Chest cold pregnant
Bronchitis While Pregnant: Prevent and Treat
When you’re expecting, your growing belly can make it difficult to take in full, deep breaths. And bronchitis, an inflammation of the lower respiratory tract, can make taking in deep breaths even harder.
Bronchitis is inflammation of the airways that causes you to develop extra mucus. Acute bronchitis is most often caused by infection. It results in lots of coughing. You might also have a fever, sore throat, shortness of breath, chest pain, chills, and body aches.
While you may not normally call your doctor for these symptoms, you have to be more careful during pregnancy. Now you’re living for two (or more).
Bronchitis is fairly common, especially during the winter months. Taking preventive steps is important to help you and your baby-to-be stay well.
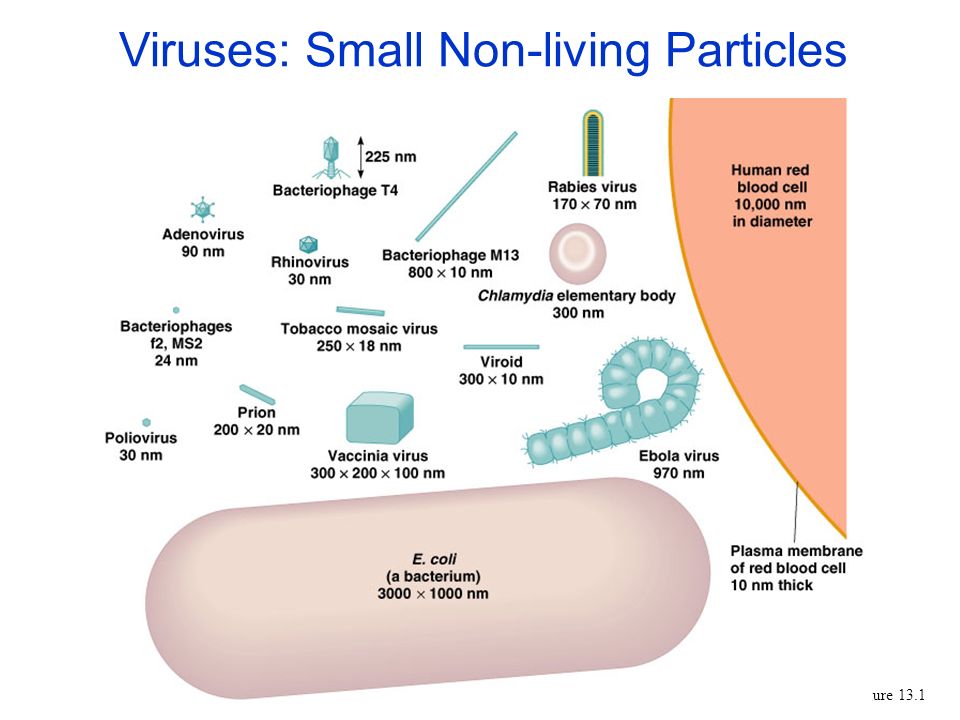
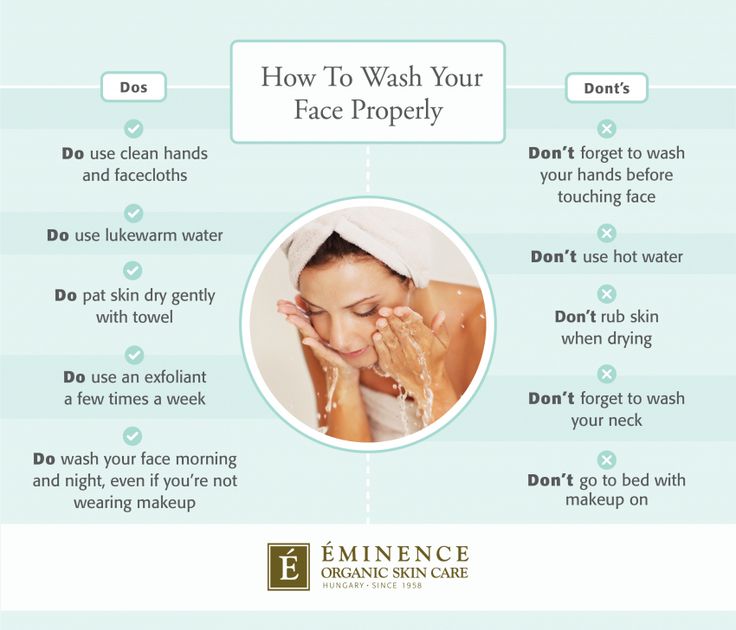
Bronchitis can be the result of a bacterial or viral infection. Both are unfortunately easy to catch. One of the best ways to protect against bronchitis is to wash your hands often.
