How many contractions are normal at 36 weeks
Symptoms, Development, Movement, and More
After 36 weeks, you’ve officially reached 9 months of pregnancy and are finally in the home stretch.
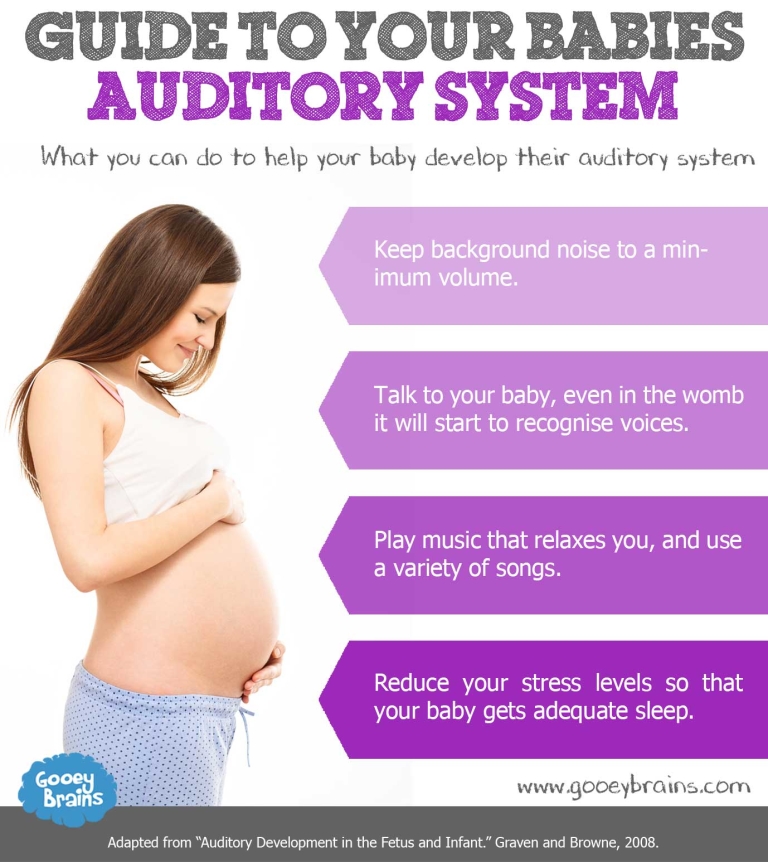
From growing fingernails to developing strong, healthy bones, your baby is growing rapidly during your last month of pregnancy and starting to get ready for birth.
You can take several steps to ensure you’re fully prepared as well, from packing a birth bag to picking a pediatrician.
In this article, we’ll cover everything you need to know once you’ve reached 36 weeks of pregnancy, including how your baby is developing, what symptoms you should expect, and how you can prepare for a safe and healthy delivery.
Changes in your body
Does it feel like there’s no more room at the baby inn? It may feel like that, but your baby will continue to grow until your due date arrives — a date only your baby knows, which might be driving you mad with uncertainty.
Whenever you feel tired from your pregnancy, just remind yourself that your baby will benefit from every last moment it spends in your womb.
As of next week, your baby will be considered early term, according to the American College of Obstetricians and Gynecologists (ACOG). Full term is now considered 40 weeks.
Try to enjoy these last few special weeks of your pregnancy, because your baby will be here before you know it.
That said, you’re no doubt exhausted from carrying around your growing belly, and you might be weary with worry. Even if this isn’t your first pregnancy, every pregnancy and every baby is different, so feeling a little anxious about the unknown is totally expected.
If you find that your anxiety is impacting your daily life or your relationships, you should bring it up with your doctor.
One symptom during week 36 to look out for is contractions. This could mean your baby is coming early or might just be Braxton-Hicks contractions.
Overall, you’ll probably continue experiencing many of the same symptoms you’ve encountered throughout your third trimester, such as:
- fatigue
- frequent urination
- heartburn
- leaky breasts
Leaky breasts
Many pregnant people experience breast leakage in their third trimester.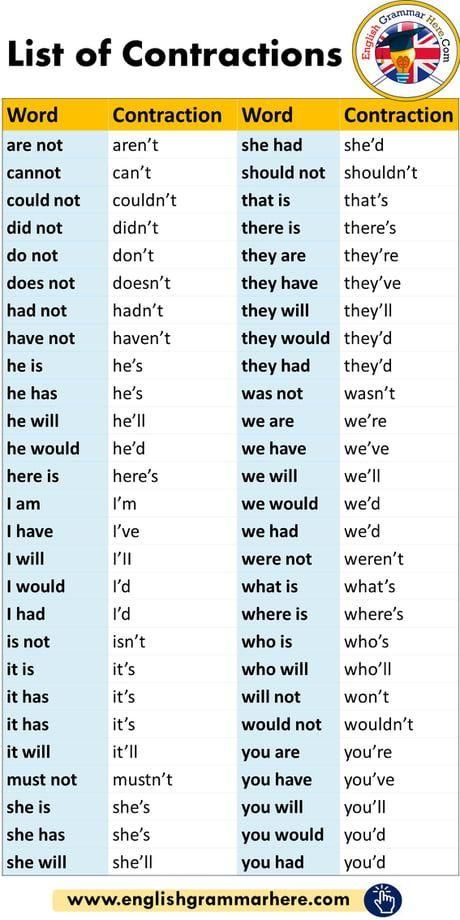
This thin, yellowish fluid, known as colostrum, will provide your baby with nutrients in the first days of life. Even if you aren’t planning to breastfeed or chestfeed, your body will still produce colostrum.
If you’re finding the leakage uncomfortable, try wearing nursing pads. You could stock up on these anyway, as you’ll likely need them post-delivery (whether or not you breastfeed), and there’s no reason you can’t use them now.
Nursing pads are relatively inexpensive and available at most major retailers that sell baby products. They can also be purchased in bulk and will come in handy after the baby is born and nursing.
Contractions
Sometimes babies decide to come early, so you should be on the lookout for contractions.
These feel like a tightening or cramping in your uterus, similar to menstrual cramps. Some women feel them in their back as well. Your stomach will feel hard to the touch during a contraction.
Each contraction will grow in intensity, peak, and then slowly subside. Think of it as a wave, rolling into the shore, then gently making its way back out to sea. As your contractions become closer together, the peaks will occur sooner and last longer.
Think of it as a wave, rolling into the shore, then gently making its way back out to sea. As your contractions become closer together, the peaks will occur sooner and last longer.
Some women confuse contractions with Braxton-Hicks contractions, which are sometimes referred to as “false labor.” Braxton-Hicks contractions are intermittent, don’t have a pattern to them, and don’t grow in intensity.
If you’re experiencing contractions, it’s important to time them. There are many mobile apps available that make it easy to time and record your contractions. Alternatively, you can track them the old-fashioned way, using a watch or timer (or counting the seconds out loud) and a pen and paper.
To track your contractions, record the time they start and when they end. The length of time between when one starts and when the next one starts is referred to as the frequency of contractions. Bring this record with you when you go to the hospital.
