Can babies grow out of lactose intolerance
What should I do if I think my baby is allergic or intolerant to cows' milk?
If you think your baby is having a reaction to cows' milk, see your GP to discuss your concerns.
They will be able to assess if your baby's symptoms may be caused by a cows' milk allergy or something else. Make sure you get medical advice before taking cows' milk out of your child's diet as it contains important nutrients.
Cows' milk allergy in babies
Cows' milk allergy (CMA), also called cows' milk protein allergy, is one of the most common childhood food allergies. It is estimated to affect around 7% of babies under 1, though most children grow out of it by the age of 5.
CMA typically develops when cows' milk is first introduced into your baby's diet either in formula or when your baby starts eating solids.
More rarely, it can affect babies who are exclusively breastfed because of cows' milk from the mother's diet passing to the baby through breast milk.
There are 2 main types of CMA:
- immediate CMA – where symptoms typically begin within minutes of having cows' milk
- delayed CMA – where symptoms typically begin several hours, or even days, after having cows' milk
Symptoms of cows' milk allergy
Cows' milk allergy can cause a wide range of symptoms, including:
- skin reactions – such as a red itchy rash or swelling of the lips, face and around the eyes
- digestive problems – such as stomach ache, vomiting, colic, diarrhoea or constipation
- hay fever-like symptoms – such as a runny or blocked nose
- eczema that does not improve with treatment
Occasionally CMA can cause severe allergic symptoms that come on suddenly, such as swelling in the mouth or throat, wheezing, cough, shortness of breath, and difficult, noisy breathing.
A severe allergic reaction, or anaphylaxis, is a medical emergency – call 999 or go immediately to your local hospital A&E department.
Treatment for CMA
If your baby is diagnosed with CMA, you'll be offered advice by your GP or an allergy specialist on how to manage their allergy. You may also be referred to a dietitian.
Treatment involves removing all cows' milk from your child's diet for a period of time.
If your baby is formula-fed, your GP can prescribe special infant formula.
Do not give your child any other type of milk without first getting medical advice.
If your baby is exclusively breastfed, the mother will be advised to avoid all cows' milk products.
Your child should be assessed every 6 to 12 months to see if they have grown out of their allergy.
Read more about cows' milk allergy.
Could it be lactose intolerance?
Lactose intolerance is another type of reaction to milk, when the body cannot digest lactose, a natural sugar found in milk. However, this is not an allergy.
Lactose intolerance can be temporary – for example, it can come on for a few days or weeks after a tummy bug.
Symptoms of lactose intolerance include:
- diarrhoea
- vomiting
- stomach rumbling and pains
- wind
Treatment for lactose intolerance
Treatment depends on the extent of your child's intolerance. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.
Your child may be referred to a dietitian for specialist advice.
Read more about treatment for lactose intolerance in children.
Further information:
- Colic
- Food allergies in babies and children
- Reflux in babies
- How can I tell if my baby is seriously ill?
- When should I start giving my baby solids?
