Full term triplet pregnancy
Multiple birth - triplets or more
Multiple birth - triplets or more | Pregnancy Birth and Baby beginning of content5-minute read
Listen
If you are pregnant with triplets or more, the birth will need careful planning.
The main risk with carrying multiples is that they will be born prematurely. Your medical team will help you plan your babies' birth. This may include deciding where and when your babies will be born.
Planning for your multiple birth
When you are pregnant with triplets or more, it is important to plan the birth. Your medical team will consider the risks of premature birth. They will weigh this against the risks of continuing the pregnancy for both you and your babies, based on your individual situation.
Generally, the longer your babies can stay in your uterus, the better. But when you are pregnant with triplets or more, complications can often develop. This can often mean that it's better for you and your babies if they are born early.
A normal pregnancy lasts 40 weeks. The average length of a pregnancy for triplets is 32 weeks. For quadruplets, the average length is 30 weeks.
Continuing a multiple pregnancy past 36 weeks can be risky for you and your babies. So, it's usually considered best to deliver them early.
When deciding when and how the babies should be born, your doctor will consider different factors. Your medical team will think about:
- the position of each baby
- the weight of each baby
- your health
- the babies’ health
A caesarean section is usually considered safest when there are 3 or more babies.
Giving birth to triplets or more vaginally is very rare. It is not recommended because of the higher risk of labour complications and infant mortality.
Since almost all triplets or more will be born prematurely, they will need special care. This may include a stay in a neonatal intensive care unit (NICU).
This may include a stay in a neonatal intensive care unit (NICU).
It’s important to plan to have the birth in a hospital with all the facilities that you and your babies will need.
Caesarean section
A caesarean section is usually the safest option when you are carrying 3 or more babies. This may be because of:
- the position of the babies
- the position of the placenta (or placentas)
- the risk of one of the placentas or umbilical cords being compressed during a vaginal birth
- the risk of the babies becoming entangled during a vaginal birth
If you are carrying triplets or more, you will usually be offered a planned caesarean.
If your babies are going to be born early (preterm), your doctor may recommend giving you steroid injections. The injections are given to you before the birth.
Steroids can help develop your babies’ lungs. This can help them breathe more easily after birth. Steroids can also reduce the risk of other problems in babies born preterm.
Multiple babies and preterm labour
If you are expecting multiple babies and you go into labour, contact your doctor or midwife and go to your local hospital emergency department. The signs and symptoms of labour are the same as with normal labour. These include:
- contractions
- sudden breaking of the waters
- a ‘show’
During pregnancy, a plug of mucus seals the cervix. A 'show' is when the plug comes away and out of the vagina.
Women who are pregnant with multiple babies may go into labour naturally before 35 weeks. This happens in around 3 out of 4 cases.
Contact your medical team immediately if you have any signs of preterm labour. It may be possible to slow down or stop the labour. You will most likely be admitted to hospital.
If you go into labour spontaneously, you will likely be given a caesarean after you arrive at hospital.
Babies born before 34 weeks may need help with breathing, feeding and keeping warm. They are at greater risk of complications than babies born at full term.
They are at greater risk of complications than babies born at full term.
The neonatal intensive care unit (NICU) is specialised to care for premature and sick newborn babies. This unit has experienced medical staff and equipment.
When your babies no longer need this high level of care, they may be transferred. They may then spend time in the special care nursery or special care baby unit.
Resources and support
If you are preparing for a multiple birth, there are different organisations you can turn to for information.
The Australian Multiple Birth Association can provide support and resources for families expecting multiple babies.
The Royal Women's Hospital Melbourne offers online education for those expecting a multiple birth.
The Australian Breastfeeding Association can provide information on breastfeeding multiple babies, and link you to services such as lactation consultants.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Available 7am to midnight (AET), 7 days a week.
Sources:
Twin Research Australia (Multiple Perspectives: What support do multiple birth families need to live happy and healthy lives?), Australian Multiple Birth Association (What to expect when you're expecting multiples), Queensland Health (Steroids in pregnancy), Government of Western Australia (Multiple Pregnancy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2022
Back To Top
Related pages
- Twins, triplets and multiples
Need more information?
Multiple pregnancy (triplets or more)
Learning you're pregnant with triplets or more can be a shock, but overall, most parents find having multiple babies to be a positive experience.
Read more on Pregnancy, Birth & Baby website
Types of multiple pregnancy
Multiple pregnancies, including twins, triplets and more, are rare but require lots of support. Find out about different types of multiple pregnancy here.
Read more on Pregnancy, Birth & Baby website
Raising multiple babies
Raising multiple babies - triplets or more - involves planning, hard work, and well designed routines. But with support, raising multiples does get easier.
Read more on Pregnancy, Birth & Baby website
Twins, triplets and multiples
If you are having twins, triplets or more, find out everything you need to know about your pregnancy, the birth, feeding and raising your babies.
