Difference between vaccine and injection
Vaccines and Immunization - A Brief Overview
Monkeypox arrived in Alaska in July. While the risk of monkeypox to the general public is currently low, the news reminds us of the importance of immunizations and vaccinations for other communicable diseases like measles, mumps, polio, etc. This article explains what they are, how long they last, why we need them, and more.
What is the difference between vaccination and immunization?
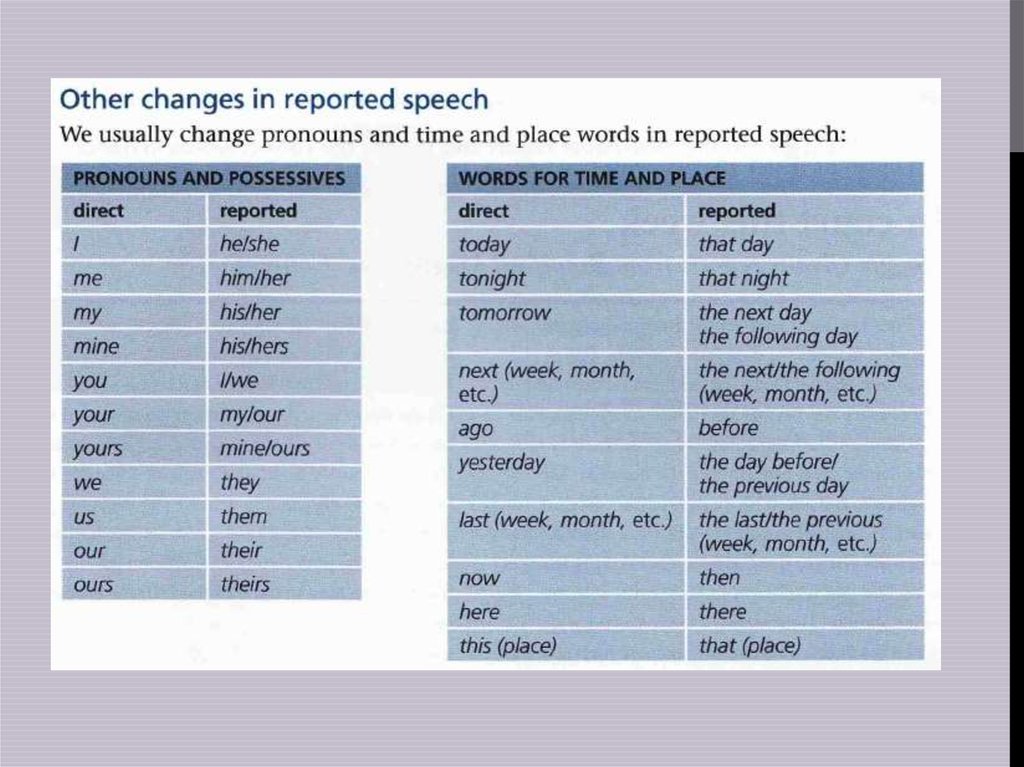
A vaccination is an injection you are given with the vaccine itself. Immunization is what the body does after it receives the injection. The vaccine stimulates the body’s immune system so it can recognize the disease and protect you from future infections (i.e., you become immune to the infection). “Vaccination” and “immunization” are often used interchangeably, but their meanings are not the same.
Getting immunized can protect our bodies from life-threatening viral infections such as hepatitis, HPV, measles, and so much more. Millions of people are safe today from unnecessary deaths from 16 dangerous infectious diseases because of the availability of vaccines.
When do we need vaccines?
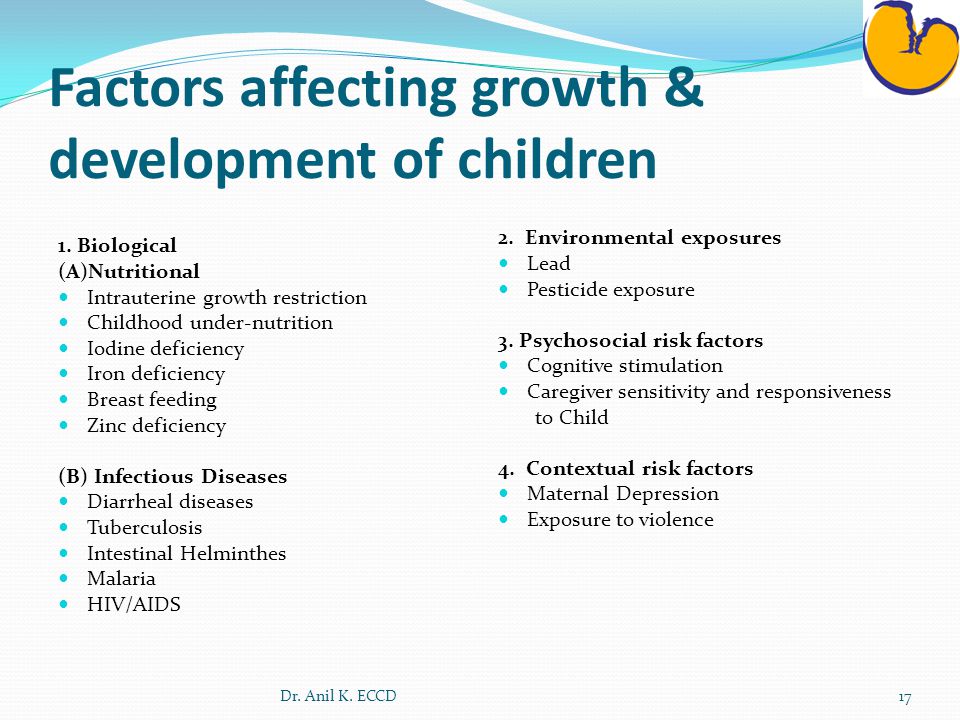
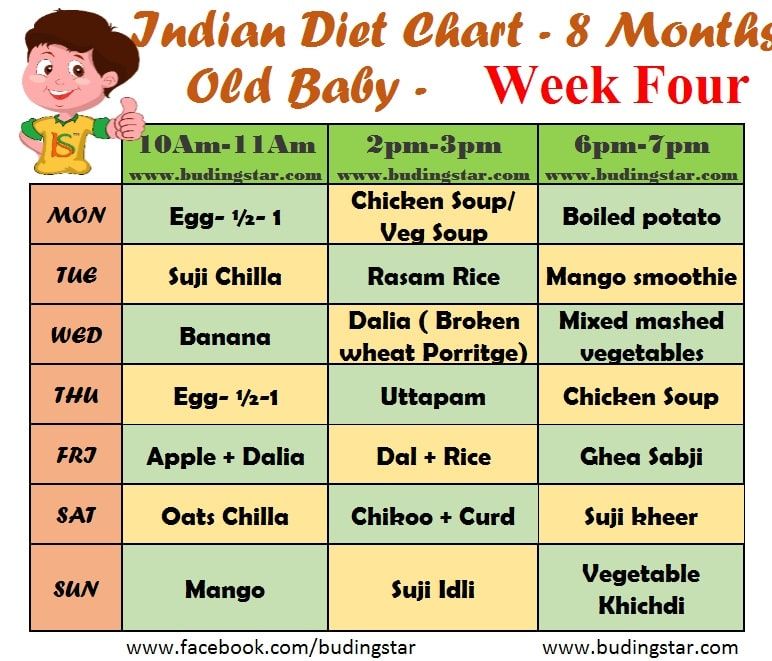
At birth, a pediatrician can provide parents with a list of vaccines and the timeframe for administering each of them. Babies indeed get antibodies from their mothers, but these antibodies wear off after a certain period. For this reason, regular shots are required from 0-6 years of age. Newborns are susceptible to millions of pathogens, which are mostly tolerated by their immune system, while others are deadly. Children need long-term protection that comes from immunization. Therefore, making sure that he or she gets the vaccines needed by following the CDC’s recommended immunization schedule.
Do vaccines last a lifetime?
