When does milk supply increase
How to increase your milk supply
Is your milk supply really low?
New mothers who are learning to breastfeed often worry that they might not be making enough milk for their baby. Their breasts might stop feeling full and their baby might sometimes be unsettled, or not want to be put down between feeds. There are many reasons for babies to be unsettled and breasts usually get softer after the first few weeks – these are not proof of low milk supply. If your baby is growing as expected (at least 20-30g a day, on average, during the first three months) just on your milk, then your milk supply is fine. If your baby does not grow well on your milk alone, then you may be making less milk than your baby needs.
The most common reason for genuine low milk supply is a slow start with breastfeeding, when not enough milk was removed from your breasts in the early days after birth. It may be possible to turn this around, with prompt action. Some other causes of low milk supply, such as previous breast surgery and some hormonal conditions, may mean that there is a limit to how much milk you can produce. Many nursing parents can make more milk than they are making, and you never know what you can do until you try!
Increasing low milk supply is hard work. It takes time, energy and commitment. It is important to be realistic from the start about your goal and how much time and energy you are able to invest. It works best when you have lots of practical and emotional support, so you can concentrate on your baby and your milk supply. Remember that this won’t be forever – it is a short-term investment for long-term gain. Set yourself short-term goals, e.g. 48-72 hours, then review your progress. If you are not able to increase your milk supply as much as you would like, or decide that it is not realistic to try, you can still have a close, happy feeding relationship with your baby.
While you are working on your milk supply:
- Find skilled feeding support. LLL is here to help! You can find information about ways we can support you here. We can also help you connect with other women who have experienced low milk supply.
- Track how you are doing. Keep a record of how much milk you express and the amount of formula or donated breastmilk your baby takes (if relevant) and how many wet and dirty nappies your baby produces. Tracking changes over time is useful to show how well your plan is working and can help you decide what to do next.
- Monitor your baby’s health and growth. Your baby needs to be weighed regularly while you are working on your milk supply. Your midwifery or health visiting team will usually do this. For more complex feeding issues, you may be referred to a local specialist infant feeding team or clinic. Any baby who is not growing as expected should be under the care of a doctor. This is because occasionally, slow growth can be caused by underlying health issues in the baby, rather than low milk supply.
How milk production works
Milk production starts in the middle trimester of pregnancy. After birth, milk continues to be made in the breasts in response to milk being removed. The most common reason for low milk production is a slow start with breastfeeding – not enough milk being removed from the breasts in the early days after birth.
The most common reason for low milk production is a slow start with breastfeeding – not enough milk being removed from the breasts in the early days after birth.
Milk supply usually reaches its peak around four weeks after birth, with most of the increase happening in the first two weeks. If not enough milk is removed during this time, your breasts may end up making less milk than your baby needs. It may be possible to increase milk production, by removing more milk from your breasts. The earlier you start this, and the more energy you put into it, the higher your chances of making more milk. Even if more time has passed, it may still be possible to increase your milk production to some extent, but unfortunately there is no guarantee of being able to make a full milk supply.
Any amount of milk you are able to produce is valuable to your baby. Breastfeeding is about much more than just milk and you can enjoy nurturing your baby at the breast, however much milk you are making.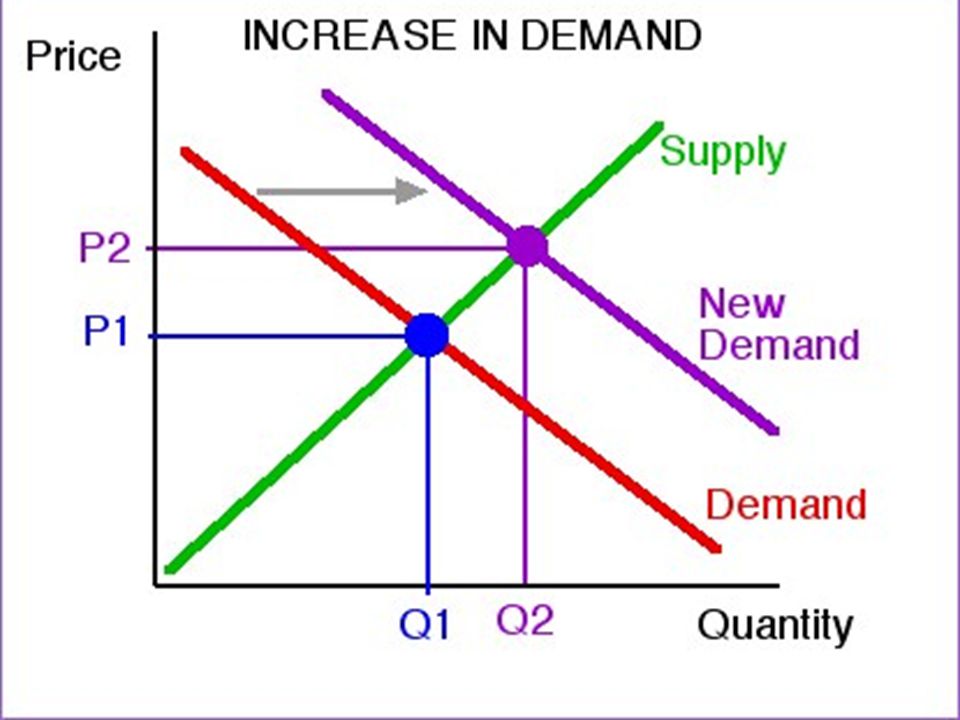
For more detailed information about how milk production works see How Milk Production Works.
Risk factors for low milk supply
These include:
- Previous breast surgery (especially reduction) or radiation
- Retained placenta
- Unusually small/thin/unequally sized/widely spaced breasts
- A history of infertility with hormonal cause
- Hormonal conditions like thyroid problems or polycystic ovary syndrome (PCOS).
If you have any risk factors for low milk supply, you may be referred to an infant feeding specialist. Some of these conditions are treatable. Even if you have underlying factors that can’t be treated, you may still be able to make more milk than you are currently making.