Read more on Pregnancy, Birth & Baby website
Feeding multiple babies
Feeding multiple babies, such as triplets or more, can be challenging at first, but even breastfeeding is possible with some expert help.
Read more on Pregnancy, Birth & Baby website
Fraternal twins & identical twins | Raising Children Network
Whether you’re having fraternal twins or identical twins, it’s good to find out during pregnancy. Get the facts you need about different types of twins.
Read more on raisingchildren.net.au website
Twins and multiple births - Better Health Channel
betterhealth.vic.gov.au
Read more on Better Health Channel website
Breastfeeding triplets, quads or more! | Australian Breastfeeding Association
Some mothers find breastfeeding one baby demanding. Breastfeeding three or four or more could be viewed as a definite challenge. But many mothers succeed. Knowing how breastfeeding works will help you understand how it is possible to breastfeed twins, triplets, quads or more.
Breastfeeding three or four or more could be viewed as a definite challenge. But many mothers succeed. Knowing how breastfeeding works will help you understand how it is possible to breastfeed twins, triplets, quads or more.
Read more on Australian Breastfeeding Association website
Breastfeeding twins | Australian Breastfeeding Association
This article is a shortened version of our booklet 'Breastfeeding:twins, triplets and more' in which we have drawn from the experiences of other mothers of twins to put together information and ideas. We hope these will help you deal with the challenges of breastfeeding and parenting your babies.
Read more on Australian Breastfeeding Association website
Vaginal birth after caesarean (VBAC)
If you've delivered a baby by caesarean (C-section), you may have a choice with your next pregnancy - a vaginal birth after caesarean (VBAC) or a planned (elective) caesarean.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Twins, Triplets, Complications & Symptoms
What is a multiple pregnancy?
A multiple pregnancy is a pregnancy where you’re carrying more than one baby at a time. If you’re carrying two babies, they are called twins. Three babies that are carried during one pregnancy are called triplets. You can also carry more than three babies at one time (high-order multiples). There are typically more risks linked to a multiple pregnancy than a singleton (carrying only one baby) pregnancy.
There are typically more risks linked to a multiple pregnancy than a singleton (carrying only one baby) pregnancy.
How do multiple pregnancies happen?
There are two main ways that a multiple pregnancy can happen:
- One fertilized egg (ovum) splits before it implants in the uterine lining.
- Two or more separate eggs are fertilized by different sperm at the same time.
These two different types of multiple pregnancy result in either identical or fraternal siblings. The difference between identical and fraternal babies goes back to how the multiple pregnancy happens.
Identical twins or triplets happen when a single egg is fertilized and then later splits. These newly divided embryos are identical. Children that are identical multiples will look like each other and be the same sex.
Fraternal multiples develop from separate eggs that are fertilized by a different sperm. Because these are different eggs and different sperm, the genetic material is varied. These children won’t look identical and can be different sexes from each other.
These children won’t look identical and can be different sexes from each other.
In a pregnancy with triplets or more, your babies could be all identical, all fraternal or a mixture of both. This can happen if your body releases multiple eggs and more than one is fertilized. In a case where you have both identical and fraternal multiples, more than one egg was fertilized and then at least one of those eggs also split after fertilization.
Are identical twins or triplets always the same sex?
Because identical twins or triplets share genetic material, they are always the same sex. The sex of a baby is determined by the particular sperm cell that fertilizes the egg at conception. There are two kinds of sperm cells — those carrying an X chromosome or Y chromosome. The mother’s egg carries an X chromosome. If a sperm cell carrying an X chromosome fertilizes the egg, it will make a XX combination (female). If the sperm cell is carrying a Y chromosome, you end up with an XY pairing (male).
Identical multiples start as one egg and then split, so whatever chromosome combination is present at fertilization is the sex of all multiples.
What increases the chance of a multiple pregnancy?
There are several factors that can increase the risk of a multiple birth. You might be at a higher risk of getting pregnant with more than one baby at a time if you:
- Are older (women in their 30s are at a higher risk of multiples because the body starts to release multiple eggs at one time when you get older).
- Are a twin yourself or have twins in your family.
- Are using fertility drugs.
You might also be at a higher risk of a multiple pregnancy if you are taller than average or have a higher body weight.
Another risk factor for a multiple pregnancy is genetic. There is an increased possibility of a multiple pregnancy if you are a multiple yourself, or if multiples run in your family. This heredity trait is generally passed down through the maternal (mother’s) side of the family.
The use of fertility drugs can be another reason you might have a multiple birth. Treatments for infertility can increase your risk of a multiple pregnancy because procedures, like in vitro fertilization (IVF), often involve transferring more than one fertilized egg into your uterus. Your provider usually transfers more than one egg at a time to increase the odds of a successful pregnancy.
How common are multiple births?
Multiple births have become more common in recent years because more people are using fertility drugs and procedures, such as IVF, to help conceive a baby.