- National Institute for Health and Care Excellence (NICE): food allergy in children
Page last reviewed: 12 July 2019
Next review due: 12 July 2022
Lactose Intolerance in Infants & Children: Parent FAQs
By: Anthony Porto, MD, MPH, FAAP
It can be difficult to know whether your infant or child is having symptoms of lactose intolerance or whether he or she may have a milk allergy.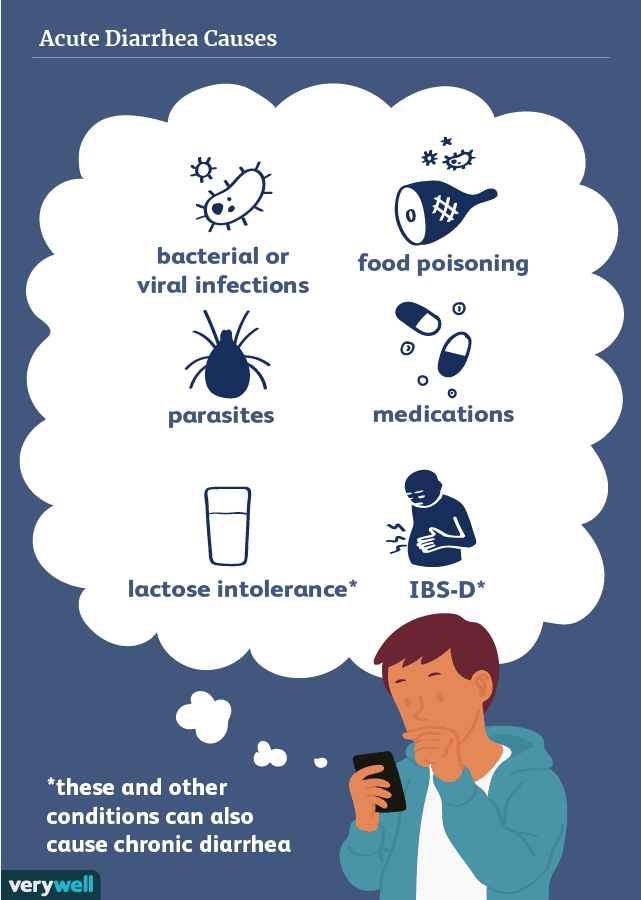
The following frequently asked questions from parents will help you learn more about the common symptoms of lactose intolerance, diagnosis, and treatment options.
Is lactose intolerance the same thing as a milk allergy?
No. Many parents confuse the terms lactose intolerance and milk allergy. While they may share similar symptoms, they are entirely different conditions. Lactose intolerance is a digestive problem, while milk allergy involves the immune system. So, while lactose intolerance can cause a great deal of discomfort, it will not produce a life-threatening reaction such as anaphylaxis.
Milk allergies tend to appear within the first year of life, while an infant's digestive system is still quite immature. Lactose intolerance can start in childhood into adolescence and can become more noticeable into adulthood.
What is lactose?
Lactose is a sugar found in foods that many children love—milk and dairy products, such as frozen yogurt and cheeses. The list of other foods containing lactose is long and includes some breads, cereals, and frozen or canned foods.
The list of other foods containing lactose is long and includes some breads, cereals, and frozen or canned foods.
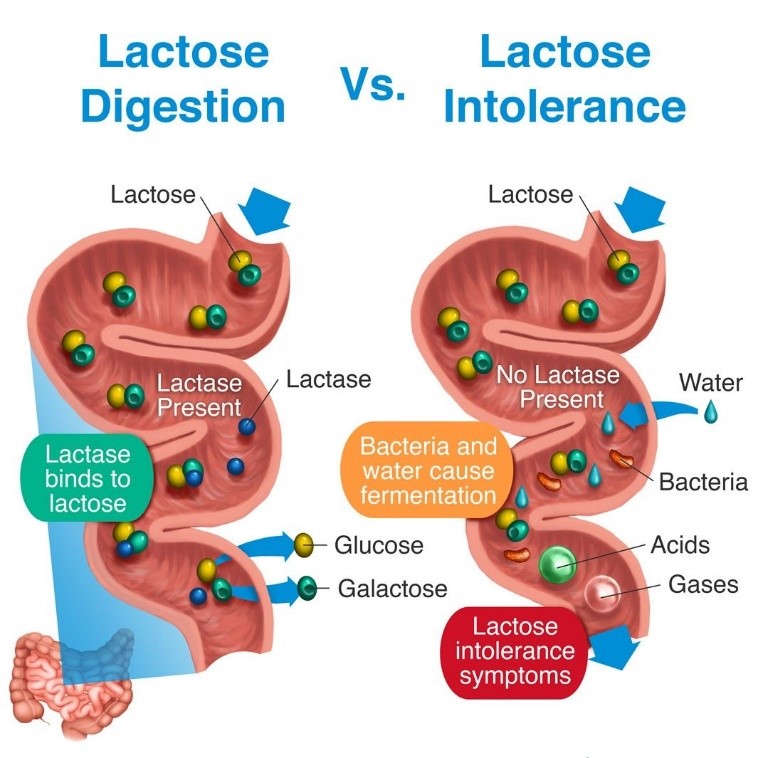
Lactose is broken down by the lactase enzyme located in the small intestine—the organ where most food digestion and nutrient absorption takes place. When we eat lactose, lactase breaks lactose down into two simple sugars: glucose and galactose. The body then absorbs these simple sugars into our intestines. When there is a decrease or loss of the lactase enzyme, we cannot break down or absorb lactose. The unabsorbed lactose can lead to symptoms, which is called an intolerance.
