Epidural risks for baby
Epidurals and Birth Injuries
Labor and delivery is an extraordinarily painful experience for women and maternal pain-management has become an important aspect of modern obstetrical practice. The epidural has become the most widely utilized method for managing pain during childbirth and is administered to millions of women in labor every year. Recent estimates suggest that an epidural is given to the mother in over half of all deliveries in the United States and Canada. Seventy-one percent of pregnant women get either an epidural or some other spinal anesthesia. Although epidurals are generally considered safe they do present a number of risks and negative side effects which can potentially increase the risk of complications and related birth injuries. Women have to way the pros and cons of epidurals to make the choice that is best for them.
What is an Epidural?
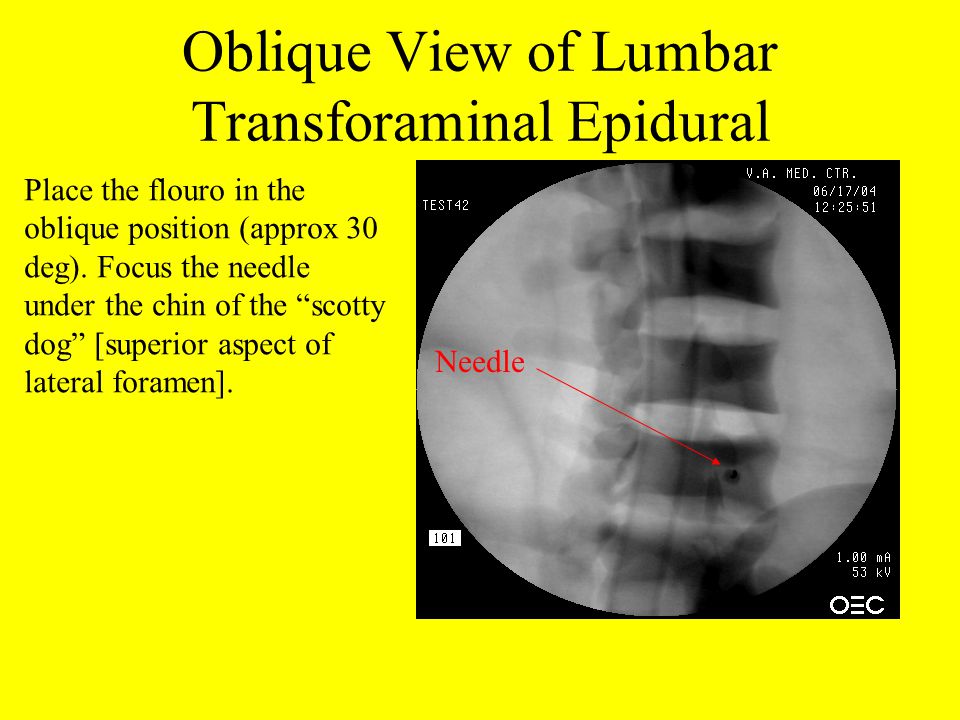
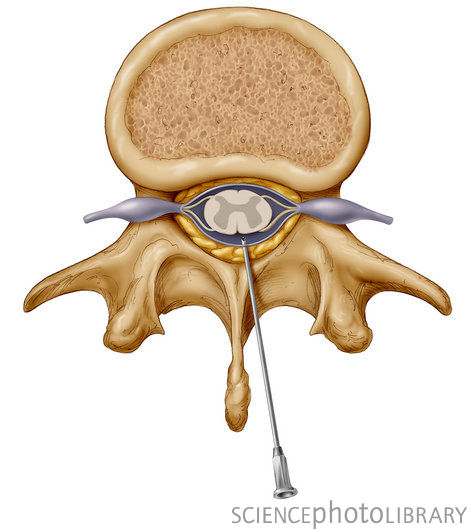
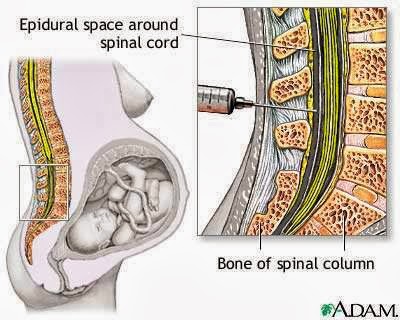
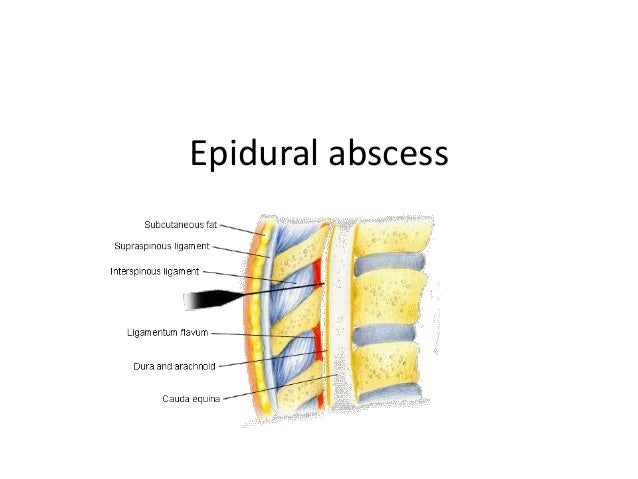
The epidural is a particular method of administering regional anesthesia that basically numbs the lower half of the mother's body to block the pain from labor and birth. Anesthetic medication is injected directly into an area of the mother's spine called the epidural space (which is where the name "epidural" comes from). The epidural space is a fluid filled area which encases the outside of the spinal cord. The body transmits pain signals to the brain through nerve pathways that connect to the spine. Injecting anesthetics into the epidural space is very effective at blocking the transmission of pain signals through these nerve channels.
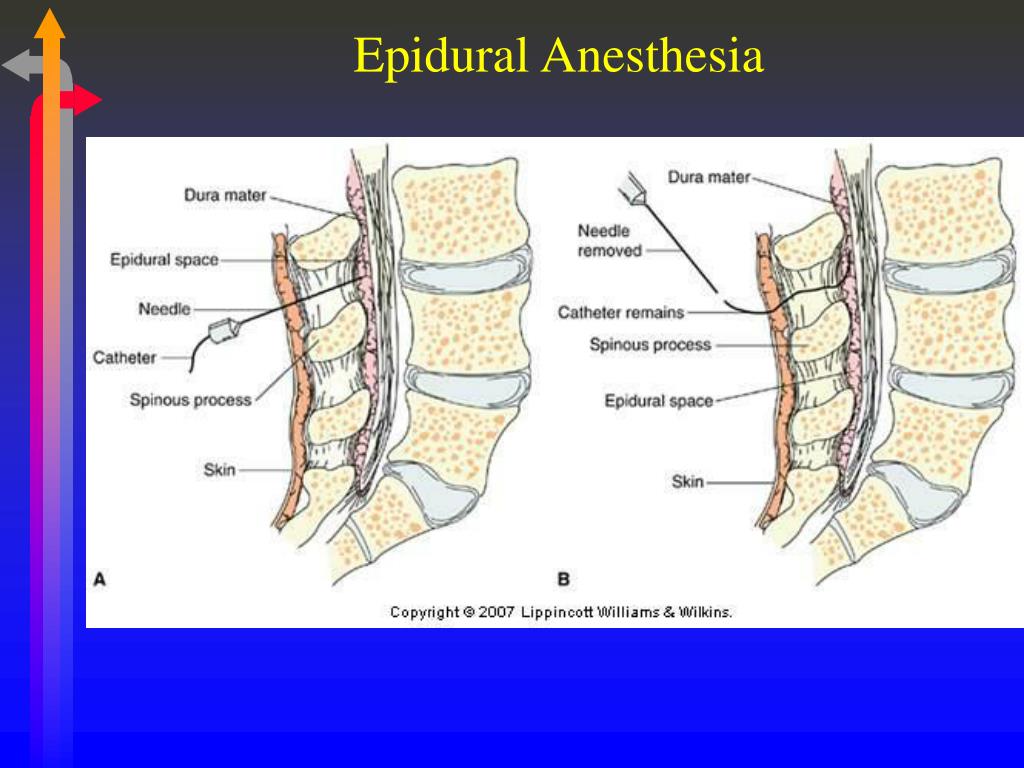
A single injection of anesthetics into the epidural space is not sufficient to last for the entire labor and delivery. To prevent the medication from wearing off, the anesthesiologist inserts a special type of needle that stays in the mother's back and is attached to a catheter or drip device. This gives doctors 2 options. They can either use the catheter to administer additional doses of medication as needed; or they can attach the catheter to a pump device which will continuously supply the medication in small amounts. Getting the needle inserted correctly can be difficult and may require several attempts. Epidurals are highly effective at eliminating pain and fewer than 1 out of 100 mothers require additional pain relief after an epidural.
