How long should diarrhea last in a child
Diarrhea in Children | Johns Hopkins Medicine
What is diarrhea?
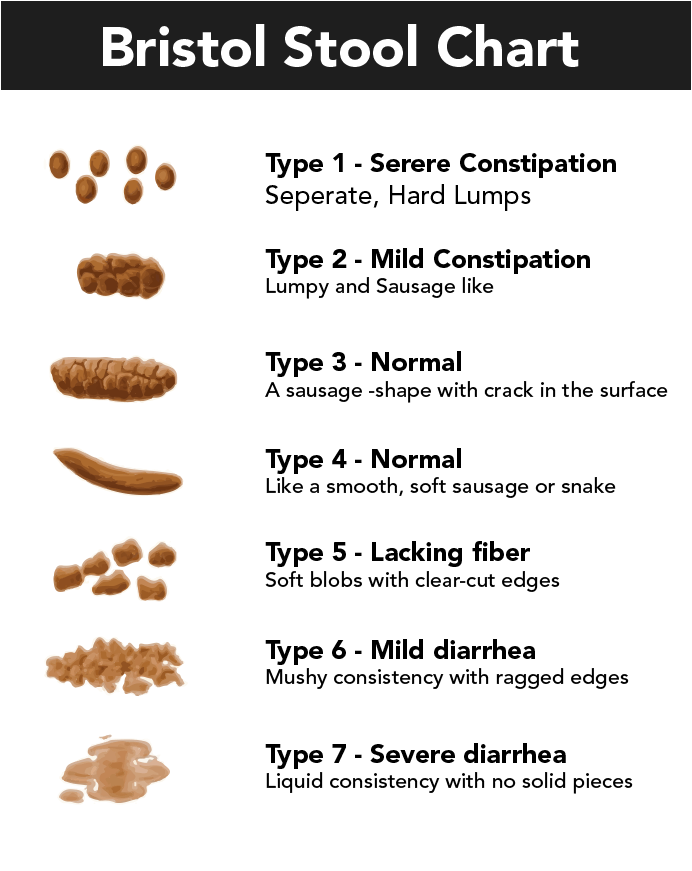
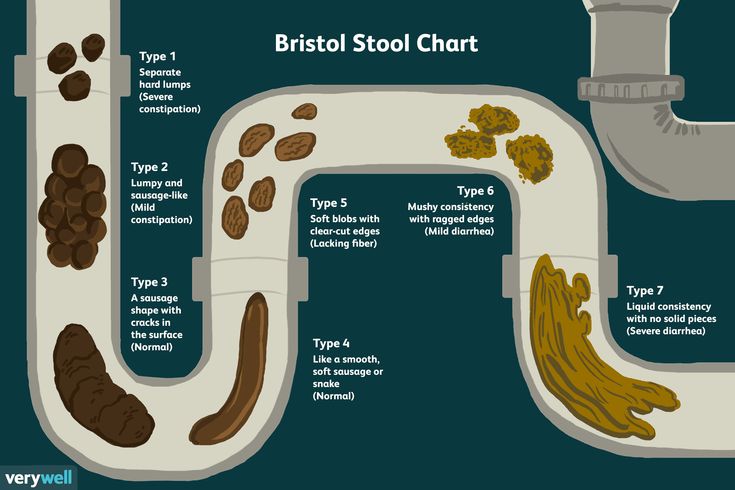
Diarrhea is when stools (bowel movements) are loose and watery. Your child may also need to go to the bathroom more often.
Diarrhea is a common problem. It may last 1 or 2 days and go away on its own. If diarrhea lasts more than 2 days, your child may have a more serious problem.
Diarrhea may be either:
Short-term (acute). Diarrhea that lasts 1 or 2 days and goes away. This may be caused by food or water that was contaminated by bacteria (bacterial infection). Or it may happen if your child gets sick from a virus.
Long-term (chronic). Diarrhea that lasts for a few weeks. This may be caused by another health problem such as irritable bowel syndrome. It can also be caused by an intestinal disease. This includes ulcerative colitis, Crohn’s disease, or celiac disease. Giardia may also cause chronic diarrhea.
What causes diarrhea?
Diarrhea may be caused by many things, including:
Bacterial infection
Viral infection
Trouble digesting certain things (food intolerance)
An immune system response to certain foods (food allergy)
Parasites that enter the body through food or water
Reaction to medicines
An intestinal disease, such as inflammatory bowel disease
A problem with how the stomach and bowels work (functional bowel disorder), such as irritable bowel syndrome
Surgery on the stomach or gallbladder
Children who visit some foreign countries are at risk for traveler's diarrhea. This is caused by having food or water that is not safe because of bacteria, viruses, or parasites.
Severe diarrhea may mean a child has a serious disease. Talk with your child's healthcare provider if symptoms don’t go away. Also talk with the provider if symptoms stop your child from doing daily activities. It may be hard to find out what is causing your child’s diarrhea.
What are the symptoms of diarrhea?
Symptoms can occur a bit differently in each child. They can include:
Cramping
Belly (abdominal) pain
Swelling (bloating)
Upset stomach (nausea)
Urgent need to use the bathroom
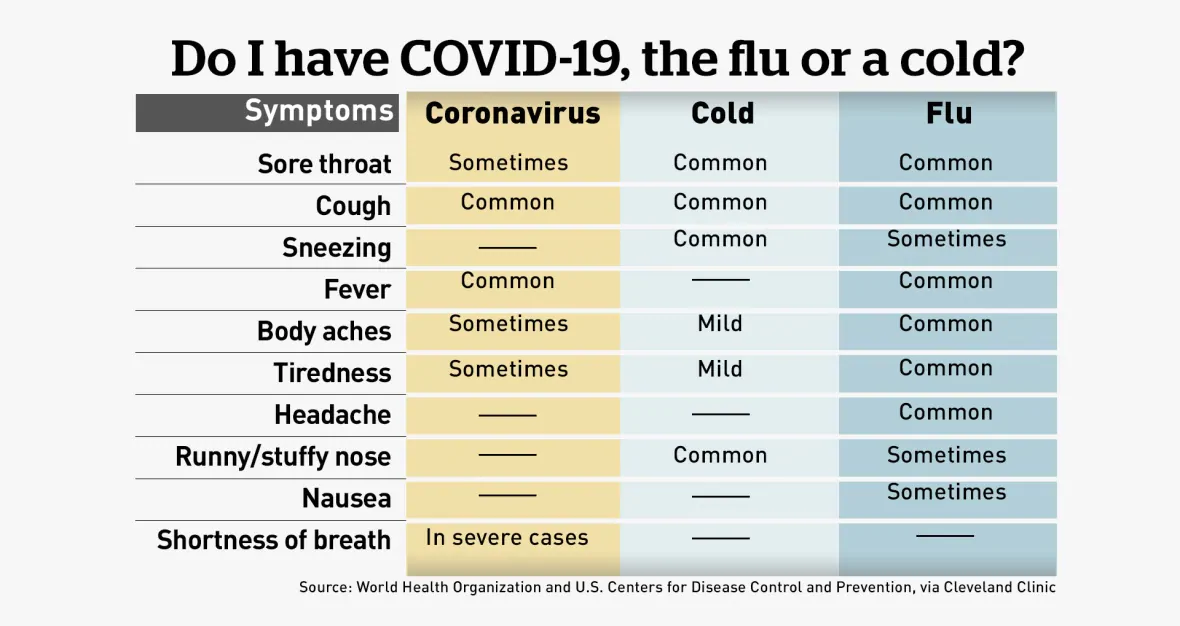
Fever
Bloody stools
Loss of body fluids (dehydration)
Incontinence
The symptoms of diarrhea may look like other health problems. Severe diarrhea may be a sign of a serious disease. Make sure your child sees his or her healthcare provider for a diagnosis.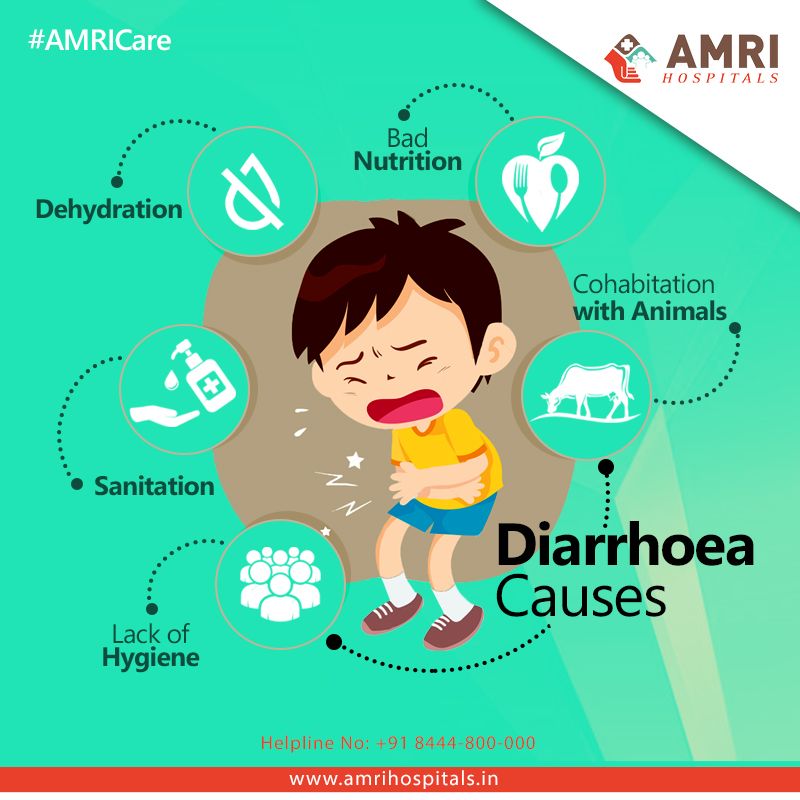
How is diarrhea diagnosed?
The healthcare provider will ask about your child’s symptoms and health history. He or she will give your child a physical exam. Your child may have lab tests to check blood and urine.
Other tests may include:
A stool culture to check for abnormal bacteria or parasites in your child’s digestive tract. A small stool sample is taken and sent to a lab.
A stool evaluation to check the stool for blood or fat
Blood tests to rule out certain diseases
Imaging tests to rule out structural problems
Tests to check for food intolerance or allergies
