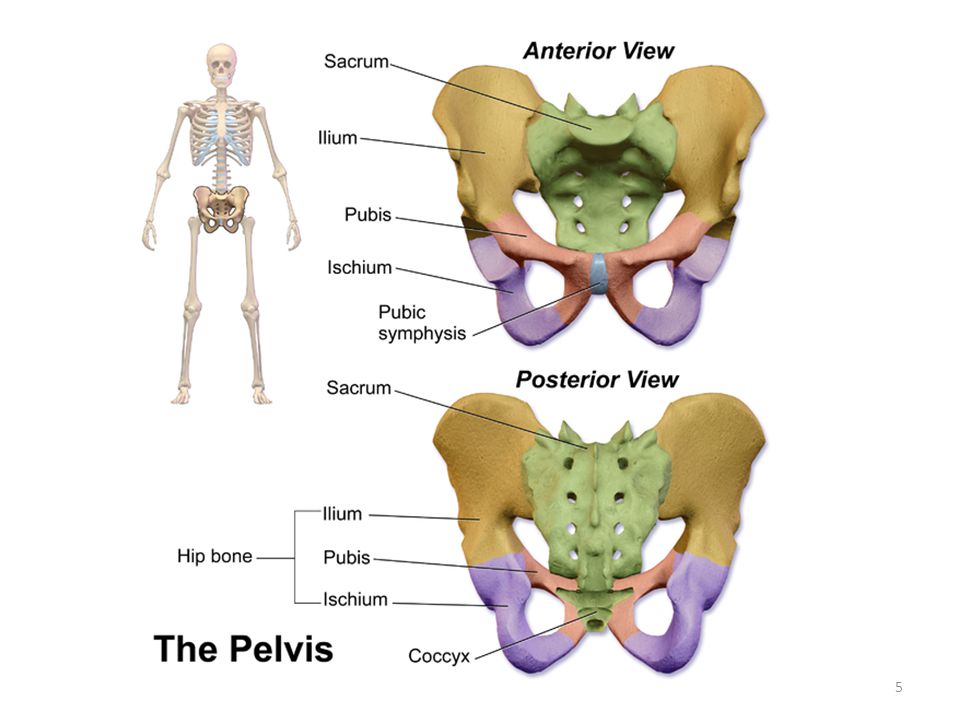
How many bones are in the pelvic girdle
3D Skeletal System: The Pelvic Girdle
Posted on 1/25/13 by Courtney Smith
I must put my hand on my hip at least a thousand times a day. I don't know what it is—it's a habit that I can't seem to break. Mostly, I think it's because I never quite know what to do with my hands if I'm just standing. But there's something to be said for resting your hand on something sturdy—even when the sturdy thing is you!
The pelvic girdle may look like one giant bone, but it's actually made of three. The pelvic girdle connects the bones of the lower limbs to the axial skeleton by different attachment sites, and supports the vertebral column.
The hip bones are a major component of the pelvic girdle. Check out our free eBook to learn more!
And I'm going to be honest: I find the pelvic girdle to be one of the most beautiful structures in the entire body. I mean, look at it!
Check out more Anatomy & Physiology videos on our YouTube page.
Okay, let's take a look at the pelvic girdle, its relationship with the femur, and its responsibilities in the body.
Bones of the Pelvic Girdle
When we're born, we have over 300 bones. As we grow, some bones fuse together, leaving us with 206 by the time we're adults. The pelvic girdle, as I said above, is made up of three fused bones: the ischium, the ilium, and the pubis.
The pubis forms the anterior part of the pelvic girdle. It is a flattened, irregular-shaped bone that articulates with the pubic symphysis, a cartilaginous joint.
Image captured from Human Anatomy Atlas.
| Did you know? The pelvic girdle is part of the appendicular skeleton, which also includes the shoulder girdle and the upper and lower limbs. |
The ilium is the largest and most recognizable part of the pelvis: it looks like the top of a wing. If your hip bones "stick out" (are visible through your skin), it's usually the ilium you're seeing; they protrude outwards.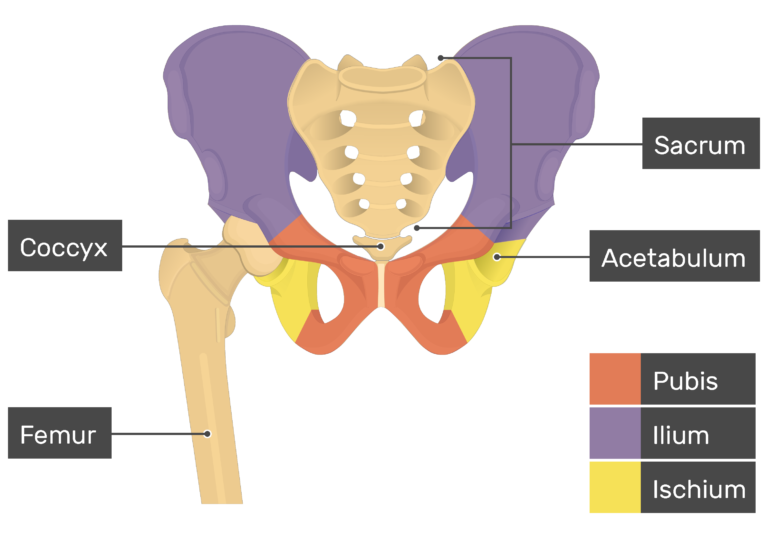 The ilium articulates with the sacrum, forming the posterior wall of the pelvic cavity. The iliac crest, the superior-most area of bone, is the attachment site for several muscles, including the latissimus dorsi and gluteus maximus.
The ilium articulates with the sacrum, forming the posterior wall of the pelvic cavity. The iliac crest, the superior-most area of bone, is the attachment site for several muscles, including the latissimus dorsi and gluteus maximus.
Image captured from Human Anatomy Atlas.
The ischium, located directly below the pubis, forms the bottom of the "wing." Together with the pubis, the ischium forms the obturator canal, the large hole in the bone. The obturator canal is the attachment site for the obturator muscles, as well as nerves and blood vessels.
Image captured from Human Anatomy Atlas.
Acetabulum and the Pelvic Girdle
The femur and the pelvic girdle have a very special relationship—it's special in that it allows you to walk. Take a look at the femur (see image). The helmet-like structure highlighted in teal is the head. Many bones have a head. What's special about this particular head is its role as the ball in the ball-and-socket hip joint.
Image captured from Human Anatomy Atlas.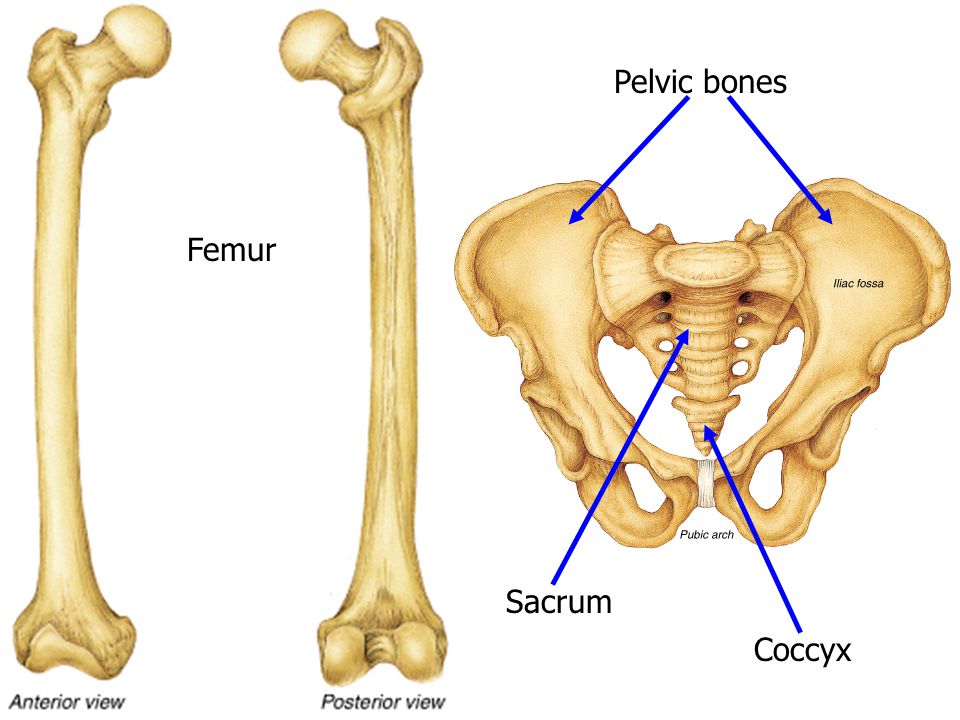
The pubis, ischium, and ilium have a hand in creating the acetabulum, the deep, hemispherical, cup-shaped depression (the socket) with which the head of the femur articulates. The head of the femur fits perfectly in this cavity; its ball shape allows it to roll the femur, rotating it in a way that facilitates walking. Ligaments hold the bones together.
