Blood test at 12 weeks pregnant
Screening for Down's syndrome, Edwards' syndrome and Patau's syndrome
You will be offered a screening test for Down's syndrome, Edwards' syndrome and Patau's syndrome between 10 and 14 weeks of pregnancy. This is to assess your chances of having a baby with one of these conditions.
Down's syndrome is also called trisomy 21 or T21. Edwards' syndrome is also called trisomy 18 or T18, and Patau's syndrome is also called trisomy 13 or T13.
If a screening test shows that you have a higher chance of having a baby with Down's syndrome, Edwards' syndrome or Patau's syndrome, you'll be offered further tests to find out for certain if your baby has the condition.
What are Down's syndrome, Edwards' syndrome and Patau's syndrome?
Down's syndrome
Down's syndrome causes some level of learning disability.
People with Down's syndrome may be more likely to have other health conditions, such as heart conditions, and problems with the digestive system, hearing and vision. Sometimes these can be serious, but many can be treated.
Read more about Down's syndrome
Edwards' syndrome and Patau's syndrome
Sadly, most babies with Edwards' syndrome or Patau's syndrome will die before or shortly after birth. Some babies may survive to adulthood, but this is rare.
All babies born with Edwards' syndrome or Patau's syndrome will have a wide range of problems, which can be very serious. These may include major complications affecting their brain.
Read more about Edwards' syndrome and Patau's syndrome.
What does screening for Down's syndrome, Edwards' syndrome and Patau's syndrome involve?
Combined test
A screening test for Down's syndrome, Edwards' syndrome and Patau's syndrome is available between weeks 10 and 14 of pregnancy. It's called the combined test because it combines an ultrasound scan with a blood test. The blood test can be carried out at the same time as the 12-week scan.
It's called the combined test because it combines an ultrasound scan with a blood test. The blood test can be carried out at the same time as the 12-week scan.
If you choose to have the test, you will have a blood sample taken. At the scan, the fluid at the back of the baby's neck is measured to determine the "nuchal translucency". Your age and the information from these 2 tests are used to work out the chance of the baby having Down's syndrome, Edwards' syndrome or Patau's syndrome.
Obtaining a nuchal translucency measurement depends on the position of the baby and is not always possible. If this is the case, you will be offered a different blood screening test, called the quadruple test, when you're 14 to 20 weeks pregnant.
Quadruple blood screening test
If it was not possible to obtain a nuchal translucency measurement, or you're more than 14 weeks into your pregnancy, you'll be offered a test called the quadruple blood screening test between 14 and 20 weeks of pregnancy. This only screens for Down's syndrome and is not as accurate as the combined test.
This only screens for Down's syndrome and is not as accurate as the combined test.
20-week screening scan
For Edwards' syndrome and Patau's syndrome, if you are too far into your pregnancy to have the combined test, you'll be offered a 20-week screening scan. This looks for physical conditions, including Edwards' syndrome and Patau's syndrome.
Can this screening test harm me or my baby?
The screening test cannot harm you or the baby, but it's important to consider carefully whether to have this test.
It cannot tell you for certain whether the baby does or does not have Down's syndrome, Edward's syndrome or Patau's syndrome, but it can provide information that may lead to further important decisions. For example, you may be offered diagnostic tests that can tell you for certain whether the baby has these conditions, but these tests have a risk of miscarriage.
Do I need to have screening for Down's syndrome, Edwards' syndrome and Patau's syndrome?
You do not need to have this screening test – it's your choice. Some people want to find out the chance of their baby having these conditions while others do not.
You can choose to have screening for:
- all 3 conditions
- Down's syndrome only
- Edwards' syndrome and Patau's syndrome only
- none of the conditions
What if I decide not to have this test?
If you choose not to have the screening test for Down's syndrome, Edwards' syndrome or Patau's syndrome, you can still choose to have other tests, such as a 12-week scan.
If you choose not to have the screening test for these conditions, it's important to understand that if you have a scan at any point during your pregnancy, it could pick up physical conditions.
The person scanning you will always tell you if any conditions are found.
Getting your results
The screening test will not tell you whether your baby does or does not have Down's, Edwards' or Patau's syndromes – it will tell you if you have a higher or lower chance of having a baby with one of these conditions.