No. Antibodies wear off over time, especially when your immune system is weak. Therefore, health care providers recommend you get another set of vaccines called “booster shots” in adulthood to retain the integrity of your immune system.
What happens if a person is hypersensitive to vaccines?
Hypersensitivity to vaccines is rare. In some cases, people may be too old, too young, or have vulnerable immune systems. However, one should never lose hope. You can still be protected from pathogens even if your body cannot tolerate vaccines; this is called herd immunity.
What is Herd Immunity?
Herd immunity is indirect protection for people with hypersensitivity to immunization. It can happen naturally when a considerable percentage of the population in an area is vaccinated, creating a measure of protection to individuals who are not immunized.
Questions… Questions.
As new parents, you may have a million questions about vaccinations and the safety of your child. Sunshine Community Health Center has well-trained staff, who can answer your queries and provide you assurance to keep your little angels safe.
The National Immunization Awareness month encourages and reminds everyone to get their shots regularly, avoid the spread of disease, and protect those individuals who cannot get immunized. Bee Wise, Immunize.
Immunisation or vaccination - what's the difference?
Immunisation or vaccination - what's the difference? | Pregnancy Birth and Baby beginning of content6-minute read
Listen
What is a vaccine?
Vaccination prepares the immune system to fight against a future infection. Vaccines often contain tiny amounts of dead or weakened viruses or bacteria, called antigens. The immune system responds to these antigens without you getting sick, effectively training the immune system to fight the disease if exposed to it in the future.
The immune system responds to these antigens without you getting sick, effectively training the immune system to fight the disease if exposed to it in the future.
Some vaccines need to be given more than once — known as ‘booster’ vaccinations. Some vaccines, such as the seasonal influenza (flu) vaccine, only work for a short period of time. This is because the virus itself can change over time.
Vaccines are usually given with an injection.
What is in vaccines?
Some vaccines contain a very small dose of a live but weakened form of a virus. Some vaccines contain a very small dose of killed bacteria or small parts of bacteria, and other vaccines contain a small dose of a modified toxin produced by bacteria.
Vaccines may also contain either a small amount of preservative or a small amount of an antibiotic to preserve the vaccine. Some vaccines may also contain a small amount of an aluminium salt, which helps produce a better immune response.
How does immunisation work?
The terms ‘vaccination’ and ‘immunisation’ don’t mean quite the same thing.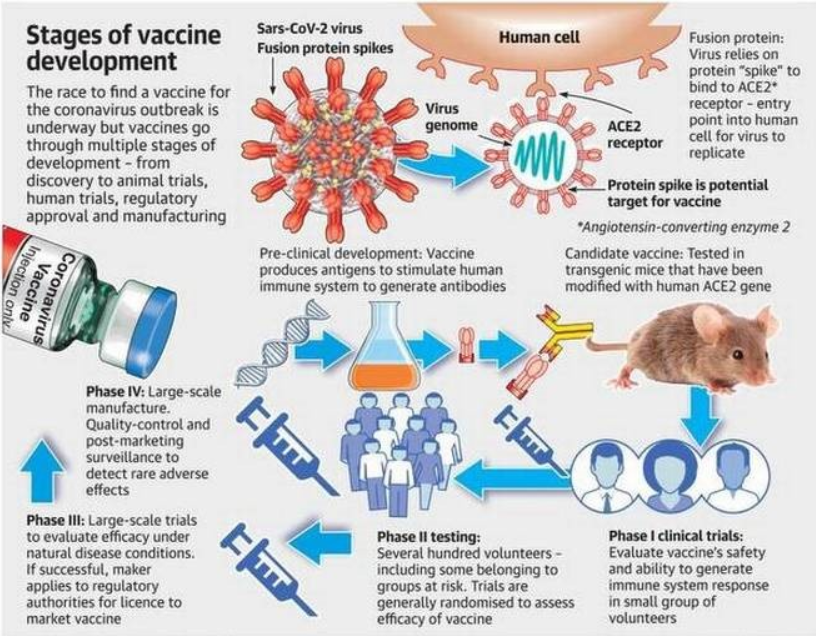 Vaccination is the term used for getting a vaccine — that is, actually getting the injection or taking an oral vaccine dose. Immunisation refers to the process of both getting the vaccine and becoming immune to the disease following vaccination.
Vaccination is the term used for getting a vaccine — that is, actually getting the injection or taking an oral vaccine dose. Immunisation refers to the process of both getting the vaccine and becoming immune to the disease following vaccination.
All forms of immunisation work in the same way. When someone is injected with a vaccine, their body produces an immune response in the same way it would following exposure to a disease but without the person getting the disease. If the person comes in contact with the disease in the future, the body is able to make an immune response fast enough to prevent the person developing the disease or developing a severe case of the disease.
What’s the difference between a booster dose and a primary vaccine course?
A primary vaccine course involves the vaccine doses you need for very good protection against a disease.
A booster dose refers to an extra dose of a vaccine that is given after you’ve completed the primary vaccine course.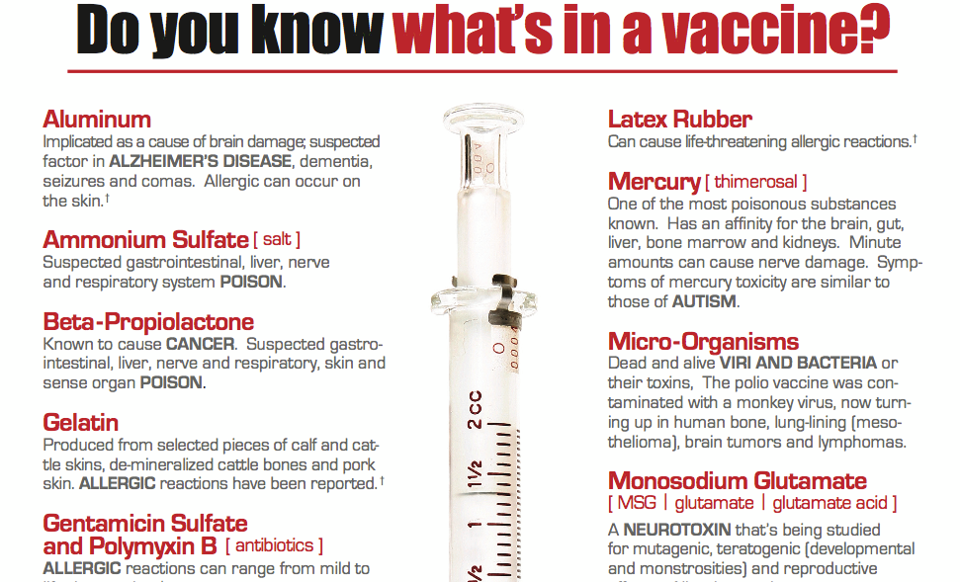
It gives your immune system a 'boost' and helps provide a higher level of protection from the disease.
Booster doses are common with diseases such as COVID-19, tetanus and whooping cough (pertussis).
How long do immunisations take to work?
In general, the normal immune response takes approximately 2 weeks to work. This means protection from an infection will not occur immediately after immunisation. Most immunisations need to be given several times to build long-lasting protection.
A child who has been given only 1 or 2 doses of the DTPa vaccine is only partially protected against diphtheria, tetanus and pertussis (whooping cough) and may become sick if exposed to these diseases until they have all the doses they need. However, some of the new vaccines, such as the meningococcal ACWY vaccine, provide long-lasting immunity after only one dose.
How long do immunisations last?