Effective attachment
A baby who isn’t deeply attached at the breast may not be able to get enough milk, and feeding may also be uncomfortable for you. Squashed (“new lipstick”) nipples after a feed, skin damage and pain that lasts throughout feeds are all signs of shallow attachment.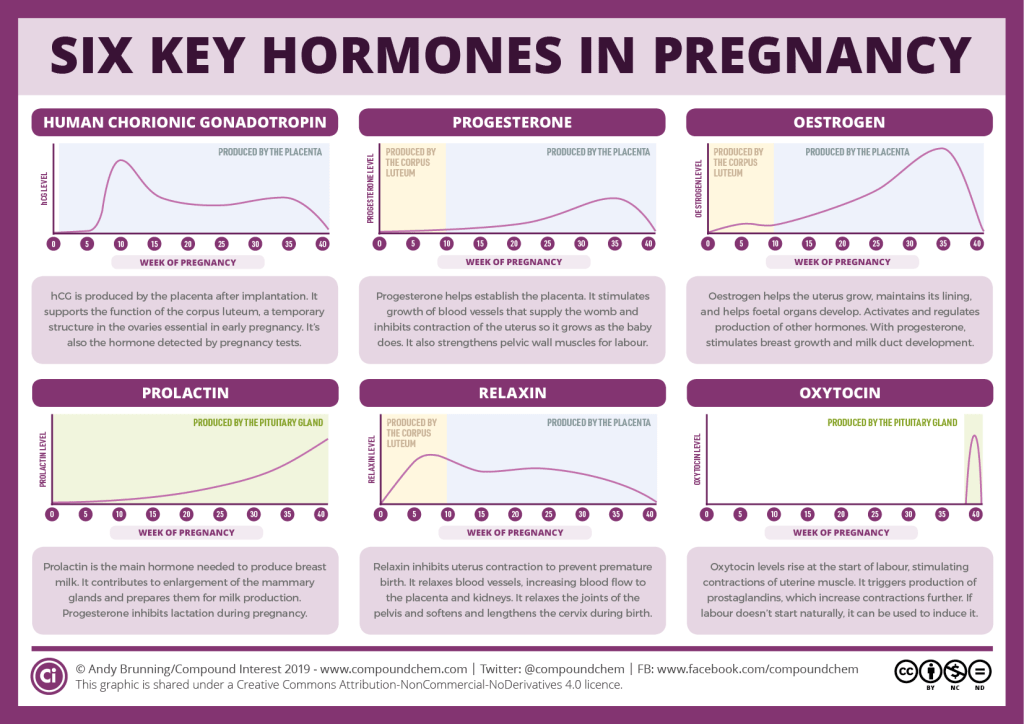 You can read more about positioning and attachment here.
You can read more about positioning and attachment here.
Face to face help (including via video call) is usually best when working on attachment. If feeding doesn’t become more comfortable and/or effective even with skilled help, your baby may be referred for an oral assessment (a thorough examination of their mouth) to check for tongue tie, which is a problem for a small number of babies and can be treated. You can read more about this here and here.
Hold your baby skin to skin
This helps your milk-making hormones to work well, keeps your baby calm and happy, helps you and your baby feel connected and encourages interest in feeding. You can read more about holding your baby skin to skin here.
How often and when to feed
While you are working to increase your milk supply, you will want to encourage your baby to feed as often as possible. Signs of interest in feeding include your baby turning their head and opening their mouth (rooting), licking lips, mouthing hands, restlessness and making small sounds. Try to offer a feed when your baby is first interested, before they become upset. If your breasts are feeling full or you just feel like feeding your baby, you can offer your baby a feed, even if they are not asking.
Try to offer a feed when your baby is first interested, before they become upset. If your breasts are feeling full or you just feel like feeding your baby, you can offer your baby a feed, even if they are not asking.
- You may want to avoid using a dummy, a baby swing, or swaddling your baby, as these can make it difficult to tell if your baby is interested in feeding.
- Don’t give your baby water, tea or any other non-milk drinks.
- Breastfeeds don’t have to be regular (e.g. every 2-3 hours). Your baby just needs to have enough feeds in 24 hours, whenever they are awake enough and interested. Most young babies need at least 8-12 feeds in 24 hours. Don’t watch the clock – watch your baby and count feeds.
Keep your baby feeding actively when they are at the breast
Knowing when your baby is feeding actively at the breast, with deep sucks and swallowing after every one-two sucks, can be very helpful. While you are working to increase your milk supply, you will want to make sure that milk is removed from your breasts as effectively as possible.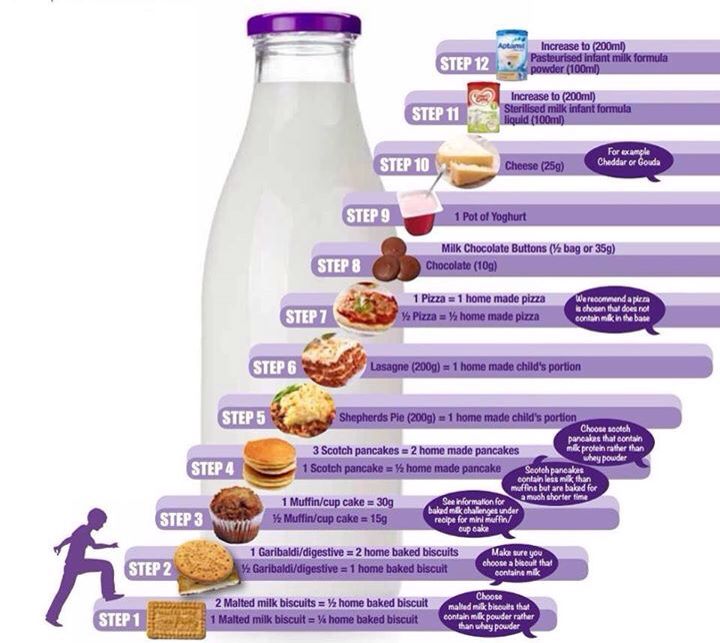 If your baby is mostly doing light, fluttery sucks with very little swallowing (three or more sucks per swallow), they are not removing much milk. If your goal is to increase the amount of milk removed from your breasts, you may want to end the feed and use a breast pump instead to maximise efficient milk removal.
If your baby is mostly doing light, fluttery sucks with very little swallowing (three or more sucks per swallow), they are not removing much milk. If your goal is to increase the amount of milk removed from your breasts, you may want to end the feed and use a breast pump instead to maximise efficient milk removal.
Breast compressions and switching sides can help to keep your baby actively feeding for longer. Start compressing your breast as soon as your baby stops actively feeding. You can read about how to do compressions here. When your baby is no longer actively feeding even with compressions, repeat on the other side. Offer as many breasts as your baby will take – it can be more than two!
Some babies seem to want to feed all the time and protest when you take them off the breast. If they are not growing well, it may be because they are not yet breastfeeding effectively. To increase your milk supply, you may temporarily need to limit their time at the breast, to give you more time to express your milk.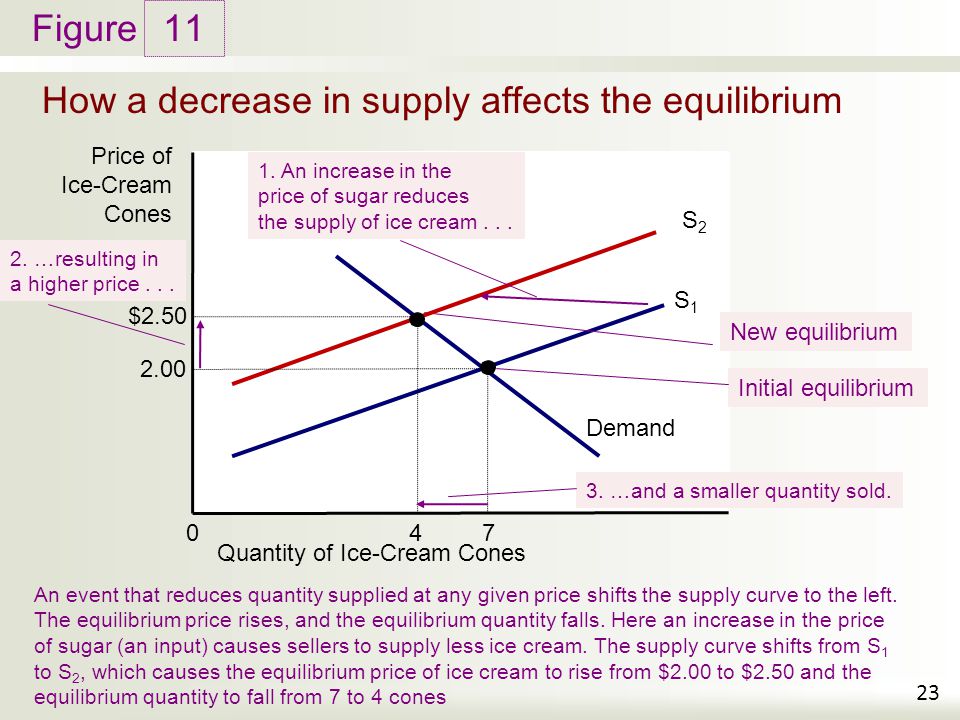
Increasing breast stimulation by expressing your milk
If the steps above do not result in increased milk supply, the next step is to increase stimulation of your breasts by expressing your milk:
- An LLL Leader and/or your local infant feeding specialist will agree with you how many times in 24 hours to aim for at first. For more impact, you can increase the number of sessions. For maximum effect, you would aim to express 8-12 times in 24 hours (this is the number of times most babies need to feed).
