Anus during pregnancy
Causes, in Pregnancy, Home Remedies, Treatment
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Overview
Anus pain is known as proctalgia and can have many causes. The anus is where your large intestine opens into your buttocks at the rectum. The anus is the last passageway of the gastrointestinal (GI) tract.
The anus is surrounded by muscles known as sphincter muscles. These tighten and relax the anus when you pass waste. Your tailbone (coccyx), the last bone in your spine, and many nerves are also near your anus.
Read on to learn what causes anus pain, how you can treat it at home, what medical treatments are available, and how you can help prevent this type of pain.
Anal pain can have a variety of causes.
1. Sitting for a long time
Sitting down for a long time, especially on a hard surface, can cause temporary anal pain by putting pressure on anal nerves and muscles. Even sitting for a short time on a hard surface can cause anal pain that lasts for hours after you get up.
You don’t need to see your doctor for this kind of pain.
If the pain persists for a few days after a long period of sitting, see your doctor. They can diagnose any injury to your anus muscles, tailbone, or the surrounding structures.
2. Diarrhea
Diarrhea happens when you pass watery, loose stool more than three times in a day. Diarrhea can have many causes, such as dietary changes (being dehydrated or not eating enough fiber), and infections like gastroenteritis, colitis, or diverticulitis.
Frequently passing stool can make your anus sore. This can get worse from wiping or cleaning. Your anal tissue can become raw and bleed, too.
Other diarrhea symptoms include:
- feeling bloated or gassy
- cramping in your lower abdomen
- feeling nauseous
- not being able to hold in your stool
Diarrhea often goes away on its own. Seek emergency medical attention if you have any of the following symptoms, though:
Seek emergency medical attention if you have any of the following symptoms, though:
- diarrhea for more than two days
- fever
- blood in your stool
- black or discolored stool
- loss of consciousness
3. Injury
Falling on your butt can injure the muscles, bones, or nerves around the anus. The sudden impact of a hard surface can bruise or damage your skin, muscles, or nerve endings as well as potentially fracture bones.
This type of injury is most common during activities like contact sports, such as football and soccer, or activities like skateboarding, rollerblading, or gymnastics.
Depending on how severe the injury is, pain may radiate up from your anus to your lower back and feel like a constant ache or throb. You may notice bruises on your buttocks.
Seek immediate medical attention if:
- the pain is sharp and constant
- you can’t walk or get up without severe pain
- you lose sensation in your lower back or in one or both legs
4.
 Fissures
FissuresAnal fissures happen when your anal tissues tear. Passing especially hard or large stool is the most common culprit. The pain is often sudden and sharp at first. Your anus may ache for hours or days afterward until the fissure heals.
Symptoms of an anal fissure include:
- feeling sudden, unusual pain in or around your anus when you pass stool
- bleeding from your anus, especially when you wipe
- pain that lasts for hours after you pass stool
Fissures don’t always require immediate medical treatment. See your doctor if the pain persists or gets significantly worse when you sit down, pass stool, or walk.
5. Hemorrhoids
Hemorrhoids happen when anal blood vessels are swollen. Straining to pass stool or being constipated are often the causes of hemorrhoids.
When you have a hemorrhoid, you may feel a lump near your anus. The pain may be generally dull but sharp when you sit down. You may not feel comfortable sitting without a special cushion or pillow. In some cases, you may not notice any symptoms.
In some cases, you may not notice any symptoms.
Common symptoms of hemorrhoids include:
- constant pain, soreness, or itching around your anus
- bleeding from your anus when you pass stool
- sharp anal pain if blood in the hemorrhoid becomes clotted
Hemorrhoids can go away on their own, but severe hemorrhoids may require medical treatment. See your doctor right away if you:
- have trouble passing stool
- can’t sit without sharp or severe pain
- notice blood in your stool
6. Menstruation
Menstruation can cause anal pain along with other symptoms related to your digestive tract.
Your rectum and anus may be more sensitive during this time. This can make your anus feel tender, sore, or uncomfortable. Common period symptoms, such as diarrhea and bloating, can make anal pain even more pronounced.