A sigmoidoscopy. This test lets the healthcare provider check the inside of part of your child’s large intestine. It helps to tell what is causing diarrhea, stomach pain, constipation, abnormal growths, and bleeding. It uses a short, flexible, lighted tube (sigmoidoscope). The tube is put into your child’s intestine through the rectum.
 This tube blows air into the intestine to make it swell. This makes it easier to see inside.
This tube blows air into the intestine to make it swell. This makes it easier to see inside.
How is diarrhea treated?
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
Dehydration is the major concern with diarrhea. In most cases, treatment includes replacing lost fluids. Antibiotics may be prescribed when bacterial infections are the cause.
Children should drink lots of fluids. This helps replace the lost body fluids. If your child is dehydrated, be sure to:
Offer drinks called glucose-electrolyte solutions. These fluids have the right balance of water, sugar, and salts. Some are available as popsicles.
Avoid juice or soda. They may make diarrhea worse.
Not give plain water to your baby
Not give too much plain water to kids of any age. It can be dangerous.
Keep breastfeeding your baby. Breastfed babies often have less diarrhea.
Keep feeding your baby formula, if you were already doing so
What are the complications of diarrhea?
The greatest complication of diarrhea is dehydration. This is more likely with young children and those with a weakened immune system. Dehydration can be mild, moderate, or severe. Mild dehydration is the loss of fluid. Moderate or severe dehydration puts stress on the heart and lungs. In the worst cases it can lead to shock, which is life-threatening.
What can I do to prevent diarrhea?
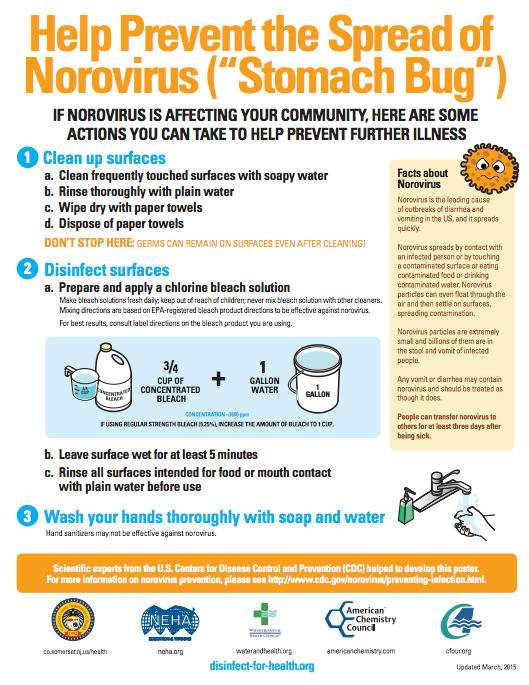
Proper handwashing can reduce the spread of bacteria that may cause diarrhea.
A rotavirus vaccine can prevent diarrhea caused by rotaviruses. Ask your child's healthcare provider which vaccines are right for your child.
When you travel, make sure anything your child eats and drinks is safe. This is even more important if you travel to developing countries.
Travel safety tips for drinking and eating include:
Not drinking tap water or using it to brush teeth
Not using ice made from tap water
Not drinking unpasteurized milk (milk that has not gone through a process to kill certain bacteria)
Not eating raw fruits and vegetables unless you wash and peel them yourself
Not eating raw or undercooked meat or fish
Not eating food from street vendors or food trucks
Talk with your child's healthcare provider before traveling.
When should I call my child's healthcare provider?
Call your child's provider if your child is less than 6 months old or has any of the following symptoms:
Belly pain
Blood in the stool
Frequent vomiting
Doesn’t want to drink liquids
High fever
Dry, sticky mouth
Weight loss
Urinates less frequently (wets fewer than 6 diapers per day)
Frequent diarrhea
Extreme thirst
No tears when crying
Sunken soft spot (fontanelle) on baby’s head
Key points about diarrhea
Diarrhea is loose, watery stool. Your child may also have to go to the bathroom more often.