- A double electric breast pump, preferably a large “hospital grade” pump, is usually the best tool for this job. Smaller single electric and manual pumps are designed for occasional expressing, not the big task of increasing milk supply.
- You don’t need to pump after set intervals (most babies don’t feed after set intervals either), just as often as you can. The important thing is how many times you express in 24 hours – it’s up to you when you do it. It’s fine to take a break for a few hours to go out or to sleep! More, shorter expressions often work better than fewer, longer ones and it’s fine to stop in the middle of pumping, if you need to do something.
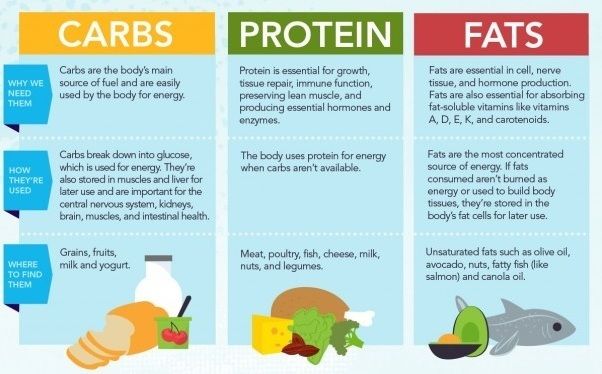 Even if you only have a few minutes, it’s worth pumping. Notice the times of day or night when you can express most and aim to pump more often then. First thing in the morning and in the quiet hours of the night can work well. Experiment to see what works best.
Even if you only have a few minutes, it’s worth pumping. Notice the times of day or night when you can express most and aim to pump more often then. First thing in the morning and in the quiet hours of the night can work well. Experiment to see what works best. - Use your hands as well as your pump. Try massaging your breasts before and during pumping. You might want to buy or make a “hands-free pumping bra” to hold your pump in place. Some women find that they can express lots of milk by hand after they have finished pumping. You can see how to use your hands to express more milk in this video.
- Try covering the collection bottle with a sock so you can’t see it. Frustration about how slowly it is filling with milk can make it even slower!
- Try visualisation, e.g. a flowing fountain, or milk pouring into a bottle.
- Many women find that they get most milk in the first few minutes of pumping. To make the most of this, it can work well to pump very frequently for short periods, stopping and starting as many times as possible.
 This is sometimes called ‘power pumping’.
This is sometimes called ‘power pumping’. - Try pumping with a piece of your baby’s clothing near enough to smell, or while looking at your baby, or holding your baby skin to skin.
You can find more tips on how to express milk here.
Balancing breastfeeding and expressing
The priority at this stage is to increase your baby’s milk intake and your milk supply. This may mean limiting your baby’s time at the breast, for now, to free up enough time to express. Your baby has lots of time to learn to breastfeed. Your milk supply will become more difficult to increase as time goes on, so it is important to act quickly. This might feel all wrong – you want to breastfeed, not pump! Remember that it is an investment of your time now to help your baby breastfeed later. As your milk supply increases, breastfeeding will get easier and more rewarding for your baby. When breastfeeding is going well, you will be able to let your baby feed as much as they want.
How to feed expressed milk to your baby
There are lots of options – an LLL Leader can help you choose some to try, including paced bottle feeding and more,
cup feeding, and at-breast supplementers (lactation aid).
Keeping the breast a happy place for your baby
If your baby is upset, try offering some extra milk before offering the breast. This helps your baby to associate the breast with feeling full and happy, rather than hungry and frustrated.
- Babies enjoy ending a feed by falling asleep at the breast. You can offer expressed or formula milk between breasts, allowing your baby to finish with the second breast.
- You can give milk by bottle or cup with your baby’s cheek against your breast.
- If a supplementer is used, your baby can drink expressed milk while breastfeeding.
Domperidone
This is a prescription medication that can help to increase milk supply in some women, whilst they are taking the tablets.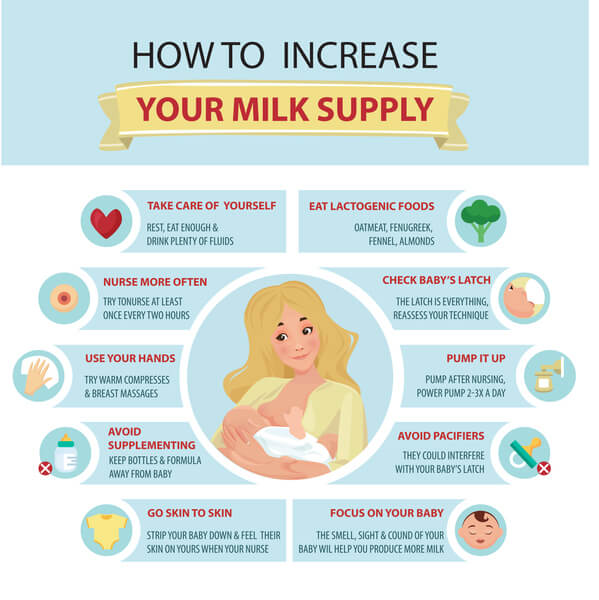 It is not suitable for everyone, e.g. it is not safe for those with certain heart conditions. Because of this, doctors are currently discouraged from prescribing domperidone to anyone. However, the NHS states that domperidone may be appropriate in some cases, so if you would like to try it, it’s worth discussing with your GP, and taking along some information for them to read.
It is not suitable for everyone, e.g. it is not safe for those with certain heart conditions. Because of this, doctors are currently discouraged from prescribing domperidone to anyone. However, the NHS states that domperidone may be appropriate in some cases, so if you would like to try it, it’s worth discussing with your GP, and taking along some information for them to read.
The most important thing to do to increase milk supply is to remove more milk from your breasts, so don’t worry if you can’t or prefer not to take domperidone.
Formula milk
Some babies need extra milk for a short time or longer term if their mother is not making a full milk supply. If donated human milk is not available, the only safe alternative is infant formula milk. You can find LLLGB’s information on milk sharing here.
It is never safe to suddenly stop or reduce supplements of formula or donor breastmilk. This needs to be done gradually, to allow your own milk supply time to increase. and it is very important that your baby is weighed regularly, to make sure that they continue to get enough milk. It would usually be appropriate to weigh your baby every 1-2 weeks while working on reducing supplements. You can read about how to use donor milk or formula to support breastfeeding here.
and it is very important that your baby is weighed regularly, to make sure that they continue to get enough milk. It would usually be appropriate to weigh your baby every 1-2 weeks while working on reducing supplements. You can read about how to use donor milk or formula to support breastfeeding here.