The protective effect of immunisations is not always lifelong. Some, like tetanus vaccine, can last up to 10 years depending on your age, after which time a booster dose may be given.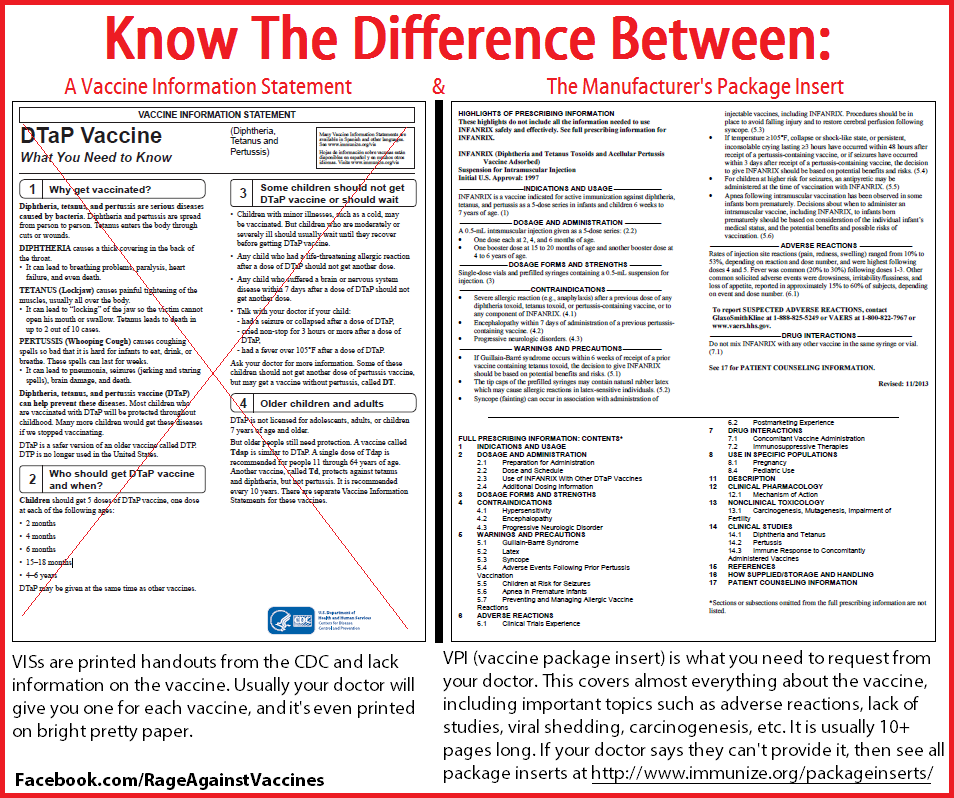 Some immunisations, such as whooping cough vaccine, give protection for about 5 years after a full course. Influenza immunisation is needed every year due to frequent changes to the type of flu virus in the community.
Some immunisations, such as whooping cough vaccine, give protection for about 5 years after a full course. Influenza immunisation is needed every year due to frequent changes to the type of flu virus in the community.
Is everyone protected from disease by immunisation?
Even when all the doses of a vaccine have been given, not everyone is protected against the disease. Measles, mumps, rubella, tetanus, polio, hepatitis B and haemophilus influenzae type b (Hib) vaccines protect more than 95% of children who have completed the course. One dose of meningococcal ACWY vaccine at 12 months protects over 90% of children.
Three doses of whooping cough vaccine protect about 85% of children who have been immunised, and will reduce the severity of the disease in the other 15% if they do catch whooping cough. Booster doses are needed because immunity decreases over time.
Some vaccinations, like for COVID-19, won’t necessarily prevent you from catching the disease, but can reduce the risk of serious illness.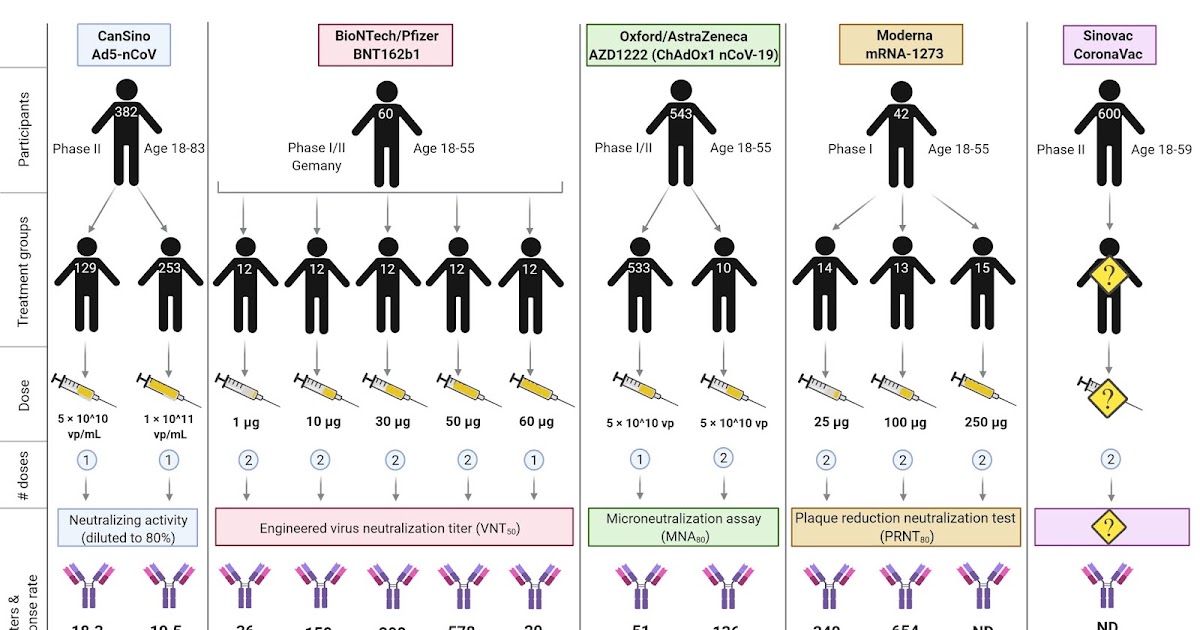
How are vaccines approved in Australia?
Before a vaccine becomes available in Australia, it must pass the rigorous approval processes of the Therapeutic Goods Administration (TGA). This includes assessing every ingredient in the vaccine for safety, quality and effectiveness.
A clinical trial is a scientific study conducted by the makers of a vaccine. Clinical trials of medicines are done in phases.
The TGA carefully assesses the results of clinical trials, as well as the way in which the trials were run. The TGA also checks that the trials involved enough human participants that represented the people for whom the vaccine is intended.
The TGA ensures that vaccine manufacturers meet manufacturing quality standards. TGA laboratories assess the quality of every batch of a vaccine before it can be supplied in Australia.
Sometimes a ‘provisional approval pathway’ is needed for the temporary registration of promising new medicines and vaccines — where the need for early access outweighs any risks.
Resources and support
In Australia, vaccines are funded by the National Immunisation Program and protect millions of Australians from vaccine-preventable diseases.
If you have any questions, you can speak to your doctor or call healthdirect on 1800 022 222 (known as NURSE-ON-CALL in Victoria).
Sources:
Department of Health (The Australian Immunisation Handbook), Raising Children Network (Immunisation in childhood), Raising Children Network (Immunisation FAQs), Department of Health (National Immunisation Program Schedule), Australian Government Department of Health (COVID-19 vaccines), NSW Health (Booster vaccination - frequently asked questions), Therapeutic Goods Administration (COVID-19 vaccine approval process)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Related pages
- Immunisation and vaccinations for your child
- Vaccinations and pregnancy
Need more information?
Immunisation | Tasmanian Department of Health
Learn about information about immunisation, vaccines and diseases preventable by immunisation in Tasmania.
Read more on Tasmanian Department of Health and Human Services website
Immunisation and vaccinations for your child
Immunisation is a simple, safe and effective way of protecting children against certain diseases. Discover more about childhood vaccinations.
Read more on Pregnancy, Birth & Baby website
Immunisation | SA Health
Information for consumers on vaccines, immunisation programs and immunisation records for you and your children
Read more on SA Health website
Immunisation records | NCIRS
Your immunisation history statement has all your vaccines that have been recorded on the Australian Immunisation Register (AIR)
Read more on National Centre for Immunisation Research and Surveillance (NCIRS) website
What is immunisation? | Australian Government Department of Health and Aged Care
On this page Immunisation or vaccination — what's the difference? Australia's National Immunisation Program Immunisation is a safe and effective way of protecting you and your child against serious diseases.
