How to treat earache in a child
What's the Best Ear Infection Treatment for Kids?
Five tips to help relieve ear infection symptoms at home
Five tips to help relieve ear infection symptoms at home
If your little one is cranky, unusually fussy and tugging at his or her ear or is feverish and having difficulty sleeping, chances are it may be due to an ear infection.
Ear infections in children often go away on their own or in some cases with antibiotic treatment. The challenge for many parents is knowing what to do, what to watch for and when to call their pediatrician.
Five out of six children experience an ear infection by the time they are 3 years old, according to the National Institutes of Health. The odds are that your child will have an ear infection before kindergarten.
What causes an ear infection?
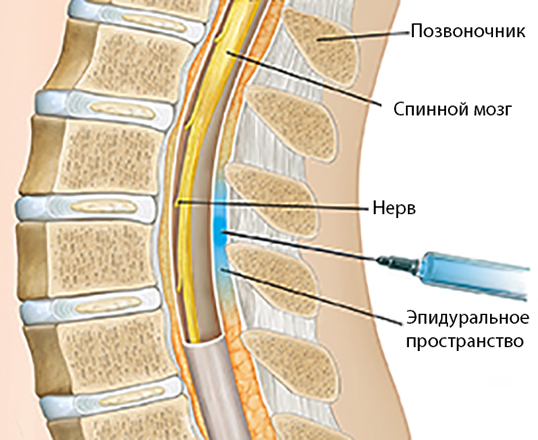
Ear infections can be caused by either bacteria or a virus, often following a cold. The common cold can cause the middle ear to become inflamed and fluid to build up behind the eardrum. The Eustachian tube, which connects the ears, nose and throat, can also become swollen.
“Children are more susceptible to ear infections than adults because they have shorter and narrower Eustachian tubes, and it is easier for germs to reach the middle ear and for fluid to get trapped there,” says Kara Hutton, MD, a pediatrician at Scripps Clinic Rancho Bernardo. “Babies and children also have weaker immune systems, so it is more difficult for their bodies to fight an infection.”
The onset of ear infections is often on day three of a cold. Ear infections peak at age 6 months to 2 years, and are a common problem until age 8, according to the American Academy of Pediatrics.
What is the best treatment for ear infection?
Some ear infections require antibiotic treatment, but many can get better without this medicine.
If you suspect your child has an ear infection, your pediatrician can diagnose it and determine the appropriate treatment.
“Common ear infections often do not require antibiotics, except in severe cases or in infants younger than six months,” says Dr. Hutton. “Many ear infections will resolve on their own within a week.”
Hutton. “Many ear infections will resolve on their own within a week.”
For mild cases, your doctor might recommend watchful waiting to give your child’s immune system time to fight off the infection or delayed antibiotic prescribing, which gives you time to see if your child is still sick before filling it.
Five tips for ear infection treatment at home
Even when antibiotics are prescribed, they won’t take effect for 24 to 48 hours. Your child need not suffer needlessly. There are simple, effective ways to reduce your child’s discomfort and pain during an ear infection.
1. Fever and pain medicine: based it on age, consult with doctor
Over-the-counter medications can help reduce pain and fever in your child. Based it on age and weight and consult with your pediatrician if necessary.
Read labels and instructions carefully when giving fever-reducing medications. “It’s very important to follow instructions and give the appropriate dosage according to your child’s weight and age,” says Dr. Hutton.
Hutton.
- For children younger than 6 months, give only acetaminophen, such as Tylenol.
- For children older than 6 months, you may give also give an ibuprofen product, such as Advil, for fever and pain.
- Infants younger than 3 months old who have a fever need immediate medical attention even if they appear well and show no other signs of being ill.
- Do not give aspirin to children because it can cause Reye’s syndrome, a rare but very serious illness that harms the liver and brain, according to the Centers for Disease Control and Prevention (CDC).
2. Place a cold pack or warm compress over your child’s ear
Put a cold wet washcloth on the outer ear for 20 minutes to help with pain until the pain medicine starts to work.
Some children prefer a warm compress to help alleviate pain. Use a warm washcloth and apply until it becomes cool. “Make sure that the compress is only warm, not hot,” says Dr. Hutton.
3. Keep child hydrated
Make sure to keep your child well hydrated. Give lots of cold fluids.
Give lots of cold fluids.
4. Elevate your child’s head
“Keeping your child’s head elevated can ease some of the pressure,” says Dr. Hutton.