Whether or not you are producing all the milk your baby needs, you can still have a great feeding relationship with your baby. The breast can still work beautifully to calm, comfort and soothe your baby, even if your milk supply remains low. Any amount of your milk that your baby gets will be beneficial to them. Some of the immune components of milk become concentrated so that babies get the same amount, no matter how much of your milk they get each day. Whatever feeding looks like for you and your baby, we are here to support you.
Summary
Stage 1 – make sure your baby is feeding as effectively as possible
- Consider risk factors for low milk supply.

- Make sure that your baby is well positioned and attached at the breast. This will include checking for any reason the baby might not be able to attach and feed well (e.g. tongue tie).
- Hold your baby skin to skin as much as possible.
- Offer the breast as soon as your baby shows any signs of interest in feeding, at least 8-12 times in 24 hours, waking baby if necessary.
- Switch sides and use breast compressions to increase milk flow.
Stage 2 – if milk supply has not increased enough
- Express your milk at a frequency agreed with an LLL Leader and/or infant feeding specialist.If your baby is still not growing well, increase the number of expressions. For maximum effect, aim for at least 8 times in 24 hours. This may mean temporarily limiting your baby’s time at the breast, to give you enough time to express.
- Feed as much expressed milk as your baby wants to drink by cup, paced bottle-feeding, finger feeding or nursing supplementer.
- Aim to keep your baby’s time at the breast happy and relaxed, and to end feeds with your baby at the breast (if necessary, after giving your baby extra milk at the start or in the middle of the feed) as often as you can.
- Consider using the medication domperidone, which may help increase your milk supply.
- If necessary, use enough formula milk to make sure your baby grows as expected and seems satisfied.
Further reading
Getting breastfeeding back on track after a difficult start
How milk production works
My baby needs more milk
Expressing your milk
Relactation and induced lactation – bringing back milk supply after a break or bringing in a milk supply when you haven’t been pregnant.
Books
Making More Milk, by Diana West & Lisa Marasco (2019)
Defining Your Own Success: Breastfeeding After Breast Reduction Surgery by Diana West (2001)
Breastfeeding Without Birthing by Alyssa Schnell – for non-gestational parents who are inducing lactation.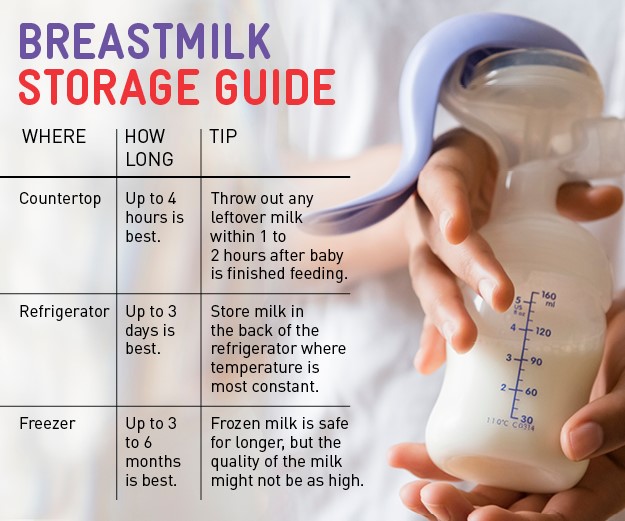
Written by Jayne Joyce and Emily Tammam, LLL Oxfordshire, February 2021
Low milk supply? How to increase breast milk supply
Many mums worry they have a poor milk supply, but it can be hard to know for sure. Read on to find out whether you really have low milk supply and what you can do about it
Share this content
“Have I got enough breast milk?” is something new mothers often worry about – but chances are, if your baby’s healthy and growing well you’re doing great. However, if you’re concerned about your breast milk supply, it’s important to seek advice early. If it turns out things are fine, you’ll quickly be reassured. Plus, you’ll avoid the trap of giving your baby formula unnecessarily, which may cause your own milk supply to drop.
Reasons for low milk supply
A small number of new mums have difficulty producing enough breast milk due to medical reasons, which include:
- Excessive blood loss (more than 500 ml/17.
 6 fl oz) during the birth or retained fragments of the placenta can delay your milk coming in (which usually happens around three days after the birth).1
6 fl oz) during the birth or retained fragments of the placenta can delay your milk coming in (which usually happens around three days after the birth).1 - A history of polycystic ovarian syndrome, diabetes, thyroid or other hormonal disorders. Mums with these conditions sometimes experience a low milk supply.2
- The rare medical condition mammary hypoplasia, in which there isn’t enough milk-producing glandular tissue within the breast.3
- Previous breast surgeries or breast trauma – although many mums who have had surgery go on to breastfeed successfully.4
If any of these conditions applies to you, see a lactation consultant or breastfeeding specialist.
How breast milk supply works
Once your breast milk has come in, your breasts start to make milk through a process of ‘supply and demand’. Each time milk is removed, either by your baby feeding or by expressing, your breasts make more.
That’s why giving bottles of formula can reduce your milk supply – your body isn’t getting the message to produce more breast milk, because none is being removed.
The way your baby nurses also affects your supply. The more frequently and effectively she breastfeeds, the more milk you’ll make. If your baby doesn’t take enough milk during a feed, it’s essential to express regularly to protect your milk supply – see below for more advice.
Signs your baby isn’t getting enough milk
Even though low milk supply is rare, your baby may still struggle to get enough for other reasons during her first few weeks. She may not be breastfeeding frequently enough, or for long enough, particularly if you’re trying to stick to a breastfeeding schedule rather than feeding on demand. She may not be latching well, or might have a condition that makes it harder to take in milk.
The following are signs your baby isn’t getting enough milk:
- Poor weight gain. It’s normal for newborns to lose 5% to 7% of their birth weight in the first few days – some lose up to 10%. However, after that they should gain at least 20 to 30 g (0.
 7 to 1 oz) per day and be back to their birth weight by day 10 to 14.5,6,7 If your baby has lost 10% or more of her birth weight, or she hasn’t started gaining weight by days five to six, you should seek medical advice immediately.
7 to 1 oz) per day and be back to their birth weight by day 10 to 14.5,6,7 If your baby has lost 10% or more of her birth weight, or she hasn’t started gaining weight by days five to six, you should seek medical advice immediately. - Insufficient wet or dirty nappies. The number of poos and wees your baby has per day is a good indicator of whether or not she is getting enough milk – see our article explaining the pattern your baby should be following in Breastfeeding your newborn: What to expect in the first week. Seek medical advice if you’re concerned or if you have noticed her dirty nappies decreasing in wetness and heaviness.
- Dehydration. If your baby has dark-coloured urine, a dry mouth or jaundice (yellowing of the skin or eyes), or if she is lethargic and reluctant to feed, she could be dehydrated.6 Fever, diarrhoea and vomiting, or overheating, can cause dehydration in infants. If you notice any of these symptoms, seek medical advice quickly.
