Headaches and fatigue during pregnancy
[Headache, fatigue and edema of the lower limbs during the third trimester of normal pregnancy]
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
. 1996 Nov 18;158(47):6778-80.
[Article in Danish]
M Lebech 1 , M Hansen, A Knudsen
Affiliations
Affiliation
- 1 Gynaekologisk-obstetrisk afdeling, Hjørring/Brønderslev Sygehus.
- PMID: 8992699
[Article in Danish]
M Lebech et al. Ugeskr Laeger. .
. 1996 Nov 18;158(47):6778-80.
Authors
M Lebech 1 , M Hansen, A Knudsen
Affiliation
- 1 Gynaekologisk-obstetrisk afdeling, Hjørring/Brønderslev Sygehus.

- PMID: 8992699
Abstract
A series of 180 pregnant women with normal pregnancies participated in the study. A questionnaire concerning the presence of headache, fatigue and oedema of the lower limbs was filled out daily from the 30th gestational week to delivery. After the study period 120 questionnaires, of whom eight were excluded, were available for analysis. The weekly prevalences of headache and fatigue during the observation-period were nearly constant with values of 20% and 50%, respectively. The weekly prevalence of oedema increased significantly from 20% in the 31st week to 60% in the 42nd gestational week. Thirty-five percent had not suffered from headache, 22% did not report fatigue, and 42% did not describe oedema at all during the third trimester. The prevalence of headache and fatigue correlated significantly to increasing parity whereas headache was significantly correlated to decreasing age. Headache, fatigue, and oedema are common symptoms in the third trimester of normal pregnancy, and as such their presence alone should not usually give cause for suspicion of disease.
Headache, fatigue, and oedema are common symptoms in the third trimester of normal pregnancy, and as such their presence alone should not usually give cause for suspicion of disease.
Similar articles
-
The effect of pregnancy and parity on headache prevalence: the Head-HUNT study.
Aegidius K, Zwart JA, Hagen K, Stovner L. Aegidius K, et al. Headache. 2009 Jun;49(6):851-9. doi: 10.1111/j.1526-4610.2009.01438.x. Headache. 2009. PMID: 19545250
-
Longitudinal changes in the continuous glucose profile measured by the CGMS in healthy pregnant women and determination of cut-off values.
Siegmund T, Rad NT, Ritterath C, Siebert G, Henrich W, Buhling KJ. Siegmund T, et al. Eur J Obstet Gynecol Reprod Biol. 2008 Jul;139(1):46-52.
 doi: 10.1016/j.ejogrb.2007.12.006. Epub 2008 Feb 8. Eur J Obstet Gynecol Reprod Biol. 2008. PMID: 18262325
doi: 10.1016/j.ejogrb.2007.12.006. Epub 2008 Feb 8. Eur J Obstet Gynecol Reprod Biol. 2008. PMID: 18262325 -
Natural course and pathogenesis of transient focal neurologic symptoms during pregnancy.
Liberman A, Karussis D, Ben-Hur T, Abramsky O, Leker RR. Liberman A, et al. Arch Neurol. 2008 Feb;65(2):218-20. doi: 10.1001/archneurol.2007.50. Arch Neurol. 2008. PMID: 18268190
-
[Idiopathic oedema].
Courtnadge C, Madsen F, Bygum A. Courtnadge C, et al. Ugeskr Laeger. 2017 Nov 27;179(48):V06170450. Ugeskr Laeger. 2017. PMID: 29208198 Review. Danish.
-
Approach to the pregnant patient with headache.

Martin SR, Foley MR. Martin SR, et al. Clin Obstet Gynecol. 2005 Mar;48(1):2-11. doi: 10.1097/01.grf.0000153208.93620.39. Clin Obstet Gynecol. 2005. PMID: 15725852 Review. No abstract available.
See all similar articles
Publication types
MeSH terms
Cite
Format: AMA APA MLA NLM
Send To
Headache during pregnancy: Symptoms, treatments, and remedies
- Pregnancy
- Your Body
By Hallie Levine
|
|
November 29, 2021
A mild headache during pregnancy is normal, especially in the first trimester as your hormone levels fluctuate. Tension headaches are common, while some women might experience their first migraine during pregnancy. (On the flip side, many women find that pregnancy makes their migraines go away!) If you have a severe headache in the second or third trimester, call your healthcare provider right away, as it could be a sign of preeclampsia. Otherwise, exercising, changing your sleep habits, and taking acetaminophen (with your doctor's okay) are some safe ways to treat pregnancy headaches.
