Can you deliver triplets naturally
Multiple birth - triplets or more
Multiple birth - triplets or more | Pregnancy Birth and Baby beginning of content5-minute read
Listen
If you are pregnant with triplets or more, the birth will need careful planning.
The main risk with carrying multiples is that they will be born prematurely. Your medical team will help you plan your babies' birth. This may include deciding where and when your babies will be born.
Planning for your multiple birth
When you are pregnant with triplets or more, it is important to plan the birth. Your medical team will consider the risks of premature birth. They will weigh this against the risks of continuing the pregnancy for both you and your babies, based on your individual situation.
Generally, the longer your babies can stay in your uterus, the better. But when you are pregnant with triplets or more, complications can often develop. This can often mean that it's better for you and your babies if they are born early.
A normal pregnancy lasts 40 weeks. The average length of a pregnancy for triplets is 32 weeks. For quadruplets, the average length is 30 weeks.
Continuing a multiple pregnancy past 36 weeks can be risky for you and your babies. So, it's usually considered best to deliver them early.
When deciding when and how the babies should be born, your doctor will consider different factors. Your medical team will think about:
- the position of each baby
- the weight of each baby
- your health
- the babies’ health
A caesarean section is usually considered safest when there are 3 or more babies.
Giving birth to triplets or more vaginally is very rare. It is not recommended because of the higher risk of labour complications and infant mortality.
Since almost all triplets or more will be born prematurely, they will need special care. This may include a stay in a neonatal intensive care unit (NICU).
This may include a stay in a neonatal intensive care unit (NICU).
It’s important to plan to have the birth in a hospital with all the facilities that you and your babies will need.
Caesarean section
A caesarean section is usually the safest option when you are carrying 3 or more babies. This may be because of:
- the position of the babies
- the position of the placenta (or placentas)
- the risk of one of the placentas or umbilical cords being compressed during a vaginal birth
- the risk of the babies becoming entangled during a vaginal birth
If you are carrying triplets or more, you will usually be offered a planned caesarean.
If your babies are going to be born early (preterm), your doctor may recommend giving you steroid injections. The injections are given to you before the birth.
Steroids can help develop your babies’ lungs. This can help them breathe more easily after birth. Steroids can also reduce the risk of other problems in babies born preterm.
Multiple babies and preterm labour
If you are expecting multiple babies and you go into labour, contact your doctor or midwife and go to your local hospital emergency department. The signs and symptoms of labour are the same as with normal labour. These include:
- contractions
- sudden breaking of the waters
- a ‘show’
During pregnancy, a plug of mucus seals the cervix. A 'show' is when the plug comes away and out of the vagina.
Women who are pregnant with multiple babies may go into labour naturally before 35 weeks. This happens in around 3 out of 4 cases.
Contact your medical team immediately if you have any signs of preterm labour. It may be possible to slow down or stop the labour. You will most likely be admitted to hospital.
If you go into labour spontaneously, you will likely be given a caesarean after you arrive at hospital.
Babies born before 34 weeks may need help with breathing, feeding and keeping warm. They are at greater risk of complications than babies born at full term.
They are at greater risk of complications than babies born at full term.
The neonatal intensive care unit (NICU) is specialised to care for premature and sick newborn babies. This unit has experienced medical staff and equipment.
When your babies no longer need this high level of care, they may be transferred. They may then spend time in the special care nursery or special care baby unit.
Resources and support
If you are preparing for a multiple birth, there are different organisations you can turn to for information.
The Australian Multiple Birth Association can provide support and resources for families expecting multiple babies.
The Royal Women's Hospital Melbourne offers online education for those expecting a multiple birth.
The Australian Breastfeeding Association can provide information on breastfeeding multiple babies, and link you to services such as lactation consultants.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Available 7am to midnight (AET), 7 days a week.
Sources:
Twin Research Australia (Multiple Perspectives: What support do multiple birth families need to live happy and healthy lives?), Australian Multiple Birth Association (What to expect when you're expecting multiples), Queensland Health (Steroids in pregnancy), Government of Western Australia (Multiple Pregnancy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2022
Back To Top
Related pages
- Twins, triplets and multiples
Need more information?
Multiple pregnancy (triplets or more)
Learning you're pregnant with triplets or more can be a shock, but overall, most parents find having multiple babies to be a positive experience.
Read more on Pregnancy, Birth & Baby website
Types of multiple pregnancy
Multiple pregnancies, including twins, triplets and more, are rare but require lots of support. Find out about different types of multiple pregnancy here.
Read more on Pregnancy, Birth & Baby website
Raising multiple babies
Raising multiple babies - triplets or more - involves planning, hard work, and well designed routines. But with support, raising multiples does get easier.
Read more on Pregnancy, Birth & Baby website
Twins, triplets and multiples
If you are having twins, triplets or more, find out everything you need to know about your pregnancy, the birth, feeding and raising your babies.
Read more on Pregnancy, Birth & Baby website
Feeding multiple babies
Feeding multiple babies, such as triplets or more, can be challenging at first, but even breastfeeding is possible with some expert help.
Read more on Pregnancy, Birth & Baby website
Fraternal twins & identical twins | Raising Children Network
Whether you’re having fraternal twins or identical twins, it’s good to find out during pregnancy. Get the facts you need about different types of twins.
Read more on raisingchildren.net.au website
Twins and multiple births - Better Health Channel
betterhealth.vic.gov.au
Read more on Better Health Channel website
Breastfeeding triplets, quads or more! | Australian Breastfeeding Association
Some mothers find breastfeeding one baby demanding. Breastfeeding three or four or more could be viewed as a definite challenge. But many mothers succeed. Knowing how breastfeeding works will help you understand how it is possible to breastfeed twins, triplets, quads or more.
Breastfeeding three or four or more could be viewed as a definite challenge. But many mothers succeed. Knowing how breastfeeding works will help you understand how it is possible to breastfeed twins, triplets, quads or more.
Read more on Australian Breastfeeding Association website
Breastfeeding twins | Australian Breastfeeding Association
This article is a shortened version of our booklet 'Breastfeeding:twins, triplets and more' in which we have drawn from the experiences of other mothers of twins to put together information and ideas. We hope these will help you deal with the challenges of breastfeeding and parenting your babies.
