Hospital baby monitor
Fetal Heart Monitoring | Johns Hopkins Medicine
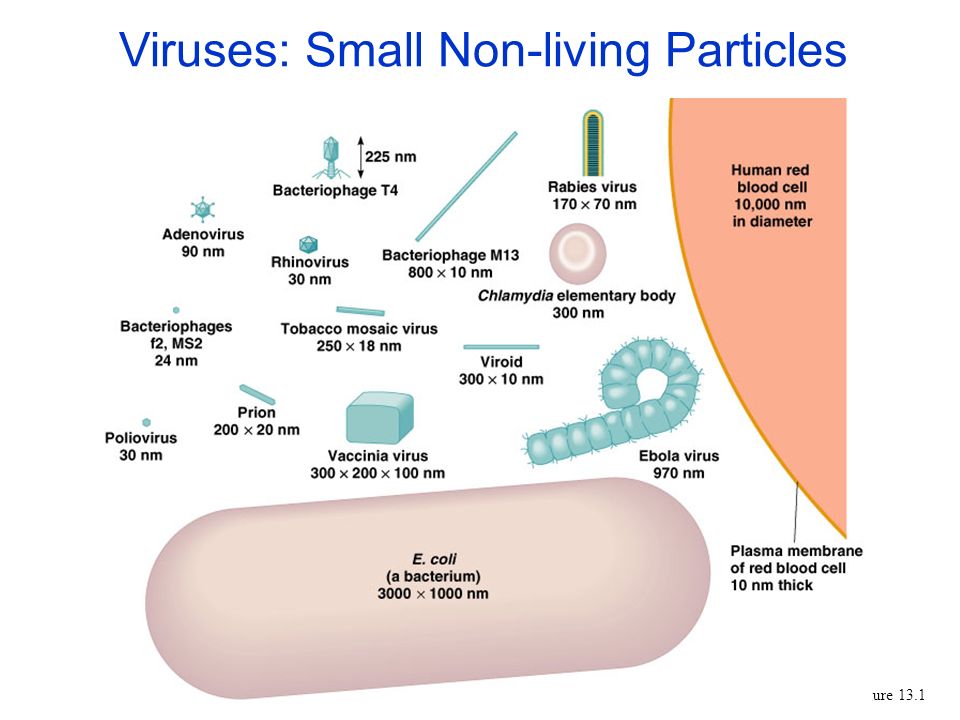
What is fetal heart monitoring?
Fetal heart rate monitoring measures the heart rate and rhythm of your baby (fetus). This lets your healthcare provider see how your baby is doing.
Your healthcare provider may do fetal heart monitoring during late pregnancy and labor. The average fetal heart rate is between 110 and 160 beats per minute. It can vary by 5 to 25 beats per minute. The fetal heart rate may change as your baby responds to conditions in your uterus. An abnormal fetal heart rate may mean that your baby is not getting enough oxygen or that there are other problems.
There are 2 ways to do fetal heart monitoring, external and internal:
External fetal heart monitoring
This method uses a device to listen to and record your baby’s heartbeat through your belly (abdomen). One type of monitor is a Doppler ultrasound device. It’s often used during prenatal visits to count the baby’s heart rate. It may also be used to check the fetal heart rate during labor. The healthcare provider may also check your baby’s heart rate continuously during labor and birth. To do this, the ultrasound probe (transducer) is fastened to your belly. It sends the sounds of your baby’s heart to a computer. The rate and pattern of your baby’s heart rate are shown on a screen and printed on paper.
Internal fetal heart monitoring
This method uses a thin wire (electrode) put on your baby’s scalp. The wire runs from the baby through your cervix. It is connected to the monitor. This method gives better readings because things like movement don’t affect it. But it can only be done if the fluid-filled sac that surrounds the baby during pregnancy (amniotic sac) has broken and the cervix is opened. Your provider may use internal monitoring when external monitoring is not giving a good reading. Or your provider may use this method to watch your baby more closely during labor.
During labor, your healthcare provider will watch your uterine contractions and your baby’s heart rate. Your provider will note how often you are having contractions and how long each lasts. Because the fetal heart rate and contractions are recorded at the same time, these results can be looked at together and compared.
Your provider will note how often you are having contractions and how long each lasts. Because the fetal heart rate and contractions are recorded at the same time, these results can be looked at together and compared.