What are the signs of a multiple pregnancy?
The only way to know if you’re pregnant with more than one baby during your pregnancy is through an ultrasound exam with your healthcare provider. During this test, your provider can look at images of the inside of your uterus and confirm how many babies are in there.
You might experience more intense symptoms during a multiple pregnancy than with a single pregnancy. These can include:
These can include:
- Severe nausea and vomiting (morning sickness).
- Rapid weight gain in the first trimester of pregnancy.
- Sore or very tender breasts.
- High human chorionic gonadotrophin (hCG) levels — this hormone is made during pregnancy and is what a pregnancy test picks up.
- High amounts of the protein alpha-fetoprotein in your blood.
Apart from an ultrasound, your provider might suspect multiples if there’s more than one heartbeat detected during a fetal Doppler scan.
What complications are linked to multiple births?
Anyone can experience complications during pregnancy — regardless of how many babies you’re carrying. However, most healthcare providers consider multiple pregnancies higher risk than single pregnancies. This doesn’t mean that every woman who carries more than one baby during a pregnancy is going to have problems. If you’re pregnant with multiples, your provider will want to watch you for possible complications that can happen when you carry more than one baby at once. Your provider will talk to you about each risk factor and frequently check with you to make sure you aren’t experiencing anything concerning.
Your provider will talk to you about each risk factor and frequently check with you to make sure you aren’t experiencing anything concerning.
Possible complications include:
- Premature labor and birth: The most common complication of multiple births is premature labor. If you’re pregnant for multiples, you are more likely to go into premature labor (before 37 weeks) than a woman carrying only one baby. The goal for many moms of multiples is to complete 37 weeks. This is considered term in a twin pregnancy and reaching this week of gestation increases the chance the babies will be born healthy and at a good weight. Babies that are born prematurely are at risk of another complication of multiple births — low birth weight.
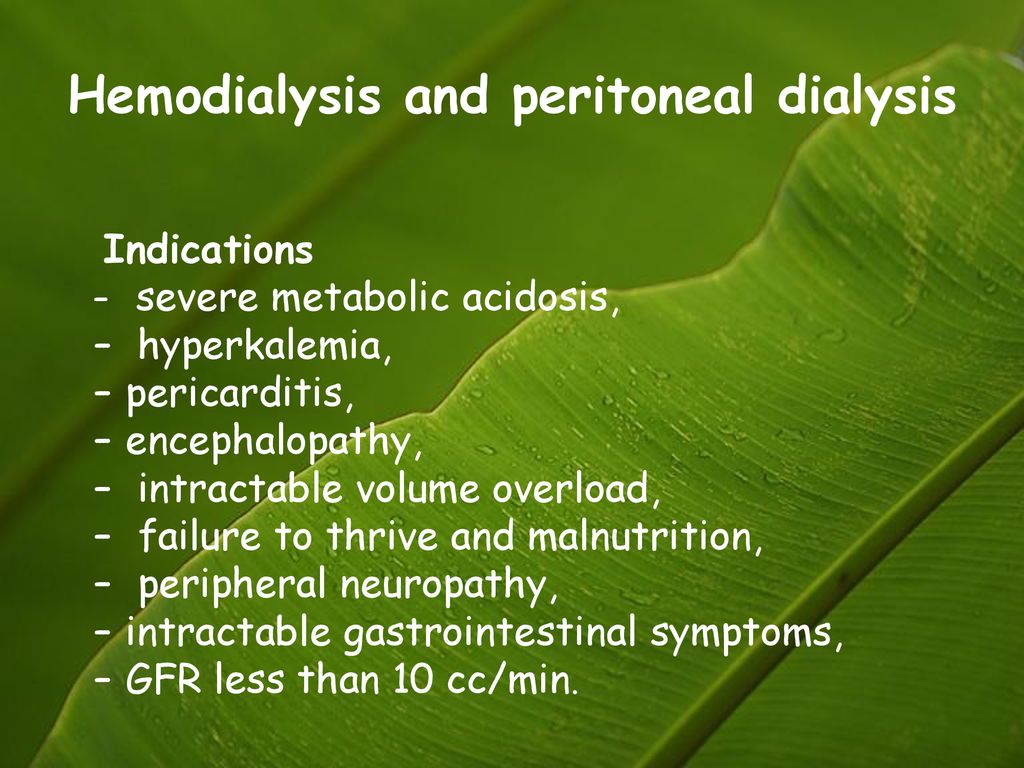
- Preeclampsia or gestational hypertension (high blood pressure): High blood pressure is called hypertension. During pregnancy, your healthcare provider will watch your blood pressure carefully to make sure you don’t develop gestational hypertension (high blood pressure during pregnancy).
 This can lead to a dangerous condition called preeclampsia. Complications related to high blood pressure happen at twice the rate in women carrying multiples compared to women pregnant with only one baby. This complication also tends to happen earlier in pregnancy and be more severe in multiple pregnancies than single pregnancies.