Tension headaches are common, while some women might experience their first migraine during pregnancy. (On the flip side, many women find that pregnancy makes their migraines go away!) If you have a severe headache in the second or third trimester, call your healthcare provider right away, as it could be a sign of preeclampsia. Otherwise, exercising, changing your sleep habits, and taking acetaminophen (with your doctor's okay) are some safe ways to treat pregnancy headaches.
Photo credit: iStock.com / damircudic
- What causes a headache during pregnancy?
- Common types of pregnancy headaches
- Is it common to get a migraine during pregnancy?
- What can I take for a headache while pregnant?
- Other ways to prevent or treat a headache during pregnancy
- When should I be worried about headaches during pregnancy?
What causes a headache during pregnancy?
Pregnancy headaches are a common experience, especially in the first trimester. You can blame your hormones: Some women are more sensitive to the increase in estrogen that occurs during pregnancy. You may also notice more headaches in early pregnancy thanks to an increase in blood volume during the first trimester, or if you're quitting or cutting back on caffeine – the withdrawal can make your head pound.
You can blame your hormones: Some women are more sensitive to the increase in estrogen that occurs during pregnancy. You may also notice more headaches in early pregnancy thanks to an increase in blood volume during the first trimester, or if you're quitting or cutting back on caffeine – the withdrawal can make your head pound.
Other possible causes of pregnancy headaches include:
- A lack of sleep or general fatigue
- Sinus congestion or a stuffy nose
- Allergies
- Eyestrain
- Stress
- Depression
- Hunger
- Dehydration
It's normal to get tension headaches when you're pregnant, especially in the first trimester. Migraine sufferers usually get some relief when they're expecting – although some women may actually end up getting their first migraine during pregnancy.
If you have headaches in your first trimester, you'll probably find that they decrease or even disappear completely during the second trimester, after the flood of hormones stabilizes and your body gets used to its altered chemistry.
Common types of pregnancy headaches
There are many different types of headaches you may experience while pregnant, and it isn't always easy to tell which kind you have. Here, a few key differences:
Tension headaches are one of the most common kinds of headaches during pregnancy, especially in the first trimester. They can feel like a squeezing pain or a steady dull ache on both sides of your head or at the back of your neck. If you've always been susceptible to tension headaches, pregnancy can make them worse.
Sinus headaches typically feel like pressure or pain in your cheeks, around your eyes, and in your forehead. They occur most often after you've had a cold or a respiratory infection. People commonly mistake migraine headaches for sinusitis – if you're getting more headaches but otherwise have been healthy, you might be having migraines. But if you're feeling congested, you might have a sinus infection requiring treatment.
Cluster headaches are much less common, and experts aren't sure if pregnancy affects the frequency or intensity of them. Cluster headaches are marked by sudden, severe pain usually around one eye or temple, sometimes with teary eyes or a stuffy nose. They tend to occur at the same time each day, often a few hours after falling asleep, over weeks or months.
Migraine headaches cause moderate to severe throbbing pain, typically on one side of the head. They can also be accompanied by other symptoms, such as nausea, vomiting, or sensitivity to light and noise. If untreated, they can last from four to 72 hours and may be aggravated by physical activity as well as many of the same factors that trigger more typical headaches. Migraines are most common in the first trimester, and tend to ease up in the second and third trimester, as your body adjusts to hormones.
Some migraine sufferers have a condition known as migraines with aura – that is, headaches that are preceded by symptoms that may include visual changes (such as bright flashing lights or blind spots), sensations of numbness or "pins and needles," weakness, and speech disturbances. These symptoms may start up to an hour before a migraine starts and may last as long as an hour.
These symptoms may start up to an hour before a migraine starts and may last as long as an hour.
Is it common to get a migraine during pregnancy?
The frequency of pregnancy migraines varies. Experts estimate that about 1 in 5 women will have a migraine at some point in their life, and studies have shown a small number of women experience their first migraine while pregnant, most often in the first trimester.
Some good news about migraines during pregnancy: In one study, about two-thirds of women who were prone to migraines noticed that their migraines actually improved when they were pregnant. (This is more likely to happen if your migraines tend to be worse around the time of your periods or start when you first begin menstruating.) Other women noticed no change or found that their migraines become more frequent and intense.
However, women who have migraines tend to have higher rates of preeclampsia, a serious high-risk pregnancy condition marked by high blood pressure – especially if they didn't get migraines before pregnancy – so it's important to let your healthcare provider know if you suddenly start having them.
What can I take for a headache while pregnant?