Find out the top 5 tips to know if your baby is getting enough milk
Misconceptions about low milk supply
Newborns typically feed very often – around 10 to 12 times a day, or every two hours – and this is not a sign that you don’t have enough milk. Don’t forget that your baby also nurses for comfort, and it’s difficult to tell how much milk your baby takes during each feed – amounts can vary.
The following are all perfectly normal and are not signs of a poor milk supply:
- your baby wants to feed frequently
- your baby doesn’t want to be put down
- your baby is waking in the night
- short feeds
- long feeds
- your baby will take a bottle after a feed
- your breasts feel softer than they did in the early weeks
- your breasts don’t leak milk, or they used to leak and have stopped
- you can’t pump much milk
- you have small breasts
What to do if you have low milk supply
If you suspect your baby is not getting enough milk, see a lactation consultant or breastfeeding specialist. They will assess whether you have low milk supply and observe a breastfeed to see if your baby is latched on well and taking in enough milk. They may suggest adjusting your feeding position or your baby’s latch so she can feed more efficiently.
They will assess whether you have low milk supply and observe a breastfeed to see if your baby is latched on well and taking in enough milk. They may suggest adjusting your feeding position or your baby’s latch so she can feed more efficiently.
You could also try having more skin-to-skin contact with your baby before and during feeds to stimulate the hormone oxytocin, which gets your milk flowing. Or use relaxation techniques, such as listening to your favourite calming music, to reduce any anxiety that could be affecting your supply.8
With support, most mums with low milk supply are able to partially breastfeed their babies, and some will manage to develop a full milk supply.
If your baby is not yet taking enough milk directly from the breast, perhaps because she was premature or has special needs, you may need to express to protect your milk supply, and your healthcare professional may prescribe galactogogues (medication to increase milk production).
If you’re not yet able to express enough breast milk for your baby, you’ll need to supplement her with donor milk or formula, under the guidance of a medical professional.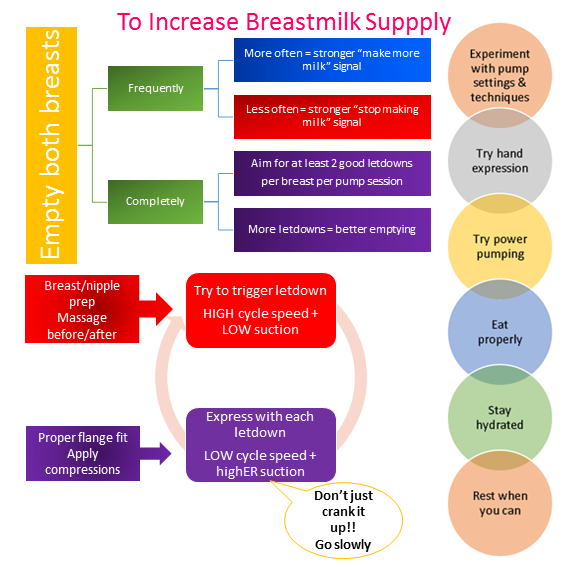 A supplemental nursing system (SNS) can be a satisfying way for her to get all the milk she needs at the breast.
A supplemental nursing system (SNS) can be a satisfying way for her to get all the milk she needs at the breast.
How to increase milk supply with a breast pump
If you need to encourage your milk supply in the first five days after birth, you can use a double electric breast pump with initiation technology, such as the Medela Symphony. This type of pump is designed to mimic the way a baby stimulates the breasts while feeding, and has been found to increase longer-term milk production.9
Once your milk has come in, double pumping means you can express more milk in less time.10 This method also drains the breasts better, which also helps with milk supply.
Although every mum is different, it’s often a good idea to express milk straight after, or an hour after, a feed. This may seem counterintuitive, because it’s usually easier to pump from a full breast. But you should think of your pumping session as ‘putting in a milk order’ for the next day.
At first you may only collect small amounts, but don’t be discouraged – with regular pumping, this will increase. Aim to be removing milk (by breastfeeding as well as pumping) eight to 12 times a day, including one session at night when your levels of the milk-producing hormone prolactin are highest. The more frequently milk is removed, the better. After two or three days of regular pumping you should see a significant increase in supply. For advice on getting more milk from each pumping session, read breast pumping tips.
Hands-on pumping to increase expressed milk
If your baby is not breastfeeding directly at all, or you can’t yet pump enough milk for her, a technique called ‘hands-on pumping’ can be useful. It has been shown to increase the amount of milk mums can express in a session.11,12 The whole process takes around 25 to 30 minutes. Remember, the emptier your breasts, the more quickly they’ll make milk.
Follow these simple steps:
- Massage your breasts.

- Double pump using an expressing bra to keep your hands free.
- While pumping, use your fingers and thumb to compress your breast for a few seconds. Release and repeat. Use compressions on both breasts until your milk flow slows to a trickle.
- Massage your breasts again.
- Finish by hand expressing or single pumping, using breast compressions and switching between breasts to drain them as fully as possible.
Once your baby is gaining weight and you’ve increased your supply, then you can move on to feeding her exclusively at the breast.
References
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Vanky E et al. Breastfeeding in polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2008;87(5):531-535.
3 Neifert MR et al. Lactation failure due to insufficient glandular development of the breast. Pediatrics. 1985;76(5):823-828.
4 Neifert M et al. The influence of breast surgery, breast appearance, and pregnancy-induced breast changes on lactation sufficiency as measured by infant weight gain. Birth. 1990;17(1):31-38.
5 C Tawia S, McGuire L. Early weight loss and weight gain in healthy, full-term, exclusively-breastfed infants. Breastfeed Rev. 2014;22(1):31-42.
6 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p.
7 World Health Organisation. [Internet]. Child growth standards; 2018 [cited 2018 Feb]
8 Keith DR et al. The effect of music-based listening interventions on the volume, fat content, and caloric content of breast milk-produced by mothers of premature and critically ill infants. Adv Neonatal Care. 2012;12(2):112-119
9 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants.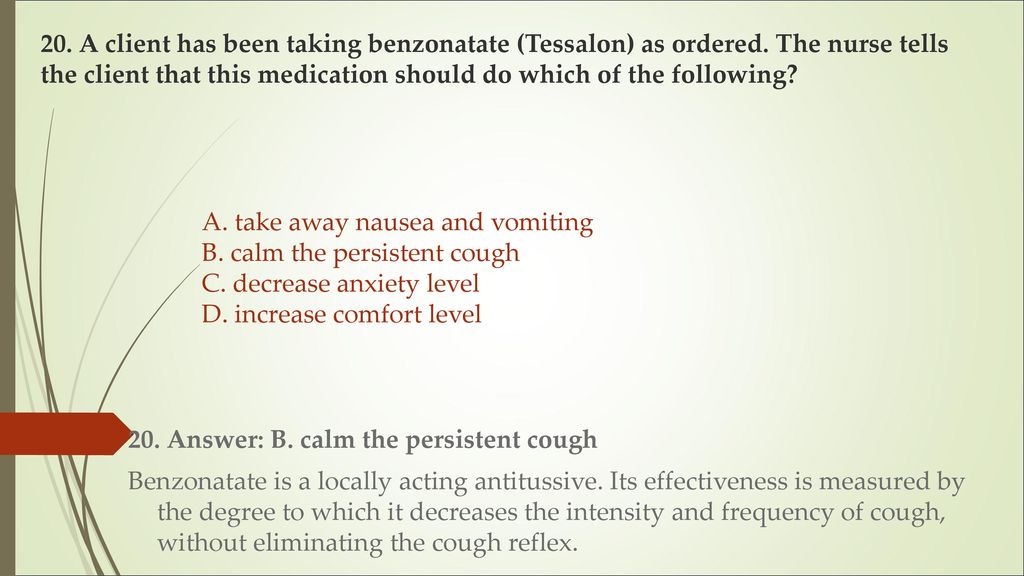 J Perinatol. 2012;32(2):103-10.