Read more on Australian Breastfeeding Association website
Vaginal birth after caesarean (VBAC)
If you've delivered a baby by caesarean (C-section), you may have a choice with your next pregnancy - a vaginal birth after caesarean (VBAC) or a planned (elective) caesarean.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.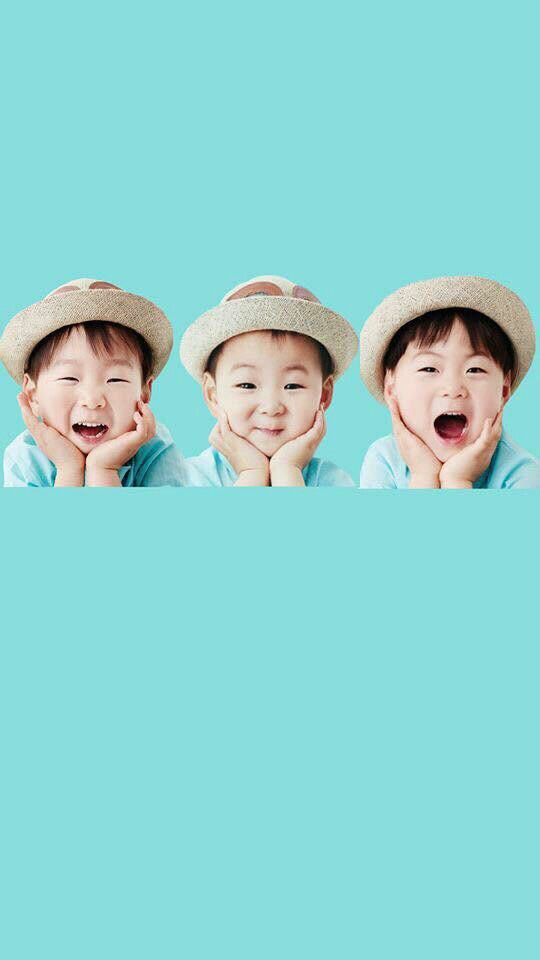
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
vaginally born triplets | AIMS
To read or download this Journal in a magazine format on ISSUU, please click here
AIMS Journal, 2017, Vol 29, No 4
By Rowena Hazell
I had two children, and very much wanted a third child to complete my family. When I finally became pregnant, I started bleeding at about 6 weeks. The bleeding continued, and at 7 weeks I was sent for a scan. I was feeling very sick, which I thought might be a good sign, but the midwife said it might not be. She carefully prepared me that this might be a miscarriage. The sonographer told me that if I was 6 weeks pregnant, we might not see a heartbeat, but that if I was sure of my dates, we should do. I lay on the bed staring hard at the sonographer’s face, looking for clues. Why was the scan taking so long? Why was the assistant leaving the room? Then the sonographer turned to me and said, ‘I didn’t see just one heartbeat. I didn’t see two heartbeats. I saw three heartbeats.’
The bleeding continued, and at 7 weeks I was sent for a scan. I was feeling very sick, which I thought might be a good sign, but the midwife said it might not be. She carefully prepared me that this might be a miscarriage. The sonographer told me that if I was 6 weeks pregnant, we might not see a heartbeat, but that if I was sure of my dates, we should do. I lay on the bed staring hard at the sonographer’s face, looking for clues. Why was the scan taking so long? Why was the assistant leaving the room? Then the sonographer turned to me and said, ‘I didn’t see just one heartbeat. I didn’t see two heartbeats. I saw three heartbeats.’
I was stunned. I thought so many things … There goes my home waterbirth … I can’t even breastfeed one myself, how am I going to breastfeed three? (I have a condition called insufficient glandular tissue, which limits the amount of milk I can produce) … How are triplets even born, is it one baby then one placenta, or all three babies and then the placentas?
The assistant who had left the scan room had gone to let everyone know the results. On my way out I saw the triage midwife and said to her, ‘I told you I felt REALLY sick!’
On my way out I saw the triage midwife and said to her, ‘I told you I felt REALLY sick!’
When I got home, very bizarrely, on the top of my Facebook newsfeed was a photo of an American mum, breastfeeding her triplets. I reposted the photo without comment, sat and stared at my scan photos, and tried to imagine how this might change things, compared to the single pregnancy I had been hoping for and expecting.
At my first appointment with the multiples specialist, it had sunk in a bit. There was so much information to take in. I was told about survival rates and percentages of babies born at different gestations who would have disabilities. The doctor discussed ‘selective reduction’ (abortion of one or two foetuses) with me, and pushed me to seriously consider this. Even though this was upsetting, I felt it was actually right for the doctor to push me to think about these things because carrying more than two babies makes premature labour – with all the risks for the babies – highly probable. So you do have to consider whether one baby on its own would have a better chance for a good outcome.
So you do have to consider whether one baby on its own would have a better chance for a good outcome.
Maybe I might have felt differently if I had ‘done something’ to conceive triplets, if I’d had IVF for example. But in my head, my body had got pregnant with three babies naturally, so after consideration, it felt like the right choice was to let nature take its course, and continue the pregnancy with all three babies. However, I worried about whether I would be as pressured at all appointments, so I took a friend who was a student midwife with me to the next appointment to tell the specialist my decision. I was pleasantly surprised to find that the pressure had simply been to consider the issues, and that my decision was accepted and supported.
Planning three births
My birth plan caused more controversy though. The hospital had quite a lot of experience of caring for women who vaginally birthed their twins, which gave me some confidence. But conceiving triplets is rare, and birthing them vaginally is even rarer. I arranged a birth planning meeting with the Head of Midwifery, because the multiples specialist told me that although he would ‘support’ my choice to birth vaginally, he himself does not cover Labour Ward, and so could not be involved at all really with the delivery.
I arranged a birth planning meeting with the Head of Midwifery, because the multiples specialist told me that although he would ‘support’ my choice to birth vaginally, he himself does not cover Labour Ward, and so could not be involved at all really with the delivery.
The Head of Midwifery arranged for a Labour Ward obstetrician to come to our meeting also. They began by discussing external holding – this is where the second baby in a twin birth is held in a head-down position by a midwife with her hands on the woman’s tummy after the birth of the first twin. They said that they were not sure whether this was a good idea with a triplet birth, so they had Googled it, and found some information from Australia, which said this was not helpful for the birth of the second baby in a triplet birth. The fact they had had to Google it amused me.
The Multiples Consultant had strongly advised me that I should have a ‘just-in-case’ epidural. A big concern with the birth of multiples is that once the first baby is out there is a lot of room for the others to get into different positions. This is why they do the external holding – but with a triplet birth this may be less safe, because you don’t know which baby is going to be born next, and it is less clear which limbs belong to which baby. If the next baby does get in the wrong position, for example a transverse position, then an internal version would be needed. This literally involves the obstetrician putting their hand inside the womb to turn the baby. It is very painful, hence the argument for the just-in-case epidural. That was quite a scary decision – ‘What happens if the next baby does get in the wrong position?’ I asked. They told me they would use a hand-held Doppler scanner to check the second and third babies’ positions, so it wouldn’t be undiagnosed, but an internal version would be needed immediately. I asked the obstetrician if she had ever performed an internal version (it sounded so strange). She said she had, most of them with epidurals in place, and once without, which was more difficult but still doable.
