Are you born with epilepsy
Genetic Causes of Epilepsy | Epilepsy Foundation
- Home
- Causes of Epilepsy
- Genetic Causes of Epilepsy
What Is Genetic Epilepsy?
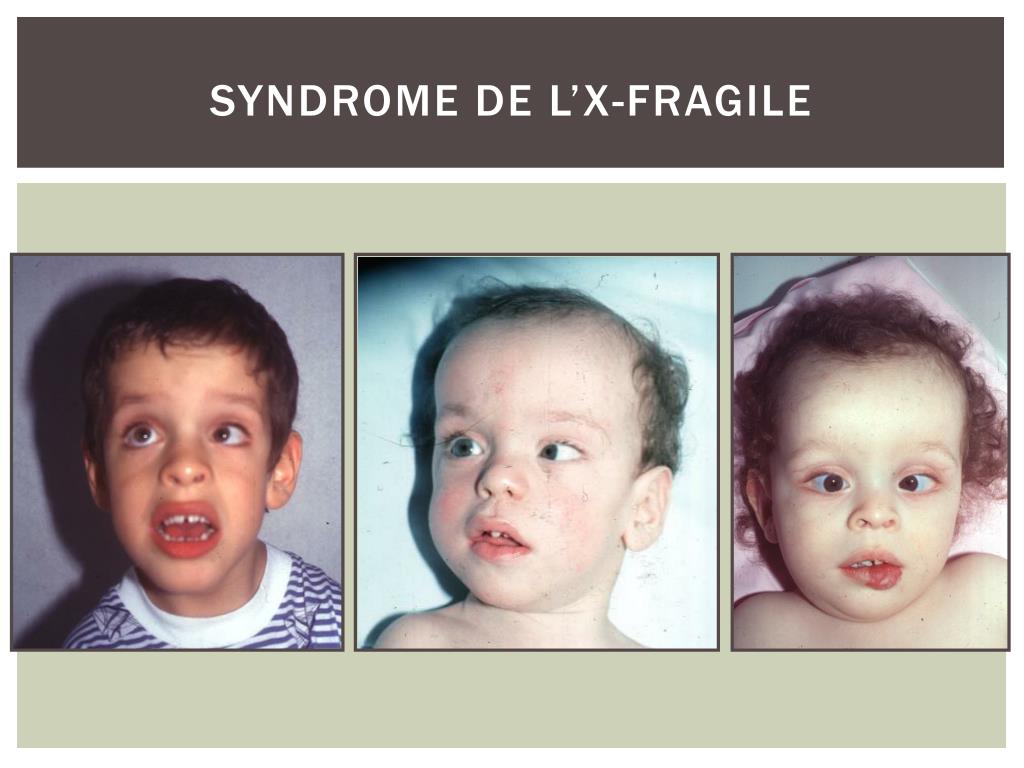
Epilepsy is said to have a genetic cause if seizures are the result of a known or presumed genetic defect or problem associated with epilepsy. A genetic epilepsy might not be inherited. Some genetic pathogenic variants (or changes in genes) can occur spontaneously in a child without being present in either parent. Furthermore, some epilepsies with a genetic cause may also have additional environmental causes as well.
What are the symptoms of genetic epilepsy?
Genetic epilepsies can present with a broad range of seizure types. Genetic factors are more likely if there is a strong history of epilepsy in other family members.
However, genetic causes are also common in children who develop epilepsy very early in life, and who have a normal MRI and other blood tests. In these cases, the genetic change usually happens for the first time the child, and a family history of epilepsy is often absent.
How do you get a genetic epilepsy?
A genetic epilepsy occurs when an individual inherits a gene, or a number of genes that result in a higher likelihood of seizures. In many cases of idiopathic generalized epilepsy (such as childhood absence epilepsy, juvenile absence epilepsy, juvenile myoclonic epilepsy or epilepsy with generalized tonic-clonc seizures alone), epilepsy is the result of inheriting a number of abnormal genes, each of which contribute a relatively small amount to the risk of seizures. If one inherits a number of these genes, epilepsy is more likely.
How do you treat it?
Most often, treatment for genetic epilepsy is with anti-seizure medicine, that is chosen based on the seizure type or syndrome.
Some genetic changes result in metabolic abnormalities and a specific supplement or special diet can be helpful.