It may be caused by many things, including bacterial infection or viral infection.
Dehydration is the major concern with diarrhea.
In most cases, treatment involves replacing lost fluids.
The rotavirus vaccine can prevent diarrhea caused by that virus.
Proper handwashing can help prevent diarrhea.
When you travel, make sure anything your child eats and drinks is safe.
Next steps
Tips to help you get the most from a visit to your child’s health care provider:
Before your visit, write down questions you want answered.
At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you for your child.
If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Diarrhea (for Parents) - Nemours KidsHealth
What Is Diarrhea?
Diarrhea is frequent soft or loose bowel movements (poop).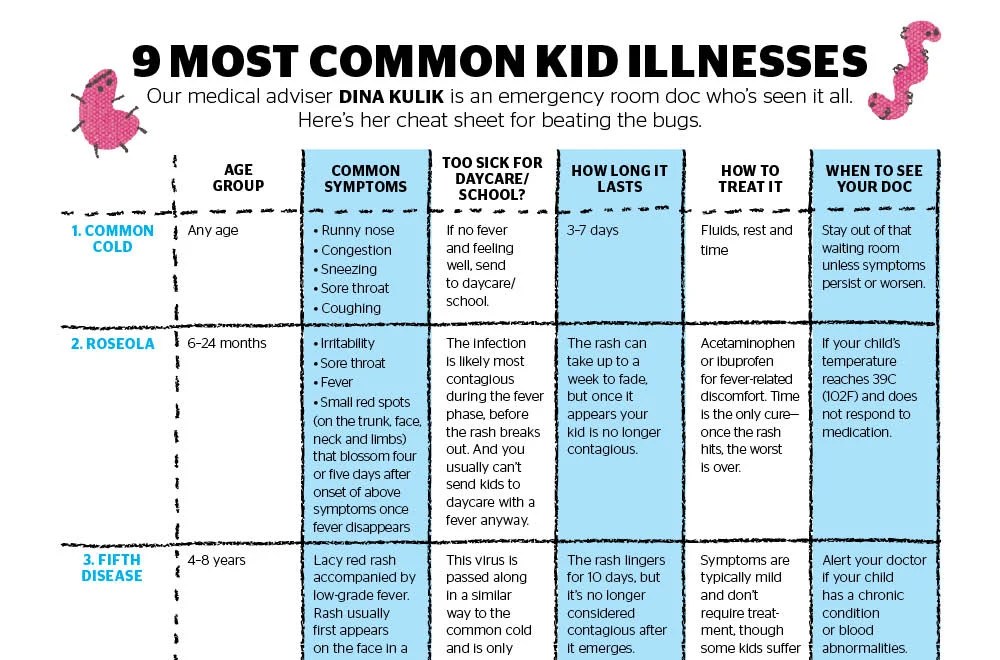 Most kids have diarrhea from time to time. It usually doesn't last long and often gets better on its own.
Most kids have diarrhea from time to time. It usually doesn't last long and often gets better on its own.
What Causes Diarrhea?
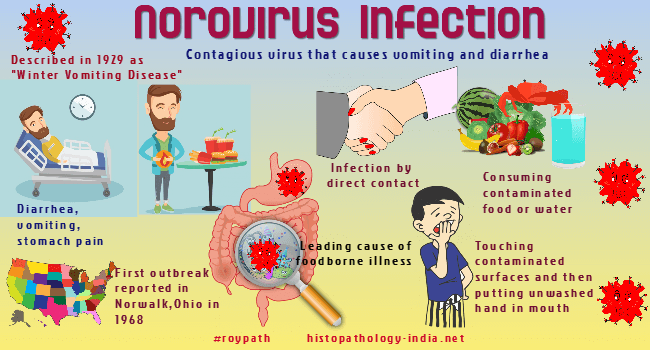
Diarrhea (dye-uh-REE-uh) is usually caused by an infection in the intestines, called gastroenteritis (gastro-en-ter-EYE-tiss).
Gastroenteritis can cause crampy belly pain, followed by diarrhea that lasts about 3–5 days. Other symptoms may include:
- fever
- loss of appetite
- nausea (an uncomfortable feeling before vomiting)
- vomiting
- weight loss
- dehydration
Children with diarrhea lasting longer than a couple of weeks may have other symptoms, depending on the cause.
The germs that cause gastroenteritis are:
- viruses (most common)
- bacteria
- parasites
Viruses
Viral gastroenteritis (or "stomach flu") is a top cause of diarrhea in kids. It also can bring on nausea, vomiting, and belly pain. Symptoms usually last a few days, and kids can get dehydrated if they don’t drink enough liquids while they’re sick.
Rotavirus is a common cause of watery diarrhea in infants and young children. Outbreaks are more common in the winter and early spring, especially in childcare centers. The rotavirus vaccine can protect children from this illness.
Norovirus is another common virus that causes watery diarrhea along with the other symptoms of gastroenteritis. Often, it’s spread through contaminated food and water.
Bacteria
Many different types of bacteria can cause diarrhea, including E. coli, Salmonella, Campylobacter, and Shigella. These bacteria are often responsible for food poisoning, which can cause diarrhea and vomiting within a few hours of eating contaminated food.
Parasites
Giardia is the most common parasitic infection that causes diarrhea in kids. Young children are more likely to get giardia, especially in childcare centers.
What Else Can Cause Diarrhea?
Kids can sometimes get diarrhea from:
- drinking too much juice and other sugar-sweetened beverages (sometimes called “toddler’s diarrhea”)
- food allergies
- lactose intolerance
- antibiotics
- medical problems like celiac disease and inflammatory bowel disease (Crohn's disease and ulcerative colitis), and irritable bowel syndrome
How Do Doctors Find the Cause of Diarrhea?
Doctors will:
- ask about what the child ate most recently, when symptoms began, and how often and how long the diarrhea is happening
- ask specific questions about the diarrhea: Is it watery? Is there blood in the poop?
- do an exam
- order a stool test, urine test, or blood test to check for dehydration and to see what’s causing the diarrhea, if needed
How Is Diarrhea Treated?
Diarrhea from viral gastroenteritis goes away on its own. Kids with bacterial diarrhea may need an antibiotic. Parasites always need treatment with anti-parasitic medicines. Don't give your child an over-the-counter anti-diarrhea medicine unless your doctor tells you to do so.
Kids with bacterial diarrhea may need an antibiotic. Parasites always need treatment with anti-parasitic medicines. Don't give your child an over-the-counter anti-diarrhea medicine unless your doctor tells you to do so.
Kids who aren't vomiting can continue eating and drinking as usual, if they feel up to it. Serve smaller portions of food until they feel better. Continuing a regular diet may shorten the amount of time they have diarrhea. Babies can continue to breastfeed or drink formula as long as they are not throwing up repeatedly.
If diarrhea is not from an infection, treatment will depend on what’s causing the problem.
How Can Parents Help?
For kids who show signs of mild dehydration, doctors recommend giving oral rehydration solutions (ORS) such as Pedialyte, Enfalyte, or a store brand. It has the right amount of water, sugar, and salt to help with dehydration. These are available in most grocery stores and drugstores without a prescription. Your doctor will tell you what kind to give, how much, and for how long.
