How long do baby ear infections last
8 Common Signs of Ear Infection in Babies
At Tenet Healthcare, we want to provide you with tips for healthy living to ensure you live a long, pain-free life.
An ear infection or otitis media (OM) happens when the middle ear, or the space behind the eardrum and the eustachian tube, becomes inflamed due to virus or bacteria build-up. This may be triggered by a cold, an allergy, acid reflux or a throat infection.
Anyone may have an ear infection, but it’s more common in children than in adults. In fact, the National Institute on Deafness and Other Communication Disorders (NIDCD) says that five out of six children suffer from an ear infection before turning three. Children have smaller and narrower eustachian tubes, so it’s easier for viruses and bacteria to find their way into their ears. This is also why their ears get blocked and become swollen faster than adults do.
How Long Does an Ear Infection Last?
Ear infections may last from two to three days, even without medicine or any form of treatment. However, more severe cases of ear infections may last longer, usually six weeks or longer even after taking antibiotics.
What Are the Common Signs of Ear Infection in Babies?
The following signs may indicate that your baby has an ear infection:
- crying more than usual
- ear pain
- fever
- fluid or pus coming out of the ear
- having a hard time eating or drinking
- irritability
- pulling or rubbing the ear often
- sleeping difficulties
How Do Doctors Diagnose Ear Infections?
While most cases of an ear infection are not severe, we recommend that you see a pediatrician as soon as you see signs of an ear infection in your child, rather than wait for it to get worse. To be able to diagnose your child’s condition, the doctor may conduct a physical exam and use an otoscope, a device similar to a flashlight, to check the baby’s eardrum. The doctor may also ask you some questions to learn about the frequency and duration of your baby’s ear infection, any potential risk factors and more.
The doctor may also ask you some questions to learn about the frequency and duration of your baby’s ear infection, any potential risk factors and more.
What Are the Treatment Options for Ear Infection in Babies?
Once confirmed that your baby has an ear infection, the doctor may advise any of the following treatment options:
- Antibiotics
- Ear drops
- Ear tube surgery (for more severe cases)
How Can You Prevent Ear Infections in Children?
You can do several things to help lower your child’s risk of developing an ear infection, such as
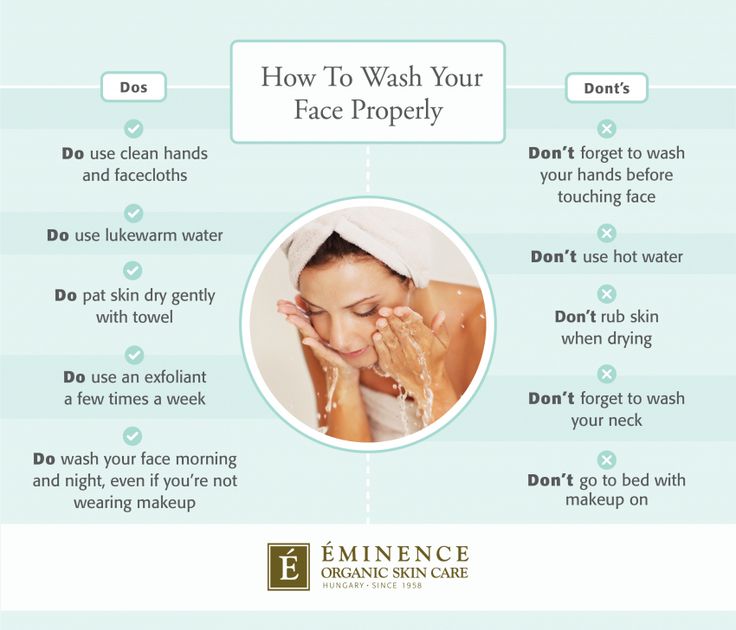
- Observing good hygiene, including washing your and your baby’s hands regularly and sanitizing your home
- Keeping your child away from other kids who have a cold
- Protecting your child against secondhand smoking
- Breastfeeding your baby during his/her first year
- Practicing proper bottle positioning (if you are bottle feeding your baby) to keep the milk from flowing into the eustachian tubes
- Getting vaccinations for meningitis, influenza and pneumonia
Final Thoughts
Ear infections may lead to more serious health issues and complications when left untreated. These may include loss of hearing, a cyst in the middle ear, a drainage from a hole in the eardrums, hardening of some tissues in the ear, facial paralysis, brain inflammation and damage to the bones in the middle ear. Please seek professional help as soon as you see signs of an ear infection in your baby to prevent greater health risks from affecting your child’s quality of life. Your child deserves a healthy and physical pain-free life, and we’re here to help. Your child’s safe care is our #1 priority.