Getting the needle inserted correctly can be difficult and may require several attempts. Epidurals are highly effective at eliminating pain and fewer than 1 out of 100 mothers require additional pain relief after an epidural.
The type of drugs delivered through epidurals are known as local anesthetics, which block pain in targeted areas of the body. The local anesthetic medications most frequently administered with epidurals are: Bupivacaine, Lidocaine, and Chloroprocaine.
Risks and Side Effects of Epidurals
Specific side effects differ somewhat depending on the type of medication used in the epidural. However, there are a number of potential side effects associated with all epidurals:
- Lower Blood Pressure: approximately 14% of women who get an epidural experience a sudden drop in blood pressure. Lower blood pressure is not a serious issue but can increase the risk of certain complication and can also cause nausea and discomfort.
- Fever: epidurals trigger a fever in around 23% of women who get them. A sudden spike in maternal fever can create serious risks for the baby. A recent study has shown that epidural induced fevers increase the chances of a baby being born with poor muscle tone, breathing issues, and lower Apgar scores.
- Urination Problems: because the epidural numbs the lower body it can cause difficulty urinating. About 15% of women experience this side effect which sometimes requires a urinary catheter.
Additional potential risks to the mother presented by epidurals include seizures, heightened risk of infection, respiratory difficulty, and nerve damage. It is not true that epidurals increase the risk of a C-section.
Epidurals Increase the Risk of a Birth Injury
Some studies have shown a link between the use of epidurals and a slightly higher rate of a baby being diagnosed with a birth injury.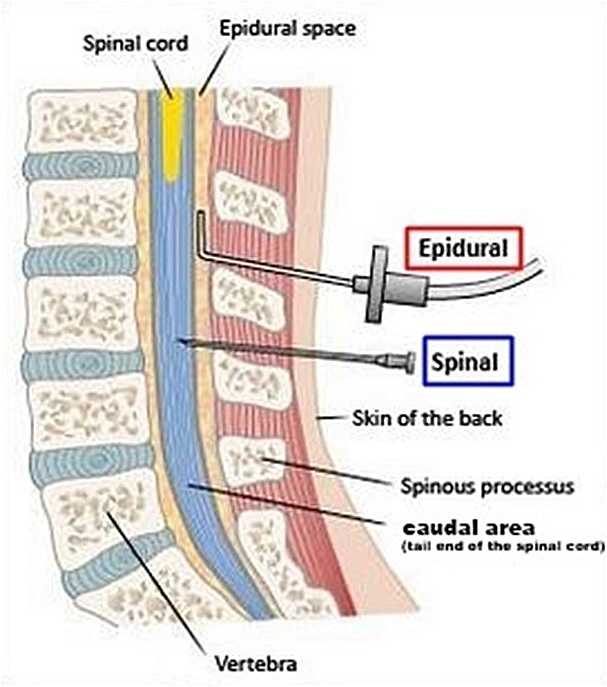 The reason for this has nothing to do with the medications used in epidurals. Although any drug given to the mother during labor also gets into the baby's system, the anesthetics used with epidurals do not cause any harm to the baby. The primary reason why getting an epidural creates a somewhat higher risk of a birth injury is that epidurals tend to slow down the birth process. Vaginal delivery of a baby and accomplished through muscle contractions and pushing by the mother. Getting an epidural makes the muscles and lower body go numb making pushing less effective. The effect of an epidural on pushing is comparable to eating or drinking right after the dentist has numbed your mouth for a cavity. You have less sensation and control over the area of the mouth that is numb making it difficult to chew and drink like normal. By numbing the mother's lower body, an epidural makes it more difficult to efficiently push the baby out.
The reason for this has nothing to do with the medications used in epidurals. Although any drug given to the mother during labor also gets into the baby's system, the anesthetics used with epidurals do not cause any harm to the baby. The primary reason why getting an epidural creates a somewhat higher risk of a birth injury is that epidurals tend to slow down the birth process. Vaginal delivery of a baby and accomplished through muscle contractions and pushing by the mother. Getting an epidural makes the muscles and lower body go numb making pushing less effective. The effect of an epidural on pushing is comparable to eating or drinking right after the dentist has numbed your mouth for a cavity. You have less sensation and control over the area of the mouth that is numb making it difficult to chew and drink like normal. By numbing the mother's lower body, an epidural makes it more difficult to efficiently push the baby out.
Anything that prolongs or delays the vaginal childbirth process will automatically increase the potential risk of a birth injury.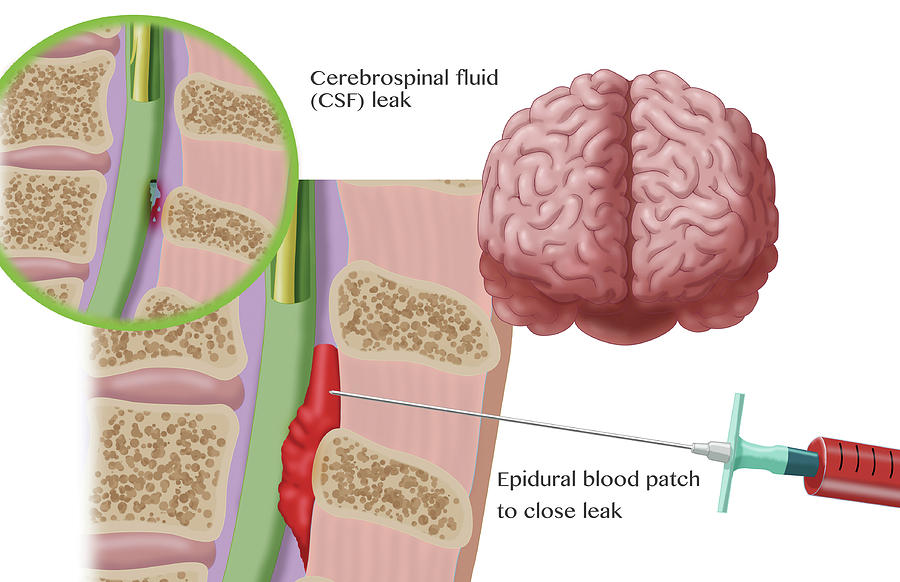 The process of labor and delivery is highly stressful for the baby. The longer a delivery drags on the more risky it become for the baby. Prolonged labor can subject to the baby to physical distress and creates the risk of oxygen deprivation and brain damage. Moreover, when delivery is not progressing fast enough it might require doctors to intervene and use delivery assistance devices such as forceps or vacuum extractors. When no epidural is given, instrument assisted delivery is necessary less than 10% of the time. However, when the mother gets an epidural the rate of instrument assisted delivery jumps up to 15%. This small increase in the rate of instrument assisted deliveries translates to a significant increase in the risk of birth injury. So while the risk does not jump off the page statistically, it is also silly to suggest that epidurals cannot contribute to birth injuries. The need for mechanical instruments is correlated with birth injuries. If epidurals increase the need for mechanical, it has to follow that they epidurals are the cause of some birth injuries.
The process of labor and delivery is highly stressful for the baby. The longer a delivery drags on the more risky it become for the baby. Prolonged labor can subject to the baby to physical distress and creates the risk of oxygen deprivation and brain damage. Moreover, when delivery is not progressing fast enough it might require doctors to intervene and use delivery assistance devices such as forceps or vacuum extractors. When no epidural is given, instrument assisted delivery is necessary less than 10% of the time. However, when the mother gets an epidural the rate of instrument assisted delivery jumps up to 15%. This small increase in the rate of instrument assisted deliveries translates to a significant increase in the risk of birth injury. So while the risk does not jump off the page statistically, it is also silly to suggest that epidurals cannot contribute to birth injuries. The need for mechanical instruments is correlated with birth injuries. If epidurals increase the need for mechanical, it has to follow that they epidurals are the cause of some birth injuries.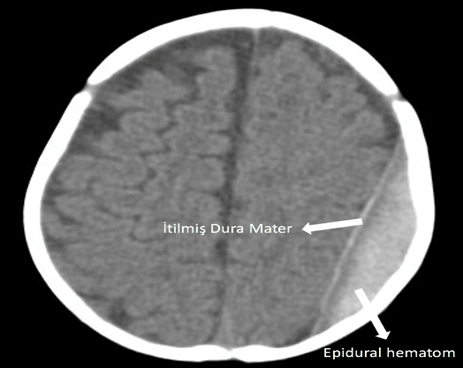
- Pros and cons of epidurals
- Other medications that cause birth injuries
Pregnancy and birth: Epidurals and painkillers for labor pain relief - InformedHealth.org
Created: March 3, 2006; Last Update: March 22, 2018; Next update: 2021.
During pregnancy, many women think about how they will be able to cope with labor pain during the birth. Some women would rather avoid medication. Others feel reassured knowing that there are effective ways to relieve the pain. Many decide to have an epidural.