This can lead to a dangerous condition called preeclampsia. Complications related to high blood pressure happen at twice the rate in women carrying multiples compared to women pregnant with only one baby. This complication also tends to happen earlier in pregnancy and be more severe in multiple pregnancies than single pregnancies. - Gestational diabetes: You can develop diabetes during pregnancy. This happens because of the increased amount of hormones from the placenta. The size of the placenta can also be a factor in this condition. If you have two placentas, there’s an increased resistance to insulin.
- Placenta abruption: This condition happens when the placenta detaches (separates) from the wall of your uterus before delivery. This is an emergency situation. Placenta abruption is more common in women who are carrying multiples.
- Fetal growth restriction: This condition can also be called intrauterine growth restriction (IUGR) or small for gestational age (SGA).
 This condition happens when one or more of your babies is not growing at the proper rate. This condition might cause the babies to be born prematurely or at a low birth-weight. Nearly half of pregnancies with more than one baby have this problem.
This condition happens when one or more of your babies is not growing at the proper rate. This condition might cause the babies to be born prematurely or at a low birth-weight. Nearly half of pregnancies with more than one baby have this problem.
Fraternal twins always have two placentas. The risks of pregnancies with fraternal twins are similar to those of pregnancies with only one baby. However, the number of possible risks are increased when compared to pregnancies with one baby.
Identical twins may have one placenta (70% of the cases) or two placentas (30% of the cases). The risks of identical twins with two placentas are similar to those listed above for fraternal twins. Identical twins with one placenta (called monochorionic) have risks that are unique to them. In 5 to 15% of the cases, they may develop a condition called twin-twin-transfusion-syndrome (TTTS). This is the consequence of vascular communications at the placenta level between the twins. Due to these communications, the twins may share their blood. When this happens — if nothing is done — there is a 90% risk that the twins will die in-utero. In-utero procedures are performed to decrease the fetal death risk for the twins.
When this happens — if nothing is done — there is a 90% risk that the twins will die in-utero. In-utero procedures are performed to decrease the fetal death risk for the twins.
Another complication that can happen in identical twins with one placenta is called twin-anemia-polycythemia sequence (TAPS). This is due to blood that goes from one twin to the co-twin because of vascular communications at the placental level. In this condition, one twin becomes anemic (low red-blood cells), whereas the co-twin becomes polycythemic (too many red-blood cells). Several treatments/interventions are performed when this happens.
A third condition that can occur in identical twins with one placenta is called” selective IUGR”. One twin grows well, whereas the co-twin does not experience much growth.
Another condition typical of identical twins is called twin-reversed-arterial-perfusion syndrome. In this condition, the heart of one twin pumps blood for the circulation of both twins. One twin does not have the heart and will not survive following birth. The outcome of the twin with the normal heart varies. Fortunately, this syndrome is rare (1 in 20,000 to 40,000) and it is amenable to in-utero procedures.
The outcome of the twin with the normal heart varies. Fortunately, this syndrome is rare (1 in 20,000 to 40,000) and it is amenable to in-utero procedures.
Identical twins with one placenta may also be in the same sac. They are called monochorionic (one placenta)-monoamniotic (one gestational sac). This pregnancy occurs in 1% of multiple gestations and it’s associated with an increased risk for one or both twins.
Your healthcare provider will diagnose the above conditions with an ultrasound.
Am I more likely to have a C-section delivery if I’m carrying multiples?
A cesarean section is a procedure used to deliver a baby through an incision (cut) in the abdomen. This type of delivery might be used for a variety of reasons, but it’s fairly common in multiple births. Your chance of having a C-section for a multiple birth is higher than if you were pregnant for only one baby. However, even in single births, a C-section can sometimes be the safest option for delivery.
Often, the babies aren’t in the right position for birth — head down. A C-section can also happen if you have a complication during pregnancy that means a vaginal birth isn’t the safest option for you or your babies. Your healthcare provider will monitor you leading up to your due date and talk to you about the best option for delivery.
What can I do to stay healthy during a multiple pregnancy?
Eating nutritious foods, getting enough rest, and visiting the doctor regularly are important steps for any pregnant woman to take toward a healthy pregnancy. These steps are especially important during multiple pregnancies.
If you’re expecting multiples, you have additional dietary needs to meet. Getting enough protein and enough hydration (fluids) is important. You’ll also need to make sure you get enough extra calories for the developing fetuses. One rule of thumb is to eat an extra 300 calories a day per baby. That means that if you’re pregnant with twins, you will need to add 600 calories to your daily diet. Talk to your healthcare provider about your diet and the specific amounts you’ll need for a healthy pregnancy.
Talk to your healthcare provider about your diet and the specific amounts you’ll need for a healthy pregnancy.
Moms of multiples might also experience the typical discomforts of pregnancy more intensely. It’s important to take good care of yourself and get plenty of rest to help ease the stresses of pregnancy.