If your water breaks, make note of the time and head to the hospital.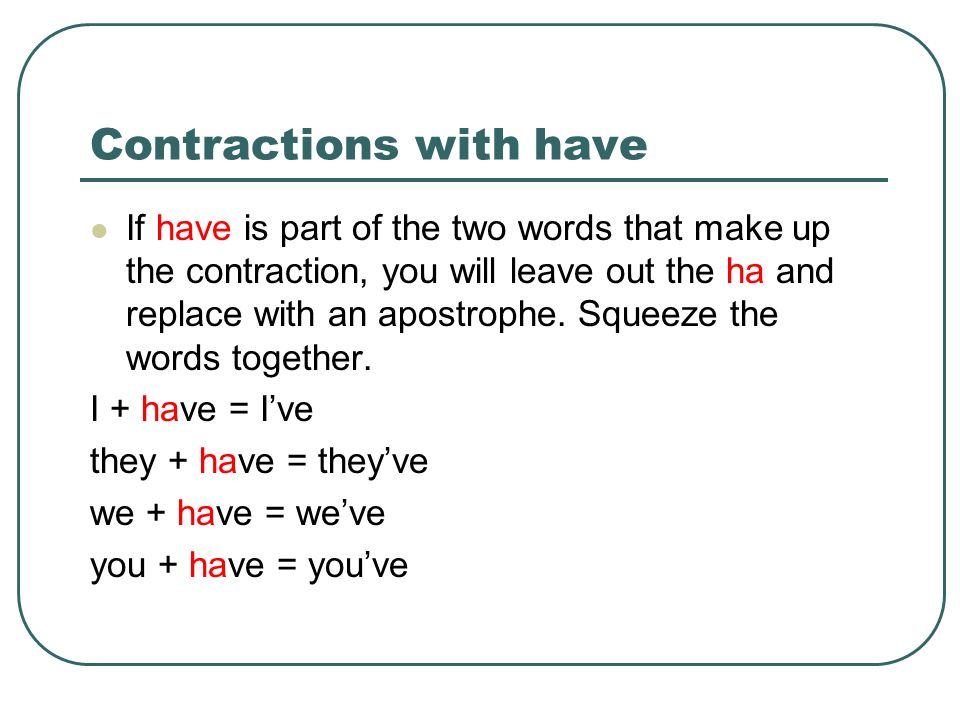
If you’re uncertain about what pains should warrant a call to your doctor or a trip to the hospital, ask your doctor now so you’ll be prepared when the time comes.
If you start to experience contractions that last for about 1 minute and come every 5 minutes for at least an hour, you’re likely on your way to your baby’s birth.
Somewhere around 18 inches in length, your baby weighs between 5 and 6 pounds at 36 weeks.
During this time, your baby’s bones will begin to harden as the lungs, reproductive organs, and nervous system continue to develop, according to ACOG.
As more fat begins to build up under the skin, your baby’s limbs may begin to look chubby. Your little one also starts having more hair on their head and grows fingernails that extend to the ends of their fingers.
Around this time, your baby may also turn into a head-down position to prepare for birth. After 37 weeks, about 97% of babies will have fully shifted into this position.
Soon, your doctor will probably check whether your baby is readying for delivery. To check this, your doctor will look to see if your baby’s head is down by your cervix.
To check this, your doctor will look to see if your baby’s head is down by your cervix.
Your baby should move into this position by 36 weeks, but don’t fret if they haven’t turned yet. Most babies will turn toward the birth canal in the last weeks of pregnancy, but 3-4% of all term pregnancies will remain breech, or feet first.
Breech presentation is always considered high risk, according to 2016 research. Most such cases result in cesarean delivery.
If your doctor suspects your baby is breech, you’ll likely be sent for an ultrasound to confirm. After that, your doctor may recommend one of several ways to help baby move downward, such as external cephalic version (ECV). ECV is a nonsurgical method sometimes used to try to turn your baby.
If you’re worried about the potentials of a breech delivery, share your concerns with your doctor. Your doctor should be able to ease your concerns with all the resources available for breech pregnancies.
In an ideal world, you’d probably like to already have everything ready for your baby’s arrival. Realistically, though, there may be several things left on your to-do list, and that’s fine. You still have time. Here are some things to focus on this week.
Realistically, though, there may be several things left on your to-do list, and that’s fine. You still have time. Here are some things to focus on this week.
Pick your pediatrician
If you haven’t chosen a pediatrician for your baby yet, you’ll want to pick one soon. While you likely have a few more weeks before your baby arrives, that time isn’t guaranteed.
Ask local friends or family members for referrals, and be sure to call ahead to schedule a tour. It’s not only easier to gauge your comfort with a doctor and the office environment in person, but you’ll likely feel less stress now that you’ve checked one more thing off your to-do list.
Pack a birth bag
Another to-do list item you should probably check off soon is packing your birth bag.
You can find countless recommendations of what to include from people who have gone through this before. To find what’s best for you, ask loved ones for their advice, then stick with what you find most important.
In general, you’ll want to pack items that will make you, your partner, and your baby comfortable. Some things you might want to pack for yourself include:
- insurance information
- a copy of your birth plan
- a toothbrush
- deodorant
- comfortable pajamas and slippers
- things that will help you relax during labor
- a book or magazines
For your baby, a car seat is a must. If you haven’t already, call your local police or fire station to see if they do car seat checks. Installing a car seat can be tricky, and it’s the last thing you’ll want to have to worry about when you’re in labor.
Get a new car seat to be sure it was manufactured with the most current safety guidelines. Car seats are meant to protect the child from one accident and then be discarded. If you buy one at a garage sale, you may not know if it has been in a motor vehicle accident.
Pack an outfit to bring baby home in, but skip the frills and pick something that will be easy to put on and take off in case of a diaper change.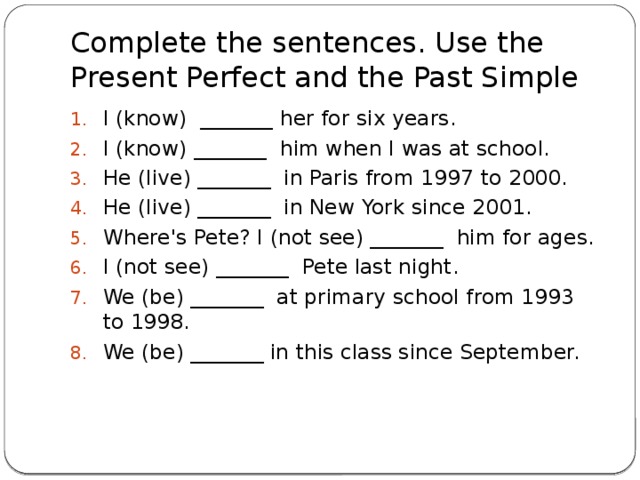 You may also want to consider packing a backup outfit, just in case your baby has an accident that makes its way out of the diaper.
You may also want to consider packing a backup outfit, just in case your baby has an accident that makes its way out of the diaper.
Think about your baby’s comfort when picking an outfit as well. If you’re delivering in the winter, pick something that will keep your baby warm. If it will be in the 90s, consider a lightweight outfit. The hospital should provide most other basics for the baby, such as diapers.
And don’t forget your partner! Their comfort will likely be far from your mind when you’re breathing through labor pains, but now is when you can show them that their comfort matters, too.
Consider packing:
- snacks you can share
- a camera
- a charger for your phone and other electronics so your partner can text or email everyone when your baby arrives
- headphones, for what could be a long day or night
- list of contacts so your partner knows who to call or email once your baby arrives
- a jacket or sweater for your partner (hospitals can get cold)
Share on Pinterest
If you’re experiencing contractions or think you may be experiencing them, call your doctor or head to the hospital.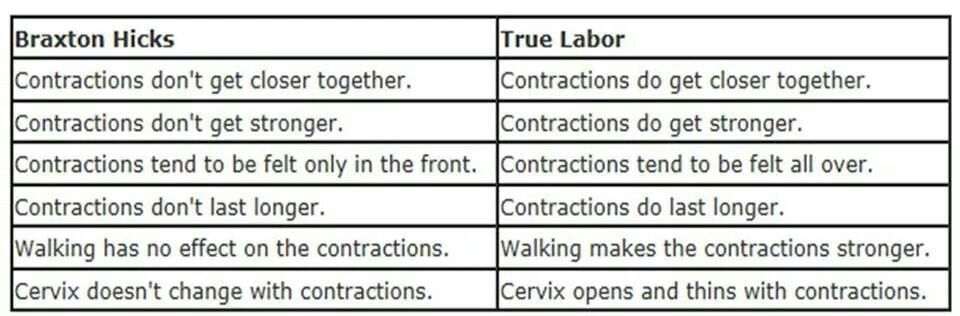 You should also call your doctor if you experience vaginal bleeding, fluid leakage, or severe abdominal pain.