Knowing that their partner, friend or another person close to them will offer encouragement and support during the birthing process can often already help women cope with labor pain. Non-medication approaches such as walking, breathing exercises, heat packs or relaxation techniques can also help to make it a little easier to bear the pain.
Hospitals also offer medications for pain relief. They effectively relieve pain, while still making it possible for the woman to be awake to experience the birth.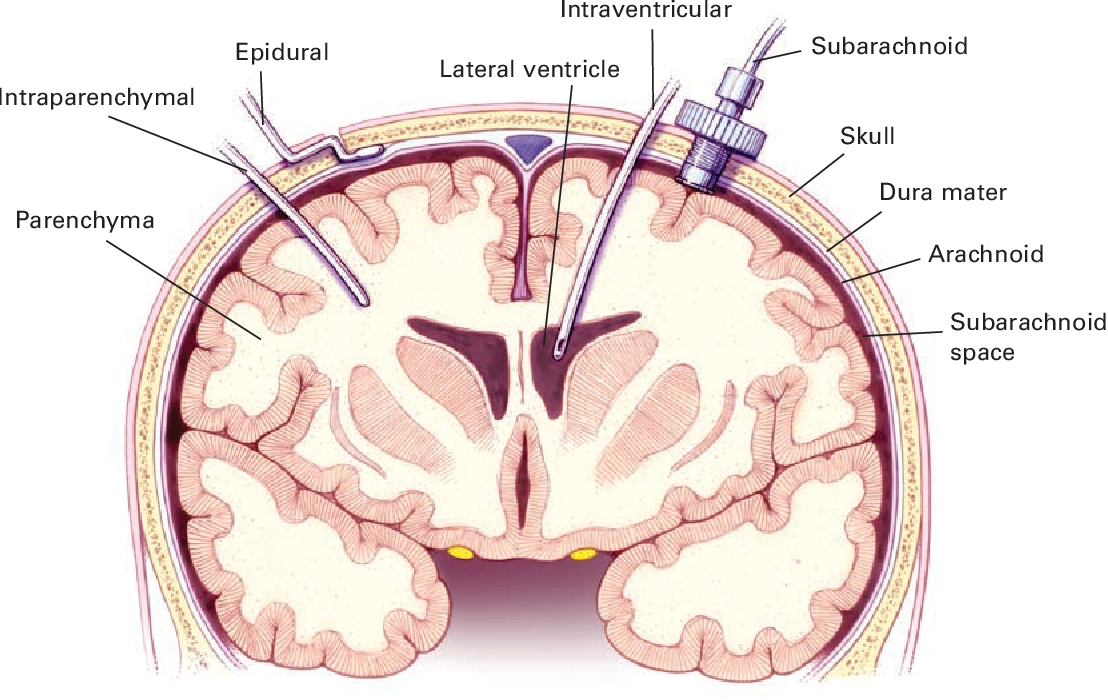 Normally, several alternatives are available to expecting mothers. The most effective is a type of local anesthetic known as an epidural. Epidurals are the most popular form of medication-based pain relief in childbirth.
Normally, several alternatives are available to expecting mothers. The most effective is a type of local anesthetic known as an epidural. Epidurals are the most popular form of medication-based pain relief in childbirth.
What is an epidural?
An epidural is a way to deliver an anesthetic so that it stops pain signals traveling from the spine to the brain. It involves injecting a small amount of anesthetic into the epidural space of the spine. The epidural space is filled with fluid and surrounds the spinal cord. Nerves that carry pain signals from the body to the brain (spinal nerves) connect to the spinal cord in certain places. The anesthetic numbs the spinal nerves, blocking the pain signals. Epidurals can't be used in women who are allergic to anesthetics or have blood clotting problems.
During labor, the medication is injected into the lumbar area, which is the lower part of the spine. If it works properly, you will no longer feel pain in the lower part of your body. But with a low dose you are still able to move your legs, or even get up and walk around with a bit of help. An epidural can also be used for partial anesthesia if the woman needs to have a Cesarean section.
But with a low dose you are still able to move your legs, or even get up and walk around with a bit of help. An epidural can also be used for partial anesthesia if the woman needs to have a Cesarean section.
Because a single injection is often not enough to last throughout the entire birth, a catheter is usually put in and then attached to the woman’s back. This thin plastic tube is pushed forward into the epidural space using a special needle. It can be used to inject more anesthetic or painkiller as needed. Doctors often do this by hand, or the catheter may be attached to a small pump that continuously supplies small amounts. Sometimes there is a patient-controlled pump. This means that you can give yourself more medication if you need it.
When epidurals are used, a small tube (cannula) is usually put into the woman’s arm as well, so that a drip can be attached to it. This is a safety precaution, for instance because your blood pressure might drop rapidly during an epidural. The cannula can then be used to very quickly supply the right drug to help increase blood pressure.
The cannula can then be used to very quickly supply the right drug to help increase blood pressure.
The dose of the anesthetic is usually increased gradually to avoid injecting too much at once. Pain relief is typically felt about 10 to 20 minutes later. It sometimes takes a while for anesthetists to get the injection in exactly the right place in the back, or they may not manage to do so at all.
How effective are epidurals?
Epidurals are very effective and can almost always relieve pain better than other medications. Most women who have an epidural feel little or no pain. About 1 out of 100 women need additional painkillers if they have an epidural. To give you an idea of what this means: About 28 out of 100 women need additional painkillers during labor if other pain relief options (not an epidural) were used first.
What are the side effects of epidurals?
An epidural can be used to deliver different types of local anesthetic, which also differ in the side effects that they cause. Some medications may cause itching. If that happens, changing the medication could solve the problem. The anesthetist will explain things in detail beforehand. Common side effects include:
Some medications may cause itching. If that happens, changing the medication could solve the problem. The anesthetist will explain things in detail beforehand. Common side effects include:
Low blood pressure: In about 14 out of 100 women, the epidural causes blood pressure to drop, which can lead to dizziness or nausea.
Fever: Epidurals cause fever in about 23 out of 100 women. By comparison, this is only the case in about 7 out of 100 women who use another type of pain management.
Problems urinating: Epidurals can make it hard to urinate too. You might need a urinary catheter to help you urinate during the epidural. Roughly 15 out of 100 women have problems urinating because of the epidural.
Epidurals can also cause numbness or tingling in the legs. If the injection goes too deep, it might make a hole in the protective layers (dura) around the spinal cord, and spinal fluid might leak out. If too much fluid is lost, it can cause severe headaches that may last up to a few days.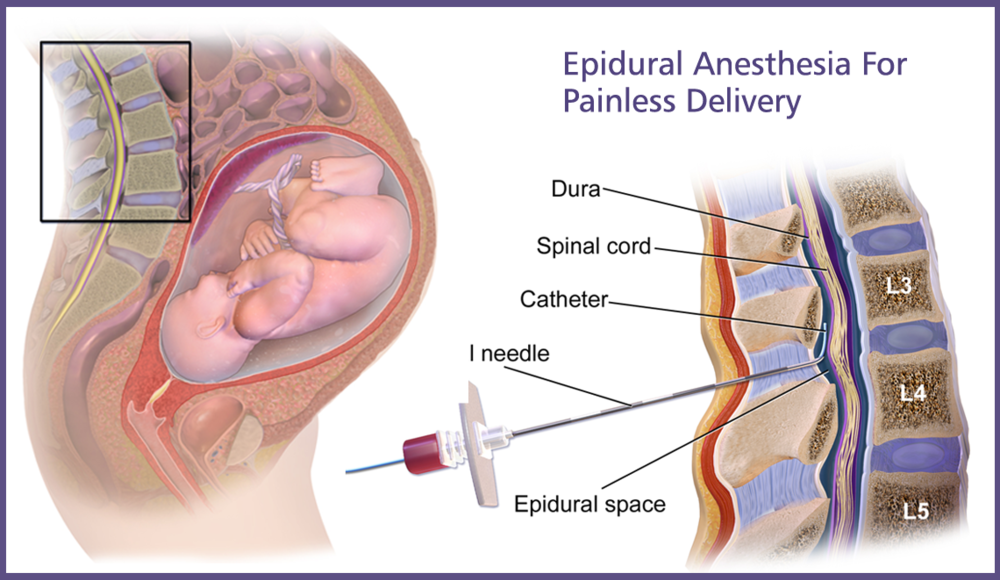 This happens in about 1 out of 100 women who have an epidural. Women who had an epidural were not generally more likely to have headaches than women who used other forms of pain relief during labor.
This happens in about 1 out of 100 women who have an epidural. Women who had an epidural were not generally more likely to have headaches than women who used other forms of pain relief during labor.
Some women are worried that epidurals might cause long-lasting back pain. But according to current knowledge, back pain isn't more common in women who had an epidural during labor than in women who used other painkillers.
How does the epidural affect the baby? Does it change the course of the birth?