As we understand more about the genetic changes in some of the rare epilepsies that are due to an abnormality in a single gene, we will begin to see treatments that can target the specific gene abnormality.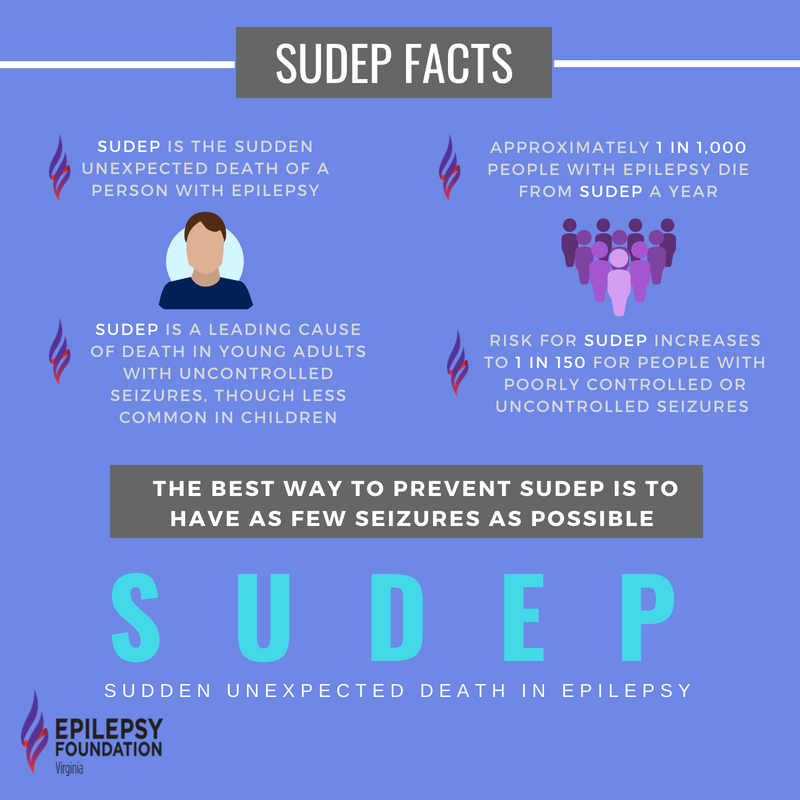 Such therapies may have the potential to reduce other challenges often seen with these epilepsies, such as learning problems and intellectual disability, as well as improve seizures. However, therapies targeting specific rare genes are in the research phase, and not yet available for these rare epilepsies.
Such therapies may have the potential to reduce other challenges often seen with these epilepsies, such as learning problems and intellectual disability, as well as improve seizures. However, therapies targeting specific rare genes are in the research phase, and not yet available for these rare epilepsies.
Types Of Genetic Epilepsy
- Specific Genetic Epilepsies
- Angelman syndrome
- CDKL5
- PCDh29
- Ring chromosome 20
- SCN8A related
- SLC2A1 (Glut1 Deficiency Syndrome)
- TBCK-related ID
- Rett-MECP2
- FOXG1
- Dup 15q
- SYNGAP1-related epilepsy
- KCNQ2
- KCNQ3
- STXBP1
- SCN1A
- SCN2A
- ARX
- CHD2
- GRIN2A
- PRRT2
- KCNT1
- CLN2 and other CLN genes
- POLG1
- Ring 14
- Phelan McDermid
- STRADA
- DNM1
- PTEN
- SLC25A22
- SPTAN1
- FOLR1
- CACNA1A
- HCN1
- WWOX
- GRIN2B
- GABRA1
- LGI1
- MEF2C
- SLC6A1
- SLC13A5
- ALDH7A1
- CHRNA4
- SMC1A
Learn More About Genetics And Epilepsy
- Genetics: The Basics
- Epilepsy and Genes
- Genetic Counseling
- Genetic Testing and Epilepsy
- Genetic Resources
Authored By:
Elaine Wirrell MD
Previous
Tuberous Sclerosis Complex (TSC)
Next
Genetic Testing for Epilepsy
Resources
Epilepsy centers provide you with a team of specialists to help you diagnose your epilepsy and explore treatment options.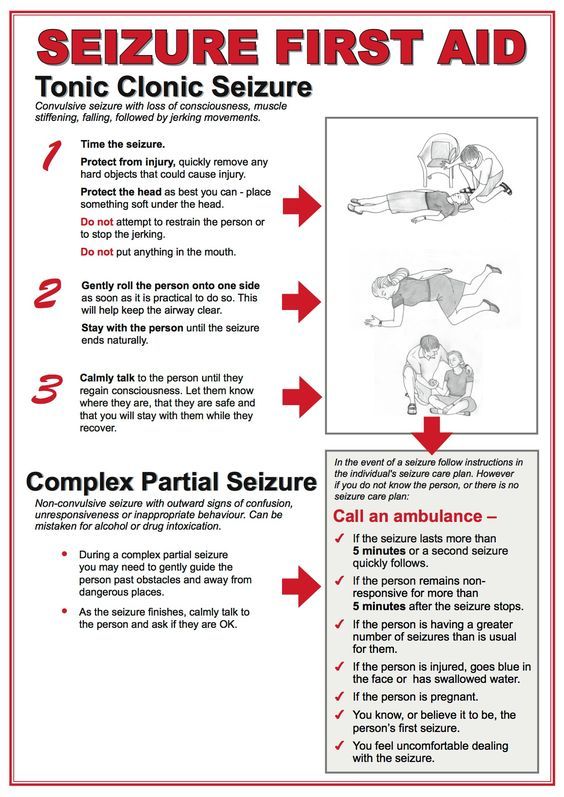
>
Find in-depth information on anti-seizure medications so you know what to ask your doctor.
>
Call our Epilepsy and Seizures 24/7 Helpline and talk with an epilepsy information specialist or submit a question online.
>
Download our seizure tracking app, print out seizure action plans, or explore other educational materials.
>
Related Stories
Healthy Living
Mental Health and Epilepsy in the Black Community
Research & Innovation
COVID-19 Vaccination and Dravet Syndrome
Research & Innovation
Nominations Open for 2023 Lifetime Accelerator Award
Ready for help? Find an Epilepsy specialist who can help guide you through your epilepsy journey.