Don’t give kids with diarrhea sports drinks, soda, or full-strength (undiluted) juice. They have too much sugar and can make some symptoms worse. Also, don’t give water alone.
In some cases, kids with severe diarrhea may need to get IV fluids (given into a vein) at the hospital treat dehydration.
When Should I Call the Doctor?
Call the doctor if your child:
- can’t drink for several hours
- is peeing less than usual
- has signs of dehydration, such as crying with few or no tears, having a dry mouth or cracked lips, feeling dizzy or lightheaded, acting very sleepy or less alert
- has a high fever
- has blood in their poop
- has diarrhea that doesn’t better after several days
Can Diarrhea Be Prevented?
Germs that cause gastroenteritis are contagious. That best way to avoid the illness is to keep the germs from spreading:
- Everyone in your family should wash their hands well and often.
 Wash for at least 20 seconds with soap and water. This is especially important after using the bathroom and before preparing or eating food.
Wash for at least 20 seconds with soap and water. This is especially important after using the bathroom and before preparing or eating food. - Clean tabletops, doorknobs, and other surfaces that get touched a lot with a cleaner that kills viruses.
- Follow food safety guidelines to prevent bacteria and viruses from getting into food and drinks (food poisoning).
- Make sure your kids get all recommended immunizations on time.
Diarrhea in a child | Treatment of diarrhea in children
Diarrhea in a child develops on the background of errors in nutrition, stress. Diarrhea is often a sign of an intestinal infection, inflammatory bowel disease, a manifestation of a food allergy, or drug damage. For the treatment of diarrhea in a child, an integrated approach is used: diet therapy, rehydration, drug therapy to eliminate the causes and consequences of diarrhea.
Causes and symptoms of diarrhea in a child
Diarrhea in children can be physiological and pathological, caused by the action of pathogens and other external stimuli. Let's consider these types in more detail.
Let's consider these types in more detail.
Physiological factors
Frequent bowel movements, liquid stools are normal for newborns and infants. Stools in infants may be pasty or unformed, and have a sour smell when breastfeeding. In children on artificial feeding, the stools are more dense and viscous.
Normally, the daily number of bowel movements in newborns is up to 8 times.
Short-term diarrhea is a frequent consequence of dietary errors. This can be caused by eating too many sweets or fatty, unhealthy foods at one time. In infants, physiological diarrhea occurs when changing the mixture, introducing complementary foods. Diarrhea can be a reaction to stress, but after the elimination of provoking factors, it disappears on its own.
With physiological diarrhea, the stool returns to normal within 1-2 days, the general state of health is normal, there are no other negative symptoms.
Acute intestinal infections (AII)
It is intestinal infections that most often cause diarrhea in children of different ages.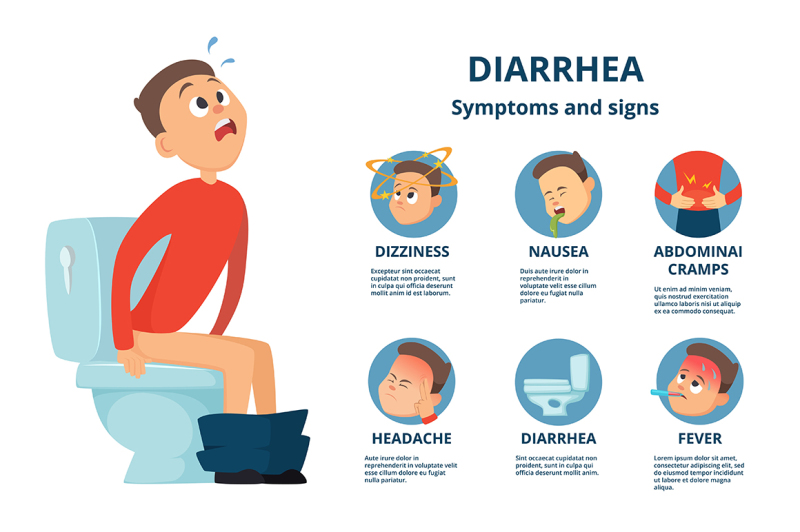 They are especially dangerous for children under 5 years of age due to the rapid development of dehydration.
They are especially dangerous for children under 5 years of age due to the rapid development of dehydration.
Intestinal infections always begin suddenly, proceed in an acute form. Infectious diarrhea is accompanied by nausea, vomiting, rumbling in the abdomen, flatulence, and sharp pain in the abdomen.
OII groups:
- Viral. The main causative agents of pathology in children are enteroviruses, rotaviruses. When entering the body, they cause loose stools with mucus impurities, the daily number of bowel movements increases up to 15–20 times. In severe secretory diarrhea, a watery discharge with a fecal odor is observed during bowel movements.
- Bacterial. Salmonellosis is accompanied by liquid green stools with a sharp unpleasant odor, with escherichiosis, stools become orange or bright yellow. With dysentery during defecation, a small amount of mucus interspersed with blood is released. A characteristic sign of cholera - feces resembles rice water.
- Protozoa. Signs of Giardia infection are similar to enterocolitis, enteritis. Amoebiasis is accompanied by mucous stools, in which there are many blood streaks.
Food allergy
In allergic enterocolitis, a child has loose stools with a lot of mucus and particles of undigested food. In a severe course of the disease, blood impurities appear in the feces. The severity of symptoms depends on the amount of the allergen that has entered the body, the type of allergic reaction.
Diarrhea occurs hours or days after exposure to the allergen. In addition, skin and respiratory signs of allergy are observed.
Chronic pathologies of the gastrointestinal tract
In diseases of the digestive system, diarrhea lasts more than two weeks, periods of remission are replaced by an exacerbation phase. The problem mainly occurs in schoolchildren against the background of non-infectious lesions of the digestive system.
Disease groups:
- Congenital pathologies.
 Protracted and repeated diarrhea in a child occurs with celiac disease, disaccharidase deficiency. Diarrhea occurs after eating intolerable foods. Fecal masses have an unpleasant odor, liquid with particles of undigested food.
Protracted and repeated diarrhea in a child occurs with celiac disease, disaccharidase deficiency. Diarrhea occurs after eating intolerable foods. Fecal masses have an unpleasant odor, liquid with particles of undigested food. - Somatic diseases. Periodically, diarrhea occurs when the rules of nutrition and treatment of cholecystitis, pancreatitis, and hepatitis are violated. Exacerbation develops after the use of prohibited foods. Loose stools are accompanied by pain in the abdomen in the area of \u200b\u200bthe diseased organ, bouts of nausea and vomiting.
- Inflammatory processes in the intestines. Crohn's disease is accompanied by repeated diarrhea, severe pain in the abdomen. In the feces, blood is often present in the form of scarlet streaks or dark clots. Signs of nonspecific ulcerative colitis - poor diarrhea, blood in the stool.
Inflammation of the appendix
In children, an attack of acute appendicitis often resembles food poisoning: there are repeated diarrhea without foreign impurities, refusal to eat, nausea, single vomiting, pain in the navel, in the right side. In this case, the protective tension of the muscles of the peritoneum, pathognomonic physical symptoms can be blurred.