In addition to milk, what other food products contain lactose?
Lactose is present in many food products and in some medications. Manufacturers also often add milk and milk products to boxed, canned, frozen, packaged, and prepared foods. People who have digestive symptoms after consuming a small quantity of lactose should be aware of the many food products that may contain even small amounts of lactose.
You can check the ingredients on food labels and the nutrition facts to find possible sources of lactose in food products. If a food label includes any of the following words, the product contains lactose:
What are some key symptoms of lactose intolerance?
The symptoms of lactose intolerance depend on the amount of lactose that's consumed. The more lactose your child consumes, the more symptoms he or she will experience. Symptoms of lactose intolerance can occur within minutes to hours after drinking milk or eating dairy products and range from mild to severe based on the amount consumed and the amount tolerated. Here are symptoms you should look out for:
Nausea
Abdominal pain, cramping, and bloating
Loose stools and gas
Watery diarrhea with gas
If I think my child might be lactose intolerant. How can I tell?
One way to check if your child has trouble digesting lactose is to take all the milk products out of your child's diet for two weeks and to then see if his or her symptoms improve. After two weeks, slowly reintroduce the products in small amounts each day to see if symptoms return. Your pediatrician can also test your child for lactose intolerance with a hydrogen breath test.
After two weeks, slowly reintroduce the products in small amounts each day to see if symptoms return. Your pediatrician can also test your child for lactose intolerance with a hydrogen breath test.
I've heard lactose intolerance can sometimes be a temporary side effect when kids are sick. Is that true?
Yes. Lactose intolerance can occur temporarily in children after a viral infection (that is why you may be told to avoid milk with lactose in it during a stomach bug) or it may be seen with conditions that lead to inflammation of the intestines, such as celiac disease.
Can infants be lactose intolerant?
Lactose intolerance is actually not very common in infants and typically only starts showing up after age three in children who were born full-term. All babies are born with lactase in their intestines. As they grow older, the lactase enzyme decreases.
Babies who were born premature are more likely to have a type of lactose intolerance called developmental lactase deficiency.
This condition usually lasts only for a short time after birth. However, the majority of premature infants will be able to consume lactose-containing formula and breast milk.
Congenital lactase deficiency is a very rare disorder in which babies can't break down the lactose in breast milk or formula. Genes inherited from parents cause this disorder. This type of intolerance results in severe diarrhea, and if not fed a lactose-free infant formula, those babies could develop severe dehydration and weight loss.
If a mother is lactose intolerant, is it safe for her to breastfeed her baby?
It's perfectly safe to breastfeed your child if you're lactose intolerant. Breastfeeding does not put your baby at greater risk of becoming lactose intolerant, and it has important health benefits for your baby.
How can my child get enough calcium in her diet if milk or lactose are reduced?
If your child has lactose intolerance, he or she can still eat lactose-free dairy products including lactose-free milk, cheese, and yogurts—all are good sources of calcium. In addition, your child can get calcium from dark green leafy vegetables such as spinach, broccoli and kale, nuts (almonds), beans (white beans), fish (sardines, salmon) and calcium-fortified orange juice. If you feel your child is not getting enough calcium, talk with your pediatrician about starting a calcium supplement.
In addition, your child can get calcium from dark green leafy vegetables such as spinach, broccoli and kale, nuts (almonds), beans (white beans), fish (sardines, salmon) and calcium-fortified orange juice. If you feel your child is not getting enough calcium, talk with your pediatrician about starting a calcium supplement.