Your provider may check the pressure inside your uterus while doing internal fetal heart monitoring. To do this, he or she will put a thin tube (catheter) through your cervix and into your uterus. The catheter will send uterine pressure readings to a monitor.
Why might I need fetal heart monitoring?
Fetal heart rate monitoring is especially helpful if you have a high-risk pregnancy. Your pregnancy is high risk if you have diabetes or high blood pressure. It is also high risk if your baby is not developing or growing as it should.
Fetal heart rate monitoring may be used to check how preterm labor medicines are affecting your baby. These are medicines are used to help keep labor from starting too early.
Fetal heart rate monitoring may be used in other tests, including:
- Nonstress test.
 This measures the fetal heart rate as your baby moves.
This measures the fetal heart rate as your baby moves. - Contraction stress test. This measures fetal heart rate along with uterine contractions. Contractions are started with medicine or other methods.
- A biophysical profile (BPP). This test combines a nonstress test with ultrasound.
Things that may affect the fetal heart rate during labor:
- Uterine contractions
- Pain medicines or anesthesia given to you during labor
- Tests done during labor
- Pushing during the second stage of labor
Your healthcare provider may have other reasons to use fetal heart rate monitoring.
What are the risks of fetal heart monitoring?
Radiation is not used for this test. The transducer usually causes no discomfort.
You may find the elastic belts that hold the transducers in place slightly uncomfortable. These can be readjusted as needed.
These can be readjusted as needed.
You must lie still during some types of fetal heart rate monitoring. You may need to stay in bed during labor.
With internal monitoring, you may have some slight discomfort when the electrode is put in your uterus.
Risks of internal monitoring include infection and bruising of your baby’s scalp or other body part.
Note: You should not have internal fetal heart rate monitoring if you are HIV positive. This is because you may pass the infection on to your baby.
You may have other risks depending on your specific health condition. Be sure to talk with your provider about any concerns you have before the procedure.
Certain things may make the results of fetal heart rate monitoring less accurate. These include:
- Obesity of the mother
- Position of the baby or mother
- Too much amniotic fluid (polyhydramnios)
- Cervix is not dilated or the amniotic sac is not broken.
 Both of these need to happen to do internal monitoring
Both of these need to happen to do internal monitoring
How do I get ready for fetal heart monitoring?
- Your healthcare provider will explain the procedure to you. Ask him or her any questions you have about the procedure.
- You may be asked to sign a consent form that gives permission to do the procedure. Read the form carefully and ask questions if anything is not clear.
- The consent form for fetal heart monitoring may be included as part of the general consent for labor and birth.
- Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, or anesthesia.
- If fetal heart rate monitoring is done along with another monitoring test, you may be asked to eat a meal before the test. This can help make your baby more active.
- The amniotic sac must be broken and your cervix must be dilated several centimeters before the internal device can be put in place.

- Follow any other instructions your provider gives you to get ready.
What happens during fetal heart monitoring?
You may have fetal heart rate monitoring in your healthcare provider's office or as part of a hospital stay. The way the test is done may vary depending on your condition and your healthcare provider's practices.
Generally, fetal heart rate monitoring follows this process:
External fetal heart monitoring
- Depending on the type of procedure, you may be asked to undress from the waist down. Or you may need to remove all of your clothes and wear a hospital gown.
- You will lie on your back on an exam table.
- The healthcare provider will put a clear gel on your abdomen.
- The provider will press the transducer against your skin. The provider will move it around until he or she finds the fetal heartbeat. You will be able to hear the sound of the fetal heart rate with Doppler or an electronic monitor.

- During labor, the provider may check the fetal heart rate at intervals or nonstop, based on your condition and the condition of your baby.
- For continuous electronic monitoring, the provider will connect the transducer to the monitor with a cable. A wide elastic belt will be put around you to hold the transducer in place.
- The provider will record the fetal heart rate. With continuous monitoring, the fetal heart pattern will be displayed on a computer screen and printed on paper.
- You may not be able to get out of bed with nonstop external fetal heart rate monitoring.
- Once the procedure is done, the provider will wipe off the gel.
Internal fetal heart monitoring
- You will be asked to remove your clothes and put on a hospital gown.
- You will lie on a labor bed. Your feet and legs will be supported as for a pelvic exam.

- Your healthcare provider will do a vaginal exam with a gloved hand to see how far you are dilated. This may be slightly uncomfortable.