This is why they do the external holding – but with a triplet birth this may be less safe, because you don’t know which baby is going to be born next, and it is less clear which limbs belong to which baby. If the next baby does get in the wrong position, for example a transverse position, then an internal version would be needed. This literally involves the obstetrician putting their hand inside the womb to turn the baby. It is very painful, hence the argument for the just-in-case epidural. That was quite a scary decision – ‘What happens if the next baby does get in the wrong position?’ I asked. They told me they would use a hand-held Doppler scanner to check the second and third babies’ positions, so it wouldn’t be undiagnosed, but an internal version would be needed immediately. I asked the obstetrician if she had ever performed an internal version (it sounded so strange). She said she had, most of them with epidurals in place, and once without, which was more difficult but still doable. That was reassuring. When I got home, I found someone online who had had an internal version without an epidural. She said it was very painful, but it was very fast. The internal bruising lasted much longer, and was more significant, and of course once the epidural wore off I would feel that anyway. I decided that I would not have a ‘just-in-case’ epidural, and would take my chances and deal with an internal version if it was needed.
That was reassuring. When I got home, I found someone online who had had an internal version without an epidural. She said it was very painful, but it was very fast. The internal bruising lasted much longer, and was more significant, and of course once the epidural wore off I would feel that anyway. I decided that I would not have a ‘just-in-case’ epidural, and would take my chances and deal with an internal version if it was needed.
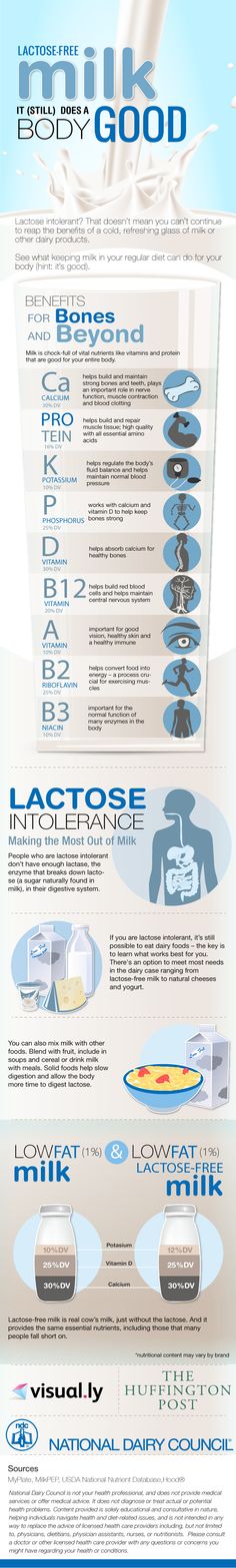
From breastfeeding my previous two children, I know that I have a rare condition called insufficient glandular tissue (IGT), where my breasts literally cannot make enough milk for my baby. Three babies were definitely going to need more milk than I could produce, but I wanted that milk to be breastmilk. This was especially important to me as my babies were very likely to be premature, and breastmilk can save the lives of premature babies.
I had managed to start collecting donor milk, together with antenatal blood tests, from the women who had donated their milk to me. I knew that, despite the antenatal screenings (as close as possible to UK Association of Milk Banks’ standards), it would be problematic to get the hospital to agree to using donor milk, and if I refused formula for my babies, it could result in a swiftly obtained court order giving the hospital shared Parental Responsibility, and then they would give them formula anyway. I discussed this with the Head of Midwifery. She got a Neonatal Intensive Care Unit (NICU) nurse to call me at around 20 weeks to discuss a plan. The NICU nurse was not helpful. She refused to make a plan with me, and disbelieved that I had IGT. She told me that I was upsetting myself over nothing, and that if I gave birth prematurely it would be my fault for upsetting myself about nothing. I did more research and found:
I knew that, despite the antenatal screenings (as close as possible to UK Association of Milk Banks’ standards), it would be problematic to get the hospital to agree to using donor milk, and if I refused formula for my babies, it could result in a swiftly obtained court order giving the hospital shared Parental Responsibility, and then they would give them formula anyway. I discussed this with the Head of Midwifery. She got a Neonatal Intensive Care Unit (NICU) nurse to call me at around 20 weeks to discuss a plan. The NICU nurse was not helpful. She refused to make a plan with me, and disbelieved that I had IGT. She told me that I was upsetting myself over nothing, and that if I gave birth prematurely it would be my fault for upsetting myself about nothing. I did more research and found:
- Milk Banks in Norway have used and distributed unpasteurised milk for many years, without incidence of infection.
- Medical papers describing how premature babies who are given formula are at much higher risk from necrotising enterocolitis – a condition which is often fatal.

- A study published in the Lancet, for babies given pasteurised and unpasteurised human milk. In the group with mixed formula and pasteurised human milk, the infection rate was 33%. For the group given only pasteurised human milk, the infection rate was 14%. The group given mixed formula and unpasteurised human milk had an infection rate of only 16%. And for the group given unpasteurised milk, it was only 11%.
- In the Czech Republic, mothers with excess milk are encouraged to donate directly to mothers who need milk, and are talked through the benefits and risks. They sign a form to attest to this.
I emailed all this information (and more) to the Patient Advice and Liaison Service (PALS), who sent replies from the Trust Solicitor, refusing to allow me to use unpasteurised privately sourced donor milk. I offered to sign a disclaimer, and pointed out that the antenatal screening the women had had was in line with the UK Association of Milk Banks policy for donor milk. I also offered to pay for pasteurised donor milk from a Milk Bank. The reply was still no. Eventually the Head of Midwifery stepped in to help me make a plan. She was happy to use pasteurised donor milk from a Milk Bank, and told me that they had reserved some milk especially for my triplets, which I was delighted about.
I also offered to pay for pasteurised donor milk from a Milk Bank. The reply was still no. Eventually the Head of Midwifery stepped in to help me make a plan. She was happy to use pasteurised donor milk from a Milk Bank, and told me that they had reserved some milk especially for my triplets, which I was delighted about.
There were also difficulties with my birth plan because I felt strongly about delayed cord clamping. Because my babies were likely to be premature and therefore low birth weight, I felt they needed every drop of their blood. However, when multiple babies share a common placenta, there is a risk of ‘twin-to-twin transfusion’ – where the baby (or babies) still inside the womb receive too much blood from the baby who has been born. This can be very damaging and even fatal to the baby who receives too much blood. The Multiples Specialist said that for this reason, current hospital policy was to ‘not allow’ delayed cord clamping, because they had had one case of twin-to-twin transfusion syndrome occur suddenly at birth. Scans showed that my triplets each had separate placentas (trichorionic), but the Multiples Specialist said that there was a 10% chance of the scans misdiagnosing the placentas as being separate. Therefore I could not have delayed cord clamping, because there was still a tiny chance it might harm the babies.