Are soy or almond milks adequate substitutes for children who are lactose intolerant?
There are many milk substitutes that a child with lactose intolerance can drink, including soy, almond, rice, hemp, and oat milk. Soy milk is a popular milk alternative, because it is a good source of calcium and protein. Almond milk has also become a popular alternative and is safe for children with lactose intolerance or a cow's milk protein allergy. Although almond is a good source of calcium, it is lower in protein and contains fewer calories than cow's milk. Before starting any alternative milks, it is important to talk with your pediatrician about which may be best for your child.
How is lactose intolerance diagnosed?
Your pediatrician will take a medical, family, and diet history to help diagnose lactose intolerance in your infant or child. During this discussion, he or she will review your child's symptoms with you.
In some cases, a hydrogen breath test is done to test for lactose intolerance. For the test, your child breathes into a container that measures breath hydrogen level before and after he or she drinks a beverage that contains a known amount of lactose. Normally, only a small amount of hydrogen is detectable in the breath when a person eats or drinks and digests lactose. An increase in hydrogen levels is considered a positive test for lactose intolerance.
Pediatricians check acidity in the stools of infants and young children who may be unable to properly do the hydrogen breath test. Acidic stool (low pH) may indicate lactose malabsorption. Another stool test (reducing substances) looks for the presence of glucose in the stool, which signifies undigested lactose.
If your child's symptoms persist, he or she may be referred to a pediatric gastroenterologist (GI) for further evaluation. Depending on the severity of your child's symptoms, the GI may perform an endoscopy to measure lactase levels directly from the intestine. This is done with a biopsy.
How much calcium and vitamin D are recommended for my child to eat each day?
The specific amount is based on your child's age. Here is a breakdown of the Recommended Dietary Allowances (RDA) for calcium and vitamin D.
How is lactose intolerance treated?
How lactose intolerance is treated depends on the extent of your child's symptoms. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.
To help alleviate symptoms if/when your child consumes lactose-containing food, your pediatrician may recommend an over-the-counter lactase enzyme supplement.
If your child's symptoms are severe and warrant removing all lactose from his or her diet, your pediatrician may refer your child to a registered dietitian. Since dairy is a good source of calcium and vitamin D—which all kids need—a registered dietitian can suggest other foods to provide those nutrients and may suggest vitamin supplements.
Is lactose intolerance a lifelong condition?
In some cases, lactose intolerance is temporary—if lactose intolerance develops after a viral illness or if it is associated with other conditions, like celiac disease. For example, once celiac disease is treated, lactase levels can become in the normal range and lactose may be tolerated in the diet. More than likely, however, lactose intolerance is long-term and requires many older children and adults to alter their diet to avoid symptoms.
Additional Information & Resources:
Vitamin D: On the Double
Milk Allergy
Infant Allergies and Food Sensitivities
Lactose Intolerance in Infants, Children and Adolescents (AAP Clinical Report)
About Dr.
 Porto:
Porto:Anthony Porto, MD, MPH, FAAP is a board certified pediatrician and board certified pediatric gastroenterologist. He is an Associate Professor of Pediatrics and Associate Clinical Chief of Pediatric Gastroenterology at Yale University and Director, Pediatric Gastroenterology at Greenwich Hospital in Greenwich, CT. He is also the medical director of the Yale Pediatric Celiac Program. Within the American Academy of Pediatrics, Dr. Porto sits on the PREP Gastroenterology Advisory Board and is a member of the Section on Gastroenterology, Hepatology and Nutrition. He is also a member of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition's Public Education Committee, a pediatric expert on nutrition for The Bump's Real Answers, and is the co-author of The Pediatrician's Guide to Feeding Babies and Toddlers. Follow him on Instagram @Pediatriciansguide.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Lactose intolerance | Symptoms, complications, diagnosis and treatment
People with lactose intolerance are unable to fully digest the lactose in milk. As a result, they develop diarrhea, gas, and bloating after eating or consuming dairy products. The condition, also called lactose malabsorption, is usually harmless, but its symptoms can be uncomfortable. Most people with lactose intolerance can manage the condition without giving up all dairy products.