- If the amniotic sac is still intact, your healthcare provider may break open the membranes with a tool. You will feel warm fluid coming out of your vagina.
- Your healthcare provider will feel the part of the baby at the cervical opening with gloved fingers. This is usually the baby’s head.
- The provider will put a thin tube (catheter) into your vagina. He or she will put a small wire at the end of the catheter on the baby’s scalp. He or she will gently turn it on the baby’s skin.
- The provider will remove the catheter and leave the wire in place on the baby’s scalp.
- The provider will connect the wire to a monitor cable. He or she will keep it in place with a band around your thigh.
- You may not be able to get out of bed with nonstop internal fetal heart rate monitoring.

- Once the baby is born, the provider will remove the wire.
What happens after fetal heart rate monitoring?
You do not need any special care after external fetal heart monitoring. You may go back to your normal diet and activity unless your healthcare provider tells you otherwise.
After internal fetal heart rate monitoring, your healthcare provider will check your baby’s scalp for infection, bruising, or a cut. The provider will clean the site with an antiseptic.
Your healthcare provider may give you other instructions, based on your situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure
What is fetal monitoring? Is continuous or intermittent monitoring best?
What is fetal monitoring?
Fetal monitoring is when your healthcare practitioner and nurse keep tabs on your baby's heart rate during labor. They do this to check how he's doing and see how he's tolerating your contractions.
They do this to check how he's doing and see how he's tolerating your contractions.
The monitoring is typically done with one of these devices:
- an electronic fetal monitor
- a handheld Doppler device (like the one your caregiver used to listen to your baby during your prenatal visits), or
- a stethoscope-like device called a fetoscope
Your health provider will check your baby's heart rate either continuously with an electronic fetal monitor, or periodically (this is called intermittent auscultation). Intermittent monitoring is done with an electronic fetal monitor, a handheld Doppler device, or a fetoscope.
If you have a high-risk pregnancy or are having your labor induced or augmented with medication, you'll likely be hooked up to an electronic fetal monitor continuously throughout labor. If your pregnancy is low-risk and you go into labor spontaneously, your baby's heart rate may only be monitored intermittently.
What is continuous external electronic fetal monitoring like?
An electronic device called a transducer that is attached to wide, stretchy bands will be placed around your abdomen. This device monitors your baby's heartbeat. Another device that tracks your contractions is usually attached to a second band around your abdomen.
This device monitors your baby's heartbeat. Another device that tracks your contractions is usually attached to a second band around your abdomen.
The transducers are connected to a machine near your bed that records this information on paper. You'll hear the galloping sound of your baby's heart if the monitor's volume is turned up. If you or your partner is interested, ask your nurse or practitioner how the machine works and how to tell when it registers a contraction.
Electronic fetal monitoring isn't painful. That said, some moms-to-be find it somewhat uncomfortable to have the transducers strapped to their belly during labor. Being tethered to a monitor can limit your movement and may make it harder for you to cope with contractions, too.
Some hospitals have devices that work wirelessly so you can walk around while you're being monitored. Ask your provider if this option is available at the place you’re planning to deliver.
How is periodic fetal monitoring (intermittent auscultation) done?
Your provider or labor nurse will hold the handheld Doppler device, external fetal monitor probe or fetoscope against your belly and listen to your baby's heartbeat, just as she did during prenatal visits. She'll also assess your contractions by laying her hands on your belly.
She'll also assess your contractions by laying her hands on your belly.
The nurse or provider will check your baby's heartbeat at specific intervals. This might happen every 15 to 30 minutes in the active phase of the first stage of labor, and every five to 15 minutes during the second (pushing) stage.
Here's what she'll be listening for:
- "Baseline" heart rate: This is your baby's heart rate between contractions when he's not moving (normal is between 110 and 160 beats per minute).
- Heart rate during and shortly after contractions: This will give your provider a sense of how your baby is tolerating labor.
In addition to the planned interval checks, your baby's heart rate will be evaluated as needed, such as when your water breaks. If your caregiver suspects a problem is developing, she'll check the heart rate more frequently. You may end up with electronic fetal monitoring for a time – or, if necessary, for the duration of your labor.
Which is better: Continuous fetal monitoring or intermittent auscultation?