These may include loss of hearing, a cyst in the middle ear, a drainage from a hole in the eardrums, hardening of some tissues in the ear, facial paralysis, brain inflammation and damage to the bones in the middle ear. Please seek professional help as soon as you see signs of an ear infection in your baby to prevent greater health risks from affecting your child’s quality of life. Your child deserves a healthy and physical pain-free life, and we’re here to help. Your child’s safe care is our #1 priority.
Sources:
National Institute of Deafness and Other Communication Disorders
KidsHealth
Harvard Health Publishing
Healthline
Ear Infections in Babies and Toddlers
Featured Expert:
Ear infections in babies and toddlers are extremely common. In fact, according to the National Institutes of Health, five out of six children will experience an ear infection before their third birthday.
"Many parents are concerned that an ear infection will affect their child's hearing irreversibly—or that an ear infection will go undetected and untreated," says David Tunkel, M.D., Johns Hopkins Medicine pediatric otolaryngologist (ENT). "The good news is that most ear infections go away on their own, and those that don't are typically easy to treat."
Childhood Ear Infections Explained
Ear infections happen when there is inflammation— usually from trapped bacteria—in the middle ear, the part of the ear connects to the back of the nose and throat. The most common type of ear infection is otitis media, which results when fluid builds up behind the eardrum and parts of the middle ear become infected and swollen.
If your child has a sore throat, cold, or an upper respiratory infection, bacteria can spread to the middle ear through the eustachian tubes (the channels that connect the middle ear to the throat). In response to the infection, fluid builds up behind the eardrum.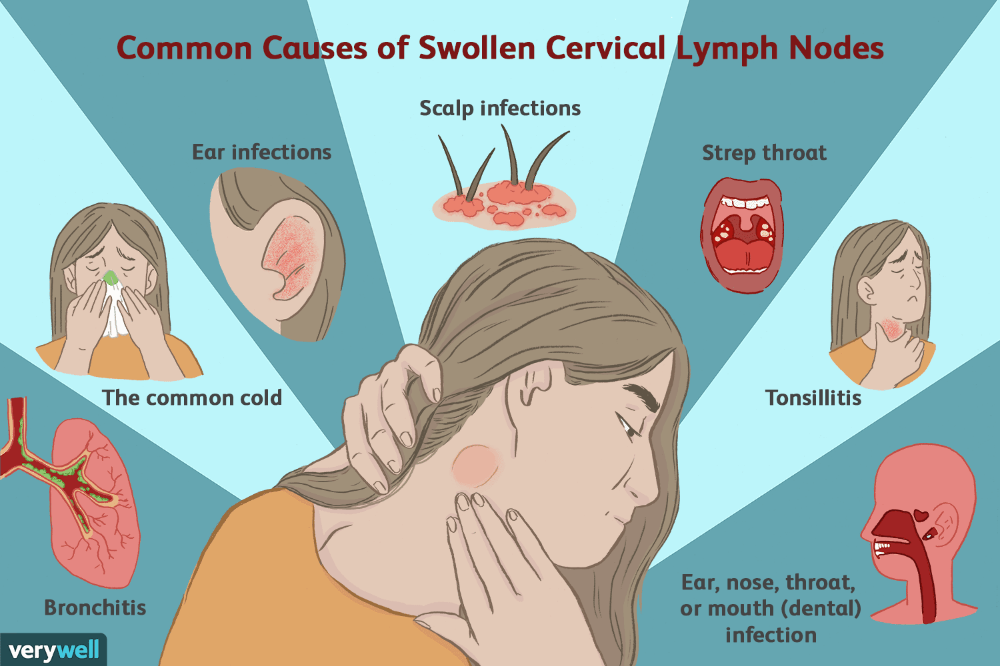
Children are more likely to suffer from ear infections than adults for two reasons:
- Their immune systems are underdeveloped and less equipped to fight off infections.