You should also call your doctor if you experience vaginal bleeding, fluid leakage, or severe abdominal pain.
As your baby continues to grow, there’s less room for them to move. While baby’s movements have probably slowed down some, you should still feel them.
If you notice a decrease in movement (fewer than 10 movements in an hour) or if you’re concerned about your baby’s movement, contact your doctor.
While a decrease in movement could be nothing, it could also be a sign that your baby is in distress. It’s always better to play it safe and contact your healthcare professional.
Is it safe to deliver at 36 weeks?
Babies are considered late preterm at 36 weeks. While it’s best to wait until at least 39 weeks if possible, some babies are born prematurely and early delivery may even be necessary in some cases.
Although the risk of complications is significantly reduced after 36 weeks, late preterm infants are still at risk for several health concerns, including:
- feeding difficulties
- neurodevelopmental delays
- hyperbilirubinemia, or high bilirubin levels
- respiratory troubles
- low blood sugar
- temperature instability
Your doctor can help you determine the risks associated with preterm delivery for your baby and develop a plan to ensure a safe and healthy delivery.
What are the chances of going into labor at 36 weeks?
According to the National Vital Statistics System, approximately 7% of births in the United States occur at 34 to 36 weeks.
People who have had a preterm birth before, those who are pregnant with multiple babies, and those with certain medical conditions may be at a higher risk of early delivery.
What should I avoid at 36 weeks pregnant?
You should avoid alcohol use and smoking during pregnancy to reduce the risk of issues like miscarriage, early delivery, and fetal alcohol syndrome.
You should also steer clear of unpasteurized dairy products and raw or undercooked meat, eggs, poultry, and fish to prevent foodborne illness.
Additionally, be sure to limit caffeine intake to less than 200 mg per day and avoid fish high in mercury, such as shark, swordfish, or raw shellfish.
You are almost at the finish line. Remember to enjoy these last couple of weeks. Take naps whenever you can, and continue eating healthy, balanced meals. You’ll be thankful for the extra nutrients and energy once your big day arrives.
You’ll be thankful for the extra nutrients and energy once your big day arrives.
Symptoms, Development, Movement, and More
After 36 weeks, you’ve officially reached 9 months of pregnancy and are finally in the home stretch.
From growing fingernails to developing strong, healthy bones, your baby is growing rapidly during your last month of pregnancy and starting to get ready for birth.
You can take several steps to ensure you’re fully prepared as well, from packing a birth bag to picking a pediatrician.
In this article, we’ll cover everything you need to know once you’ve reached 36 weeks of pregnancy, including how your baby is developing, what symptoms you should expect, and how you can prepare for a safe and healthy delivery.
Changes in your body
Does it feel like there’s no more room at the baby inn? It may feel like that, but your baby will continue to grow until your due date arrives — a date only your baby knows, which might be driving you mad with uncertainty.
Whenever you feel tired from your pregnancy, just remind yourself that your baby will benefit from every last moment it spends in your womb.
As of next week, your baby will be considered early term, according to the American College of Obstetricians and Gynecologists (ACOG). Full term is now considered 40 weeks.
Try to enjoy these last few special weeks of your pregnancy, because your baby will be here before you know it.
That said, you’re no doubt exhausted from carrying around your growing belly, and you might be weary with worry. Even if this isn’t your first pregnancy, every pregnancy and every baby is different, so feeling a little anxious about the unknown is totally expected.
If you find that your anxiety is impacting your daily life or your relationships, you should bring it up with your doctor.
One symptom during week 36 to look out for is contractions. This could mean your baby is coming early or might just be Braxton-Hicks contractions.
Overall, you’ll probably continue experiencing many of the same symptoms you’ve encountered throughout your third trimester, such as:
- fatigue
- frequent urination
- heartburn
- leaky breasts
Leaky breasts
Many pregnant people experience breast leakage in their third trimester.
This thin, yellowish fluid, known as colostrum, will provide your baby with nutrients in the first days of life. Even if you aren’t planning to breastfeed or chestfeed, your body will still produce colostrum.
If you’re finding the leakage uncomfortable, try wearing nursing pads. You could stock up on these anyway, as you’ll likely need them post-delivery (whether or not you breastfeed), and there’s no reason you can’t use them now.
Nursing pads are relatively inexpensive and available at most major retailers that sell baby products. They can also be purchased in bulk and will come in handy after the baby is born and nursing.
Contractions
Sometimes babies decide to come early, so you should be on the lookout for contractions.
These feel like a tightening or cramping in your uterus, similar to menstrual cramps. Some women feel them in their back as well. Your stomach will feel hard to the touch during a contraction.
Each contraction will grow in intensity, peak, and then slowly subside. Think of it as a wave, rolling into the shore, then gently making its way back out to sea. As your contractions become closer together, the peaks will occur sooner and last longer.
Think of it as a wave, rolling into the shore, then gently making its way back out to sea. As your contractions become closer together, the peaks will occur sooner and last longer.
Some women confuse contractions with Braxton-Hicks contractions, which are sometimes referred to as “false labor.” Braxton-Hicks contractions are intermittent, don’t have a pattern to them, and don’t grow in intensity.
If you’re experiencing contractions, it’s important to time them. There are many mobile apps available that make it easy to time and record your contractions. Alternatively, you can track them the old-fashioned way, using a watch or timer (or counting the seconds out loud) and a pen and paper.
To track your contractions, record the time they start and when they end. The length of time between when one starts and when the next one starts is referred to as the frequency of contractions. Bring this record with you when you go to the hospital.
If your water breaks, make note of the time and head to the hospital.
If you’re uncertain about what pains should warrant a call to your doctor or a trip to the hospital, ask your doctor now so you’ll be prepared when the time comes.
If you start to experience contractions that last for about 1 minute and come every 5 minutes for at least an hour, you’re likely on your way to your baby’s birth.
Somewhere around 18 inches in length, your baby weighs between 5 and 6 pounds at 36 weeks.
During this time, your baby’s bones will begin to harden as the lungs, reproductive organs, and nervous system continue to develop, according to ACOG.
As more fat begins to build up under the skin, your baby’s limbs may begin to look chubby. Your little one also starts having more hair on their head and grows fingernails that extend to the ends of their fingers.
Around this time, your baby may also turn into a head-down position to prepare for birth. After 37 weeks, about 97% of babies will have fully shifted into this position.