In this case, the protective tension of the muscles of the peritoneum, pathognomonic physical symptoms can be blurred.
Consequence of antibiotic therapy
The problem often occurs in children of the first years of life due to the inferiority of the intestinal microflora. Most often, loose stools are observed during treatment with macrolides, lincosamides, cephalosporin or tetracycline antibiotics. Diarrhea up to 15 times a day, feces frothy, greenish, with a pungent odor.
Diarrhea in newborns
Diarrhea in newborns is most often physiological, diarrhea occurs against the background of adaptation of the digestive tract. If the number of bowel movements in infants up to three months is not more than 7 times a day, there are no other negative symptoms, there is no reason for concern.
Abnormal diarrhea in a newborn may be a manifestation of hereditary diseases - enzymatic deficiency, congenital chloride diarrhea or exudative enteropathy. Less commonly, the cause of diarrhea in infants is a viral infection, dysbiosis.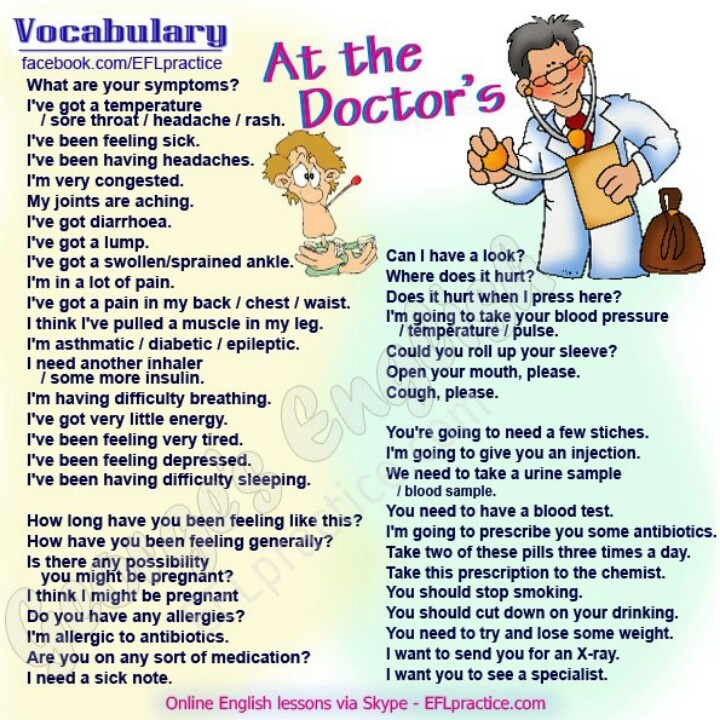 Dysbacteriosis develops against the background of late attachment to the breast, with artificial feeding, errors in the mother's diet, and taking antibiotics.
Dysbacteriosis develops against the background of late attachment to the breast, with artificial feeding, errors in the mother's diet, and taking antibiotics.
Diarrhea in an infant up to one year old
After the introduction of complementary foods, food allergies and intolerance to certain products often appear. Diseases are manifested in the form of foamy stools, bloating.
Celiac disease, or gluten intolerance, develops 1–3 months after the introduction of products that contain barley, wheat, rye into the child's diet. The second common cause of diarrhea in children under one year old is an allergy to cow's milk protein, which manifests itself after the introduction of dairy products.
Loose stools can be caused by the abuse of juices, water, mixtures. Such diarrhea does not apply to pathologies, it disappears after correction of feeding.
Diarrhea in children from one year old
After 12 months, the child begins to actively explore everything around, often puts hands and foreign objects in his mouth.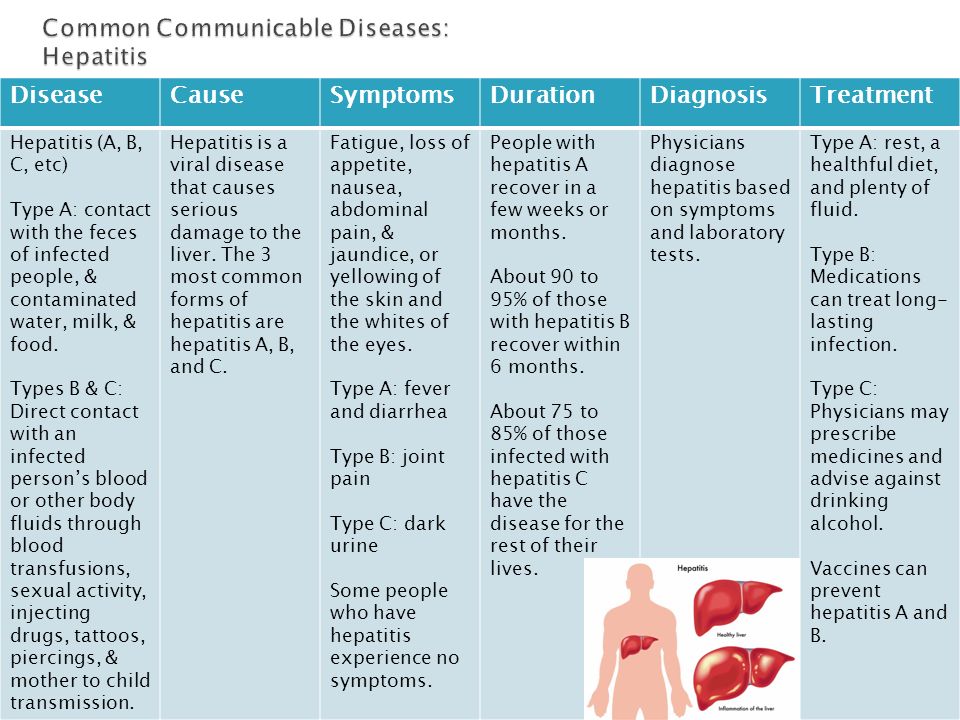 As a result, the likelihood of poisoning, the development of infectious diarrhea of a viral or bacterial nature increases.
As a result, the likelihood of poisoning, the development of infectious diarrhea of a viral or bacterial nature increases.
Diarrhea may be caused by atony or weak bowel contraction. The problem occurs with some lesions of the nervous system, stress.
After 18 months, the child may develop adult-type lactase deficiency. In infancy, there was enough lactase, but as they grow older, the synthesis of the enzyme slowed down. After a year, there may be debuts of inflammatory, autoimmune bowel diseases, irritable bowel syndrome. Most often, these diseases begin after severe stress, nervous shock.
Do's and Don'ts:
- force-feed if you have no appetite;
- give antibiotics, antidiarrheals, enzymes and other medicines without a doctor's prescription;
- use potassium permanganate for gastric lavage;
- vomiting and diarrhea are protective reactions, as the body is cleansed of toxins, so it is impossible to immediately give medicines for diarrhea and vomiting;
- prohibit drinking water for fear of vomiting.
Be sure to call a doctor if:
- there are blood impurities in the feces, vomit;
- dark green vomit;
- the child completely refuses to eat, drink;
- there was a sharp and severe pain in the right side of the abdomen;
- the temperature rose sharply;
- diarrhea lasting more than 8–12 hours;
- the child is constantly thirsty;
- there were signs of dehydration - dry skin and mucous membranes, a decrease in the volume of urine and the number of urination, no tears when crying, retraction of the fontanel in the baby.