In some cases, you might want to find a healthcare provider who has experience with multiple births. Specialized healthcare can help ensure that you and your babies are receiving the best care available. The need for frequent, intensive prenatal care is very important in a multiple pregnancy. Talk to your family doctor or OBGYN about their recommendations for specialists.
Can I be active and exercise during a multiple pregnancy?
Exercise and activity is an important part of any pregnancy. In most cases, you can absolutely exercise during a multiple pregnancy. Low-impact exercises are a great way to stay in shape and maintain your health throughout pregnancy. Some low-impact exercises to try during a multiple pregnancy can include:
Some low-impact exercises to try during a multiple pregnancy can include:
- Swimming.
- Walking.
- Prenatal yoga.
Even though activity is wonderful during pregnancy, you should talk to your healthcare provider about the best activities for you. Some more strenuous activities might not be a good idea during a multiple pregnancy, including:
- Jogging.
- Aerobics that involve jumping.
It’s also important to remember that your exercise routine might need to change over time if you experience any complications.
Prolongation of pregnancy with triplets after the birth of the first fetus (description of observation)
Perinatal morbidity and mortality among preterm infants is significantly higher than among full-term infants. Premature births account for approximately 70% of all early neonatal deaths. One of the most important independent risk factors for preterm birth is multiple pregnancy. At the same time, triplets pregnancy in more than 97% of cases is completed before 37 weeks. The average gestational age at the time of the birth of triplets is 33 weeks [1]. It is especially important to emphasize that with triplets, early preterm birth is very common. In recent years, after a decline in the 1980s, the frequency of multiple pregnancies has been steadily increasing. In Russia, in recent years, approximately every hundredth birth is a twin birth, and the frequency of triplets over the past 20 years has increased by 5.5 times [2].
The average gestational age at the time of the birth of triplets is 33 weeks [1]. It is especially important to emphasize that with triplets, early preterm birth is very common. In recent years, after a decline in the 1980s, the frequency of multiple pregnancies has been steadily increasing. In Russia, in recent years, approximately every hundredth birth is a twin birth, and the frequency of triplets over the past 20 years has increased by 5.5 times [2].
Unfortunately, there are currently no effective methods for preventing preterm birth in multiple pregnancies. The results of reviews of the Cochrane Library indicate no effect of β-mimetic agents on the outcome of multiple pregnancies [3, 4]. The effectiveness of progesterone, which reduces the risk of preterm birth in singleton pregnancies, has not been proven in multiple pregnancies [5]. In addition, even the effectiveness of preventing fetal respiratory distress syndrome (RDS) with corticosteroids has not been confirmed in multiple pregnancies [6].
All these facts dictate the need to find new ways to reduce perinatal losses in multiple pregnancies. One of these methods is the delayed birth of fetuses after the birth of the first. In most cases, labor continues after the birth of the first fetus, but sometimes labor can be stopped at this stage. Such a tactic in many cases improves the outcome for the second (third) fetus, whose gestational age at the time of delivery is longer than that of the first. And, if for twins a lot of cases of delaying the birth of the second fetus have already been described, including three cases carried out by us [7], then the cases of prolongation of pregnancy after the birth of the first fetus from triplets are described much less: only a few - in different publications [8-10 ]. At the same time, all authors note an increase in survival in the second / third fetuses.
A relatively significant number of triplets with pregnancy prolongation was described by B. Arabin and van J. Eyck [11], who shared 17 years of experience in prolonging pregnancy after the birth of the first fetus from a multiple pregnancy in one perinatal center in the United States. During this time, an attempt to prolong pregnancy was made in 38 triplets. In 26 cases, second and third births occurred immediately despite tocolytic therapy. Only 12 patients managed to delay the birth of the second fetus. It should be noted that if between the birth of the first and second fetus it was possible to achieve an interval of 2-13 days (and in one case even 144 days), then between the birth of the second and third fetus the interval never reached even 2 days. In cases where the first fetus was born before 25 weeks ( n =7), all the first twins died, and 2 of the next 14 twins survived. If labor began after 25 weeks ( n =5), 3 out of 5 first and 4 out of 10 subsequent children survived [11].
During this time, an attempt to prolong pregnancy was made in 38 triplets. In 26 cases, second and third births occurred immediately despite tocolytic therapy. Only 12 patients managed to delay the birth of the second fetus. It should be noted that if between the birth of the first and second fetus it was possible to achieve an interval of 2-13 days (and in one case even 144 days), then between the birth of the second and third fetus the interval never reached even 2 days. In cases where the first fetus was born before 25 weeks ( n =7), all the first twins died, and 2 of the next 14 twins survived. If labor began after 25 weeks ( n =5), 3 out of 5 first and 4 out of 10 subsequent children survived [11].
At the same time, management after the birth of the first fetus is not clearly defined, and different methods are used in different centers, ranging from expectant management to suturing the cervix [12, 13].