Soon, your doctor will probably check whether your baby is readying for delivery.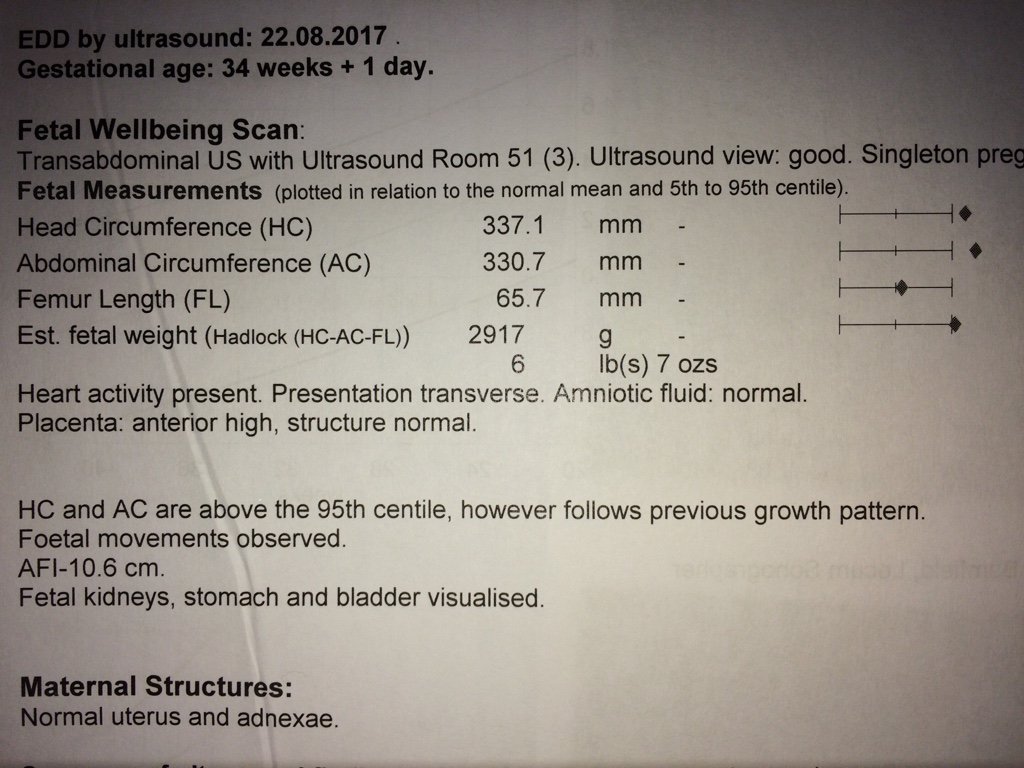 To check this, your doctor will look to see if your baby’s head is down by your cervix.
To check this, your doctor will look to see if your baby’s head is down by your cervix.
Your baby should move into this position by 36 weeks, but don’t fret if they haven’t turned yet. Most babies will turn toward the birth canal in the last weeks of pregnancy, but 3-4% of all term pregnancies will remain breech, or feet first.
Breech presentation is always considered high risk, according to 2016 research. Most such cases result in cesarean delivery.
If your doctor suspects your baby is breech, you’ll likely be sent for an ultrasound to confirm. After that, your doctor may recommend one of several ways to help baby move downward, such as external cephalic version (ECV). ECV is a nonsurgical method sometimes used to try to turn your baby.
If you’re worried about the potentials of a breech delivery, share your concerns with your doctor. Your doctor should be able to ease your concerns with all the resources available for breech pregnancies.
In an ideal world, you’d probably like to already have everything ready for your baby’s arrival.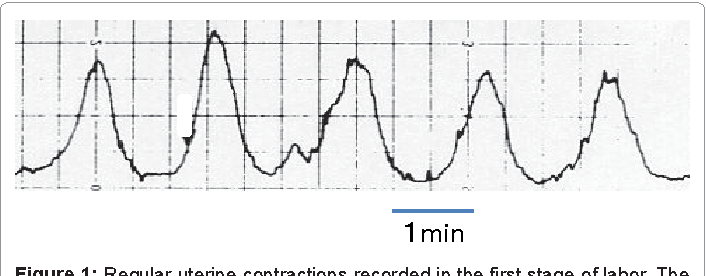 Realistically, though, there may be several things left on your to-do list, and that’s fine. You still have time. Here are some things to focus on this week.
Realistically, though, there may be several things left on your to-do list, and that’s fine. You still have time. Here are some things to focus on this week.
Pick your pediatrician
If you haven’t chosen a pediatrician for your baby yet, you’ll want to pick one soon. While you likely have a few more weeks before your baby arrives, that time isn’t guaranteed.
Ask local friends or family members for referrals, and be sure to call ahead to schedule a tour. It’s not only easier to gauge your comfort with a doctor and the office environment in person, but you’ll likely feel less stress now that you’ve checked one more thing off your to-do list.
Pack a birth bag
Another to-do list item you should probably check off soon is packing your birth bag.
You can find countless recommendations of what to include from people who have gone through this before. To find what’s best for you, ask loved ones for their advice, then stick with what you find most important.
In general, you’ll want to pack items that will make you, your partner, and your baby comfortable. Some things you might want to pack for yourself include:
- insurance information
- a copy of your birth plan
- a toothbrush
- deodorant
- comfortable pajamas and slippers
- things that will help you relax during labor
- a book or magazines
For your baby, a car seat is a must. If you haven’t already, call your local police or fire station to see if they do car seat checks. Installing a car seat can be tricky, and it’s the last thing you’ll want to have to worry about when you’re in labor.
Get a new car seat to be sure it was manufactured with the most current safety guidelines. Car seats are meant to protect the child from one accident and then be discarded. If you buy one at a garage sale, you may not know if it has been in a motor vehicle accident.
Pack an outfit to bring baby home in, but skip the frills and pick something that will be easy to put on and take off in case of a diaper change.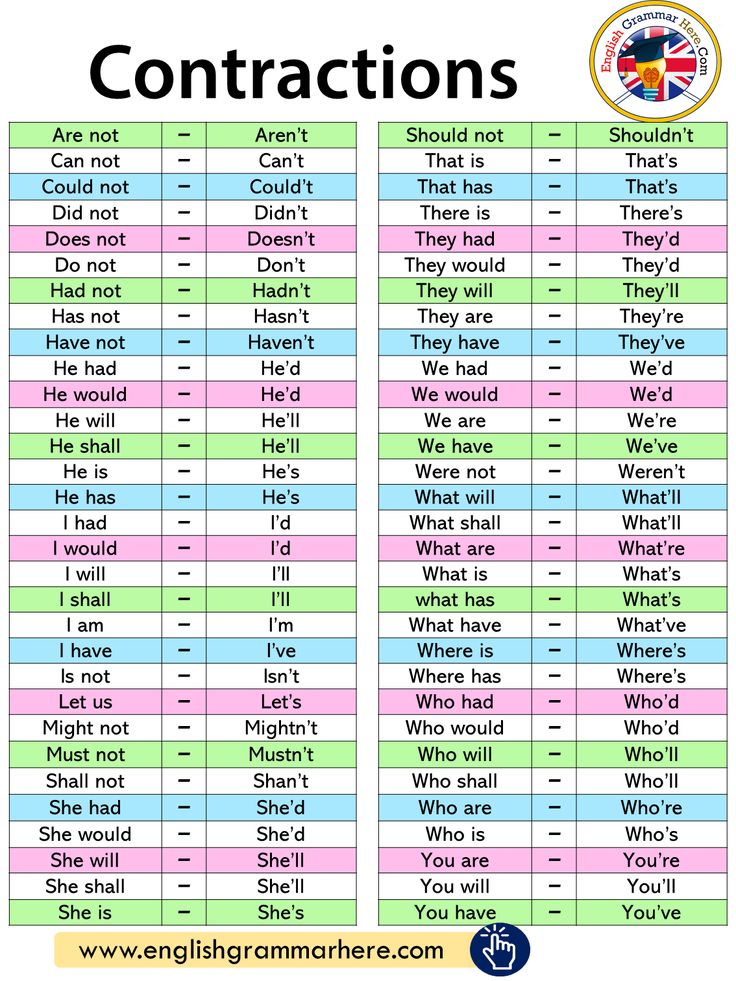 You may also want to consider packing a backup outfit, just in case your baby has an accident that makes its way out of the diaper.
You may also want to consider packing a backup outfit, just in case your baby has an accident that makes its way out of the diaper.
Think about your baby’s comfort when picking an outfit as well. If you’re delivering in the winter, pick something that will keep your baby warm. If it will be in the 90s, consider a lightweight outfit. The hospital should provide most other basics for the baby, such as diapers.
And don’t forget your partner! Their comfort will likely be far from your mind when you’re breathing through labor pains, but now is when you can show them that their comfort matters, too.
