My newborn has a rash
Common childhood rashes | Pregnancy Birth and Baby
Most children experience a rash at one time or another, and many disappear without treatment. Others may be accompanied by fever, itchiness and other symptoms. Here is a guide to some common rashes in kids.
Meningitis rash
If you think your child might have meningitis rash, go to the nearest emergency department immediately. You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to half of newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get acne on their cheeks and nose in the first few months of life. These pimples normally clear up without any treatment, usually in a few months, but sometimes it can take a year.
Nappy rash
Nappy rash is an inflammation of the skin in the nappy area that looks red, sore and inflamed. Nappy rash is caused by a number of things, including urine or poo irritating the baby’s skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby’s skin has developed a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme
Erythema multiforme is a rash triggered by an infection, medication or an illness. Red spots develop on the hands or feet before spreading across both sides of the body (over a day or so). The spots are not usually itchy, but might become raised or blistered.
Your baby might feel unwell or have a mild fever before the rash appears. Erythema multiforme is not contagious, and usually clears up without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up.
Rashes that might be itchy
Eczema
Eczema causes the skin to become itchy, red, dry and cracked, especially in the creases at the knees and elbows. It is usually treated with corticosteroid creams to reduce inflammation, and moisturisers to stop the skin from drying out.
Eczema is a long-term condition that can show up when babies are only a few months old. Certain triggers, such as viral infections, soap and pool chlorine, can cause symptoms to appear.
Ringworm (tinea)
Ringworm is a contagious, mild skin infection that causes a ring-like red rash with a clear centre. It can occur almost anywhere on the body, although the most common areas are the baby’s scalp, feet and groin.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to counteract heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, for whom it is not usually serious, but it can be dangerous for newborn babies. It is common in children who have scabies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. You should keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.
Hives (urticaria)
Hives is a raised, red, itchy rash that can appear on any part of the body at any time, but is common on the chest, stomach and back, as well as the throat and limbs. Hives usually disappears within a few days without any treatment. Your pharmacist can advise you about over-the-counter medications to treat hives.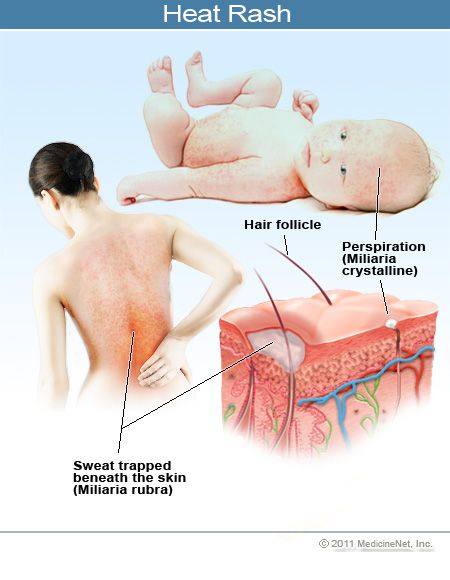 If the rash doesn't go away, you should see your doctor.
If the rash doesn't go away, you should see your doctor.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It usually affects only children over 10.
It begins with a single pink or tan patch on the chest or back. Oval red patches then appear on the chest or back and limbs over the next weeks. They might be itchy, and your child might feel tired and unwell.
The exact cause of pityriasis rosea is unclear, and experts believe it is probably not contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and come into contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. Usually they heal without treatment within 6 months, but it might take longer.
They can be itchy. Usually they heal without treatment within 6 months, but it might take longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
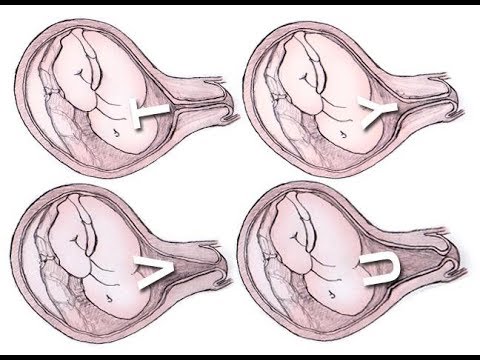
The virus can affect a pregnant woman, potentially causing a type of anaemia in her unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with women who are, or might be, pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness that causes a rash on the palms of the hands and soles of the feet. It is not the same as the foot-and-mouth disease that affects farm animals.
It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth, and also in the nappy area, that last 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without major problems but in rare cases it can be more serious especially in people whose immune system is not functioning normally or pregnant women. These rare problems include infections of the brain and heart muscle and miscarriage in pregnant women.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. Kids with roseola infantum have raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
The rash usually lasts 3 to 5 days.
The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion. If your child has a convulsion (fit), call triple zero (000) immediately and ask for an ambulance. Febrile convulsions are scary to see but are generally not harmful.
When to seek help
Many babies develop a skin rash in their first days or weeks as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own. But if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from women who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You should also keep them away from women who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Learn more here about the development and quality assurance of healthdirect content.
Newborn Rashes and Skin Conditions
Written by Steven Jerome Parker, MD
Reviewed by Dan Brennan, MD on July 23, 2021
In this Article
- Common Rashes in Newborns
- Common Rashes in the First Few Months of a Baby's Life
- Tips for Concerned Parents
- When to Worry About Baby's Rash
A newborn's skin is prone to rashes of all sorts.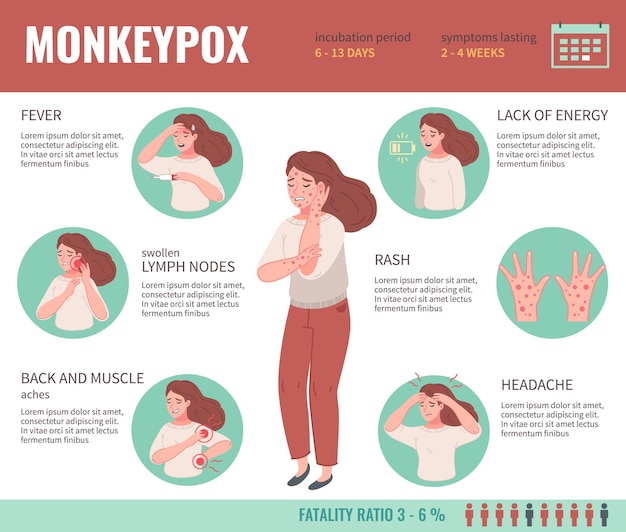 Fortunately, most of these rashes are harmless and go away on their own.
Fortunately, most of these rashes are harmless and go away on their own.
Common Rashes in Newborns
- Pink pimples ('neonatal acne') are sometimes thought to be caused by exposure in the womb to maternal hormones. No treatment is needed, just time. They can last for weeks or even months on a baby's skin.
- Erythema toxicum is another common newborn rash. It looks like red blotches with ill-defined borders that are slightly raised, and may have a small white or yellow dot in the center. Its cause is unknown, and it resolves without treatment after a few days or weeks.
- Dry, peeling skincan be seen in almost all normal babies, but is especially noticeable in babies born a little late. The underlying skin is perfectly normal, soft, and moist.