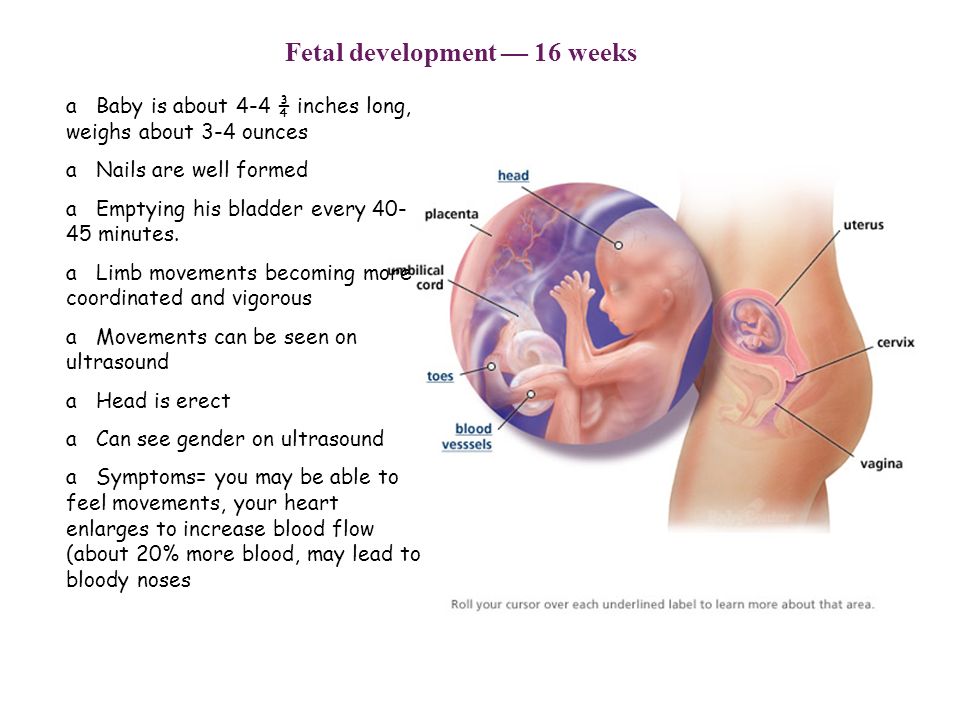
Any medication that a woman uses during labor enters the child’s body as well, through the umbilical cord. This includes painkillers and anesthetics delivered through epidurals. But anesthetics don't have a stronger effect on the baby than other painkillers that might be considered for use during childbirth. Epidurals have no known long-term disadvantages. One difference, though, is that births take a bit longer on average in women who have epidurals. That could be because some babies take a longer time to move into the right position when an epidural is used.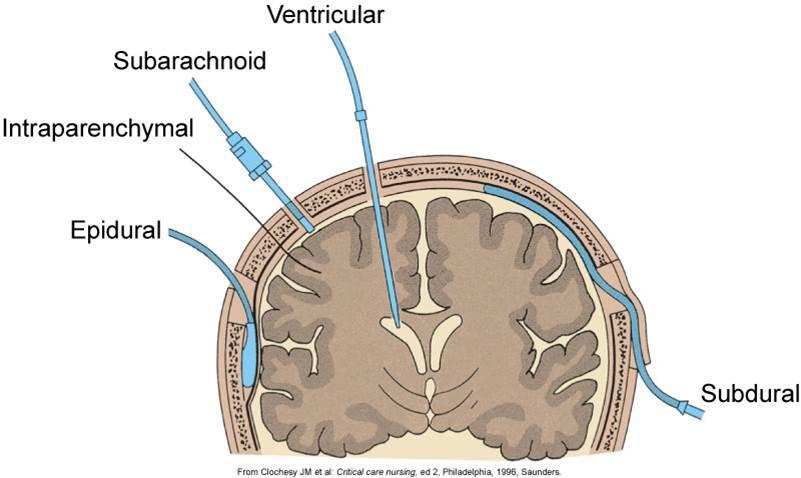
When women have an epidural, their baby is more likely to need to be delivered with the help of instruments that use vacuum suction (a “ventouse” delivery) or forceps. These are known as assisted or instrumental deliveries.
About 10 out of 100 women who don't have an epidural need an instrumental delivery, compared to
about 14 out of 100 women who have an epidural.
Before a child can be born using a vacuum delivery or forceps, an episiotomy (cut made in the back of the vagina) is usually necessary, which then needs to be stitched.
Some women still feel the desire to push despite having an epidural. But because the epidural means they can't feel when it is time to push, doctors and midwives need to let them know when they should start pushing.
Can you stand up if you have an epidural?
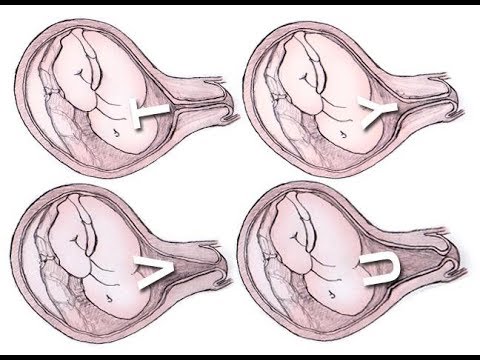
The epidural can be set at a dose that is low enough for the woman to get up and walk around during the first phase of labor. In this early part of labor, the cervix (opening of the womb) becomes shorter and opens fully. This is called full dilation. Walking around is supposed to help make the birth easier. But studies that compared women who walked around with women who remained lying down during an epidural found that this made no difference to the birth.
This is called full dilation. Walking around is supposed to help make the birth easier. But studies that compared women who walked around with women who remained lying down during an epidural found that this made no difference to the birth.
During the second phase of labor, when the baby is pushed out, women are sometimes advised to sit up a bit more, for instance by adjusting the head of the bed or leaning on their partner. It's not known whether this really affects the course of the birth, so it's best for the woman to choose the position that feels most comfortable.
Do epidurals make Cesarean sections more likely?
Epidurals do not increase the chances of needing a Cesarean section. However, if a woman needs to have a Cesarean section, a higher-dose epidural can be used instead of a general anesthetic. This means that she can be awake to experience the birth of her child. A curtain is placed in front of the woman’s belly during the Cesarean section so that neither she nor her partner, who is sitting next to her, can see the procedure.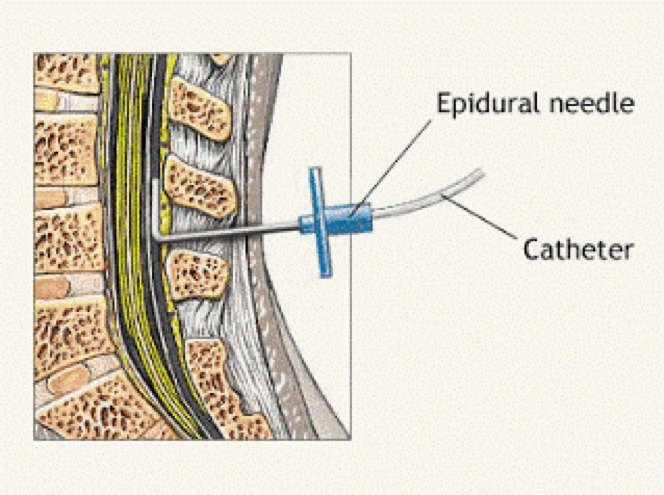 She can remain awake enough to be able to take her baby in her arms immediately after the operation.
She can remain awake enough to be able to take her baby in her arms immediately after the operation.
Spinal and pudendal nerve blocks
Spinal anesthesia works in a similar way to epidurals, but the anesthetic is injected even closer to the spinal cord: into an area called the subarachnoid space. This causes the entire lower half of the body to feel numb. Spinal anesthesia, also known as a spinal block, has a faster effect than an epidural. For this reason, it's used if a Cesarean section needs to be done but it's too late to start an epidural.
It's also possible to combine a spinal block and an epidural. But it's not clear if this has major advantages or disadvantages compared with just an epidural. The combination means that the pain-relieving effect starts faster, but it's also more likely to cause itching.
Something known as a pudendal nerve block can be performed during the second phase of labor, when the baby is pushed out. This involves injecting an anesthetic into the vaginal and perineal tissue (the tissue between the vagina and the anus). But this is usually not done unless the birth isn't progressing properly, and the child needs to be delivered with the help of a suction cup or forceps.
But this is usually not done unless the birth isn't progressing properly, and the child needs to be delivered with the help of a suction cup or forceps.
How effective are painkillers?
Painkillers can also be injected directly into the bloodstream or inhaled (breathed in). These affect the woman’s whole body, not just her abdomen. One advantage over local anesthetics is that a catheter isn't needed. But painkillers aren't as reliable as epidurals, and some also have more side effects.