Image captured from Human Anatomy Atlas.
Male and Female Pelvic Girdle
In addition to supporting the vertebral column and allowing you to walk, the pelvic girdle—along with the sacrum and the coccyx—forms the walls of the pelvic cavity, which contains and protects some of the reproductive, digestive, and urinary organs.
The pelvic girdle is delicate and shallower in the female pelvis than the male—the ilia are less sloped, and the superior aperture is more circular.
Be sure to subscribe to the Visible Body Blog for more anatomy awesomeness!
Are you an instructor? We have award-winning 3D products and resources for your anatomy and physiology course! Learn more here.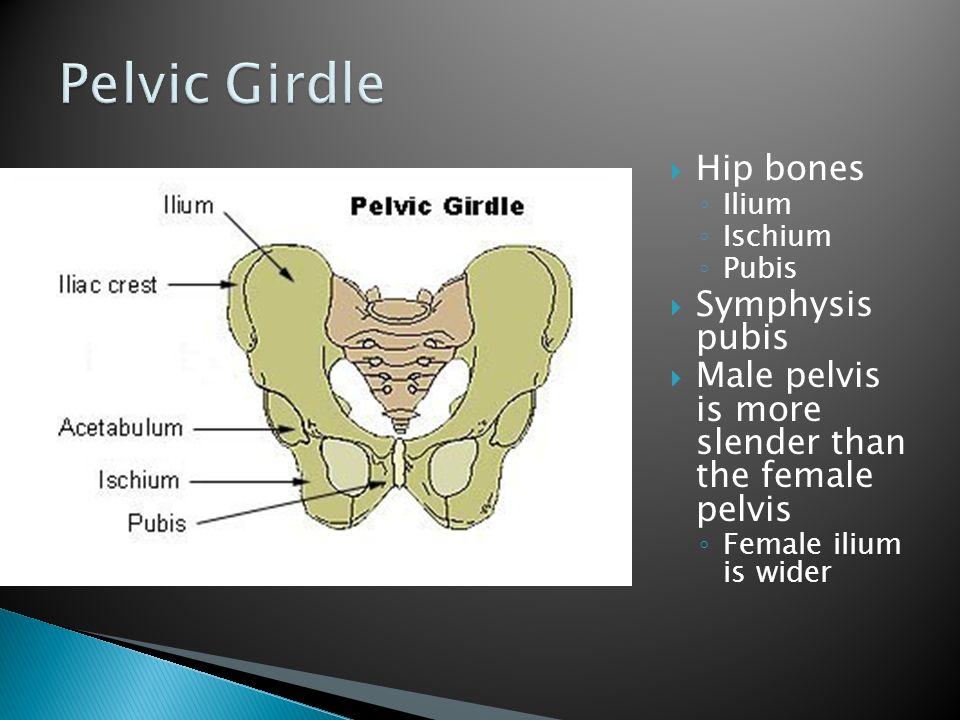
Related Posts:
- 3D Skeletal System: Five Cool Facts about the Femur
- 3D Skeletal System: Function of the Sphenoid
- 3D Skeletal System: The Atlas, Axis, and Atlanto-Axial Relationship
Additional Sources:
-Gray's Anatomy
The Pelvic Girdle - Structure - Function - Assessment
- 1 Structure of the Pelvic Girdle
- 2 Functions of the Pelvis
- 3 The Greater and Lesser Pelvis
- 3.1 Pelvic Inlet
- 3.2 Pelvic Outlet
- 4 Adaptation for Childbirth
- 5 Clinical Relevance: Assessment of the Female Bony Pelvis
- 5.1 Obstetric Conjugate
- 5.2 Diagonal Conjugate
The pelvic girdle is a ring-like bony structure, located in the lower part of the trunk. It connects the axial skeleton to the lower limbs.
In this article, we shall look at the anatomy of the pelvic girdle – its bony landmarks, functions, and its clinical relevance.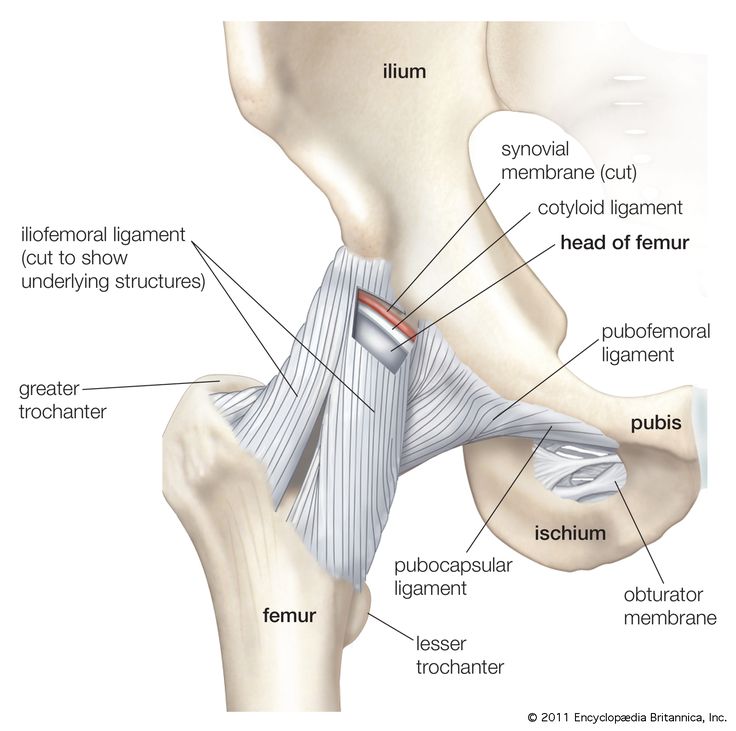
The bony pelvis consists of the two hip bones (also known as innominate or pelvic bones), the sacrum and the coccyx.
There are four articulations within the pelvis:
- Sacroiliac joints (x2) – between the ilium of the hip bones, and the sacrum
- Sacrococcygeal symphysis – between the sacrum and the coccyx.
- Pubic symphysis – between the pubis bodies of the two hip bones.
Ligaments attach the lateral border of the sacrum to various bony landmarks on the bony pelvis to aid stability.
By TeachMeSeries Ltd (2022)
Fig 1 – The pelvic girdle is formed by the hip bones, sacrum and coccyx.
Functions of the PelvisThe strong and rigid pelvis is adapted to serve a number of roles in the human body. The main functions being:
- Transfer of weight from the upper axial skeleton to the lower appendicular components of the skeleton, especially during movement.
- Provides attachment for a number of muscles and ligaments used in locomotion.
- Contains and protects the abdominopelvic and pelvic viscera.
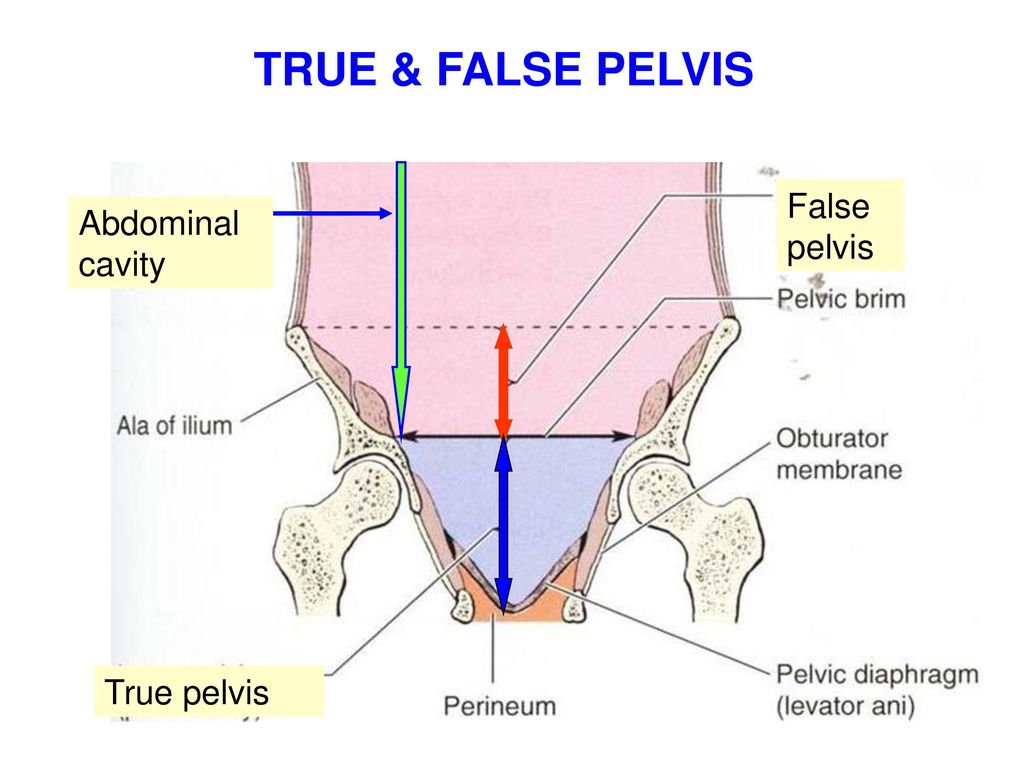
The osteology of the pelvic girdle allows the pelvic region to be divided into two:
- Greater pelvis (false pelvis) – located superiorly, it provides support of the lower abdominal viscera (such as the ileum and sigmoid colon). It has little obstetric relevance.
