than 5 days can adversely affect the quality of spermatozoa.
In addition, much depends on the lifestyle of parents - stress and heavy workload reduce fertility in both men and women. It's no surprise that many successful pregnancies have started during family vacations.
If less than 6-12 months have passed since the first attempt, you can try several “life hacks”:
Choose the best time to conceive. According to some reports, the day of ovulation and 2-3 days before it are best suited for conception.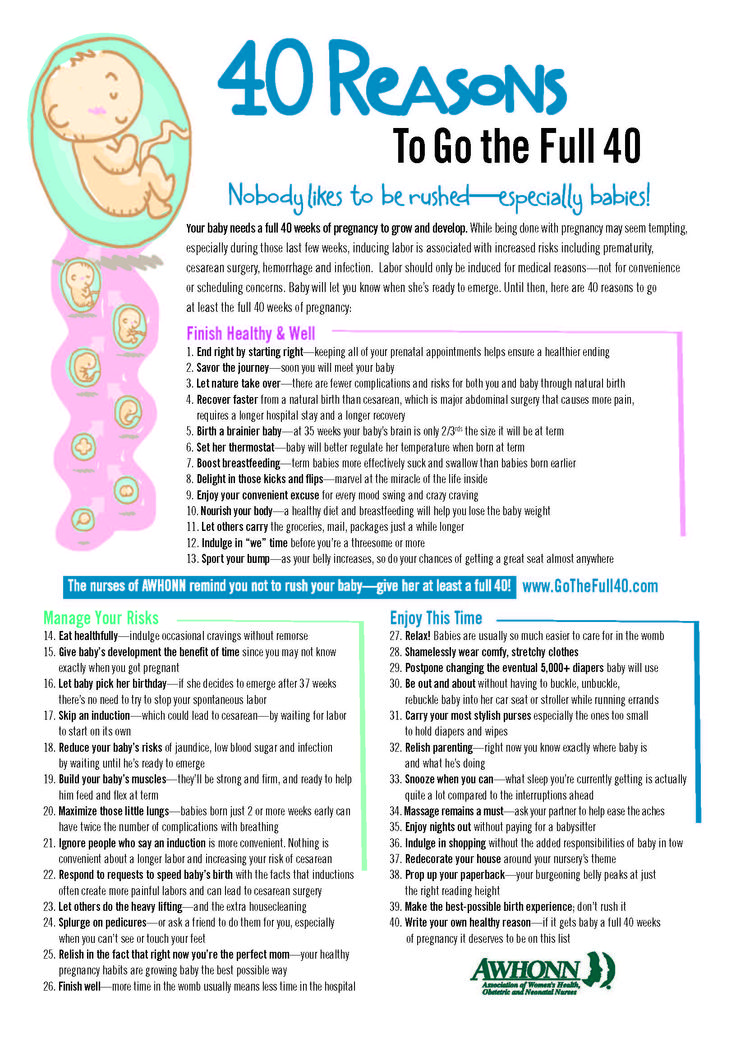 To find out when ovulation occurs, a urinary express test for luteinizing hormone will help - a day or two before ovulation it will become positive. However, calculating the optimal time is not always the best option.
To find out when ovulation occurs, a urinary express test for luteinizing hormone will help - a day or two before ovulation it will become positive. However, calculating the optimal time is not always the best option.
I always oppose the calculation of the optimal time for conception, because because of this, sex begins on a schedule in a couple's life, and this is one continuous stress. It seems to me that it is more reasonable to have sex 2-3 times a week during the entire cycle.
Kosolapova Inna Vladimirovna, gynecologist-reproductologist of the Fomina Clinic, chief physician
Do not use lubricants. Water-based, oil-based and silicone-based lubricants reduce sperm survival. But lubricants based on hydroxyethylcellulose have less effect on sperm survival - so if there is a lack of lubrication, you can continue to use them.
Stop dieting. Good nutrition is the key to a successful pregnancy. But don't overeat either. There is evidence that a body mass index (BMI) of 19 is ideal for pregnancy. -thirty. In women who have a BMI greater or less, the time to conception increases.