Lactase deficiency, an enzyme produced in the small intestine, is usually responsible for lactose intolerance. Many people have low lactase levels but can digest dairy products without problems. If you are actually lactose intolerant, lactase deficiency leads to symptoms after you eat dairy products.
Signs and symptoms of lactose intolerance usually begin 30 minutes to two hours after eating or drinking foods containing lactose. General signs and symptoms include:
General signs and symptoms include:
- Diarrhea
- Nausea and sometimes vomiting
- Abdominal cramps
- Inflate
- Gases
Make an appointment with your doctor if you often experience symptoms of lactose intolerance after eating dairy products, especially if you are worried about getting enough calcium.
Causes
Lactose intolerance occurs when the small intestine does not produce enough enzyme (lactase) to digest milk sugar (lactose).
Normally, lactase converts milk sugar into two simple sugars, glucose and galactose, which are absorbed into the bloodstream through the intestinal lining.
If you are lactase deficient, the lactose in food moves to the large intestine instead of being processed and absorbed. In the colon, normal bacteria interact with undigested lactose, causing the signs and symptoms of lactose intolerance.
There are three types of lactose intolerance.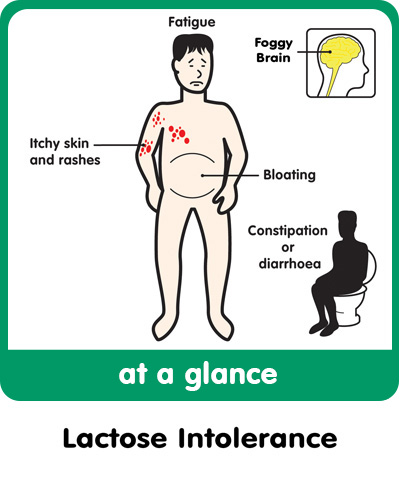 Various factors cause lactase deficiency underlying each type.
Various factors cause lactase deficiency underlying each type.
Primary lactose intolerance
This is the most common type of lactose intolerance. People with primary lactose intolerance begin their lives by producing large amounts of lactase, a must for babies who get all their nutrients from milk. As children replace milk with other foods, their lactase production usually decreases but remains high enough to digest the amount of dairy in a normal adult diet.
In primary lactose intolerance, lactase production drops dramatically, making it difficult for adults to digest dairy products. Primary lactose intolerance is genetically determined, which occurs in a significant proportion of people of African, Asian, or Hispanic ancestry. This condition is also common among Mediterranean or South European ancestry.
Secondary lactose intolerance
This form of lactose intolerance occurs when the small intestine reduces its production of lactase after illness, injury, or surgery involving the small intestine.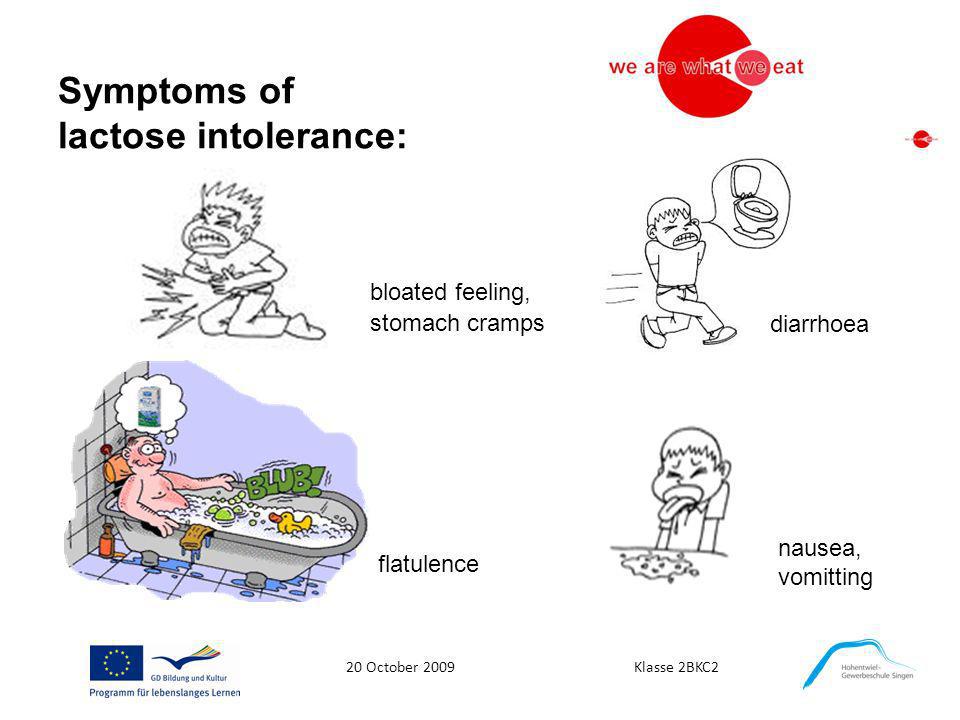 Diseases associated with secondary lactose intolerance include celiac disease, bacterial overgrowth, and Crohn's disease. Treating the underlying disorder can restore lactase levels and improve symptoms and signs, although this may take some time.