- Lesser pelvis (true pelvis) – located inferiorly. Within the lesser pelvis reside the pelvic cavity and pelvic viscera.
The junction between the greater and lesser pelvis is known as the pelvic inlet. The outer bony edges of the pelvic inlet are called the pelvic brim.
By TeachMeSeries Ltd (2022)
Fig 2 – The greater and lesser pelvis. The lesser pelvis is the ‘true’ pelvis and contains the pelvic cavity.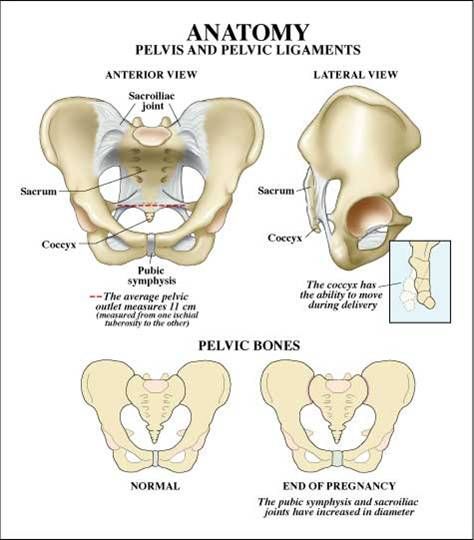
The pelvic inlet marks the boundary between the greater pelvis and lesser pelvis. Its size is defined by its edge, the pelvic brim.
The borders of the pelvic inlet:
- Posterior – sacral promontory (the superior portion of the sacrum) and sacral wings (ala).
- Lateral – arcuate line on the inner surface of the ilium, and the pectineal line on the superior pubic ramus.
- Anterior – pubic symphysis.
The pelvic inlet determines the size and shape of the birth canal, with the prominent ridges a key site for attachment of muscle and ligaments.
Some alternative descriptive terminology can be used in describing the pelvic inlet:
- Linea terminalis – the combined pectineal line, arcuate line and sacral promontory.
- Iliopectineal line – the combined arcuate and pectineal lines. This represents the lateral border of the pelvic inlet.

By TeachMeSeries Ltd (2022)
Fig 3 – Looking down onto the pelvis, the borders of the pelvic brim.
Pelvic OutletThe pelvic outlet is located at the end of the lesser pelvis, and the beginning of the pelvic wall.
Its borders are:
- Posterior: The tip of the coccyx
- Lateral: The ischial tuberosities and the inferior margin of the sacrotuberous ligament
- Anterior: The pubic arch (the inferior border of the ischiopubic rami).
The angle beneath the pubic arch is known as the sub-pubic angle and is of a greater size in women.
By TeachMeSeries Ltd (2022)
Fig 4 – The borders of the pelvic outlet.
Adaptation for ChildbirthThe majority of women have a gynaecoid pelvis, as opposed to the male android pelvis. The slight differences in their structures creates a greater pelvic outlet, adapted to aid the process of childbirth.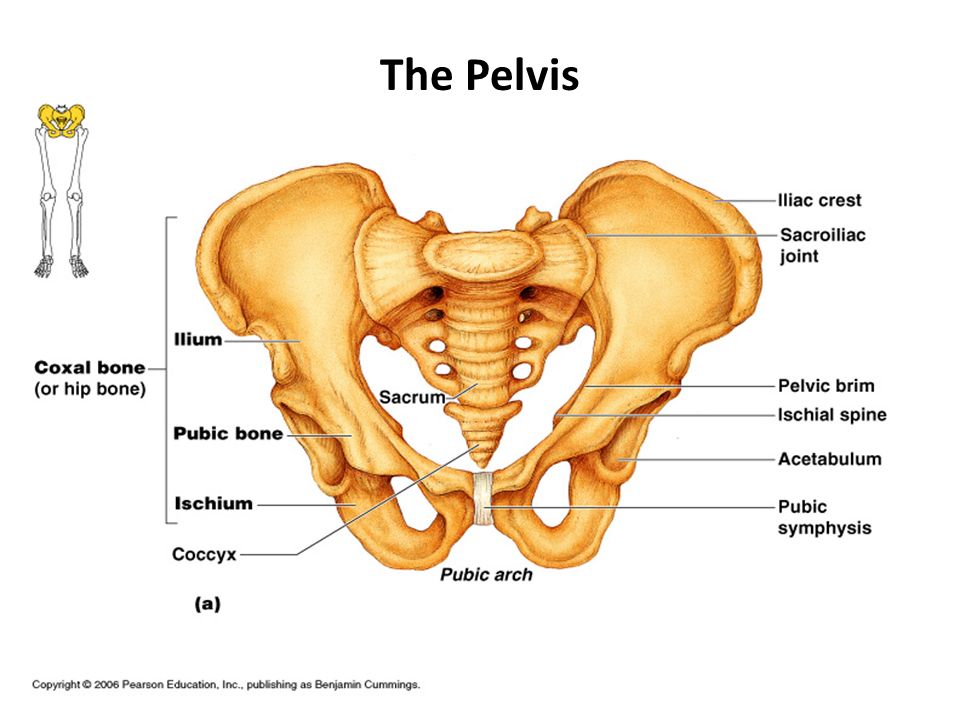 When comparing the two, the gynaecoid pelvis has:
When comparing the two, the gynaecoid pelvis has:
- A wider and broader structure yet it is lighter in weight
- An oval-shaped inlet compared with the heart-shaped android pelvis.
- Less prominent ischial spines, allowing for a greater bispinous diameter
- A greater angled sub-pubic arch, more than 80-90 degrees.
- A sacrum which is shorter, more curved and with a less pronounced sacral promontory.
In addition to the bony adaptations, the sacrotuberous and sacrospinous ligaments can stretch under the influence of progesterone and increase the size of the outlet further.
By TeachMeSeries Ltd (2022)
Fig 5 – Gynaecoid pelvis vs the android pelvis.
Clinical Relevance: Assessment of the Female Bony Pelvis
The lesser pelvis is the bony canal through which the fetus has to pass during childbirth.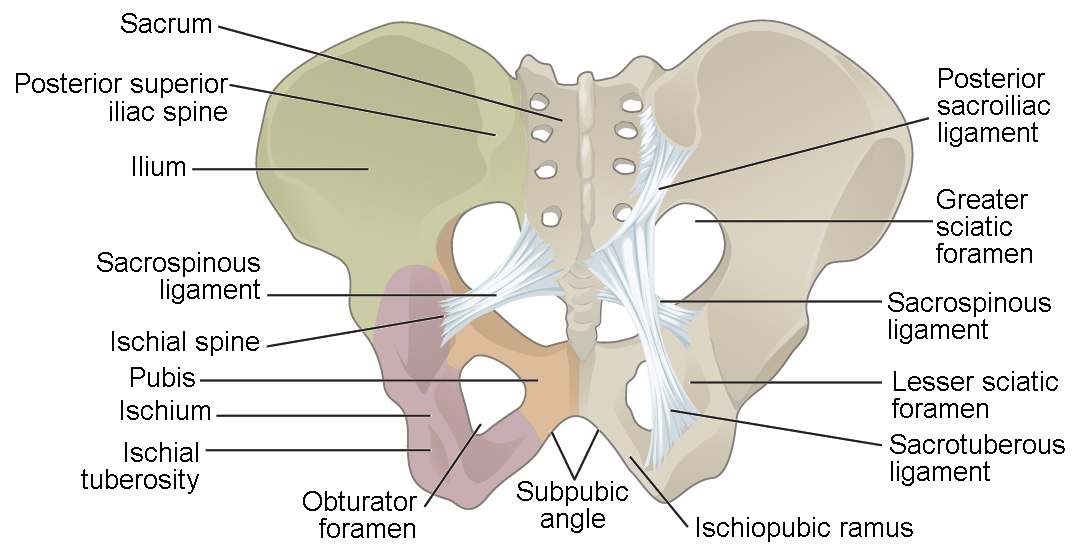 It is therefore of great importance to determine the diameter of this canal and therefore the childbearing capacity of the mother.