It's always best to talk to your healthcare provider before taking any medicines while you're pregnant, but when it comes to headache relief, acetaminophen (Tylenol) is considered the safest over-the-counter pain reliever to take during pregnancy, if used as directed. Don't exceed the recommended daily dose, and because acetaminophen may not be safe to take for prolonged periods, take it only as it's needed.
If your headaches aren't getting any better, your ob-gyn or midwife may be able to prescribe some other safe options, so talk to them.
If you're prone to severe migraines, ask your provider which medications you can take. One well-known class of migraine drugs, triptans, have been generally shown to be safe during pregnancy, but you may need to be monitored by a maternal-fetal medicine specialist (MFM) or a neurologist during your pregnancy if you're taking them.
Other ways to prevent or treat a headache during pregnancy
Here are some more ways to find pregnancy headache relief:
Figure out your headache triggers. Headache specialists often recommend keeping a headache diary to help you identify specific triggers. The next time you get a migraine or headache, write down everything you ate for the 24 hours prior and what you were doing when your headache started.
Headache specialists often recommend keeping a headache diary to help you identify specific triggers. The next time you get a migraine or headache, write down everything you ate for the 24 hours prior and what you were doing when your headache started.
Some common migraine triggers include foods that contain:
- Monosodium glutamate (MSG)
- Nitrites and nitrates (common in processed meats like hot dogs, salami, and bacon)
- Artificial sweeteners
Other foods that can trigger a headache include:
- Certain beans and nuts
- Aged cheeses and cultured dairy products (like buttermilk and sour cream)
- Some fresh fruits (including bananas, papayas, avocados, and citrus)
- Smoked fish
- Chocolate and carob
- Fermented or pickled foods (like soy sauce or sauerkraut)
Other triggers may include:
- Glaring or flickering lights
- Loud noises
- Excessive heat or cold
- Strong odors
- Fasting
- Tobacco smoke
Use a compress. You may be able to find relief if you apply a warm or cool compress to your forehead or the base of your skull.
You may be able to find relief if you apply a warm or cool compress to your forehead or the base of your skull.
Take a shower. For some migraine sufferers, a cold shower brings fast – if temporary – headache relief. If you can't take a shower, splash cool water on your face. A warm shower or bath can soothe tension headaches.
Don't go hungry or thirsty. To prevent low blood sugar (a common headache trigger), eat small meals frequently. When you're on the go, take along some healthy snacks, such as crackers, fruit, or yogurt. Stay away from straight sugar, like candy or soda, which can make your blood sugar spike and crash.
Don't forget to drink plenty of water and stay hydrated. Sip water slowly if you've recently vomited from a migraine.
Avoid fatigue. Get plenty of sleep at night. When you're having a migraine, it might be helpful to sleep in a quiet, dark room.
Exercise. Some evidence shows that regular exercise during pregnancy can reduce the frequency and severity of migraines and reduce the stress that can cause tension headaches. If you're prone to migraines, get started slowly – a sudden burst of activity could trigger one. (And don't exercise once a migraine has started because it will aggravate the headache.)
Some evidence shows that regular exercise during pregnancy can reduce the frequency and severity of migraines and reduce the stress that can cause tension headaches. If you're prone to migraines, get started slowly – a sudden burst of activity could trigger one. (And don't exercise once a migraine has started because it will aggravate the headache.)
Exercises to help you maintain good posture may be especially helpful with headaches during the third trimester.
Try relaxation techniques. Biofeedback, meditation, prenatal yoga, and self-hypnosis may be helpful for reducing stress and headaches in some sufferers.
Get a massage. Some women who suffer from tension headaches swear by massage, although it's unclear whether it's effective in preventing or relieving headaches. A full-body massage (ideally from a therapist who specializes in prenatal massage) can release tension in the muscles of your neck, shoulders, and back.
If a professional massage isn't an option, ask your partner to rub your back and head.
Consider acupuncture. Acupuncture treatment is generally considered safe during pregnancy, although whether it can provide pregnancy headache relief is a topic of debate. If you'd like to try it, ask your healthcare provider for a referral and keep them posted on your treatments. If you prefer to see an acupuncture practitioner who's also an M.D., check out the American Academy of Medical Acupuncture.
When should I be worried about headaches during pregnancy?
In the second or third trimester, a severe headache could be a sign of preeclampsia. Other symptoms of preeclampsia include an unusual amount of protein in the urine, vision changes, and liver and kidney abnormalities.
Call your healthcare provider right away if:
- You're in your second or third trimester and have a bad headache or a headache for the first time. It may or may not be accompanied by visual changes, sharp upper abdominal pain or nausea, or swelling in your hands or face.
 You'll need to have your blood pressure and urine checked right away to be sure you don't have preeclampsia.