- Their eustachian tubes are smaller and more horizontal, which makes it more difficult for fluid to drain out of the ear.
"In some cases, fluid remains trapped in the middle ear for a long time, or returns repeatedly, even when there's no infection," Tunkel explains.
Ear Infection Signs and Symptoms
The telltale sign of an ear infection is pain in and around the ear. Young children can develop ear infections before they are old enough to talk. That means parents are often left guessing why their child appears to be suffering. When your child can't say "my ear hurts," the following signs suggest an ear infection could be the culprit:
- Tugging or pulling the ear
- Crying and irritability
- Difficulty sleeping
- Fever, especially in younger children
- Fluid draining from the ear
- Loss of balance
- Difficulty hearing or responding to auditory cues
Signs that require immediate attention include high fever, severe pain, or bloody or pus-like discharge from the ears.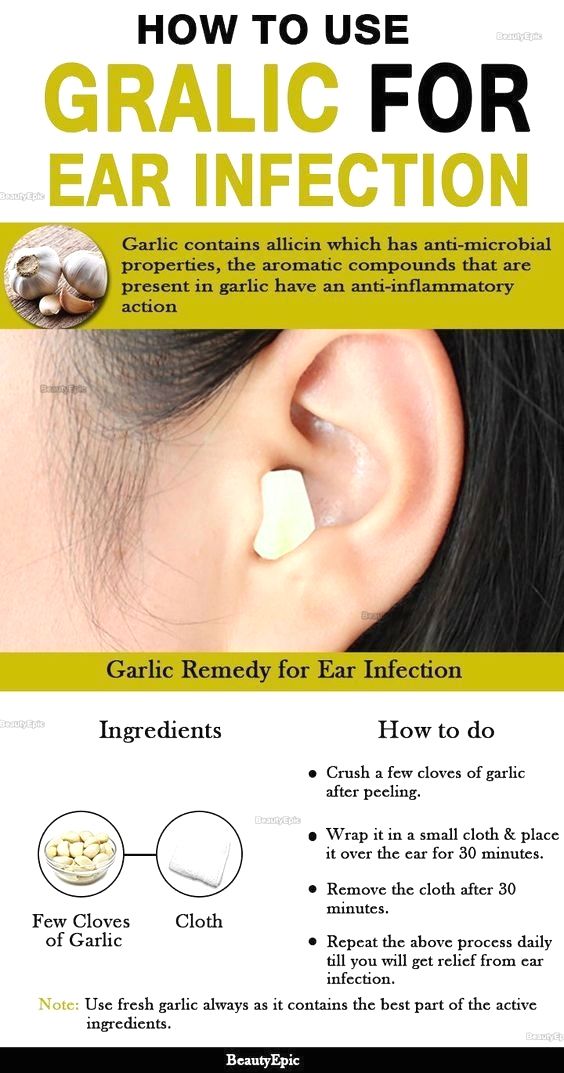
Pediatric Otolaryngology
Our pediatric otolaryngologists provide compassionate and comprehensive care for children with common and rare ear, nose, and throat conditions. As part of the Johns Hopkins Children's Center, you have access to all the specialized resources of a children's hospital.
Learn more about Pediatric Otolaryngology
Ear Infection Treatments
Most ear infections go away without treatment. "If your child isn't in severe pain, your doctor may suggest a 'wait-and-see' approach coupled with over-the-counter pain relievers to see if the infection clears on its own," Tunkel says.
The reason: Treating an infection with antibiotics may cause the bacteria causing the infections to become resistant to those antibiotics—and that makes treating future infections more difficult. Equally important, in most cases antibiotics aren't necessary. Otitis media tends to get better without them. While you may be tempted to treat your child's ear infection with homeopathic or natural medicine, Tunkel warns they aren’t well studied.