Opioids
Opioids can be injected into muscle tissue or “dripped” into the bloodstream using an infusion (a drip). Although opioids don't offer as much pain relief as epidurals when they are used in this way, they can help in some women. But studies show that as many as two thirds of women who are given opioids still have moderate to severe pain one or two hours later. Possible side effects include a drop in blood pressure, nausea, vomiting and drowsiness. The higher the dose, the more likely it is that the woman will experience side effects.
Opioids can sometimes affect the baby’s breathing after birth. Then the baby may be given a drug called an opioid antagonist to counteract this effect. The mother may be given this drug too. But opioid antagonists not only reduce the side effects of the opioid; they also reduce the pain-relieving effects.
Laughing gas ("gas and air")
Inhaling painkillers through a mask used to be a common and popular way to relieve labor pain in Germany. Laughing gas (nitrous oxide) was generally used for this purpose. It was given together with oxygen – a combination known as “gas and air.” Although this approach is still common in some other countries, it is very rarely used in Germany nowadays because it's not as reliable as other pain-relieving drugs. One advantage, though, is that women can regulate how much of it they breathe in. Laughing gas has a rapid effect, but it also wears off quickly. It may cause nausea, vomiting, drowsiness or dizziness. There are no known side effects for the baby, but more research is being done in this area.
Further options
Other medications like acetaminophen (paracetamol), non-steroidal anti-inflammatory drugs (NSAIDs) or sedatives are rarely used to treat labor pain. Compared with the other available options, they aren't very effective.
Sources
Anim-Somuah M, Smyth R, Jones L. Epidural versus non-epidural or no analgesia in labour. Cochrane Database Syst Rev 2011; (12): CD000331. [PubMed: 22161362]
Kibuka M, Thornton JG. Position in the second stage of labour for women with epidural anaesthesia. Cochrane Database Syst Rev 2017; (2): CD008070. [PMC free article: PMC6464234] [PubMed: 28231607]
Klomp T, van Poppel M, Jones L, Lazet J, Di Nisio M, Lagro-Janssen ALM. Inhaled analgesia for pain management in labour. Cochrane Database Syst Rev 2012; (9): CD009351. [PubMed: 22972140]
Lawrence A, Lewis L, Hofmeyr GJ, Styles C. Maternal positions and mobility during first stage labour. Cochrane Database Syst Rev 2013; (10): CD003934.
 [PubMed: 24105444]
[PubMed: 24105444]Likis FE, Andrews JC, Collins MR, Lewis RM, Seroogy JJ, Starr SA et al. Nitrous oxide for the management of labor pain. August 2012. (AHRQ Comparative Effectiveness Reviews; Band 67).
Othman M, Jones L, Neilson JP. Non-opioid drugs for pain management in labour. Cochrane Database Syst Rev 2012; (7): CD009223. [PubMed: 22786524]
Simmons SW, Taghizadeh N, Dennis AT, Hughes D, Cyna AM. Combined spinal-epidural versus epidural analgesia in labour. Cochrane Database Syst Rev 2012; (10): CD003401. [PMC free article: PMC7154384] [PubMed: 23076897]
Ullman R, Smith LA, Burns E, Mori R, Dowswell T. Parenteral opioids for maternal pain relief in labour. Cochrane Database Syst Rev 2010; (9): CD007396. [PMC free article: PMC4233118] [PubMed: 20824859]
Wang K, Cao L, Deng Q, Sun LQ, Gu TY, Song J et al. The effects of epidural/spinal opioids in labour analgesia on neonatal outcomes: a meta-analysis of randomized controlled trials.
 Can J Anaesth 2014; 61(8): 695-709. [PubMed: 25011701]
Can J Anaesth 2014; 61(8): 695-709. [PubMed: 25011701]IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
all “for” and “against” / “Waiting for a baby”
Olesya Butuzova
Any pregnant woman is waiting for childbirth - the long-awaited moment of meeting her baby.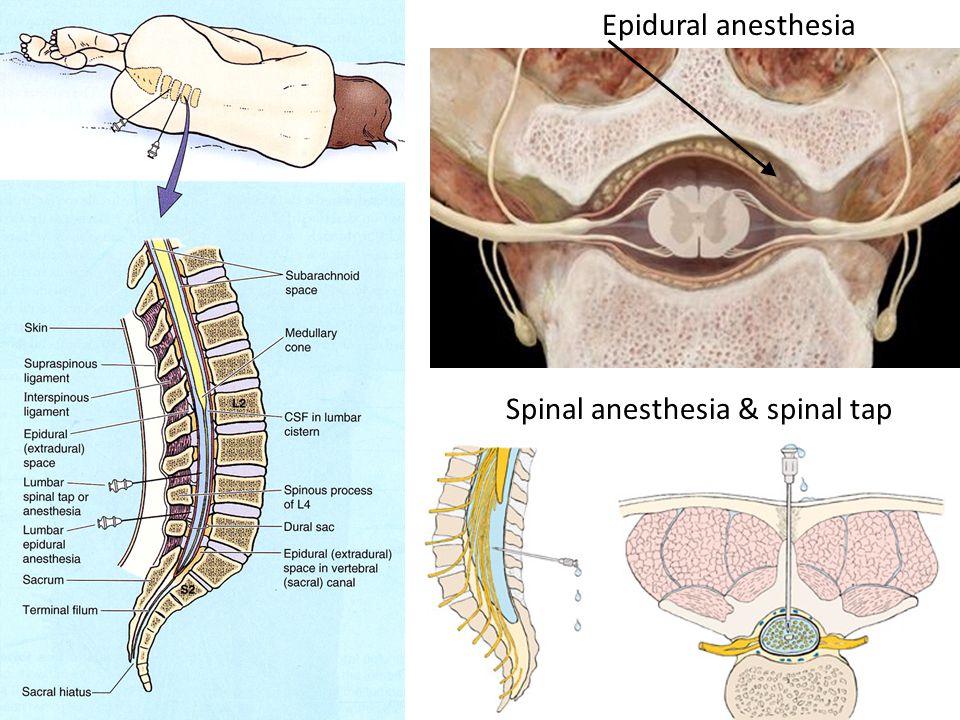 However, many also experience a contradictory feeling - fear. As a rule, most women who have heard enough stories of "experienced" girlfriends are afraid of pain. That is why a modern pregnant woman thinks not only about the name for the future crumbs, but also about ... pain relief. The most common and, perhaps, the favorite method of pain relief during childbirth is currently epidural anesthesia.
However, many also experience a contradictory feeling - fear. As a rule, most women who have heard enough stories of "experienced" girlfriends are afraid of pain. That is why a modern pregnant woman thinks not only about the name for the future crumbs, but also about ... pain relief. The most common and, perhaps, the favorite method of pain relief during childbirth is currently epidural anesthesia.
The essence of this pain relief technique is to inject a local anesthetic under the dura mater of the spinal cord, where the roots of the spinal nerves pass. By "stunning" them, you can save the pregnant woman from pain.
Why is epidural anesthesia good?
Epidural anesthesia is not in vain so popular among both obstetrician-gynecologists and women in labor. It eliminates the pain and gives the woman the opportunity to rest. With a small injection of the drug, the woman in labor can move independently without experiencing discomfort. During the caesarean section, the mother is conscious and does not miss the wonderful moment of the first meeting with the baby.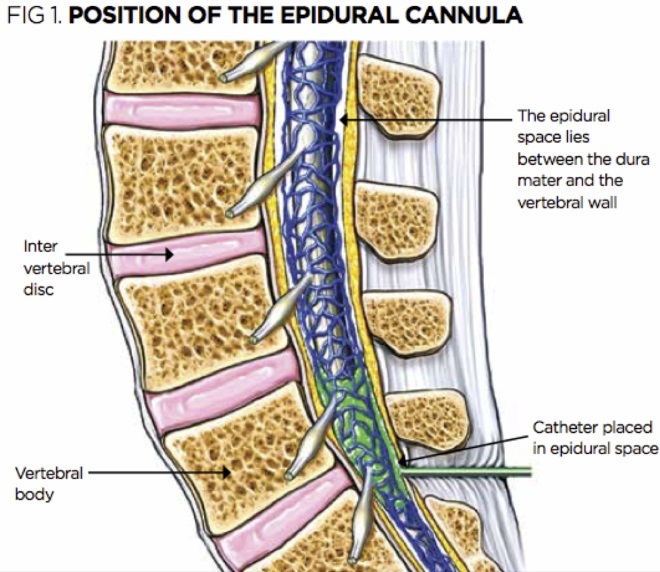
As a rule, the administration of the drug is carried out in doses, it comes directly to the destination - to the nerve roots, therefore, the dosages are minimal. All this allows the liver to quickly cleanse the blood and dispose of the remnants without missing the medicine to the baby. Thus, epidural anesthesia is practically safe for the baby.
Only pain relief?
Initially, the purpose of epidural anesthesia was not to facilitate the process of childbirth for mothers, but to stop certain threatening conditions.