It is therefore of great importance to determine the diameter of this canal and therefore the childbearing capacity of the mother.
The diameter can be determined by a pelvic examination or radiographically. There are two measurements that are of importance:
Obstetric ConjugateIn order to determine the narrowest fixed distance that the fetus would have to negotiate, the minimum antero-posterior diameter of the pelvic inlet is measured.
This distance is between the sacral promontory and the midpoint of the pubic symphysis (where the pubic bone is thickest) and is known as the obstetric conjugate (or true conjugate). However, this measurement cannot be assessed clinically, due to the presence of the bladder.
Diagonal Conjugate
The diagonal conjugate is the alternative, measuring from the inferior border of the pubic symphysis to the sacral promontory and can be measured manually via the vagina.
(To do this you use the tip of your middle finger to measure the sacral promontory and then using the other hand to mark the level of the inferior margin of the pubic symphysis on the examining hand. You then use the distance between the index finger and the pubic symphysis to measure the diagonal conjugate, ideally 11cm or greater)
In addition to measuring the diagonal conjugate, a mid-pelvis check is carried out. Here, the clinician is testing for straight side walls and measuring the bispinous diameter which is narrowest part of the pelvic canal. The width of the subpubic angle at the pelvic outlet can be determined by the distance between the ischial tuberosities.
By TeachMeSeries Ltd (2022)
Fig 6 – Assessment of the female pelvis, via the diagonal conjugate
printPrint this Article
Encyclopedia - Pelvic girdle
The pelvic girdle bears the weight of the entire upper body, and the lower limbs rest against it. This part of the body experiences a lot of pressure from both sides - from below and from above, it promotes the movements of the lower limbs and protects important internal organs.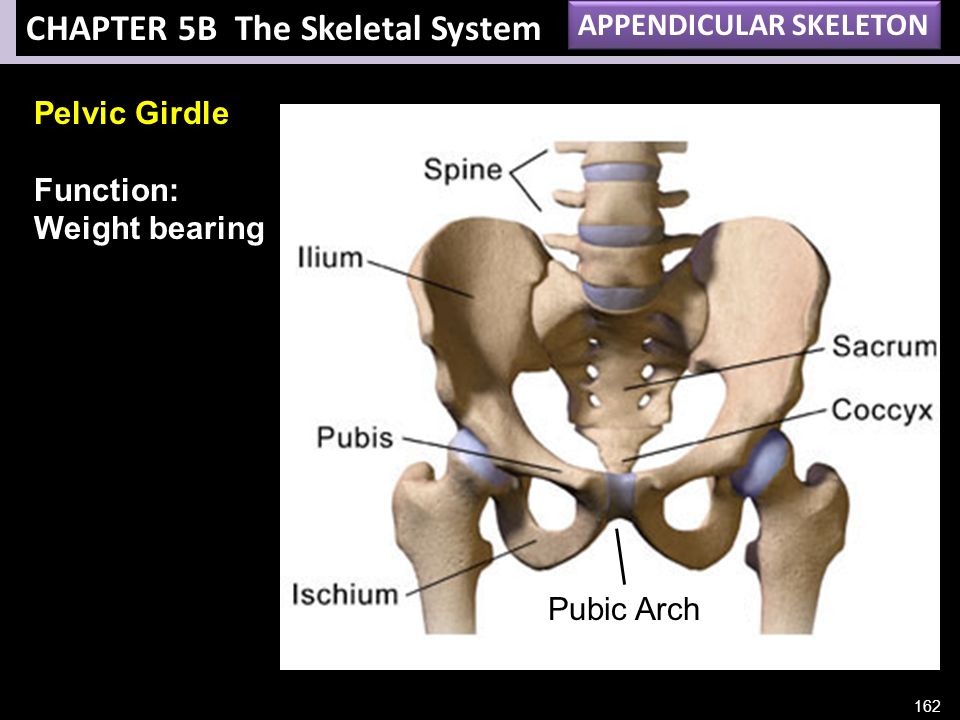 The most important function of the pelvis is locomotor, contributing to the movement of the body in space.
The most important function of the pelvis is locomotor, contributing to the movement of the body in space.
Differences between the human pelvis and the pelvis of other mammals are related
with an upright body position. Only in humans transverse dimensions
the pelvis is more straight (anterior-posterior). Even the pelvis of the great apes
already more elongated. In the human fetus, the pelvis has the same shape,
as the pelvis of four-legged mammals. Pelvis transformations begin
under the influence of mechanical loads: gravity of the body, pressure in the hip
joint during movements, etc. Active formation of sex differences
in the structure of the pelvis occurs during puberty under the action of
hormones. Characteristically, with reduced ovarian function (female
gonads) slows down the formation of female
features - the pelvis remains relatively narrow.
Pelvic bones
The pelvic girdle, or pelvis, is a strong bone ring that is located in the lower part of the skeleton of the human torso.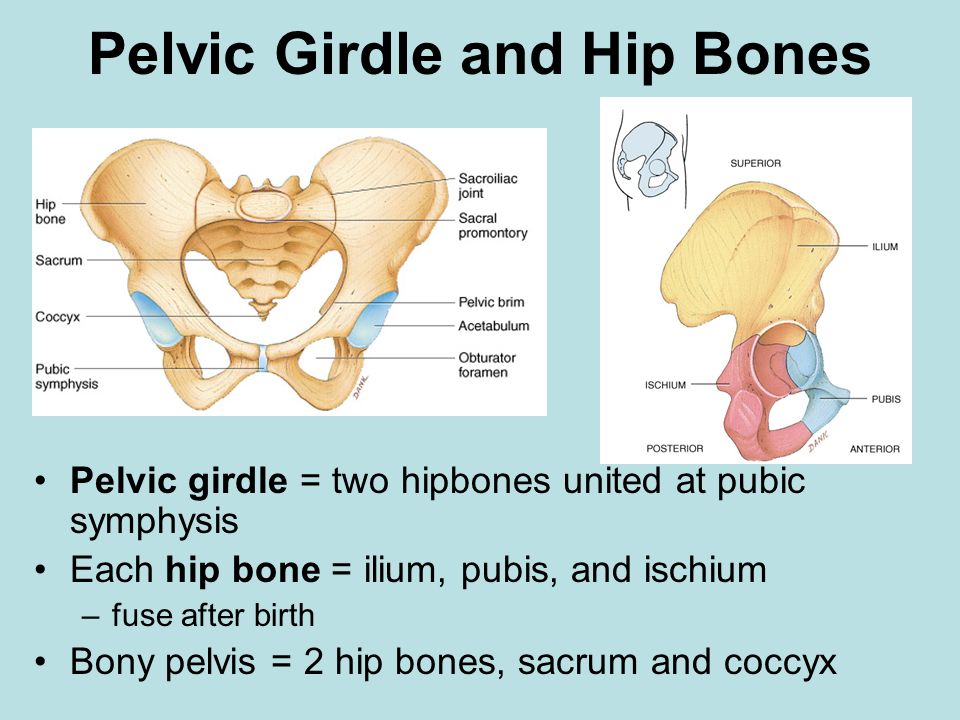 It is formed from almost immovably connected bones: unpaired - the sacrum and two massive, flat - right and left pelvic bones. A sacrum is wedged between the pelvic bones, to which is attached a small bone - the coccyx - a rudimentary remnant of the caudal skeleton.
It is formed from almost immovably connected bones: unpaired - the sacrum and two massive, flat - right and left pelvic bones. A sacrum is wedged between the pelvic bones, to which is attached a small bone - the coccyx - a rudimentary remnant of the caudal skeleton.
In children under 16, each pelvic bone consists of 3 separate bones: the ilium, ischium and pubis, interconnected by layers of cartilage. After 16 years they grow together. In this place there is a deep fossa - the acetabulum. It includes the head of the femur, forming the hip joint.
Structure of the ischium
The ischial bone has a powerful ischial tuberosity on which the human body rests when sitting. If a person is standing, the ischial tuberosity is hidden by a thick layer of gluteal muscles and fatty tissue.