Otitis media tends to get better without them. While you may be tempted to treat your child's ear infection with homeopathic or natural medicine, Tunkel warns they aren’t well studied.
Your best bet is to work with your child's health care provider to determine the appropriate course of action. In nearly every case, treatment decisions depend on the child’s age, degree of pain and presenting symptoms.
Under 6 months
Babies under six months almost always receive antibiotics. At this age, children are not fully vaccinated. Equally important, there's no research about the safety of skipping antibiotics for babies under 6 months of age — and complications from ear infections can be more severe when they occur in young babies. Bacteria trapped behind the eardrum can spread to other parts of the body and cause serious infections.
6 months to 2 years
For children between the ages of 6 months and 2 years, the American Academy of Pediatrics (AAP) recommends shared decision-making between parents and providers about whether to treat ear infections that are not severe. The best course is often to watch the child for two to three days before prescribing antibiotic treatment. If the child is in pain, or the ear infection is advanced, your child's doctor may suggest immediate antibiotic treatment.
The best course is often to watch the child for two to three days before prescribing antibiotic treatment. If the child is in pain, or the ear infection is advanced, your child's doctor may suggest immediate antibiotic treatment.
Over 2 years
With children over the age of 2, ear infections that are not severe are likely to clear on their own, without treatment. "In the meantime, you can treat pain with over-the-counter medications, such as ibuprofen or acetaminophen," Tunkel says. If there's no improvement after two to three days, antibiotics may be warranted.
Unfortunately, some children suffer from recurrent ear infections, sometimes up to five or six a year. Kids who get repeated infections may benefit from a surgical procedure where doctors insert small tubes in the eardrums to improve air flow and prevent fluid buildup. "Tubes don't prevent all ear infections, but they make managing them significantly easier," Tunkel explains.
Ear Infection Prevention
There are several steps you can take to reduce your child's risk of developing ear infections, including:
- Vaccinate your child: Children who are up-to-date on their vaccines get fewer ear infections than their unvaccinated counterparts.
 The 13-valent pneumococcal conjugate vaccine (PCV13) protects against 13 types of infection-causing bacteria.
The 13-valent pneumococcal conjugate vaccine (PCV13) protects against 13 types of infection-causing bacteria. - Consider breastfeeding: Breast milk contains antibodies that may help reduce the risk of ear infections and a host of other ailments. Whether you feed milk or formula, make sure your child sits up during feedings to prevent fluid from flowing into the middle ear.
- Wash your hands frequently: The best way to protect your child against cold and flu is to keep your hands clean. Wash your hands with soap and water and scrub them clean for a full 20 seconds each time you visit the sink.
- Steer clear of sick people: Don't allow your child to spend time with children or adults who are sick.
- Avoid secondhand smoke: Studies show that children who are exposed to secondhand smoke are up to three times more likely to develop ear infections than those who don't have those exposures.

Whether your child has ear infections or not, it's important to ensure they're able to hear well. "No child is too young to have a hearing test," Tunkel says. "We use a variety of techniques to test infant hearing and we can identify a hearing problem even in newborns."
Ear inflammation in a child: how to prevent complications
Otitis is one of the most common diseases in childhood. According to international statistics, 98% of children suffer from ear inflammation at least once, 60% experience the disease twice. What is effective prevention and how otitis is treated, said the otorhinolaryngologist of the Morozov Children's Hospital, Candidate of Medical Sciences, holder of the status of "Moscow Doctor" Alexander Mikhailovich Ivanenko.
Why does otitis occur?
Depending on the location of the inflammatory process, otitis can be external, medial or internal. Otitis externa is caused by microbes and fungi, most often manifested by damage to the skin of the ear canal and boils in the auricle.
Acute otitis media is an acute inflammation of the mucous membrane of the middle ear cavity. It develops against the background of respiratory infections. Ear infection occurs through the auditory tube, when mucus from the nasopharynx enters the middle ear and viruses, bacteria, fungal flora freely penetrate from the nasopharynx through the mouth of the auditory tube into the tympanic cavity.