J Perinatol. 2012;32(2):103-10.
10 Prime DK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med. 2012;7(6):442-447.
11 Stanford University School of Medicine [Internet]. Stanford, CA, USA: Maximizing Milk Production with Hands-On Pumping; 2017. [Accessed 30.04.2018].
12 Morton J et al. Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. J Perinatol. 2009;29(11):757-764.
Breast milk production | Baby's needs
Did you know that the amount of breast milk adapts to your baby's needs? In this article, you will learn amazing facts about breast milk production in the first days, weeks and months.
Share this information
Your body is capable of producing breast milk for your baby at every stage of development. Understanding how milk production “turns on”, what happens to milk when you feed your baby, and why production adjusts to his needs as he grows, will help you start this amazing process in the right way.
Day one: milk production at birth
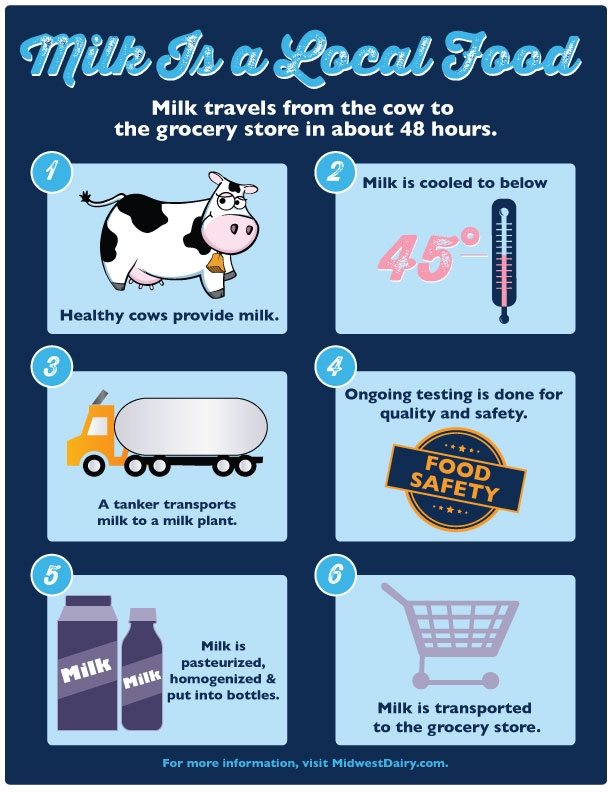
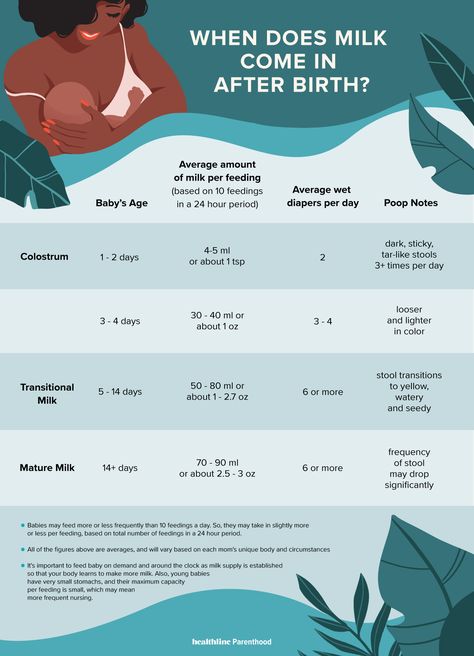
The baby is usually ready to breastfeed from birth. When he grabs the breast and begins to suck rhythmically, the milk-producing cells “turn on” and the formation of the first breast milk, colostrum, starts. 1 Try to feed your baby as much as possible in the first hour of his life, and then as soon as he shows interest in feeding. This will help lay the foundation for good milk production later on. 2
The first days: the arrival of milk
At this stage, your body's level of progesterone, the
pregnancy hormone, which begins to fall after the placenta comes out, is reduced, and the hormones responsible for milk production - prolactin, insulin and hydrocortisone - are included in the work. These hormones will help start milk production. 3 Around the third day of your baby's life, milk will begin to come in and you will feel that your breasts have filled up and become noticeably firmer. 1
1
First month: shaping milk production
During the first weeks, your body will be especially sensitive to the amount of milk produced as it learns to produce the right amount. Prolactin levels increase dramatically each time you empty your breasts, thereby helping shape the lactation process. It also contributes to the maturation of your milk in terms of composition. At this stage, transitional milk is produced and the amount continues to grow. 3.4
For good long-term milk production, it is very important that you are close to your baby during the first few weeks. The more often you breastfeed, the more milk will be produced. This process resembles the law of supply and demand. Each time after emptying the breast, whether it is feeding the baby or pumping, even more milk will be produced.
Remember that it is normal for newborns to eat frequently, perhaps even every 45 minutes, and this does not mean that they are not getting enough milk.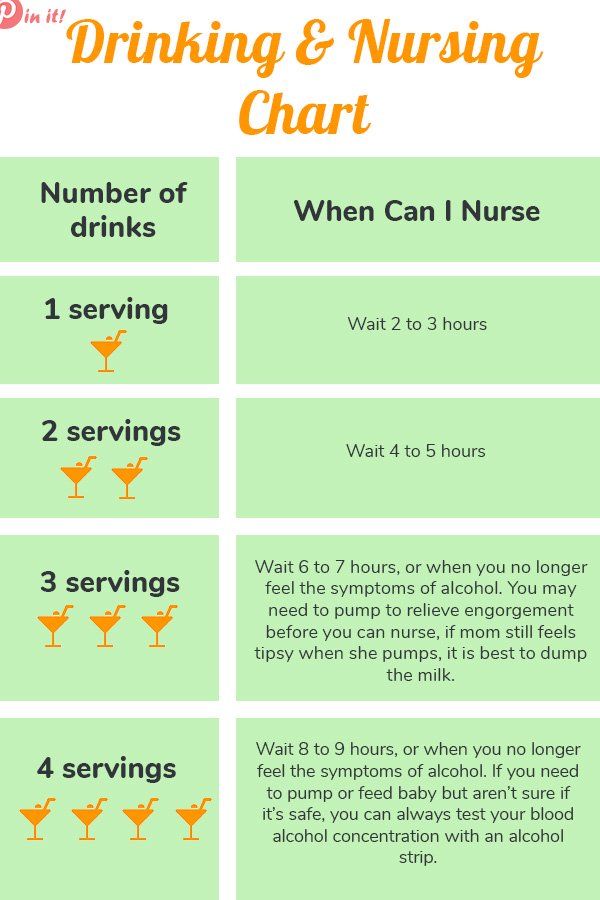 Frequent feedings help shape milk production, so feed your baby on demand, not on a schedule.
Frequent feedings help shape milk production, so feed your baby on demand, not on a schedule.