- Thus, epidural anesthesia has a number of beneficial effects:
- Eases the pain of childbirth and gives the woman the opportunity to rest and gain strength for the important period of attempts.
- Reduces high blood pressure, hyperventilation of the lungs and adrenaline levels, which has a calming effect on the body. Epidural anesthesia facilitates the opening of the cervix and reduces trauma during preterm labor, coordinates contractions and the work of the muscles of the uterus.

- And, most importantly, such pain relief is much safer than using intravenous drugs.
How is the procedure carried out?
In order to puncture, the doctor must first position the pregnant woman correctly (which can be difficult with painful contractions). It is recommended that the woman in labor sit on a chair, facing the back or lie on her side, curled up.
The puncture site is carefully cleaned with antiseptic solutions to minimize the risk of infection.
The skin and subcutaneous tissue are punctured with a local anesthetic to numb the insertion of a needle under the dura mater of the spinal cord.
With a special needle, the doctor enters the epidural space and passes a catheter through it, through which the drug is delivered.
Medical indications for epidural anesthesia:
- Caesarean section.
- Diseases of the heart, including defects, - the load on the heart decreases.
- Diseases of the kidneys.
- Diabetes mellitus.
- High blood pressure. Epidural anesthesia helps to reduce it.
- Preterm pregnancy. Epidural anesthesia helps to relax the muscles of the pelvic floor and reduce the resistance exerted by the baby's head. The baby comes out smoothly and gently.
- Discoordination of labor - a condition in which contractions become irregular, frequent, painful and unproductive. They exhaust a woman, but do not contribute to the birth of a child. Epidural anesthesia puts in order the tone of the uterus and muscle contractions, thereby coordinating labor activity.
But epidurals are not for everyone. There is a whole list of contraindications to such anesthesia.
Our expert
Alla Misyutina, doctor of the INVITRO Medical Offices Department
. However, epidural anesthesia is one of the preferred methods of anesthesia in obstetrics.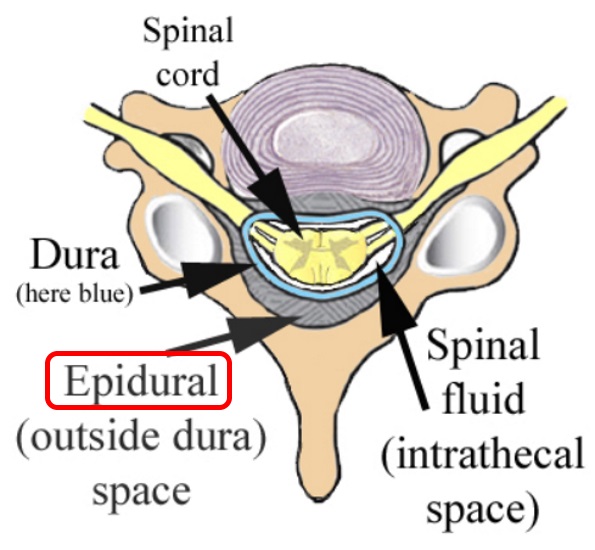 The onset of action of this pain relief is gradual and slow. Pain relief usually develops 10-20 minutes after epidural administration and may be continued until the end of labor as additional doses of drugs can be administered through the epidural catheter. After childbirth, the catheter is removed and after a few hours all sensations return to normal. Anesthesia involves a complete blockage of sensations and movements, it is used more often during a caesarean section.
The onset of action of this pain relief is gradual and slow. Pain relief usually develops 10-20 minutes after epidural administration and may be continued until the end of labor as additional doses of drugs can be administered through the epidural catheter. After childbirth, the catheter is removed and after a few hours all sensations return to normal. Anesthesia involves a complete blockage of sensations and movements, it is used more often during a caesarean section.
Epidural analgesia is sometimes performed during childbirth, with the help of which only painful sensations are removed. Then the nerves responsible for motor functions remain partially in working order, and if desired, the woman can move - roll over, sit down, stand. Contractions become painless and are felt by the woman in labor only as pressure below, on the rectum. With a competent approach of doctors - gynecologists and anesthesiologists - the risk is minimal. Obstetrician-gynecologists widely promote this type of pain relief, and many women easily agree to its use.
About side effects
But, like any other useful medical manipulation, epidural anesthesia is not without side effects.
The most common is lowering blood pressure. This is fraught with impaired placental blood flow and hypoxia, that is, oxygen starvation in the baby.
The second serious reaction may be allergic. To prevent anaphylactic shock at the beginning of the procedure, a trial administration of the drug is carried out. If the woman in labor felt pain, burning or itching in the puncture area, then the doctors “cover up” the anesthesia with antiallergic drugs.
When pierced, the drug may enter the spinal canal, which is fraught with difficulty breathing and a drop in blood pressure. It is also possible to injure the roots of the spinal nerves and pain in the limbs. When the drug is injected under the dura mater of the spinal cord, there is a risk of getting into the epidural veins. In such cases, severe complications develop - a sharp drop in blood pressure, heart rhythm disturbance and dizziness.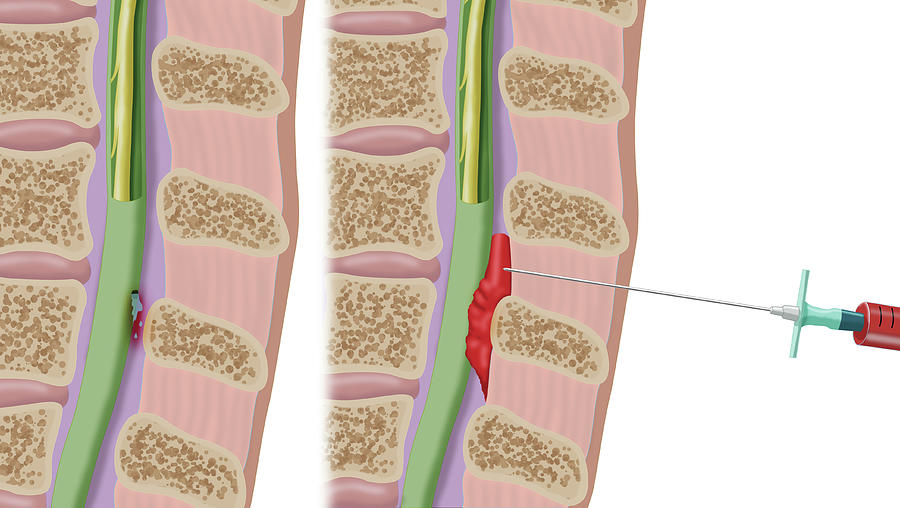 Often this situation is accompanied by numbness of the tongue.
Often this situation is accompanied by numbness of the tongue.
Bacteria entering the puncture site can lead to meningitis.
If the dura mater is damaged and, as a result, cerebrospinal fluid enters the epidural space, headache may occur. It appears a few days after childbirth and can last up to a month and a half.
With regard to side effects on the part of the child, this may be respiratory depression, dysmotility, difficulty sucking.
However, I would like to note that according to statistics, all these complications are rare.
Thus, epidural anesthesia is an effective way of pain relief during childbirth, helping the mother to gain strength before meeting the baby. As well as a medical procedure that eliminates a number of complications during childbirth. Although whether to use epidural anesthesia, if there is no indication for it, is, of course, up to you to decide.
List of contraindications for epidural anesthesia:
- High intracranial pressure.
- Low blood pressure (below 100 mmHg).
- Curvature of the spine.
- Unconscious state of a woman in labor.
- Sepsis.
- Bleeding or bleeding disorder.
- Serious neurological or mental illness of the woman in labor.
- Allergy to drugs used for epidural anesthesia.
harm or benefit • Bee
How justified is the use of anesthesia in the most important process for women - childbirth? Approximately 50% of women in labor today use epidural anesthesia. Can it be done by all women who want to avoid pain during childbirth? Is it safe for mother and baby? With such questions, we turned to our experts - obstetrician-gynecologist Elena Matiyak and neonatologist Vasilisa Avramenko.
Epidural anesthesia - pain relief in which a drug is injected through a catheter into the epidural space of the spine, blocking the transmission of impulses along the peripheral nerves.In Russia, lidocaine, bupivacaine, ropivacaine are administered.
Nature has provided its own pain relief mechanisms - the release of endorphins in the body to avoid pain shock. But the fear of pain is one of the biggest fears of pregnant women, especially primiparas. Much of this fear stems from a lack of information. Or, conversely, an overabundance of conflicting information, especially negative.
"Fear - pain - spasm - pain - fear" - this is how the French obstetrician Michel Auden describes this "vicious circle". Fear is one of the important factors in the occurrence of pain in childbirth, if there are no other physical causes for it.