Structure of the pubic bone
The pubic bone has 2 branches connected to each other at an angle. These branches, together with the branch of the ischium, limit a large obturator foramen on the pelvic bone, covered with a dense membrane.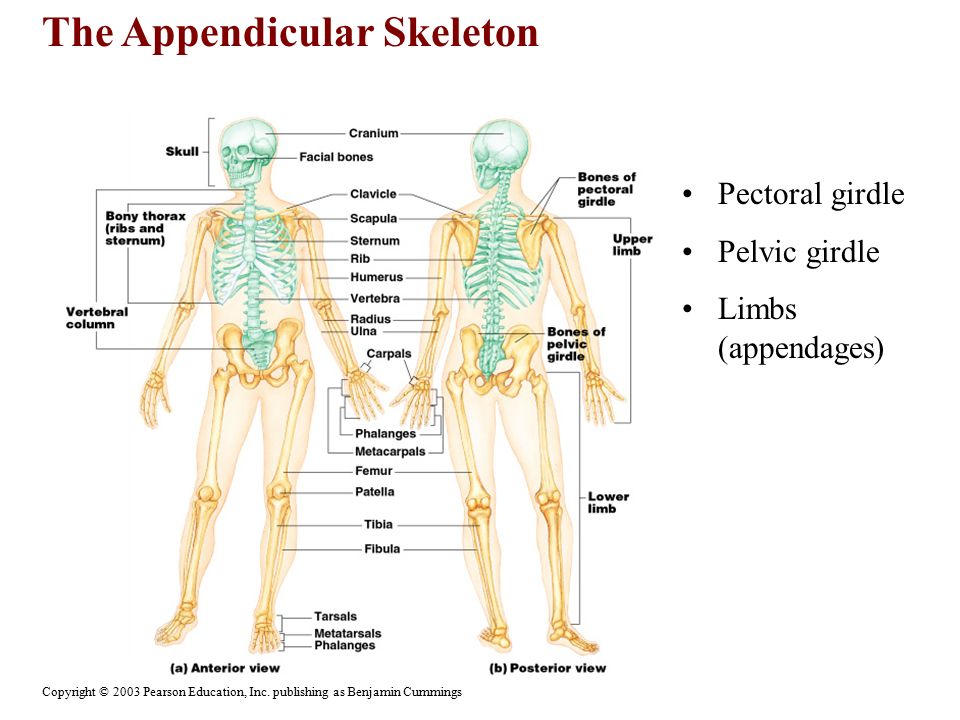 The pubic bones on the right and left are interconnected by cartilage - thus, the pubic symphysis (half-joint), one of the joints of the pelvic girdle, is formed. The elevation of the skin above the site of the symphysis is called the pubis.
The pubic bones on the right and left are interconnected by cartilage - thus, the pubic symphysis (half-joint), one of the joints of the pelvic girdle, is formed. The elevation of the skin above the site of the symphysis is called the pubis.
The value of the pubic symphysis is especially great for the female body. By the time of childbirth, the cartilaginous layer between the pubic bones softens, and the gap inside it allows the bones to move apart and thereby somewhat expand the birth canal.
Structure of the ilium
The ilium consists of a body and a thin wing, which expands upward and ends in a long crest. The crest serves as an attachment site for the broad abdominal muscles. The deepening of the inner surface of the wing forms the iliac fossa. It is in this hole on the right that the cecum with the appendix (appendix) is located.
Behind the ilium there is an articular surface, shaped like an auricle. It connects tightly with exactly the same surface on the sacrum, forming a flat sacroiliac joint.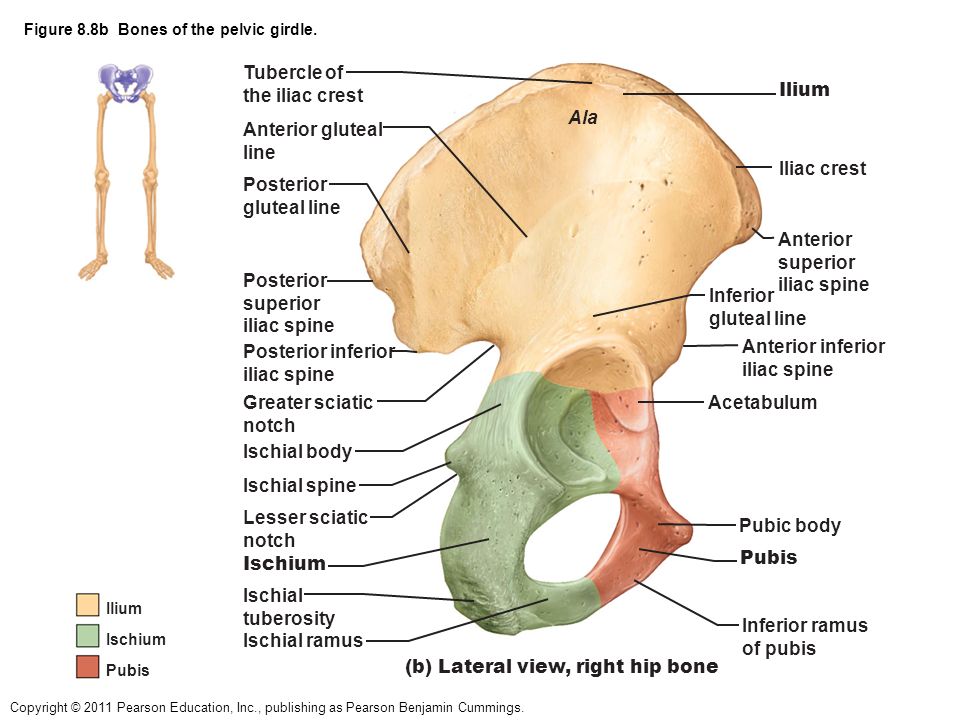 This joint is strengthened on all sides by bundles of ligaments, which, by their strength, are considered the most powerful in the human body.
This joint is strengthened on all sides by bundles of ligaments, which, by their strength, are considered the most powerful in the human body.
Pelvic angle
The pelvic bones are the attachment point for the muscles of the abdomen, back and lower extremities. In the vertical position of a person, the pelvis is tilted forward at an angle of 45-60 degrees relative to the horizontal plane. The value of the angle depends on the posture, in women it is greater than in men.
Large and small pelvis
There are large and small pelvis. The boundary line separating them runs along the inner surface of the pelvic bones from the protrusion on the spine - the cape (the junction of the last lumbar vertebra with the sacrum) to the upper edge of the pubic symphysis.
Large basin
The large pelvis is the upper part of the pelvis, formed by the deployed wings of the ilium. It is the lower wall of the abdominal cavity and serves as a support for the internal organs.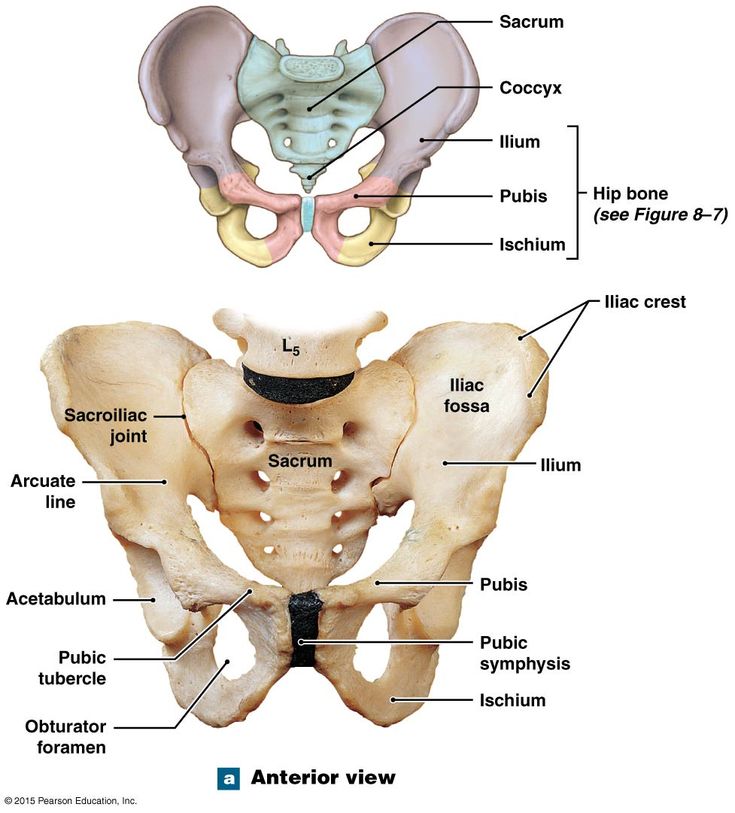
Pelvis
The small pelvis is located below the large one and is bounded behind by the sacrum and coccyx, in front and from the sides - by the ischial and pubic bones. It distinguishes between the entrance, exit and cavity. The pelvic cavity contains the bladder, rectum and internal genital organs (ovaries, fallopian tubes, uterus and vagina, prostate, seminal vesicles and vas deferens). The entrance to the small pelvis is open to the abdominal cavity and corresponds to the boundary line with the large pelvis. The exit from the pelvic cavity is closed by the muscles that form the pelvic diaphragm, the urethra and rectum pass through it in men, the urethra, rectum and vagina in women. Outside, this area of the body stands out as the perineum.