Scans showed that my triplets each had separate placentas (trichorionic), but the Multiples Specialist said that there was a 10% chance of the scans misdiagnosing the placentas as being separate. Therefore I could not have delayed cord clamping, because there was still a tiny chance it might harm the babies.
In the UK, all decisions are the mother’s until the baby is born because the baby is not considered a separate entity until the moment of birth. This means a hospital cannot overrule any decisions a woman makes about her body before a baby is born. However, as soon as a baby is born, a hospital has a duty of care to that baby. In a multiple birth, decisions about a baby who is born can affect a baby who is not, and vice versa.
The Trust Solicitor was contacted again, this time by the Multiples Specialist. He eventually confirmed that I had the right to insist on delayed cord clamping, but only because the potential harm is to the baby or babies still in the womb. Therefore I was legally allowed to make a decision about the baby who was born, that was potentially harmful to the unborn babies, because the Trust’s duty of care was only to the baby who was already born. It sounded slightly ridiculous to me that I was allowed to potentially cause harm to my unborn babies. But actually, sudden onset at birth twin-to-twin transfusion syndrome is quite rare even in twins who do share a placenta, and the Multiples Specialist calculated that even with the 10% chance of every scan being wrong, the actual risks were around .001%, and so I was quite confident this was a decision that was in my babies’ best interests, rather than one that would harm them. [AIMS note: TTTS in pregnancy is discussed in this article, but in this case, Rowena is referring to TTTS during birth. More information on this is available from TAMBA (link: https://www.tamba.org.uk/file/TTTS-Guide.pdf).]
It sounded slightly ridiculous to me that I was allowed to potentially cause harm to my unborn babies. But actually, sudden onset at birth twin-to-twin transfusion syndrome is quite rare even in twins who do share a placenta, and the Multiples Specialist calculated that even with the 10% chance of every scan being wrong, the actual risks were around .001%, and so I was quite confident this was a decision that was in my babies’ best interests, rather than one that would harm them. [AIMS note: TTTS in pregnancy is discussed in this article, but in this case, Rowena is referring to TTTS during birth. More information on this is available from TAMBA (link: https://www.tamba.org.uk/file/TTTS-Guide.pdf).]
At the meeting, both the Head of Midwifery and the Labour Ward Obstetrician supported my decision not to have continuous monitoring. With a triplet birth, I would have had bands around me for two babies, and one for my contractions, and then a scalp monitor for the third baby. In previous labours I had found any clothes really distracting and uncomfortable, so the thought of several bands round my tummy, and a scalp monitor, was not appealing.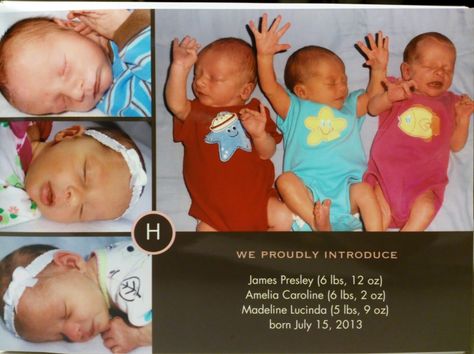 Cardiotocography (CTG) monitoring is also notorious for raising false alarms, leading to unnecessary interventions. The Head of Midwifery fully documented my birth choices, including no ‘just-in–case’ epidural, that I was not having CTG monitoring, and that I wanted to be in water for the first stage of labour, so I didn’t really need to write a birth plan. This then ensured that whichever midwives and obstetricians were on shift when I went into labour would know that my choices were informed choices, and would be less twitchy about them. My friend later told me that the Head of Midwifery had previously been an independent midwife with experience of twin homebirth. I felt lucky – she was the perfect person to be supporting me. It now felt like my plans were all in place, and I could enjoy the last few months of pregnancy.
Cardiotocography (CTG) monitoring is also notorious for raising false alarms, leading to unnecessary interventions. The Head of Midwifery fully documented my birth choices, including no ‘just-in–case’ epidural, that I was not having CTG monitoring, and that I wanted to be in water for the first stage of labour, so I didn’t really need to write a birth plan. This then ensured that whichever midwives and obstetricians were on shift when I went into labour would know that my choices were informed choices, and would be less twitchy about them. My friend later told me that the Head of Midwifery had previously been an independent midwife with experience of twin homebirth. I felt lucky – she was the perfect person to be supporting me. It now felt like my plans were all in place, and I could enjoy the last few months of pregnancy.
One labour …
The last few months turned out to be only the last few weeks of pregnancy. I had a few false starts of labour. At 29 weeks I went into pre-term labour and went into hospital. I was given a steroid injection to help my babies’ lungs mature. The UK policy for pre-term labour is that, if pre-term labour happens, it is taken as an indication that there must be a problem, and it is assumed that the babies would be better off in an incubator than in a womb. Therefore they usually only give 24 hours of the Atosiban drip (a drug that stops labour), to give the steroid injection time to work. After that, they will not try to prevent labour continuing. I understand this policy, but think that it is not necessarily appropriate for multiples pregnancies. I felt my pre-term labour might not have indicated a problem, but might have been just because there was so little room inside for the babies. In the USA, hospitals are willing to prescribe many drugs to try to stop pre-term labours in multiples pregnancies – I wish they would do that here too.
I was given a steroid injection to help my babies’ lungs mature. The UK policy for pre-term labour is that, if pre-term labour happens, it is taken as an indication that there must be a problem, and it is assumed that the babies would be better off in an incubator than in a womb. Therefore they usually only give 24 hours of the Atosiban drip (a drug that stops labour), to give the steroid injection time to work. After that, they will not try to prevent labour continuing. I understand this policy, but think that it is not necessarily appropriate for multiples pregnancies. I felt my pre-term labour might not have indicated a problem, but might have been just because there was so little room inside for the babies. In the USA, hospitals are willing to prescribe many drugs to try to stop pre-term labours in multiples pregnancies – I wish they would do that here too.
I asked the Multiples Consultant about this, and he did agree to give me a second 24 hours of Atosiban (because NICE guidelines say ‘up to 48 hours’), but after that nature would have to take its course. After this I was moved to a different ward. Because of the move, I missed a meal. In the new ward, the contractions started again. I quickly ate a sandwich, aware that I would need my energy, and labour stopped. I then woke up at 5am with a few contractions; I ate two biscuits, and labour stopped again! When I got home, I searched online for this and found that low blood sugar can precipitate labour. So from then on, every time I had contractions, I ate something. When I got up to go to the loo in the middle of the night, I made sure I ate a substantial snack – a banana, a biscuit and a glass of milk. I think this really helped to keep my babies in.