Read more on Department of Health and Aged Care website
Where can I get immunised? | Australian Government Department of Health and Aged Care
You can get vaccinations from a range of vaccination providers, including your local GP and school-based immunisation programs.
Read more on Department of Health and Aged Care website
Immunisation schedules | NCIRS
The Australian National Immunisation Program (NIP) is funded by the Australian government and implemented by state and territory departments of health
Read more on National Centre for Immunisation Research and Surveillance (NCIRS) website
Kids - Immunisation Coalition
Find out how to protect your kids from infectious diseases.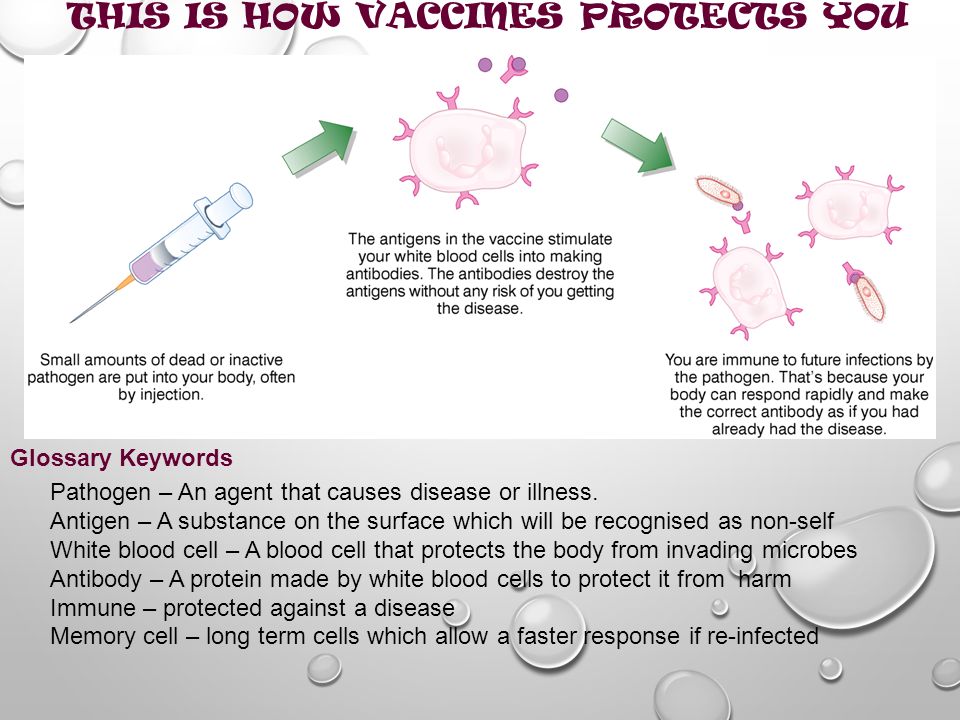 Keep up to date with the Childhood National Immunisation Program schedule.
Keep up to date with the Childhood National Immunisation Program schedule.
Read more on Immunisation Coalition website
Keeping your child’s vaccinations up to date during COVID-19
The COVID-19 pandemic has led to a decrease in children getting their routine childhood vaccinations.
Read more on Pregnancy, Birth & Baby website
Vaccination matters
Ensure your decisions about immunisation are based on fact. When doing your personal reading, make sure your source of information is based on scientific fact.
Read more on Queensland Health website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.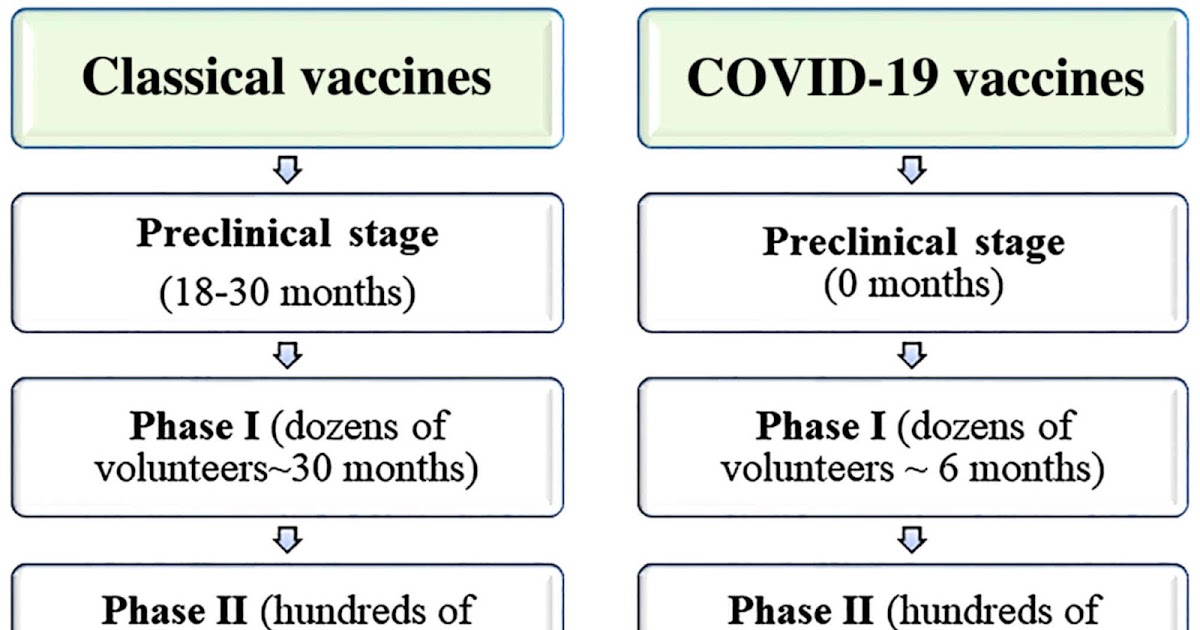
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.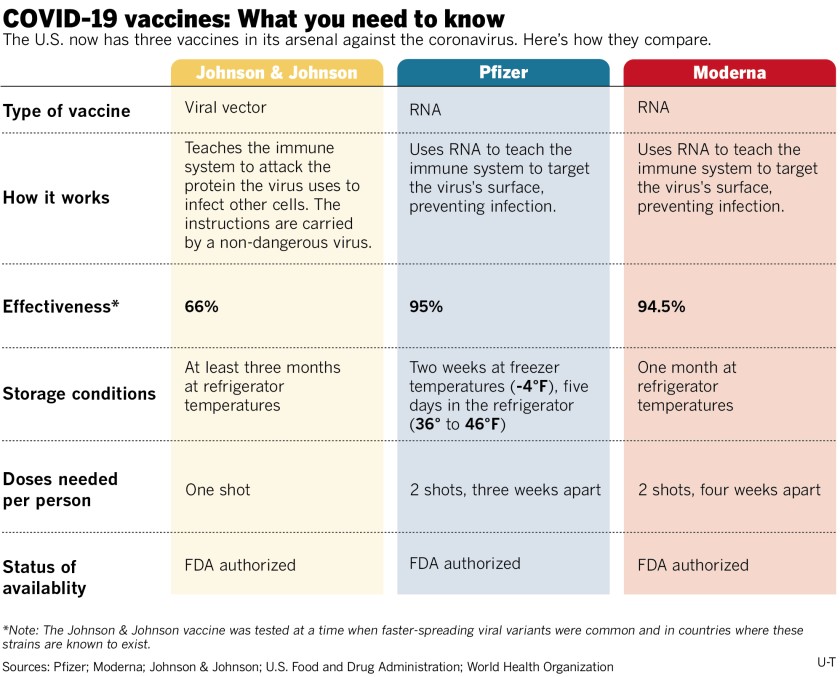
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Immunizations and vaccines: what is the difference
We work without days off and holidays
COVID 19 antibody tests
Let's get some terminology out of the way. At the household level, many do not feel the difference between serum, vaccine and vaccination, vaccination and immunization - we will try to explain to you the main terms used in vaccine prevention. This article does not claim to be fundamental - it is only a quick reference.