The pelvic organs differ from the abdominal organs in that they can
significantly change its volume: periodically filled
and the bladder and rectum are emptied, enlarged
and the uterus moves during pregnancy.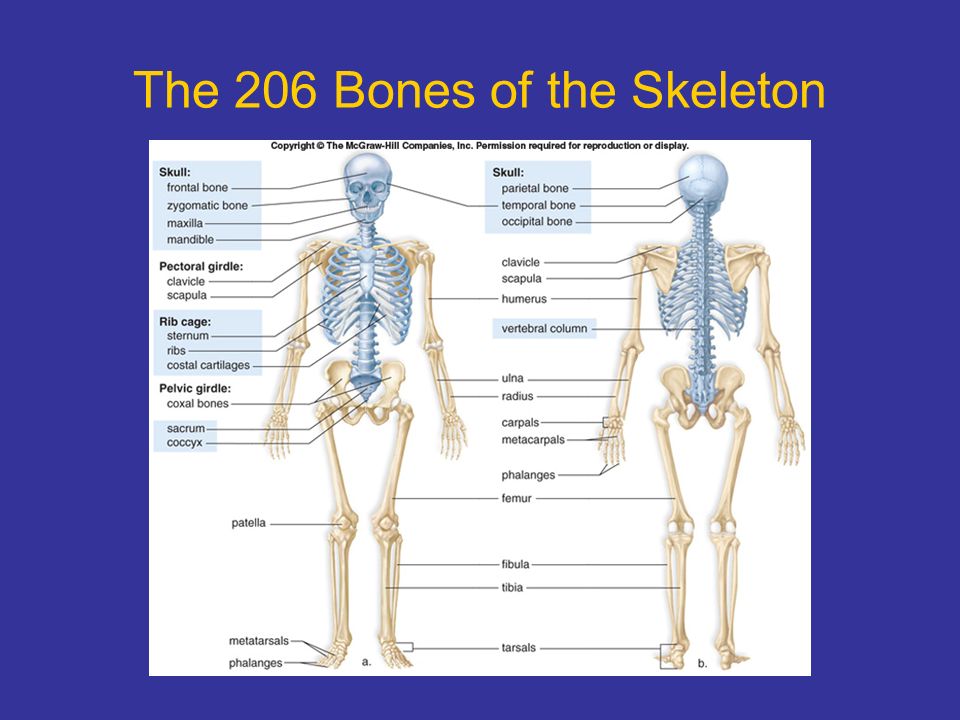 It affects
It affects
on the work of other organs and blood supply.
Pelvis female and male
In no part of the skeleton are sex differences as pronounced as in the pelvis. Sex differences in the pelvis begin to appear in children between the ages of 8 and 10 years. The average size of the male pelvis is about 2 cm smaller than the average size of the female pelvis. The female pelvis is wider and shorter than the male, the wings of the ilium are deployed more strongly. The angle between the lower branches of the pubic bones is rounded in the form of a pubic arch, the cape almost does not protrude into the pelvic cavity, and due to the wide, short and flat sacrum, the pelvic cavity has the shape of a cylinder.
Male pelvic structure
In men, the pelvis is already higher: the wings of the ilium are located almost vertically, the sacrum is strongly concave, and the promontory clearly protrudes into the cavity of the small pelvis, the subpubic angle is sharp.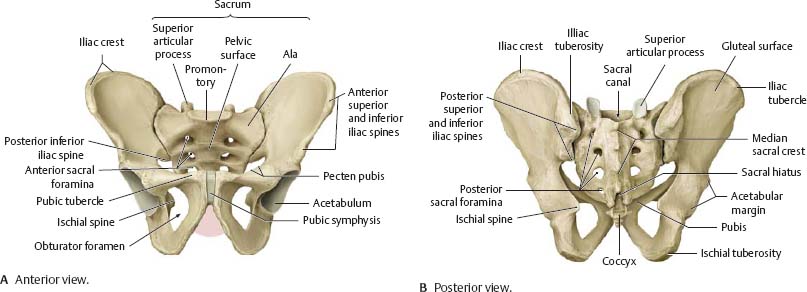 As a result, both the entrance and exit from the male pelvis are greatly narrowed, and its cavity itself has a conical shape.
As a result, both the entrance and exit from the male pelvis are greatly narrowed, and its cavity itself has a conical shape.
The structure of the pelvis in women
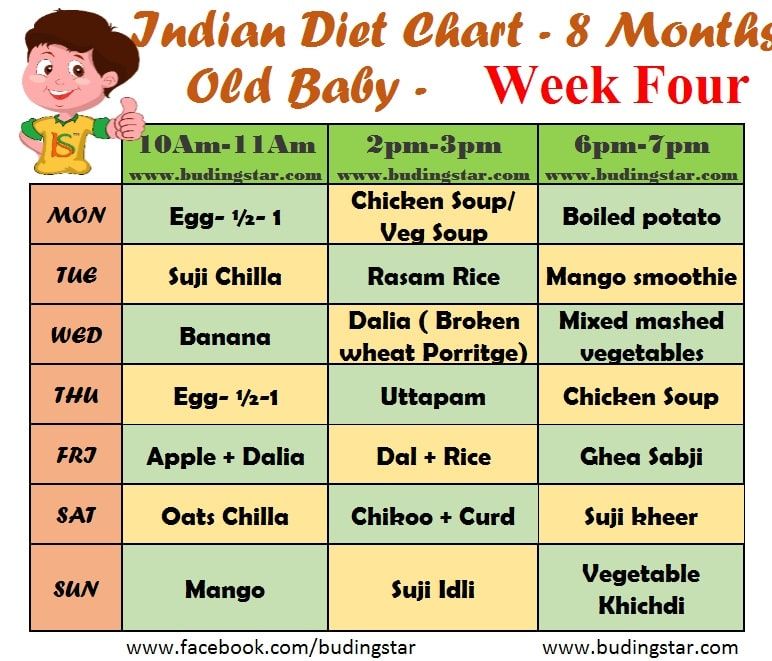
The fetus moves through the small pelvis in women during childbirth, so its shape and size are of great importance for a normal birth act. The dimensions of the small pelvis are determined by indirect measurements of the large pelvis with obstetric compasses. The internal dimensions are determined during a vaginal examination and with the help of ultrasound.
For example, the distance between protruding tubercles on the iliac crest (the so-called superior anterior iliac spines) in women is normally 25–27 cm, and the distance between the most distant points of the crest on the right and left is 28–30 cm. The size of the entrance and exit from the small pelvis, which in both direct and transverse dimensions are about 11–13 cm in women. The direct size of the exit from the small pelvis (the distance between the lower edge of the pubic symphysis and the top of the coccyx), equal to 10 cm, increases by 1.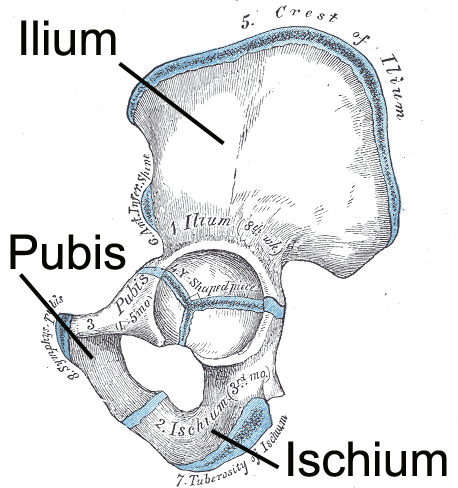 5–2 cm due to the deviation of the tip of the coccyx posteriorly.
5–2 cm due to the deviation of the tip of the coccyx posteriorly.
With violations in the development of the girl, due to rickets, spondylitis, coxitis and other diseases and poor nutrition, neglect of physical education or too much physical activity, deviations in the normal development of the pelvis are possible - a narrow pelvis. With a small degree of narrowing, childbirth is possible, but they are long and difficult. With a greater narrowing, there are obstacles to the passage of the fetus through the birth canal.