Find a Doctor Near You
Structural Causes of Epilepsy | What Is Structural Epilepsy?
On this page:
What Is A Structural Epilepsy?
Epilepsy is said to have a structural cause if there is a distinct abnormal structural cause present in the brain that is known to substantially increase the risk of seizures.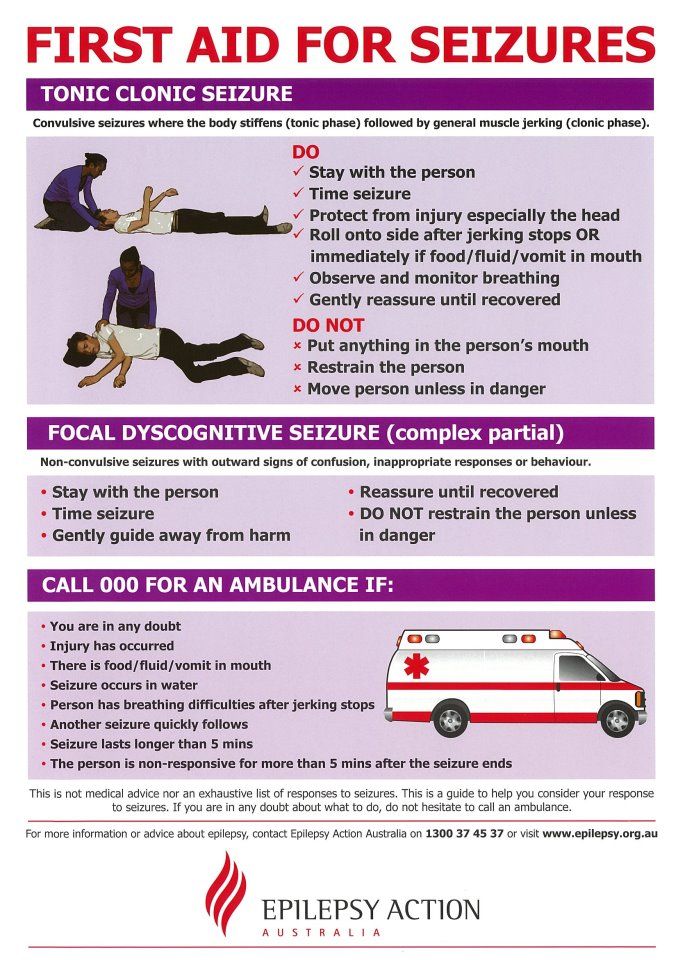 Most of these causes can be seen on imaging of the brain with an MRI.
Most of these causes can be seen on imaging of the brain with an MRI.
What Are The Symptoms Of A Structural Epilepsy?
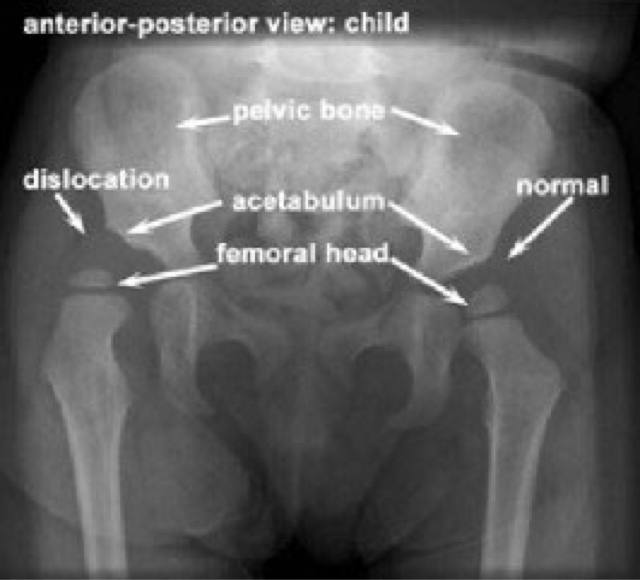
Structural epilepsies in older children and adults most commonly present with focal seizures and have very similar symptoms from event to event. In some cases, seizures can spread to both sides of the brain, leading to a generalized tonic-clonic seizure.
Persons with structural causes may also have other symptoms that reflect a structural abnormality in one brain area, such as difficulty using one arm or leg, or one half of the body, difficulty with speech, difficulty with vision on one side, and so forth.
Infants and young children with structural epilepsies may also present with focal seizures or may present with other seizure types such as infantile spasms or tonic seizures. In such cases, there is often a slowing of development once seizures begin.
In most persons with a structural epilepsy, the brain MRI is abnormal.
How Do You Get A Structural Epilepsy?