-thirty. In women who have a BMI greater or less, the time to conception increases.
You can calculate your BMI manually by dividing your weight by your height squared. Alternatively, you can use the built-in calculator on the website of the medical organization, or download a special application.
Quit smoking and alcohol. Smoking increases the risk of infertility by 1.6 times. It is also better not to abuse alcohol - eat more than 20 grams of ethanol per day, the risks of "earning" infertility increase by 60%.
On the other hand, the position of the body during sex, based on the available data, does not affect the result in any way. The "missionary" position is suitable for conception just like any other.
If more than a year has passed and nothing helps, it's time to see a doctor. The diagnosis of "infertility" has the right to make only an obstetrician-gynecologist (reproductologist).
It is important to understand that infertility is not only a woman's problem.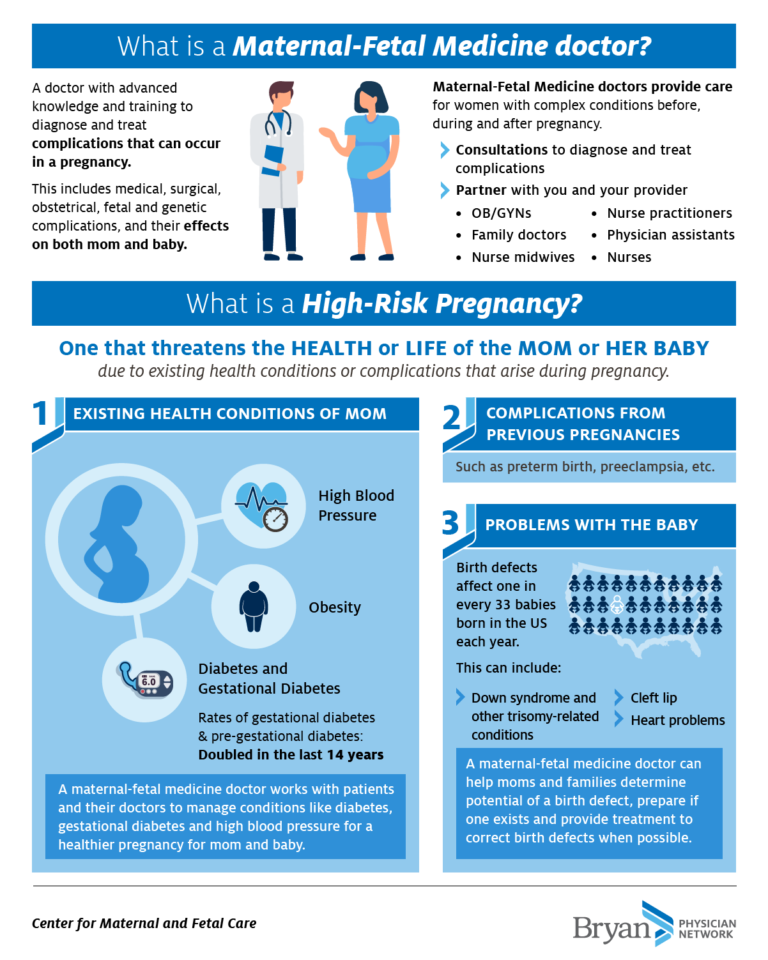 According to statistics, in the absence of children in a third of cases, the mother is “to blame”, in a third - the father, and in another third of cases the cause of infertility cannot be established. This means that with the diagnosis of "infertility" it is necessary to examine both partners.
According to statistics, in the absence of children in a third of cases, the mother is “to blame”, in a third - the father, and in another third of cases the cause of infertility cannot be established. This means that with the diagnosis of "infertility" it is necessary to examine both partners.
Male infertility is diagnosed by a urologist/andrologist. But if you go to a family planning center, a reproductologist can make a diagnosis.