Diagnosis
If your child has frequent diarrhea, visit the pediatrician. After collecting anamnesis, physical examination, consultation with a gastroenterologist, allergist, infectious disease specialist may be required.
Diagnostic methods:
- Ultrasound of the abdominal cavity. Assign to exclude urgent surgical conditions, to study the structural features of the gastrointestinal tract.
 It is possible to identify chronic inflammatory processes, congenital malformations, symptoms of damage to the liver, pancreas, and other organs of the gastrointestinal tract.
It is possible to identify chronic inflammatory processes, congenital malformations, symptoms of damage to the liver, pancreas, and other organs of the gastrointestinal tract. - X-ray of the gastrointestinal tract with contrast. The study of the state of the walls of the stomach, intestines, colon.
- Fecal analysis. The coprogram shows the presence of undigested food particles, striated muscle fibers, an increase in the level of mucus, leukocytes.
- Bakposev, PCR of feces. Assign to exclude or confirm viral, bacterial intestinal infections.
- Clinical, biochemical blood test. It is carried out to identify the inflammatory process, assess the functioning of internal organs, the degree of dehydration, and select effective therapy.
- Serological blood tests are necessary in severe infectious pathologies.
Treatment
Before diagnosis, the main goal is to avoid dehydration. The child needs to drink a little salted water, dried fruit compote, rice water - often, but in small portions of 1-2 tsp. every 5-10 minutes, the liquid should be warm. After each bowel movement, drink 50–200 ml of water. To quickly cleanse the body of toxins, give enterosorbents.
every 5-10 minutes, the liquid should be warm. After each bowel movement, drink 50–200 ml of water. To quickly cleanse the body of toxins, give enterosorbents.
Conservative therapy in a satisfactory condition of the child can be carried out on an outpatient basis. In severe, dangerous pathological conditions, hospitalization in the infectious, gastroenterological, and surgical departments is required.
The treatment regimen depends on the severity of dehydration:
- For mild exsicosis, oral rehydration agents are prescribed. Breastfed babies need to breastfeed more often.
- For moderate dehydration, an increased fluid load is administered orally in the first 4 hours to eliminate the effects of frequent defecation. After improving the patient's well-being, they are transferred to standard maintenance rehydration.
- For severe dehydration, saline solutions are given intravenously. The volume depends on the patient's body weight, blood test results.

Diet therapy is an important part of the treatment of diarrhea in a child. In the early days, sparing nutrition is shown: slimy soups, pureed cereals, biscuit cookies, stewed vegetables in a small amount. Gradually, lean meat dishes, dairy products are introduced into the diet. If diarrhea is caused by diseases of the gastrointestinal tract, intolerance to certain foods, the diet is prescribed taking into account the underlying disease.
Drugs for drug therapy are selected according to the cause of diarrhea in a child. For mild and moderate intestinal infections, specific treatment is not required. Antibiotics are prescribed for severe bacterial infections, primary or secondary immunodeficiency, with a history of severe concomitant diseases.
Pathogenetic treatment - enterosorbents, drugs for vomiting and diarrhea. Probiotics and prebiotics are prescribed to restore the balance of the intestinal microflora.
Acute appendicitis requires emergency surgery.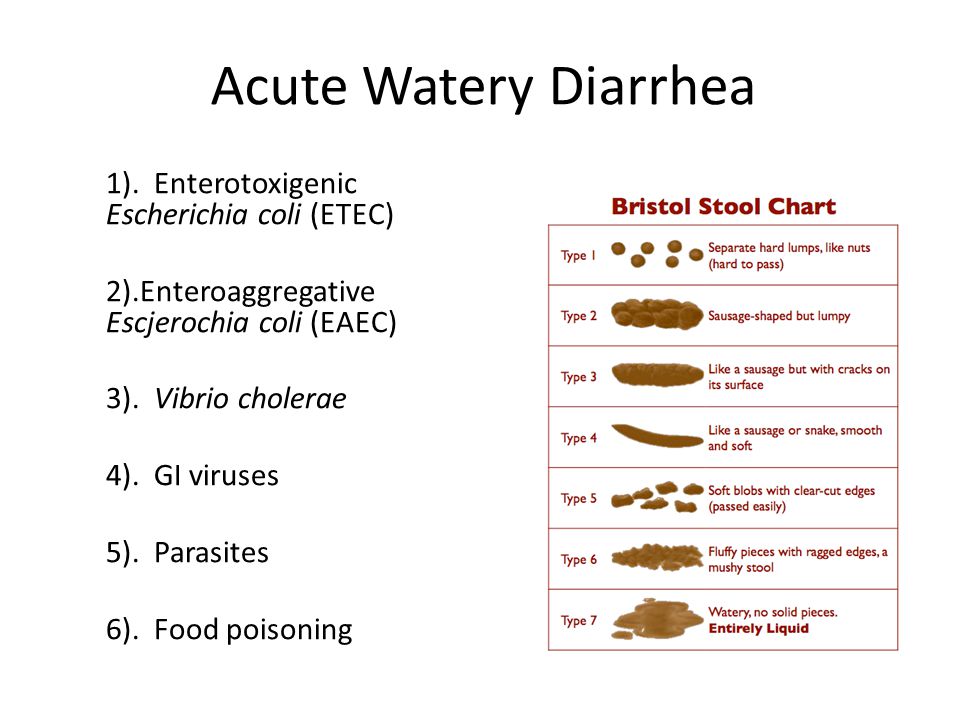 Elective surgeries are performed for severe, recurrent bowel diseases - Crohn's disease, ulcerative colitis. Surgical treatment is necessary to eliminate bleeding, remove the ulcerated area, segmental resection, and anastomosis.
Elective surgeries are performed for severe, recurrent bowel diseases - Crohn's disease, ulcerative colitis. Surgical treatment is necessary to eliminate bleeding, remove the ulcerated area, segmental resection, and anastomosis.
Features of the treatment of diarrhea in newborns, infants and toddlers
Diarrhea often occurs in children of different ages, and parents are not always in a hurry to see a doctor. But in infants, diarrhea is more severe than in adults, and severe dehydration quickly develops, since there is practically no internal fluid supply. Therefore, with frequent and loose stools in a child, it is imperative to consult a doctor.