- Little white bumps on the nose and face (milia) are caused by blocked oil glands. When a baby's oil glands enlarge and open up in a few days or weeks, the white bumps disappear.

- Salmon patches (called a ''stork bite'' at the back of the neck or an ''angel's kiss'' between the eyes) are simple nests of blood vessels (probably caused by maternal hormones) that fade on their own after a few weeks or months. Occasionally, stork bites never go away.
- Jaundiceis a yellow coloration on baby's skin and eyes. It is caused by an excess of bilirubin (a breakdown product of red blood cells). If the bilirubin level becomes sufficiently high, blue or white lights may be focused on the baby's skin to lower the level, because excess bilirubin can sometimes pose a health hazard.
- Congenital Melanocytosis, previously called Mongolian spots, are very common in any part of the body of dark-skinned babies. They are flat, gray-blue in color (almost looking like a bruise), and can be small or large. They are caused by some pigment that didn't make it to the top layer when baby's skin was being formed. They are harmless and usually fade away by school age.
New rashes may appear in babies after a few days, weeks, or even months.
Common Rashes in the First Few Months of a Baby's Life
- Cradle cap(seborrhea) often shows up at 1-2 months of age. Greasy, yellowish crusts appear on the scalp and may include a red, irritating rash on the face, behind the ears, on the neck, and even in the armpits. Your doctor will tell you how to best treat this common condition, depending on your baby's symptoms.
- Eczemais red, itchy patches on the skin, often seen on the baby's chest, arms, legs, face, elbows, and behind the knees. It is caused by dry, sensitive skin, and sometimes allergies (although it can be difficult at this age to know what the trigger might be). Your doctor can determine if the rash looks like eczema and prescribe the appropriate treatment. In general, treatment consists of:
- Using a very gentle soap
- Using a gentle detergent and no fabric softener in baby's laundry
- Using skin moisturizers
- Applying a steroid cream (like hydrocortisone or even a stronger one) if the eczema won't go away
- Prickly heat looks like small red bumps, mostly on areas of your baby's body that tend to overheat and sweat, like the neck, diaper area, and armpits.
 The treatment is to try to keep the area dry and avoid overheating by dressing them in loose-fitting clothing.
The treatment is to try to keep the area dry and avoid overheating by dressing them in loose-fitting clothing. - A fungal infection(candidiasis) can show up in different ways on your baby. On the tongue, it is called thrush and looks like dried milk, which, unlike milk, cannot be scraped off. In the diaper area, candidiasis looks like an intense red rash, often with smaller bumps around the edges. A fungal infection loves moist, dark areas, so you'll find redness due to it in the creases of the thighs. Candidiasis is treated with antifungal oral gel or liquid medicine (for oral thrush) or antifungal cream (for the diaper area), or both.
Tips for Concerned Parents
In the first few months of a baby's life, any rash associated with other symptoms (such as fever, poor feeding, lethargy, or cough) needs to be evaluated by a doctor as soon as possible.
When to Worry About Baby's Rash
While most rashes are not serious, a few need very close attention:
- Fluid-filled blisters (especially ones with opaque, yellowish fluid) can indicate a serious infection, like a bacterial infection or herpes.
- Small red or purplish dots over the body (''petechiae'') can be caused by a viral infection or a potentially very serious bacterial infection. These will not lighten with pressure. Any infant with possible petechiae should be evaluated by a doctor immediately.
Skin rash in a child causes and diagnostic rules
From the condition of the skin, you can determine whether the function of the body is impaired. The rash varies in small red, intermittent, patchy, colorless, watery, vacant, itchy, knots and nodules. Children's rashes are much more common than adults. Basically, this is due to the influence of external factors (sunlight, temperature, humidity, harmful substances, chemicals, etc.) on the skin. The skin is also affected by the body's process and disease.
If you have a baby rash, you should consult a pediatric dermatologist. The First Children's Medical Center provides competent pediatric dermatologist services in Saratov. Here you can not only get your doctor's advice, but also take all the necessary tests and hear the opinions of related experts. By contacting a doctor in a timely manner, you can find the cause of the rash, remove it and eliminate the risk of recurrence and complications.
Causes of rashes
The reason for this is physiological, which is accompanied by a natural reaction to the body's process. In addition, the background may have a pathological cause.
- Disability and parasites.
- Chemicals, harmful substances
- Metabolism; toxic substances, toxic substances, chemicals, toxic substances, toxic substances, etc.
- Specific vitamins: toxic substances, chemicals, toxic substances, toxic substances and other substances.
- Antibacterial agent; poison; poison; poison; poison;
- Gastrointestinal and renal functional disorders.
- External factors, internal factors
So we can conclude that baby rashes don't come out without a reason.
From a parent's point of view, every breakthrough looks almost the same. However, it can distinguish the first primary rash, and not the primary rash or near the primary rash can be distinguished over time.
Types of rashes
Various childhood diseases appear as a combination of primary and secondary symptoms. The primary rash is different. It is important for parents to respond quickly and confirm the formation formed in the child's body.
- The bumpy details of these rashes are all deep in the dermis, in other words, the rash is not a surface. There is no cavity, it looks a bit like tuberculosis, and the color of the skin may change to red or purple.
- Blister (blister). Therefore, people name most of the things that can be done on the skin. However, the blisters are actually pink rounded shapes and there are no cavities or contents. True blisters are short, last for a few minutes to a few hours, and then disappear without a trace. For example, there is a burning.
- Water blister rash. This rash is also called nodularity because the appearance is similar to nodules with different skin colors and undertones. Papules are superficial and deep, and papules may disappear without a trace.
- Water blister rash. This rash looks like a blister on the skin. In some cases, a colorless or bloody serum may be hidden. COSS integrate alone or merge to form many rooms. Open blisters are the same size as the bottom of the blisters and leave skin on skin.
- Pompholygous (with two sexes). This type of rash also appears in the form of a whistle, but it is characterized by a more impressive size, 5 mm or more in diameter, compared to a small whistle. Such blisters may contain mucus or serum content as small whirlpools.
- Tonu pustules are eruptions of abscesses. From superficial to deep skin. The opening of superficial pustules passes without a trace. Opened medium-deep pustules (boils, carbuncles) can cause severe scarring and scarring.
- Rash on the body. This type of rash does not appear on the surface of the skin, but is characterized by a change in the shade of some parts of the body. Such rashes are vascular or petrifying.
- Roseola is the name given to a rash that occurs in many infectious conditions.
All elements of a pink or moderately reduced rash. The structure of roseola resembles spots. When stretched or pressed on the skin, the rash turns pale and disappears for a while.
- hemorrhagic rash. This type of rash appears as red blood that forms at the sites of ruptured blood vessels. Stretching the skin does not stop the bleeding.
The appearance of the secondary rash is also different. Represents a bench, with the transformation of elements of the primary rash (usually blisters or pustules) into crusts after opening. Growth is often seen as secondary symptoms such as fissures, erosions, abrasions of epithelial cells, abrasions, scars and ulcers.