As a primary source of terms, we used queries that are most often typed in search engines on the topic of vaccination: in the search, people usually write in ordinary, conversational language.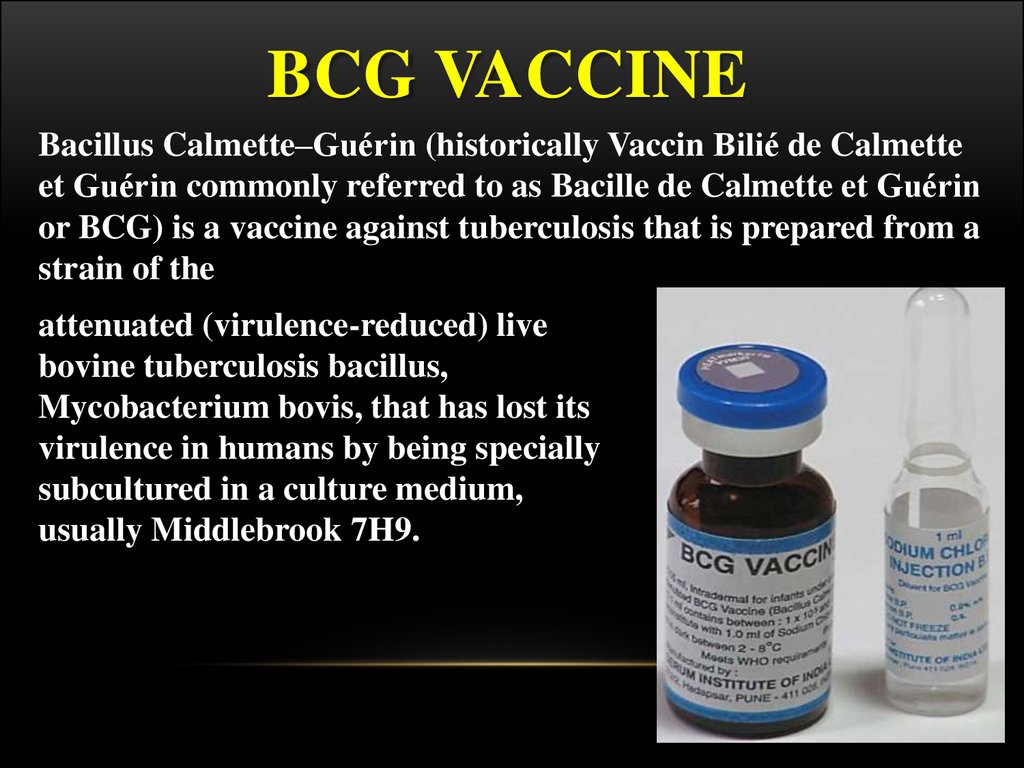 Here we will try to avoid complex medical terminology, because the article is written for people who are far from medicine.
Here we will try to avoid complex medical terminology, because the article is written for people who are far from medicine.
Vaccination is perhaps the main method of preventing many serious infectious diseases. The essence of the method is the artificial reproduction of the immune response of the human body, so that in the future the antibodies produced themselves fight the infection (it is also called active immunity).
Immunoprophylaxis is a broader concept than vaccination: it can be "specific" and "non-specific". The first means measures against a specific infection - this, in fact, is vaccination. The second implies a much wider range of ways to increase the immunity of the body as a whole, and not just creating a barrier for specific diseases: hardening, quality nutrition, proper rest and work, minimizing stress - in short, everything that helps the body stay healthy. In addition, immunoprophylaxis allows the creation of passive immunity by introducing ready-made antibodies in sera.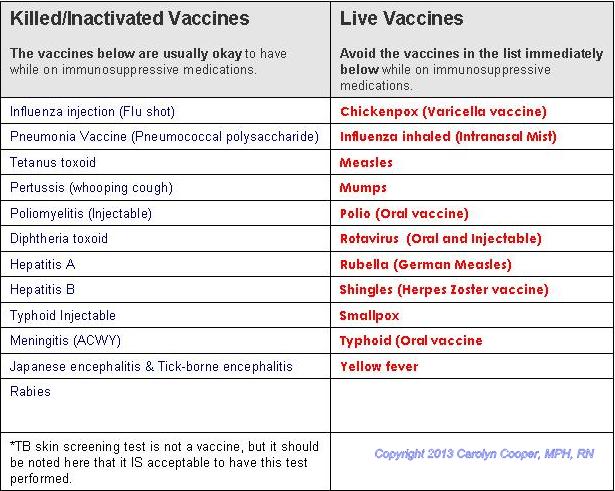
Vaccination is essentially the same as vaccination, the difference is purely semantic: the word "vaccination" is shorter and easier to pronounce, although the second term is more correct from the point of view of medical science.
Immunization is the same as immunization.
A vaccine is a medical product that is given to a person to develop active immunity to one or more specific diseases. Please note: we are talking about the "drug", and not about the procedure for using it. Sometimes vaccination is understood as the procedure for administering a vaccine, but we will use the word "vaccination" for this.
Serum and vaccine solve the same tasks - they contribute to the development of acquired immunity organisms. But there is also a fundamental difference between them: the vaccine contains weakened or dead agents of infection, and the serum contains ready-made antibodies against a specific disease. Serum is usually used to fight an already begun disease, that is, it is, in fact, a medicine, not a prophylactic.
Inoculation is the procedure for administering a preparation with antigenic material, ie a vaccine or serum. Once again: "vaccine" and "serum" are drugs, "vaccination" is the process of introducing them into the human body. We will adhere to such a division of concepts, but deviations are sometimes possible.
Revaccination is a way to support post-vaccination immunity through repeated vaccinations. Many vaccinations are valid for a limited period, after which the acquired immunity weakens. It is assumed that the primary vaccination has already been carried out, and, based on this, a revaccination schedule is drawn up.
Revaccination is the same as revaccination.
Re-vaccination - the procedure for introducing vaccinations during re-vaccination, that is, during revaccination.
Mandatory vaccination - a list of vaccinations that the state considers necessary: their set and timing are regulated by the National Immunization Schedule. Strictly speaking, there are no mandatory vaccinations in Russia, even children without them are admitted to kindergartens, but only if their parents have officially confirmed their refusal to be vaccinated.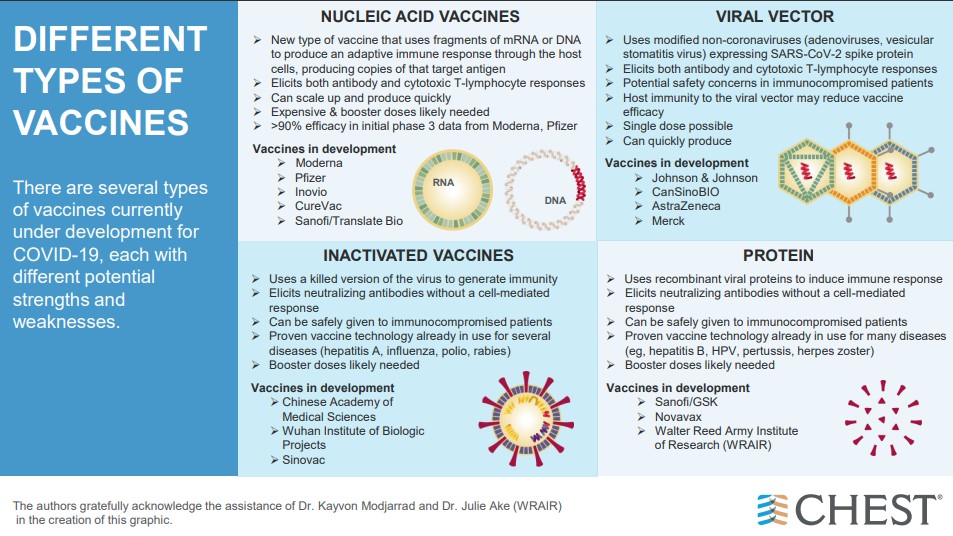
Immunization schedule - a list and schedule of vaccinations. Usually associated with the concept of mandatory vaccinations and the National Immunization Schedule, but can be used wherever it is required to describe the set and timing of vaccinations, for example, during revaccination.