You don’t need to see your doctor to treat these symptoms. They usually go away once your period is over.
7. Anal spasms (proctalgia fugax)
Anal spasms happen when you get sharp, unexpected anal pain due to anal sphincter muscle contractions. It’s relatively common. A 2013 review estimates it affects between 8 and 18 percent of people.
The cause of this condition isn’t well known. It’s more likely to occur if you have irritable bowel syndrome (IBS) or anxiety as well as after hemorrhoid surgery or a hysterectomy.
When you’re pregnant, your uterus becomes enlarged, which puts pressure on your anus. That can lead to discomfort or pain. This extra pressure can also cause hemorrhoids, which can make your anus uncomfortable.
Anal pain during pregnancy is most common during the third trimester, when your baby is larger and may put more pressure on your anal nerves. Contractions during labor can also cause pain in your anus.
In many cases, you should be able to treat anal pain at home. Here are some home remedies to try:
- Take a sitz bath.
 Buy a sitz bath at your local drugstore or online and mount it in your toilet bowl. Fill it with warm water and Epsom salt, then sit on top of the sitz bath with the water immersing your anus. Soak for 15 to 20 minutes.
Buy a sitz bath at your local drugstore or online and mount it in your toilet bowl. Fill it with warm water and Epsom salt, then sit on top of the sitz bath with the water immersing your anus. Soak for 15 to 20 minutes. - Use over-the-counter (OTC) creams or ointments. Apply a small amount of cream or ointment, such as lidocaine or cortisone, to reduce pain and speed up the healing process of irritated skin.
- Use a cold compress. You can make your own cold compress at home by wrapping an ice pack or bag of frozen vegetables in a towel. Press it against your anal area to help relieve pain. Do this 20 minutes at a time, three to four times daily.
- Take OTC pain medicine for pain relief. Ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) can temporarily relieve anal pain until any cuts or injuries heal.
Seek emergency medical treatment if:
- Your anal pain makes you unable to walk, pass waste, stand, or sit.

- You notice blood in your stool.
- You have a fever.
- You’re severely dehydrated.
- You can’t eat or pass stool.
Medical treatment depends on the cause of pain and the severity of your symptoms.
Treatment for injuries
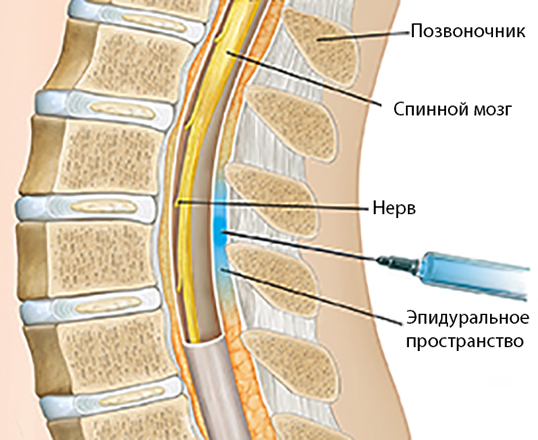
You may need X-rays or other imaging tests to see the extent of any damage to your tailbone or spine. Severe spinal injuries may require surgery or long-term rehabilitation to restore any lost mobility.
Treatment for diarrhea
If you’re severely dehydrated, you may need intravenous fluids (IV) to replenish your body fluids. If a bowel disorder is causing diarrhea, such as IBS or Crohn’s disease, your doctor may prescribe you medication or a treatment plan to help reduce symptoms.
Treatment for a fissures
Chronic anal fissures may require surgery so that you can pass stool without injuring your sphincter muscles. Your doctor may also recommend adding fiber to your diet to help you pass stool more easily.
Treatment for hemorrhoids
Your doctor may wrap the hemorrhoid with a rubber band until it shrinks. Surgery to cut or freeze the hemorrhoid are also possible treatment options. In severe cases, your doctor may need to remove the hemorrhoid tissues and blood vessels in a hemorrhoidectomy procedure.