Where a skin rash can appear
A small, red rash is a type of rash that is more common in children of all ages, especially in early childhood, kindergarten, and high school.
On the hairline, face, armpits, shoulders, abdomen, back, buttocks, groin and groin, small, non-dominant rashes can be seen. Such rashes are caused by allergies (food, drug, cosmetic). It can also be the result of overheating or non-compliance with sanitary rules. This leads to chafing and knocking. In one-year-olds, the rash may cover the head as the skin regulates body temperature.
Such rashes are caused by allergies (food, drug, cosmetic). It can also be the result of overheating or non-compliance with sanitary rules. This leads to chafing and knocking. In one-year-olds, the rash may cover the head as the skin regulates body temperature.
The skin on the face may be covered with red rashes in some viral diseases. A child may develop a rash on his face if he does not receive suspicious new foods or medicines and does not change his lifestyle. In this case, it is necessary to take a temperature measurement and contact a pediatrician.
Red rashes of various sizes and types may appear on the hands and feet of children due to viral or bacterial infections, red fever, measles or leukemia.
Colorless rashes become more visible over time and are much more difficult to detect. Often these types of rashes indicate the early stages of allergy development. An almost invisible rash that is colorless or very pale may cover the body and be rough to the touch. It resembles a gooseberry, runs over the skin during chills and chills. Eruptions occur close to each other and can be huge.
It resembles a gooseberry, runs over the skin during chills and chills. Eruptions occur close to each other and can be huge.
A watery rash is a clear sign of infections, allergies, insect bites, and sunburn.
These areas may develop blisters filled with fluid.
- On the face (orbital triangle, lips, nose).
- For ribs, limbs, genitals, groin, inner waist, etc.
- near the anus.
In this case, the development of an infection originating from blisters or herpes is suspected. In much the same way, allergic reactions to the use of skin care products, in contact with chemicals and toxins, have caused local reactions resembling chemical burns.
Due to prolonged exposure to the sun, foamy rashes on the skin can turn red, causing the skin to turn red and slightly swollen.
When blisters appear on the skin of the hands and feet, "dyshidrosis" is possible, which is a blockage of the sweat glands. Blisters on the palms and heels are caused by the development of a fungal disease.
Purulent rash
Purulent rash is characteristic of bacterial infections. Such diseases most often develop under the influence of Staphylococcus aureus. It may also be due to the impact on the body of epidermal staphylococcus aureus, streptococcus and other microorganisms.
Such rashes can appear microscopically on the skin, wounds, wounds, which facilitates the penetration of internal microorganisms. Also, if the rash initially itches and itches and the baby begins to comb it, it becomes infected with bacteria and pustules appear.
Pustules on the knees and elbows in childhood can occur as a result of frequent falls and frequent skin injuries. The formation of a deep abscess is called a pyometra.
What parents need to do
To assess this condition, the parent should examine the child's skin and remove clothing. It is necessary to determine the nature of the rash (vesicles, opacities, papules, etc.) and the area. It is necessary to remember and analyze the state before the rash appears.
You will then have your temperature taken, your neck and tonsils examined, and other signs checked. You need to decide whether to call a doctor at home or visit a medical facility yourself.
What not to do when a rash appears
- Compression of pustules.
- Comb the rash.
- Self processing -.
- opening blister
- Since the application on fair skin complicates the diagnostic measures.
Do not forget that there are infectious diseases with rashes. In this regard, you should refrain from visiting the clinic with your child, as you can infect someone else in the hope that your turn will come. In such cases, it is recommended to call a doctor at home.
Diagnosis of the disease
Before treating a rash, it is important to find out the real cause of the rash. The choice of treatment depends on what caused the rash.
This is a diagnosis.
- are removed from the skin.
- Accumulation of fluid contained in vesicles and pustules.

- Get blood, stool and urine tests.
If necessary, you can visit a specialist nearby, such as a pediatrician, allergist, infectious disease specialist or gastroenterologist.
The treatment of rashes does not consist only of local treatment. To fix the problem, complex treatment is usually required. The main goal is to change the baby's habitat, revise the menu, take medicine.
Pediatric Dermatology Treatment
If a rash develops on a child's skin, it is important not to treat it alone, as treatment may worsen symptoms. If you have modulated your child's skin, you need to ask your child's dermatologist for help.
The pediatrician at the pediatric medical center will be diagnosed with the latest research methods. As a result of the test, if it is found that the skin disease is a symptom of other diseases, dermatologists consult, treat and treat them with the help of relevant specialists (digestive, allergic department, endocrinology, gynecology, surgery, etc. ). request.
). request.
Reservations for pediatric dermatologists in Saratov are accepted from 8.00 to 20.00 at the first DMC by calling (8452) 244-000. Reception will be made in advance.
Food allergy is called a pathological reaction of the body to food ingredients. In this article, pediatrician Olga Nikolaevna Trekteteva explains in detail the symptoms of an allergy to a newborn and treatment.
Children's food allergies are said to be around 10%. This is quite a large percentage, and the increase was recently increased. It is not unusual for a mother who complains of her child's food allergy symptoms to see pediatrics. In order to effectively treat children's food allergies, doctors must not only prescribe medications, but also explain the rules of child care and explain the subtle differences in food therapy.
The genetic background is important in the onset of an allergy. Therefore, if moms and dads have an allergic reaction, children can also cause higher food intolerances.
Types of food allergies in infants
Food allergies are roughly divided into two types: a reaction that occurs immediately after ingestion and an accumulated allergy. To cause an allergic reaction, allergens must be repeated into the body. Allergies are divided into types of skin symptoms, food, breath, etc., depending on the most damaged organ system.
Food allergy symptoms in infants
1. Food allergy symptoms are varied. The most common symptoms are a rash. Immediately after the allergen invades the body, hives can occur, which is an acute allergic reaction. A bright red swelling appears on the baby's skin with different sizes and shapes. Clear bubbles may appear in the center of the spot. The size varies from a few millimeters to several centimeters. This rash usually occurs within 1-3 days. But showing the child to the teacher is still worth it. Sometimes kids need to be prescribed medication so they get more immediate help in major rashes and places of failure. It is necessary to remember which product caused such a reaction and no longer gives.
It is necessary to remember which product caused such a reaction and no longer gives.
2. Other types of rash are not as severe. Therefore, it may not be possible to clearly define the relationship between exterior and product. Such a battle is usually not bright, small. It tends to be a wave current. The rash usually becomes bright in the evening and becomes thinner in the morning. The skin is dry, peeled, and sometimes cracked. It can often be done on the cheek, buttocks, outer waist, and arms. This type of rash requires special medical expert precautions and special treatments.
The most common symptoms are digestive symptoms. Swelling of the oral mucosa, swelling of the esophagus, single or frequent vomiting. In many cases, these symptoms strongly appear immediately after the use of allergens. In addition, children may suffer from abdominal pain. Sometimes you become sullen, get up or twist your legs. Food allergies can appear when the stool becomes loose. Both diarrhea and constipation can occur. Significant signs of a food allergy include large amounts of backflow, slight weight gain, anorexia, and weakness. Gastrointestinal symptoms may not be accompanied by a rash.