You'll need to have your blood pressure and urine checked right away to be sure you don't have preeclampsia. - You have a headache (even a mild one) and you've been having high blood pressure.
- You have a sudden "explosive" headache. This type of headache is a violent pain that wakes you up, doesn't go away, or feels unlike anything you've ever experienced.
- Your headache is accompanied by a fever or a stiff neck.
- Your headache gets worse and you have other problems, such as blurry vision or other visual disturbances, slurred speech, drowsiness, numbness, or a change in sensation or alertness.
- You have a headache after any kind of head injury.
- You have nose congestion, as well as pain and pressure underneath your eyes or other face or tooth pain. (This could be a sinus infection that calls for antibiotics.)
- You notice any abnormal changes in vision, such as getting headaches after reading or looking at a computer screen.
In any case, don't hesitate to call your ob or midwife whenever you're worried about a headache during pregnancy. Even if you've had headaches before, talking to them can help you decide which treatment might be best for you while you're pregnant.
Even if you've had headaches before, talking to them can help you decide which treatment might be best for you while you're pregnant.
Read More:
Your first trimester pregnancy checklist
Pregnancy symptoms you should never ignore
Common pregnancy aches and pains
Sources
BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies.
American Academy of Otolaryngology-Head and Neck Surgery. Undated. Sinus headaches. http://www.entnet.org/content/sinus-headaches [Accessed October 2021]
American College of Obstetricians and Gynecologists. 2019. Chronic Hypertension in Pregnancy. Washington, D.C. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2019/01/chronic-hypertension-in-pregnancy [Accessed October 2021]
2019. Chronic Hypertension in Pregnancy. Washington, D.C. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2019/01/chronic-hypertension-in-pregnancy [Accessed October 2021]
American College of Obstetricians and Gynecologists. 2020. Preeclampsia and high blood pressure during pregnancy. https://www.acog.org/Patients/FAQs/Preeclampsia-and-High-Blood-Pressure-During-Pregnancy [Accessed October 2021]
American Migraine Foundation. Sinus headaches. https://americanmigrainefoundation.org/understanding-migraine/sinus-headaches/ [Accessed October 2021]
American Migraine Foundation. 2017. Migraine and pregnancy: How hormones affect head pain. https://americanmigrainefoundation.org/resource-library/migraine-pregnancy-hormones/ [Accessed October 2021]
Mayans, L. 2018. Acute Migraine Headache: Treatment Strategies. American Family Physician 83(3):271-280. https://www.aafp.org/afp/2018/0215/p243.html [Accessed October 2021]
Office on Women's Health. 2019. Migraine. https://www.womenshealth.gov/a-z-topics/migraine [Accessed October 2021]
2019. Migraine. https://www.womenshealth.gov/a-z-topics/migraine [Accessed October 2021]
UpToDate. 2020. Headache in pregnant and postpartum women. https://www.uptodate.com/contents/headache-in-pregnant-and-postpartum-women#H711083317 [Accessed October 2021]
American Heart Association. 2014. Cardiovascular Physiology of Pregnancy. https://www.ahajournals.org/doi/full/10.1161/circulationaha.114.009029 [Accessed November 2021]
Cleveland Clinic. 2019. Headaches and Food. https://my.clevelandclinic.org/health/articles/9648-headaches-and-food [Accessed November 2021]
Journal of Injury and Violence Research. 2012. Review of headache in pregnancy. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3571605/ [Accessed November 2021]
Clinical Obstetrics and Gynecology. 2012. Headache and Neurological Disease in Pregnancy. https://pubmed.ncbi.nlm.nih.gov/22828113/ [Accessed November 2021]
Show more
advertisement | page continues below
advertisement
Featured video
All pregnancy, parenting, and birth videos >
Headache during pregnancy: where does it come from and how to get rid of it
Share
0When to call an ambulance
Urgently dial 103 or 112 if you have Clinical guidelines for the diagnosis and treatment of tension headache the following symptoms:
- sudden and severe headache;
- consciousness Preeclampsia becomes confused or lost altogether;
- pain worsens over 5 minutes;
- flies, spots flash in the eyes;
- throbbing and noisy in the ears;
- speech has become slurred, words are drawn out;
- arms and legs weaken, convulsions set in;
- severe neck stiffness Meningitis, chin cannot reach chest;
- fever ALGORITHMS for providing emergency medical care outside a medical organization 39°C and above;
- increased heart rate at rest;
- severe shortness of breath;
- the child pushes without stopping or suddenly stops;
- leaking High blood pressure and pregnancy: Know the facts of water or blood;
- lower abdomen hurts, as if contractions had begun.