After this I was moved to a different ward. Because of the move, I missed a meal. In the new ward, the contractions started again. I quickly ate a sandwich, aware that I would need my energy, and labour stopped. I then woke up at 5am with a few contractions; I ate two biscuits, and labour stopped again! When I got home, I searched online for this and found that low blood sugar can precipitate labour. So from then on, every time I had contractions, I ate something. When I got up to go to the loo in the middle of the night, I made sure I ate a substantial snack – a banana, a biscuit and a glass of milk. I think this really helped to keep my babies in.
At 32 weeks I had a really horrendous scan. The sonographer tried to make me lie on my back, but by now my tummy was so huge that I couldn’t breathe if I lay on my back. The sonographer was truly awful, really prodding and poking me, and the scan was not just uncomfortable, it was very painful. I was very distressed during the scan and after.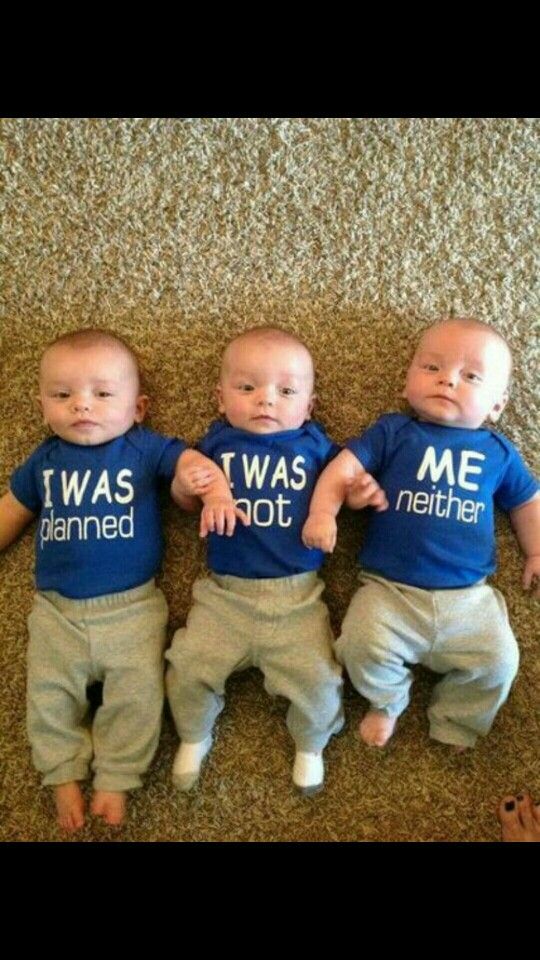 My friend who is a doula came with me, and she later described it as an assault. I wished one of us had spoken up during the appointment, not just talked about it afterwards. The scan had shown my babies were in the same position they had been throughout, lined up like three dominos, ready for birth.
My friend who is a doula came with me, and she later described it as an assault. I wished one of us had spoken up during the appointment, not just talked about it afterwards. The scan had shown my babies were in the same position they had been throughout, lined up like three dominos, ready for birth.
I had a really uncomfortable night, and at an appointment with the Multiples Specialist the next day I discovered that my two boys were now transverse. I think the painful prodding was so rough that it had made them move, and with my babies in this position there was less room for them, which made my tummy much more uncomfortable.
That evening, I had more contractions, and they weren’t going away. At 10pm I realised this was definitely it, and went into hospital in early labour. I arrived at 11pm, at 32 weeks and 2 days pregnant. Everyone writing in my notes kept putting 32+2, though after I had been there an hour I kept saying ‘it’s 32+3 actually’, as it was now after midnight. The extra day felt important to me. Every day matters when your baby is premature.
The extra day felt important to me. Every day matters when your baby is premature.
I had been given pethidine in my first labour and had an awful time. I had also tried gas and air, and didn’t like that, so I just wanted to use water for pain relief (but understood actually giving birth in water would never be recommended because the babies would be premature). As the pool in the Labour Ward is rarely used, I hoped I would be able to use it. However, when I arrived, someone else was in it, much to my disappointment. Someone from NICU then appeared in the room, to give me a presentation about NICU care. This seemed very surreal to me, but it is what they do for all women arriving in premature labour. A few days later, I discovered a glossy brochure with pictures of shiny incubators in it, though I have no memory of having been given it. It must be very traumatic for women who were not expecting their babies to need NICU care and whose premature labour was unexpected. At least I had had time before labour to think about it and come to terms with it.
After I had been in hospital an hour, the Head of Midwifery came in. She must have asked to be called when I came in, and she cared for me during my labour. Otherwise I would just have been cared for by the duty obstetrician, who might or might not have had experience of multiple births before. I was glad to see the Head of Midwifery. She cared for me very respectfully.
I tried to find music I wanted, but I couldn’t. Vocalising had helped in my previous labour, but this time it felt like it used up too much energy. I spent most of my labour draped over a beanbag on the bed. The room was dimly lit, and the Head of Midwifery and the Obstetrician were very quiet. The Head of Midwifery would catch my eye when she thought I was having a contraction, and I would just nod slightly at her, so she didn’t have to ask me, which was wonderful.
… three babies, born
Finally, I was told the pool was vacant, cleaned, refilled and waiting for me. That was wonderful news, but as I was being wheeled along the corridor I knew that if I got in, I wouldn’t be getting out. I think I was probably in transition, and I didn’t want to tell them that because I wanted to get in the pool. In the corridor I told my doula ‘I think I need a poo’ and I was suddenly wheeled at high speed into the pool room, as everyone realised I was about to give birth. My daughter, Bee, was born just a few minutes later and was handed to me for just a precious few moments while they let her cord pulse.
I think I was probably in transition, and I didn’t want to tell them that because I wanted to get in the pool. In the corridor I told my doula ‘I think I need a poo’ and I was suddenly wheeled at high speed into the pool room, as everyone realised I was about to give birth. My daughter, Bee, was born just a few minutes later and was handed to me for just a precious few moments while they let her cord pulse.
If I had had a Caesarean birth, the theatre would have been so full of people – as well as the usual doctors, midwife and anaesthetist for me, there would have been a midwife and a neonatal doctor for each of my three babies, because they would all have been born within minutes of each other. However, because I was giving birth vaginally, only one baby was born at a time. The Head of Midwifery made sure only the midwife and neonatal doctor relevant to the baby currently being born were in the room – the rest waited elsewhere. This kept the number of people in the room to a minimum, and really protected my privacy.