Significant signs of a food allergy include large amounts of backflow, slight weight gain, anorexia, and weakness. Gastrointestinal symptoms may not be accompanied by a rash.
4 Respiratory symptoms may appear in infancy, although the incidence is low. When food enters the mucous membrane, swelling of the upper respiratory tract can occur. It is an acute, life-threatening illness. You need to consult a doctor immediately. If you are exposed to allergens for a long time, you may develop allergic rhinitis or asthma. In many cases, this reaction does not occur after swallowing food, but after inhaling particles. The most common cause of respiratory allergies is inhaling the smoke that comes out when you cook or fry fish.
In addition, there is also a serious acute allergic reaction such as Quinkehremen and anaphylactic shock. Such a reaction occurs immediately after contact with allergens and develops very quickly. This is extremely rare and requires urgent medical attention.
Causes of food allergies in newborns
It is very rare for a newborn baby to cause food allergies. Babies receive only breast milk. This is food made by nature for a child, and there will be nothing else. Therefore, the peak food allergy for breast milk is considered to be around 4-5 months after birth, which begins to produce additional foods that are added to breast milk, such as vegetables, fruits, grains, meats, and dairy products. In the case of a child raised in milk, the situation is slightly different. Powdered milk itself can cause food intensity. Therefore, when choosing a mixture, it is better to consult an expert.
What is the most common allergen in infants?
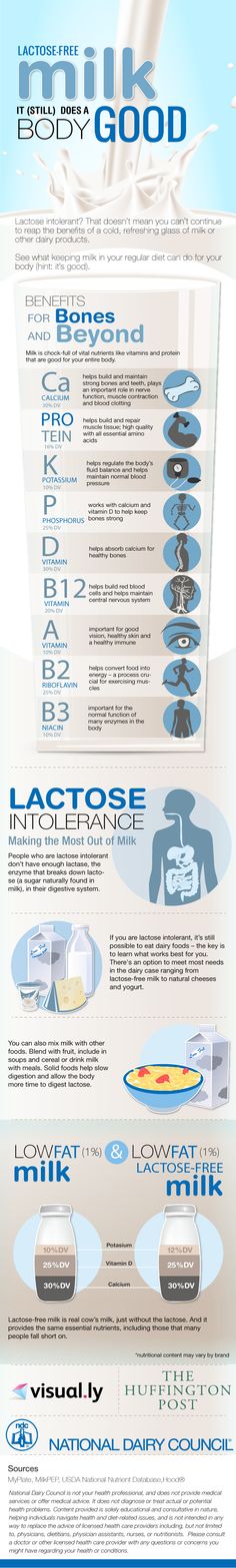
1. 1st place is intensity for milk proteins. Most modern baby milk is based on milk proteins. For this reason, the child causes allergies in the mixture. Also, if the mother's diet is rich in dairy products, babies who are breastfeeding may also react to milk. It is not a specific milk component or powdered milk. Milk ingredients contain many proteins such as albumin, globulin and casein. Some of them can cause allergic reactions, while others do not. Casein makes up about 80% of all milk protein. The ingredients contained in milk are the same as goat's milk. This explains that the baby has a crossover reaction to milk and goat milk. Therefore, if the milk is intolerable, it is not recommended to replace it with a recipe using goat milk or goat milk for baby food. Certain proteins are destroyed by heat treatment. This is because the reactivity of boiled milk (ability to react) is low. There is a protein similar to that of beef and calf. In intolerance to this kind of protein, children will cross milk and meat products.
Milk ingredients contain many proteins such as albumin, globulin and casein. Some of them can cause allergic reactions, while others do not. Casein makes up about 80% of all milk protein. The ingredients contained in milk are the same as goat's milk. This explains that the baby has a crossover reaction to milk and goat milk. Therefore, if the milk is intolerable, it is not recommended to replace it with a recipe using goat milk or goat milk for baby food. Certain proteins are destroyed by heat treatment. This is because the reactivity of boiled milk (ability to react) is low. There is a protein similar to that of beef and calf. In intolerance to this kind of protein, children will cross milk and meat products.
2. The next most common cause of a child's allergy is eggs. In the composition of eggs, allergens also act as albumin, a protein. Therefore, it is recommended to include eggs from egg yolk and small amounts when including eggs in a meal. Please carefully observe the child's reaction to this product. In the first feeding of eggs, it is important to carefully observe the reaction with the protein. Please note that the pasta and bakery contain eggs.
In the first feeding of eggs, it is important to carefully observe the reaction with the protein. Please note that the pasta and bakery contain eggs.
3. Gluten is well known as a cause of food intolerance. It is a protein found in some grains. It is recommended to start adding foods that are gluten-free to avoid side effects. Soba, corn, rice, etc. High gluten foods like Maneuvera, Christos and Automeal should be introduced almost a year in advance. During the first year of reaction to gluten, there is not much intolerance to milk proteins and egg whites.
4. In addition, colorful vegetables and fruits can cause food reactions. Carrots, beets, pumpkin, peach, etc. A good idea is to take green vegetables and white vegetables like zucchini, cabbage, broccoli, etc. And it's better to start with a blue apple or pear for your child's fruit. Exotic fruits such as mango and kiwi should not be rushed.
Be aware that any product can cause an allergic reaction. If you are giving your baby for the first time, your mother should remember the risk of intolerance. In particular, don't be impatient to introduce inferior foods. In the morning, give you some unfamiliar foods so that you can reduce the reaction during the day.
In particular, don't be impatient to introduce inferior foods. In the morning, give you some unfamiliar foods so that you can reduce the reaction during the day.
How to recognize a food allergy and not confuse it with other diseases?
In most cases, the diagnosis of food allergy requires a doctor's consultation and a detailed examination of the mother. Mom sometimes reveals that he is allergic to food or introduces a specific product for the doctor. It can be difficult to make such a diagnosis at the same time. After that, a doctor can be scheduled for the test. Start, all the calculations of blood cells. If necessary, a specific allergy test will be performed, such as an immunoglobulin test and for subsequent ages. These tests have been selected as the most useful in recent clinical guidelines. Also, depending on the symptoms your child is concerned about, you may need to consult an allergy, dermatology, gastrointestinal department, etc. In addition, additional tests from the gastrointestinal tract.
Treatment and prevention of allergies
According to the latest recommendations, breastfeeding is the mainstay of childhood food allergies. Babies who have grown up with only breast milk for a few months are unlikely to develop food allergies. At the same time, healthy breastfeeding does not require special foods. Meals should be perfect and varied, including protein, fat and carbohydrates. It also contains trace elements and vitamins. In addition, it is recommended that the mother of a child at risk of food intolerance not restrict the diet. It is necessary to completely eliminate foods that have reacted from their mother, and make a food diary.
If artificial nutrition is needed for children with a predisposition to allergies, special hypoallergenic mixtures are chosen. The mixture should be selected by a specialist for the treatment of existing conditions. According to the latest clinical guidelines, in case of intolerance to cow's milk proteins, fully hydrolyzed proteins or mixtures with an amino acid composition are chosen. In this case, it is not advisable to prescribe hypoallergenic mixtures or mixtures based on goat milk protein. Soy-based milk powder itself can cause allergic reactions.