If you have screening for all 3 conditions, you will receive 2 results: 1 for your chance of having a baby with Down's syndrome, and 1 for your joint chance of having a baby with Edwards' syndrome or Patau's syndrome.
If your screening test returns a lower-chance result, you should be told within 2 weeks. If it shows a higher chance, you should be told within 3 working days of the result being available.
This may take a little longer if your test is sent to another hospital. It may be worth asking the midwife what happens in your area and when you can expect to get your results.
You will be offered an appointment to discuss the test results and the options you have.
The charity Antenatal Results and Choices (ARC) offers lots of information about screening results and your options if you get a higher-chance result.
Possible results
Lower-chance result
If the screening test shows that the chance of having a baby with Down's syndrome, Edwards' syndrome and Patau's syndrome is lower than 1 in 150, this is a lower-chance result. More than 95 out of 100 screening test results will be lower chance.
A lower-chance result does not mean there's no chance at all of the baby having Down's syndrome, Edwards' syndrome or Patau's syndrome.
Higher-chance result
If the screening test shows that the chance of the baby having Down's syndrome, Edwards' syndrome or Patau's syndrome is higher than 1 in 150 – that is, anywhere between 1 in 2 and 1 in 150 – this is called a higher-chance result.
Fewer than 1 in 20 results will be higher chance. This means that out of 100 pregnancies screened for Down's syndrome, Edwards' syndrome and Patau's syndrome, fewer than 5 will have a higher-chance result.
A higher-chance result does not mean the baby definitely has Down's syndrome, Edwards' syndrome or Patau's syndrome.
Will I need further tests?
If you have a lower-chance result, you will not be offered a further test.
If you have a higher-chance result, you can decide to:
- not have any further testing
- have a second screening test called non-invasive prenatal testing (NIPT) – this is a blood test, which can give you a more accurate screening result and help you to decide whether to have a diagnostic test or not
- have a diagnostic test, such as amniocentesis or chorionic villus sampling (CVS) straight away – this will tell you for certain whether or not your baby has Down's syndrome, Edwards' syndrome or Patau's syndrome, but in rare cases can cause a miscarriage
You can decide to have NIPT for:
- all 3 conditions
- Down's syndrome only
- Edwards' syndrome and Patau's syndrome only
You can also decide to have a diagnostic test after NIPT.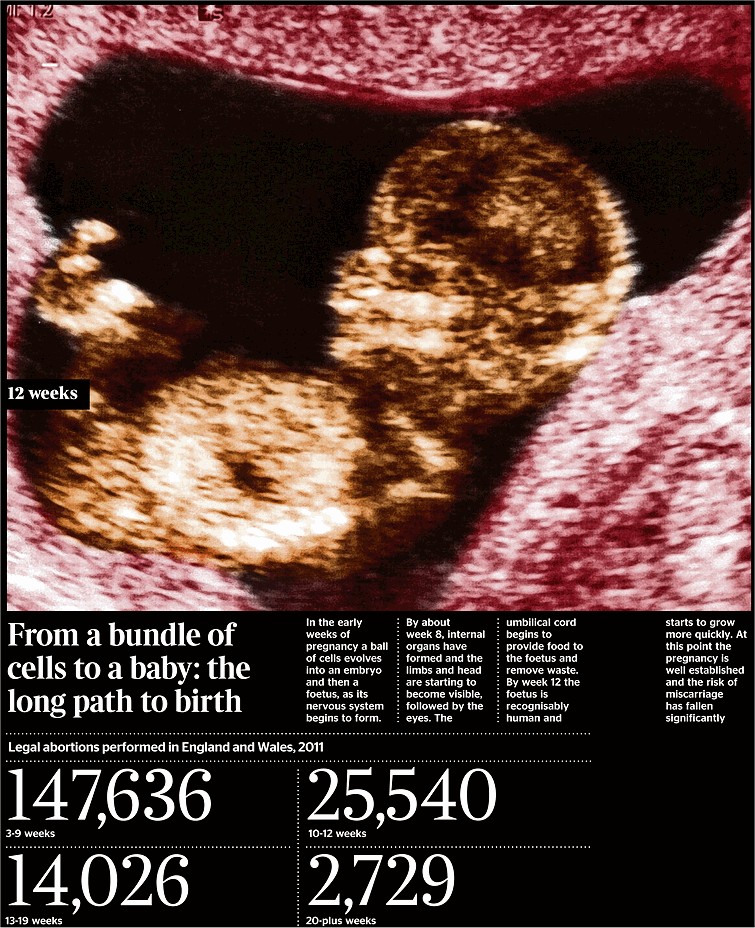
NIPT is completely safe and will not harm your baby.