Avoiding exposure to people that have bronchitis or other respiratory conditions is also important. If a loved one has an infection, try to stay away as much as you can. This is especially true if they have a fever.
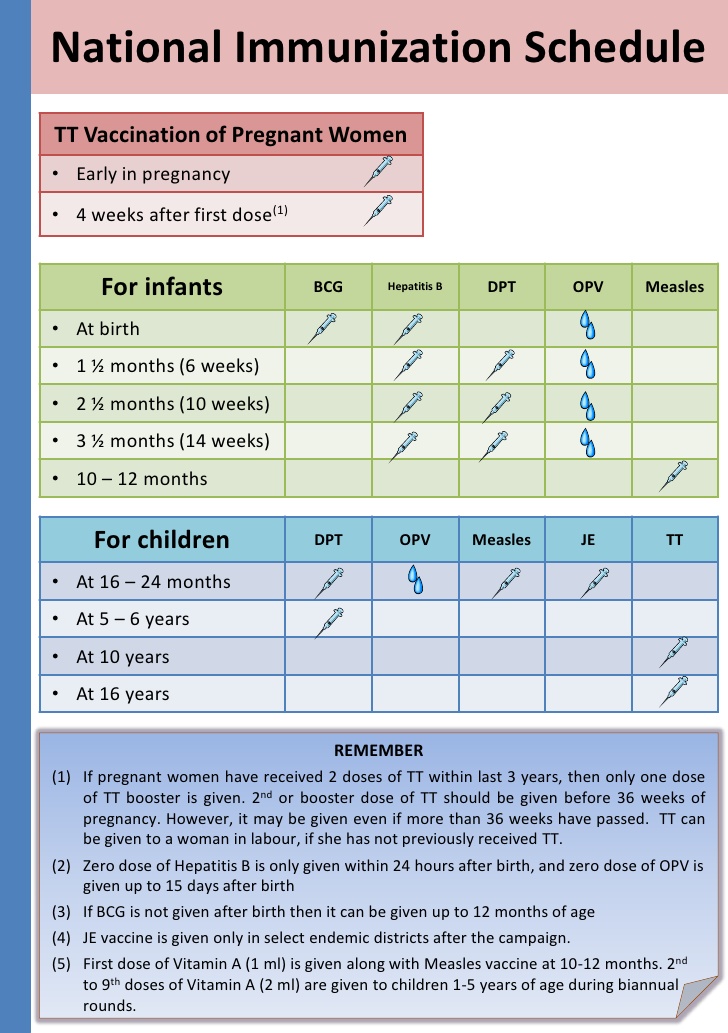
The flu virus can cause bronchitis, so be sure to get an annual flu shot. You can also encourage those around you to get the shot. The flu shot doesn’t contain live viruses, so it shouldn’t make you sick.
Getting the flu shot can also boost your baby’s immune system for about six months after birth. That means your little one will be less likely to experience the flu virus.
Avoiding cigarette smoke is also important in preventing bronchitis. Smoking irritates the airway linings, hindering the body’s natural defense system against infections.
Unfortunately, for some expectant moms, bronchitis can quickly progress to a more severe respiratory disorder. One example could be pneumonia. Seek emergency medical treatment if you experience the following symptoms:
- chest pain
- coughing up blood
- fever greater than 100.