Consider packing:
- snacks you can share
- a camera
- a charger for your phone and other electronics so your partner can text or email everyone when your baby arrives
- headphones, for what could be a long day or night
- list of contacts so your partner knows who to call or email once your baby arrives
- a jacket or sweater for your partner (hospitals can get cold)
Share on Pinterest
If you’re experiencing contractions or think you may be experiencing them, call your doctor or head to the hospital.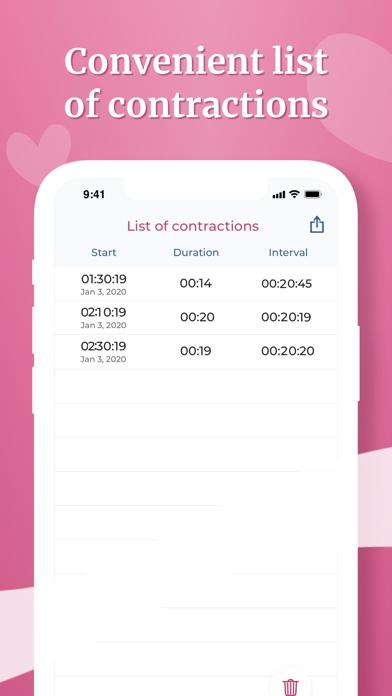 You should also call your doctor if you experience vaginal bleeding, fluid leakage, or severe abdominal pain.
You should also call your doctor if you experience vaginal bleeding, fluid leakage, or severe abdominal pain.
As your baby continues to grow, there’s less room for them to move. While baby’s movements have probably slowed down some, you should still feel them.
If you notice a decrease in movement (fewer than 10 movements in an hour) or if you’re concerned about your baby’s movement, contact your doctor.
While a decrease in movement could be nothing, it could also be a sign that your baby is in distress. It’s always better to play it safe and contact your healthcare professional.
Is it safe to deliver at 36 weeks?
Babies are considered late preterm at 36 weeks. While it’s best to wait until at least 39 weeks if possible, some babies are born prematurely and early delivery may even be necessary in some cases.
Although the risk of complications is significantly reduced after 36 weeks, late preterm infants are still at risk for several health concerns, including:
- feeding difficulties
- neurodevelopmental delays
- hyperbilirubinemia, or high bilirubin levels
- respiratory troubles
- low blood sugar
- temperature instability
Your doctor can help you determine the risks associated with preterm delivery for your baby and develop a plan to ensure a safe and healthy delivery.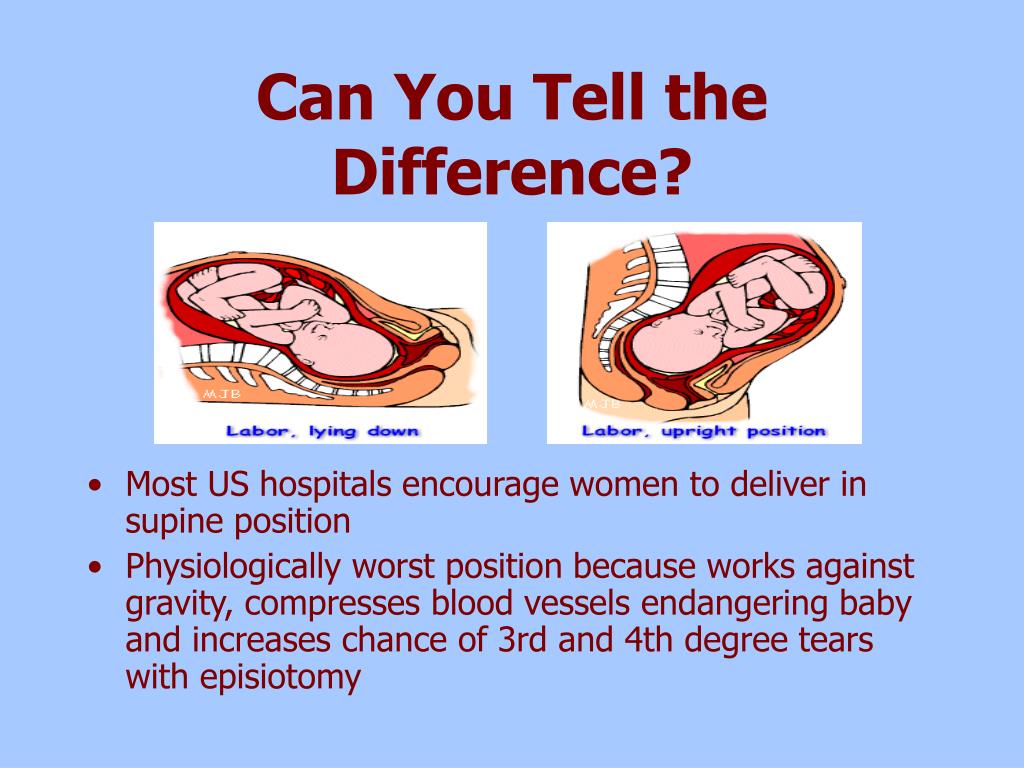
What are the chances of going into labor at 36 weeks?
According to the National Vital Statistics System, approximately 7% of births in the United States occur at 34 to 36 weeks.
People who have had a preterm birth before, those who are pregnant with multiple babies, and those with certain medical conditions may be at a higher risk of early delivery.
What should I avoid at 36 weeks pregnant?
You should avoid alcohol use and smoking during pregnancy to reduce the risk of issues like miscarriage, early delivery, and fetal alcohol syndrome.
You should also steer clear of unpasteurized dairy products and raw or undercooked meat, eggs, poultry, and fish to prevent foodborne illness.
Additionally, be sure to limit caffeine intake to less than 200 mg per day and avoid fish high in mercury, such as shark, swordfish, or raw shellfish.
You are almost at the finish line. Remember to enjoy these last couple of weeks. Take naps whenever you can, and continue eating healthy, balanced meals. You’ll be thankful for the extra nutrients and energy once your big day arrives.
You’ll be thankful for the extra nutrients and energy once your big day arrives.
what is happening, the development of pregnancy and fetus
Week by week
33 - 36 weeks of pregnancy
Elena Gevorkova
Obstetrician-gynecologist, Moscow
33rd week
BABY
At the 33rd week, the weight of the fetus is 1800-1900 g, and the body length is 43-44 cm. The amount of subcutaneous fat increases, due to which the folds and wrinkles on the baby's body are smoothed out, the skin turns pink. The fluffy hairs that cover the body of the fetus, which are called lanugo, become smaller, and the hair on the head darkens and thickens. The baby's skin is covered with a thin layer of cheese-like lubricant, its largest amount accumulates in the folds - axillary, cervical, inguinal - as well as on the back of the body and face. Grease is a viscous mass of white color, it is a secret of the sebaceous glands, mixed with skin scales. Its function is to protect the baby's skin from damage and facilitate its passage through the birth canal.
Its function is to protect the baby's skin from damage and facilitate its passage through the birth canal.
By this time, the movements of the fetus gradually change their habitual character - they become more and more limited and less pronounced in amplitude due to insufficient space. However, the strength of the movements increases, since by this time the muscular system of the fetus is already sufficiently strengthened. Sharp and strong tremors of the fetus can be sensitive to the internal organs of a pregnant woman. Depending on the position of the baby, the liver, stomach, bladder, ribs, etc. may “suffer”. By 33 weeks, the movements of the fetus are already quite coordinated.
FUTURE MOTHER
The height of the fundus of the uterus from the level of the pubis at this time is 34 cm. The volume of the abdomen is increased due to the weight of the baby, placenta, amniotic fluid. The increase in uterine pressure and strong tremors of the fetus can cause some discomfort in the pregnant woman. Many movements previously available to the expectant mother, such as squats, become limited. Moderate physical activity - walking, fitness, etc. - Requires frequent respite.
Many movements previously available to the expectant mother, such as squats, become limited. Moderate physical activity - walking, fitness, etc. - Requires frequent respite.