Discuss with your healthcare professional which tests are right for you.
Whatever results you get from any of the screening or diagnostic tests, you will get care and support to help you to decide what to do next.
If you find out your unborn baby has Down's syndrome, Edwards' syndrome or Patau's syndrome
If you find out your baby has Down's syndrome, Edwards' syndrome or Patau's syndrome a specialist doctor (obstetrician) or midwife will talk to you about your options .
You can read more about what happens if antenatal screening tests find something.
You may decide to continue with the pregnancy and prepare for your child with the condition.
Or you may decide that you do not want to continue with the pregnancy and have a termination.
If you are faced with this choice, you will get support from health professionals to help you make your decision.
For more information see GOV.UK: Screening tests for you and your baby
The charity Antenatal Results and Choices (ARC) runs a helpline from Monday to Friday, 10am to 5.30pm on 020 7713 7486.
The Down's Syndrome Association also has useful information on screening.
The charity SOFT UK offers information and support through diagnosis, bereavement, pregnancy decisions and caring for all UK families affected by Edwards' syndrome (T18) or Patau's syndrome (T13).
First trimester tests during pregnancy
Written by WebMD Editorial Contributors
Routine tests help keep close tabs on you and your baby. That’s why it’s so important to keep all your prenatal appointments. Screening tests can spot potential problems early.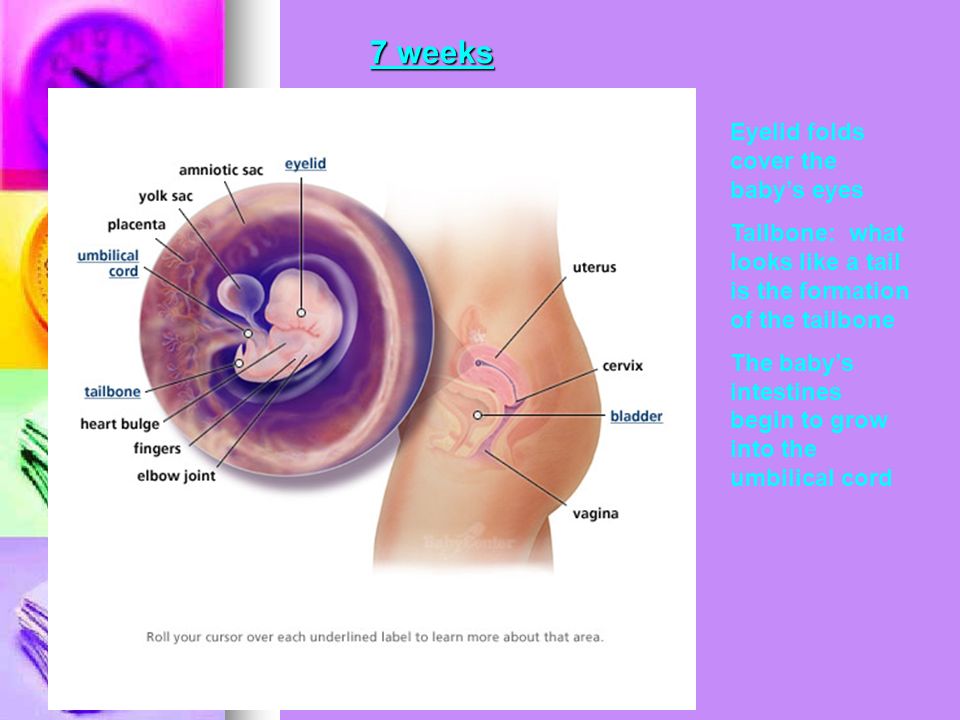
These tests usually include:
History and physical exam. During your first or second prenatal visit, you’ll answer a lot of questions about your health and family history. This information helps the doctor know whether you have any specific risks to address, such as an inherited genetic disorder. You will also have a physical exam. Your doctor will calculate your due date based on the date of your last menstrual period.
Pelvic exam and Pap smear.Prenatal testing during the first trimester begins with a pelvic exam and Pap smear to check the health of your cervical cells. This testing screens for cervical cancer and for certain sexually transmitted diseases (STDs).