 4°F, or 38°C
4°F, or 38°C - shortness of breath that doesn’t get better with rest
While a large portion of bronchitis-related cases are due to a virus, sometimes bacteria can lead to bronchitis.
Bacteria-caused bronchitis can be treated with antibiotics if symptoms become severe or don’t seem to be getting better after a week. Check with your doctor to see if you’ll need antibiotics.
If your doctor suspects your bronchitis is due to a bacterial infection, they may prescribe antibiotics. While not all antibiotics are considered safe during pregnancy, some are.
The following antibiotics are typically considered safe during pregnancy:
- amoxicillin
- ampicillin
- clindamycin
- erythromycin
- penicillin
- nitrofurantoin
You shouldn’t take a class of antibiotics called tetracycline antibiotics. Examples include doxycycline and minocycline. These are associated with potentially causing discoloration to a baby’s teeth.
The antibiotics trimethoprim and sulfamethoxazole also are pregnancy no-no’s. They’ve been known to cause birth defects.
Antibiotics aren’t always necessary to treat bronchitis. A virus usually causes the condition and antibiotics won’t kill a virus. But if your symptoms aren’t getting better after a few days, see your doctor. They will evaluate you further and look for bacterial causes of infection.
Always check with your doctor before trying any at-home treatments. You’ll want to make sure they’re safe for you and your growing little one. While these treatments won’t cure bronchitis, they can help you feel better as your body heals.
Try irrigating your nasal passages using a mixture of 8 ounces warm water, 1/2 teaspoon of salt, and 1/2 teaspoon of baking soda. This can help you feel less stuffy.
Lean forward over a sink with your head at a 45-degree angle so that one nostril is pointed toward the sink. Using a syringe or squeeze bottle, pour the water into your nostril as you breathe through your mouth. The water should come out on the other side of your nose.
The water should come out on the other side of your nose.
Repeat this process about three to four times per day.
Other at-home treatment options include:
- Vicks vapor rub
- using a humidifier
- rest and fluids
- steamy shower
- pregnancy-safe hot tea
While you should always check with your doctor first, you may be able to take some over-the-counter antihistamines after the first trimester.
You can take the following medications to help dry up the extra mucus that has built up in your lungs after your first trimester:
- chlorpheniramine (Chlor-Trimeton)
- loratadine (Claritin)
- Novahistine
- pseudoephedrine (Sudafed)
- Tylenol Cold & Sinus
Most respiratory infections like bronchitis are not associated with a high risk for pregnancy complications or birth defects. But that doesn’t address the discomfort you experience while you are recovering from bronchitis. Take preventive measures and check in with your doctor for treatment options..jpg)
Bronchitis While Pregnant: Prevent and Treat
When you’re expecting, your growing belly can make it difficult to take in full, deep breaths. And bronchitis, an inflammation of the lower respiratory tract, can make taking in deep breaths even harder.
Bronchitis is inflammation of the airways that causes you to develop extra mucus. Acute bronchitis is most often caused by infection. It results in lots of coughing. You might also have a fever, sore throat, shortness of breath, chest pain, chills, and body aches.
While you may not normally call your doctor for these symptoms, you have to be more careful during pregnancy. Now you’re living for two (or more).
Bronchitis is fairly common, especially during the winter months. Taking preventive steps is important to help you and your baby-to-be stay well.
Bronchitis can be the result of a bacterial or viral infection. Both are unfortunately easy to catch. One of the best ways to protect against bronchitis is to wash your hands often.
Avoiding exposure to people that have bronchitis or other respiratory conditions is also important. If a loved one has an infection, try to stay away as much as you can. This is especially true if they have a fever.
The flu virus can cause bronchitis, so be sure to get an annual flu shot. You can also encourage those around you to get the shot. The flu shot doesn’t contain live viruses, so it shouldn’t make you sick.
Getting the flu shot can also boost your baby’s immune system for about six months after birth. That means your little one will be less likely to experience the flu virus.