It is very important to mentally prepare a woman during pregnancy, to tell her about the birth process, to calm her down, to set her up to the fact that this is a natural process that is controlled by the body itself. If the expectant mother is at home in a stressful environment, then this can then come back to haunt painful childbirth, discoordination of labor activity. Ideally, loved ones should create favorable conditions for the woman, and the husband, if possible, should be with her in childbirth.
Ideally, loved ones should create favorable conditions for the woman, and the husband, if possible, should be with her in childbirth.
Experts say that any support during childbirth helps to experience pain - whether it be a husband, sister, doula, personal midwife. If a woman is with a person she trusts, this strengthens her faith in herself, and therefore reduces her need for pain relief. More often, pain relief is requested by those who are in childbirth alone, especially often - primiparous.
Elena Macyak: “Today, maternity hospitals are returning to the tactics of conducting natural childbirth without the use of epidural anesthesia. Anesthesia is carried out only if there is evidence for this: an increase in pressure in a woman in labor, discoordination of labor (strong uterine contractions in the absence of cervical dilatation), a very low pain threshold. Without special need, no one will anesthetize a woman in labor, especially a primiparous, even if she asks” .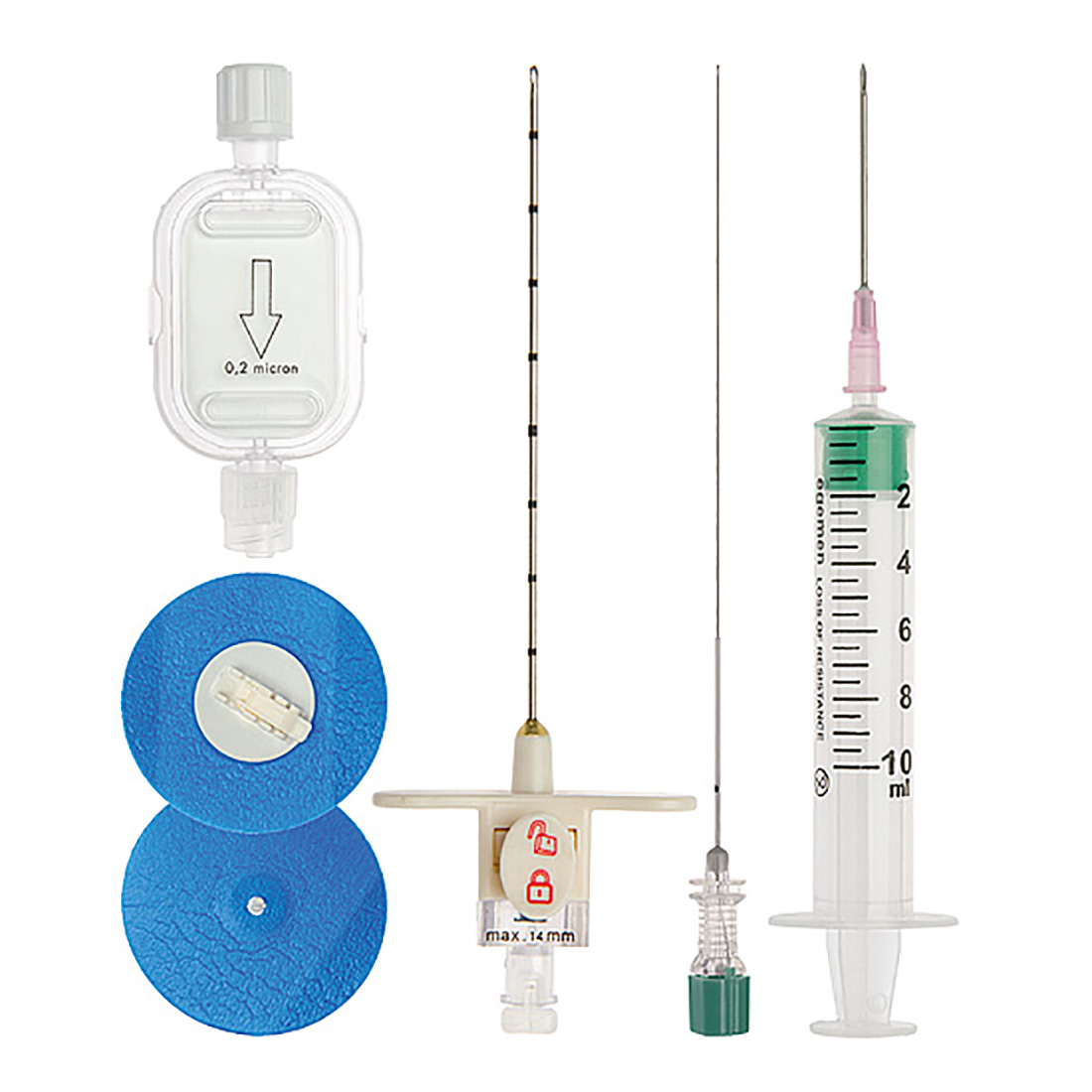
It is important to take into account the period of childbirth, the most optimal is when the dilatation is 5-6 cm. In any case, childbirth is an individual process, and the final decision on the use of epidural anesthesia is made by the obstetrician-gynecologist together with the anesthesiologist, based on the condition of the woman in labor and the child. And it is carried out with the obligatory consideration of the results of the electrotocogram.
In fact, epidural anesthesia, like any other medical procedure, has its contraindications .
On the part of the mother these are blood diseases accompanied by clotting disorders, diseases of the red bone marrow, severe liver pathology, pustular rashes at the site of the proposed catheter insertion, individual intolerance to drugs used for anesthesia, diseases of the nervous system, pathology of the spine, the risk of postpartum bleeding, pathology of placental attachment and others.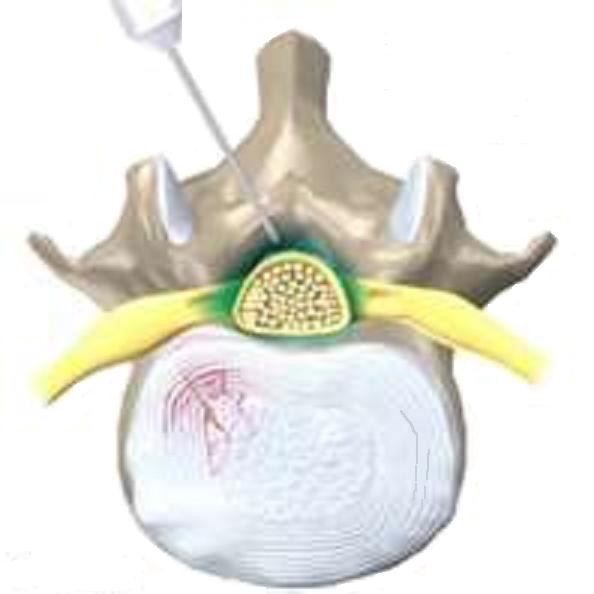
On the part of the child — large fetus, discrepancy between the size of the fetus and the size of the woman's pelvis, poor electrotocogram readings.
As with any medical procedure, epidural anesthesia is associated with certain risks .
Violation of technique (needle entry into the subarachnoid or spinal space, damage to the spinal cord), incorrect dosage of the drug can lead to paralysis of the lower extremities, lethargy of the nervous system, respiratory disorders, palpitations. But these risks in modern conditions are minimized, since the manipulation is carried out by qualified specialists who act according to an officially approved protocol and use a technique for checking the location of the needle (the so-called “loss of resistance” technique).
Possible individual reactions to pain relief - nausea, vomiting, dizziness, decreased pressure, back pain, headache. If an allergy to an anesthetic is detected for the first time during the manipulation, then there is a high probability of developing allergic reactions of varying severity, including anaphylactic shock.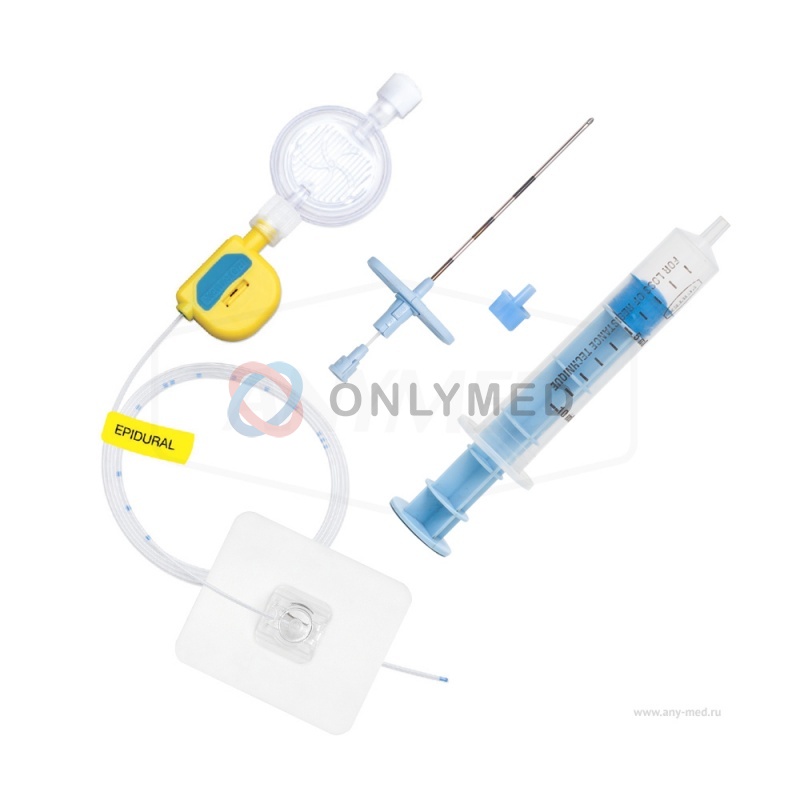
Epidural anesthesia may also affect the course of the birth process.