Diseases associated with secondary lactose intolerance include celiac disease, bacterial overgrowth, and Crohn's disease. Treating the underlying disorder can restore lactase levels and improve symptoms and signs, although this may take some time.
Congenital or developing lactose intolerance
This disorder is passed from generation to generation in a form of inheritance called autosomal recessive. Premature babies may also be lactose intolerant due to insufficient lactase levels.
Factors that may make you or your child more likely to become lactose intolerant, include:
- Growing up. Lactose intolerance usually appears in adulthood. This disease is rare in children and young children.
- Ethnos. Lactose intolerance is most common in African, Asian, Hispanic, and American Indian people.
- Premature birth. Babies born prematurely may have low lactase levels because the small intestine does not develop lactase-producing cells until late in the third trimester.

- Diseases affecting the small intestine. Small intestinal problems that can cause lactose intolerance include bacterial overgrowth, celiac disease, and Crohn's disease.
- Some treatments for cancer. If you've had radiation therapy for abdominal cancer or intestinal complications from chemotherapy, you're at increased risk of lactose intolerance.
Lactose intolerance | Tervisliku toitumise informatsioon
Essence of disease and frequency of manifestation
Lactose intolerance, or hypolactasia, is caused by the inability of the human body to produce enough lactase, an enzyme that breaks down milk sugar called lactose.
Lactose, or milk sugar, is a disaccharide that cannot be absorbed through the walls of the small intestine and must first be broken down into two simple sugars, glucose and galactose.
After eating products containing milk sugar, with a lack of lactase, lactose enters the large intestine, in the microflora of which it decomposes, forming gases (hydrogen, methane and carbon dioxide), as well as acids.
Symptoms range from mild abdominal pain to cramps and diarrhea.
People with low lactase activity tolerate lactose differently.
Most people tolerate the daily intake of lactose equivalent to half to one glass of milk. If milk is consumed with food, the patient tolerates lactose more easily, since lactose is absorbed more slowly. The same applies to full-fat milk, since fat slows down the elimination of food from the stomach.
Lactase appears in the human digestive tract approximately eight weeks before birth and is most active during infancy. When other foods appear in the child's diet and the need for such large amounts of lactase disappears, the activity of the enzyme begins to gradually decrease. Lactase activity is promoted by eating foods containing lactose.