Due to anatomical features, the smaller the child, the shorter and wider the auditory tube connecting the ear cavity with the nasopharynx. Therefore, in an infant who spends most of his time lying down, and in a younger child who does not know how to clean his nose, mucus can flow at any time. In adolescence, the auditory tube is a tortuous narrow tube, so the infection from the nasopharynx to the middle ear is less likely to pass.
Adenoid vegetations also contribute to the development of ear inflammation. This is the growth of the nasopharyngeal tonsil, which is the main focus of bacterial infection in the nasopharynx.
How does the disease manifest itself?
The main symptom of otitis media is pain in the ear. Children under one year old, as a rule, refuse to eat, because sucking movements cause pain. Babies often touch their ears, rub them, and cry. You can suspect otitis media by pressing on the tragus of the child's auricle.
The key method for diagnosing otitis media is otoscopy - an examination by a doctor of the external auditory canal and eardrum using a special instrument.
How to treat otitis?
If the inflammatory process is at the initial stage, outpatient treatment is carried out. The therapy is selected by a pediatrician or an otorhinolaryngologist depending on the child's condition. Be sure to use vasoconstrictor drops in the nose.
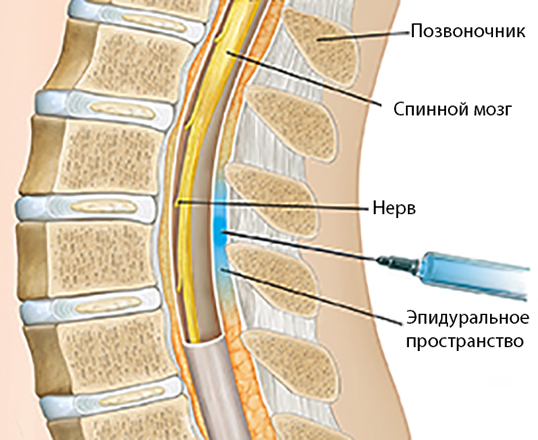
If medical assistance is not provided in a timely manner, the inflammatory process turns into acute catarrhal otitis media, and then into acute purulent otitis media, characterized by the appearance of purulent discharge from the ear. In some cases, with inadequate outflow of contents or its absence, the child in the hospital undergoes paracentesis - an incision in the eardrum. The intervention is performed under anesthesia. Then medical conservative treatment continues.
In some cases, with inadequate outflow of contents or its absence, the child in the hospital undergoes paracentesis - an incision in the eardrum. The intervention is performed under anesthesia. Then medical conservative treatment continues.
Which preventive measures are most effective?
There is an opinion among many parents that otitis media can be prevented by “covering the ears with cotton wool in the street” or “putting a few hats on the child”. Such recommendations will not insure against otitis media.
Due to the fact that ear infection occurs through the auditory tube that communicates with the nasopharynx, it is necessary to carefully care for the nasal cavity if the child has a runny nose. Otherwise, mucus flows from the nasopharynx into the middle ear, which leads to an inflammatory process in the ear.
In case of excessive growth of the nasopharyngeal tonsil, its removal is recommended.
Otitis media in a child - symptoms and treatment of otitis media 2019.

Otitis media is the medical name for inflammation of the middle ear caused by infection wide ear canal than older children or adults). Acute otitis media is an infection that usually develops due to the accumulation of fluid in the middle ear. Otitis can be caused by viruses or bacteria. Most children with otitis media first develop an acute respiratory viral infection or acute respiratory disease, which then progresses to otitis media, causing inflammation and swelling in the nasal passages and the Eustachian tube. The risk of recurrent middle ear infections is increased in children who:
- Attending a nursery or kindergarten
- Exposed to cigarette or stove smoke in the home
- Have enlarged adenoids that may obstruct the drainage of the Eustachian tube
Symptoms of acute otitis media usually include ear pain and fever. Otitis media with effusion (fluid or pus), also known as adhesive otitis media, occurs when there is fluid in the middle ear after the infection has cleared. This condition usually does not cause pain, but it can cause hearing loss in a child.