In this case, it is not advisable to prescribe hypoallergenic mixtures or mixtures based on goat milk protein. Soy-based milk powder itself can cause allergic reactions.
Proper introduction of complementary foods is also an important step in the prevention and treatment of food allergies. Introduce complementary foods early - not earlier than 4 months and not later than 6 months. Choose hypoallergenic foods first, such as Chinese cabbage, green leafy vegetables, and gluten-free cereals. On one day, the babies were given only a small amount of one complementary food and a possible reaction was observed. In the beginning, limit the introduction of new foods to once a week. Mothers of babies who are predisposed to allergies or already suffering from allergies are advised to keep a food diary. In it, the mother writes down all the foods that she gives the child during the day, and possible reactions to them.
If necessary, the doctor may prescribe medication for your child. They can be considered for both oral administration and dermal treatment. Children with chronic allergic rashes are shown special skin care. Also, after washing, it is necessary to use a special care product - conditioner. It is better to consult a doctor about which conditioner to choose. If you have gastrointestinal or respiratory symptoms, you may need special treatment from your doctor.
They can be considered for both oral administration and dermal treatment. Children with chronic allergic rashes are shown special skin care. Also, after washing, it is necessary to use a special care product - conditioner. It is better to consult a doctor about which conditioner to choose. If you have gastrointestinal or respiratory symptoms, you may need special treatment from your doctor.
Eruptions often appear on the body in children. This may indicate a problem such as an allergy or skin disease. However, in most cases, rashes on the children's body do not pose a threat and go away on their own.
However, if you develop a rash or fever, feel unwell, behave abnormally, or are worried about skin changes, be sure to contact your pediatrician to rule out a serious illness or infection. treatment if necessary.
This article contains information about what causes the rash, but do not take it as a self-diagnosis. This is just an overview of the most common causes of rashes in children. Your pediatrician will be able to tell you more about your child's health. We will talk about the causes of rashes in infants separately.
Your pediatrician will be able to tell you more about your child's health. We will talk about the causes of rashes in infants separately.
Chickenpox (chickenpox)
Chickenpox is a common viral illness affecting most children. Chickenpox causes an itchy red patchy rash on the body that turns into blisters of fluid. The blisters then dry out, form a crust, and eventually flake off. Some children have few spots, while others have a rash all over their body.
Eczema
Eczema is a condition in which the skin becomes red, itchy, dry and cracked. The most common is atopic dermatitis, which is more common in children but occasionally occurs in adults.
Atopic dermatitis usually causes a rash on the feet (knees), hands (elbows), neck and face (eyelids, ears and cheeks). This is a clear illness, but if the child subsequently becomes infected with the herpes simplex virus, the dermatitis may worsen, and small blisters (called irritable fever) may appear along with the high fever.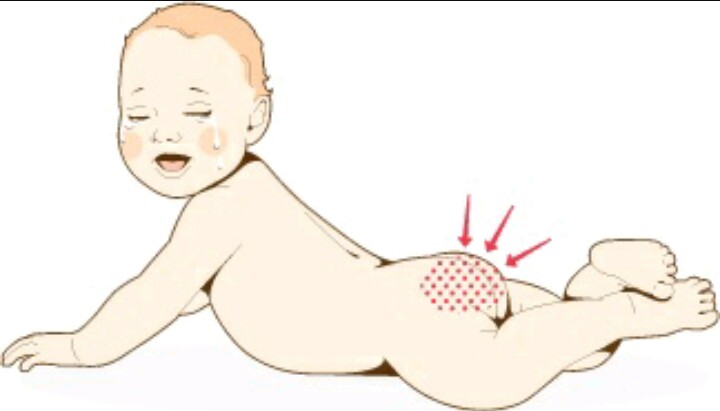
Impetigo
Impetigo is a highly contagious disease caused by bacteria. It is characterized by the formation of pustules and blisters on the skin. There are two types of impetigo.
- Bullous contagious impetigo - large painless blisters filled with fluid.
- Impetigo is highly contagious and causes pustules that break open quickly, forming yellow-brown crusts.
If you think your child has impetigo, talk to your pediatrician. You will be given antibiotic cream and should be cured within 7-10 days.
Ringworm
Ringworm is a common, highly contagious infection that causes round, red rash patches on the skin. The plaques can appear anywhere on the body, but are most common on the scalp, legs, and groin.
Consult a dermatologist for an accurate diagnosis. Lichen interstitialis is treated with antifungal agents that are applied to the skin in the form of creams, ointments, shampoos, or given as tablets. Quarantine is provided for the period of illness, children cannot attend school and kindergarten.
Prickly heat
Sweaty babies may experience this option, for example, when worn in extremely hot or humid conditions. In older children, it develops when hygiene rules are not followed or when wearing uncomfortable synthetic clothing. Small red rashes and blisters appear on the skin, but they usually heal quickly without special treatment. To do this, bathe them regularly and wear them according to the weather.
Exudative erythema multiforme
Pustular erythema - skin reaction caused by:
- bacterial infection
- Herpes simplex virus
Round red spots appear on the arms and legs, which gradually increase and spread throughout the body. Favorite places of rashes Hands, less often feet, to a lesser extent the face, neck, shins, soles of the feet. Sometimes elements of the rash are observed in the oral cavity. The center of the spot gradually turns pale, forming elements that can merge with each other. In addition to blemishes, it can also cause blisters on the skin.
In subtle erythema multiforme, the pediatric focus is often disturbing, the rash is accompanied by fever. Recovery takes 2 to 6 weeks. Rarely, excretory erythema multiforme may develop in response to drugs such as antibiotics or antispasmodics. This is more dangerous, the disease can be life-threatening. Call your pediatrician if you develop a rash and feel unwell.
Keratosis follicularis (“goosebumps”)
Thylakotase is a common, asymptomatic condition in which the skin on the forearms becomes rough and itchy when cold. You can also get goosebumps on your lower back and cheeks.
It usually starts in childhood and worsens during adolescence. After that, the condition subsides and may even disappear completely with age. There is no specific treatment for follicular keratosis, but it usually does not matter much.
Hand-foot-mouth syndrome (viral pemphigus)
Hand-foot-mouth syndrome and viral pemphigus are common benign diseases caused by Coxsackie enteroviruses. Accompanied by rashes and small blisters on the palms and feet of children. Mouth ulcers and general malaise may also occur. Itching is usually not noticeable.
The child's immune system fights the virus on its own and symptoms usually disappear within 7-10 days. However, FMD is a highly contagious disease.
Molluscum contagiosum
Molluscum contagiosum is a skin disease caused by a virus that causes small hard blisters to form on the skin.
Molluscum contagiosum most commonly develops in children between 1 and 5 years of age who infect each other. As a rule, there is no pain, but sometimes itching may occur. Without treatment, it usually resolves within 18 months. In some cases, skin formations can be removed, but in this case, you should consult a dermatologist.