Avoiding cigarette smoke is also important in preventing bronchitis. Smoking irritates the airway linings, hindering the body’s natural defense system against infections.
Unfortunately, for some expectant moms, bronchitis can quickly progress to a more severe respiratory disorder. One example could be pneumonia. Seek emergency medical treatment if you experience the following symptoms:
- chest pain
- coughing up blood
- fever greater than 100.
 4°F, or 38°C
4°F, or 38°C - shortness of breath that doesn’t get better with rest
While a large portion of bronchitis-related cases are due to a virus, sometimes bacteria can lead to bronchitis.
Bacteria-caused bronchitis can be treated with antibiotics if symptoms become severe or don’t seem to be getting better after a week. Check with your doctor to see if you’ll need antibiotics.
If your doctor suspects your bronchitis is due to a bacterial infection, they may prescribe antibiotics. While not all antibiotics are considered safe during pregnancy, some are.
The following antibiotics are typically considered safe during pregnancy:
- amoxicillin
- ampicillin
- clindamycin
- erythromycin
- penicillin
- nitrofurantoin
You shouldn’t take a class of antibiotics called tetracycline antibiotics. Examples include doxycycline and minocycline. These are associated with potentially causing discoloration to a baby’s teeth.
The antibiotics trimethoprim and sulfamethoxazole also are pregnancy no-no’s. They’ve been known to cause birth defects.
Antibiotics aren’t always necessary to treat bronchitis. A virus usually causes the condition and antibiotics won’t kill a virus. But if your symptoms aren’t getting better after a few days, see your doctor. They will evaluate you further and look for bacterial causes of infection.
Always check with your doctor before trying any at-home treatments. You’ll want to make sure they’re safe for you and your growing little one. While these treatments won’t cure bronchitis, they can help you feel better as your body heals.
Try irrigating your nasal passages using a mixture of 8 ounces warm water, 1/2 teaspoon of salt, and 1/2 teaspoon of baking soda. This can help you feel less stuffy.
Lean forward over a sink with your head at a 45-degree angle so that one nostril is pointed toward the sink. Using a syringe or squeeze bottle, pour the water into your nostril as you breathe through your mouth. The water should come out on the other side of your nose.
The water should come out on the other side of your nose.
Repeat this process about three to four times per day.
Other at-home treatment options include:
- Vicks vapor rub
- using a humidifier
- rest and fluids
- steamy shower
- pregnancy-safe hot tea
While you should always check with your doctor first, you may be able to take some over-the-counter antihistamines after the first trimester.
You can take the following medications to help dry up the extra mucus that has built up in your lungs after your first trimester:
- chlorpheniramine (Chlor-Trimeton)
- loratadine (Claritin)
- Novahistine
- pseudoephedrine (Sudafed)
- Tylenol Cold & Sinus
Most respiratory infections like bronchitis are not associated with a high risk for pregnancy complications or birth defects. But that doesn’t address the discomfort you experience while you are recovering from bronchitis. Take preventive measures and check in with your doctor for treatment options.
What is breast swelling? | Breast swelling
Some mothers experience breast swelling when milk begins to flow in the first days after childbirth. Usually this phenomenon is temporary and easily eliminated. Read our article to find out how to help yourself.
Share this information
Sioned Hilton, health visitor, neonatal nurse and lactation consultant:
Schoned, a mother of three, has been supporting families with newborns and young children for over 30 years. She provides advice on breastfeeding and pumping, both in clinics and at home. In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians.