For low-risk pregnancies, experts agree there's no need for continuous fetal monitoring. Periodic monitoring (intermittent auscultation) is just as effective.
A few studies have found that babies may be marginally safer when monitored continuously, but results are inconclusive. What's more, using continuous monitoring in low-risk pregnancies can increase the risk of false readings that lead to the mother undergoing unnecessary procedures.
Here's what studies show:
- Mixed results. One analysis of 13 randomized research trials showed that newborns were less likely to have seizures when monitored continuously rather than intermittently. But their Apgar scores were the same regardless of monitoring type, and the monitoring method did not influence babies' risk of death or long-term problems such as cerebral palsy.
- Questionable findings. A large study that looked at birth certificate records found that continuous electronic monitoring was associated with a lower rate of newborn deaths.
 However, more than a few experts have criticized this study because of problems with the quality of the data and factors, such as the length of each pregnancy, that were not taken into account, and which may have affected the results.
However, more than a few experts have criticized this study because of problems with the quality of the data and factors, such as the length of each pregnancy, that were not taken into account, and which may have affected the results. - False positives. With electronic monitoring. it's possible for readings to indicate a problem when the baby is actually fine. For the mother, continuous monitoring is associated with more deliveries by c-section and more assisted deliveries, using forceps and vacuum.
Why would I need continuous electronic fetal monitoring?
You'll have continuous electronic fetal monitoring if:
- You have pregnancy complications or develop any during labor
- You have a preexisting medical condition, such as chronic hypertension, diabetes or heart disease
- You get an epidural
- You require oxytocin (Pitocin) to induce or augment labor
Even if your pregnancy and labor are low risk, chances are high you'll receive continuous fetal monitoring. Intermittent auscultation is more labor intensive for hospital staff, so hospitals and practitioners generally prefer continuous fetal monitoring for all laboring women, regardless of risk factors.
Intermittent auscultation is more labor intensive for hospital staff, so hospitals and practitioners generally prefer continuous fetal monitoring for all laboring women, regardless of risk factors.
That said, if you have a low-risk pregnancy and no complications during labor, the American College of Obstetricians and Gynecologists considers intermittent auscultation an acceptable method. And it's the preferred method of the American College of Nurse-Midwives for women with no risk factors. That's because intermittent auscultation is associated with fewer c-sections and forceps and vacuum deliveries, and there's no proof that it makes any difference for the babies.
Can I ask for intermittent instead of continuous fetal monitoring?
Yes, if you're planning an unmedicated childbirth and don't have any high-risk conditions.
Discuss your preference with your practitioner. Find out ahead of time about her views, the hospital policy, and whether or not there's typically enough staff available for the intermittent checks. In most practices in which intermittent monitoring is an option, your provider may still want to connect you to the monitor for an initial 20- to 30-minute check when you're admitted to the hospital in labor.
In most practices in which intermittent monitoring is an option, your provider may still want to connect you to the monitor for an initial 20- to 30-minute check when you're admitted to the hospital in labor.
If you're laboring in a birth center or at home, you'll definitely be monitored intermittently. You'll have a caregiver with you at all times so the checks can be performed as frequently as needed. If you develop a condition that requires continuous monitoring, you'll need to be transferred to a hospital.
When is internal fetal monitoring used?
Your practitioner may do internal fetal heart rate monitoring if the external monitor isn't picking up well (which sometimes happens if you're moving around a lot or are obese) or she has concerns and wants a more accurate reading,.
An internal heart rate monitor is connected to a wire electrode that is inserted through your cervix and placed onto the part of your baby that is closest, usually the scalp.
Your practitioner may also decide to get more information about the strength of your contractions by inserting a special catheter-like gauge through your cervix for internal uterine monitoring.
What will my practitioner do if she has concerns about my baby's heart rate?
If your baby's heart rate is persistently flat, slow or fast your provider may try some simple interventions. These include:
- asking you to change your position
- giving you more fluids through an IV
- giving you supplemental oxygen.
Depending on your situation, other interventions may be necessary, too. These might include
- stopping oxytocin (Pitocin) if your labor is being induced or augmented;
- giving you medication to relax your uterus and decrease your contractions;
- if your membranes are ruptured, infusing sterile fluid into your uterus through a slender catheter to help cushion the umbilical cord from incidental pressure.