Molluscum contagiosum is highly contagious, but most adults develop immunity to the virus and are less likely to become infected through contact with it.
Pityriasis rosea
Rosacea dandruff is a relatively common skin condition. Rounded pink spots appear on the skin, the central part of which gradually turns pale and begins to peel off. The rash is sometimes accompanied by mild itching. After a few weeks, the spots spread all over the body.
Rounded pink spots appear on the skin, the central part of which gradually turns pale and begins to peel off. The rash is sometimes accompanied by mild itching. After a few weeks, the spots spread all over the body.
Older children and young people between the ages of 10 and 35 are most commonly affected. Dandruff rosacea usually resolves without treatment within 2 to 12 weeks. Its cause is unknown.
Scabies
Scabies is a contagious skin disease caused by tiny, itchy mites that burrow on the skin. This causes a rash with intense itching. Children become infected with scabies through close contact, such as when playing with sick adults or children.
Ticks prefer thin skin between fingers, skin folds, curved limbs and groin. In young children, the legs, arms, buttocks, face, and scalp are usually affected. It leaves small red bumps or silvery lines on the skin, usually on the palms and soles. Infants often develop blisters on their feet. If you suspect you have scabies, call your doctor for treatment (lotion or cream).
Urticaria (urticaria)
Urticaria is a disease characterized by red, itchy, burning rashes on the skin. This is caused by the release of histamine into the skin. Causes redness, swelling and itching.
Urticaria can be caused by a variety of factors, including allergens (eg food and latex), irritants (eg nettles), medications, and natural factors such as sunlight and heat. However, in most cases the cause cannot be determined. This is a common skin reaction in children. The rash usually resolves quickly with antihistamines.
Erythema infectiosum ("fifth disease")
Erythema injectio ("fifth disease") is a viral disease that is common in children that has a red rash on the cheek. In principle, children between the ages of 6 and 10 are eligible. In most cases, the health condition does not appear much and it will subside after a few days, so this is usually not required. This can take 4 to 5 weeks. If you have a rash or fever, contact your doctor.
Psoriasis (psoriasis)
Psoria is a disease in which red spots appear on the skin, covered with a silver scale. Psoriasis can cause beauty defects, and if the course is long, nails and joints can be invaded. This is a chronic condition, but there are treatments to help relieve symptoms, improve the appearance of the rash, and avoid complications.
Cellulitis or phlegmon
Bizitis and sputum is an inflammation of the skin and subcutaneous tissues caused by bacteria. The affected area becomes red, tender, swollen and hot. Changes in the skin are accompanied by high fever, pain and severe exhaustion. If these symptoms appear, contact your pediatrician immediately.
Measles
Motor sickness is a severe infectious disease caused by a virus. Measles can be contracted if you are not vaccinated or have not previously been vaccinated, but if you are one to four years old, you will have measles disease.
Hagan is characterized by a small, reddish brown rash that basically appears behind the ears and then spreads to the head, neck, legs and torso. Children are likely to have flu-like symptoms and a high fever. If you notice the above signs, contact your pediatrician at home.
Children are likely to have flu-like symptoms and a high fever. If you notice the above signs, contact your pediatrician at home.
Scarlet fever
- And it is also a contagious infectious disease in children. The pathogen is a bacterium. A two-year-old child was the most affected. In the scarlet aroma, there is a bright pink rash that is characteristic of the body, and when you touch it, it looks like paper. In many cases, it starts with a sore throat, headache, and fever, and a rash develops after 12-48 hours. If you think your baby is red, contact your family doctor immediately.
Meningitis
A child's rash may be caused by "meningitis t-mamigitis", a disease that leads to death. The rash resembles roots or appears in red spots. It usually disappears after 2-3 hours. And due to serious causes and dangerous complications, the skin can be bruised. A sign that can be considered for meningitis in children.
- Children are repressed, react to others weak, limited and acute.

- The child is frustrated and hates to be hugged.
- I hate hugs, hate hugs, hate hugs, hate hugs, hate hugs, hate hugs.
- Vomiting and refusal to eat
- Blue and white and spots.
- Anorexia
- The expression is complex.
- We have severe drowsiness.
- It's warm.
- Red rash that does not go away even when pressed against hard objects (eg glass).
Trust your intuition. If you think you have had meningitis, contact your pediatrician at home immediately, and if your condition is serious, call an ambulance (03 from the landline, 911 or 112 from your mobile phone).
Rash in a child: which doctor should I contact?
When you go to your child's body, you can use this service to find a good doctor.
Follow the link to find a clinic where you can call a pediatrician at home.
You might also be interested in reading
Napoprovku.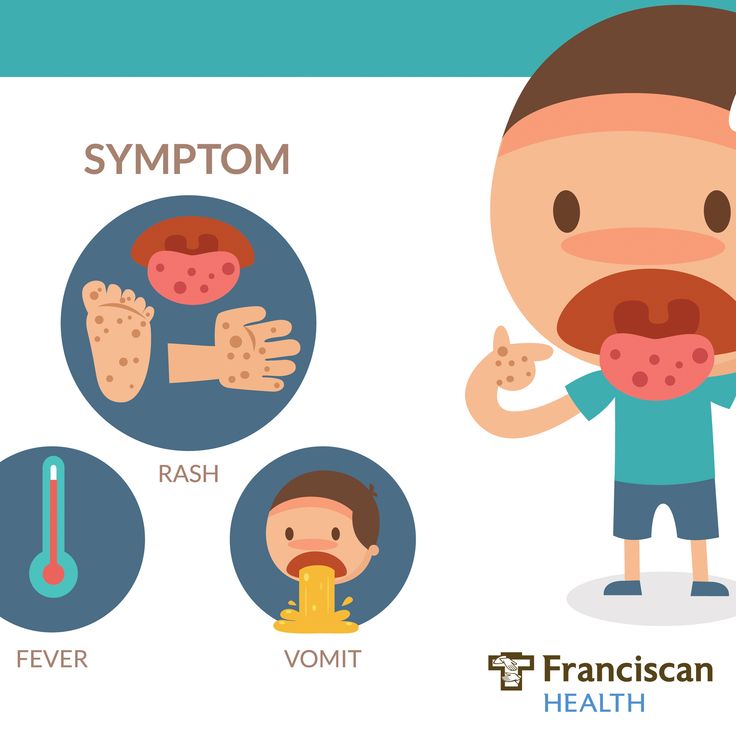 ru was responsible for the localization and translation, and the NHS selection provided the original content for free. Retrieved from www.nhs.uk. Choice The NHS has not endorsed the local content or translation of the website's original content and is not responsible.
ru was responsible for the localization and translation, and the NHS selection provided the original content for free. Retrieved from www.nhs.uk. Choice The NHS has not endorsed the local content or translation of the website's original content and is not responsible.
Copyright notice
All published materials are reviewed by physicians. However, no matter how reliable the articles are, it is not possible to consider all the characteristics of an individual's disease. Therefore, the information posted on this website is not an alternative to consulting a doctor, but additional. These articles have been created for the purpose of providing information and having advice.