Blood tests. During one of your first visits, your doctor or midwife will identify your blood type and Rh (rhesus) factor, screen for anemia, check for immunity to rubella (German measles), and test for hepatitis B, syphilis, and HIV and other STDs.
Depending on racial, ethnic, or family background, you may be offered tests and genetic counseling to assess risks for diseases such as Tay-Sachs, cystic fibrosis, and sickle cell anemia (if these weren't done at a preconception visit). Testing for some of these diseases can also be done with saliva.
Testing for some of these diseases can also be done with saliva.
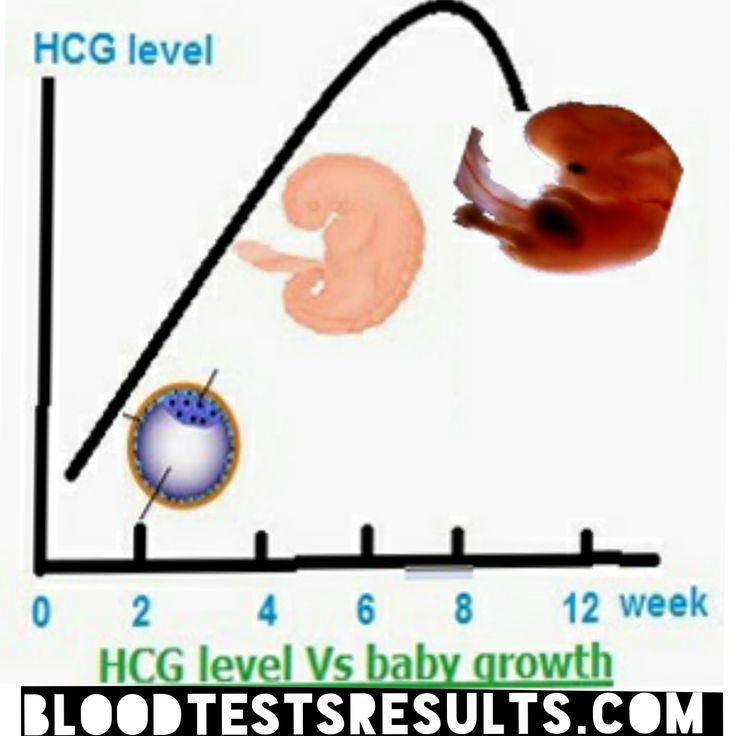
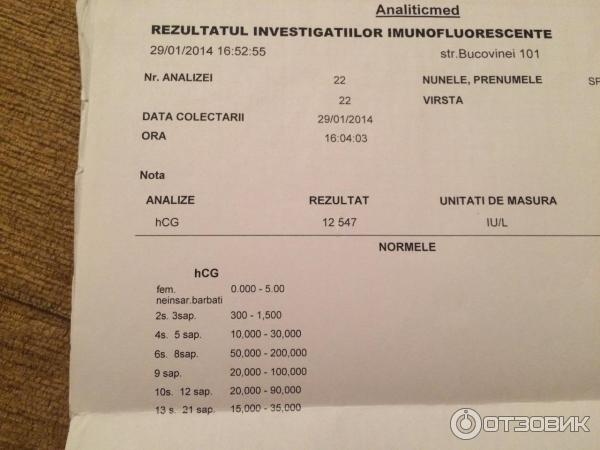
You might be tested for exposure to diseases such as toxoplasmosis and varicella (the virus that causes chickenpox. Your health care provider may also want to check your levels of hCG, a hormone secreted by the placenta, and progesterone, a hormone that helps maintain the pregnancy.
Urine tests. You will also be asked early on for a urine sample so that your doctor or midwife can look for signs of kidney infection and, if necessary, can confirm your pregnancy by measuring the hCG level. (A blood hCG test to confirm pregnancy may be used instead.) Urine samples will be collected regularly to spot glucose (a sign of diabetes) and protein, which could show preeclampsia, a pregnancy-induced disease marked by high blood pressure.
In the later part of the first trimester you will be offered genetic testing. Some people feel like these tests may cause them undue stress, and they prefer to make sure the baby is genetically normal after delivery. Others want all the testing they can get, realizing that these tests sometimes are not 100% accurate. Talk with your doctor or with a genetic counselor about the pros and the cons before you decide. There are different genetic testing options that involve blood tests alone or with an ultrasound that involve no risk to the fetus. If these noninvasive tests are abnormal, you might have further tests.