Bee stayed on my chest for a few moments before her cord was clamped and cut, and she was whisked away for checks. I had wanted a longer delay for clamping for my babies, but had agreed to 90 seconds, by which time most of the blood would be transferred. Shortly after this, Bee was taken by the midwife and neonatal doctor to NICU. It felt strange when they took her, even though I had been expecting it.
After Bee was born, labour just seemed to stop. Nothing happened for an hour and a half. I think this was because there was now more room in my uterus, and everything was comfortable again. The waters around my boys were intact, and had I been really in control of all the decisions, I might have liked to just carry on being pregnant with them, until labour restarted by itself. I have read that this has sometimes taken days or even weeks for other people. However, I didn’t feel strongly enough about this to want to debate it then. I was encouraged to move, but contractions didn’t restart. After an hour or so, everyone in the room was glancing at the clock. Eventually the Head of Midwifery suggested breaking my waters. I didn’t really want this, but I trusted her, so I agreed, and it worked. I wouldn’t have changed this decision. The Head of Midwifery then did some internal holding, and the Obstetrician did some external holding, as it was now clear that the second baby was in the right position. The Head of Midwifery then guided me in pushing, which I did need at this point (unlike with Bee, because this time I did not have any natural urge to push). So my son Alexis was born. Again I held him, though on my tummy not chest as his cord was so short. We waited before clamping and cutting the cord, and then he too was taken to NICU.
After an hour or so, everyone in the room was glancing at the clock. Eventually the Head of Midwifery suggested breaking my waters. I didn’t really want this, but I trusted her, so I agreed, and it worked. I wouldn’t have changed this decision. The Head of Midwifery then did some internal holding, and the Obstetrician did some external holding, as it was now clear that the second baby was in the right position. The Head of Midwifery then guided me in pushing, which I did need at this point (unlike with Bee, because this time I did not have any natural urge to push). So my son Alexis was born. Again I held him, though on my tummy not chest as his cord was so short. We waited before clamping and cutting the cord, and then he too was taken to NICU.
Thirty minutes later my third triplet, Lenny, was born, with similar holding and guided pushing. I found this helpful, as my body was a bit like ‘we’ve got the baby out, let’s go to sleep’, not seeming to realise there was still another baby to give birth to. Again, when he was born I held him for a few minutes. My doula managed to take some wonderful (and quite discreet) photos of my babies being born, which I love. The pictures surprise me a little, because everything is so brightly lit. My memory of the birth is that everything was quite dark and dim, but maybe that is because my eyes were mostly closed.
Again, when he was born I held him for a few minutes. My doula managed to take some wonderful (and quite discreet) photos of my babies being born, which I love. The pictures surprise me a little, because everything is so brightly lit. My memory of the birth is that everything was quite dark and dim, but maybe that is because my eyes were mostly closed.
Although I had had physiological third stages for my previous births, I had agreed to Syntometrine to deliver the placenta to minimise bleeding, which seemed reasonable to me. Everyone else in the room was fascinated by this giant fused triple placenta! It weighed the same amount as one whole baby.
When all my babies had been taken away, and the placenta had been examined, they said I might as well get into the pool. It was lovely wallowing in such a huge bath after giving birth, and I felt euphoric … but strange, because my babies had disappeared.
NICU
As I tried to get back out of the pool, I had a weird sensation of not being able to breathe, as if all my body was suddenly too heavy. That was odd. On the postnatal ward I couldn’t sit up or stand for more than five minutes without finding breathing difficult. I was having to be wheeled across to NICU in a wheelchair because I couldn’t walk far. The midwives didn’t know why, didn’t take it seriously, and looked at me quite oddly when I said I needed to use a wheelchair. One of the other mums I met had brought a corset in, because she said that she had had severe diastasis recti before. This is when the stomach muscles have separated so much that for a while after birth they simply don’t hold your organs properly in the right place. The mum described it to me as your diaphragm not holding everything in, so it falls out of the bottom of your tummy. This was exactly what it felt like was happening to me! The midwives on the ward didn’t seem to have heard of this, but they did send a physio to see me. The physio made a corset out of a double layer of their largest Tubigrip, and immediately I could breathe, sit up, and walk again with ease.
That was odd. On the postnatal ward I couldn’t sit up or stand for more than five minutes without finding breathing difficult. I was having to be wheeled across to NICU in a wheelchair because I couldn’t walk far. The midwives didn’t know why, didn’t take it seriously, and looked at me quite oddly when I said I needed to use a wheelchair. One of the other mums I met had brought a corset in, because she said that she had had severe diastasis recti before. This is when the stomach muscles have separated so much that for a while after birth they simply don’t hold your organs properly in the right place. The mum described it to me as your diaphragm not holding everything in, so it falls out of the bottom of your tummy. This was exactly what it felt like was happening to me! The midwives on the ward didn’t seem to have heard of this, but they did send a physio to see me. The physio made a corset out of a double layer of their largest Tubigrip, and immediately I could breathe, sit up, and walk again with ease.
My birth had been a great experience, but NICU was sadly not. The plan the Head of Midwifery had put in place to reserve donor milk for my triplets was overruled by the NICU paediatrician, on the grounds that my babies were not premature enough to qualify for it, and they had already used most of the Milk Bank milk that the Head of Midwifery had understood was reserved for my babies. I was trying to express colostrum, but apart from an initial few drops there was literally nothing at all for about five days. My babies needed milk. The paediatrician suggested pre-term formula, but I was very reluctant. I wanted to use donor milk from my friends, if the Milk Bank milk wasn’t available to them, but the paediatrician said the hospital would not allow this. Eventually they agreed to allow Milk Bank milk to be used for one week, while the issue was debated and resolved.
The Head of Midwifery and one of the neonatologists eventually came up with a plan. They would agree to my babies having one milk donor, as long as she was screened by the hospital, and came to express at the hospital under their controlled conditions. Her milk and my milk could be given to my babies whilst they were in NICU. When I took my babies home, I could feed them however I chose, so I could then use my donor milk for them without the hospital feeling liable. I was extremely lucky to know one good friend who had such oversupply that she was able to express an extra litre per day in addition to feeding her own baby, and she happened to live very close to the hospital.
Her milk and my milk could be given to my babies whilst they were in NICU. When I took my babies home, I could feed them however I chose, so I could then use my donor milk for them without the hospital feeling liable. I was extremely lucky to know one good friend who had such oversupply that she was able to express an extra litre per day in addition to feeding her own baby, and she happened to live very close to the hospital.