At home, you need to give your child a little water to make up for the lack of liquid. Slightly salted water is suitable for small children. Older children - rice water, weak tea without sugar, vegetable broth, special pharmacy solutions for rehydration. You can not drink sweet and carbonated drinks, juices. But if the child wants to drink only forbidden drinks and they do not cause an attack of vomiting, let him drink.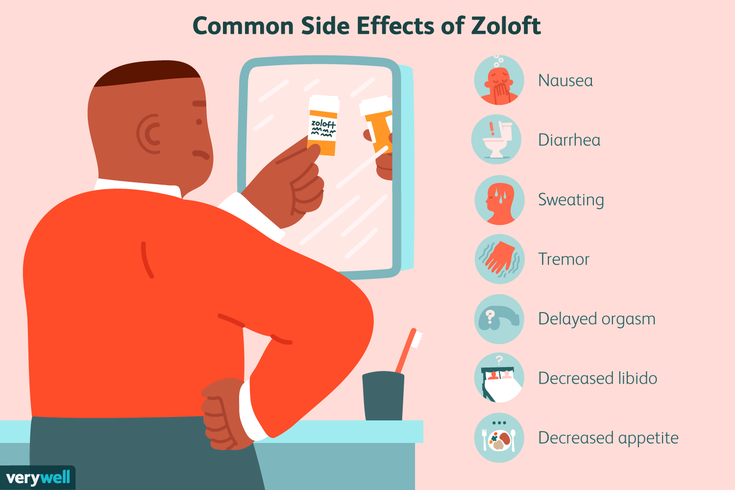 In such situations, it is important that some kind of liquid constantly enters the body.
In such situations, it is important that some kind of liquid constantly enters the body.
There are no restrictions on the amount of fluid consumed. Minimum - 50-200 ml after each bowel movement. In severe dehydration, the fluid is urgently started to be administered intravenously.
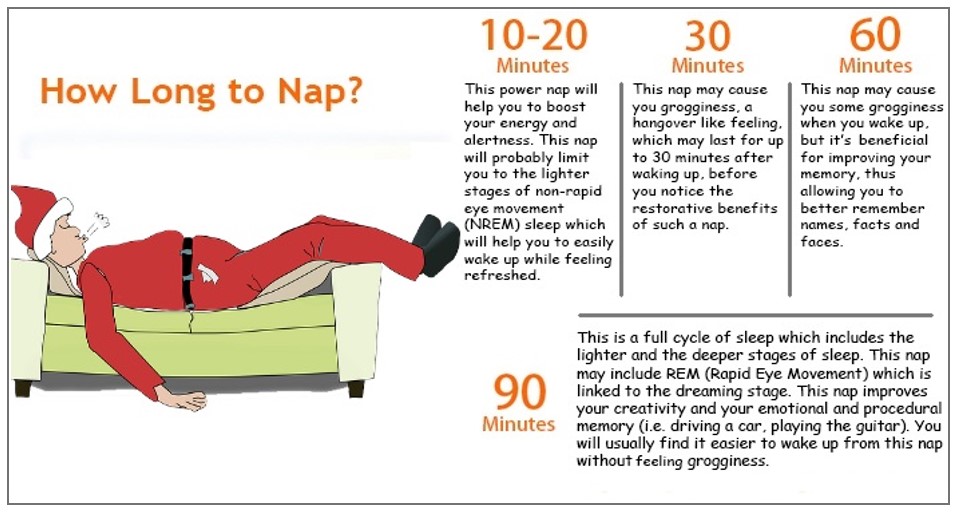
With diarrhea, appetite often disappears, it is recommended to completely refuse food for 4-6 hours, but this method is not suitable for small children. With diarrhea, the absorption of nutrients is disrupted, and a long break between meals is dangerous.
Children with diarrhea should be given light but nutritious meals. During the acute period, a diet of rice, applesauce, bananas and toast or crackers is indicated, with the addition of tea. The diet helps to cope with diarrhea, but contains little protein, so you can’t stick to it for a long time.
Babies with diarrhea can be switched to a lactose-free formula. If diarrhea started after the introduction of complementary foods, it is better to temporarily stop complementary foods.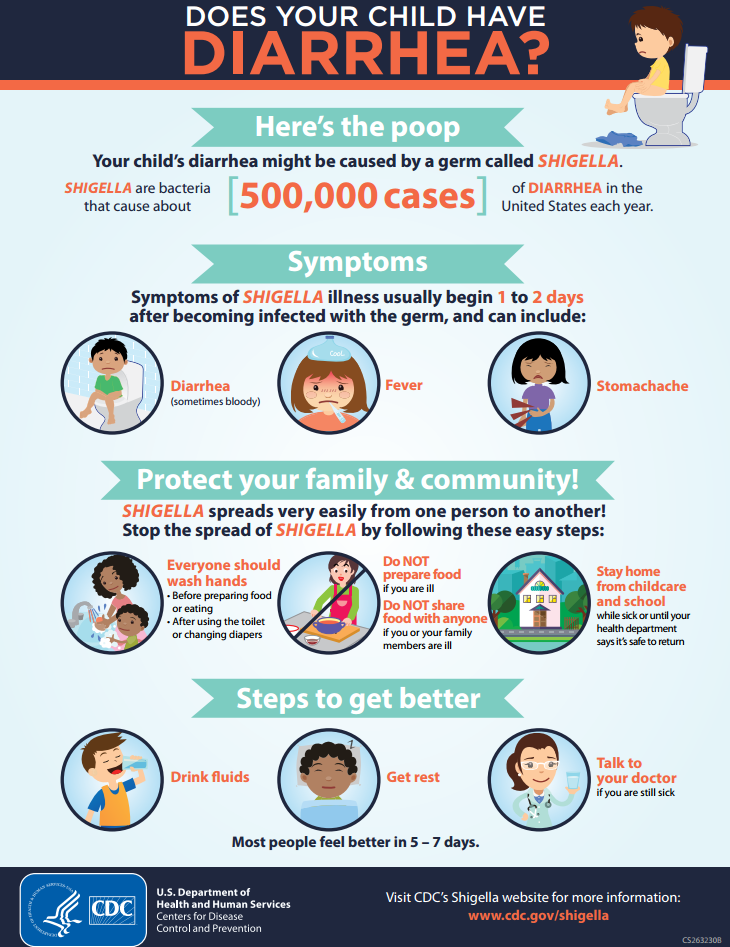
Antiviral and antimicrobial drugs, enzymes can only be prescribed by a doctor. Self-medication will do more harm than good. Sorbents can be given independently, preferably in the form of a suspension, powder. Activated charcoal adversely affects the thin gastric mucosa.
Prevention
To avoid a recurrence of diarrhea in a child, it is necessary to thoroughly wash vegetables, fruits, and hands. The baby can only drink purified water. Children should not be given food without proper heat treatment.
Babies should be gently weaned from the habit of putting their hands in their mouths, trying everything by mouth. If this has not been done yet, you should often carry out wet cleaning using natural safe detergents, disinfect nipples, toys.
Viral gastroenteritis (children)
Most cases of diarrhea and vomiting in children are caused by a virus. This is viral gastroenteritis. Many people call it "stomach flu" but it has nothing to do with the flu. This virus infects the stomach and intestinal tract. The disease lasts from 2 to 7 days. Diarrhea means loose or watery stools that are different from a baby's normal bowel movements.
This virus infects the stomach and intestinal tract. The disease lasts from 2 to 7 days. Diarrhea means loose or watery stools that are different from a baby's normal bowel movements.
The child may also have the following symptoms:
The main danger of this disease is that it leads to dehydration. This is the loss of a large amount of water and mineral salts by the body. In such cases, fluid loss by the body must be replenished. This is done with oral rehydration solution. These solutions are available from pharmacies and most grocery stores without a prescription.