If your child is older than 2 and no longer sleeps in a crib, use a pillow, but never use a pillow with an infant. You can keep an infant upright in a car seat to alleviate pressure.
5. Watch for ear discharge
Pus discharge can be normal with an ear infection. Most often, this heals after the ear infection is treated. Wipe the discharge away. Careful not to plug the ear with cotton as retained pus can cause an infection of the lining of the ear canal.
When to call your doctor
Pediatricians recommend calling your doctor if:
- Fever lasts more than two days on antibiotics
- Ear pain becomes severe or crying becomes nonstop
- Ear pain lasts more than three days on antibiotics
- Ear discharge is not better after three days on antibiotics
- Your child becomes worse
Talk with your pediatrician if your child suffers recurrent ear infections, especially if you have a family history of allergies and asthma
Preventing ear infections
While you can’t fend off every germ, there are steps you can take to reduce the risk of an ear infection, including by:
- Breastfeeding your infant to pass along immunities
- Avoiding secondhand smoke
- Washing your hands
- Keeping immunizations up to date
Earache - NHS
Earache and ear pain is common, particularly in young children. It can be painful, but is not usually a sign of anything serious.
It can be painful, but is not usually a sign of anything serious.
How long earache lasts
It depends on what's causing it. Most earaches in children are caused by an ear infection, which usually start to improve after a few days.
Spotting earache in babies and young children
A young child might have earache if they:
- rub or pull their ear
- do not react to some sounds
- have a temperature of 38C or above
- are irritable or restless
- are off their food
- keep losing their balance
Earache and ear pain can affect 1 or both ears.
How to treat earache yourself
There are some things you can do to help relieve earache and ear pain.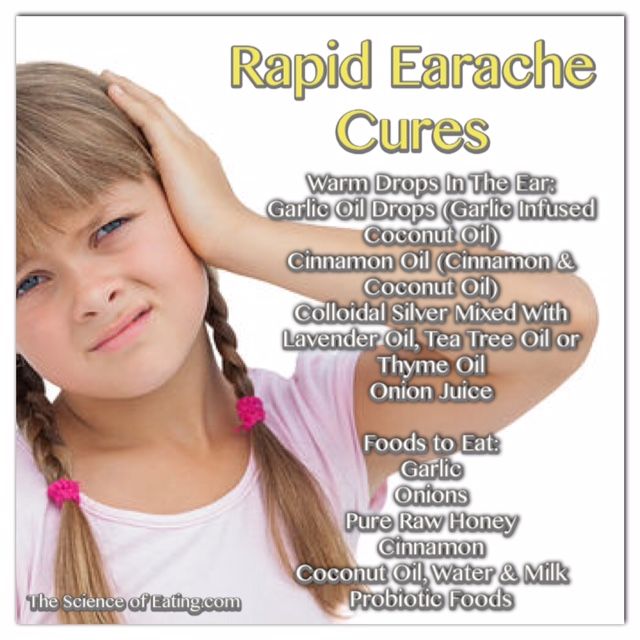
Don’t
-
do not put anything inside your ear, such as cotton buds
-
do not try to remove earwax
-
do not let water get inside your ear
A pharmacist can help with earaches
A pharmacist might be able to tell you:
- what you can do to treat earache yourself
- if you can buy anything to help (for example, eardrops)
- if you need to see a GP
Non-urgent advice: See a GP if you or your child:
- have earache for more than 3 days
- keep getting earache
Urgent advice: Ask for an urgent GP appointment or get help from NHS 111 if:
You or your child have earache and:
- become generally unwell
- a very high temperature or feel hot and shivery
- swelling around the ear
- fluid coming from the ear
- hearing loss or a change in hearing
- something stuck in the ear
- your child is under 2 and has earache in both ears
You can call 111 or get help from 111 online.
What causes earache and pain
Earache and pain can be caused by many things, but sometimes it's not known by what.