Baby skin rash often sues during a pediatric consultation. Usually parents consider the cause of the rash to be children's eating habits. There are so many allergic rashes for children, but I will analyze them for what other reasons and how to treat them.
Physiological rashes
These are the types of rashes that appear on newborns. There seem to be various reasons. No special treatment is required and it disappears naturally. These are the following.
There seem to be various reasons. No special treatment is required and it disappears naturally. These are the following.
- Birotome a - Necessary white spots for the nose and forehead of newborns. Usually it naturally cuts to the first birth age. Special processing is not required.
- Seborrheic dermatitis or milky white crust - development in the year after birth. In tender reddish skin and normal skin, white and yellowish dark skin appears. It can be easily separated from the skin without giving any discomfort. There is no need for treatment. You may want to use shampoos and bubble baths dedicated to the treatment of seborrheic dermatitis sold in pharmacies.
- Dess (acne) for babies. It occurs in a newborn within one year of birth. I sometimes stay for a long time. The reason is that the change is due to hormones. The rash is similar to adult acne. Redness and thickening appear on the skin. Then a head appears with a white and yellowish content. For treatment, use a preservative if needed and a retinoid for severe changes.
- Post-erythema of newborns, approximately 2-5 days after birth and completely disappears after 2-3 weeks. This is redness of the skin filled with white or yellow content or shrine. It can appear anywhere on your body. The cause of the occurrence has not been fully elucidated. There is no need for treatment. He disappears without permission.
-Mongolian spots a-pigmented spots with green, blue and gray, usually found on the back and buttocks of a newborn. Appears from birth. Pass independently at the age of 3 years. The kids are not in trouble. There is no need for treatment.
- Marble-like skin pigmentation - may increase or decrease over time with a delicate network of blood vessels on the surface of a child's skin. The reason is that the child's autonomic nervous system is immature. Pass without permission. There is no need for treatment.
Allergic rashes
One of the causes of dry skin in children is allergies. Pathogens are divided into food and contact. Respiratory allergens rarely cause a rash. Exposure to allergens causes skin redness, swelling, itching, and sometimes clear blisters. If there is a strong reaction, the bubbles will be large. Damage to the epithelium of the bladder exposes the wound surface and heals under the crust. Acute allergic rashes usually disappear quickly after contact with the allergen is stopped. Rash from prolonged exposure to an allergen is usually less intense. treated worse. Makes it difficult to identify allergens. Severe cases require medical attention and more intensive treatment.
Respiratory allergens rarely cause a rash. Exposure to allergens causes skin redness, swelling, itching, and sometimes clear blisters. If there is a strong reaction, the bubbles will be large. Damage to the epithelium of the bladder exposes the wound surface and heals under the crust. Acute allergic rashes usually disappear quickly after contact with the allergen is stopped. Rash from prolonged exposure to an allergen is usually less intense. treated worse. Makes it difficult to identify allergens. Severe cases require medical attention and more intensive treatment.
Atopic dermatitis
This is a skin disease that is accompanied by a violation of its barrier function and the development of inflammation. Atopic dermatitis first appears around 3 months of age. It flows like a wave through a period of improvement. In most cases, it is completely cured within 7 years. Approximately 10% of the changes remain for life. This is dry skin with slight redness, peeling, itching, sometimes small blisters with transparent contents appear. In severe cases, the redness may disappear, and the surface of the skin may crack, with a yellow or clear liquid leaking from it. Topical corticosteroids, pimeclalimus, and toclalimus in ointment or gel form are used to relieve flare-ups. Continue to use emollients to maintain remission and improve skin barrier properties. Antihistamines may be recommended to relieve itching.
In severe cases, the redness may disappear, and the surface of the skin may crack, with a yellow or clear liquid leaking from it. Topical corticosteroids, pimeclalimus, and toclalimus in ointment or gel form are used to relieve flare-ups. Continue to use emollients to maintain remission and improve skin barrier properties. Antihistamines may be recommended to relieve itching.
Miliaria in infants
Predominantly localized in skin folds. It is characterized by redness of the skin and the appearance of small white dots. The reason is a decrease in the secretion of sweat glands and the inflammation that accompanies it. Contact dermatitis and diaper dermatitis is redness and inflammation of the skin caused by prolonged contact with the urine, feces and saliva of children. Both symptoms usually go away on their own with proper hygiene. Dry creams and powders containing zinc may help. Antifungals and antibiotics are used in severe cases with an infected rash.
Rashes associated with skin infections
Chickenpox is an acute, widespread infection that mainly affects children of preschool and primary school age. Symptoms of poisoning appear, sometimes accompanied by an increase in body temperature and the appearance of a characteristic rash. The chickenpox rash begins with red patches on the scalp. Then gradually lower your torso and limbs. It can also appear on the mucous membranes of the mouth and genitals. Soap bubbles with transparent contents appear instead of spots. Blisters appear, accompanied by itching of varying intensity. After that, the air bubbles dry up and become covered with a yellow crust, which eventually disappears. One large element can leave a permanent scar on the skin. Treatment is symptomatic. At high temperatures, use an antipyretic. Topically apply an antiseptic to the skin and mucous membranes to prevent infection of the elements. Antihistamines are indicated for severe itching. It will heal on its own in about 10 days. There are vaccines to prevent chickenpox.
Symptoms of poisoning appear, sometimes accompanied by an increase in body temperature and the appearance of a characteristic rash. The chickenpox rash begins with red patches on the scalp. Then gradually lower your torso and limbs. It can also appear on the mucous membranes of the mouth and genitals. Soap bubbles with transparent contents appear instead of spots. Blisters appear, accompanied by itching of varying intensity. After that, the air bubbles dry up and become covered with a yellow crust, which eventually disappears. One large element can leave a permanent scar on the skin. Treatment is symptomatic. At high temperatures, use an antipyretic. Topically apply an antiseptic to the skin and mucous membranes to prevent infection of the elements. Antihistamines are indicated for severe itching. It will heal on its own in about 10 days. There are vaccines to prevent chickenpox.
- As an infectious disease that appears when fever, catalysis and rash appear on the 3rd - 4th day. Rash of measles appears in the mouth. And this extends to the face and to the body. The component of the rash is large and brown. There is no specific treatment for this rash. There is vaccination.
Rash of measles appears in the mouth. And this extends to the face and to the body. The component of the rash is large and brown. There is no specific treatment for this rash. There is vaccination.
-Reval a is an infectious disease that appears with fever, catalog symptoms, conjunctivitis and rash. Rufella rash is small, bright, spreads over the entire skin. This disease has no silver bullet. Rubla has a vaccine.
- Pidera (sudden rash) ... This is a viral disease that develops mainly in children after 10 months. Up to two years of age. Appears with severe poisoning and acute onset with high fever. On the 3rd day, body temperature appears, and several elements of red rash appear. It starts from your head and gradually descends throughout your body. I don't care about the baby's rash. It heals naturally in 2-3 days. This disease does not require treatment.