Elena Macyak: “During the action of epidural anesthesia, a woman often does not take an active part in childbirth, and therefore certain problems arise, especially for primiparas, who say: “I don’t know how to behave, I don’t feel my body.” In this case, it is necessary that the doctor, the midwife suggest how and what to do so that the child is born safely” .
Vasilisa Avramenko: "If the birth is not the first one, then we must take into account what happened in the first birth - for example, secondary weakness of labor that develops against the background of epidural anesthesia" .
Scientific studies have shown that epidural anesthesia often leads to an increase in the time of the second stage of labor. The frequency of the use of oxytocin (that is, rhodostimulation) is increasing due to the weakness of labor activity.
Epidural anesthesia may affect uterine contractility in the third stage of labor. As a result, the development of hypotension of the uterus and the occurrence of bleeding are possible. This requires urgent action by the doctor and further postpartum treatment of the woman in labor.
As a result, the development of hypotension of the uterus and the occurrence of bleeding are possible. This requires urgent action by the doctor and further postpartum treatment of the woman in labor.
Vasilisa Avramenko: “In my practice, there were cases when the risks associated with epidural anesthesia manifested themselves. Among them is the weakness of labor activity, the lengthening of the process of passage of the fetus through the birth canal. They help with the introduction of oxytocin, and sometimes you have to apply a vacuum extractor. In response to this, the child seems to get tired in childbirth, he needs more time to adapt to independent living. He may be more lethargic or, conversely, more agitated after birth, have a temporary circulatory disorder due to spasm of skin vessels " .
In some cases, due to the lengthening of the birth process, the child develops hypoxia, he defecates meconium (the name of the first stool accumulated during 9 months of pregnancy) before birth into the amniotic fluid, and they turn green.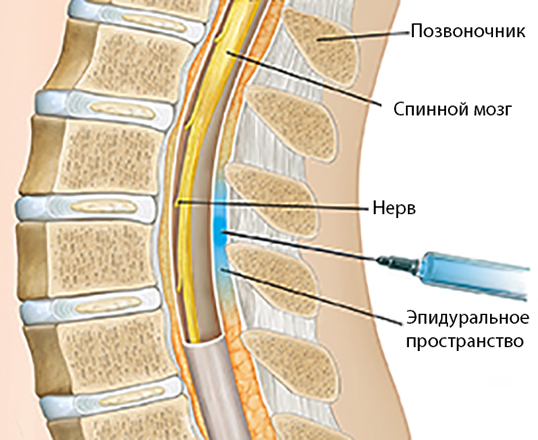 Sometimes these children require observation in the neonatal intensive care unit.
Sometimes these children require observation in the neonatal intensive care unit.
If we talk about the delayed effect of epidural anesthesia, then the results of a number of studies indicate a slowdown in the flow of milk in the mother. Although, according to the international database, the drugs used for epidural anesthesia themselves are compatible with breastfeeding and are quickly excreted from the mother's body (in about 2-4 hours).
According to scientific studies, there is no direct relationship between the frequency of caesarean sections and the use of epidural anesthesia. After all, caesarean section as a special method of delivery is possible only if there are certain indications. In any case, the decision is made by the council, based on the condition of the woman and the fetus.
Vasilisa Avramenko: “Out of control maternal pain stress can lead to a decrease in oxygen in the blood due to excessive production of stress hormones (adrenaline, cortisol) and, consequently, to hypoxia in the child.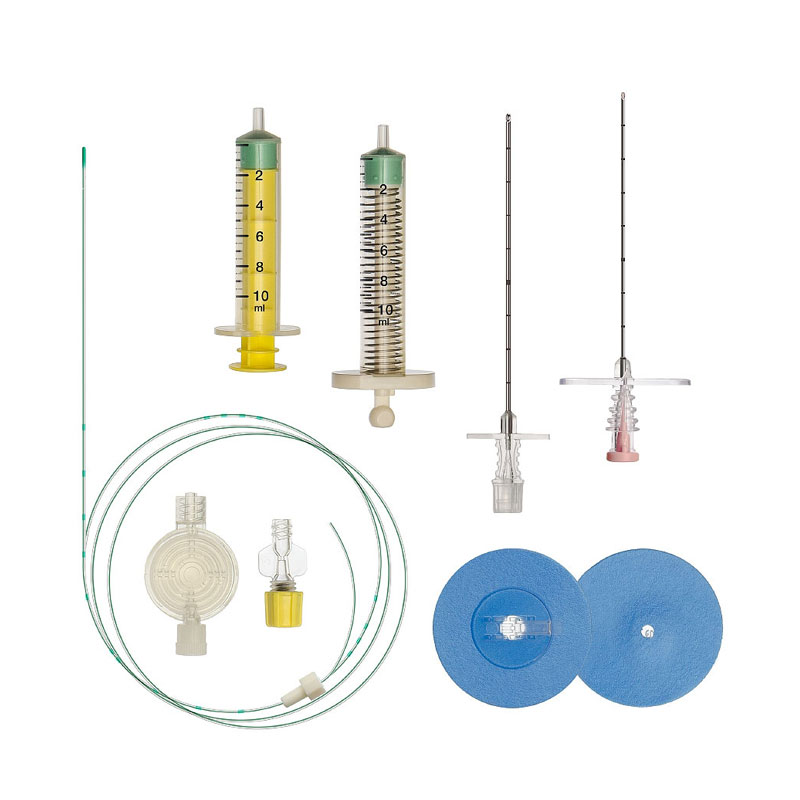 As a result, difficult childbirth (long, painful or with a poor outcome), which will require not only physical, but also psychological rehabilitation of the woman. In this case, pain relief can provide comfort for the woman, reduce emotional and hormonal stress for the mother, and hence for the child.0146 .
As a result, difficult childbirth (long, painful or with a poor outcome), which will require not only physical, but also psychological rehabilitation of the woman. In this case, pain relief can provide comfort for the woman, reduce emotional and hormonal stress for the mother, and hence for the child.0146 .
Pain causes an increase in heart rate and an increase in the sympathetic nervous system, so if you have heart disease or dystonia, epidural anesthesia can also be useful.
Epidural anesthesia in combination with spinal anesthesia is effective, for example, in planned operative delivery in patients with placenta accreta. Also, the use of epidural analgesia, by reducing pain, helps to set a woman up for natural childbirth after a previous caesarean section.
Vasilisa Avramenko: “The technique of epidural anesthesia is being improved. For example, there is patient-controlled epidural anesthesia (or “mobile”), when a woman is not given an anesthetic drug all the time, but she regulates its administration herself.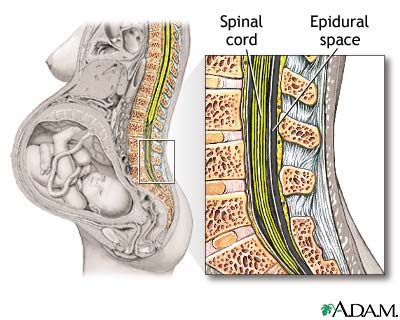 The use of a lower concentration and volume of the drug makes it possible to block the channels of pain perception, and when using "mobile" epidural anesthesia, the sensitivity of the motor nerves is preserved. The woman remains able to walk during anesthesia. I think this is a way out for those who are unable to go through childbirth without support.0146 .
The use of a lower concentration and volume of the drug makes it possible to block the channels of pain perception, and when using "mobile" epidural anesthesia, the sensitivity of the motor nerves is preserved. The woman remains able to walk during anesthesia. I think this is a way out for those who are unable to go through childbirth without support.0146 .
The presence of such an effective and generally safe method in the arsenal of an obstetrician-gynecologist makes it possible to provide assistance to those who need it and for whom it is applicable.
Epidural anesthesia can be used outside of labor as well as paravertebral and spinal anesthesia.
Let's summarize
Epidural anesthesia is a method that can be used during childbirth, taking into account indications and contraindications.
Before using epidural anesthesia, you need to weigh the pros and cons, assess the risks, assess the condition of the fetus.