Others want all the testing they can get, realizing that these tests sometimes are not 100% accurate. Talk with your doctor or with a genetic counselor about the pros and the cons before you decide. There are different genetic testing options that involve blood tests alone or with an ultrasound that involve no risk to the fetus. If these noninvasive tests are abnormal, you might have further tests.
One first semester genetic test combines a blood test with an ultrasound to screen for Down syndrome. It may be available between 11 and 14 weeks of pregnancy. The results of a blood test that measures hCG and PAPP-A (pregnancy-associated plasma protein A) in maternal blood are used with an ultrasound measurement of the skin at the back of the fetus’ neck (called nuchal translucency). The procedure may be able to spot many Down syndrome cases and other genetic conditions. However, as with all screening methods, a more invasive diagnostic technique like CVS is used if results are positive.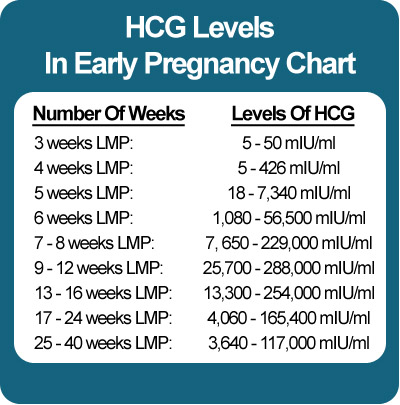
Noninvasive prenatal testing (NIPT). This cell-free fetal DNA test can be done as early as after 10 weeks of pregnancy. The test uses a blood sample to measure the relative amount of free fetal DNA in a mother's blood. It's thought that the test can detect 99% of all Down syndrome pregnancies. It also tests for some other chromosomal abnormalities.
Chorionic villus sampling (CVS). If you're 35 or older, have a family history of certain diseases, or have had a positive result on noninvasive genetic tests, you will be offered this invasive test, usually between 10 and 12 weeks of pregnancy. CVS can detect many genetic defects, such as Down syndrome, sickle cell anemia, cystic fibrosis, hemophilia, and muscular dystrophy. The procedure involves threading a tiny catheter through your cervix or inserting a needle into your abdomen to get a tissue sample from the placenta. The procedure carries a 1% risk of inducing miscarriage and is about 98% accurate in ruling out certain chromosomal birth defects. But, in contrast to amniocentesis, it does not help in detecting neural tube disorders, such as spina bifida and anencephaly, or abdominal wall defects.
But, in contrast to amniocentesis, it does not help in detecting neural tube disorders, such as spina bifida and anencephaly, or abdominal wall defects.
Be sure to discuss all of your testing options with your doctor so that together you can decide on the ones that will be best for you.
If you’re expecting twins, it’s a high-risk pregnancy. For this reason, your doctor will want to watch you and your babies closely. You'll have all the routine tests, but expect to have some of them earlier and more often.
Your doctor may suggest that you see a perinatologist, also called a maternal fetal medicine specialist. These doctors are obstetricians who specialize in high-risk pregnancies. They may work with your regular obstetrician to manage your pregnancy and order tests.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Frequently asked questions about biochemical screening of pregnant women
What tests are performed on pregnant women?
Currently, two main types of tests are recommended for pregnant women in St. Petersburg:
Petersburg:
- analysis for PAPP-A and beta-hCG in the period of 9-13 weeks
- analysis for AFP and hCG.
Should I do a “triple test”?
Some private laboratories use the so-called “triple test”, using kits that, in addition to AFP and hCG, have added the determination of the concentration of another hormone - unconjugated estriol. According to modern data, its assessment for clarifying the risks of fetal chromosomal pathology has too little weight and is highly dependent on many other factors of the woman's condition, which is not significant for calculating risks for fetal chromosomal pathology. If the results of the “double” test reveal an increased risk for you, it is better to contact a geneticist and understand the situation, taking into account a professional clinical assessment of the test results.
How important is it to accurately indicate the weight of a pregnant woman when taking blood for “fetal proteins”?
Each woman's weight must be recorded on the examination referral. In the absence of such information, the risk can be calculated "according to the average" weight of pregnant women in this period - 60 kg.