Structural abnormalities can be congenital or acquired.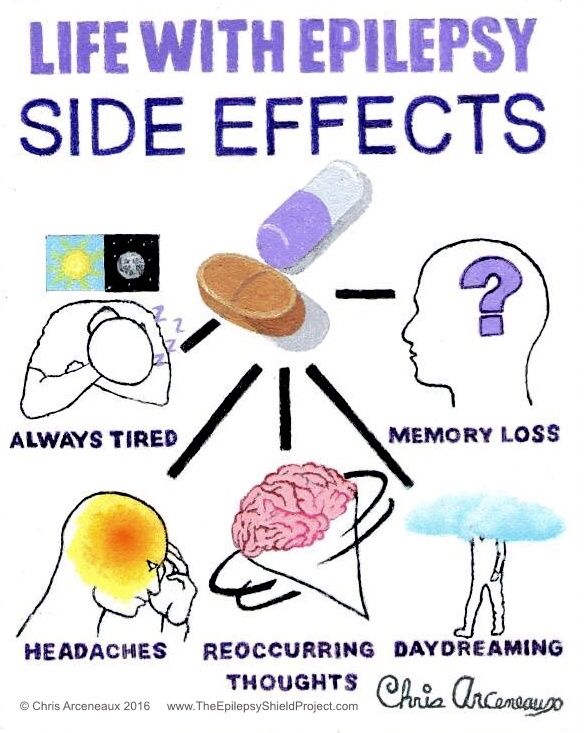
- A congenital cause is a developmental change in the brain that a person is born with. Some congenital structural causes may also have a genetic component. In most cases, these changes are seen in babies born to women whose pregnancies have been otherwise normal, and we do not understand why these changes occur. In some cases of congenital structural causes, seizures begin very early in life. In other cases, seizures begin many years after birth, often in later childhood or even early adulthood.
- An acquired cause is due to a process or injury that occurs in someone with previously normal brain structure. Examples are brain tumors, strokes or head trauma. These injuries lead to the brain being more susceptible to seizures and epilepsy can occur.
How Do You Treat It?
Anti-seizure medicines are most commonly the initial treatment for persons with a structural abnormality. However, in some cases, such as tumors or blood vessel abnormalities, surgery is required to treat the underlying cause.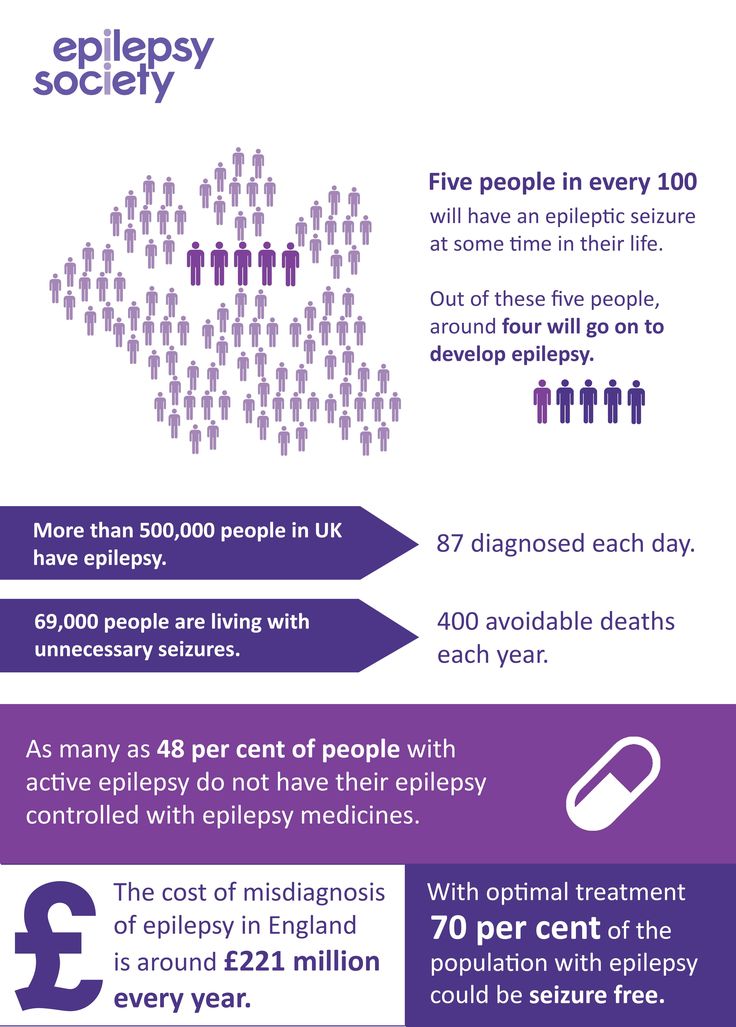
While many persons with structural cases will have their seizures controlled with anti-seizure medicine, a proportion will continue to have seizures, and will develop drug-resistant epilepsy. Many persons with structural epilepsy and drug-resistant seizures can be candidates for epilepsy surgery. It is recommended that persons who continue to have seizures despite trials of two anti-seizure medications be seen at a Comprehensive Epilepsy Center.
Specific Structural Causes Associated With Epilepsy
- Hypothalamic hamartoma
- Aicardi syndrome
- Focal cortical dysplasia
- Cavernous and other vascular malformations
- Dysembryoplastic neuroepithelial tumors (DNETS), gangliogliomas and low-grade tumors
- Mesial temporal sclerosis (MTS)
- Multiple Sclerosis
- Traumatic brain injury (TBI)
- Perinatal brain injury
- Vascular injury
- Hemimegalencephaly
- Schizencephaly
- Periventricular nodular heterotopia (PVNH)
- Polymicrogyria (PMG)
Neurocutaneous syndromes are a group of neurologic (brain, spine, and peripheral nerve) disorders that can cause cutaneous (skin) manifestations, such as tumors that grow inside the brain, spinal cord, organs, skin, and skeletal bones. These disorders frequently also cause seizures, brain malformations, eye lesions, and intellectual disability.