It may not always be possible to prevent anal pain. But there are things you can do to reduce your risk:
- Stay hydrated. Drink at least 64 ounces of water per day to make your stool easier to pass.
- Sit with good posture. When sitting,straighten your back and keep your knees bent at a 90-degree angle.
- Get up and walk around at least once every 30 to 50 minutes. This reduces long-term pressure on muscles and nerves in your anus and lower spine.
- Don’t strain when you pass stool. Straining can cause discomfort, hemorrhoids, and anal fissures.
- Eat a healthy diet.
 Eat plenty of fiber so that you regularly pass stool and prevent constipation.
Eat plenty of fiber so that you regularly pass stool and prevent constipation. - Wear loose, breathable underwear. Wear 100 percent cotton underwear to prevent your anus from becoming moist with sweat, which could lead to irritation.
- Consider using moist wipes or jets of water instead of toilet paper. Toilet paper can scratch and cut your anal skin, making you more prone to infections. Moist wipes and bidets are gentler on your skin.
- Don’t eat raw, uncooked, or untrustworthy food. Food and unfiltered water can contain bacteria or other microbes that can lead to diarrhea. Make sure your food is properly cooked and that your water is clean.
Many things can lead to anal pain, some serious and others not.
If the pain is bearable and starts to fade quickly after it starts, there’s no need for concern. If pain persists for more than a few days and accompanies other painful or disruptive symptoms, see your doctor for immediate treatment.
Hemorrhoids During Pregnancy: Causes and Prevention
Hemorrhoids — swollen veins in the anus and rectum — are common during pregnancy, especially in the third trimester when the enlarged uterus puts pressure on the veins.
Hemorrhoids can be painful. They may also itch, sting, or bleed, especially during or after a bowel movement.
While your body is going through all sorts of physical changes during pregnancy, hemorrhoids can be one more unwanted irritation. But the good news is that they generally aren’t harmful to your health or the health of your baby, and they’re usually a short-term problem. Though pushing during labor can worsen hemorrhoids, they typically go away on their own after you give birth. (1)
Some women get hemorrhoids for the first time when they’re pregnant. But if you’ve had hemorrhoids before, you’re more likely to get them again when you’re pregnant.
What Can Cause Hemorrhoids During Pregnancy
As your unborn baby grows, your uterus gets bigger and begins to press against your pelvis. This growth puts a lot of pressure on the veins near your anus and rectum, and these veins may become swollen and painful as a result.
This growth puts a lot of pressure on the veins near your anus and rectum, and these veins may become swollen and painful as a result.
The increase in the hormone progesterone during pregnancy can also contribute to the development of hemorrhoids, as it relaxes the walls of your veins, making them more prone to swelling. An increase in blood volume, which enlarges veins, can also contribute to hemorrhoids during pregnancy. (1)
Three common additional causes of hemorrhoids during pregnancy include:
- Straining during bowel movements
- Straining from carrying extra pregnancy weight
- Sitting or standing for long periods of time
Hemorrhoids are most common in pregnant women who experience constipation.
As many as 38 percent of pregnant women become constipated at some point during their pregnancy, according to research published in the journal BMJ Clinical Evidence. (2)
One cause of constipation during pregnancy may be when the growing uterus pushes against the bowel. Iron supplements you may take can also contribute to constipation, so it’s worth trying to get the iron you need naturally through your diet. (3)
Iron supplements you may take can also contribute to constipation, so it’s worth trying to get the iron you need naturally through your diet. (3)
Pregnancy hormones can also slow down the movement of food through the digestive tract, making constipation more likely.
How to Prevent Hemorrhoids During Pregnancy
Avoiding constipation is key to preventing hemorrhoids during pregnancy. Here are some tips for preventing constipation:
Eat lots of high-fiber foods. There are plenty of good ways to incorporate more fiber into your diet. Fiber-filled foods include fruits like pears (especially when you include the skin), avocados, and berries; vegetables such as broccoli, artichokes, and Brussels sprouts; whole grains such as oatmeal, brown rice, quinoa, and even popcorn; legumes including various kinds of beans, lentils, and green peas; and don’t forget nuts and seeds.