Most often, female infertility is associated with problems in the reproductive system: in the ovaries, fallopian (or fallopian) tubes, through which the egg passes from the ovaries to the uterus, and in the uterus itself. To figure out what exactly “broke down” in the female reproductive system, the doctor will collect an anamnesis, carefully examine the patient and prescribe tests. We talk more about this in the article "Diagnostics of female infertility".
Infertility is treated, and quite successfully — according to statistics, after diagnosis and therapy, children appear in 50% of women (without the use of assisted reproductive technologies: IVF, etc.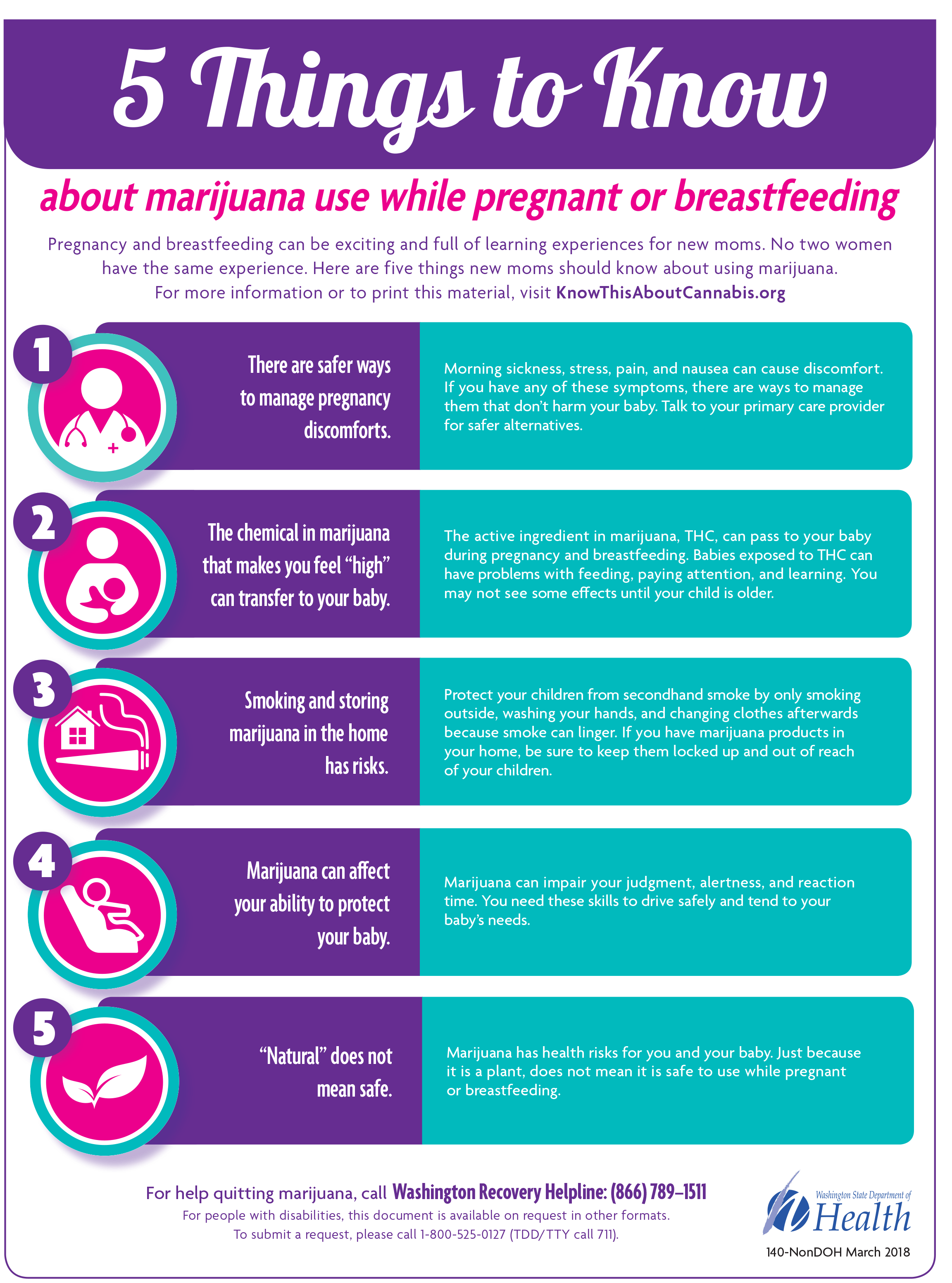 ). On the other hand, success depends on many factors, from the age and history of previous pregnancies to problems with the partner's sperm. Many factors influence the possibility of getting pregnant, so it can be difficult to predict the result.