If your baby's heart rate continues to be questionable or takes a turn for the worse, and your practitioner is uncomfortable letting him stay in the birth canal any longer, you might have an assisted delivery if you’re already 10 centimeters dilated, or a c-section if delivery is not imminent.
Keep in mind that some dips in a baby's heart rate are normal. Also, certain heart rate changes are considered a sign of well-being. For example, when your baby moves, his heart rate should go up, just as yours does when you exercise.
Don't panic if you've been listening to the galloping of your baby's heartbeat and it suddenly stops. Most likely, the transducer on your belly has shifted out of place and lost contact with the heartbeat. Call the nurse so she can adjust it.
Throughout labor, your practitioner will evaluate your baby's heart rate frequently and watch for anything that could signal a problem. Even if someone is not present with you in your room, don't worry. Most hospitals have central monitoring where providers and nurses can watch fetal heart rates from afar.
advertisement | page continues below
Rating of baby monitors: the best for your baby
Compiling this rating, we tried to figure out: by what criterion to evaluate the quality of the device? Why would all mothers unanimously recognize one baby monitor as good and another not?
It turned out that such a rating is impossible, because all parents have different needs. Therefore, we will make our rating based on the functionality of the devices.
Therefore, we will make our rating based on the functionality of the devices.
No device performs worse or better: brands that produce baby monitors monitor the excellent quality of the devices. But there are differences in price and functionality. We will start with the richest device in terms of functions - and end up with the most inexpensive one. So you will choose the best baby monitor for yourself.
- Ramili Baby RA300SP2 with advanced breathing monitor. The breath monitor is a sensitive sensory "mat" that fits under the baby's mattress and notifies parents in the event of a breathing failure. The baby monitor has a long range of 650 m. This is twice as long as usual. The picture is completed by all the possible functions that can be imagined: they are described on the product page. On our website you will find the lowest price for this baby monitor in Russia.
- The next is the same Ramili Baby RA300 in a lightweight form: without breathing monitors. It should be noted that this baby monitor can be equipped with additional devices of your choice.
 One example of this is connecting two child units to one parent unit. Now, if the parents have two children, there is no need to buy a second baby monitor.
One example of this is connecting two child units to one parent unit. Now, if the parents have two children, there is no need to buy a second baby monitor. - Baby Monitor Switel BCC58. Its functionality includes a reception range of up to 300 meters, two-way radio communication, mains or battery operation, LCD display with all important indications, sound level adjustment and microphone sensitivity, voice activation, air temperature measurement with alarm, MAXI ECOmode no radiation mode, night light , five melodic lullabies, a parent unit search function, and other useful features.
- Switel BCC38 made in Switzerland has a completely different format: the parent and child units are made in the form of two full-fledged walkie-talkies. They are equipped with an interference suppression system, which guarantees a stable connection and no failures. The features of the device are the reception range up to 300 meters, automatic voice activation, digital one-way communication; light indication of the volume of crying and the signal level between the blocks, operation from the mains or AAA batteries.

- We have come to the most budget model - Motorola MBP140. She is simple and reliable. It has a range of 300 m, has a night light, two-way communication, a rechargeable battery, a highly sensitive speaker and some other pluses.
There are many dozens of other models of baby monitors, but these walkie-talkies are the most popular in their price ranges and, again, perfectly protect the baby's sleep without failures and shortcomings. Look at their looks, features, compare them to your needs and budget and you will be able to make the right choice.
We would be happy to advise you. Call!
%d1%80%d0%b0%d0%b4%d0%b8%d0%be%d0%bd%d1%8f%d0%bd%d1%8f - doctors and pharmacies of Nizhny Novgorod
| Mamrosenko Hello, how can I get to the Healthy Krasnodar clinic https://czm-krasnodar.ru/? answers 0 |
| Lyudmila Hello! How can you make an appointment with a plastic surgeon? After the accident, the girl has a small .  .. .. answers 0 |
| Irina We need medical help, we can’t cope at home. My leg hurts, an 83-year-old woman suffered covid in December 2020 at home. They did an ultrasound ... answers 0 |
| Alena Good afternoon! I have a positive analysis for HPV 16. I pierced injections of Allokin-Alpha subcutaneously 6 pcs. Husband has analysis ... answers 0 |
| Maria Call 89154394959 Maria |
| RADUGA | RADUUGA | RADUUGA | RADUUGA , especially when I go out into the street, in unfamiliar companies ... answers 1 |