Based on literature data and our own experience [14], we concluded that pregnant women with bichorial twins/trichorial triplets between 18 and 32 weeks of gestation should be selected for attempting to delay the delivery of the second fetus. Contraindications to the procedure were clinical or laboratory signs of chorioamnionitis, placental abruption, rupture of the fetal bladder of the second fetus, anomalies in the development of the second fetus, maternal conditions in which pregnancy prolongation is contraindicated (preeclampsia, etc.). Here is our observation of prolongation of pregnancy after the birth of the first fetus from triplets.
Contraindications to the procedure were clinical or laboratory signs of chorioamnionitis, placental abruption, rupture of the fetal bladder of the second fetus, anomalies in the development of the second fetus, maternal conditions in which pregnancy prolongation is contraindicated (preeclampsia, etc.). Here is our observation of prolongation of pregnancy after the birth of the first fetus from triplets.
Patient K ., 38 years old. Menstrual function without features. Husband 63 years old, healthy. Since 2009, she has been examined and treated for infertility. In 2009, a diagnostic laparoscopy was performed, during which no organic obstacles to pregnancy were identified, but ovarian cauterization was performed. In 2010, 2011 and 2013, intrauterine insemination with ovulation stimulation was performed 3 times. The pregnancy did not occur. In 2014, repeated diagnostic laparoscopy, after which a decision was made to prepare for in vitro fertilization (IVF). In 2014, the IVF procedure was performed with the replanting of three embryos, all the embryos took root.
The initial weight of the patient before the onset of pregnancy was 115 kg with a height of 178 cm. From the beginning of pregnancy, the patient received hormonal support with micronized progesterone. In the course of ultrasound examinations at 12, 15, 18 and 21 weeks, no abnormalities were detected. Ultrasound examination in the period of 24-25 weeks in the consultative and diagnostic department of City Clinical Hospital No. 24 revealed shortening of the cervix to 5 mm and prolapse of the amniotic sac into the cervical canal. The patient was referred for hospitalization.
A pregnant woman was admitted to the Perinatal Center of City Clinical Hospital No. 24 at 24–25 weeks of gestation with a diagnosis of pregnancy at 24–25 weeks. Trichorionic triplets. ECO. The threat of premature birth. Isthmic-cervical insufficiency (ICN). Prolapse of the fetal bladder. OAGA. Obesity III. Varicose veins. When examined with the help of mirrors, prolapse of the fetal bladder beyond the external os, more than 1 cm in diameter, was found. 13 days after hospitalization, premature rupture of the membranes of the first fetus was recorded. Taking into account the gestation period of 26 weeks, the absence of signs of an infectious process (normal level of blood leukocytes, negative procalcitonin test, normal body temperature), a decision was made to prolong the pregnancy.
13 days after hospitalization, premature rupture of the membranes of the first fetus was recorded. Taking into account the gestation period of 26 weeks, the absence of signs of an infectious process (normal level of blood leukocytes, negative procalcitonin test, normal body temperature), a decision was made to prolong the pregnancy.
Regular labor activity developed 16 days after hospitalization (at 26–27 weeks). First fetus in cephalic presentation. A decision was made to carry out childbirth through the birth canal, followed by an attempt to stop labor. The patient received written informed consent.
A live premature girl was born 680 g, 32 cm, with an Apgar score of 4 and 5 points. The anhydrous interval of the first fetus was 3 days 17 hours. After the birth of the first fetus, tocolysis with atosiban was started, the umbilical cord was cut as high as possible with the help of mirrors. After 2 hours, a control ultrasound examination was performed: there were two fetuses in the uterine cavity, the first in cephalic presentation, the heartbeat of both fetuses was 130–140 beats/min, Doppler blood flow was within the normal range. Discharge from the genital tract is bloody, scanty. The uterus is in a normal tone. Considering the satisfactory condition of the fetuses and the pregnant woman, the absence of labor activity, the patient was transferred to the department of pathology of pregnant women. A second course of prevention of fetal RDS with betamethasone was started (more than 2 weeks have passed since the first course).
Discharge from the genital tract is bloody, scanty. The uterus is in a normal tone. Considering the satisfactory condition of the fetuses and the pregnant woman, the absence of labor activity, the patient was transferred to the department of pathology of pregnant women. A second course of prevention of fetal RDS with betamethasone was started (more than 2 weeks have passed since the first course).
After 3 days, the patient developed regular labor activity, tocolytic therapy had no effect, and a live premature girl 800 g, 33 cm was born in cephalic presentation, with an Apgar score of 5 and 6 points. Despite an attempt to stop labor, after 5 minutes a third live premature girl was born in a pure breech position, weighing 750 g, 31 cm tall, with an Apgar score of 5 and 6 points. The postpartum period in the patient proceeded without complications.