RELATED: 11 High-Fiber Foods to Add to Your Diet
Drink plenty of fluids. Aim for 10 8-ounce glasses of water each day.
Aim for 10 8-ounce glasses of water each day.
Use the toilet as soon as you feel the urge. “Holding it in” can contribute to constipation.
Try not to sit or stand for long periods of time. If you sit down at work, make sure to get up and walk around for a few minutes every hour. At home, try to rest on your side when reading or watching TV, to relieve downward pressure on your rectal veins.
Ask your doctor about using a stool softener. This can help if other methods fail to ease your constipation. Using laxative pills for constipation is not recommended during pregnancy, as they can cause dehydration and might stimulate uterine contractions. (3)
Do Kegel exercises daily. Kegel exercises strengthen the pelvic floor muscles that help support your rectum and can improve circulation in the rectal area. You can do Kegel exercises just about anywhere — at home, in your car, at the office — but first you need to make sure you’re isolating and contracting the correct muscles.
Identify the right muscles by stopping urination midstream. (This is strictly for the purpose of identifying which muscles we’re talking about — you don’t want to do Kegels while urinating, as this could increase your risk for a urinary tract infection). (4)
Once you know which muscles to use, tighten them and hold the contraction for five seconds. Then relax for five seconds. Work up to holding the contraction for 10 seconds. Try to do at least three sets of 10 reps a day.
RELATED: 10 Foods to Help Relieve Constipation
RELATED: Constipation Causes, Symptoms, and Relief
How to Treat Hemorrhoids During Pregnancy
Hemorrhoids usually get better on their own after pregnancy, but there are a number of things you can do to ease any itching and pain in the meantime:
Soak your rectal area in warm water several times a day. A sitz bath, or small basin that fits over the toilet seat, can help. These devices can be purchased at most drug stores. You can also fill your regular bathtub with a few inches of warm water to create a similar effect.
These devices can be purchased at most drug stores. You can also fill your regular bathtub with a few inches of warm water to create a similar effect.
Apply ice packs or cold compresses to the area several times a day. The cold can reduce swelling and help relieve pain.
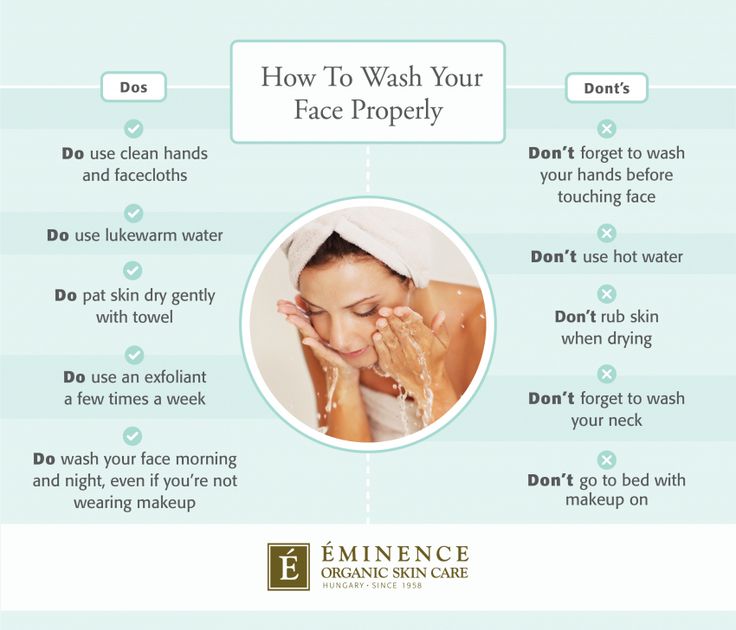
Keep the anus clean and dry. Try using moist towelettes or baby wipes to gently clean the area after bowel movements. This can be more gentle than dry toilet paper.
Be sure to pat — not wipe — the area dry after bathing or making a bowel movement. Excess moisture can cause irritation.