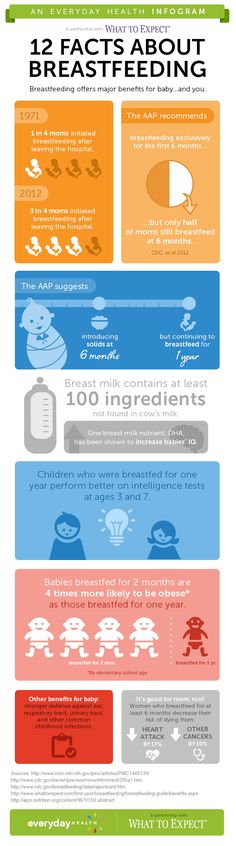
When you start breastfeeding, you first produce a small amount of colostrum, which gradually increases over the first few days. After about two to four days, production increases significantly. This phenomenon is called the "arrival" of milk. 1
One of the signs that milk is starting to come in is a change in the breast - it fills up and becomes firmer. This is due not only to an increase in the amount of milk, but also to increased blood flow and additional lymphatic fluid to the breast tissues. 2
This is due not only to an increase in the amount of milk, but also to increased blood flow and additional lymphatic fluid to the breast tissues. 2
If the child eats well and often, then for most mothers this feeling of heaviness disappears over time without any complications. However, some women produce so much milk that their breasts fill up and become painful and very hard. This condition is called breast swelling. And although everything usually passes in a day or two, this period can be quite painful.
How does breast swelling manifest itself?
Swelling may affect one or both breasts. It can cause swelling, sometimes down to the armpits, and a throbbing sensation. The chest becomes quite hot, sometimes lumps are felt in it. All this is due to the fact that a huge number of processes take place inside. You may also notice other symptoms, such as the skin on your breasts becoming shiny and tight, and your nipples becoming hard and flat. Swelling of the mammary glands can even cause a temperature to rise to 37. 5–38.3°C (99–101°F). 3
5–38.3°C (99–101°F). 3
In addition to painful sensations, breast swelling is also dangerous because it can make breastfeeding difficult, and this, in turn, will worsen the situation even more. If the baby finds it difficult to latch on because the nipples are flat and the breast tissue is firmer, nipples may become inflamed. In addition, in the event of a poor grip, he will not be able to completely empty the chest. Thus, if left untreated, swelling of the mammary glands can lead to blockage of the milk ducts, mastitis, and reduced milk production.
What causes breast swelling?
Usually breast swelling is due to the fact that the child does not feed often enough (less than eight times a day). In principle, this can happen to any mother, but women who have undergone various breast surgeries, including breast augmentation, are more prone to swelling of the mammary glands. 2 Wearing a bra that is the wrong size or that is too tight can increase discomfort and lead to clogged milk ducts and even mastitis.
Breast swelling can occur in both breastfeeding mothers and mothers who are not or cannot breastfeed. The hormonal changes that occur after the birth of a baby and the release of the placenta and increase milk production are independent of whether you are breastfeeding or not. Swelling can also occur if the number of feedings is drastically reduced, for example, if the child becomes ill, sleeps longer, starts eating solid foods, or goes to nursery.
How to treat breast swelling?
2The best cure for swollen breasts is a hungry baby! Try to empty your breasts as much and as often as possible to facilitate the release of milk. To do this, feed your baby on demand, preferably eight to twelve times a day.
Maintain skin-to-skin contact with your baby, cuddling as often as possible during the day and at night when you are awake. This will allow him to smell the attractive smell of your milk and have easy access to the breast, and you will be able to better monitor signs that he is hungry and, accordingly, feed more often. Let the baby eat enough from one breast before offering the second.
Let the baby eat enough from one breast before offering the second.
It's a good idea to see a lactation consultant or specialist to check if your baby is properly grasped and positioned. It depends on how well he will eat and empty his chest. The tips below will also help you relieve the symptoms of breast swelling.
Tips for relief of breast swelling 2
- Breastfeed at least eight times a day.
- Make sure your baby is latching on well.
- Try other feeding positions.
- Gently massage your breasts during feeding to improve the flow of milk.
- Express some milk by hand or with a breast pump before feeding to soften the nipple and make it easier for your baby to latch on.
- If your breasts are still firm and full after a feed, pump more until you feel better.
- If your baby cannot breastfeed, express milk for him. Pumping must be continued until the breast becomes softer, and do this at least eight times a day.

- Try the areola pressure softening technique. This helps to remove excess fluid from the breast. A lactation consultant or specialist will show you how to do this.