In the first child, despite the introduction of a surfactant, respiratory failure gradually increased, the ventilation regimens gradually became tougher, and death occurred on the 4th day. The second and third children received respiratory support with binasal CPAP (positive expiratory pressure breathing) after surfactant administration. On the 3rd day, the second fetus developed episodes of apnea, the frequency of which gradually increased, in connection with which the child was transferred to mechanical ventilation on the 5th day, myoclonic convulsions appeared on the 8th day, and signs of renal failure appeared on the 18th day. . At the age of 1 month 12 days, death was recorded against the background of increasing multiple organ failure. The third child against the background of increasing respiratory failure on the 8th day of life was transferred to mechanical ventilation, which was carried out for 1 month. From the 18th day of life, he stopped receiving cardiotonic therapy; from the 23rd day, enteral nutrition was started. The child was on independent breathing from 39-th days of life. Discharged home at the age of 2 months of life. Thus, only the third child of the triplets survived.
The second and third children received respiratory support with binasal CPAP (positive expiratory pressure breathing) after surfactant administration. On the 3rd day, the second fetus developed episodes of apnea, the frequency of which gradually increased, in connection with which the child was transferred to mechanical ventilation on the 5th day, myoclonic convulsions appeared on the 8th day, and signs of renal failure appeared on the 18th day. . At the age of 1 month 12 days, death was recorded against the background of increasing multiple organ failure. The third child against the background of increasing respiratory failure on the 8th day of life was transferred to mechanical ventilation, which was carried out for 1 month. From the 18th day of life, he stopped receiving cardiotonic therapy; from the 23rd day, enteral nutrition was started. The child was on independent breathing from 39-th days of life. Discharged home at the age of 2 months of life. Thus, only the third child of the triplets survived.
Based on the foregoing, it should be noted that the practice of prolonging pregnancy for the second and third fetuses in triplets after the birth of the first has the right to exist. It is very likely that the repeated course of RDS prevention, as well as the additional 3 days spent in the uterus, increased the chances of survival of the second and third fetuses.
In addition, this case is an additional vivid illustration of the need for strict legal restrictions on the number of transferred embryos during IVF [15]. The probability of a favorable completion of this pregnancy was minimized at the moment when the fertility specialist decided to implant not one, but three embryos.
Management of multiple pregnancy - clinic Family Doctor
Doctors
Clinic doctors
Multiple pregnancy is not only a great happiness, but also an increased burden on the body of the expectant mother. Therefore, special standards apply for its management: more frequent visits to the gynecologist and an extended examination, other recommendations regarding lifestyle.
Therefore, special standards apply for its management: more frequent visits to the gynecologist and an extended examination, other recommendations regarding lifestyle.
It is good if the management of multiple pregnancy begins with its early diagnosis. The sooner this fact is revealed, the higher the chances of drawing up the most successful management plan and timely implementation of measures to prevent possible complications. For patients who plan to conceive and are at risk for multiple pregnancies, it is extremely important to start monitoring immediately after a successful conception.
Why multiple pregnancy occurs
The probability of multiple pregnancy is significantly higher in some categories of patients:
- heredity;
- women planning to conceive after giving up hormonal contraceptives;
- women over 35;
- those who have congenital non-standard structural features of the uterus;
- expectant mothers who have taken advantage of the possibilities of modern reproductive technologies (IVF procedure, etc.
 ).
).
The number of fetuses can be any, as a rule, we are talking about twins or triplets. There are identical (fertilization of one egg, the birth of identical twins) and twin pregnancies. In the second case, two (or more) eggs are fertilized, as a result, different children are born. It is this case that is more often caused by the woman's age, interference in the reproductive processes (IVF, ovulation stimulation, the abolition of COCs). These factors lead to more active work of the ovaries, as a result of which several eggs mature in one menstrual cycle at once.
How and for how long is diagnosed
Early diagnosis is the key to a healthy, successful and full-term multiple pregnancy. The doctor can establish the fact of the presence of two or more fetuses for a short period of time, up to 5 weeks.
The basis for suspecting a larger number of fruits is an examination. The volume of the uterus will be larger than for the expected period. Without fail, a woman takes an analysis for hCG in dynamics - the level of human chorionic gonadotropin, growing at a fast pace, is a sign of multiple pregnancy. Subsequently, during palpation, the doctor will determine the parts of several fetuses, and when listening to heart sounds, they will be observed in different parts of the abdomen.
Without fail, a woman takes an analysis for hCG in dynamics - the level of human chorionic gonadotropin, growing at a fast pace, is a sign of multiple pregnancy. Subsequently, during palpation, the doctor will determine the parts of several fetuses, and when listening to heart sounds, they will be observed in different parts of the abdomen.