These disorders frequently also cause seizures, brain malformations, eye lesions, and intellectual disability.
Neurocutaneous syndromes that can be associated with seizures include
- Incontinentia pigmenti
- Neurofibromatosis Type 1
- Sturge Weber Syndrome (Encephalotrigeminal Angiomatosis)
- Tuberous Sclerosis Complex
Authored By:
Elaine Wirrell MD
on Wednesday, December 30, 2020
on Monday, October 15, 2018
Epilepsy in children: Part 1 - manifestations and first aid for seizures
Seizures are common in children and adults. According to the World Health Organization, up to 10% of the world's population experience at least one seizure during their lifetime. Most often, seizures occur in childhood and old age.
Epilepsy is a chronic disease with recurrent convulsive and non-convulsive seizures resulting from excessive electrical discharges in the brain. There are many forms of epilepsy with different clinical manifestations and causes - from hereditary diseases to the consequences of brain injuries. Currently, a separate area dedicated to epilepsy has emerged in neurology - epileptology. A neurologist who specializes in diagnosing and treating epilepsy is called an epileptologist.
Currently, a separate area dedicated to epilepsy has emerged in neurology - epileptology. A neurologist who specializes in diagnosing and treating epilepsy is called an epileptologist.
What do seizures look like?
The special literature describes dozens of types of seizures, and even more - their combinations, so you should limit yourself to basic concepts. The most famous are the so-called generalized tonic-clonic seizures with loss of consciousness, tension and twitching throughout the body. In addition, there are myoclonic seizures, which are short shudders in the whole body or in any part of it, often without a change in consciousness - for example, shuddering of the hands with objects falling out of them, or a sudden fall as if from a blow to the knees.
Tonic attacks are manifested by sufficiently prolonged muscle tension in any part of the body.
In children, an attack can often look like tension and trembling of the arm, half of the face with speech impairment while maintaining consciousness.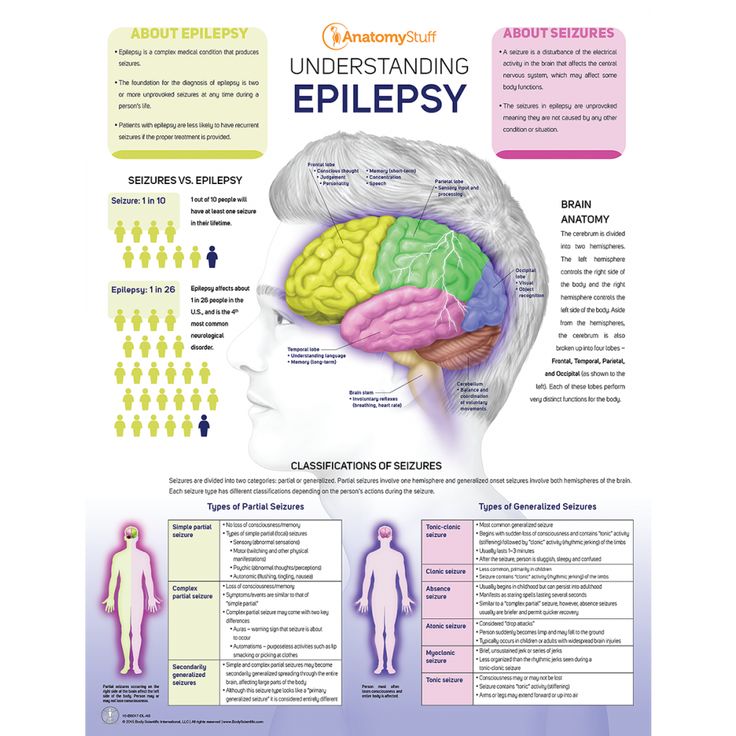
At an early age, special attacks are often observed - spasms, which are short-term shudders with the dilution of the limbs, or vice versa, "squeezing into a ball", repeated several times within a short time.
One of the most common types of seizures is absence, in which the child freezes and does not respond to calls.
An important symptom during an attack is asymmetry of movements, for example, turning the head and eyes to the side, raising and tensing one arm, twitching the corner of the mouth on one side. This may indicate the focal nature of the attack, that is, its connection with a specific limited area of \u200b\u200bthe brain.
It is very important to remember the appearance of the patient during an attack, even better - record the attack on video - a mobile phone camera will be enough. The typical pattern of seizures often makes it possible to assess the prognosis from the very beginning and determine the need and possibility of treatment.
Are seizures always associated with epilepsy?