Here are some of the most common causes:
| Symptoms | Possible condition |
|---|---|
| Ear pain with toothache | Children teething, dental abscess |
| Ear pain with change in hearing | Glue ear, earwax build-up, an object stuck in the ear (do not try to remove it yourself – see a GP), perforated eardrum (particularly after a loud noise or accident) |
| Ear pain with pain when swallowing | Sore throat, tonsillitis, quinsy (a complication of tonsillitis) |
| Ear pain with a fever | Ear infection, flu, cold |
Page last reviewed: 29 April 2022
Next review due: 29 April 2025
Otitis in a child: symptoms, first aid
Children often get ARVI. Most infections pass quickly due to the protective functions of the baby's body, proper care, as well as adequate treatment. However, in some cases SARS occur with complications. Otitis media is one of the most common complications of viral respiratory infections in children. This is facilitated by the features of the anatomical structure in young children - a short, wide and more horizontal auditory tube, which connects the nasopharyngeal cavity and the middle ear, which means that the infection can easily penetrate from the nasopharynx. Otitis can cause infectious diseases such as measles, rubella. Sometimes it happens that frequent profuse regurgitation of the baby becomes the cause of otitis media, while the remnants of food can enter the middle ear through the auditory tube and cause inflammation. The cause of repeated otitis often becomes adenoiditis.
Most infections pass quickly due to the protective functions of the baby's body, proper care, as well as adequate treatment. However, in some cases SARS occur with complications. Otitis media is one of the most common complications of viral respiratory infections in children. This is facilitated by the features of the anatomical structure in young children - a short, wide and more horizontal auditory tube, which connects the nasopharyngeal cavity and the middle ear, which means that the infection can easily penetrate from the nasopharynx. Otitis can cause infectious diseases such as measles, rubella. Sometimes it happens that frequent profuse regurgitation of the baby becomes the cause of otitis media, while the remnants of food can enter the middle ear through the auditory tube and cause inflammation. The cause of repeated otitis often becomes adenoiditis.
How otitis media manifests itself
In young children, the onset is usually sudden, with a sharp pain in the ear. Older children may complain of hearing loss. Pain in the ear may be accompanied by a rise in temperature up to 40 0 C. It is more difficult to suspect otitis in infants, because. they can't complain about the pain. Parents may suspect otitis in a baby by the following signs:
Older children may complain of hearing loss. Pain in the ear may be accompanied by a rise in temperature up to 40 0 C. It is more difficult to suspect otitis in infants, because. they can't complain about the pain. Parents may suspect otitis in a baby by the following signs:
- Crying, crying.
- Anxiety, capriciousness, sleep disturbances, refusal of the breast.
- Attempts to finger the ear, rolling the head on the pillow.
- Increased screaming and crying when pressing on the tragus of the ear.
Discharge from the ear is another sign of otitis media. They can be serous or purulent, have an admixture of blood. Discharge from the ears with otitis occurs as a result of perforation (rupture) of the eardrum. Lack of treatment for this condition can lead to a persistent hearing loss in a baby, which once again confirms the need for immediate medical attention at the first sign of otitis media.
Treatment of otitis media and first aid
Treatment of otitis media must be prescribed by a physician. No need to get involved in treatment without an examination by an otorhinolaryngologist. Usually otitis is treated with antibiotics, the course of treatment is 7-10 days. The toilet of the external auditory canal, the restoration of the patency of the Eustachian tube and the normalization of pressure in the tympanic cavity, local and general anti-inflammatory therapy, antibiotic therapy are among the main areas of treatment for otitis media. In some cases, the patient is shown paracentesis - a therapeutic puncture of the eardrum. Again, please note that only a doctor can prescribe specific drugs for your child.
No need to get involved in treatment without an examination by an otorhinolaryngologist. Usually otitis is treated with antibiotics, the course of treatment is 7-10 days. The toilet of the external auditory canal, the restoration of the patency of the Eustachian tube and the normalization of pressure in the tympanic cavity, local and general anti-inflammatory therapy, antibiotic therapy are among the main areas of treatment for otitis media. In some cases, the patient is shown paracentesis - a therapeutic puncture of the eardrum. Again, please note that only a doctor can prescribe specific drugs for your child.
Help at home:
The use of vasoconstrictor nasal drops is an essential component of the treatment of otitis media. These drugs restore the patency of the auditory tube, which helps to normalize the pressure in the tympanic cavity.
- Put vasoconstrictor drops in your child's nose. Choose a drug that you have already taken.
- For fever and/or severe pain, give your child an age-appropriate antipyretic. Paracetamol and ibuprofen preparations effectively relieve pain in otitis media.
- Place with otitis indicated dry heat. It is enough to put on a hat or a scarf that covers the ears. Do not use hot compresses or heating pads unless directed by a doctor. Remember! Any thermal procedures are CONTRAINDICATED for suppuration and elevated temperature.