Driving features
Conducting multiple pregnancy is carried out with special attention. Features of observation when carrying two or more babies are as follows:
- relatively more frequent visits to the obstetrician-gynecologist: 1 time in 14 days up to 30 weeks and every week until childbirth;
- the appointment of increased doses of vitamins, minerals;
- a more rigorous assessment of the dynamics of weight gain: an increase of no more than 25 kg is considered normal;
- drawing up a special plan for physical activity, its significant reduction from 20-25 weeks;
- more frequent ultrasound, which is associated with the need to assess the dynamics of fetal development and take measures in case of delay, as well as to prevent the threat of preterm birth.
 It is important to assess the condition of the placenta in order to timely determine the compliance of its changes with the gestational age;
It is important to assess the condition of the placenta in order to timely determine the compliance of its changes with the gestational age; - the appointment of drugs that prevent common complications (fetoplacental insufficiency, anemia, preeclampsia, etc.).
Recommendations and standards
There are special standards for the management of two, three and more pregnancies. Immediately after the diagnosis, the doctor will develop a regimen of physical activity and nutrition. This will ensure the high needs of the expectant mother in proteins, fats, carbohydrates, vitamins and minerals, as well as maintain normal health in conditions of high stress on the spine.
Particular attention is paid to the functions of the heart and blood vessels, kidneys. Therefore, the patient more often gives urine tests, additional consultation with a cardiologist, nephrologist, urologist may be required.
The high risk of preterm birth obliges to monitor the slightest changes. If the patient feels well and there are no complications, she is sent to the maternity hospital 2-3 weeks before the preliminary date of delivery. If we are talking about triplets, in 4 weeks.
If the patient feels well and there are no complications, she is sent to the maternity hospital 2-3 weeks before the preliminary date of delivery. If we are talking about triplets, in 4 weeks.
At 30-34 weeks, the likelihood of preterm birth is especially high, which is associated with maximum tension and stretching of the uterus. In addition, shortening and partial opening of the cervix is often observed. The doctor will definitely recommend bed rest if necessary, which will increase the chances of carrying it to the due date. Drugs that relieve muscle spasm, as well as tocolytics, drugs that affect the contractile activity of the uterus, can be prescribed.
FPI or fetoplacental insufficiency is more often observed precisely when carrying several fetuses. Abnormal location of the placenta is also common. This obliges to regularly monitor the condition of the fetus and placenta: perform Doppler ultrasound, CTG. So, starting from the 30th week, it is better to do this once every 7 days until delivery. An experienced specialist should evaluate the blood flow in each fetus individually. FPI can be prevented with the help of preventive drug therapy: drugs that improve uteroplacental, fetoplacental blood flow, antioxidants, metabolic drugs, etc.
An experienced specialist should evaluate the blood flow in each fetus individually. FPI can be prevented with the help of preventive drug therapy: drugs that improve uteroplacental, fetoplacental blood flow, antioxidants, metabolic drugs, etc.
Features of delivery
Delivery can be natural or by caesarean section. In the absence of pathologies and complications, the presence of two fetuses, favorable examination results, a natural option is allowed. Indications for operative delivery are as follows:
- clinically narrow pelvis;
- features of the presentation of one of the fetuses;
- transverse arrangement of one or both babies;
- signs of hypoxia in at least one fetus;
- pregnancy complications in the mother.
These indications are more often related to the planning of the operation. An emergency cesarean may be required after the onset of labor. The doctor makes a decision based on the situation. In some cases, the first child is born naturally, and the second through surgery.
In some cases, the first child is born naturally, and the second through surgery.
The presence of three or more babies is a direct indication for a planned operation. This will significantly reduce the likelihood of complications for both mother and children.
You can apply for a comprehensive pregnancy management service to experienced obstetrician-gynecologists at the Family Doctor clinic. Modern equipment with diagnostic equipment, highly qualified doctors, the ability to undergo all the necessary examinations in one place - all this is the standard for providing high-quality medical care to an expectant mother.
You can make an appointment with an obstetrician-gynecologist at the Family Doctor clinic, a specialist in multiple pregnancy, by calling the contact center in Moscow +7 (495) 775 75 66 or through the online registration form.
The information was checked and confirmed by the obstetrician-gynecologist of the clinic "Family Doctor"
Obstetrician-gynecologists
On medical recording
Gravchikova Tatyana Petrovna
Akusher-gynecologist, doctor of ultrasound diagnostics, leading specialist of the clinic
Clinic on Novoslobodskaya
On medical records
Zakharova Irina Aleksandrovna
Akusher-gynecologist, doctor of ultrasound diagnostic0003
Clinic on Novoslobodskaya
On medical records
Zlatopolskaya Evgenia Leonidovna
Obstetrician-Gynecologist, Ultrasound diagnostic doctor
Clinic on Novoslobodskaya
On Medica, Marina Mikharevna
Ulteskoye,
specialist of the clinic
Clinic on Ozerkovskaya
0003
Clinic for Usacheva
On medical records
Cousin Anastasia Vadimovna
Oblain-gynecologist, Ultrasound diagnostic doctor
Clinic
On Dolce
, Akusherkova, Ultarova doctor, Ultarovova.