“In the first few weeks you may feel like you don’t have enough milk because your baby will be feeding all the time, but that’s okay,” says UK mom-of-two Jo, “We tend to think that the baby wants to eat every few hours, but that is not necessarily the case."
Don't forget that babies also breastfeed for comfort. Breastfeeding helps them calm down and adjust to their new life outside the womb. In addition, feeding helps to establish a connection between you.
Stable milk production in the first month
If you follow your baby's needs and feed him as often and for as long as he wants, milk production should adjust. 5
Some mothers try to increase the period between feedings so that the breasts can produce more milk during this time, but this should not be done, as this may have the opposite effect. 2
If you are unable to breastfeed directly for the first two weeks, express your milk to build and maintain your milk supply during this critical period and beyond.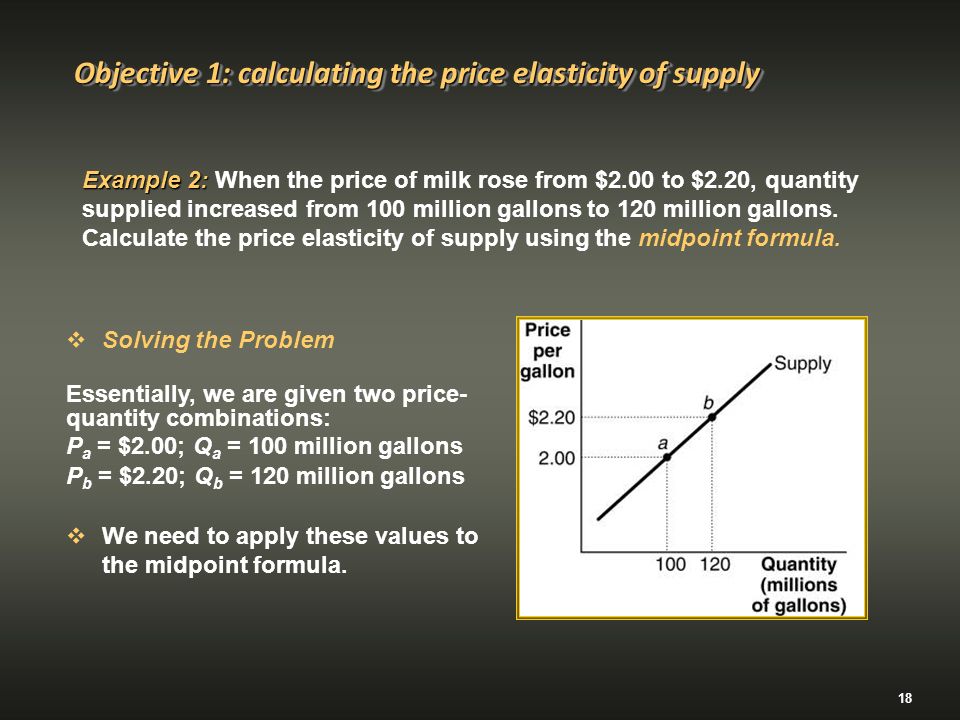
Did you know that feeding your baby extra formula unnecessarily can reduce your milk production? The chest will not receive a signal to increase production, because it will not be emptied. In addition, if the baby sleeps longer after formula, he may miss his usual next feeding time.
This is a kind of “supplementing trap”. After three to four days of formula supplementation, during which the breasts have emptied less, the body will receive a signal that breastfeeding has stopped, and the amount of milk produced will begin to decrease. As a result, the baby will remain hungry and will need additional formula supplementation. And so on in a circle ... As a result, this will lead to really low milk production, and the baby will eat mainly the mixture.
Breast milk production after six weeks
After a month of breastfeeding, post-feeding bursts of prolactin secretion begin to decrease, milk matures, and the body gets used to producing as much milk as your baby needs. In fact, the chest begins to work "on autopilot." 4 You may also notice at this time that your breasts are softer and your milk flow has stopped.
In fact, the chest begins to work "on autopilot." 4 You may also notice at this time that your breasts are softer and your milk flow has stopped.
At this stage, women often have fears of "losing milk".
However, this only means that milk production has been established and now fully meets the needs of the child. It is noteworthy that although the baby continues to grow, he will consume approximately the same amount of milk both at six weeks and at six months. You may notice that the baby began to suckle the breast longer, but less often. On some days he may eat a little less than usual - his appetite changes in the same way as an adult.
Now your body will produce exactly the amount of milk,
as much as your baby needs. Therefore, the more milk the baby
drinks (or you express), the more it will produce.
How does this happen? The reason for this is thought to be the so-called "feedback lactation inhibitor" that controls milk production.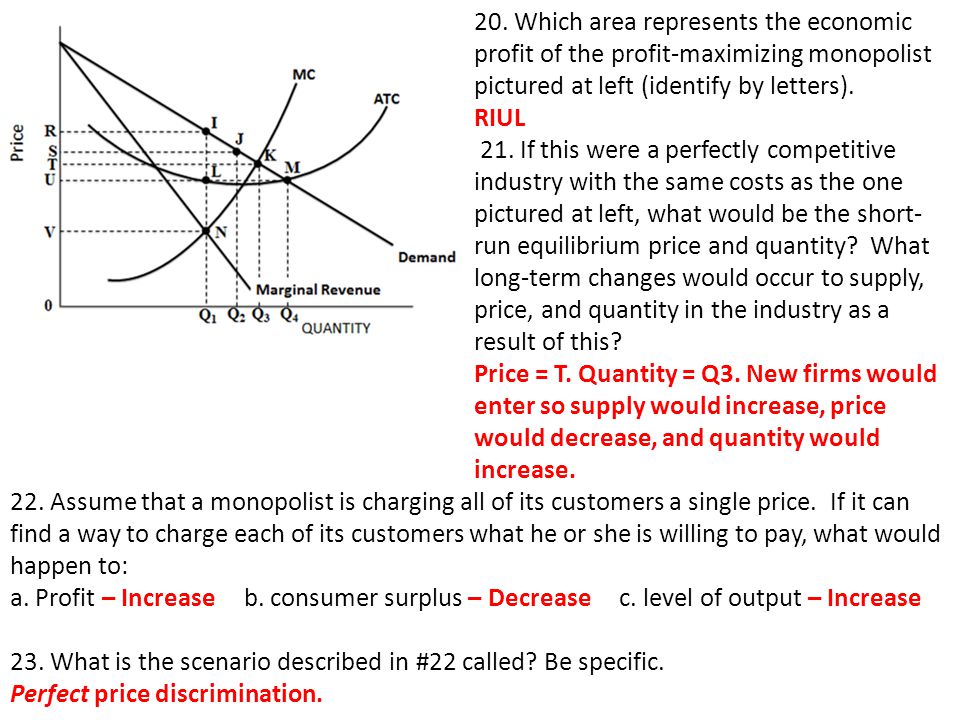 The more milk in the breast, 2 the higher the inhibitor level, so a full breast produces less milk than one that has been emptied.
The more milk in the breast, 2 the higher the inhibitor level, so a full breast produces less milk than one that has been emptied.
What is the rate of milk production?
Mothers often worry about their milk supply and think about how to increase it. However, if the baby is healthy and growing well, problems usually do not arise.