). On the other hand, success depends on many factors, from the age and history of previous pregnancies to problems with the partner's sperm. Many factors influence the possibility of getting pregnant, so it can be difficult to predict the result.
If the problem is overweight or underweight, normalizing the weight is often enough for a successful pregnancy. True, much more often the problem is associated with sex hormones - in this situation, the doctor will select the appropriate medication. And if the problem is in the obstruction of the fallopian tubes or in the uterus itself, surgery may be required.
In vitro fertilization (IVF) is available for patients for whom these treatments are not suitable or have not worked.
The essence of IVF is that the patient's ovaries are stimulated with the help of hormones, then the egg is taken and fertilized with the husband's sperm, then the embryo is “grown” for some time in a special incubator and transplanted into the mother's uterus.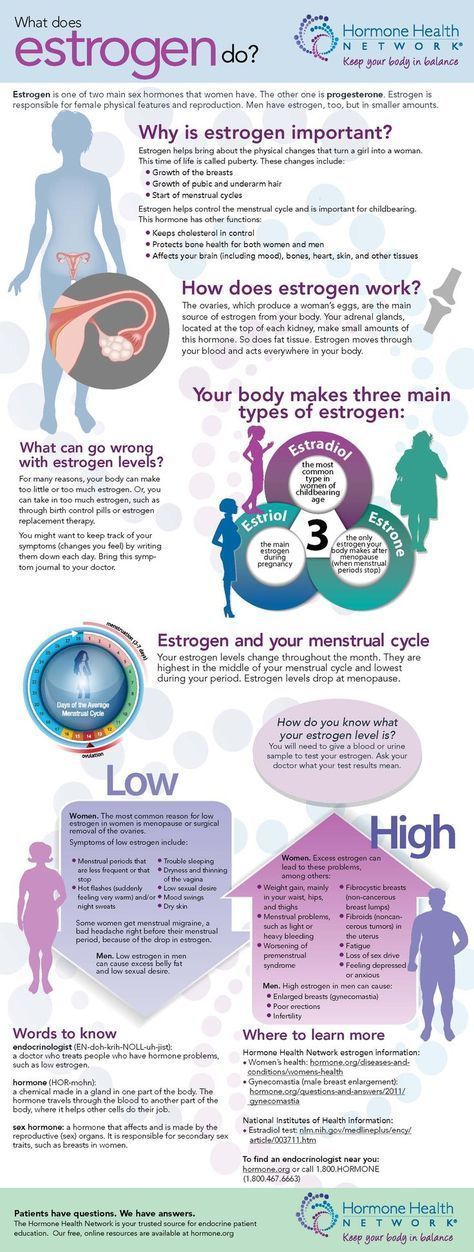 A baby is born in the same way as other children conceived "naturally".
A baby is born in the same way as other children conceived "naturally".
In Russia, the IVF procedure can be done free of charge under the CHI policy. However, it is important to understand that this is a complex treatment method that requires serious preparation and gives the best result until the age of 40-45. It is difficult to predict how successful IVF will be. According to statistics, the procedure ends with the birth of a live and healthy baby in about 27% of cases.
At the same time, IVF success rates vary greatly not only in different countries, but also in different clinics in the same city. There are clinics in which in 30-40% of cases it is possible to achieve a positive result on the first try.
Very often, mothers are concerned about possible health problems that may occur in children conceived through IVF. But in recent times there has been much less cause for concern than 20 years ago.
When the method was first created, all viable embryos that were obtained after fertilization were placed into the uterus of mothers “just in case”.