Why pregnant women can get headaches
Pregnancy headaches are not always life threatening. But the doctor needs to be told about it in any case. If the symptom appeared for the first time and does not hurt much, postpone the conversation until a scheduled visit. If your headache is recurring or gets worse, it's best to make an appointment as soon as possible. The gynecologist will decide what needs to be done or refer you to another doctor.
There are many causes of headaches. Scientists have found Characteristics and diagnoses of acute headache in pregnant women — a retrospective cross‑sectional study that in pregnant women in 57% of cases it is primary, that is, not associated with other diseases. The most common are migraines and tension headaches.
Everything else is a secondary headache caused by various pathologies. Usually it is high blood pressure and infections. But there are also more dangerous reasons.
1. Stress and fatigue
A pregnant woman's body experiences increased stress, because it has to work for two. If at the same time the expectant mother is exposed to stress, strong feelings or sleeps little, she gets Clinical guidelines for the diagnosis and treatment of tension headache tension headache.
If at the same time the expectant mother is exposed to stress, strong feelings or sleeps little, she gets Clinical guidelines for the diagnosis and treatment of tension headache tension headache.
Discomfort lasts from 30 minutes to several days. The head hurts in the forehead, occiput, both temples. But there is no feeling that they put on a tight hoop or helmet. The pain does not get worse when bending over, walking, or climbing stairs, bright lights, or sounds.
What to do
Tension headache can go away on its own: enough Clinical practice guidelines for the diagnosis and treatment of tension headache get some fresh air or sleep. Sometimes pleasant emotions help, which distract from experiences.
If the pain persists for 2-3 consecutive days, see a doctor. He will select painkillers that are safe for the child.
2. Taking Medications
Any medicine that enters the stomach or bloodstream can cause headaches even if the dosage is correct. In pregnant women, this often occurs due to drugs for high blood pressure, heart disease, antibiotics, anticonvulsants.
In pregnant women, this often occurs due to drugs for high blood pressure, heart disease, antibiotics, anticonvulsants.
Long-term use of non-steroidal anti-inflammatory drugs for headaches may cause Clinical guidelines for the diagnosis and treatment of tension-type headache the opposite effect: the pills do not remove, but provoke symptoms.
What to do
If your head hurts a few hours after taking the medicine, you need to see a doctor to change the medicine. Do not drink non-steroidal anti-inflammatory drugs for more than 3-5 days. If they do not help, you need to tell the doctor about it.
3. Love or avoidance of coffee
Headache during pregnancy can be caused by coffee Drug-induced headache: a management strategy. Unpleasant symptoms occur if you drink more than 3-4 cups a day.
Abrupt refusal of coffee is also harmful. It is worth finding out about pregnancy and stop brewing a fragrant drink, and after 1-2 days Caffeine‑withdrawal headache will appear in the temples and the back of the head. The Vågå study of headache epidemiology aching pain.
The Vågå study of headache epidemiology aching pain.
What to do
Coffee is better Caffeine and adaptive changes in the circulatory system during pregnancy refuse during pregnancy. If a headache occurs a day after this, you can drink a small cup of the drink and wait a day again. Gradually, the dependence on coffee will pass.
Coffee drinkers can Caffeine reduce their drink intake to 1-2 cups per day.
4. Infection with fever
Acute viral (usually ARVI) or bacterial (eg, streptococcal tonsillitis) infections cause fever and headache. This is a normal reaction to foreign microorganisms.
But any infection is dangerous for pregnant women The role of infection in miscarriage. It can cause fetal defects, growth retardation and even miscarriage. And with meningitis, especially listeriosis, there is a threat to the life of the mother.
What to do
If you have a headache with fever, call your doctor. He will prescribe safe medications or give you a referral to the hospital if a serious infection is suspected. In this case, Meningitis needs strong antibiotics, drips to maintain the body and sometimes hormones.
In this case, Meningitis needs strong antibiotics, drips to maintain the body and sometimes hormones.
5. Preeclampsia and preeclampsia
After 20 weeks, preeclampsia may develop in pregnant women. This disease is GESTOSIS: THEORY AND PRACTICE, in which one of three symptoms or a combination of them may appear: high blood pressure, edema and protein in the urine.
Without proper treatment, preeclampsia progresses to preeclampsia Preeclampsia. The pressure rises sharply, the head and lower abdomen hurt unbearably, the baby pushes unusually hard or, on the contrary, suddenly subsides Placental abruption. Preeclampsia can lead to placental abruption, damage to the liver and other organs, bleeding, and even seizures. Without urgent medical care, the fetus and mother die.