This condition usually does not cause pain, but it can cause hearing loss in a child.
Children with acute otitis media usually get better quickly with anti-inflammatory medication and proper care. Sometimes, if the doctor is sure that the disease is caused by bacteria, the child may be given antibiotics. Children who develop adhesive otitis media and other complications may need additional treatment with physical therapy.
Otitis media symptoms in children
Most children with acute otitis media will complain of ear pain. If the child is still small and does not know how to speak, otitis may be indicated by a long aching cry, the child's refusal to breastfeed. Other symptoms may include:
- Irritability, capriciousness
- "forced" position (if the pain is on one side, the child can put his hand to the ear or try to lie on the sore ear)
- Lethargy, weakness
- sleep disorders
- fever
- decreased or lack of appetite
- vomiting
Because many cases of otitis media are caused by a viral infection, other symptoms associated with the infection, such as runny nose, watery eyes, or cough, can often be present.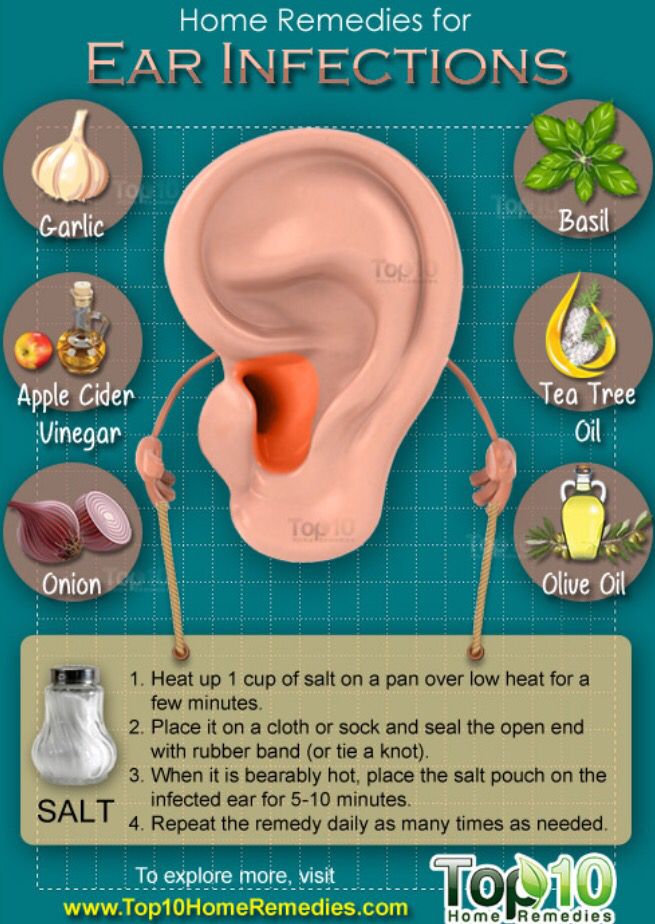
Diagnosis of otitis media
If your child has an earache for more than 2 days, or if your child is under 2 years old and you suspect that he or she has an earache, you should urgently seek help from an otolaryngologist, pediatrician or general practitioner. practices. Delay can threaten the fact that the child will lose his hearing or become completely deaf.