Author: Olga Gurova, Candidate of Biological Sciences, Senior Researcher, Associate Professor, Department of Human Anatomy, Peoples' Friendship University of Russia
The material uses photographs owned by shutterstock.com
Fracture of the pelvis - symptoms, treatment and consequences
A fall from a height or an accident increases the risk of a pelvic fracture.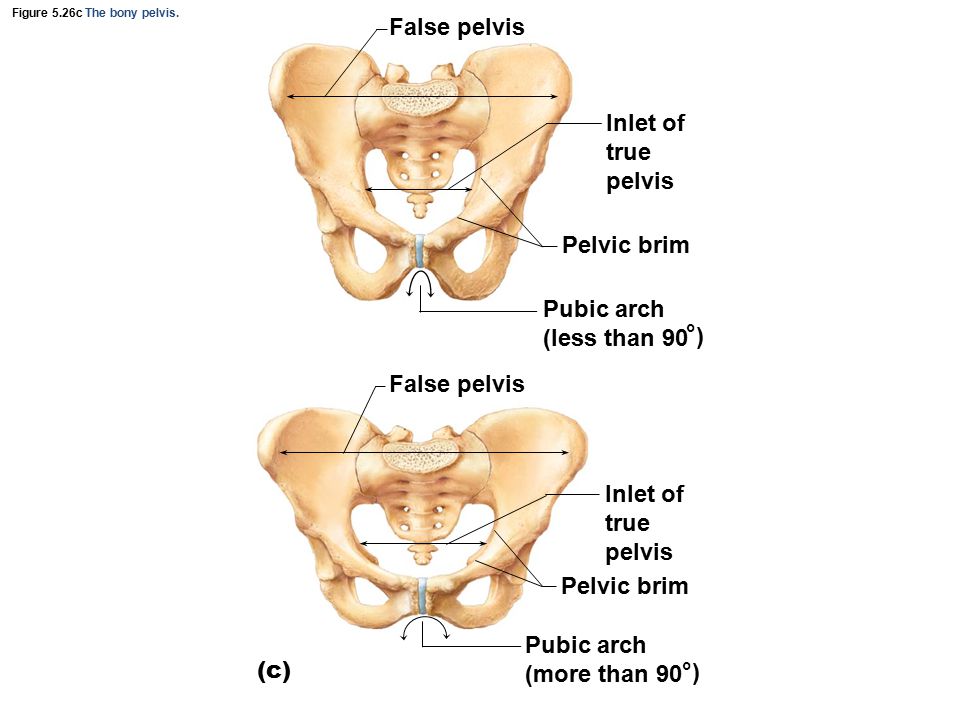 A large amount of blood flows from fragments of bones and soft tissues. The danger is the developing pain shock against the background of damage. Violation of the integrity of the pelvis affects the work of internal organs, therefore, it is accompanied by complications.
A large amount of blood flows from fragments of bones and soft tissues. The danger is the developing pain shock against the background of damage. Violation of the integrity of the pelvis affects the work of internal organs, therefore, it is accompanied by complications.
Types of injury
Destruction of the pelvis is accompanied by damage to blood vessels, nerves and ligaments. Allocate rotational and vertical instability of the pelvic ring. In the first case, there is a change in position in the horizontal plane with rotation around the sacrum and sacroiliac joints. In the second case, the bone moves towards the head.
According to the classification of the international AO/ASIF system, the following types of pelvic injuries are distinguished:
- Stable - affects the area outside the pelvic ring. This group includes fractures of the iliac wing, superior and inferior iliac spine, ischial tuberosity, sacral and coccygeal area below the joint.
- Rotationally unstable - ligaments of the back and bottom remain intact, but the sides of the pelvic part are damaged. These include an open book injury when the pubic symphysis is torn. The integrity of the sacroiliac ligaments, pubic and ischial bones is violated. This leads to bruising of the vagina, urethra, bladder and rectum.
- Fracture of the pelvic ring - part of the skeleton is displaced vertically and horizontally. The sacrum and iliac region are completely broken, which is accompanied by a violation of the integrity of the joint. This includes bilateral anterior or posterior displacement injuries in combination with acetabular injury.
Characteristic symptoms
The main common symptom is traumatic shock. The condition occurs after the loss of a large amount of blood. The affected skin turns pale and intense sweating begins. The pulse becomes frequent, and the pressure decreases, so fainting occurs.
Externally, the affected area is deformed, swelling and bruising of soft tissues appear.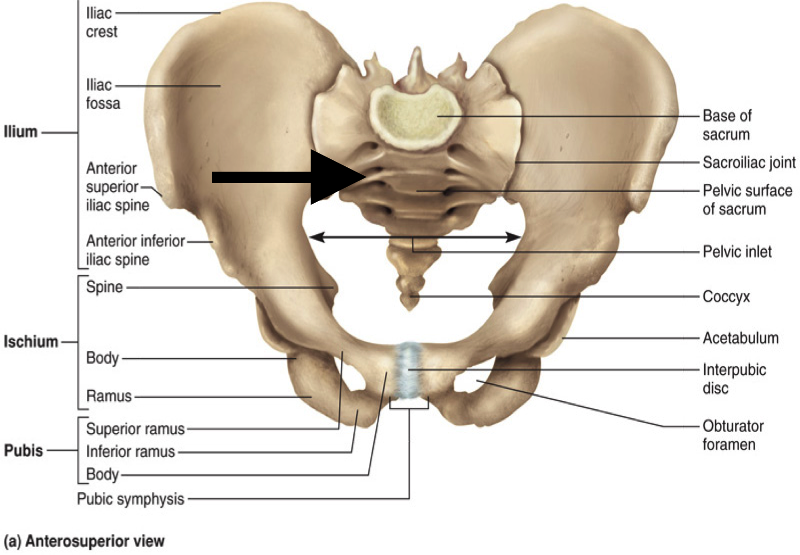 Sharp pains are felt in the pelvic region, and the mobility of bone fragments is accompanied by a crunch. When the anterior superior spine is torn off, the limb becomes shorter. With impacted fractures, it is difficult to raise the leg with the knee extended. Depending on the injured area, the symptoms are as follows:
Sharp pains are felt in the pelvic region, and the mobility of bone fragments is accompanied by a crunch. When the anterior superior spine is torn off, the limb becomes shorter. With impacted fractures, it is difficult to raise the leg with the knee extended. Depending on the injured area, the symptoms are as follows:
- Broken ilium gives out strong pain. Broken upper section hinders the movement of the joint.
- Bruise of the coccyx is accompanied by pain, which is aggravated by pressing on the lower part of the sacrum. Difficulty passing a bowel movement. If the nerve is affected, the sensitivity of the buttocks decreases.
- In case of violations of the pelvic ring, the pubic region and perineum hurt, if its integrity is preserved. Foot movements increase discomfort. When the anterior half ring is injured, pain is felt in the pelvis.
- Fracture of the superior and ischial ramus of the pubis is characterized by the frog posture. In this state, the knees are bent and the feet are turned outward.
 The first minutes the victim does not complain of pain, but gets tired.
The first minutes the victim does not complain of pain, but gets tired. - In case of rupture of the symphysis, it is painful to spread the legs.
- Bilateral fracture characterized by asymmetry of the pelvis and bruising around the scrotum and perineum.
- Trauma to the acetabulum results in dysfunction of the hip joint.
Severe injuries cause problems with internal organs. Damage to the urethra is accompanied by urinary retention and bruising. A ruptured bladder is indicated by blood in the urine.
First aid
First check the general condition of the injured person. With an open fracture, stop bleeding with a tourniquet or improvised means. Wounds are treated with antibiotics. The main task is to eliminate traumatic shock and relieve pain. To do this, use analgesics and raise the stretcher by 45 cm. The victim is covered with a blanket to warm.
Further stabilize the cervical region with a collar. A 30 cm high roller is placed under the half-bent knees.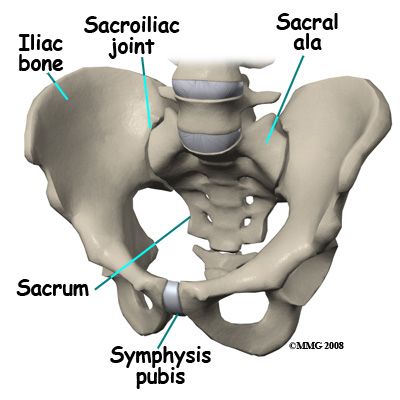 The pelvis is tied with material to reduce displacement.
The pelvis is tied with material to reduce displacement.
It is impossible to constantly move the patient in order to prevent repeated displacement of bones and injury to internal organs.
Transportation is handled with care as immobility is difficult. A comfortable position is the frog pose, when the knees are raised and spread apart.
Therapeutic measures
The initial actions are aimed at eliminating the state of shock, so they use painkillers and normalize blood circulation. Intrapelvic anesthesia of the injured area is performed, but with marginal closed fractures, the anesthetic is injected into the hematoma. In the case of isolated fractures, a portioned blood transfusion occurs over 2–3 days.