The vaccination schedule is the same as the vaccination schedule.
Vaccination schedule - the same as the vaccination schedule.
Vaccination 2020 is a combination often found in search queries: people want to know which vaccinations are mandatory for the current year, and what changes have been made to the vaccination calendar.
Inoculation is the same as "inoculation". This is usually written in search queries by those who do not know the difference between a vaccine and an inoculation.
To be vaccinated or vaccinated - "to vaccinate" is a more medical term, an example of professional slang. In everyday life, the word "do" or "do" is usually used. In most cases, we will use the everyday option, but in some more "medical" articles, professional terms are not excluded.
Vaccination schedule - commonly used as a synonym for vaccination schedule.
Deciphering vaccinations - unlike analyzes, where deciphering is understood as the interpretation of their results, in vaccination it is deciphering the abbreviations of vaccines, for example, DTP.
Vaccination room - a place (room) where preventive and diagnostic vaccinations are given. Not to be confused with a treatment room, where other procedures, such as IVs, may be performed.
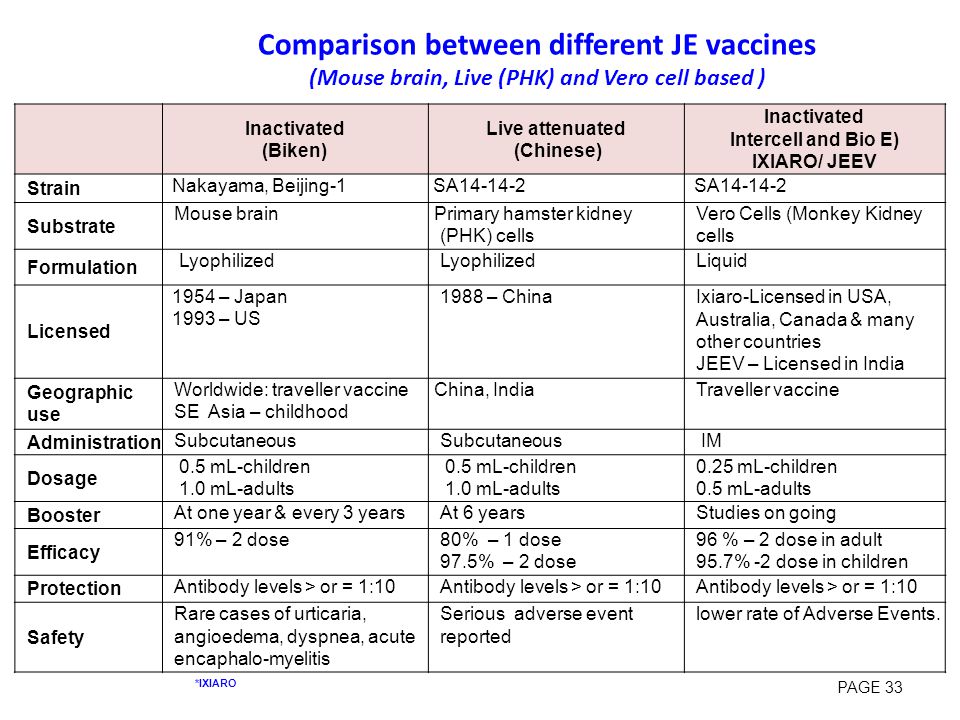
Live vaccines are one of the types of vaccines that contain weakened or killed infectious agents in the preparation. The classification of vaccines divides them into live, chemical, synthetic, inactivated (there is no single classification), but "live vaccines" are the most famous of them.
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- 9000
- О
- П
- Р
- С
- Т
- У
- Ф
- Х
- Ц
- Ч
- Ш
- Щ
- Ъ
- Ы
- Ь
- Э
- Yu
- I
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Latest information
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Questions and answers /
- Questions and answers /
- Vaccines and immunization: What is vaccination?
August 30, 2021 | FAQ
Revised August 10, 2021
What is vaccination?
Vaccination is a simple, safe and effective way to protect against diseases before a person comes into contact with their pathogens.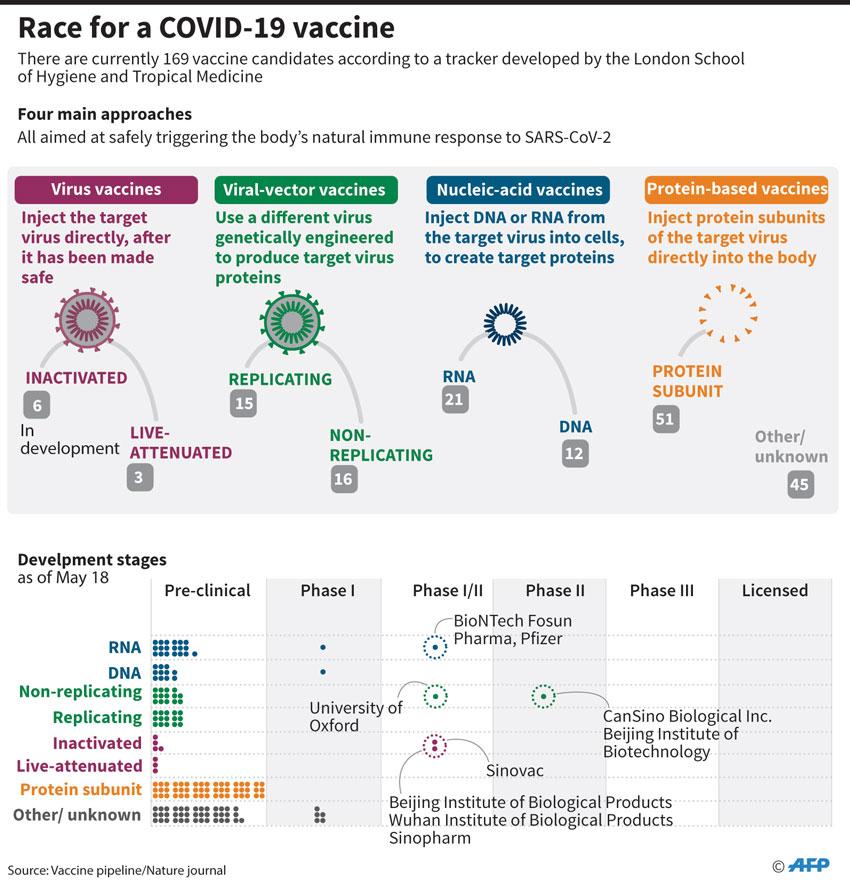 Vaccination activates the body's natural defense mechanisms to build resistance to a range of infectious diseases and makes your immune system stronger.
Vaccination activates the body's natural defense mechanisms to build resistance to a range of infectious diseases and makes your immune system stronger.
Like diseases, vaccines train the immune system to produce specific antibodies. However, vaccines contain only killed or attenuated forms of the causative agents of a particular disease - viruses or bacteria - that do not lead to the disease and do not create the risk of complications associated with it.
Most vaccines are administered by injection, although oral administration is also available. vaccines (given by mouth), and nasal spray vaccines (given through the nose).
What is the principle of the vaccine?
Vaccines reduce the risk of disease by activating natural defense mechanisms to build immunity to the pathogen. Vaccination provokes the body's immune response. Immune system:
- Recognizes pathogens such as viruses or bacteria.
- Starts production of antibodies. Antibodies are proteins naturally produced by the body's immune system to fight disease.
- Remembers the causative agent of the disease in order to deal with it in the future. If this pathogen enters the body again, the immune system will quickly destroy it, preventing the development of the disease.