Apply baking soda (wet or dry) to the area to alleviate itching. (3)
Apply treatments containing witch hazel. Products like Tucks Medicated Cooling Pads can help keep the area clean and relieve pain and itching around the anus.
But before you use any products, be sure to ask your doctor or healthcare provider to recommend a topical hemorrhoid cream or medicated wipe that’s safe to take during your pregnancy.
Additional reporting by Deborah Shapiro.
Treatment for Hemorrhoids
Most hemorrhoids can be treated at home or with simple medical procedures.
By Lindsey Konkel
What Are Hemorrhoids? Symptoms, Causes, Diagnosis, Treatment, and Prevention
By Lindsey Konkel8 Myths You’ve Been Told About Hemorrhoids
By Mikel TheobaldAbdominal Pain: Is It Appendicitis or Something Else?
Several conditions can cause pain in the lower right abdomen, and they can be difficult to distinguish from the symptoms of appendicitis pain.
By Joseph Bennington-Castro
What Happens to Your Health When You Aren’t Treated for Hepatitis C
Although medication can cure hepatitis C, millions of people aren’t taking it. Problem is, if the virus isn’t treated, it can cause serious health complications...
Problem is, if the virus isn’t treated, it can cause serious health complications...
By Jennifer Acosta Scott
Signs, symptoms and causes of hemorrhoids in pregnant women - NEARMEDIC network of clinics
Dear patients, we apologize. Callback is temporarily unavailable. Call our telephone numbers.
The main causes of hemorrhoids in pregnant women may be as follows:
- Chronic constipation. In this case, the stretching and tension of the walls of the rectum increases during defecation, which leads to the formation of hemorrhoids. In pregnant women, constipation occurs much more often due to a decrease in intestinal tone.
- Inactive lifestyle. With hypodynamia, blood stagnation occurs in the venous plexus of the rectum, which eventually leads to vein thrombosis and the formation of hemorrhoids. Features of the condition do not always allow pregnant women to be mobile, therefore they have a high risk of developing this disease.

- Violation of blood circulation in the lower half of the body. During pregnancy, the uterus grows and compresses the inferior vena cava. This leads to stagnation of blood in the veins of the legs and rectum. During childbirth, a woman's intra-abdominal pressure rises greatly - this can cause hemorrhoids after pregnancy.
Signs of hemorrhoids in pregnant women
The longer the period, the higher the likelihood of developing the disease. Most often, hemorrhoids appear in the 3rd trimester or after childbirth.
The blood vessels of the hemorrhoidal plexus of the rectum gradually dilate. Over longer periods, the stretching of the veins becomes even stronger. With the expansion of the walls of the veins of the rectum, they lose their elasticity. This provokes protrusion of the veins under the mucous membrane.
If hemorrhoids protrude only into the lumen of the rectum and do not come out of the anus, then we are talking about the treatment of hemorrhoids of the 1st stage. The farther, the larger the knots become and the more they sag from the anus. In the second stage of hemorrhoids, the nodes sag from the anus, but are easily set back on their own. The third stage occurs when the nodes can no longer cope back.
The farther, the larger the knots become and the more they sag from the anus. In the second stage of hemorrhoids, the nodes sag from the anus, but are easily set back on their own. The third stage occurs when the nodes can no longer cope back.
The symptoms of the disease depend on its stage.
- Internal hemorrhoids. Symptoms are mild, there is no sagging of hemorrhoids from the anus. At this stage, women may experience pain during bowel movements, slight bleeding or fresh blood in the stool, and itching and discomfort in the anus.
- External hemorrhoids. The main symptom is the sagging of one or more purple-red nodes from the anus. This manifestation is the main sign of what is required, and not of another disease, such as anal fissure. Walking, sitting and defecation in this case become extremely painful.
Urgent medical assistance is required in case of infringement of the hemorrhoid - a pregnant woman experiences very severe pain in the anus with fever.
Treatment of hemorrhoids during pregnancy
If a woman already has any symptoms of hemorrhoids - itching, pain in the anus, bleeding from the anus, etc. - professional treatment is required.