What to do
When the first signs of preeclampsia appear, the pregnant woman is hospitalized to find treatment. After that, she is discharged home under the supervision of her gynecologist.
But if her health worsens, the doctor again sends the woman to the Preeclampsia hospital, where she is prescribed drugs to reduce pressure, special drips to keep her body functioning. If improvement does not occur within a day, a caesarean section is performed.
6. Migraine
One of the causes of migraine Migraine is a change in estrogen levels. But the disease very rarely appears due to pregnancy. On the contrary, in 70% of women the symptoms subside dramatically Migraine and pregnancy: a particular example of the course of the disease after conception. And yet migraine torments Migraine many.
It may begin with an aura: flashes of light, spots before the eyes, tingling in the hands or numbness of half of the face, sometimes tinnitus. Each symptom can last from 20 minutes to an hour.
A migraine attack develops after the aura. In this case, one side of the head hurts and throbs, nausea or vomiting appears. A woman is irritated by bright lights, loud noises, smells. They make the pain worse.
They make the pain worse.
Seizures last from a few hours to a week or more. After a migraine, there is a feeling of severe fatigue, exhaustion, and an awkward turn of the head can return the pain.
What to do
Any medication for migraine during pregnancy must be prescribed by a doctor. In some cases drugs are used Headache in Pregnancy and the Puerperium from the group of beta-blockers.
Studies have shown Migraine and pregnancy: a particular example of the course of the disease, that often migraine in pregnant women is associated with a lack of magnesium. The doctor will help you choose the appropriate type of vitamin and mineral complex and its dosage.
7. Cerebrovascular disease
Hormone problems in some pregnant women increase blood clotting, which increases the risk of Headache and pregnancy: a systematic review of thrombosis, stroke, or meningeal hemorrhage. These conditions are very dangerous: a woman can die within a few minutes or remain disabled.
Vascular involvement is always accompanied by several symptoms:
- severe headache on one side;
- nausea and vomiting;
- blurred vision;
- loss of consciousness;
- convulsions.
What to do
Urgently call an ambulance. The pregnant woman must be laid or seated so that she does not hit when she falls. You can't give medicine! You can only open the window so that there is more air in the room.
What treatment will prescribe Headache and pregnancy: a systematic review by a physician, depends on the specific disease. These can be drugs that reduce blood clotting and dissolve blood clots. In some cases, urgent surgery is needed.
8. Brain Tumors
Studies show that progesterone and estrogen during pregnancy may cause or accelerate the growth of neoplasms in the brain. Symptoms of the disease appear slowly, over several months, and depend on the size and location of the tumor.
Headache may gradually increase Brain tumor, then vision, speech, hearing deteriorate, limbs become numb and convulsions appear. Sometimes it is difficult for a woman to keep her balance.
Sometimes it is difficult for a woman to keep her balance.
What to do
If a pregnant woman often has a headache or she forgets what she wanted to buy in the store and how to cook her favorite borscht, confuses her way home, you need to go to a neurologist. First, he will prescribe standard treatment, simple and safe medicines, rest, good sleep.
If this does not help, the symptoms do not disappear or worsen, a deep examination is needed Brain tumor. The pregnant woman will be sent for an MRI of the brain. This procedure is safe for the fetus. If the diagnosis is confirmed, surgery may be required.
What to do if the doctor cannot find the cause of the pain
If you have been examined and the doctor cannot tell you why your head hurts and diagnoses you with vascular dystonia, this is a reason to be wary. There is no such disease.
Seek another doctor. Perhaps he uses new diagnostic methods that will help to deal with the problem and choose a treatment.
How to avoid headaches during pregnancy
Specialists recommend What can I do about headaches during pregnancy? I'd rather not take medication. next:
- Avoid triggers. For example, if you notice that certain foods, smells, or situations cause headaches, try not to encounter them.
- Protect yourself from stress, do not worry about trifles.
- Move more. During pregnancy, walk every day in the fresh air and do special exercises for expectant mothers.