Subsequent therapy depends on the severity of the injury. There are conservative, surgical treatment or surgical traction. Light bruises without complications are treated conservatively. It consists in prolonged immobilization of the injured.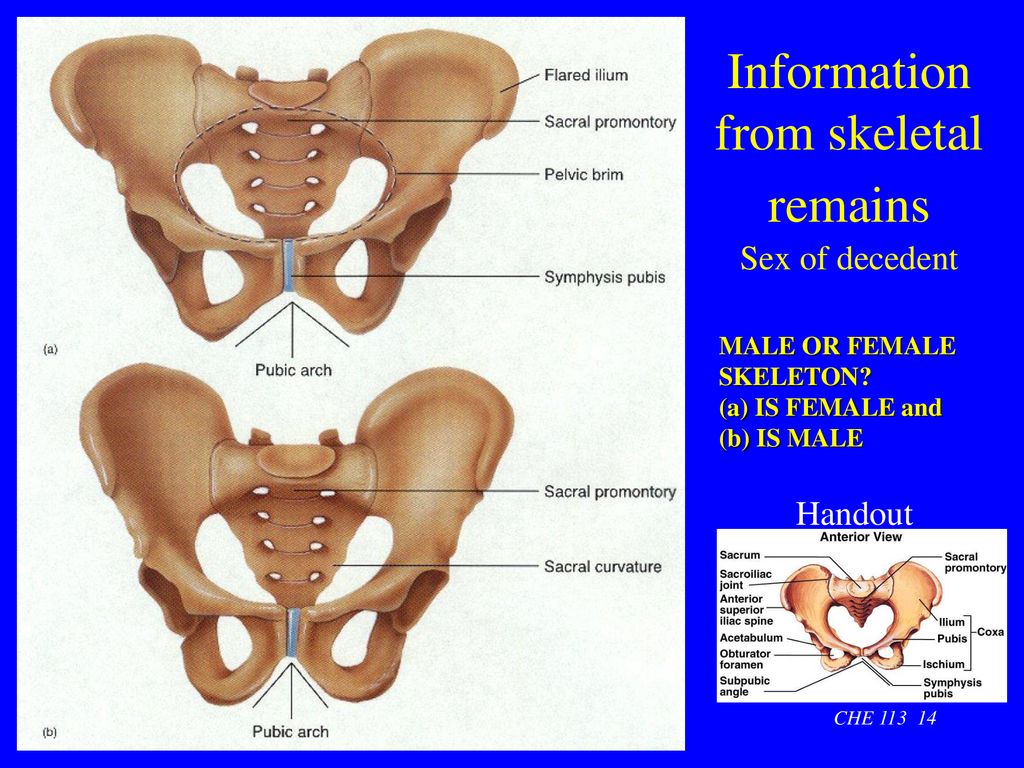 With marginal fractures, the leg is bent and a roller is placed so that the bones grow together correctly. After 2 weeks they try to walk.
With marginal fractures, the leg is bent and a roller is placed so that the bones grow together correctly. After 2 weeks they try to walk.
For pelvic ring injuries, lie still for 3-4 weeks. With bruises of the sacrum and coccyx, a soft pillow is placed under the pelvis. During this period, they are engaged in developing physical education, physiotherapy and massage. If at the end of therapy the pain does not go away, an operation is prescribed to remove the coccyx.
When a displaced fracture is diagnosed, surgical traction is used. A special needle is passed through the damaged part of the skeleton and fixed in the desired position. The pose is fixed with an apparatus with a suspended load of 7–8 kg. For balance, adhesive traction is applied to a healthy thigh and lower leg.
After 10 days, the load on the leg is reduced, and after 5-6 weeks the process is completed. Bilateral damage requires skeletal traction on both legs, and if the symphyses are torn, a hammock is used. With such violations, walking with crutches is allowed after 3 months.
With such violations, walking with crutches is allowed after 3 months.
Surgical intervention is performed in case of severe injuries: large shift of fragments, dysfunction of vital organs, comminuted fractures. For osteosynthesis, metal structures are used to fix parts of the pelvis. After the operation is completed, medications are prescribed and a rehabilitation program is developed.
The victim must stay in the hospital for the period prescribed by the doctor. If the treatment gives good results, the ability to work is restored after 4-6 months.
In old age, the recovery process is delayed for 8 months or more. It is not always possible to establish the previous functionality, so some patients remain disabled.
Rehabilitation and recovery
These injuries take a long time to heal, and immobilization is fraught with a deterioration in the ability to move. To restore the working capacity of the limbs, a complex of rehabilitation measures is carried out.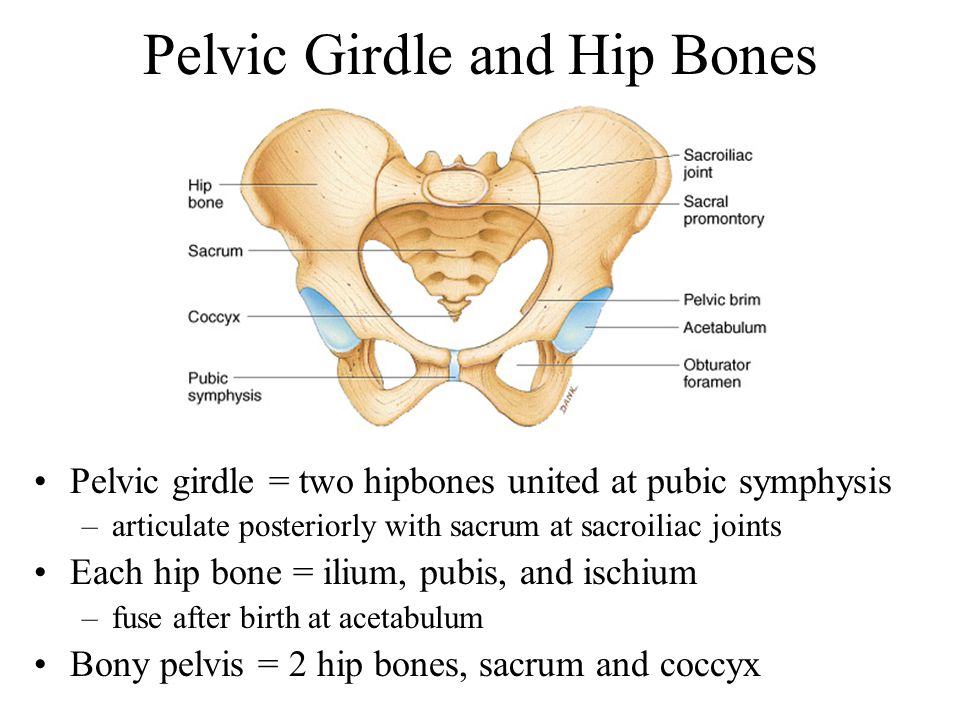 A set of procedures is selected individually for each patient. Ways to restore pelvic function include the following:
A set of procedures is selected individually for each patient. Ways to restore pelvic function include the following:
- exercise therapy;
- massage for leg development;
- physiotherapy;
- proper nutrition.
Exercise therapy is divided into 3 blocks of exercises, which differ in the level of complexity. You can not endure the pain that appeared in the process of gymnastics. Physical education is done with the permission of the surgeon, so as not to harm. In the initial phase, the blood supply in the buttocks and lower extremities is normalized. At the next stage, the exercises strengthen the pelvic girdle and muscles of the limbs. The last block includes gymnastics to restore the ability to walk.
Watch this video on YouTube
Massage is started 5 days after the fracture. The master makes leisurely rubbing or movements to vibrate soft tissues. Massage the legs and buttocks.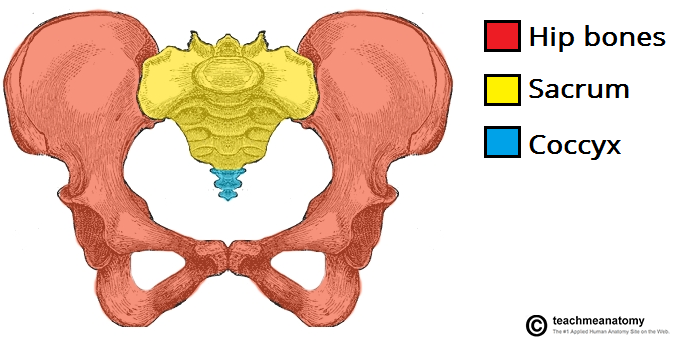 The average course is 15 sessions.
The average course is 15 sessions.
Possible consequences
Fracture in the pelvic region is complicated by contusion of internal organs. If the bladder is damaged, it is not possible to empty it, so a catheter is inserted. Blood that appears during a rectal examination indicates damage to the rectum. The consequences of the injury are detected after 2-3 days or after a long time.
Bruises of blood vessels, tendons and muscles are found at an early stage. With an injury to the pubic bone, disturbances in the reproductive system are possible. Early systemic consequences of pelvic dysfunction include:
- aseptic infection;
- with an open fracture, there is a risk of sepsis;
- long bone recovery period;
- hypovolemic shock.
Watch this video on YouTube
As time goes by, there are late effects. After the treatment of the fracture, the pain does not go away if the nerve endings are affected.