- If milk leaks, try taking warm showers or applying warm flannel to your breasts just before feeding or pumping to soften your breasts and make it easier for your milk to flow. You should not, however, warm the chest for more than two minutes, as this can only increase swelling.
- If your milk isn't leaking, try applying cold compresses, chilled gel pads, or even frozen green peas wrapped in a towel for ten minutes after feeding to reduce swelling and relieve pain.
- Put clean cabbage leaves in your bra. Yes Yes! For many moms, it really helps reduce swelling and discomfort, and there are scientific explanations for this. 4
- Take an anti-inflammatory pain reliever. While breastfeeding, you can take some medications, in consultation with your doctor. Always consult your doctor, follow the drug manufacturer's instructions and the pharmacist's recommendations.
 To learn more about medications and breastfeeding, read our article on breastfeeding when sick.
To learn more about medications and breastfeeding, read our article on breastfeeding when sick. - Wear an appropriately sized and comfortable nursing bra, avoid underwire or no bra at all.
- Do not skip feedings or stop breastfeeding abruptly as this may increase breast swelling.
Seek medical advice if your 5 temperature rises above 38 °C or if your baby is unable to suckle due to breast swelling.
And in any case, try to remain calm. Your body is just getting used to producing milk and feeding your baby. Breast swelling should go away on its own soon after you both get comfortable with breastfeeding.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2007;12(4):211-221.
2 Berens P, Brodribb W. ABM Clinical Protocol# 20: Engorgement, Revised 2016. Breastfeed Med . 2016;11(4):159-163. - Behrens P, Brodrhibb W, "AVM Clinical Protocol #20: Engorgement, 2016 edition". Brestfeed Med (Breastfeeding Medicine). 2016;11(4):159-163.
3 Affronti M Low-grade fever: how to distinguish organic from non-organic forms. Int J Clin Pract. 2010;64(3):316-321. - Affronti M. et al., "Subfebrile temperature: how to distinguish organic from non-organic cases." Int Zh Klin Prakt. 2010;64(3):316-321.
4 Boi B et al. The effectiveness of cabbage leaf application (treatment) on pain and hardness in breast engorgement and its effect on the duration of breastfeeding. JBI Libr Syst Rev . 2012;10(20):1185-1213. - Boys B. et al., "Effectiveness of cabbage leaf (as a drug) for breast pain and engorgement, and its effect on the duration of breastfeeding." JBAi Libr Sist Rev. 2012;10(20):1185-1213.
- Boys B. et al., "Effectiveness of cabbage leaf (as a drug) for breast pain and engorgement, and its effect on the duration of breastfeeding." JBAi Libr Sist Rev. 2012;10(20):1185-1213.
5 NHS Choices. How do I take someone's temperature? [Internet]. UK: NHS Choices; updated 2016 June 29. Available from : www.nhs.uk/chq/pages/1065.aspx?categoryid=72 - NHS Choice. "How to measure the temperature?" [Internet]. United Kingdom: NHS Choice, 29 June 2016 edition Article linked: www.nhs.uk/chq/pages/1065.aspx?categoryid=72
Pregnancy and the mammary gland
During pregnancy, in addition to growing hips and tummy, the breast undergoes one of the most amazing transformations. From the end of the first trimester, she prepares to produce milk.
From the end of the first trimester, she prepares to produce milk. It is especially important to monitor the condition of the mammary glands during this period, because many hormonal changes occur in the body.
In order for the expectant mother to feel good and also be able to easily establish breastfeeding, let's figure out together how to protect yourself from breast diseases.
What happens to the breasts during pregnancy
At 4-5 weeks, the breasts become more sensitive , soreness similar to PMS symptoms may appear. This is normal and you should not be afraid. Hypersensitivity usually goes away after the first trimester, but sometimes persists until the very birth. After 6 weeks, there is more melanin in the woman's body, which is why the nipples and areolas become darker.