Approximately three quarters of the world's population, especially the representatives of the yellow and black races, lactase activity is so low that they cannot tolerate milk at all. Among the peoples of Northern Europe and their North American descendants, who have been engaged in pastoralism for a long time, this activity has been better preserved.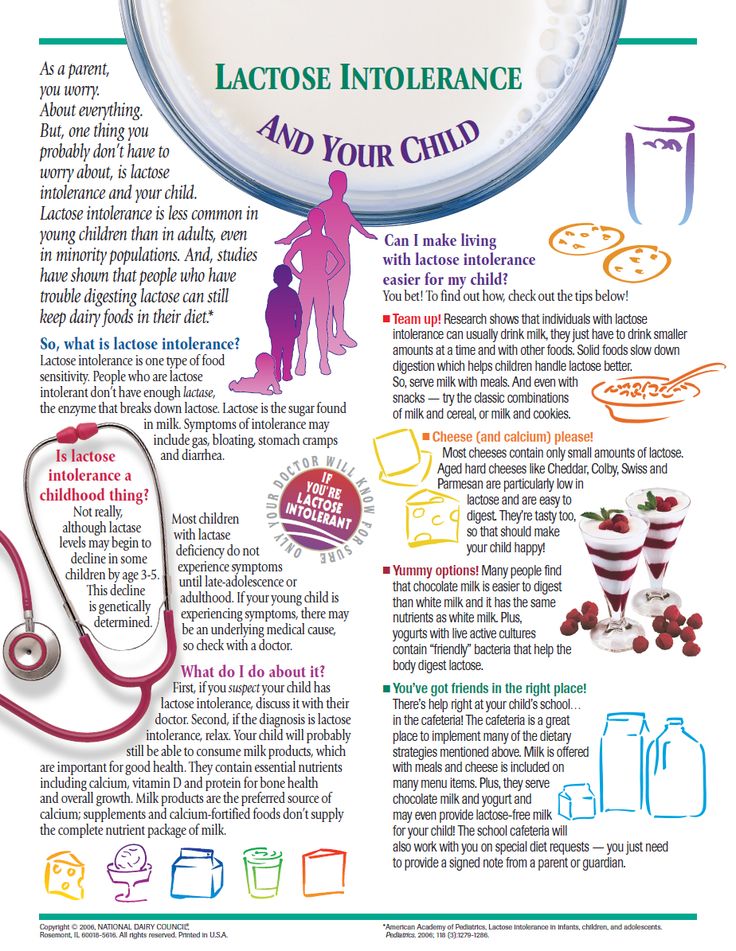
It is believed that about a quarter of the Estonian population suffers from some degree of lactose intolerance. However, many simply do not know about this, and this is not a problem for them, because they do not drink so much milk that it causes them inconvenience.
Lactose intolerance occurs in two forms
Primary lactase deficiency is hereditary, age-dependent and usually manifests between 5 and 20 years of age. Typically, 50-70% of lactase activity is retained. Not treated.
Secondary lactase deficiency is caused by temporary damage to the small intestine, which can be caused by malnutrition, celiac disease, inflammation of the small intestine, gastroenteritis and other diseases. Secondary lactase deficiency also occurs in infants and young children after bowel disease. Symptoms of the disease usually disappear within 2-4 weeks.
Diagnosis and control of lactose intolerance
Lactose intolerance can be guessed from its manifestations./s3.gy.digital/boxpharmacy/uploads/asset/data/11813/frisolac_lactose_free6001pps0.jpg) Since lactose intolerance requires reducing the consumption of lactose-containing dairy products, which occupy a very important place in the human diet, you should first carefully make sure that we are talking about this particular disease.
Since lactose intolerance requires reducing the consumption of lactose-containing dairy products, which occupy a very important place in the human diet, you should first carefully make sure that we are talking about this particular disease.
In the diagnosis of lactose intolerance, for example, a lactose tolerance test is used, during which the patient is given 50 g of lactose (an amount approximately equal to that contained in a liter of milk) and the blood glucose level is determined before taking the solution, after 20 and 40 minutes after. If blood glucose levels do not rise, lactose intolerance is present.
Another option is breath analysis. If the hydrogen content in it increases, this indicates that under the influence of the microflora of the large intestine, lactose fermentation is taking place, and the patient has lactose intolerance.
Depending on the severity of the disease, the amount of lactose in the diet should be reduced to a greater or lesser extent.