And home
In the end, my babies had no formula. I found donors amongst friends and via Human Milk for Human Babies. They had only human milk for around eight months. I am so grateful to the women who donated their milk to my babies. By the time they were a few weeks old, they were needing an extra 1.5 litres of milk per day in addition to mine. I fed them myself as frequently as I could, sometimes almost constantly rotating them, tandem-feeding two at the same time as bottle-feeding the third.
When you register the birth of multiple babies, they record their times of birth, not just the date, so that it is recorded who is the oldest. Here is my babies’ birth information for you:
Here is my babies’ birth information for you:
|
Time of birth |
Apgar scores |
Weight |
|
|
Beatrix (Bee) |
5.34am |
8 9 8 |
3lb 14.5oz |
|
Alexis |
7.16am |
9 10 - |
4lb 5oz |
|
Valentin (Lenny) |
7.47am |
8 9 10 |
4lb 3oz |
From left to right: Beatrix, Valentin and Alexis at three months old:
With thanks to Mari Greenfield for her contribution to the writing of this article.
AIMS supports all maternity service users to navigate the system as it exists, and campaigns for a system which truly meets the needs of all.
The AIMS Journal spearheads discussions about change and development in the maternity services. From the beginning of 2018, the journal has been published online and is freely available to anyone with an interest in pregnancy and birth issues. Membership of AIMS continues to support and fund our ability to create the online journal, as well as supporting our other work, including campaigning and our Helpline. To contact the editors, please email: [email protected]
How to conceive twins naturally: table, folk remedies
PreviousNext
- Factors affecting the possibility of having twins
- How to Increase Your Chances of Conceiving Twins Naturally
Contents:
One child is enough for someone, and someone just dreams of having two in the family at once.
To answer the question of how to conceive twins or twins, you need to understand the mechanism of these phenomena. The difference between twins and twins is simple: identical twins, similar to each other, like two drops of water, are children born from one fertilized egg, which divides into two after fertilization, and twins appear with the simultaneous fertilization of two eggs at once, while children may be of different sexes and not at all similar to each other. It should be noted that nature has a mechanism that levels the birth of twins, since it is more difficult to endure and grow it. But there are various factors that contribute to the simultaneous maturation of two eggs, due to which the conception of twins occurs. It is impossible to plan the pregnancy of identical twins, just as it is impossible to give an absolute guarantee of the conception of twins, but it is quite possible to provoke the simultaneous maturation of two eggs.
Factors affecting the possibility of having twins:
-
heredity - the probability of conceiving twins is higher in those women in whose family there have already been multiple pregnancies;
-
overweight - it has been noticed that twins are more often born precisely in obese women;
-
over 30 years of age - the body can provoke the maturation of several follicles at once to increase the likelihood of conception;
-
pregnancy during lactation increases the possibility of conceiving twins;
-
with each subsequent pregnancy, the chances of having twins increase;
-
mother's ethnicity - not at all puzzled over how to conceive twins, African women give birth to several children at once much more often than everyone else.
 But the least likely multiple pregnancy occurs in Asian women.
But the least likely multiple pregnancy occurs in Asian women.
What factors influence the conception of a boy or a girl, read also in our articles.
How to Increase Your Chances of Having Twins Naturally
First of all, you should consult with your doctor, perhaps he will advise what to do to conceive twins. It is better to prepare for this conversation: bring medical records (yours and your partner), find out in advance what diseases relatives on both sides suffer from and whether there were multiple pregnancies in the female line.
You may be lucky and your doctor will be able to give you a magic table on how to conceive twins, or teach you how to conceive twins by ovulation.
Among the medical methods that a doctor can also advise, there is treatment with drugs that include follicle-stimulating hormone, as a result of which two eggs can mature at the same time. Moreover, after the abolition of hormonal contraceptives, the so-called rebound effect is observed, when both ovaries are put into operation at once and twins can be conceived.
Also, do not forget about artificial insemination, when two or three fertilized eggs are implanted in a woman at once.
There are folk ways to conceive twins. First of all, the recommendations relate to nutrition designed to promote the maturation of more follicles. You will have to lean on dairy products, chicken eggs, whole grains, walnuts, pumpkin, bananas, carrots, red fish, liver. Try to find a product such as yams, which contain a set of substances that stimulate the ovaries. The largest number of twins is born in the Igbo city of Orana in southwestern Nigeria, for which it is even called the "Land of the Twins". The main food of the population there is yams.
A prerequisite to conceive twins is to give up alcohol and smoking.
To activate the work of the ovaries, you can start taking folic acid daily a few months before the planned conception, after consulting with your doctor.
It has been established that most twins are born in July, and least of all in the first month of winter. This may be due to the length of daylight hours, which affects the release of follicle-stimulating hormone. Therefore, conception is best planned for the fall.
This may be due to the length of daylight hours, which affects the release of follicle-stimulating hormone. Therefore, conception is best planned for the fall.
Climate can also indirectly affect - long daylight hours, high humidity, solar activity activate the ovaries. Therefore, you can plan a month-long vacation to a suitable place to increase your chances.
An interesting established fact is that twins are born four times more often in women who are already mothers of twins. Therefore, it is worth giving birth to twins only once, as the next time it will be easier to adjust.
PreviousNext
Management of multiple pregnancy - clinic Family doctor
Doctors
Clinic doctors
Multiple pregnancy is not only a great happiness, but also an increased burden on the body of the expectant mother. Therefore, special standards apply for its management: more frequent visits to the gynecologist and an extended examination, other recommendations regarding lifestyle.
Therefore, special standards apply for its management: more frequent visits to the gynecologist and an extended examination, other recommendations regarding lifestyle.
It is good if the management of multiple pregnancy begins with its early diagnosis. The sooner this fact is revealed, the higher the chances of drawing up the most successful management plan and timely implementation of measures to prevent possible complications. For patients who plan to conceive and are at risk for multiple pregnancies, it is extremely important to start monitoring immediately after a successful conception.
Why multiple pregnancy occurs
The probability of multiple pregnancy is significantly higher in some categories of patients:
- heredity;
- women planning to conceive after giving up hormonal contraceptives;
- women over 35;
- those who have congenital non-standard structural features of the uterus;
- expectant mothers who have taken advantage of the possibilities of modern reproductive technologies (IVF procedure, etc.
 ).
).