In the absence of such information, the risk can be calculated "according to the average" weight of pregnant women in this period - 60 kg.
All women are different - there are pregnant women weighing 45 and 145 kg. For a more accurate assessment of the results, an amendment is introduced in accordance with the "weight category". But absolute accuracy is not required here - individual grams will not change the calculations. An individual approach is important. Therefore, we always measure a woman's weight before taking tests.
I took a blood test for fetal proteins, as the doctor prescribed them immediately after taking them, now I'm worried, so I had a hearty breakfast in the morning. Will this affect the outcome of the study? Can I retake blood on an empty stomach?
Don't worry! Unlike most "adult" tests that are sensitive to food intake, the measurement of the amount of any proteins entering the mother's blood from the fetus is not dependent on the time of the meal.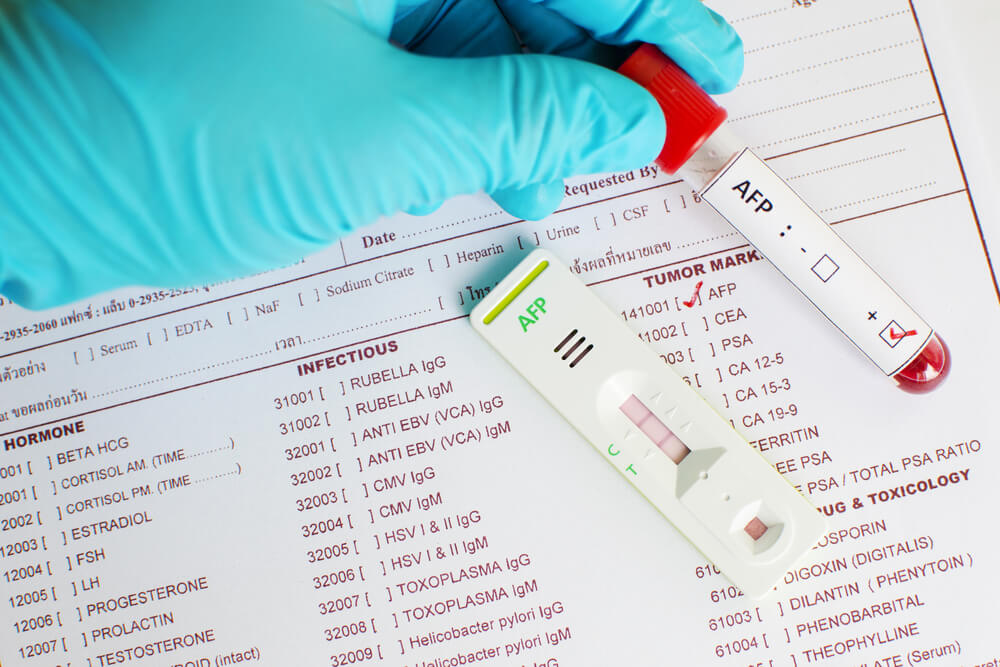 The most important thing here is to know exactly the gestational age established by ultrasound. It makes no sense to retake the analysis. And it is very important for pregnant women to eat breakfast and continue to eat more often during the day than usual.
The most important thing here is to know exactly the gestational age established by ultrasound. It makes no sense to retake the analysis. And it is very important for pregnant women to eat breakfast and continue to eat more often during the day than usual.
In clinics where an individual approach to the examination of pregnant women is possible, and of course, in our Center for Fetal Medicine, blood for screening tests can be donated throughout the working day.
Which test is better - PAPP-A and beta-hCG or AFP and hCG?
At present, the first one has the absolute advantage. It has been proven that it is more specific for assessing risks for chromosomal pathology, including Down syndrome. Its important advantage is that it is carried out in the first trimester, you can donate blood from the age of 9weeks of pregnancy (determined by the size of the fetus on ultrasound). The most optimal terms for this analysis are 9-12 weeks. A study period of up to almost 14 (13 weeks 6 days) is allowed, but the reliability of the risk assessment will be lower.
If you have completed a full first trimester test, performed an ultrasound and received a conclusion from a geneticist about a low risk to the fetus for chromosomal pathology, it is not worth testing for AFP and hCG.
In special cases, after the first screening, a test for AFP and hCG is prescribed as an additional test on the recommendation of a geneticist.