The doctor will examine the child's ears and eardrums with an instrument called an otoscope. In acute otitis media, the eardrum will be inflamed and bulging due to a buildup of fluid in the middle ear. The doctor will take the temperature and examine the child for other infections (such as bronchitis). There are no specific tests to diagnose otitis media. One of the effective diagnostic methods is ENT endoscopy using a flexible ENT endoscope, which is successfully carried out in our medical center by experienced ENT doctors. Such diagnostics are absolutely painless and can be performed according to the doctor's indications in the youngest children, from the age of 9months.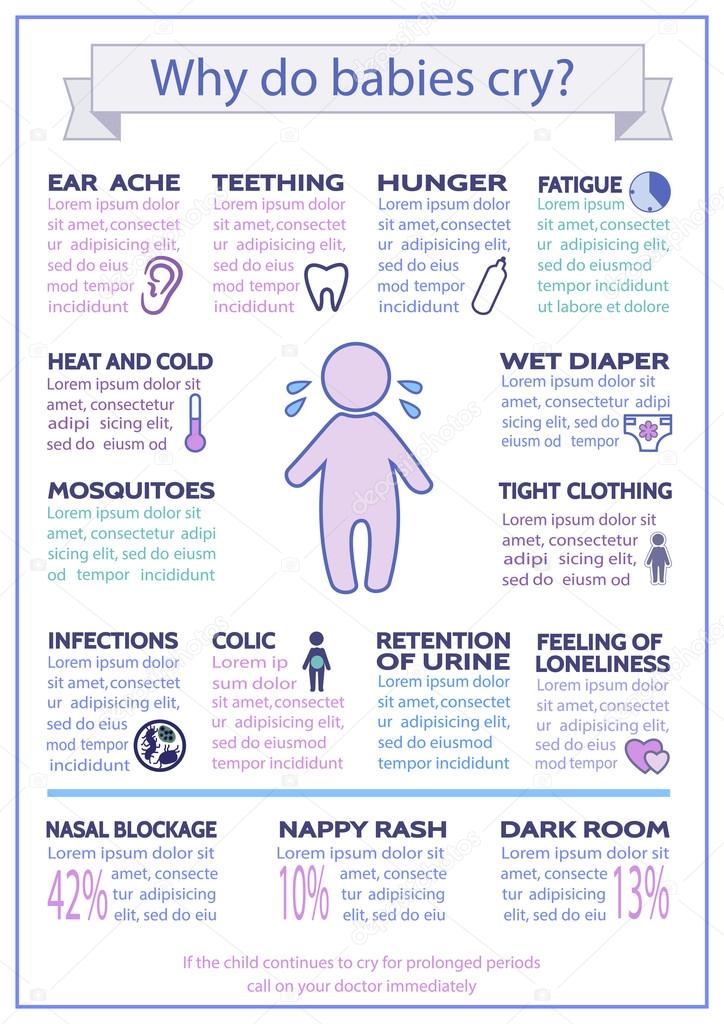
Treatment for otitis media
Treatment for a child will depend on their age and health.
It is generally assumed that children over 6 months of age who have mild otitis media are initially given only anti-inflammatory drugs. If symptoms persist for more than 48 hours or if they worsen, then broad-spectrum antibiotics may be needed. it is extremely important to prevent complications of the disease in any way. The first antibiotic of choice for the treatment of acute otitis media in children is amoxicillin. An alternative antibiotic will be given if the child is allergic to penicillin. Antihistamines and corticosteroids have not been shown to be of any benefit in the treatment of acute otitis media.
Possible complications
Perforation (rupture) of the eardrum is a common complication of acute otitis media in children. This can lead to leakage of fluid from the ear, while fluid or pus begins to flow from the middle ear cavity, which alleviates the child's condition: pain in the ear decreases due to reduced pressure on the eardrum. By itself, the rupture of the eardrum does not lead to deafness; in the process of treating otitis media, the integrity of the membrane is quickly restored. Treatment is the same as for acute otitis media. The child should not be immersed in water or go to the pool until the eardrum is healed.
By itself, the rupture of the eardrum does not lead to deafness; in the process of treating otitis media, the integrity of the membrane is quickly restored. Treatment is the same as for acute otitis media. The child should not be immersed in water or go to the pool until the eardrum is healed.
Otitis media sometimes develops after an acute ear infection. This means that there is fluid in the middle ear (otitis media with effusion), which can cause temporary hearing loss. Most children with this complication recover within 3 months without the need for special treatment. In the chronic form of the disease, treatment with a tympanostomy may be required - inserting a small drainage tube into the eardrum to drain fluid and allow air into the middle ear to restore hearing.
Chronic suppurative otitis media is a middle ear infection with perforation of the tympanic membrane and discharge of fluid from the ear that lasts at least 6 weeks.