“I was worried that my newborn daughter was not getting enough milk as she was feeding very quickly and always from one breast even though I offered both,” says Marjorie, mother of two in the UK, “But when I pumped from using a breast pump, I was surprised at how much milk I produced, and calmed down. I just had to keep feeding her little and often.”
Keep in mind, however, that not all mothers are able to express a lot of milk right away. You can also try hand expressing milk and see if there is a change in breast fullness.
If you're worried about your milk supply, read our tips for symptoms of too little or too much milk.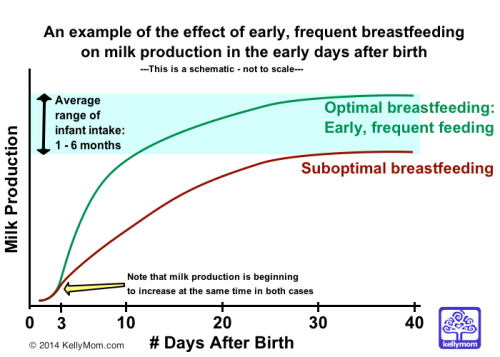
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet Gynecol Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". F Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
3 Ostrom KM. A review of the hormone prolactin during lactation. Prog Food Nutr Sci . 1990;14(1):1-43. - Ostrom KM, "Review of the role of the hormone prolactin during lactation." Prog Food Nutr Sai. 1990;14(1):1-43.
1990;14(1):1-43. - Ostrom KM, "Review of the role of the hormone prolactin during lactation." Prog Food Nutr Sai. 1990;14(1):1-43.
4 Cox DB et al. Blood and milk prolactin and the rate of milk synthesis in women. Exp Physiol. 1996;81(6):1007-1020. - Cox D.B. et al., Effects of blood and milk prolactin on milk production in women. Exp Physiol. 1996;81(6):1007-1020.
5 Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-95. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3): e 387-95.
How to increase the amount of milk for a nursing mother? – an article in the blog of the Health Center for Children in Moscow
Breastfeeding is a guarantee of good health and mental peace of the child for years to come. But besides this, breastfeeding solves most of the mother's issues: from financial issues to the convenience of building your day and bonding with your baby. Galina Vladimirovna Loseva, our most sought-after pediatrician with more than 20 years of experience, tells how to increase the amount of milk for good nutrition of a child
But besides this, breastfeeding solves most of the mother's issues: from financial issues to the convenience of building your day and bonding with your baby. Galina Vladimirovna Loseva, our most sought-after pediatrician with more than 20 years of experience, tells how to increase the amount of milk for good nutrition of a child
The problem of lack of milk can occur both in the early neonatal period, when lactation is becoming established, and later, for example, during lactation crises, which can occur at certain periods of time (3-6 weeks, 3-4 months, 6 months), as well as after temporary weaning during the mother’s illness or the need to take certain medications that are incompatible with breastfeeding.
Ways to increase lactation:
- Feeding on demand , especially during lactation. Frequent feedings in the first weeks of life are essential for maximizing the number of prolactin receptors to ensure sufficient milk production in the long term.
 Without these receptors, lactation will be at risk by 2-3 months of age. It is advisable to attach the baby to the breast as soon as possible after childbirth. If possible, do not use bottle supplements without a good reason. Night feedings are obligatory, the need for them usually lasts up to about 6 months.
Without these receptors, lactation will be at risk by 2-3 months of age. It is advisable to attach the baby to the breast as soon as possible after childbirth. If possible, do not use bottle supplements without a good reason. Night feedings are obligatory, the need for them usually lasts up to about 6 months. - Proper breastfeeding. The baby must have both the nipple and areola. His mouth should be wide open with his lower lip turned outward
- You can use post-feeding pump to increase milk production. And at the same time, freeze milk to create a reserve in case the mother leaves or a case of illness in which it is necessary to interrupt breastfeeding.
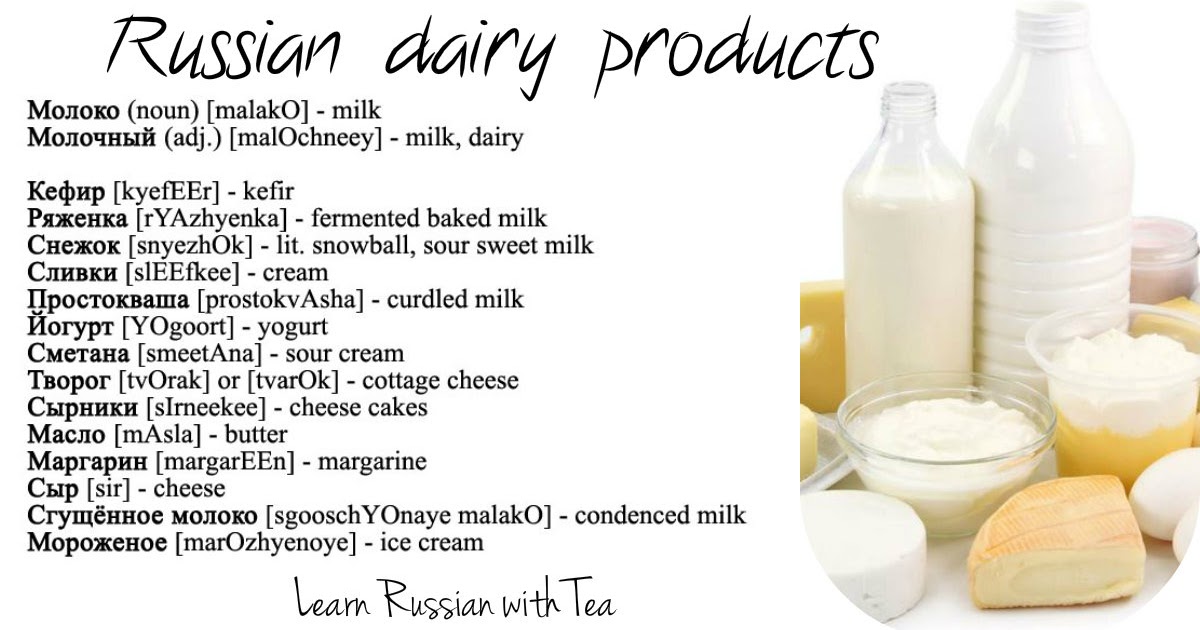
- Rational nutrition of a nursing woman. The menu should contain cereals, vegetables, fish, meat, eggs, fruits, dairy products are better than sour-milk, a small amount of nuts is acceptable. The use of strict hypoallergenic diets in a woman without an allergic history is unacceptable. Spicy dishes, spices, fried foods are excluded, this can affect the taste and smell of milk.

- Drinking enough liquid - water, green tea, compotes, fruit drinks. Drinks should preferably be warm or hot. It is recommended to take liquid 20-40 minutes before feeding.
- Avoid alcohol, nicotine, including passive smoking.
- Compliance with the rest regimen , psycho-emotional peace, positive attitude. This is largely determined by the attitude of close people who can help a nursing mother in household chores, caring for other children, etc.
- Warm shower, light breast massage just before feeding.
- If you still need supplementary feeding, then it is better to give it with a pipette, spoon, syringe without a needle.
- Pharmacy products: Laktogon, Femilak. From herbs, galega, cumin, anise are considered safe. However, relying only on these funds is not worth it if the above points are not observed. They can be used as ancillary, as an addition to the diet of a nursing mother, which may be insufficient for certain reasons.