By 10-12 weeks of gestation, a complex duct system develops in the breast , the glandular tissue grows, and the nipples become more swollen and bulging, a noticeable vein network appears on the chest. This is normal and usually goes away after the baby is born.
At the beginning of the second trimester, yellowish discharge appears from the nipples . This is not milk yet, but similar in composition, but more nutritious colostrum is the first food for babies. So the mother's body prepares for a meeting with a newborn. Colostrum may be more actively secreted during intimacy or after a shower. Some women may experience even slight spotting from the nipple. They are associated with the destruction of small capillaries caused by the growth of ducts. Do not worry, but be sure to inform the gynecologist who is observing you
This is not milk yet, but similar in composition, but more nutritious colostrum is the first food for babies. So the mother's body prepares for a meeting with a newborn. Colostrum may be more actively secreted during intimacy or after a shower. Some women may experience even slight spotting from the nipple. They are associated with the destruction of small capillaries caused by the growth of ducts. Do not worry, but be sure to inform the gynecologist who is observing you
By 18 weeks, the bust may increase by 1-3 sizes . Therefore, it is very important to choose the right underwear that will not restrict movement and will be able to support the grown volumes well. It is recommended to pay attention to cotton bras with wide straps, pitted, but with lower support.
How to prepare your breasts for pregnancy
If you are just planning to become a mother, you should definitely pay attention to breast health.
Usually, experts recommend a routine ultrasound, but if you are over 30 years old or women in your family have breast problems, it is better to have a mammogram as well.
Mammograms are X-rays that are good at identifying even small tumors and cysts in tissues. In case of urgent need, it is also done for pregnant women, protecting the tummy from X-rays with a special apron. But such studies are not routinely carried out so as not to risk the health of the fetus.
If any pathologies were found , for example, a cyst, removal of will most likely be recommended. This is important to do before pregnancy and childbirth, as during lactation, cysts can block the ducts and become inflamed, causing mastitis.
Therefore, it is very important to trace any diseases or changes before conception and stop them surgically or conservatively.
Bad advice: what not to do
There are many myths around breast preparation for lactation. For example, that the nipples need to be trained and rubbed with a wet towel to avoid cracks on them later.
In fact, the nipples of a woman who has given birth are quite capable of withstanding feeding, and cracks appear not from excessive sensitivity, but due to improper attachment of the baby.
In addition, the areola secretes its own protective layer, which helps the skin adapt to lactation. And if you often rub and wash your breasts, especially with soap, it will break down, which will lead to cracks in the nipples. If you have uterine tone, actively rubbing your nipples is also not recommended, as this can increase muscle tension.
Marketers actively advertise creams and oils for cracks and stretch marks. However, the effectiveness of such funds has not been scientifically proven. The number of stretch marks is associated to a greater extent with the hereditary elasticity of the skin.
So to deal with them, it is better to choose good supportive underwear and take a contrast shower.
Pregnancy risk factors
Hormonal changes and other changes in the body of a future mother can be a big test for a woman's body. Pregnancy usually does not provoke the appearance of pathologies. But, if a woman had an untracked tumor before pregnancy, during these 9 months under the influence of hormones, it can begin to grow actively, because up to 70% of tumors are estrogen-dependent.
Pregnancy, childbirth and lactation have long been thought to reduce the risk of breast cancer. Researchers have now found that this is not true.
Firstly, the risk of oncology decreases only for hormone-dependent cancers and in the long term, that is, after 15-20 years. But immediately after pregnancy increase.
This means that all women, regardless of age or status, should be screened annually.
Sometimes women, experiencing pain in the chest, are afraid to go to the doctor, so as not to hear a frightening diagnosis. But breast cancer does not hurt, it is usually accompanied by other symptoms, such as :
- Formation of dense lumps and bumps in breast tissues;
- Asymmetric lumps and swellings in the chest;
- Sudden retraction of one or both nipples;
- Enlarged lymph nodes in the armpits.
During pregnancy, the diagnosis is complicated by the peculiarities of the physiological state of the woman.