If you missed the first screening test, then, of course, you need to donate blood at least for the second one within 15 to 18 weeks.
I would like to emphasize that, on the recommendation of international experts in prenatal diagnosis, analysis for PAPP-A and beta-hCG in a period of 9-12 weeks is recommended for all pregnant women at any age.
I went through the IVF procedure and used a donor cell, because my cells do not mature at the age of 46. Now 12 weeks. How do I correctly pass a biochemical test?
You urgently need to donate blood for PAPP-A and beta-hCG and perform an ultrasound. From your age, the IVF procedure itself does not change the amount of proteins. And the risk "by proteins" will be assessed depending on certain concentrations.
From your age, the IVF procedure itself does not change the amount of proteins. And the risk "by proteins" will be assessed depending on certain concentrations.
But the computer program calculates the "combined" risks - by proteins, by ultrasound and by the age of the woman, more precisely, by the "age of the egg." Accordingly, for this analysis, the age of the egg donor must be indicated in the calculation referral. If you do not know it exactly, you can calculate by low age risk, since all donors have age restrictions for participating in the IVF program. If you have already been calculated according to your age, don't worry, we can reassess the risks taking into account real data and issue you a Medical Genetic Conclusion based on the results of prenatal studies.
Doctors of the Fetal Medicine Center are one of the leading specialists in prenatal diagnostics, candidates of medical sciences, doctors of the highest categories with a narrow specialization and extensive experience in prenatal medicine.
All ultrasound examinations in the center are carried out according to the international standards FMF (Fetal Medicine Foundation) and ISUOG (International Society for Ultrasound in Obstetrics and Gynecology).
Ultrasound doctors have international certificates from the Fetal Medicine Foundation (Fundamental Medicine, UK), which are are confirmed annually.
We take care of the most complex cases and, if necessary, it is possible to consult with specialists from King's College Hospital, King's College Hospital (London, UK).
The pride of our Centers - modern and high-tech medical equipment from General Electric: expert-class ultrasonic devices Voluson E8 / E10
The capabilities of these devices allow us to talk about a new level of information content.
You can make an appointment and get an expert opinion of our ultrasound specialists by calling the single contact center +7 (812) 458-00-00
Citizens | Ministry of Health of the Kaliningrad Region
| Gestational age | Analyzes | Events (registration, medical examinations, doctor visit schedule) |
| Up to 12 weeks | Early registration in the antenatal clinic Taking medications: folic acid throughout the first trimester, no more than 400 mcg / day; potassium iodide 200-250 mcg/day (in the absence of thyroid disease) | |
| At first appearance | An obstetrician-gynecologist collects anamnesis, conducts a general physical examination of the respiratory, circulatory, digestive, urinary system, mammary glands, anthropometry (measuring height, body weight, determining body mass index), measuring the size of the pelvis, examining the cervix in the mirrors, bimanual vaginal study | |
| Not later than 7-10 days after the initial visit to the antenatal clinic | Inspections and consultations: - general practitioner; - a dentist; - an otolaryngologist; - an ophthalmologist; - other medical specialists - according to indications, taking into account concomitant pathology | |
| First trimester (up to 13 weeks) (and at first visit) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol. 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, to the herpes simplex virus (HSV), to cytomegalovirus (CMV), determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of the main blood groups (A, B, 0) and Rh-affiliation. In Rh-negative women: a) examination of the father of the child for group and Rh-affiliation. 7. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 8. Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida. 9. PCR chlamydial infection, PCR gonococcal infection, PCR mycoplasma infection, PCR trichomoniasis. | Visiting an obstetrician-gynecologist every 3-4 weeks (with the physiological course of pregnancy). Electrocardiography (hereinafter - ECG) as prescribed by a general practitioner (cardiologist). Up to 13 weeks of pregnancy are accepted: - folic acid no more than 400 mcg / day; - potassium iodide 200-250 mcg / day (in the absence of thyroid disease) |