Thus, vaccination is a safe and rational way to induce an immune response in the body without the need to infect it with a particular disease.
Our immune system has a memory. By receiving one or more doses of a vaccine, we are usually protected against a particular disease for many years, decades, or even a lifetime. This is what makes vaccines so effective. Vaccines keep us from getting sick, which is much better than having to treat the disease when it has already begun.
When should I get vaccinated (or have my child vaccinated)?
Vaccines protect us throughout our lives and at all ages - from birth, through childhood, through adolescence and into old age. In most countries, people are given vaccination cards that show which vaccinations an adult or child has received and when the next vaccinations are due.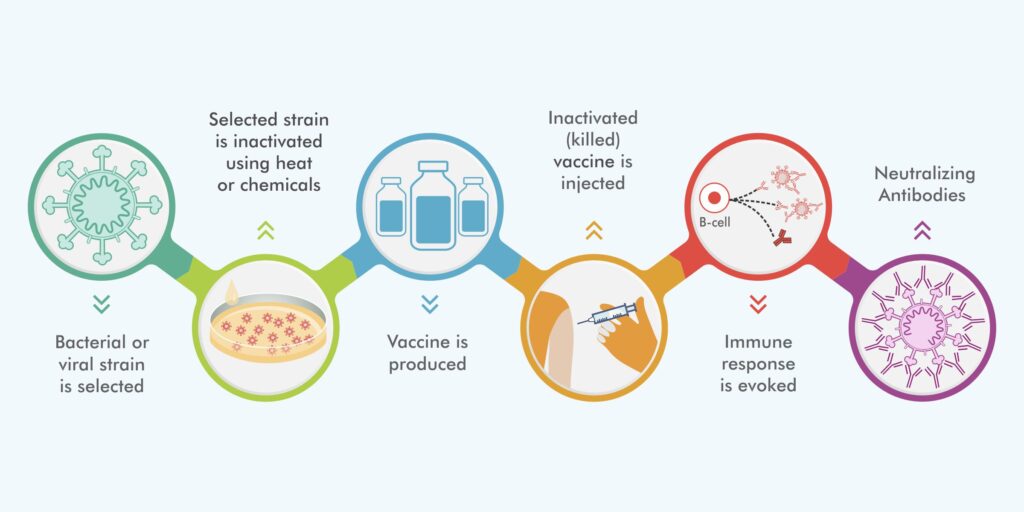 It is important that all indicated vaccinations are up to date.
It is important that all indicated vaccinations are up to date.
By delaying vaccination, we put ourselves at risk of becoming seriously ill. If we wait until the moment when a vaccine is urgently needed - for example, if an outbreak of a disease has begun - then it may be too late to get the desired effect of vaccination or all the necessary doses of the vaccine.
Why do I need to be vaccinated?
Without vaccination, we are at risk of serious diseases such as measles, meningitis, pneumonia, tetanus and polio. Many of these diseases are life threatening. The WHO estimates that childhood vaccines alone save more than 4 million lives each year.
Although some diseases are becoming less common, their pathogens continue to circulate in some or all regions of the world. In today's world, infectious diseases can easily cross borders and infect anyone who lacks immunity to them.
There are two main reasons to get vaccinated: to protect yourself and to protect others. Since some people, such as newborns and people with serious illnesses or those with certain allergies, may not be vaccinated, their protection against vaccine-preventable diseases depends on the availability of vaccinations in others.
Since some people, such as newborns and people with serious illnesses or those with certain allergies, may not be vaccinated, their protection against vaccine-preventable diseases depends on the availability of vaccinations in others.
Who should not be vaccinated?
Almost anyone can get vaccinated. However, for people with certain diseases and conditions, some vaccinations are contraindicated or should be deferred to a later date. These diseases and conditions may include:
- chronic diseases or treatments (eg chemotherapy) that suppress the immune system;
- Extremely rare acute and life-threatening allergic reactions to vaccine components;
- severe illness at the time of vaccination. However, these children should be vaccinated as soon as they recover. Moderate malaise or subfebrile temperature is not a contraindication for vaccination.
Often these factors need to be taken into account depending on the type of vaccine. If you are not sure whether you or your child should get a particular vaccine, ask your doctor.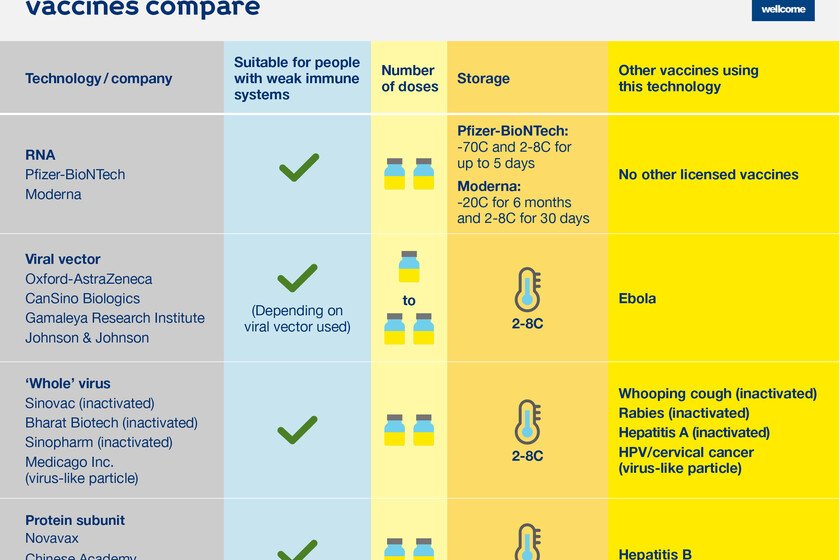 Your doctor will help you make an informed decision about your or your child's vaccinations.
Your doctor will help you make an informed decision about your or your child's vaccinations.
A number of vaccines for some other diseases, including Ebola or malaria, are currently under development or experimental use, but these vaccines have not yet been introduced in mass use throughout the world.
Not all vaccinations may be required in your country. Vaccinations against certain diseases may only be required for people who travel to certain countries or who are at increased risk due to their professional activities. Ask your doctor what vaccinations you and your family members need.
Why are vaccinations started at such an early age?
In their daily lives, young children may find themselves in many different places and come into contact with a wide variety of people, thereby exposing them to a serious risk of infection. The WHO-recommended immunization schedule allows infants and young children to be protected as early as possible against a range of diseases. Often, infants and young children are most at risk of illness because their immune systems are not yet fully developed and their bodies are less able to fight off infections. Therefore, it is extremely important to vaccinate children according to the recommended schedule.
Often, infants and young children are most at risk of illness because their immune systems are not yet fully developed and their bodies are less able to fight off infections. Therefore, it is extremely important to vaccinate children according to the recommended schedule.
What is included in the vaccine?
All components of a vaccine play an important role in its safety and efficacy. The composition of vaccines, in particular, includes the following components:
- Antigen. This is a killed or weakened form of any microorganism - a virus or a bacterium - on which our body learns to recognize and destroy the causative agent of the disease if it encounters it in the future.
- Adjuvants that help enhance the body's immune response. Without them, vaccines would be less effective.
- Preservatives to keep vaccines effective.
- Stabilizers to preserve the vaccine during storage and transport.
The names of vaccine components written on vaccine packages can be confusing. However, many of them are naturally present in the body, environment and food. All of the components of vaccines, like the vaccines themselves, are subject to rigorous testing and monitoring for their safety.
However, many of them are naturally present in the body, environment and food. All of the components of vaccines, like the vaccines themselves, are subject to rigorous testing and monitoring for their safety.
Are vaccines safe?
Vaccination is safe and usually causes minor and temporary side effects, such as arm pain or mild fever. More serious side effects are possible, but they are extremely rare.
Any licensed vaccine is rigorously tested through several phases of clinical trials before it is approved for use and regularly evaluated after introduction. Scientists are also constantly monitoring information from a range of sources for signs that a given vaccine may pose a health risk.