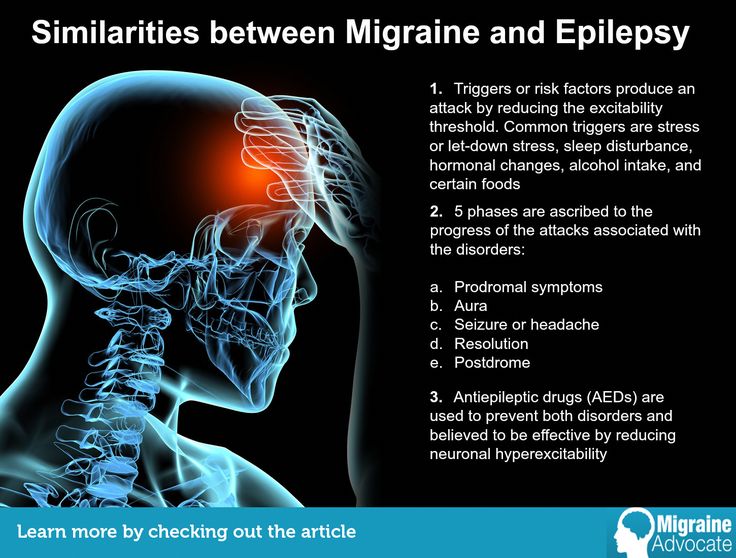
Not at all necessary. Seizures of various kinds - convulsive and non-convulsive - can occur in children with fever (febrile convulsions), poisoning, dehydration, head injuries, cerebrovascular accidents. In addition, outwardly it can be difficult to distinguish fainting, sleep disorders, some forms of migraine, various movement disorders, and psychological disorders from seizures. An important difference between paroxysms in most of these disorders and epileptic seizures is the connection with a provoking factor or an acute damaging effect (trauma, poisoning, overheating). In epilepsy, seizures in most cases are spontaneous or are caused by simple stimuli (light flashes, deep forced breathing).
Risk of relapse
For a healthy child, the risk of recurrence of a spontaneous attack is 24% within 1 year. In the presence of previous neurological disorders (for example, cerebral palsy), the probability of a second attack within a year is 37%, and if the attacks were repeated within a day, it is 70%.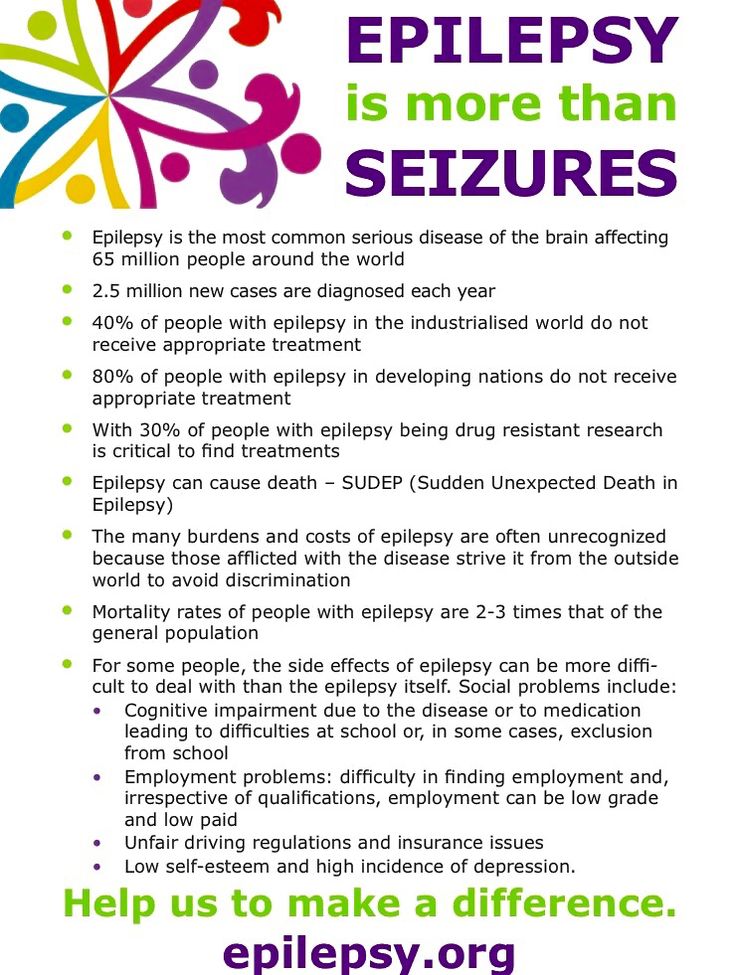 However, if the attack was accompanied by some acute condition (overheating, infection, trauma), then the risk is usually many times less.
However, if the attack was accompanied by some acute condition (overheating, infection, trauma), then the risk is usually many times less.
What should I do if I have a seizure?