At NEARMEDIC, the first stage of treatment is the preventive measures described above, which stop the progression of the disease. Then the woman is prescribed drugs, both local and systemic. But due to pregnancy, local therapy is preferable, as this reduces the risk of side effects, increases the effectiveness of treatment and reduces the negative effects of drugs on the child. In any case, the medicine is prescribed only by the attending physician who observes the woman during pregnancy.
In the case when a woman already has prolapsed nodes that cannot be set, an operation is prescribed. Other indications for surgical intervention are infringement or necrosis of the hemorrhoid, as well as acute inflammation. Most often, in NEARMEDIC surgery is postponed until the postpartum period, and during pregnancy they are limited to conservative treatment.
Prevention of hemorrhoids during pregnancy
Due to the fact that all pregnant women are at high risk of developing hemorrhoids, NEARMEDIC clinic doctors strongly recommend that preventive measures be taken throughout pregnancy, without waiting for symptoms to appear.
- Elimination of constipation. To do this, you need to adjust your diet: eat more foods that contain coarse vegetable fiber - vegetables, fruits, cereals, cereals, prunes. Dairy products also have a beneficial effect on digestion. On the contrary, it is better to refuse meat and other foods rich in protein. As well as from an excess of fat, coffee and hot spices.
- Hygiene. It is recommended to wash the perineum and anus after each act of defecation. In addition, once a day you can take sitz baths with antiseptics: chamomile infusion, a weak solution of potassium permanganate, etc.
Doctors
Who treat hemorrhoids during pregnancy
More doctorsClinics in Moscow
For all questions, you can contact the single contact center: +7 (495) 6-171-171
Pregnancy hemorrhoids | TS Clinic — Krasnodar
If you periodically or regularly feel:
- itching, burning
- pain in the region of the anus, in the rectum.
 May be during or after defecation
May be during or after defecation - discomfort in the rectum
- blood: in stool or on toilet paper
- sensation of incomplete bowel movement or foreign body in the anus
The presence of these symptoms may indicate serious pathologies, including cancer. Treatment of hemorrhoids and rectal fissures in the initial stages will allow treatment with minimally invasive methods and avoid a serious surgical operation.
Pregnancy is a wonderful but difficult time in a woman's life. In connection with the development of the fetus and placenta in the mother's body, there are significant changes in the function of all the most important organs and systems, which are aimed at creating optimal conditions for the growth and development of the child.
Pregnancy from the very first day is accompanied by endocrine changes in the mother, affecting all spheres of her life.
Therefore, "start" to the development of hemorrhoids is not the day of birth, but the first day of pregnancy!
The heart functions during pregnancy with an increased load due to the expansion of peripheral vessels, an increase in the volume of circulating blood, the development of the uteroplacental circulation, a progressive increase in the body weight of a pregnant woman, etc. Compression of the iliac veins (due to an enlarged uterus) contributes to venous stasis in the small pelvis and legs and increases the risk of venous thrombosis. Also, during pregnancy, there is a significant (up to 150-200%) increase in the content of plasma coagulation factors.
Compression of the iliac veins (due to an enlarged uterus) contributes to venous stasis in the small pelvis and legs and increases the risk of venous thrombosis. Also, during pregnancy, there is a significant (up to 150-200%) increase in the content of plasma coagulation factors.
HEMORRHOIS (Greek haimorrhois bleeding; obsolete kidney) - dilation of the cavernous veins (calf) of the distal (final) section of the rectum and anus.
First, the venules increase in volume, their walls thicken, then a hemorrhoid is gradually formed.
In women, external hemorrhoids are more often detected, which she can detect on her own in the form of "swellings" in the anus. They are most noticeable and pronounced after emptying and in the evening. If at the same time the pregnant woman does not experience pain and there is no discharge of blood from the rectum, then there is no cause for concern.
Further, hemorrhoids can increase in size, and blood clots form in the lumen of the vessels due to stagnation, due to which the nodes become more dense and painful.