A change in the center of gravity increases the load on the spine, which can manifest itself as pain in the lower back, sacrum, and pelvic region. The pressure of the uterus on the stomach can cause or increase nausea, heartburn, and a feeling of heaviness. An increase of almost 1 liter of the volume of circulating blood in the body of a pregnant woman increases the load on the kidneys, and the growing uterus puts pressure on the bladder. All this can be manifested by frequent urination.
These ailments are usually associated with the mechanical pressure of the uterus on the surrounding organs; they are not symptoms of the disease and are temporary. And to relieve nausea, heartburn and a feeling of heaviness in the stomach, frequent meals in small portions are recommended.
34th week
BABY
By this time, the weight of the fetus is approximately 2100 g, and the height is 45 cm. From this period, the cheeks are very pronounced, because, developing a sucking reflex, the fetus often sucks its thumb. This leads to the fact that the baby strengthens the facial muscles, in particular the buccal. The total muscle mass of the fetus increases, the bones become denser.
From this period, the cheeks are very pronounced, because, developing a sucking reflex, the fetus often sucks its thumb. This leads to the fact that the baby strengthens the facial muscles, in particular the buccal. The total muscle mass of the fetus increases, the bones become denser.
There is an intensive functioning of the baby's internal organs. During the day, he repeatedly swallows portions of amniotic fluid. Passing through the gastrointestinal tract, the amniotic fluid stimulates the work of the muscular wall. The dense part of the amniotic fluid, which is a suspension of skin flakes, lubricant, vellus hair, is processed by the enzymes of the liver and pancreas, and the liquid part is intensively excreted by the kidneys of the fetus.
Approximately 500 ml of amniotic fluid is treated in this way per day. The production of bile continues, which accumulates in the gallbladder and, as the stomach fills with a suspension of amniotic water, enters the lumen of the small intestine.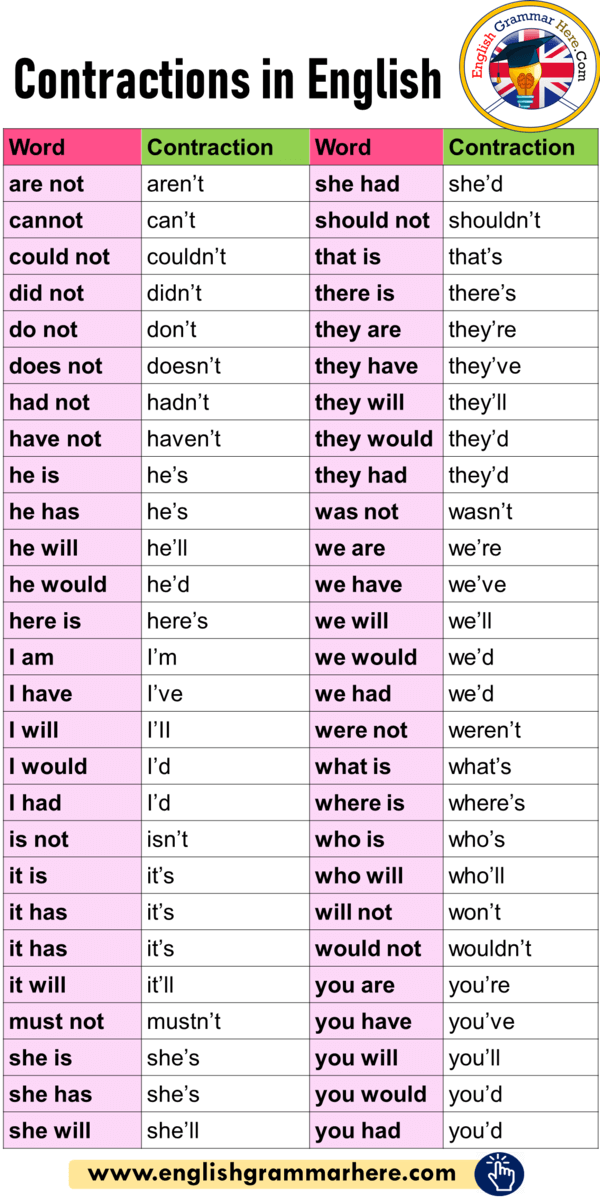 The functional development of the liver and pancreas during the prenatal period does not play a significant role, since the fetus does not have digestion; processes for the production of bile and enzymes: lipase, which breaks down fats; trypsin, which breaks down proteins; amylase, which breaks down carbohydrates, etc. - are preparatory in nature.
The functional development of the liver and pancreas during the prenatal period does not play a significant role, since the fetus does not have digestion; processes for the production of bile and enzymes: lipase, which breaks down fats; trypsin, which breaks down proteins; amylase, which breaks down carbohydrates, etc. - are preparatory in nature.
FUTURE MOTHER
Most pregnant women begin to feel rather intense false contractions at this time. Strictly speaking, false or training contractions, which are also called Braxton-Hicks contractions, can occur after the 20th week of pregnancy: the longer the period, the more frequent and pronounced the contractions. They are episodic contractions of the muscles of the uterus, lasting from a few seconds to 3-5 minutes. Braxton-Hicks contractions are not pathological - this is a completely normal process of preparing the muscles of the uterus for the difficult process of childbirth.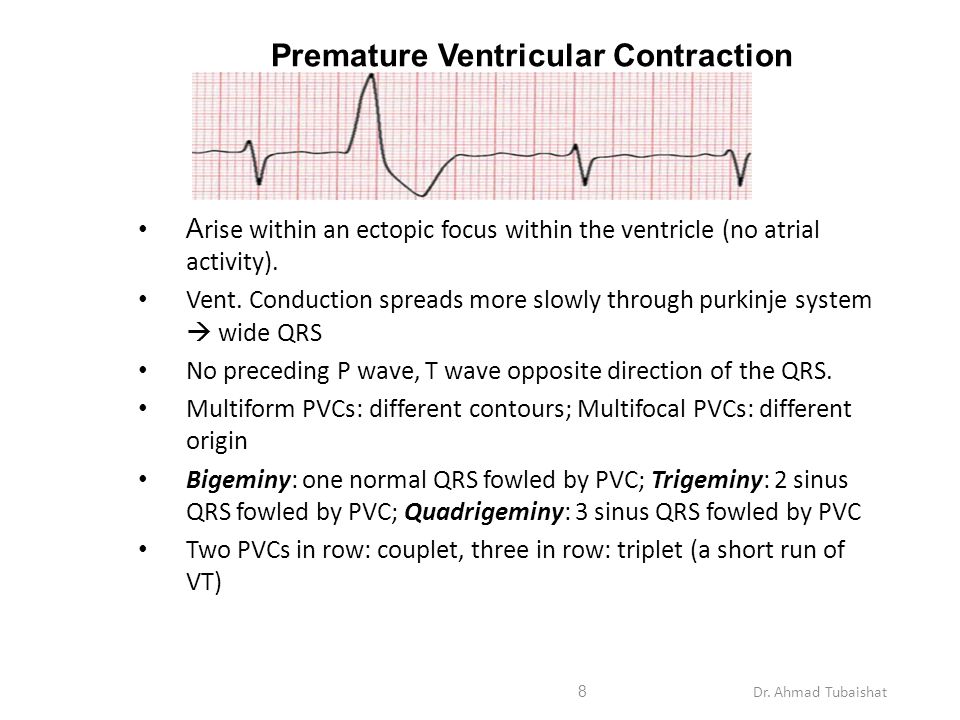 This phenomenon with varying degrees of intensity is observed in almost all pregnant women.
This phenomenon with varying degrees of intensity is observed in almost all pregnant women.
Many primiparas are concerned about the difference between preparatory contractions and labor.
Here are some differences:
- Frequency of contractions. Training bouts do not become more frequent, the intervals between them may be different. Labor pains are regular, the interval between them is reduced.
- Duration of contractions. Training bouts have different durations, from a few seconds to minutes, their duration does not increase over time. Labor pains tend to lengthen.
- Soreness. Preparatory contractions may not be accompanied by pain at all, or they may be quite noticeable, up to a feeling of sharp pain. However, their intensity weakens over time and the pain disappears. Labor pains are painful and constantly intensify.
- Localization. Braxton-Hicks contractions can be felt in various places - in the lower part of the uterus, in the region of its bottom, along the side walls, covering the entire abdomen.
 Labor pains begin with a contraction of the lower abdomen, spreading to the front. Often in childbirth, pain in the lower back is felt, while the nature of the pain resembles menstrual pain.
Labor pains begin with a contraction of the lower abdomen, spreading to the front. Often in childbirth, pain in the lower back is felt, while the nature of the pain resembles menstrual pain. - Relationship with body position. Preparatory contractions may disappear after walking or, on the contrary, rest. A change in body position can relieve the tension in some muscles, which also causes a decrease in the appearance of training contractions. Labor pains may be somewhat relieved in a certain position - when leaning forward, in the knee-elbow position, etc. - but their frequency and duration will still increase.
- Reaction to medication. The use of antispasmodic drugs - NO-ShPY, BUSCOPAN, PAPAVERIN, etc. - approved by the attending physician, can weaken or completely stop false contractions. The effect of antispasmodics on labor pains is minimal.
Any pain or discomfort should be reported to the gynecologist: this will help the expectant mother to resolve doubts and cope with anxiety. Feeling safe is the best companion of pregnancy.
Feeling safe is the best companion of pregnancy.
35th week
BABY
The length of the body of the fetus is 46--47 cm, weight - 2200-2300 g. These figures in the last weeks of pregnancy can vary greatly. The growth and weight of the fetus largely depend on heredity, individual parameters. Starting from 35 weeks, the baby will gain 200-250 g weekly. The fetus occupies almost the entire uterine cavity, its back is rounded, arms and legs are bent, brought to the body. The layer of subcutaneous fat increases significantly, which significantly “rounds” the body of the fetus. The closing of the eyelids and the contraction of facial muscles change the baby's facial expression quite often. The skin of the body becomes pink, smooth, the amount of cheese-like lubricant begins to decrease. Vellus hair covers separate small areas of the body - shoulders, back. The nails protrude beyond the tips of the fingers.
FUTURE MOTHER
The fundus of the uterus is 35 cm higher from the pubis and 15 cm higher from the navel. particularly light. The growing uterus does not allow the lungs to expand, respiratory movements are limited, which is manifested by shortness of breath. Almost all pregnant women to one degree or another experience a feeling of shortness of breath - a feeling of lack of air, frequent and shallow breathing, a desire to take a deep breath. As a rule, these sensations occur for a period of 28 weeks and reach their peak at the 35-36th week. After 37 weeks of pregnancy, the abdomen droops, which greatly facilitates breathing.
particularly light. The growing uterus does not allow the lungs to expand, respiratory movements are limited, which is manifested by shortness of breath. Almost all pregnant women to one degree or another experience a feeling of shortness of breath - a feeling of lack of air, frequent and shallow breathing, a desire to take a deep breath. As a rule, these sensations occur for a period of 28 weeks and reach their peak at the 35-36th week. After 37 weeks of pregnancy, the abdomen droops, which greatly facilitates breathing.
Shortness of breath during pregnancy is associated not only with the mechanical pressure of the uterus on the diaphragm, but also with the relaxing effect of hormones on the muscles of the bronchi and lungs. Most often, it is provoked by physical activity - climbing stairs, a long walk, etc. However, it is not uncommon for shortness of breath to occur at rest, especially when lying down. Both prolonged lying in a horizontal position and excessive exercise can contribute to increased shortness of breath.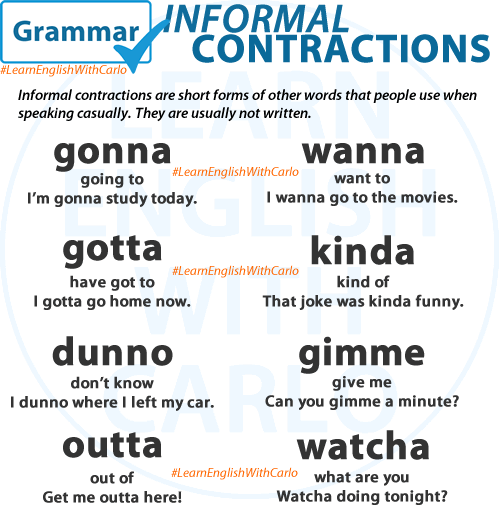 To alleviate her condition, the expectant mother needs to be rational about the daily routine - it is reasonable to alternate rest and physical activity. It is important to monitor your posture, as slouching exacerbates shortness of breath, reducing the already insufficient lung capacity. If shortness of breath is accompanied by blue lips or nails, sensations of pain behind the sternum, darkening before the eyes, nausea or vomiting, fainting, then an urgent need to consult a doctor.
To alleviate her condition, the expectant mother needs to be rational about the daily routine - it is reasonable to alternate rest and physical activity. It is important to monitor your posture, as slouching exacerbates shortness of breath, reducing the already insufficient lung capacity. If shortness of breath is accompanied by blue lips or nails, sensations of pain behind the sternum, darkening before the eyes, nausea or vomiting, fainting, then an urgent need to consult a doctor.
36th week
BABY
The growth of the fetus by this term is about 47--48 cm, and the weight is about 2300-2500 g. The fetus enters a period of intensive preparation for childbirth. Each of the organs is already functionally mature enough to ensure the viability of the fetus. 36 weeks is the beginning of the preparatory journey, and the upcoming weeks of pregnancy are designed to finally form the baby's readiness for extrauterine life.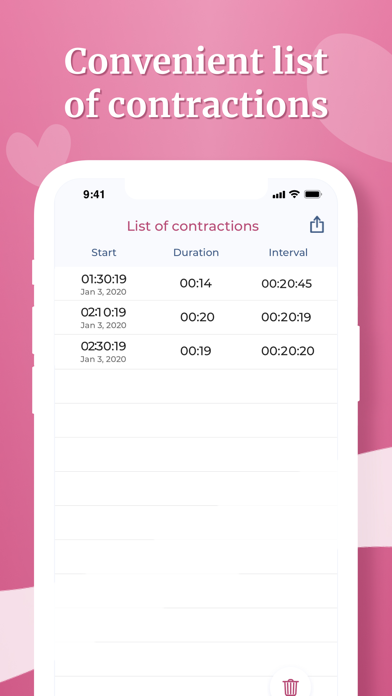
By 36 weeks, the fetus is in its final position in the uterus. As a rule, this is a longitudinal position, occipital presentation - in this case, the fetus is located head down, facing the mother's back. This is the most comfortable position that ensures the greatest safety of the baby during childbirth. More rarely, breech presentation is a condition in which the buttocks and legs of the fetus are located at the bottom of the uterus. This is a relative indication for operative delivery. The final decision on caesarean section or independent childbirth is made by doctors in each case individually.
A change in the position of the fetus in the uterus is possible, but this happens infrequently, since at this time the fetus occupies almost all the free space in the uterus, which significantly limits its motor activity. As a rule, if a change in the position of the fetus occurs, then only from the pelvic to the head. The reverse cases - the transition of the baby from the head position to the pelvic position - are practically impossible, since the head of the fetus is heavier than the buttocks and occupies the longitudinal position completely, by analogy with a float in water, the heavy part of which always outweighs.
FUTURE MOTHER
The height of the uterus is 36 cm, the volume of the abdomen is maximally increased, the bottom reaches the costal arches. At this time, the pregnant woman's body also begins its journey of preparing for the upcoming birth. Changes begin with hormonal changes: the level of special hormones, oxytocin and prostaglandins, increases slightly in a woman. These active substances play a crucial role in the process of preparing for childbirth and directly during them. A slight increase in their level from the period of 36-37 weeks of pregnancy leads to an increase in Braxton-Hicks training contractions, an increase in urination and defecation, and the appearance of more abundant mucous discharge from the vagina.
Harbingers - childbirth is coming soon!
Wrestler Maria Vladimirovna
Obstetrician-gynecologist
MD GROUP Clinical Hospital, Mother and Child Clinic Savelovskaya
False contractions
They may appear after the 38th week of pregnancy. False contractions are similar to Braxton-Hicks contractions, which a woman could already feel starting from the second trimester of pregnancy (the uterus seems to stiffen for a few seconds - a couple of minutes, then the tension in it subsides). False contractions train the uterus before childbirth, they are irregular and painless, the intervals between them are not reduced. Real labor pains, on the contrary, are regular, their strength gradually increases, they become longer and more painful, and the intervals between them are reduced. That's when you can already say that the birth began for real. In the meantime, false contractions are going on, it is not necessary to go to the maternity hospital - you can easily survive them at home.
False contractions are similar to Braxton-Hicks contractions, which a woman could already feel starting from the second trimester of pregnancy (the uterus seems to stiffen for a few seconds - a couple of minutes, then the tension in it subsides). False contractions train the uterus before childbirth, they are irregular and painless, the intervals between them are not reduced. Real labor pains, on the contrary, are regular, their strength gradually increases, they become longer and more painful, and the intervals between them are reduced. That's when you can already say that the birth began for real. In the meantime, false contractions are going on, it is not necessary to go to the maternity hospital - you can easily survive them at home.
Abdominal prolapse
Approximately two to three weeks before birth, the baby, in preparation for birth, presses the presenting part (usually the head) against the lower part of the uterus and pulls it down. As a result, the uterus moves lower into the pelvic region, its upper part ceases to put pressure on the internal organs of the chest and abdominal cavity. In the people it is called - the stomach dropped. As soon as the stomach drops, the expectant mother notices that it has become easier for her to breathe, but, on the contrary, it becomes more difficult to sit and walk. Heartburn and belching also disappear (after all, the uterus no longer presses on the diaphragm and stomach). But, having dropped down, the uterus begins to put pressure on the bladder - naturally, urination becomes more frequent.
In the people it is called - the stomach dropped. As soon as the stomach drops, the expectant mother notices that it has become easier for her to breathe, but, on the contrary, it becomes more difficult to sit and walk. Heartburn and belching also disappear (after all, the uterus no longer presses on the diaphragm and stomach). But, having dropped down, the uterus begins to put pressure on the bladder - naturally, urination becomes more frequent.
For some, uterine prolapse causes a feeling of heaviness in the lower abdomen and even slight pain in the area of the inguinal ligaments. These sensations arise due to the fact that the child's head, moving down, irritates the nerve endings of the pelvic organs.
During the second and subsequent births, the belly drops later - right before the birth. It happens that this harbinger of childbirth is not at all.
Removal of the mucous plug
This is one of the main and obvious precursors of childbirth. During pregnancy, the glands in the cervix produce a secret (it looks like a thick jelly and forms the so-called cork), which prevents various microorganisms from entering the uterine cavity. Before childbirth, under the influence of estrogens, the cervix softens, the cervical canal opens slightly and the cork can come out - the woman will see that there are mucus clots on the linen that look like jelly. Cork can be of different colors - white, transparent, yellowish-brown or pink-red. Often it is stained with blood - this is completely normal and may indicate that childbirth will occur within the next day. The mucus plug can come out all at once (at once) or come out piecemeal throughout the day.
Before childbirth, under the influence of estrogens, the cervix softens, the cervical canal opens slightly and the cork can come out - the woman will see that there are mucus clots on the linen that look like jelly. Cork can be of different colors - white, transparent, yellowish-brown or pink-red. Often it is stained with blood - this is completely normal and may indicate that childbirth will occur within the next day. The mucus plug can come out all at once (at once) or come out piecemeal throughout the day.
Weight loss
Approximately two weeks before delivery, weight loss may occur, usually by 0.5–2 kg. This happens because excess fluid is removed from the body and swelling decreases. If earlier during pregnancy, under the influence of the hormone progesterone, fluid in the body of a pregnant woman accumulated, now, before childbirth, the effect of progesterone decreases, but other female sex hormones - estrogens - begin to work hard, they remove excess fluid from the body of the expectant mother.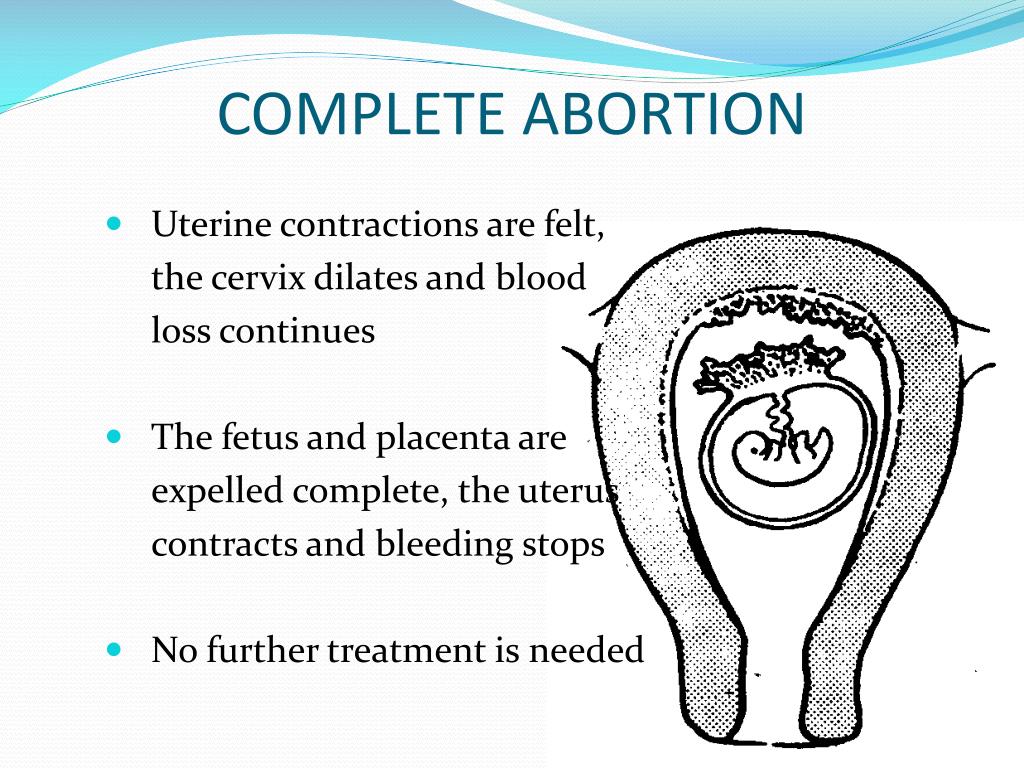
In addition, the expectant mother often notices that at the end of pregnancy it became easier for her to put on rings, gloves, shoes - this means that swelling on the hands and feet has decreased.
Changes in stool
Right before childbirth, hormones often act on the intestines - they relax its muscles, as a result, stool disorder begins. Sometimes such frequent (up to 2-3 times a day) and even loose stools are mistaken for an intestinal infection. But if there is no nausea, vomiting, discoloration and smell of feces, or any other symptoms of intoxication, you should not worry: this is one of the harbingers of the upcoming birth.
On the eve of childbirth, you often don't feel like eating at all. All this is also the preparation of the body for natural childbirth.
Mood changes
Many women experience mood changes a few days before giving birth. The expectant mother gets tired quickly, she wants to have more rest, sleep, even some kind of apathy appears.