In most cases, seizures end on their own within a few seconds or minutes. Regardless of the cause of the attack, first aid is only to prevent injury and ensure free breathing. During an attack, the patient should be away from heavy, unstable, piercing and cutting objects. Do not force the patient. In no case should you try to open your jaws and get your tongue out - it's useless. To ensure the patency of the respiratory tract, it is enough to lay the patient on his side with his face turned down. In this position, the tongue will not fall and will not block the breath. Attempts to open the teeth often result in injuries, fragments of the teeth can get into the respiratory tract and cause respiratory arrest, even death. To avoid biting the tongue after the onset of an attack is usually no longer possible, and attempts to get the tongue only lead to additional injuries.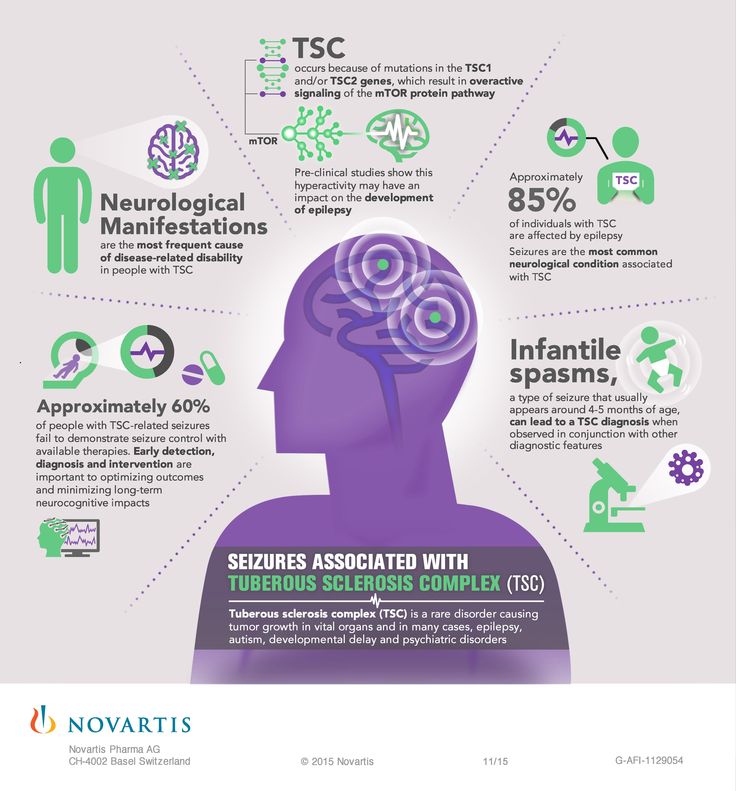 It is useless to give artificial respiration and heart massage to a person in a convulsive attack. Thus, all that is needed is to remove dangerous objects away from the patient, lay him on his side face down and call an ambulance. At the same time, it is advisable to remember the recommendation to film events - this can be done by an assistant.
It is useless to give artificial respiration and heart massage to a person in a convulsive attack. Thus, all that is needed is to remove dangerous objects away from the patient, lay him on his side face down and call an ambulance. At the same time, it is advisable to remember the recommendation to film events - this can be done by an assistant.
After the attack, the patient should be allowed to rest, drowsiness is possible. It is necessary to make sure that the patient has come to his senses, is oriented in the environment, there are no speech disorders and movements in the limbs are preserved (ask to answer simple questions, raise and hold his arms and legs). Until the complete disappearance of impaired consciousness, nothing should be given to eat or drink in order to prevent food, water or drugs from entering the respiratory tract.
For some types of seizures (eg, absences and infantile spasms), emergency care is often not required at the time of the seizure.
Symptoms of epilepsy in children, causes, prevention methods
Epilepsy is a chronic, long-term disease caused by various lesions of the central nervous system and manifested in paroxysmal conditions, and subsequently characteristic personality changes.
The causes of epilepsy have not been definitively established. More than 3/4 of all patients belong to the age group up to 18 years.
Causes
- Hereditary factors.
- Disturbances in the development of the brain, caused by both genetic diseases and infections, the effect of harmful substances on the body of a pregnant mother, a disease of her internal organs.
- Meningitis and encephalitis.
- Brain injury.
Symptoms
Classical epileptic seizure (suddenly occurring, short in time, as a rule, many times recurring, having precise time limits, a painful condition). It develops suddenly and most often for no apparent reason.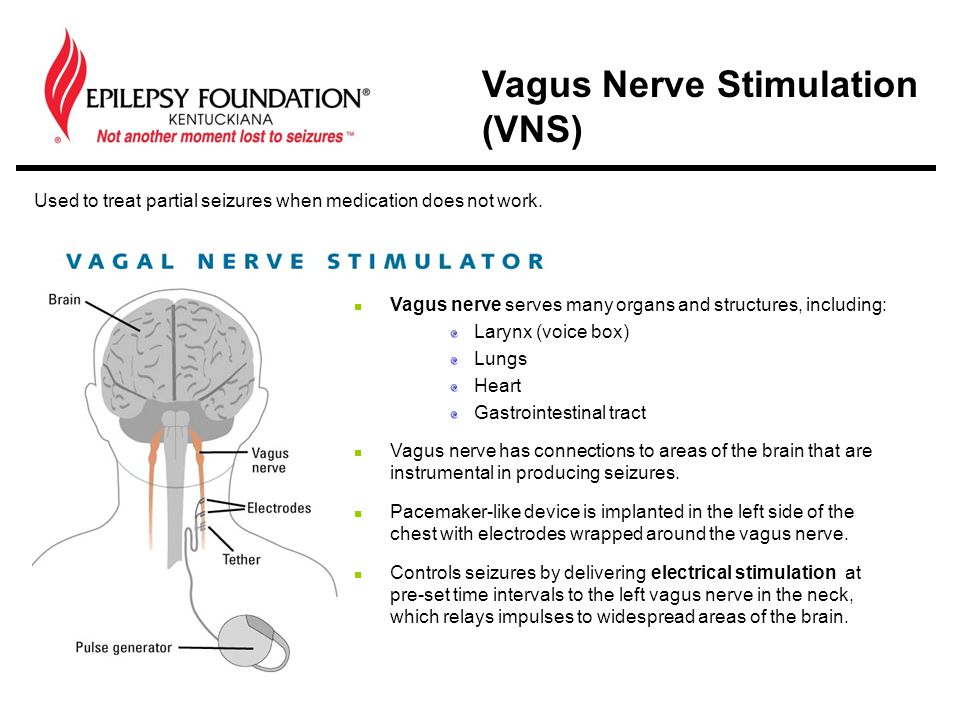
In its course, it is customary to distinguish a number of successive stages:
- 1. Precursors: headache, feeling of discomfort, dissatisfaction with one's own condition, irritability, decreased mood, decreased efficiency.