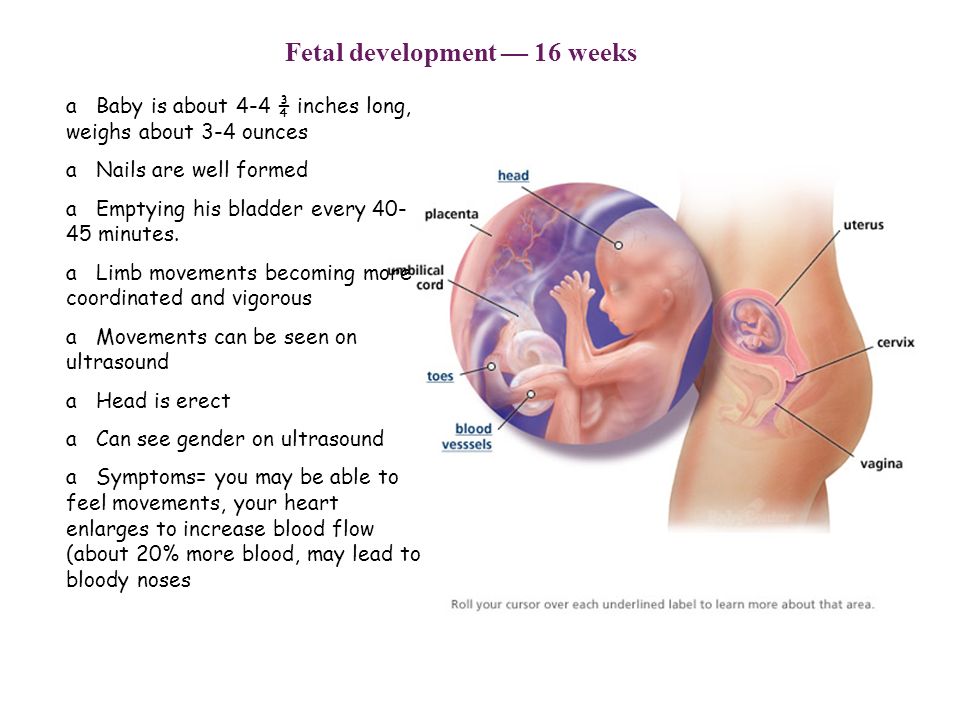
The number of fetuses can be any, as a rule, we are talking about twins or triplets. There are identical (fertilization of one egg, the birth of identical twins) and twin pregnancies. In the second case, two (or more) eggs are fertilized, as a result, different children are born. It is this case that is more often caused by the woman's age, interference in the reproductive processes (IVF, ovulation stimulation, the abolition of COCs). These factors lead to more active work of the ovaries, as a result of which several eggs mature in one menstrual cycle at once.
How and for how long is diagnosed
Early diagnosis is the key to a healthy, successful and full-term multiple pregnancy. The doctor can establish the fact of the presence of two or more fetuses for a short period of time, up to 5 weeks.
The basis for suspecting a larger number of fruits is an examination. The volume of the uterus will be larger than for the expected period. Without fail, a woman takes an analysis for hCG in dynamics - the level of human chorionic gonadotropin, growing at a fast pace, is a sign of multiple pregnancy. Subsequently, during palpation, the doctor will determine the parts of several fetuses, and when listening to heart sounds, they will be observed in different parts of the abdomen.
Without fail, a woman takes an analysis for hCG in dynamics - the level of human chorionic gonadotropin, growing at a fast pace, is a sign of multiple pregnancy. Subsequently, during palpation, the doctor will determine the parts of several fetuses, and when listening to heart sounds, they will be observed in different parts of the abdomen.
Driving features
Conducting multiple pregnancy is carried out with special attention. Features of observation when carrying two or more babies are as follows:
- relatively more frequent visits to the obstetrician-gynecologist: 1 time in 14 days up to 30 weeks and every week until childbirth;
- the appointment of increased doses of vitamins, minerals;
- a more rigorous assessment of the dynamics of weight gain: an increase of no more than 25 kg is considered normal;
- drawing up a special plan for physical activity, its significant reduction from 20-25 weeks;
- more frequent ultrasound, which is associated with the need to assess the dynamics of fetal development and take measures in case of delay, as well as to prevent the threat of preterm birth.
 It is important to assess the condition of the placenta in order to timely determine the compliance of its changes with the gestational age;
It is important to assess the condition of the placenta in order to timely determine the compliance of its changes with the gestational age; - the appointment of drugs that prevent common complications (fetoplacental insufficiency, anemia, preeclampsia, etc.).
Recommendations and standards
There are special standards for the management of two, three and more pregnancies. Immediately after the diagnosis, the doctor will develop a regimen of physical activity and nutrition. This will ensure the high needs of the expectant mother in proteins, fats, carbohydrates, vitamins and minerals, as well as maintain normal health in conditions of high stress on the spine.
Particular attention is paid to the functions of the heart and blood vessels, kidneys. Therefore, the patient more often gives urine tests, additional consultation with a cardiologist, nephrologist, urologist may be required.
The high risk of preterm birth obliges to monitor the slightest changes. If the patient feels well and there are no complications, she is sent to the maternity hospital 2-3 weeks before the preliminary date of delivery. If we are talking about triplets, in 4 weeks.
If the patient feels well and there are no complications, she is sent to the maternity hospital 2-3 weeks before the preliminary date of delivery. If we are talking about triplets, in 4 weeks.
At 30-34 weeks, the likelihood of preterm birth is especially high, which is associated with maximum tension and stretching of the uterus. In addition, shortening and partial opening of the cervix is often observed. The doctor will definitely recommend bed rest if necessary, which will increase the chances of carrying it to the due date. Drugs that relieve muscle spasm, as well as tocolytics, drugs that affect the contractile activity of the uterus, can be prescribed.
FPI or fetoplacental insufficiency is more often observed precisely when carrying several fetuses. Abnormal location of the placenta is also common. This obliges to regularly monitor the condition of the fetus and placenta: perform Doppler ultrasound, CTG. So, starting from the 30th week, it is better to do this once every 7 days until delivery. An experienced specialist should evaluate the blood flow in each fetus individually. FPI can be prevented with the help of preventive drug therapy: drugs that improve uteroplacental, fetoplacental blood flow, antioxidants, metabolic drugs, etc.
An experienced specialist should evaluate the blood flow in each fetus individually. FPI can be prevented with the help of preventive drug therapy: drugs that improve uteroplacental, fetoplacental blood flow, antioxidants, metabolic drugs, etc.
Features of delivery
Delivery can be natural or by caesarean section. In the absence of pathologies and complications, the presence of two fetuses, favorable examination results, a natural option is allowed. Indications for operative delivery are as follows:
- clinically narrow pelvis;
- features of the presentation of one of the fetuses;
- transverse arrangement of one or both babies;
- signs of hypoxia in at least one fetus;
- pregnancy complications in the mother.
These indications are more often related to the planning of the operation. An emergency cesarean may be required after the onset of labor. The doctor makes a decision based on the situation.