- if a purulent or serous fluid is discharged from the ear, remove it with a cotton turunda soaked in a 3% hydrogen peroxide solution.
Prophylaxis
It is necessary to treat the nose, nasopharynx and pharynx in time in children. This is especially true for enlarged adenoids. If the child is breathing heavily through his nose, sleeping with his mouth open, snoring, you need to contact an ENT doctor. If the doctor insists on removing the adenoids, consider and agree to this procedure. Treat other viral and bacterial diseases in a timely manner. For infants, the best prevention of otitis media is breastfeeding.
Treat other viral and bacterial diseases in a timely manner. For infants, the best prevention of otitis media is breastfeeding.
The following tips for caring for a child with SARS will help you reduce your chances of developing otitis media:
- Never force your child to blow his nose. When you blow your nose, mucus enters the Eustachian tubes, which directly contributes to the development of otitis media.
- The Eustachian tube is usually blocked by thick mucus. Therefore, try to keep the child's mucus liquid during SARS. To do this, as much of it as possible, and also maintain the optimal temperature in the apartment (no higher than 21 0 C) and humidity (60%).
- use antipyretics in the age dosage when the baby's body temperature rises above 38.5 0 C. Fever increases fluid loss and promotes drying of the mucous membranes. Therefore, its timely relief is also the prevention of otitis media.
Otorhinolaryngologist Korzun Irina Valerievna
Ear inflammation in a child: how to prevent complications
Otitis is one of the most common diseases in childhood. According to international statistics, 98% of children suffer from ear inflammation at least once, 60% experience the disease twice. What is effective prevention and how otitis is treated, said the otorhinolaryngologist of the Morozov Children's Hospital, Candidate of Medical Sciences, holder of the status of "Moscow Doctor" Alexander Mikhailovich Ivanenko.
According to international statistics, 98% of children suffer from ear inflammation at least once, 60% experience the disease twice. What is effective prevention and how otitis is treated, said the otorhinolaryngologist of the Morozov Children's Hospital, Candidate of Medical Sciences, holder of the status of "Moscow Doctor" Alexander Mikhailovich Ivanenko.
Why does otitis occur?
Depending on the location of the inflammatory process, otitis can be external, medial or internal. Otitis externa is caused by microbes and fungi, most often manifested by damage to the skin of the ear canal and boils in the auricle.
Acute otitis media is an acute inflammation of the mucous membrane of the middle ear cavity. It develops against the background of respiratory infections. Ear infection occurs through the auditory tube, when mucus from the nasopharynx enters the middle ear and viruses, bacteria, fungal flora freely penetrate from the nasopharynx through the mouth of the auditory tube into the tympanic cavity.
Due to anatomical features, the smaller the child, the shorter and wider the auditory tube connecting the ear cavity with the nasopharynx. Therefore, in an infant who spends most of his time lying down, and in a younger child who does not know how to clean his nose, mucus can flow at any time. In adolescence, the auditory tube is a tortuous narrow tube, so the infection from the nasopharynx to the middle ear is less likely to pass.
Adenoid vegetations also contribute to the development of ear inflammation. This is the growth of the nasopharyngeal tonsil, which is the main focus of bacterial infection in the nasopharynx.
How does the disease manifest itself?
The main symptom of otitis media is pain in the ear. Children under one year old, as a rule, refuse to eat, because sucking movements cause pain. Babies often touch their ears, rub them, and cry. You can suspect otitis media by pressing on the tragus of the child's auricle.
The key method for diagnosing otitis media is otoscopy - an examination by a doctor of the external auditory canal and eardrum using a special instrument.
How to treat otitis?
If the inflammatory process is at the initial stage, outpatient treatment is carried out. The therapy is selected by a pediatrician or an otorhinolaryngologist depending on the child's condition. Be sure to use vasoconstrictor drops in the nose.
If medical assistance is not provided in a timely manner, the inflammatory process turns into acute catarrhal otitis media, and then into acute purulent otitis media, characterized by the appearance of purulent discharge from the ear. In some cases, with inadequate outflow of contents or its absence, the child in the hospital undergoes paracentesis - an incision in the eardrum. The intervention is performed under anesthesia. Then medical conservative treatment continues.
Which preventive measures are most effective?
There is an opinion among many parents that otitis media can be prevented by “covering the ear with cotton wool in the street” or “putting a few hats on the child”.