It must be remembered that the risk of serious harm to health from a vaccine-preventable disease is much greater than the risk associated with vaccination. For example, tetanus can cause severe pain, convulsions and thrombosis, and measles can lead to encephalitis (infection of the brain) and blindness. Many vaccine-preventable diseases can even be fatal. The benefits of vaccination far outweigh the risks, and without vaccines, the world would experience an order of magnitude more illness and death.
Many vaccine-preventable diseases can even be fatal. The benefits of vaccination far outweigh the risks, and without vaccines, the world would experience an order of magnitude more illness and death.
My child did not receive the recommended vaccinations on time. Is it too late to get the missing vaccinations?
In most cases, it is never too late to get the missing shots. Ask your doctor how and when you or your child can get the missing shots.
Do vaccines have side effects?
Like all medicines, vaccines can cause mild side effects such as low grade fever and pain or redness at the injection site. These symptoms usually go away on their own within a few days.
Severe or long-term side effects are extremely rare. The chance of experiencing a serious adverse body reaction to a vaccine is 1 in a million.
The safety of vaccines is subject to ongoing monitoring and is continuously monitored for rare adverse reactions.
How are vaccines developed and tested?
The most commonly used vaccines have been in use for decades, and every year millions of people receive them safely. Like all medicines, every vaccine must undergo extensive, rigorous testing to assess its safety before it can be introduced in countries.
Like all medicines, every vaccine must undergo extensive, rigorous testing to assess its safety before it can be introduced in countries.
Experimental vaccines are first tested in animals to evaluate their safety and ability to prevent disease. They are then tested in human clinical trials, which consist of three phases.
• During the first phase of the trial, the vaccine is given to a small number of volunteers to evaluate its safety, make sure it generates an immune response, and determine the correct dose.
• During the second phase of the trial, the vaccine is typically administered to hundreds of volunteers, who are closely monitored for any side effects and further evaluation of its ability to generate an immune response. Data on disease outcomes are also collected at this stage whenever possible, but these data are usually not sufficient to provide a clear picture of the impact of the vaccine on the disease. Participants in this phase of the trial share the same characteristics (such as age and gender) as the people for whom the vaccine is intended.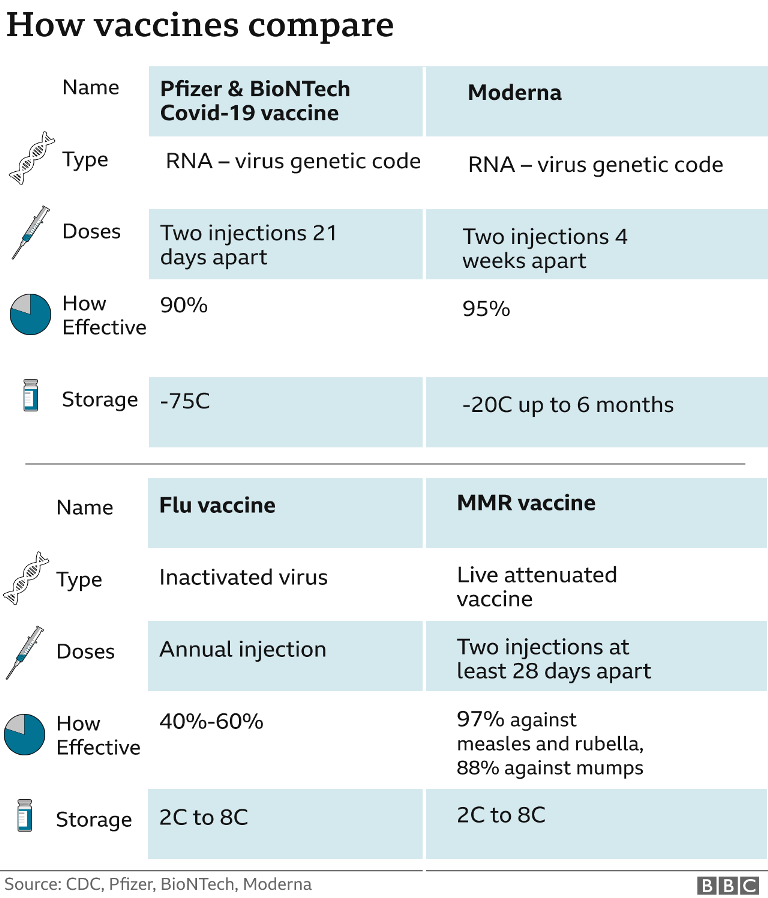 At this stage, some volunteers receive the vaccine and others do not, allowing comparisons to be made and conclusions about the vaccine to be made.
At this stage, some volunteers receive the vaccine and others do not, allowing comparisons to be made and conclusions about the vaccine to be made.
• During the third phase of the trial, the vaccine is administered to thousands of volunteers, some receiving the study vaccine and some not, as in the second phase of the trial. The data from both groups are carefully compared to determine whether the vaccine is safe and effective in protecting against the disease it is intended to target.
Following clinical trial results, a number of steps must be taken before a vaccine can be included in a national immunization program, including efficacy, safety, and manufacturing reviews for regulatory approval and public health policy approval.
Following the introduction of the vaccine, careful monitoring continues to be carried out to identify any unexpected unwanted side effects and to further evaluate its effectiveness in the context of regular use in even more people, which will allow understanding how to best use the vaccine to ensure the greatest protective effect. For more information on vaccine development and safety, click here.
For more information on vaccine development and safety, click here.
Can a child have more than one vaccine at a time?
Scientific evidence shows that the simultaneous administration of several vaccines does not have negative consequences. Every day, children are exposed to several hundred foreign substances that trigger the body's immune response. A simple meal is accompanied by the entry of new microorganisms into the body, and many bacteria live in the nose and mouth.
The ability to combine multiple vaccines (such as diphtheria, whooping cough and tetanus) reduces the number of injections and reduces discomfort for the child. In addition, it allows you to know for sure that the child received the right vaccinations at the right time and will not catch a potentially fatal disease.
Is there a link between vaccination and autism?
There is no evidence of any association between vaccination and autism spectrum disorders. This conclusion was drawn from the results of many studies conducted on very large groups of people.
In 1998, a study was published raising concerns about a possible link between the measles, mumps, and rubella (MMR) vaccine and autism, but the study later found a number of serious misrepresentations and falsified information. The journal that published this work later withdrew it, and the doctor who wrote it lost his license to practice medicine. Unfortunately, due to fears caused by this publication, vaccination rates in some countries dropped sharply, which subsequently led to outbreaks of these diseases.
We all have a responsibility to take the necessary steps to disseminate only reliable, evidence-based information about vaccines and the diseases that vaccines help prevent.
Does my daughter need to be vaccinated against the human papillomavirus (HPV)?
Almost all cases of cervical cancer are caused by sexually transmitted HPV infection. Vaccination against HPV before a person comes into contact with this virus is the most effective means of protection against this disease. Studies in Australia, Belgium, Sweden, Germany, New Zealand, the United Kingdom, the United States of America and Sweden showed that vaccination reduced the number of HPV infections among adolescent girls and young women to almost 90%.
Studies in Australia, Belgium, Sweden, Germany, New Zealand, the United Kingdom, the United States of America and Sweden showed that vaccination reduced the number of HPV infections among adolescent girls and young women to almost 90%.
Studies have proven the safety and efficacy of the HPV vaccine. WHO recommends that all girls aged 9–14 years be vaccinated with two doses of the HPV vaccine, and that women be periodically screened for cervical cancer later in life.
I have questions about vaccinations. Who should I contact?
If you have any questions about vaccinations, be sure to ask your doctor. He or she will be able to give you evidence-based information about vaccinations, including the recommended vaccination schedule in your country for you and your family members.
When looking for information about vaccines on the Internet, look only to trusted sources. To help you find these sources, WHO has reviewed and "certified" many websites in many languages around the world to contain only information based on sound scientific evidence and independent analysis by leading technical experts.