- Per n-development from preschoolers. A characteristic change appears on the red border between the lips, mucous membranes and the oral cavity. Children feel itching and tingling. Redness appears on the skin, then swells, and a multifunctional graft is formed. When the disease subsides, crusts (cabs) form instead of bubbles, and they disappear without a trace. Herpes treatment includes an antiviral form in the form of a gel, ointment and tablets.
Children feel itching and tingling. Redness appears on the skin, then swells, and a multifunctional graft is formed. When the disease subsides, crusts (cabs) form instead of bubbles, and they disappear without a trace. Herpes treatment includes an antiviral form in the form of a gel, ointment and tablets.
- Infectious flame of the angle of wheat is a viral skin lesion. This is expressed by the appearance of gradually increasing itching on unaffected skin. And a characteristic dent appears in the center. This disease is contagious, not dangerous, lasts a long time, and there is no specific treatment.
-Scarlac a is an infectious disease caused by bacteria. Appears in intense drunkenness, fever, inflammation of the tonsils and characteristic changes in the skin. The scarlet t-fever rash is patchy and not bright. It occurs in folds such as the groin, elbows, and armpits. And it spreads throughout the body. After recovery, go through without any x-traces. Some time after the disease, the skin may remain on the finger of the extremities. Scary fever is treated with oral antibiotics.
Scary fever is treated with oral antibiotics.
-Marming bacterial infection: a serious bacterial infection that also occurs due to fever, catalytic symptoms and damage to the central nervous system. The rash of meningitis infections has a characteristic appearance. These are the isolated bleeding factors that will add up to the big "subcutaneous bleeding". If such a rash appears on your child's skin, you need to consult a doctor immediately. Treatment with a systemic antibiotic. Mennititis bacterial infections have vaccines.
- Wakig a is a rash caused by bacteria. A brightly painful redness appears around the face, usually around the mouth, and then it will be covered with dirty yellow crusts. External antibiotics are used for treatment. In case of severe diseases, internal medicine is prescribed.
Counseling tells you about the problem you have, the doctor explains the situation, reads the test, answers your questions and makes the necessary suggestion.
There are various reasons for a baby's skin rash. Only typical ones are explained here. It is necessary to consult a pediatrician to understand the symptoms and understand how to help the child. Additional tests may be required.
Rashes in infants | Rassvet Clinic
Babies are generous with various rashes. According to the "good" tradition, most of them are considered allergic with all the consequences - a strict diet for a nursing mother, transfer to artificial feeding, prescription of therapeutic mixtures, etc. In fact, true allergic rashes in infants are not so common. Allergic diseases affecting the skin in infants include: atopic dermatitis, acute urticaria and angioedema. Acute urticaria is extremely rare in infants - this is an acute allergic reaction in the form of peculiar rashes like blisters (as with a nettle burn, hence the name), which suddenly appear on the skin and just as suddenly disappear without leaving any trace, usually do not exist on the skin for longer than a day and are accompanied by severe itching, which manifests itself in the general anxiety of the child. The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
Let's look at what is most often undeservedly called an allergy:
Toxic erythema newborns is a transient benign rash, the exact cause of the appearance is unknown (possibly due to skin irritation by environmental factors).
Appears at birth or in the first 24-48 hours of life. Localization - face, trunk, limbs, except for the palms and soles. Disappears on its own within 5-7 days, sometimes 3 weeks. Does not require treatment.
Neonatal acne (acne infancy, neonatal pustulosis) is caused by androgen stimulation of the baby's sebaceous glands.
The peak of rash occurs in the 3rd week of life. It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
treatment creams may be required.
Sweating rash , which occurs in poorly "ventilated" areas as a result of blockage of the sweat glands. May occur at any age.
Localization - skin folds, buttocks and back surface of the body, sometimes the face (after sleep). Depending on the depth of the lesion, it happens - crystal prickly heat, prickly heat, deep prickly heat (superficial).
The duration of the rash is from several hours to several days.
Treatment - cool water baths, air baths, prevention of overheating. Lotions containing calamine and creams with corticosteroids and antibiotics may be used to treat some cases of red and deep prickly heat.
Seborrheic dermatitis is a skin disorder that develops in areas rich in sebum. The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).
The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).
It can be foci or widespread, dermatitis with bran-like scales, which can form a crust (“cap”, gneiss) on the scalp.
Favorite localization - scalp, face, folds (!).
May begin at 1-2 weeks of age or later, resolve spontaneously within weeks or months.
Treatment consists of softening the crusts with oil or cream and then removing them, moisturizing the skin and, in some cases, applying antifungal and anti-inflammatory creams.
Simple contact dermatitis is a non-specific skin injury due to prolonged or repeated exposure to a number of substances - saliva, fruit juices, foaming bath products, detergents (their residues on the walls of the bath), etc. In infants, saliva is often causes dermatitis in the area of contact with the nipple and in the folds of the neck.
As a general rule, removal of the damaging agent and short-term use of anti-inflammatory creams will quickly lead to recovery, but some children are so sensitive that it is almost impossible to identify the causative factor.
Diaper dermatitis (prototype of contact dermatitis) is a skin lesion that occurs under the influence of physical (overheating), chemical, enzymatic (contact with sweat, urine and feces) and microbial factors. Localization - the area of the diaper or diaper fit.
Treatment is carried out using the abbreviation ABCDE (air, barrier, cleansing, diaper, education) - air, barrier, cleansing, diaper and parent education. Frequent diaper changes, washing the skin and drying it thoroughly help. Dermatitis is effectively prevented by the application to clean skin of products that completely cover it (Vaseline, zinc paste). In stubborn cases, medicated creams containing corticosteroids, antibiotics, or antifungals may be recommended.
And now a few words about AD:
Atopic dermatitis is a chronic allergic inflammation of the skin, genetically determined, associated with the loss of the skin barrier and, therefore, accompanied by dryness, itching and various rashes. In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
Starts more often not earlier than 3 months of age.
The most common localization up to 2-3 years is the face (cheeks, forehead, chin), convex parts of the limbs (extensor surfaces) and trunk, never in babies in folds (!).
Exacerbations are provoked by various factors - stress, dry air, sweat, food (histamine liberators), infections, contact with tobacco smoke, animal hair, rough fabrics, detergent residues on clothes, etc.
Treated with careful skin care and using anti-inflammatory creams.
There are also:
Pseudo-allergic reactions are reactions that look similar to allergic reactions (for example, various rashes), but are not such, due to the non-immune mechanism of their development.
The reason is an increased content of histamine (tyramine, serotonin) in foods, or the ability of foods to increase the release of these substances in the body, or their increased absorption, due to the pathology of the gastrointestinal tract (fermentopathy, inflammation in the intestinal wall, etc.). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
Treatment includes dietary advice, skin care, and in some cases, antihistamines and anti-inflammatory creams.
Clinical manifestations of atopic dermatitis, simple contact dermatitis in highly sensitive children and the manifestation of pseudo-allergic reactions are very similar to each other, so the main task remains to create a "skin barrier" by constantly moisturizing the skin with the help of emollients, stopping exacerbation with anti-inflammatory creams and eliminating exacerbation-provoking factors .