- 2. Aura. May manifest as hallucinations. In this case, the child can see various pictures, which most often have a frightening, frightening character. In addition to various visual images, auditory deceptions may also occur, and unpleasant odors may be felt.
- 3. Tonic phase of seizure. Suddenly the child loses consciousness, all the muscles are very tense, but there are no convulsions yet. The kid falls sharply to the floor, almost always bites his tongue. During the fall, a very characteristic cry is emitted, which occurs when the chest is compressed by the respiratory muscles due to its tonic tension. The patient stops breathing, the skin first turns pale, and then acquires a bluish tint.
 There is involuntary urination and defecation. Pupillary reaction to light is completely absent. This phase lasts no more than one minute, since with a longer course, death can occur from respiratory arrest.
There is involuntary urination and defecation. Pupillary reaction to light is completely absent. This phase lasts no more than one minute, since with a longer course, death can occur from respiratory arrest. - 4. Clonic phase. Characterized by the development of a classic convulsive seizure. Breathing is fully restored. Foam comes out of the patient's mouth with small amounts of blood mixed in. The phase lasts 2–3 minutes.
- 5. After the convulsions gradually subside, the child goes into a coma , which, in turn, then passes into a deep sleep. After awakening, the patient loses memory for all the events that occurred during the attack. In the future, some violations of orientation in space persist, some speech impairment
In the diagnosis of epilepsy, the most valuable and informative method is electroencephalography (EEG). With its help, it is possible to identify not only the very fact of the presence of pathological changes in the brain, but also accurately determine the size and location of the lesion.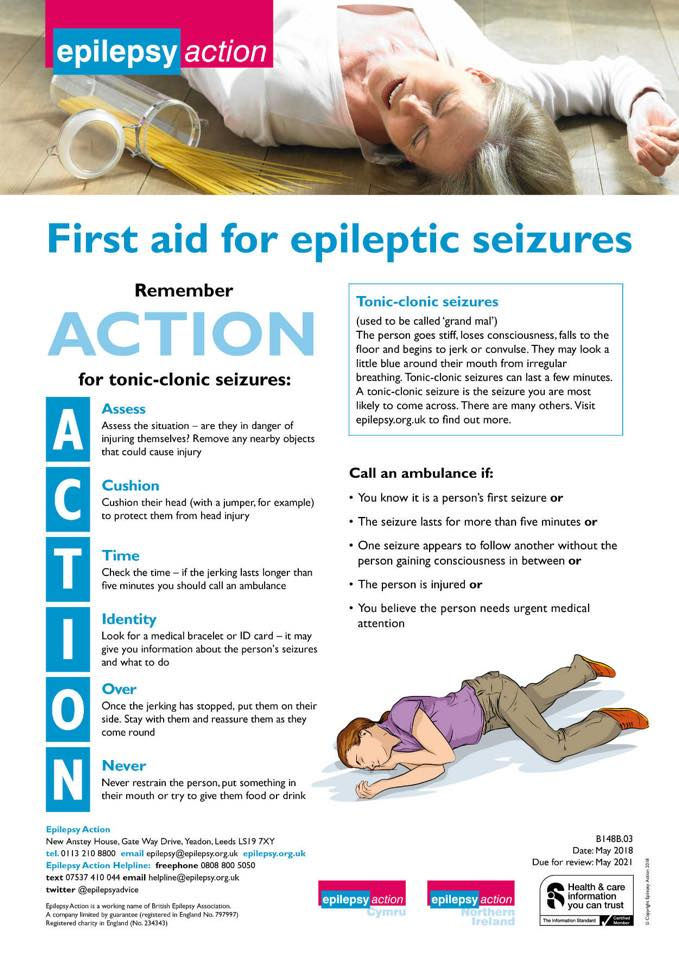 An important positive quality of the EEG is the ability to distinguish true epilepsy from other similar seizures that are not associated with epilepsy.
An important positive quality of the EEG is the ability to distinguish true epilepsy from other similar seizures that are not associated with epilepsy.
Prevention
- Early diagnosis, monitoring of the mother's condition during pregnancy. To observe a child who was born in a family with hereditary factors.
- Avoid drinking strong coffee and tea, overeating, hypothermia and overheating, staying at high altitude, as well as other adverse environmental influences.
- Adhere to a dairy-vegetarian diet.
- Perform light physical exercise, prolonged exposure to the air.
- Observe the regime of physical activity and rest.
More about pediatric neurology at the YugMed clinic
By leaving your personal data, you give your voluntary consent to the processing of your personal data. Personal data refers to any information relating to you as a subject of personal data (name, date of birth, city of residence, address, contact phone number, email address, occupation, etc.