Newborn hearing screening results
Your Baby's Hearing Screening and Next Steps
On this page:
- Why is it important to have my baby’s hearing screened early?
- When will my baby’s hearing be screened?
- How will my baby’s hearing be screened?
- What should I do if my baby’s hearing screening reveals potential hearing loss?
- The follow-up exam revealed that my baby’s hearing is fine. Does that mean we don’t need to check his or her hearing again?
- How can I help my child with hearing loss develop language skills?
- What devices could help my child hear and communicate better?
- What language and communication approaches are available for my child?
- Will my child be successful in school?
- Baby’s hearing screening and next steps: Timeline for parents
- Where can I find more information about hearing screening and communication approaches?
Most children hear and listen to sounds at and even before birth. They learn to talk by imitating the sounds they hear around them and the voices of their parents and caregivers. But that’s not true for all children. In fact, about two or three out of every 1,000 children in the United States are born with detectable hearing loss in one or both ears. More lose hearing later during childhood. Children who have hearing loss may not learn speech and language as well as children who can hear. For this reason, it’s important to detect hearing loss as early as possible.
Because of the need for prompt identification of and intervention for childhood hearing loss, universal newborn hearing screening programs currently operate in all U.S. states and most U.S. territories. With help from the federal government, every state has established an Early Hearing Detection and Intervention Program. As a result, about 98% of babies have their hearing screened before 1 month of age.
Why is it important to have my baby’s hearing screened early?
The most important time for a child to learn language (spoken or signed) is in the first 3 years of life, when the brain is developing and maturing. In fact, children with typical hearing begin learning speech and language in the first 6 months of life. This is why it is so important to screen and start interventions for hearing loss as early as possible. Research shows that children with hearing loss who get help early develop better language skills than those who don’t.
In fact, children with typical hearing begin learning speech and language in the first 6 months of life. This is why it is so important to screen and start interventions for hearing loss as early as possible. Research shows that children with hearing loss who get help early develop better language skills than those who don’t.
When will my baby’s hearing be screened?
Your baby’s hearing should be screened before he or she leaves the hospital or birthing center. If not, make sure the baby is tested during the first month of life. If your baby’s hearing was not tested within 1 month of birth, or if you haven’t been told the results of the hearing screening, ask your child’s doctor today. Quick action will be important if the screening shows potential hearing loss.
How will my baby’s hearing be screened?
A newborn undergoes a hearing screening.
Two different tests are used to screen for hearing loss in babies. Your baby can rest or sleep during both tests.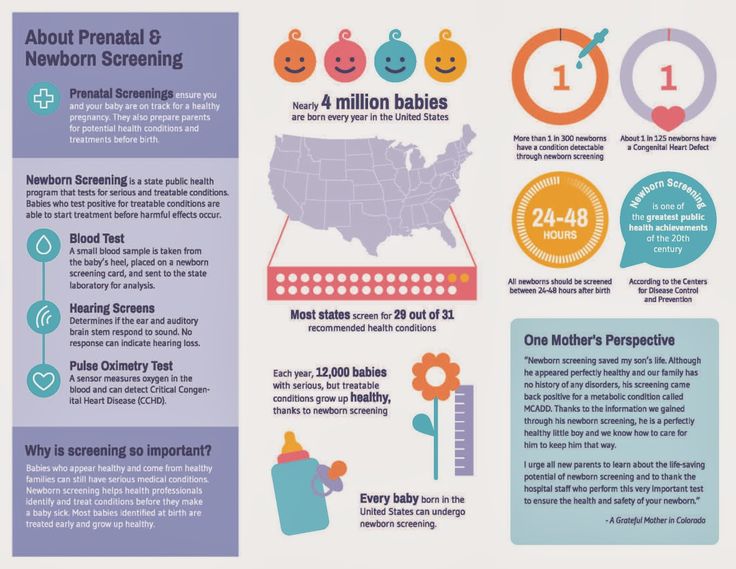
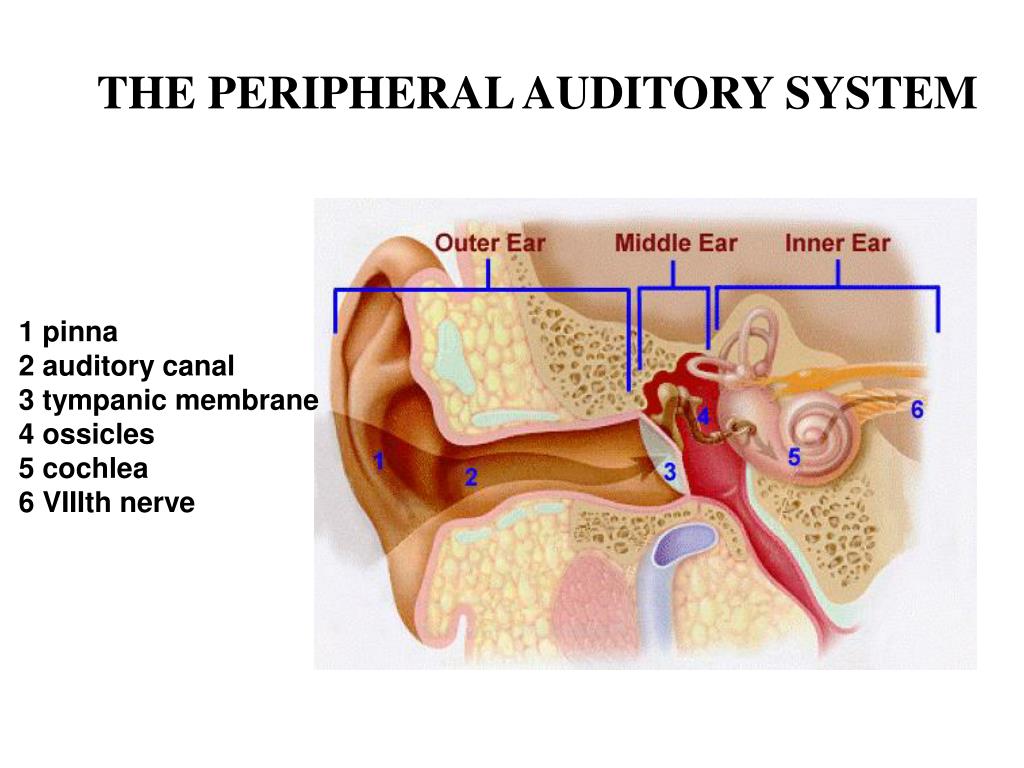
- Otoacoustic emissions (OAE) tests whether some parts of the ear respond to sound. During this test, a soft earphone is inserted into your baby’s ear canal. It plays sounds and measures an "echo" response that occurs in ears with normal hearing. If there is no echo, your baby might have hearing loss.
- The auditory brain stem response (ABR) tests how the auditory nerve and brain stem (which carry sound from the ear to the brain) respond to sound. During this test, your baby wears small earphones and has electrodes painlessly placed on his or her head. The electrodes adhere and come off like stickers and should not cause discomfort.
What should I do if my baby’s hearing screening reveals potential hearing loss?
If the results show that your baby may have hearing loss, make an appointment with a pediatric audiologist—a hearing expert who specializes in the assessment and management of children with hearing loss. This follow-up exam should be done as soon as possible, ideally by the time the baby is 2 to 3 months old. The audiologist will conduct tests to determine whether your baby has a hearing problem and, if so, the type and extent of that problem.
The audiologist will conduct tests to determine whether your baby has a hearing problem and, if so, the type and extent of that problem.
If you need help finding a pediatric audiologist, ask your pediatrician or the hospital staff who conducted your baby’s screening. They may even be able to help you schedule an appointment. You can also try the directories provided by the American Academy of Audiology or the American Speech–Language–Hearing Association. If the follow-up examination confirms that your baby has hearing loss, he or she should begin receiving intervention services as soon as possible, ideally by the age of 3 to 6 months. See our Baby’s hearing screening and next steps: Timeline for parents (below) for a guide to follow.
The pediatric audiologist may recommend that your baby visit a pediatric ear, nose, and throat (ENT) physician who specializes in conditions affecting the ear, known as a pediatric otologist. A pediatric otologist can determine possible causes of hearing loss and recommend intervention options. If your child has siblings, the audiologist or otologist may also recommend that their hearing be tested.
If your child has siblings, the audiologist or otologist may also recommend that their hearing be tested.
The follow-up exam revealed that my baby’s hearing is fine. Does that mean we don’t need to check his or her hearing again?
Not necessarily. Hearing loss can occur at any time of life. Some inherited forms of hearing loss don’t appear until a child is older. If your baby was exposed to certain infections before being born, they are more likely to have gradual hearing loss during childhood. Other factors, such as childhood illness, ear infection, head injury, certain medications, and loud noise are also linked to hearing loss in children. Use Your Baby’s Hearing and Communicative Development Checklist to monitor and track your child’s communication milestones through age 5. If you have concerns about your child’s hearing at any age, talk to your pediatrician right away.
How can I help my child with hearing loss develop language skills?
When interventions begin early, children with hearing loss can develop language skills that help them communicate freely and learn actively. The Individuals with Disabilities Education Act ensures that all children with disabilities have access to the services they need to get a good education. Your community may also offer additional services to help support your child.
The Individuals with Disabilities Education Act ensures that all children with disabilities have access to the services they need to get a good education. Your community may also offer additional services to help support your child.
Your baby’s health care team will help you find services and methods to overcome communication barriers. You may also be referred to a speech-language pathologist or a teacher who is experienced in working with children with hearing loss. Talk to and communicate with your child often and stay up-to-date with all health care appointments.
What devices could help my child hear and communicate better?
Depending on your baby’s hearing loss and communication needs, some of these devices and tools may help to maximize his or her communication skills.
- Hearing aids. Worn behind the ear, hearing aids help make sounds louder and clearer. Hearing aids can be used for different degrees of hearing loss in babies as young as 1 month.
 A pediatric audiologist who is experienced in treating infants and children can help you choose the best hearing aid and make sure that it fits securely and is properly adjusted. Read the NIDCD fact sheet Hearing Aids for more information.
A pediatric audiologist who is experienced in treating infants and children can help you choose the best hearing aid and make sure that it fits securely and is properly adjusted. Read the NIDCD fact sheet Hearing Aids for more information. - Cochlear implants. If your child cannot benefit from a hearing aid, your doctor or audiologist may suggest a cochlear implant. This electronic device can provide a sense of sound to people who are profoundly deaf or hard-of-hearing. The device converts sounds into electrical signals and carries them past the nonworking part of the inner ear to the brain. Cochlear implants can be surgically placed in children as young as 12 months, or sometimes earlier.
With training, children with cochlear implants can learn to recognize sounds and understand speech. Studies have also shown that many eligible children who receive a cochlear implant early (before 18 months of age) can develop spoken language skills at a rate comparable to children with normal hearing, and many succeed in mainstream classrooms.
 Some doctors now recommend the use of two cochlear implants, one for each ear. An audiologist or otolaryngologist who specializes in cochlear implants can help you decide if a cochlear implant is appropriate for your child. Read the NIDCD fact sheet Cochlear Implants for more information.
Some doctors now recommend the use of two cochlear implants, one for each ear. An audiologist or otolaryngologist who specializes in cochlear implants can help you decide if a cochlear implant is appropriate for your child. Read the NIDCD fact sheet Cochlear Implants for more information. - Assistive devices. As your child grows, other devices may be useful. Some devices help children hear better in a classroom. Others amplify one-on-one conversations or make talking on the phone or watching TV and videos easier. Read the NIDCD fact sheet Assistive Devices for People with Hearing, Voice, Speech, or Language Disorders for more information.
What language and communication approaches might be available for my child?
Children who are deaf or hard-of-hearing can learn to communicate in several ways. Find out as much as you can about the communication choices and ask your health care team to refer you to experts if you want to know more. Because language development begins early, regardless of the communication mode you choose, you should engage with your child and begin intervention as soon as possible.
Common approaches used to help children with hearing loss communicate and interact with others include:
- Listening and spoken language (also known as auditory-verbal): works to strengthen listening, talking, and reading skills through the use of natural hearing and hearing devices such as hearing aids and cochlear implants, without the use of manual communication.
- Auditory-oral: emphasizes residual natural hearing in combination with amplification devices and technology to help children develop speech and spoken-language skills. It includes the use of speech reading and natural gestures in the communication process.
- Cued speech: is a system of specific hand shapes and placements that represent groups of consonants and vowels and that are used in combination with natural lip movements.
- American Sign Language: is a visual-manual, natural language that is used in the American Deaf community.

- Combined approaches: use aspects of various communication approaches, some of which are listed above, to expose children who are deaf or hard-of-hearing to many ways to communicate with others.
Will my child be successful in school?
Like all children, children who are deaf or hard-of-hearing can develop strong academic, social, and emotional skills and succeed in school. Find out how your school system helps children with hearing loss. With your input, your child’s school will develop an Individualized Education Program (IEP) or Individualized Family Service Plan (IFSP) for your child, and you should ask if an educational audiologist is available to be part of the academic team. Explore programs outside of school that may help you and your child and talk with other parents who have already dealt with these issues. The Individuals with Disabilities Education Act ensures that children with hearing loss receive free, appropriate, early-intervention services from birth through the school years. Contact the U.S. Department of Education, along with resources listed in our directory of organizations.
Contact the U.S. Department of Education, along with resources listed in our directory of organizations.
An educator teaching a young boy.
Baby’s hearing screening and next steps: Timeline for parents
Use this timeline to get started.
| Make sure that your baby’s hearing is screened either before you leave the hospital or immediately afterward. After the screening, find out the results. If your newborn was not screened in the hospital, schedule a screening to occur by the time your baby is 1 month old. |
| If your baby did not pass the hearing screening, immediately schedule a follow-up appointment with a pediatric audiologist. Ask your doctor or hospital for a list of pediatric audiologists, or use the directories provided by the American Academy of Audiology and the American Speech–Language–Hearing Association. | |
If you must cancel the follow-up appointment, reschedule it! Make sure you take your baby to a follow-up examination. This can occur as early as 2 months after birth, and by age 3 months at the latest. This can occur as early as 2 months after birth, and by age 3 months at the latest. |
| If the follow-up exam shows that your baby has hearing loss, start your baby in some form of intervention as soon as possible. Your baby can start receiving intervention services as early as 3 months after birth and no later than 6 months. Interventions can include hearing devices, such as hearing aids or cochlear implants, and various language and communication approaches. Ask your health care team about the options. |
| Remain active and involved in your child’s progress. | |
| If you move or change your contact information, make sure to tell your child’s doctors and specialists. | |
Even if the follow-up exam found no sign of hearing loss in your child, continue to monitor his or her communication development. If you have concerns, speak with your child’s doctor. If your child has risk factors for childhood hearing loss, speak with an audiologist about how often his or her hearing should be monitored. If your child has risk factors for childhood hearing loss, speak with an audiologist about how often his or her hearing should be monitored. |
Where can I find more information about hearing screening and communication approaches?
The NIDCD maintains a directory of organizations that provide information on the normal and disordered processes of hearing, balance, taste, smell, voice, speech, and language.
For more information, contact us at:
NIDCD Information Clearinghouse
1 Communication Avenue
Bethesda, MD 20892-3456
Toll-free voice: (800) 241-1044
Toll-free TTY: (800) 241-1055
Email: [email protected]
NIH Publication No. 21–4968
October 2021
*Note: PDF files require a viewer such as the free Adobe Reader.
Newborn Hearing Screening FAQs - HealthyChildren.org
Before you bring your newborn home from the hospital, your baby needs to have a
hearing screening.
From birth, one important way babies can learn is through listening and hearing. Although most infants can hear fine, 1 to 3 of every 1,000 babies born in the U.S. have hearing levels outside the typical range.
Newborn screening and diagnosis helps ensure all babies who are deaf or hard of hearing are identified as soon as possible. Then, they can receive early intervention services that can make a big difference in their communication and language development.
The American Academy of Pediatrics (AAP) recommends hearing screenings for all newborns. The goal is for all babies to have a newborn hearing screening by one month of age, ideally before they go home from the hospital; identified by 3 months of age and enrolled in early intervention or treatment, if identified as deaf or hard of hearing, by the age of 6 months. |
Why do newborns need hearing screening?
The hearing screening is a first and important step in helping understand if your baby may be deaf or hard of hearing. Without newborn hearing screening, it is hard to know when there are hearing changes in the first months and years of your baby's life.
Without newborn hearing screening, it is hard to know when there are hearing changes in the first months and years of your baby's life.
Babies may respond to noise by startling or turning their heads toward the sound, for example. But this doesn't necessarily mean they can hear all the sounds around them and everything we say. Babies who are deaf or hard of hearing may hear some sounds but still not hear enough to understand spoken language.
Infants who are deaf or hard of hearing need the right supports, care, and early intervention services to promote healthy development. If the hearing status is not identified, it may have negative effects on the baby's communication and language skills. Longer term, a missed hearing loss can also impact the child's academic achievement and social-emotional development.
How is the newborn hearing screening done?
According to the most recent Centers for Disease Control and Prevention (CDC) data, over 98% of newborns in the United States receive newborn hearing screening.
There are two screening methods that may be used:
-
Automated Auditory Brainstem Response (AABR)—This screen measures how the hearing nerve and brain respond to sound. Clicks or tones are played through soft earphones into the baby's ears. Three electrodes placed on the baby's head measure the hearing nerve and brain's response.
-
Otoacoustic Emissions (OAE)—This screen measures sound waves produced in the inner ear. A tiny probe is placed just inside the baby's ear canal. It measures the response (echo) when clicks or tones are played into the baby's ears.
Both screens are quick (about 5 to 10 minutes), painless, and may be done while your baby is sleeping or lying still. One or both screens may be used.
What if my baby does not pass the initial hearing screening?
If your baby does not pass the hearing screening at birth, it does not necessarily mean that she is deaf or hard of hearing. Fluid or
vernix inside the baby's ear, for example, or too much noise in the room can affect results. In fact, most babies who do not pass the newborn screening have typical hearing. But to be sure, it is extremely important to have further testing done.
Fluid or
vernix inside the baby's ear, for example, or too much noise in the room can affect results. In fact, most babies who do not pass the newborn screening have typical hearing. But to be sure, it is extremely important to have further testing done.
About 1 or 2 in every 100 babies will not pass the initial hearing screening at birth and will need tests with an audiologist who has experience working with babies. This testing should include a more thorough hearing and medical evaluation.
Be sure to talk with your baby's pediatrician about scheduling further tests if your baby does not pass the initial hearing screening at birth. The additional testing should be done as soon as possible, but before your baby is 3 months old.
Follow-up testing may start with one more screening similar to the type done in the hospital. Some hospitals or clinics may complete a diagnostic test at the time of follow-up, instead of re-screening. In young infants, the follow-up testing may be able to be completed while the baby naps.
In young infants, the follow-up testing may be able to be completed while the baby naps.
If my baby is identified as deaf or hard of hearing, what are the treatment and intervention options?
If your baby's audiologist confirms hearing changes, treatment and early intervention with a team of providers should start as soon as possible. Just like hearing children, children who are deaf or hard of hearing can achieve many things. Studies show your baby will have the best chance for spoken language development―on par with that of hearing peers―if any hearing changes are discovered, and support and intervention begins by 6 months of age. The earlier, the better.
In addition to your pediatrician and audiologist, every baby who is deaf or hard of hearing should be seen by a pediatric
otolaryngologist who specializes in the mechanics of the ear. Your pediatrician should also recommend seeing a pediatric
ophthalmologist, because some children can also have problems with their vision, and children who are deaf or hard of hearing are dependent on their vision for language input. Many children are also seen by a
geneticist to determine if there is a hereditary cause of hearing changes.
Many children are also seen by a
geneticist to determine if there is a hereditary cause of hearing changes.
Your state Early Hearing Detection and Intervention (EHDI) program can help provide you and your pediatrician with more information. Babies who are deaf or hard of hearing should be referred to Early Intervention for evaluation and services. Additionally, the Individuals with Disabilities Education Act (IDEA) supports intervention programs for children who are deaf or hard of hearing within early intervention and school programming.
The audiologist, together with the otolaryngologist, can tell you the
type and degree of hearing change and what the next steps are. These next steps can vary depending on your family's choices, as well as the type and degree of hearing change.
If my baby passes the newborn hearing screening, does it mean he or she will not have hearing loss later?
Unfortunately, no. Some babies may develop
hearing loss later in childhood. Causes of late onset or progressive hearing loss in children can include genetics,
frequent ear infections, other infections like
measles or
meningitis, a head injury, exposure to damaging levels of
loud noises, and secondhand
smoke. Newborns who need an extended period of neonatal intensive care may also be at an increased risk for hearing loss later.
Causes of late onset or progressive hearing loss in children can include genetics,
frequent ear infections, other infections like
measles or
meningitis, a head injury, exposure to damaging levels of
loud noises, and secondhand
smoke. Newborns who need an extended period of neonatal intensive care may also be at an increased risk for hearing loss later.
Even if your baby passes the newborn hearing screening, you should still watch for possible signs of hearing loss as your child grows. Talk with your pediatrician if your child:
|
If my baby passes the first hearing test, why is more screening needed?
Even if your child shows no signs of hearing changes, the AAP recommends they be screened again at ages 4, 5, 6, 8 and 10. Additional screenings are recommended sometime between ages 11-14, 15-17, and 18-21--or any time there is a concern. More frequent follow-up screenings may be recommended for children who have a higher risk for hearing loss. Hearing loss sometimes is gradual and hard to notice at first. Routine screenings can catch hearing changes early, when providing support and resources can have the most impact on the child's development.
Hearing loss sometimes is gradual and hard to notice at first. Routine screenings can catch hearing changes early, when providing support and resources can have the most impact on the child's development.
Remember:
Timing is everything. The sooner hearing changes are identified in a baby, the more likely interventions can help her reach her full potential. Talk with your pediatrician if you have any concerns about your child's hearing.
Additional Information & Resources:
Newborn Screening Tests
Early Hearing Detection and Intervention - A Program of the American Academy of Pediatrics
Centers for Disease Control and Prevention (CDC) National Center on Birth Defects and Developmental Disabilities (NCBDDD) - Provides research, basic information and statistics regarding hearing loss, screening and diagnosis, as well as current articles and educational materials for clinicians and families.

The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Hearing screening for newborns and young children
Given the importance of early detection and timely correction of hearing impairments, the hearing screening program for all newborns is currently being implemented in more than 50 countries. Hearing screening of newborns is an integral part of the program for the early detection and correction of hearing impairments in children, aimed at improving the quality of life of children with identified impairments by preventing secondary speech disorders, speech delay, poor academic performance and psycho-emotional disorders.
Standards for the implementation of the program for the early detection and correction of hearing impairment in children were formulated by the Joint Commission on Children's Hearing (USA) in 2007 and are generally accepted throughout the world. This is the so-called “1-3-6 Principle”, according to which:
This is the so-called “1-3-6 Principle”, according to which:
- Hearing screening is carried out for all newborns until they reach the age of 1 month , optimally until they are discharged from the maternity ward
- Audiological diagnosis (determining the degree and nature of hearing impairment) with positive screening results, i.e., detection of hearing impairment, is performed on all children until they reach the age of 3 months
- Rehabilitation of hearing impairments (hearing aids) for all children with identified irreversible hearing impairments begins no later than they reach the age of 6 months
Programs for early detection and correction of hearing impairments in children are not currently implemented in Ukraine. In this regard, objective auditory screening has been established at the CSR AURORA Medical Center based on the use of the most reliable screening method - registration of short-latency auditory evoked potentials (SEPs). This screening method detects hearing loss caused by damage to the middle ear, inner ear, auditory nerve and brainstem.
This screening method detects hearing loss caused by damage to the middle ear, inner ear, auditory nerve and brainstem.
Hearing screening based on ABR registration is carried out using modern equipment by experienced specialists of the AURORA Center, the evaluation of the screening results is carried out by an otolaryngologist-audiologist. Depending on the screening results, recommendations are developed on the tactics of managing the child.
In case of a positive result of the screening test, which indicates the likelihood of a hearing impairment in a child, we recommend that a diagnostic hearing examination be performed to identify the nature and degree of hearing loss, determine treatment and diagnostic tactics.
If the screening test is negative, the doctor may recommend follow-up with a follow-up screening in a few months to detect possible late hearing loss after reviewing the pregnancy and childbirth history. This is especially important if the child has certain somatic and genetic diseases.
When should I contact AURORA Medical Center for hearing screening of newborns and young children?
Many years of experience in programs for the early detection and correction of hearing impairment in children showed that 50% of children with congenital auditory disorders had risk factors for hearing disorders.
List of risk factors for which hearing screening of newborns and young children should be mandatory.
- Maternal infections during pregnancy, in particular cytomegalovirus, rubella, syphilis, herpes, toxoplasmosis, HIV.
- Anomalies in the development of the head, face, auricles, including nonunion of the palate, skin outgrowths and pits in the auricles and ear canal, congenital cysts of the neck.
- All diseases or conditions that require a child to be in a neonatal intensive care unit for 48 hours or more
- Use of ototoxic drugs by the mother during pregnancy or by the child during the neonatal period
- Prematurity - gestational age less than 37 weeks
- Hearing disorders in next of kin,
- Neonatal hyperbilirubinemia (jaundice) with bilirubin levels greater than 200 µmol/liter
- Mechanical ventilation
- Congenital diseases that cause hearing loss: Down syndrome, Usher syndrome, Pendred syndrome, Waardenburg syndrome, Stickler syndrome, Alport syndrome, Treacher-Collins syndrome, Goldenhar syndrome, etc.

As your child gets older, hearing screening should be done if:
- Child's lag in speech development, discrepancy between speech and vocabulary for age
- Inadequate or absent response to sounds
- Frequent otitis media or isolated cases of long-standing otitis media
- Traumatic brain injury resulting in loss of consciousness and/or skull fracture
- Bacterial meningitis and other infections that may cause hearing complications (mumps, encephalitis, viral labyrinthitis, sepsis)
- Exposure to loud noise
- Alertness of parents or guardians regarding the child's hearing
- Taking ototoxic drugs
- Chemotherapy
Early detection of hearing impairment allows timely and correct choice of tactics for the treatment and rehabilitation of the child. This is an invaluable chance for hearing-impaired children to become full-fledged members of society. Hearing screening is the first step in identifying hearing loss.
Our many years of experience in providing high quality hearing care for children will help you. Contact us at AURORA Medical Center ® .
Universal newborn audiological screening: achievements and challenges
Congenital hearing loss is a fairly common pathology. Congenital hearing impairment may be the result of an unfavorable course of pregnancy (intrauterine infections, the use of ototoxic drugs, toxicosis) or perinatal pathology (prematurity, very low birth weight, hypoxia, fetal asphyxia, hemolytic disease) [1]. In half of cases of congenital deafness, hereditary etiology is determined, the most frequent genetic disorders are detected in the connexin 26 gene (GJB2 gene) [2].
According to epidemiological studies, 1 child per 1000 healthy births has congenital deafness; taking into account unilateral and mild degrees of hearing loss, the prevalence of hearing loss is 2-3 per 1000, and in the case of a newborn in the intensive care unit, this figure rises to 20-40 per 1000. This is an order of magnitude higher than the prevalence of any other congenital pathology, regarding which screens newborns [3, 4].
This is an order of magnitude higher than the prevalence of any other congenital pathology, regarding which screens newborns [3, 4].
Complete auditory stimulation in the first 6 months of a child's life is very important for the development of speech, since during this period the maturation of auditory neurons in the brainstem and the formation of neural connections with the auditory cortex take place [5]. It has been shown that success in the development of speech skills in children with congenital hearing impairments largely depends on the timing of detection and inclusion in the rehabilitation program [6].
Identification of hearing disorders by negotiability leads to very late diagnosis and delays the start of deaf pedagogical rehabilitation. The audiological screening strategy based on the analysis of risk factors and the child's behavioral responses to sounds, introduced in 1996 [7], proved to be insufficiently effective and reliable, risk factors are detected only in half of children with congenital hearing loss. Thus, to improve the effectiveness of audiological screening in children, it is necessary to use objective methods for studying hearing in newborns [8].
Thus, to improve the effectiveness of audiological screening in children, it is necessary to use objective methods for studying hearing in newborns [8].
The main criteria for the effectiveness of screening methods are high sensitivity (probability of failing the test in the presence of hearing impairment) and specificity (probability of passing the test in the absence of hearing impairment), simplicity and speed of the study, the possibility of conducting effective therapeutic and rehabilitation measures for the identified hearing pathology.
Delayed evoked otoacoustic emission (DETAE) and short-latency auditory evoked potentials (SEPs) are used as screening methods for diagnosing hearing impairment. Registration of the TEOAE is characterized by ease and speed of implementation. It is worth noting the insufficiently high specificity of the method in relation to the diagnosis of congenital hearing loss, since TTOAE is not recorded in case of impaired sound conduction as a result of obstruction of the external auditory canal or the presence of exudate in the tympanic cavity, which gives false positive results. False-negative test results occur in the presence of retrocochlear pathology, which is likely in 10% of newborns with severe hearing loss, as well as in cases of progressive hearing loss and hearing loss with late manifestations.
False-negative test results occur in the presence of retrocochlear pathology, which is likely in 10% of newborns with severe hearing loss, as well as in cases of progressive hearing loss and hearing loss with late manifestations.
Registration of ABR is characterized by higher sensitivity and specificity compared to registration of TEOAE, however, this study is longer, requires significant technical support and staff qualifications, therefore it is used to verify hearing loss. A modification of the AFRP - registration of stationary ARP - combines the advantages of both methods, but has not yet become widespread [9].
Based on the conducted controlled studies on the effectiveness of universal audiological screening of newborns [10-12] and within the framework of the Priority National Project "Health" since 2008, a program of universal audiological screening of newborns has been implemented in the Russian Federation. The goal of the program is early, up to 6 months of life, identification and rehabilitation of children with hearing impairment, which is the key to their timely speech and psychosocial development [13].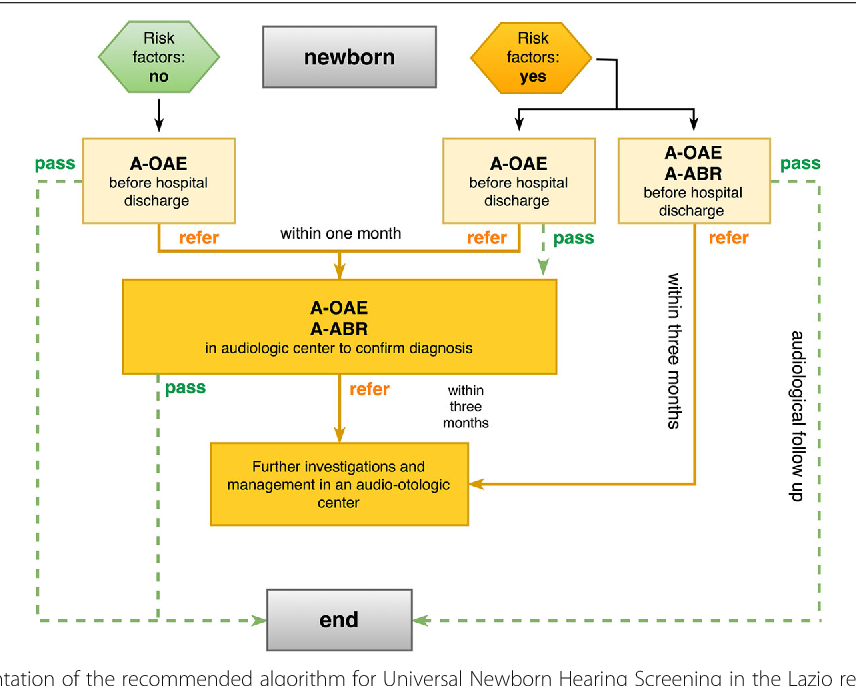
Universal audiological screening of newborns is carried out in two stages. At the 1st stage, the UAE is registered, all newborns are examined in obstetric institutions on the 3-4th day after birth, in the polyclinic on the 4-6th week of life, children with a positive screening result (“failed”) are examined in the maternity hospital, as well as children born outside maternity facilities, and children who have been screened but have risk factors for hearing loss. The 2nd stage of screening involves a full audiological examination with the registration of ABRs in hearing rehabilitation centers (surveillance centers, offices) for children aged 4-6 months who have not passed the 1st stage; in cases with confirmed hearing loss, it is necessary to form an individual rehabilitation program (see table).
The Joint Newborn Hearing Screening Committee [14] recommends that no more than 4% fail at Stage 1 screening. The number of false-positive results (erroneously detected) should be less than 3% of the entire population examined in the absence of false-negative results (not detected true hearing impairment) ideally; in the maternity hospital or during the 1st month of life, at least 95% of newborns; at follow-up, at least 70% of infants not screened at the hospital or within 1 month of life should have a final audiological examination and confirmation of hearing loss.
An important aspect of the implementation of the universal audiological screening program for newborns and children in the first year of life is the training of specialists. This implies a thematic improvement under the program "Audiological screening of newborns" for participation in the 1st stage of screening of pediatricians, neonatologists, otorhinolaryngologists, neurologists, and nurses. In connection with the introduction of audiological screening, there is an increasing need to train audiologists for a full audiological examination at the 2nd stage, and teachers of the deaf for further rehabilitation measures.
To evaluate the effectiveness of universal audiological screening in 2012, we made inquiries to regional audiological centers and offices. Responses were received from 28 regions, and the analysis included complete and convincing data from 15 regions. To assess the dynamics of the development of the audiological screening program, data from 9 regions for 2011 and 2012 were analyzed.
Most neonatal screening coverage takes place in maternity facilities, which makes it important that they are equipped with screening equipment. In 2012, out of 15 regions, the equipment of maternity hospitals was 95-100% in 12 regions, 70-80% in 2 regions (Vladimir and Tver regions), very low equipment (46%) in one region (Nizhny Novgorod region). The average equipment of maternity hospitals in 15 regions was 92.15±15.45%.
Dynamics of equipment development in 2011-2012 shown in fig. 1. Figure 1. Equipment of obstetric facilities with diagnostic equipment in 2011-2012
An increase was noted in 4 regions, a decrease in one region out of 9. It is worth noting that in some regions the total number of obstetric facilities has decreased. So, in the Vladimir region in 2011, there were 17 maternity hospitals, in 2012 - 10, in the Tver region - 42 and 37 maternity hospitals, respectively.
The average coverage of newborns by screening in maternity hospitals in 2012 was 86±10. 43%. In regions with insufficient equipment of maternity hospitals, the coverage of newborns in children's clinics in the 1st month is of particular importance. The total coverage of newborns at the 1st stage of screening should be higher than the coverage in maternity hospitals by examining children who were not screened in the maternity hospital and children born outside of maternity hospitals. Thus, the overall coverage at the 1st stage averaged 94.14±9.0%, in almost all regions it exceeded 90% (Fig. 2). Figure 2. Coverage of newborns at the 1st screening stage in 2012.
43%. In regions with insufficient equipment of maternity hospitals, the coverage of newborns in children's clinics in the 1st month is of particular importance. The total coverage of newborns at the 1st stage of screening should be higher than the coverage in maternity hospitals by examining children who were not screened in the maternity hospital and children born outside of maternity hospitals. Thus, the overall coverage at the 1st stage averaged 94.14±9.0%, in almost all regions it exceeded 90% (Fig. 2). Figure 2. Coverage of newborns at the 1st screening stage in 2012.
This fact indicates the successful implementation of the universal audiological screening program in these regions. Paradoxically, a single excess of the total coverage indicator at the 1st stage is more than 100%, which is associated with the imperfection of data collection and the re-registration of already examined children.
Dynamics for 2011-2012 For 9 regions, the following features can be noted. In 4 regions, there is an increase in the coverage of newborn screening in maternity hospitals and the overall coverage at the 1st stage. In the Voronezh region, despite a significant increase in the equipment of maternity hospitals, the coverage of newborn screening in maternity hospitals decreased from 73.8% to 68.67%, while the overall coverage remained unchanged. In the Tambov region, with constant full equipment, this indicator in maternity hospitals decreased from 89.54 to 83.8%, and the total coverage at the 1st stage increased from 95.35 to 99.29%.
In 4 regions, there is an increase in the coverage of newborn screening in maternity hospitals and the overall coverage at the 1st stage. In the Voronezh region, despite a significant increase in the equipment of maternity hospitals, the coverage of newborn screening in maternity hospitals decreased from 73.8% to 68.67%, while the overall coverage remained unchanged. In the Tambov region, with constant full equipment, this indicator in maternity hospitals decreased from 89.54 to 83.8%, and the total coverage at the 1st stage increased from 95.35 to 99.29%.
The frequency of a positive screening result (“failed”) at the 1st stage in 2012 in 15 regions averaged 3.14±2.03% of the number of newborns, which corresponds to the recommendations [14] and indicates a high efficiency of the program universal audiological screening. In dynamics for 9 regions, this indicator decreased from 4.03±2.92 to 3.40±2.47%.
The frequency of detection of severe hearing impairment in children under 1 year of age in 2012, according to data from 15 regions, averaged 0. 03±0.03% or 3 per 10,000 newborns. When compared by 9regions, severe hearing impairment was detected in 0.04±0.02% of newborns in 2011 and 0.03±0.03% in 2012
03±0.03% or 3 per 10,000 newborns. When compared by 9regions, severe hearing impairment was detected in 0.04±0.02% of newborns in 2011 and 0.03±0.03% in 2012
The frequency of detection of all hearing impairments in 2012 in 15 regions was 0.21±0.23% or 2 per 1,000 newborns, which corresponds to the data of epidemiological studies. In 9 regions, hearing impairments detected in 2011 and 2012 amounted to 0.21±0.18 and 0.25±0.30%, respectively.
Continuity of screening steps means that all children not screened in step 1 are screened in step 2 universal audiological screening. This indicator is calculated as the ratio of the number of children examined at the 2nd stage to the number of children who did not pass the 1st stage.
In 2012, in 15 regions, 76% of children who did not pass the 1st stage of screening were examined at the 2nd stage. In the Republic of Mari El, the Voronezh region, the succession of stages was very low and amounted to 25%, in the Vladimir, Saratov regions, Perm region - about 40%. In 7 out of 15 regions, a succession rate of more than 70% was noted, which indicates a sufficient effectiveness of the audiological screening program. In several regions, the stage succession rate exceeded 100%, which can be explained by the additional inclusion of children examined outside the screening program. The identification of such facts makes the task of improving the methodology for collecting information within the framework of the universal audiological screening of newborns urgent, and it becomes obvious that there is a need to create a unified database for adequate registration and tracking of children who have not passed the 1st stage of screening.
In 7 out of 15 regions, a succession rate of more than 70% was noted, which indicates a sufficient effectiveness of the audiological screening program. In several regions, the stage succession rate exceeded 100%, which can be explained by the additional inclusion of children examined outside the screening program. The identification of such facts makes the task of improving the methodology for collecting information within the framework of the universal audiological screening of newborns urgent, and it becomes obvious that there is a need to create a unified database for adequate registration and tracking of children who have not passed the 1st stage of screening.
Thus, during the implementation of the program of universal audiological screening of newborns in Russia, a significant number of maternity hospitals and children's clinics have been equipped with diagnostic equipment, and specialists for screening are being trained. Further improvement of the material base, informing the society and parents about the importance of timely diagnosis of hearing, coordination of the work of maternity hospitals, children's clinics and deafness centers, improving the methodology for collecting and analyzing data will help increase the effectiveness of the program.