Antibiotics do not help with this illness.
Home care
Follow your pediatrician's instructions.
If you give medicine to your child:
-
Do not use over-the-counter diarrhea medications unless your doctor tells you to.
-
Acetaminophen or ibuprofen can be used for pain and fever.
 Or another medicine as prescribed.
Or another medicine as prescribed. -
Aspirin as an antipyretic is contraindicated in children under 18 years of age. Its use can lead to serious liver problems and a life-threatening condition called Reye's syndrome.
To prevent the spread of disease:
-
Remember that washing your hands with soap and clean running water or using an alcohol-based disinfectant is the best way to prevent the spread of infection.
-
Teach all family members when and how to wash their hands. Wet your hands with clean running water. Apply soap to the back of your hands, between your fingers and under your nails. Rub your hands for at least 20 seconds. If you need a timer, try singing "Happy Birthday to You!" twice. from the beginning to the end. Rinse your hands well and dry with a clean towel.
-
Wash your hands before and after caring for your sick child.
-
Clean the toilet after each use.
-
Dispose of soiled diapers in an airtight container.
-
Keep the child away from other people until the doctor says so.
-
Wash your hands before and after preparing food.
-
Wash hands and utensils after using cutting boards, countertops and knives that have been in contact with raw food.
-
Keep raw meat away from cooked and ready-to-eat foods.
-
Please note that people with diarrhea or vomiting should not prepare food for others.

How to properly water and feed
The main goal in the treatment of vomiting or diarrhea is to prevent dehydration. To do this, the child should often consume liquids in small portions.
-
Fluid is now more important than food. Give a small amount of liquid at a time, especially if the child has stomach cramps or is vomiting.
-
For diarrhea: If you are giving milk to a baby and the diarrhea does not stop, refuse the milk. In some cases, milk can make diarrhea worse. If this happens, use an oral rehydration solution. Eliminate apple juice, soda, sports or other sweetened drinks. Drinks with sugar can make diarrhea worse.
-
For vomiting: Start with oral rehydration solution at room temperature.
 Give 1 teaspoon (5 ml) every 5 minutes. Even if the child is vomiting, continue to give the solution. Most of the fluid will be absorbed despite vomiting. After 2 hours without vomiting, start with a small amount of milk or formula and other liquids. Increase the amount depending on tolerance. Do not give your child plain water, milk, formula, or other liquids until the vomiting stops. Give more oral rehydration solution as vomiting decreases. Increase the interval between doses. Continue until the child has urine and is no longer thirsty (no interest in drinking). If there has been no vomiting within 4 hours, resume feeding solid food. After 24 hours without vomiting, resume normal eating.
Give 1 teaspoon (5 ml) every 5 minutes. Even if the child is vomiting, continue to give the solution. Most of the fluid will be absorbed despite vomiting. After 2 hours without vomiting, start with a small amount of milk or formula and other liquids. Increase the amount depending on tolerance. Do not give your child plain water, milk, formula, or other liquids until the vomiting stops. Give more oral rehydration solution as vomiting decreases. Increase the interval between doses. Continue until the child has urine and is no longer thirsty (no interest in drinking). If there has been no vomiting within 4 hours, resume feeding solid food. After 24 hours without vomiting, resume normal eating. -
As you feel better, you can gradually resume your child's normal diet. Don't force your child to eat, especially if they have stomach pain or cramps. Do not feed your baby large portions at a time, even if he is hungry. Tobacco smoke can make a child feel worse.
 Over time, the child can be given more food, provided it is tolerated. Foods that are allowed include cereals, mashed potatoes, applesauce, mashed bananas, crackers, dry toast, rice, oatmeal, bread, noodles, pretzel, rice or noodle soups, and cooked vegetables.
Over time, the child can be given more food, provided it is tolerated. Foods that are allowed include cereals, mashed potatoes, applesauce, mashed bananas, crackers, dry toast, rice, oatmeal, bread, noodles, pretzel, rice or noodle soups, and cooked vegetables. -
If symptoms return, return to a simple or no therapeutic diet.
Postoperative care
See your pediatrician or follow his instructions. If a stool or culture test is taken, see your doctor for results as directed.
Call 911
Call 911 if your child has any of these symptoms:
-
Labored breathing
-
Confusion
-
Extreme drowsiness or loss of consciousness
-
Trouble walking
-
Rapid pulse
-
Chest pains
-
Neck stiffness
-
Convulsions
When to seek medical help
Seek immediate medical attention in the following cases:
-
Abdominal pain worse
-
Constant pain in the right lower abdomen
-
Recurrent vomiting after first 2 hours of fluid intake
-
Episodic vomiting for more than 24 hours
-
Continuous severe diarrhea for more than 24 hours
-
Blood in stool or vomit
-
Child drinks less liquid than usual
-
Darkening or no urine for 6 to 8 hours in older children, 4 to 6 hours in toddlers
-
Whims or crying when the child cannot be soothed
-
Unusual drowsiness
-
New skin eruptions
-
Diarrhea lasting more than 10 days
-
Temperature (see Temperature and children below)
Temperature in children
Use a digital thermometer to take your baby's temperature. Never use a mercury thermometer. There are various types and ways of using digital thermometers. For example:
Never use a mercury thermometer. There are various types and ways of using digital thermometers. For example:
-
Rectal. For children under 3 years of age, rectal temperature is the most accurate.
-
Frontal (temporal). It is used for children aged 3 months and older. If a child under 3 months of age has signs of illness, this method can be used for the first measurement. The doctor may also check the rectal temperature for confirmation.
-
Ear (tympanic). The ear method is accurate for children from 6 months, but not younger.
-
Axillary (axillary). This is the least reliable method, but it can be used for the first measurement to test a child of any age who shows signs of illness.
 The doctor may also check the rectal temperature for confirmation.
The doctor may also check the rectal temperature for confirmation. -
Oral (oral). Do not take oral temperature until child is 4 years of age.
Use the rectal thermometer with care. For correct use, follow the manufacturer's directions. Insert it carefully. Make a note on it and make sure it will not be used orally. It can carry germs from the stool. If a rectal thermometer doesn't work for you, ask your doctor which thermometer is best to use. When you tell a doctor about your child's temperature, tell him what type of thermometer you took it with.
Here are some tips to help you know if your baby has a fever. Your child's doctor may give you other values. Follow your healthcare provider's instructions.
Temperature readings for infants up to 3 months:
-
Rectal or forehead thermometer: 38°C (100.
 4°F) or higher
4°F) or higher -
Underarm thermometer: temperature 37.2 °C (99 °F) or higher
Temperature readings for children aged 3 to 36 months (3 years):
-
Rectal, forehead or ear thermometer: temperature 38.9°C (102°F) or higher
-
Axillary thermometer: temperature 38.3 °C (101 °F) or higher
Call a doctor if:
-
Recurrent fever of 40°C (104°F) or more in a child of any age
-
Temperature 38°C (100.4°F) or higher in an infant under 3 months
-
Temperature lasting more than 24 hours in a child under 2 years of age
-
Temperature that persists for 3 days in a child 2 years of age or older
© 2000-2022 The StayWell Company, LLC.