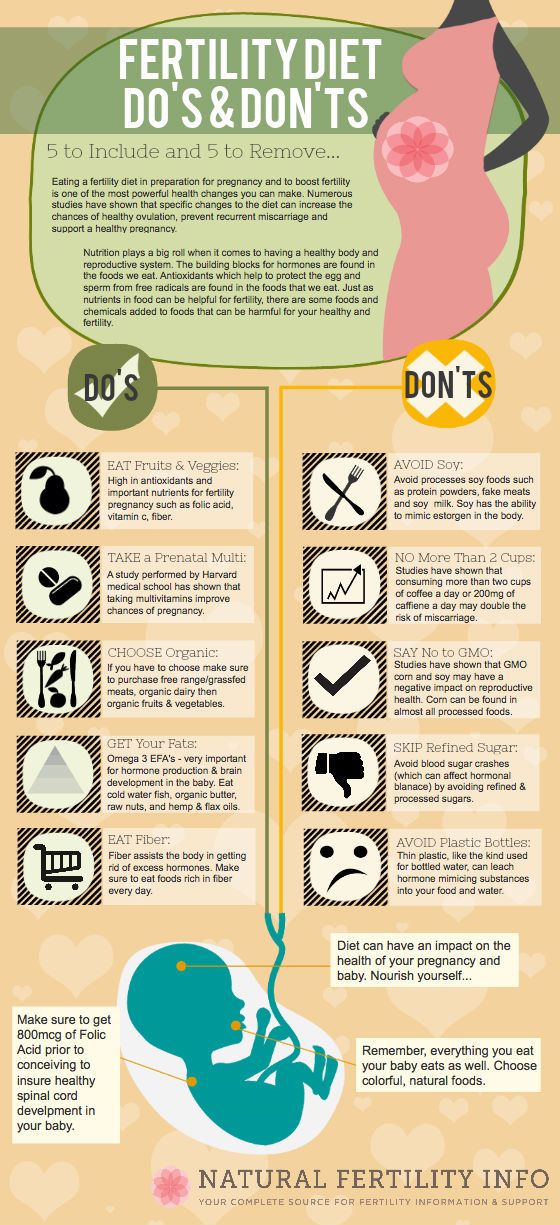
- Correct Pregnancy nutrition: Healthy‑eating basics to eat. Try to eat a lot of vegetables and fruits, dairy products, drink at least 2.4 liters of liquid. Every day, the menu should include fish, poultry or lean meat. And it is better not to buy sweet, fast food and other junk food.
- Observe Working during pregnancy: Do’s and don’ts daily routine. You need to sleep at least 8 hours a day and go to bed no later than 22-23 hours in order for melatonin to be produced normally.

- Learn to relax. Learn simple meditation techniques or breathing exercises.
Read also 🧐
- How pregnancy develops by week
- How to calculate the gestational age
- What rights does a pregnant woman have at work
- 7 best sex positions for pregnant women
- How to recognize a missed pregnancy and what to do next
Headache during pregnancy and breastfeeding
Headache during pregnancy is quite common and is usually not a health hazard.
Noise, stress, fatigue, too little outdoor activity, lack of sleep, as well as too much sleep (especially in the second half of pregnancy), insufficient fluid intake and poor nutrition are the main culprits of pregnancy headaches. Pain that occurs in early pregnancy can be associated with hormonal changes. An increase in the synthesis of estrogen and progesterone, necessary for the development of the child, causes water retention in the tissues. Edema occurs, including in the brain tissues, where nerve receptors react with pain to an increase in pressure. Fortunately, this is not dangerous for the mother and fetus.
Edema occurs, including in the brain tissues, where nerve receptors react with pain to an increase in pressure. Fortunately, this is not dangerous for the mother and fetus.
TREATMENT OF HEADACHE DURING PREGNANCY AND BREASTFEEDING AVAILABLE IN BRANCHES:
Treatment of headache during pregnancy and breastfeeding in the Primorsky district
Address: St. Petersburg , Primorsky district, st. Repishcheva, 13
Treatment of headaches during pregnancy and breastfeeding in the Petrogradsky district
Address: St. Petersburg , Petrogradsky district, st. Lenina, 5
Headache treatment during pregnancy and breastfeeding in Vsevolozhsk
Address: Vsevolozhsk , Oktyabrsky Ave, 96
Prevention of head pain during pregnancy
First of all, you need to relax. In fact, there are more important things than the mood of the boss, the colors of the wallpaper in the room, or the order in the closet. Every day you should provide yourself with 8-10 hours of sleep. It is necessary to remember about walks and regular meals, because hunger is manifested not only by sensations in the stomach, but also by a headache. Your diet should include sources of magnesium (buckwheat, flour, pumpkin seeds, cocoa, bananas), as a deficiency in this element often causes tension headaches. Such dull and not very severe pains can persist for a week.
Every day you should provide yourself with 8-10 hours of sleep. It is necessary to remember about walks and regular meals, because hunger is manifested not only by sensations in the stomach, but also by a headache. Your diet should include sources of magnesium (buckwheat, flour, pumpkin seeds, cocoa, bananas), as a deficiency in this element often causes tension headaches. Such dull and not very severe pains can persist for a week.
Even slight dehydration causes similar problems, so don't forget to drink. It is worth remembering that not all drinks are equally good during pregnancy. Coffee, tea, or thick juices can cause fluid to be lost from the body or prevent it from being absorbed. The best is pure non-carbonated water with a low mineral content (up to 500 mg elements per liter), which will not overload the kidneys, which carry a double load during pregnancy.
It is necessary to remember about a comfortable bed, because the spine can also be the cause of the headache. The mattress should not be too hard, because on a hard base your bones and muscles are constantly in tension and do not rest, and not too soft, since in this case the load on the spine will be uneven.
The mattress should not be too hard, because on a hard base your bones and muscles are constantly in tension and do not rest, and not too soft, since in this case the load on the spine will be uneven.
Headache during pregnancy: when to see a doctor?
Headache may be a symptom of hypertension, which may signal serious toxicosis. With such headaches (appear, as a rule, in the morning in the occipital region and sometimes may be accompanied by ringing or noise in the ears and overexcitation), pressure should be measured regularly during pregnancy. If the norm is exceeded, you should consult a doctor.
Breastfeeding headache
The occurrence of headache during lactation and breastfeeding is often associated with chronic lack of sleep and fatigue of new mothers. It can be tension headaches and migraine pains. With the organization of your day and frequent rest, such pains go away on their own.
However, for more serious causes (hypertension, head injuries, infectious diseases), you should see a doctor who can examine you for other conditions such as intercostal neuralgia or sciatica.
Treatment of headache during pregnancy and breastfeeding
The intake and dosage of pain medication should be discussed with the attending gynecologist. Due to the fact that many painkillers (including analgin and aspirin) have an effect that is harmful to the unborn child (teratogenic effect), restrictions on the use of medicines are introduced during pregnancy. These restrictions remain for headaches and for the period of breastfeeding for the reason described above, since all medications pass into milk.
Paracetamol-based drugs are one of the recommended mild pain relievers.
However, we also emphasize that before treating a headache, it is necessary to identify its cause so that the headache does not turn out to be a symptom of a tumor in the brain.
In our multidisciplinary clinic, you can undergo an examination and consult with competent doctors.
Reception by doctors:
Select branch"Dynasty" on Novocherkassky prospect, Krasnogvardeisky district"Dynasty" on Lenina, Petrogradsky district"Dynasty" on Repishcheva, Primorsky district"Dynasty" in VsevolozhskVisiting service
Child specialists
Online counseling
Volkonina Tatyana Evgenievna
Neurologist, pediatric neurologist
Gurbo Anna Gennadievna
Neurologist
Eroshina Ekaterina Sergeevna
Neurologist, epileptologist, cephalgologist, somnologist, acupuncturist, candidate of medical sciences, highest category, head of the neurological department
Irishina Yulia Anatolyevna
Neurologist, cephalgologist, parkinsonologist, candidate of medical sciences, highest category
Kolyada Alexander Alexandrovich
Neurologist, epileptologist, candidate of medical sciences, highest category
Krasnoperova Alina Viktorovna
Neurologist, cephalgologist, chiropractor
Loginova Anna Sergeevna
Neurologist, first category
Mariekha Elena Vladimirovna
Neurologist
Ponedelko Tatyana Sergeevna
Neurologist, vertebrologist, acupuncturist, first category
Ten Maya Viktorovna
Neurologist, cephalologist, doctor of functional diagnostics
Zinzerling Natalya Vsevolodovna
Neurologist, cephalologist, candidate of medical sciences
Cost of headache treatment during pregnancy and breastfeeding:
| Name of services | Price in rubles | |
St.:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg) Petersburg Petersburg | Vsevolozhsk | |
| Initial appointment with a neurologist 1st stage | 2100 | 1700 |
| Second stage neurologist appointment | 1900 | 1500 |
| Primary appointment with a neurologist 2nd level | 2300 | 1900 |
| Repeated appointment with a neurologist 2nd stage | 2100 | 1700 |
| Primary appointment with a neurologist Kolyad A.A. | 3200 | - |
| Repeated appointment with a neurologist Kolyad A.A. | 2900 | - |
| Primary appointment with a neurologist Yeroshina E.S./Irishina Yu.A./Tsinzerling N.V. | 4000 | 4000 |
| Repeated appointment with a neurologist Yeroshina E.S./Irishina Yu.A./Tsinzerling N.V. | 3500 | 3500 |
Primary appointment with the neurosurgeon Kholyavin A. | ||