| 1 time per month (up to 28 weeks) | Blood test for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 11-14 weeks | Biochemical screening for serum marker levels: - pregnancy-associated plasma protein A (PAPP-A), - free beta subunit of human chorionic gonadotropin (hereinafter - beta-CG) | In the office of prenatal diagnostics, an ultrasound examination (hereinafter referred to as ultrasound) of the pelvic organs is performed. According to the results of complex prenatal diagnostics, a conclusion of a geneticist is issued. |
| After 14 weeks - once | Culture of midstream urine | To exclude asymptomatic bacteriuria (the presence of bacterial colonies more than 105 in 1 ml of an average portion of urine, determined by a culture method without clinical symptoms) to all pregnant women. |
| In the second trimester (14-26 weeks) | General (clinical) analysis of blood and urine. | Visiting an obstetrician-gynecologist every 2-3 weeks (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), uterine tone, palpation of the fetus, auscultation of the fetus with a stethoscope. Potassium iodide 200-250 mcg/day |
| 1 time per month (up to 28 weeks) | Blood for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 16-18 weeks | Blood test for estriol, alpha-fetoprotein, beta-hCG | Only at late turnout unless biochemical screening for serum marker levels at 11-14 weeks |
| 18-21 weeks | The second screening ultrasound of the fetus is performed in the antenatal clinic | |
| In the third trimester (27-40 weeks) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol). 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 7. | A visit to an obstetrician-gynecologist every 2 weeks, after 36 weeks - weekly (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, VDM, uterine tone, fetal palpation, auscultation of the fetus with a stethoscope. Potassium iodide 200-250 mcg/day |
| 24-28 weeks | Oral glucose tolerance test (OGTT) | |
| 28-30weeks | In Rh-negative women with Rh-positive blood of the child's father and the absence of Rh antibodies in the mother's blood | Administration of human immunoglobulin antirhesus RHO[D] |
| 30 weeks | A certificate of incapacity for work is issued for maternity leave | |
| 30-34 weeks | The third screening ultrasound of the fetus with dopplerometry in the antenatal clinic. - general practitioner; - a dentist. | |
| After 32 weeks | At each visit to the doctor of the antenatal clinic, in addition to determining the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), the tone of the uterus, determine the position of the fetus, the presenting part, the doctor auscultates the fetus with a stethoscope. | |
| After 33 weeks | Cardiotocography (hereinafter referred to as CTG) of the fetus is performed | |
| Throughout pregnancy | In antenatal clinics there are schools for pregnant women, which are attended by expectant mothers along with fathers. In the process of learning, there is an acquaintance with the changes in the body of a woman during physiological pregnancy, acquaintance with the process of childbirth, the correct behavior in childbirth, the basics of breastfeeding. | |
| Over 37 weeks | Hospitalization with the onset of labor. According to indications - planned antenatal hospitalization. | |
| 41 weeks | Planned hospitalization for delivery | |
| No later than 72 hours after delivery | All women with an Rh-negative blood group who gave birth to a child with a positive Rh-belonging, or a child whose Rh-belonging is not possible to determine, regardless of their compatibility according to the AB0 system | Re-introduction of human immunoglobulin anti-rhesus RHO[D] |
| postpartum period | 1. Early breastfeeding 2. Recommendations for breastfeeding. 3. Consultation of medical specialists on concomitant extragenital disease (if indicated). 4. Toilet of the external genital organs. 5. Dry processing of seams (if any). |
 General (clinical) blood test.
General (clinical) blood test. 
 General (clinical) blood test.
General (clinical) blood test. 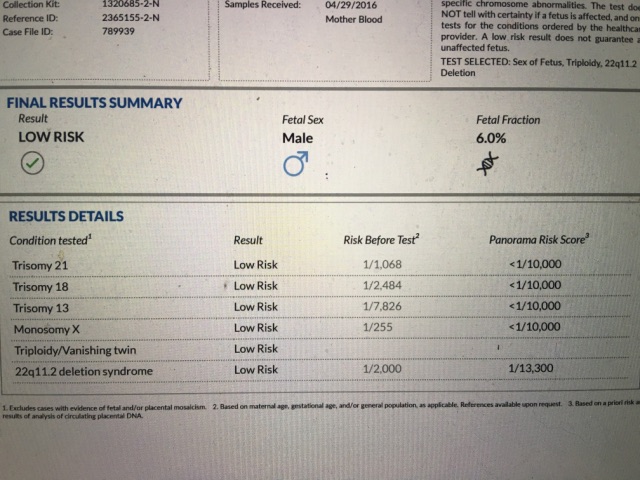 Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.
Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.  Inspections and consultations:
Inspections and consultations: