How long does an epidural last during labor
Epidurals: Meaning and Side Effects of Anesthesia During Labor
An epidural is the most common type of anesthetic used for pain relief during labor. Here’s what you should know before having an epidural, including information that dispels some common myths.
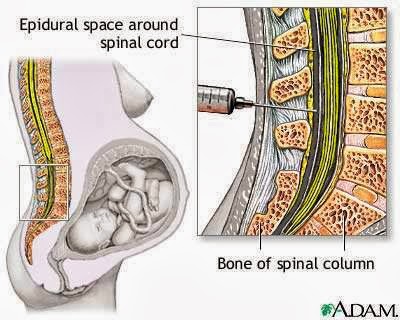
How and when is an epidural for labor pain administered?If you choose to have an epidural, an anesthesiologist will insert a needle and a tiny tube, called a catheter, in the lower part of your back. The needle is removed and the catheter left in place for delivery of the medication through the tube as needed. You can begin an epidural at any time during your labor — in the beginning, in the middle, or even toward the end — in consultation with your physician.
Does it hurt when the epidural is administered?The anesthesiologist will numb the area where the epidural is administered, which may cause a momentary stinging or burning sensation. But because of this numbing, there is very little pain associated with an epidural injection. Instead, most patients will feel some pressure as the needle is inserted.
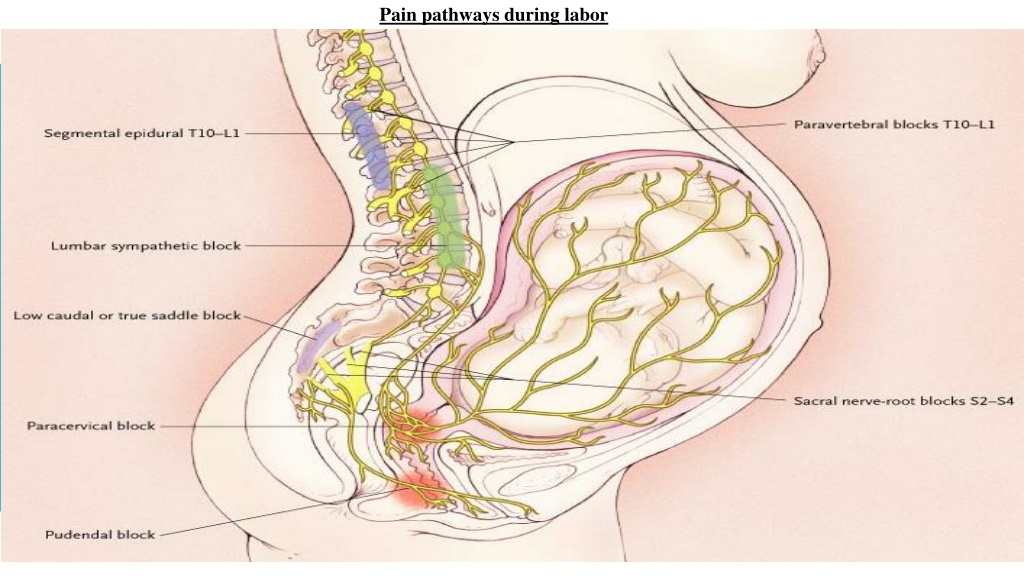
An epidural provides anesthesia that creates a band of numbness from your bellybutton to your upper legs. It allows you to be awake and alert throughout labor, as well as to feel pressure. The ability to feel second-stage labor pressure enables you to push when it’s time to give birth to your baby. It can take about 15 minutes for the pain medication to work.
How long does the pain relief last?You can continue to receive pain relief through an epidural for as long as you need it. The amount of medication you receive through the epidural can be increased or decreased as necessary.
Can an epidural slow labor or lead to a cesarean delivery (C-section)?There is no credible evidence that it does either. When a woman needs a C-section, other factors usually are at play, including the size or position of the baby or slow progression of labor due to other issues. With an epidural, you might be able to feel contractions — they just won’t hurt — and you’ll be able to push effectively. There is some evidence that epidurals can speed the first stage of labor by allowing the mother to relax.
With an epidural, you might be able to feel contractions — they just won’t hurt — and you’ll be able to push effectively. There is some evidence that epidurals can speed the first stage of labor by allowing the mother to relax.
The amount of medication that reaches the baby from the epidural is very small, and there is no evidence that it causes any harm.
Are there risks and side effects?Epidurals are very safe; serious complications are extremely rare. However, as with all medications and medical procedures, there are potential side effects:
- Decrease in blood pressure – The medication may lower your blood pressure, which may slow your baby’s heart rate. To make this less likely, you will be given extra fluids through a tube in your arm (IV), and you may need to lie on your side. Sometimes, your anesthesiologist will give you a medication to maintain your blood pressure.

- Sore back – Your lower back may be sore where the needle was inserted to deliver the medication. This soreness should last no more than a few days. There is no evidence that an epidural can cause permanent back pain.
- Headache – On rare occasions, the needle pierces the covering of the spinal cord, which can cause a headache that may last for a few days if left untreated. If this situation arises, discuss the treatment options with your anesthesiologist.
A spinal block is sometimes used in combination with an epidural during labor to provide immediate pain relief. A spinal block, like an epidural, involves an injection in the lower back. While you sit or lie on your side in bed, a small amount of medication is injected into the spinal fluid to numb the lower half of the body. It brings good relief from pain and starts working quickly, but it lasts only an hour or two and is usually given only once during labor.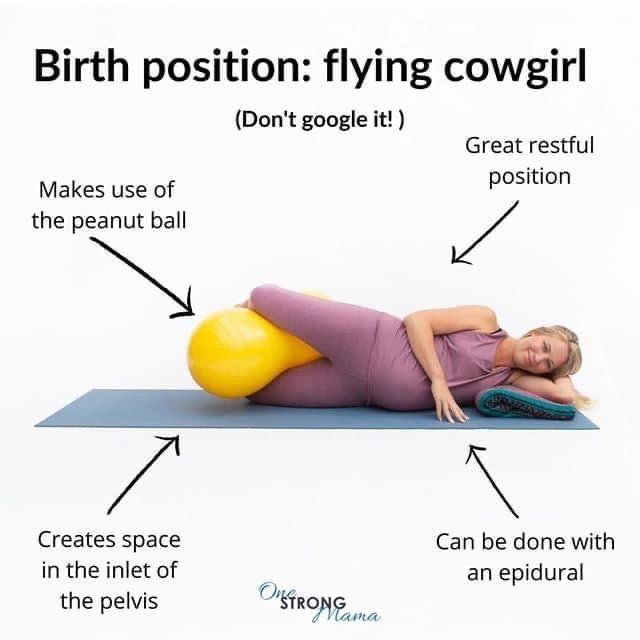 The epidural provides continued pain relief after the spinal block wears off.
The epidural provides continued pain relief after the spinal block wears off.
Anesthesiologists are committed to patient safety and high-quality care, and have the necessary knowledge to understand and treat the entire human body.
Epidural During Labor: How Does It Work?
If you’re planning to have a baby, the word “epidural” has probably come up more than a few times. While you likely have a decent idea that it’s supposed to help ease the pain of childbirth—and that there’s a needle involved—you might be a little fuzzy on the details of how it works exactly. And since people tend to have strong opinions about epidurals—is it really better than a medication-free birth?—it’s important to know the facts, so you can make the right decision for you and your growing family.
Labor and delivery is stressful no matter how you cut it, so having a basic birth plan in place can help you feel some semblance of control. To that end, you’ll want to explore your options and know what to anticipate when it comes to getting an epidural (or not).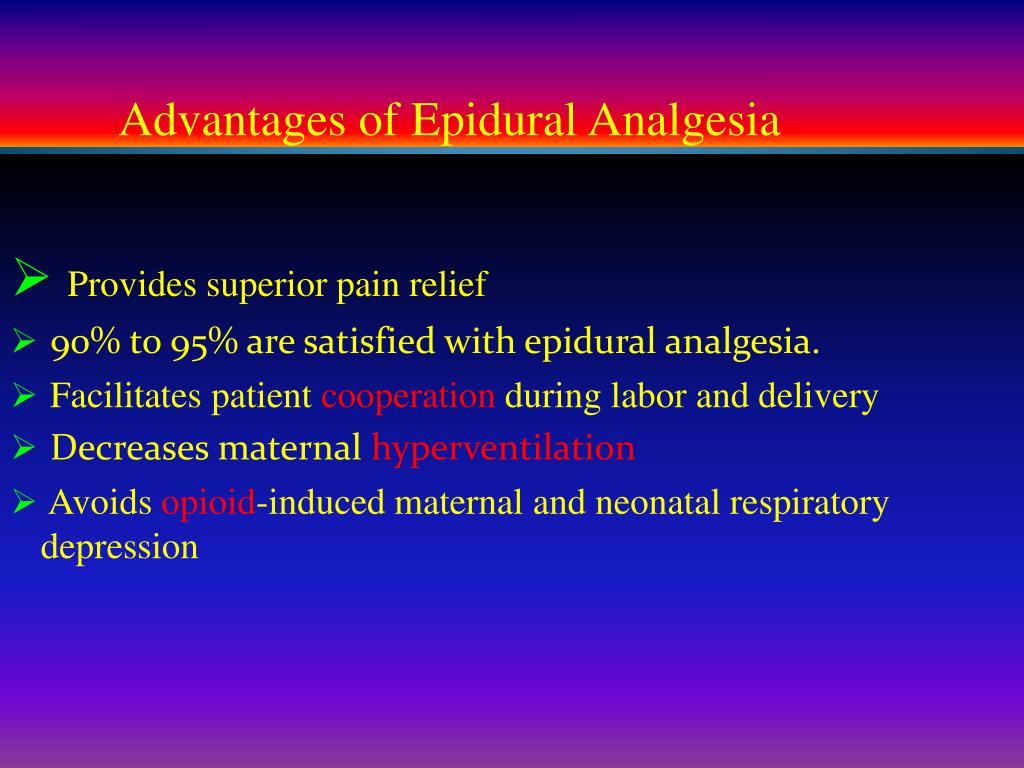 Ready to find out everything you’ve ever wanted to know about the ultimate numbing needle? We’re sharing answers to all your top questions: How long does an epidural last? Does getting an epidural hurt? And what are epidural side effects? Read on to get the facts.
Ready to find out everything you’ve ever wanted to know about the ultimate numbing needle? We’re sharing answers to all your top questions: How long does an epidural last? Does getting an epidural hurt? And what are epidural side effects? Read on to get the facts.
In this article:
What is an epidural?
When can you get an epidural?
Epidural procedure: how does an epidural work?
How long does an epidural last?
Does getting an epidural hurt?
Are epidurals safe?
Epidural side effects
Who can get an epidural?
Should you get an epidural?
What Is an Epidural?
You know those wailing women in labor you’ve seen in movies and on TV? Chances are they didn’t have an epidural. Simply put, an epidural helps to ease the pain of contractions and delivery. Numbing medication is sent to the area around your spinal cord (called the epidural space) via a catheter tube, and “this makes you numb from the belly button down,” says Erin S.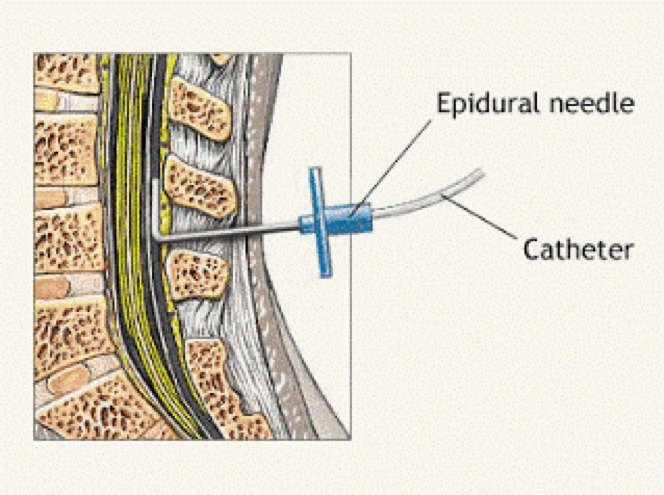 Grawe, MD, an assistant professor of clinical anesthesiology and director of perioperative services at the University of Cincinnati College of Medicine. Numb, yes, but not sleepy, which means you’ll be alert and at ease throughout baby’s delivery.
Grawe, MD, an assistant professor of clinical anesthesiology and director of perioperative services at the University of Cincinnati College of Medicine. Numb, yes, but not sleepy, which means you’ll be alert and at ease throughout baby’s delivery.
There are a few different types of epidurals that offer varying degrees of pain relief:
• Standard epidural. A “regular” epidural injects anesthetics into the epidural space of your spine to block pain in your body, making you numb from the waist down. It blocks your motor control, so while you’ll be able to move your legs around in bed, you won’t be able to walk with a full epidural, says Christine Greves, MD, an ob-gyn at the Winnie Palmer Hospital for Women & Babies in Orlando, Florida.
• Spinal injection. This one-and-done shot sends a single dose of concentrated drugs into the spine’s sac of cerebrospinal fluid, which houses the spinal cord and nerves. It provides immediate relief, but because there isn’t a catheter or continuous flow of medication, this option wears off within about two hours. It’s often used for a c-section.
It’s often used for a c-section.
• Combined spinal-epidural. This combo can offer the best of both worlds: Like a spinal, the numbing medicine is injected into the fluid sac, so you’ll feel the effects quickly, and like an epidural, a catheter is then inserted to provide ongoing pain relief.
• Low-dose epidural. This option offers a lower dose of the pain-blocking medication, leaving you with greater movement in your legs. It’s often administered in the early stage of labor, Greves says, before pain levels spike.
• Walking epidural. A walking epidural uses narcotics only to help lessen the pain without limiting your motor function. It won’t block the pain as much as a standard or low-dose epidural, Greves says, but you may be able to get up and walk around during labor, if your doctor and hospital allow it.
If you opt for a walking or low-dose epidural to begin with but decide you need more pain relief, you can upgrade your epidural as you go—but you can’t downgrade from a standard epidural to a low-dose option, or from a low-dose epidural to a walking one.
When Can You Get an Epidural?
Technically, you can get an epidural at any time during labor, but it’s often recommended that you do so during the active phase (i.e., the middle stage when your cervix begins to dilate rapidly), says Greves. That’s because an epidural could actually slow down labor, she says, so it’s best to administer it when things are already progressing quickly.
While you might be tempted to wait until you’re in teeth-clenching, unbearable pain to get an epidural, it’s actually better to do it before you reach the writhing point. A woman must be able to sit still when an epidural is administered, says Grawe—otherwise, it may be difficult for your anesthesiologist to safely give you one.
Epidural Procedure: How Does an Epidural Work?
Here’s what they didn’t teach you in biology class: Epidural medication is delivered through a tiny, flexible tube (aka a catheter) that’s inserted into your lower back. The tube goes into the epidural space, which is outside of the spinal cord and where all of the nerves live that go to the lower parts of the body, Grawe says. Doctors use the tube to administer special medication—often a combo of a local anesthetic (or numbing medicine) and a narcotic (or pain-relieving medicine)—near those nerves, and “the medication basically dazes the nerves, so you don’t feel the pain impulses coming in,” says William Camann, MD, director of obstetric anesthesia service at Brigham and Women’s Hospital in Boston and coauthor of Easy Labor: Every Woman’s Guide to Choosing Less Pain and More Joy During Childbirth.
Doctors use the tube to administer special medication—often a combo of a local anesthetic (or numbing medicine) and a narcotic (or pain-relieving medicine)—near those nerves, and “the medication basically dazes the nerves, so you don’t feel the pain impulses coming in,” says William Camann, MD, director of obstetric anesthesia service at Brigham and Women’s Hospital in Boston and coauthor of Easy Labor: Every Woman’s Guide to Choosing Less Pain and More Joy During Childbirth.
How Long Does an Epidural Last?
Don’t worry if you’re planning on getting an epidural early in labor; the pain medication won’t suddenly stop working or wear off. The epidural stays in your back so you can continue to receive the medicine throughout labor. And here’s some comforting news: Many hospitals now have patient-controlled epidurals, which allow moms-to-be to manage the flow of pain-relieving epidural medication with the simple push of a button. But don’t worry: The machine is set so that it won’t deliver too much medication.
So how long does an epidural last? An epidural can provide relief for a pretty long time, as long as your catheter is in place and you’re receiving medication—in fact, it can last reliably for up to five days, according to Grawe. “Fortunately, labor doesn’t usually take that long, so the epidural doesn’t need to last that long,” she points out.
Some doctors will request that the epidural be turned off or down during the pushing phase to allow mom to feel the pressure of baby’s head, which creates an urge to push, says G. Thomas Ruiz, MD, an ob-gyn at Orange Coast Memorial Medical Center in Fountain Valley, California. But that can still make things tricky: “Turn down the epidural too soon and the pain of contractions can inhibit pushing in some women,” Ruiz says.
Once baby is delivered, your anesthesiologist will stop the medicine and pull out the catheter. After that, Grawe says, it can take up to four hours for the numbness to wear off.
Does Getting an Epidural Hurt?
While getting an epidural is meant to reduce labor pains, many women worry and wonder: Does getting an epidural hurt? The good news is the actual process of receiving an epidural is often not as scary—or painful—as you might imagine.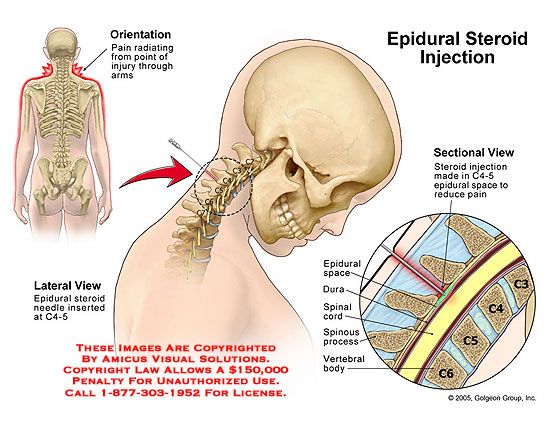
Everyone’s pain tolerance is different, Greves says, but in general, it’s not painful—and definitely not nearly as uncomfortable as active labor pains. In fact, your anesthesia provider will help ensure you’re at ease by numbing the skin on your back with a small needle even before actually placing the epidural, Grawe says. “After that, you may feel pressure and pushing in your lower back, but nothing should feel like sharp pain,” she says. If you do feel anything sharp, just let your anesthesiologist know and they can give you more numbing medicine, Grawe says. “The job of the anesthesia provider is to make sure you’re comfortable and safe during your delivery.”
How big is an epidural needle?
Still, some women are wary about getting an epidural because they’re nervous about the size of the needle. Depending on the kind of epidural you receive, it will likely be 3.5 inches long and a bit wider than an average shot. Not a fan of needles? Don’t worry—since the epidural is placed in your back, you’ll be facing away from the anesthesia provider and won’t have to see that needle at all.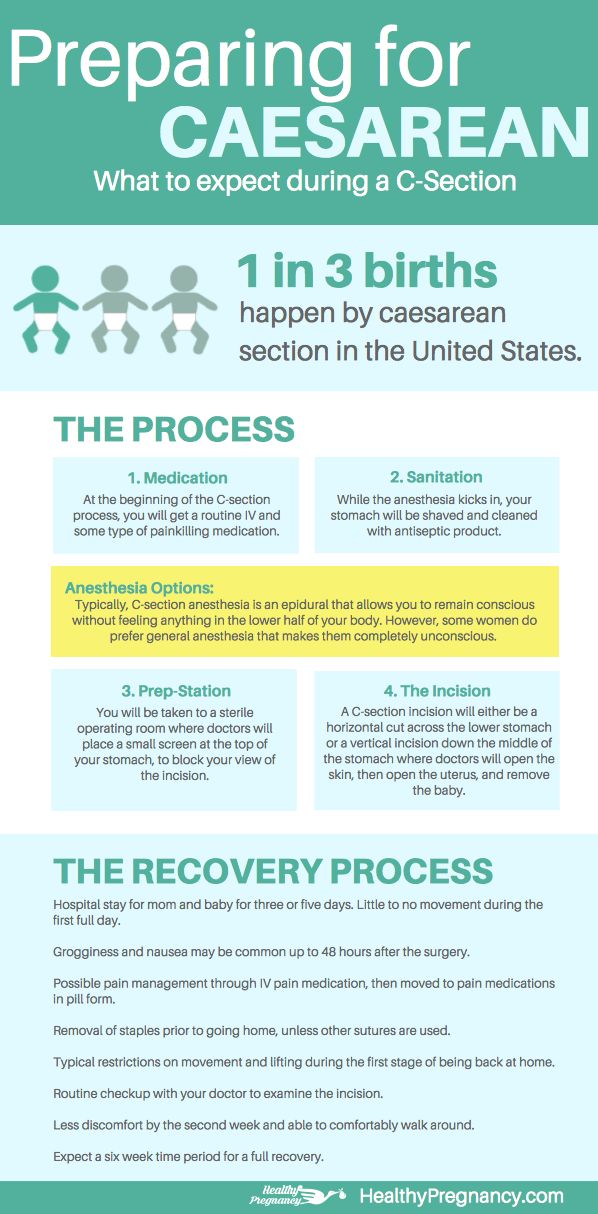
Will you feel any pain after an epidural?
An epidural numbs the pain of childbirth, but it’s important that you’re still able to feel the urge to push. Many women report feeling pressure and a decreased sensation of pain during their labor. Overall, an epidural can provide a more comfortable experience and give you some much-needed relief. (You might even be at ease enough to take a nap! After all, labor can be long and exhausting.)
Of course, it’s worth noting that epidurals aren’t always 100 percent effective. According to a report in Anesthesiology, 10 to 15 percent of women experience incomplete pain relief or localized pain. If this happens, your anesthesiologist may withdraw and replace the catheter or offer additional doses.
Are Epidurals Safe?
Don’t lose sleep at night worrying whether an epidural will cause harm to you or baby. “Epidurals are very safe,” Grawe says, “and there are no negative effects on the fetus or the labor process when used appropriately and in a carefully monitored setting.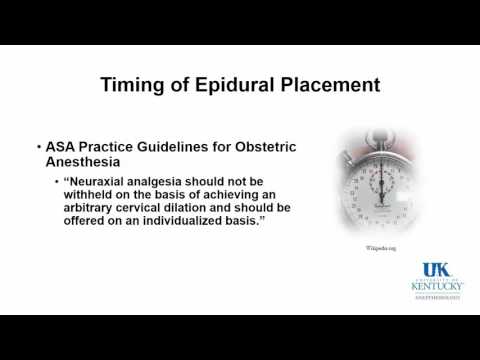 ”
”
Epidural complication rates are low: According to the American Society of Anesthesiologists, it’s just under 3 percent.
Epidural Side Effects
Epidurals are the gold standard in labor pain management, and they’re considered very safe. But there are some potential side effects. Women may have soreness in their lower back where the epidural needle was inserted, Greves says. There’s also a risk of developing what’s called a spinal or epidural headache—a headache that occurs if there’s a leak of spinal fluid around the epidural catheter. But it’s very rare, Grawe says, and happens between 0.5 to 5 percent of the time. A woman might also have an infection at the site of the catheter, and bleeding or bruising in the epidural space, which can cause nerve damage—but again, Grawe says, it’s extremely rare.
Other potential epidural side effects include:
• Drop in blood pressure. According to research, about 14 percent of women experience hypotension, or a sudden drop in blood pressure, after receiving an epidural. Your medical team will give you IV fluids, monitor your blood pressure and provide additional treatment, as needed.
Your medical team will give you IV fluids, monitor your blood pressure and provide additional treatment, as needed.
• Nausea and vomiting. The opioids in an epidural may also make you feel drowsy and nauseous.
• Itchy skin. Opioids may also make you itchy and restless. If this happens, your doctor can give you medication.
• Fever. It’s possible to spike a fever after receiving an epidural.
• Labored breathing. It’s not common, but occasionally an epidural can cause slow or labored breathing.
• Problems urinating. Since your lower body will be numb from an epidural, you won’t feel the urge to pee and will likely have a urination catheter in place. It’s removed shortly after delivery, but there’s a chance you may continue to experience decreased bladder sensitivity for a short while.
• Trouble walking. Once the epidural wears off, you’ll start to regain strength in your lower body. However, it might take you a bit to feel fully steady on your feet.
However, it might take you a bit to feel fully steady on your feet.
• Nerve damage. It’s extremely rare, but it’s possible that an epidural could reach a nerve and cause temporary or long-term numbness.
Who Can Get an Epidural?
Unfortunately, not all women are good candidates for an epidural. Your doctor will assess you to determine if it’s the right pain-management path for you. The following are among the more common reasons you may not be able to receive an epidural during labor:
• Very low blood pressure
• Some bleeding or clotting disorders
• Blood infections
• Skin infection or a brand new tattoo on the lower area of your back
Also, keep in mind that your birth plan may not be conducive to an epidural. For example, if you want to have a water birth or plan on delivering in your home or at a birthing center, you’re out of luck. You need to be in a hospital setting to get an epidural.
Should You Get an Epidural?
The choice to get an epidural during childbirth is an entirely personal one. Consider your pain tolerance, and discuss your birth plan with your doctor. Be sure to ask about the different kinds of pain-management and epidural options available at your hospital and any restrictions that may apply. Above all else, try to be flexible and keep an open mind—because your birth plan can change on a dime. Epidural or no epidural, keep your eye on the prize: a healthy, happy baby is all that matters.
Consider your pain tolerance, and discuss your birth plan with your doctor. Be sure to ask about the different kinds of pain-management and epidural options available at your hospital and any restrictions that may apply. Above all else, try to be flexible and keep an open mind—because your birth plan can change on a dime. Epidural or no epidural, keep your eye on the prize: a healthy, happy baby is all that matters.
About the experts:
William Camann, MD, is an associate professor at Harvard Medical School and the director of obstetric anesthesia service at Brigham and Women’s Hospital in Boston, Massachusetts. He received his medical degree at Pennsylvania State University College of Medicine in Hershey, Pennsylvania.
Erin S. Grawe, MD, is an assistant professor of clinical anesthesiology and director of perioperative services at the University of Cincinnati College of Medicine in Cincinnati, Ohio. She also received her medical degree there.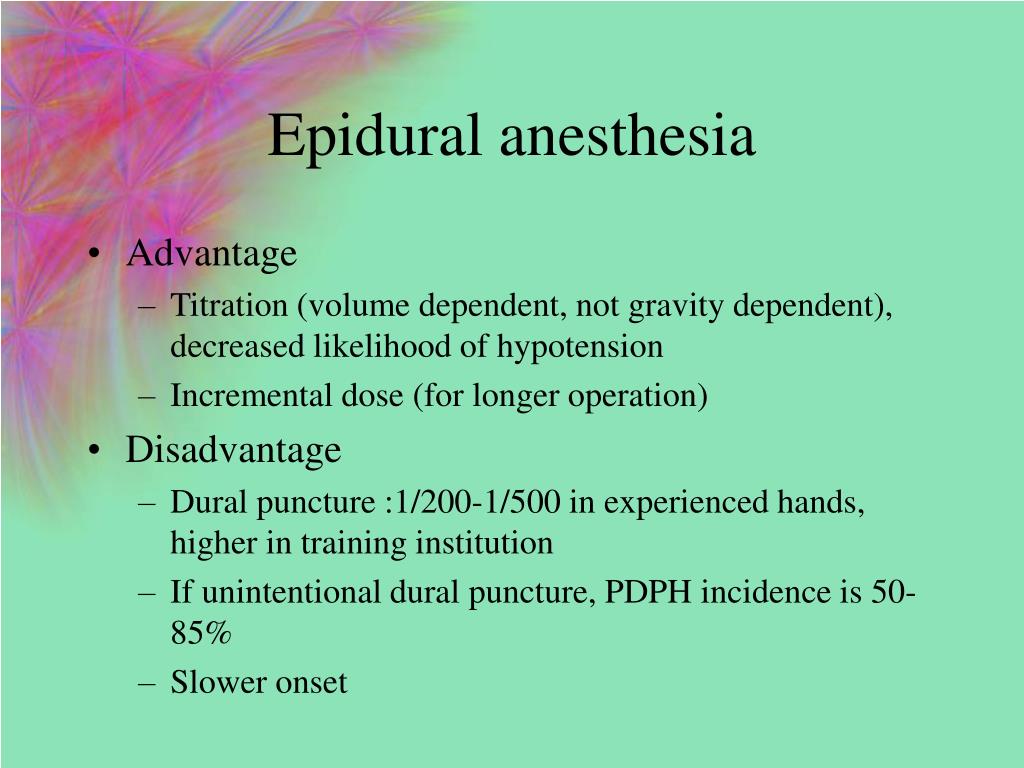
Christine Greves, MD, is an ob-gyn at the Winnie Palmer Hospital for Women & Babies in Orlando, Florida. She earned her medical degree from the University of South Florida College of Medicine in Tampa, Florida.
G. Thomas Ruiz, MD, is an ob-gyn at Orange Coast Memorial Medical Center in Fountain Valley, California. He received his medical degree from UC Irvine School of Medicine in Irvine, California.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Where to Find the Best Online Childbirth Classes
15 Important Decisions to Make Before You Go Into Labor
Hospital Bag Checklist: What to Pack in Your Hospital Bag
Not Found (#404)
Paracelsus Medical Center
Page not found.
The above error occurred while the Web server was processing your request.
Please contact us if you think this is a server error. thank you.
Please wait, download may take time
Loading...
Do you know which doctor you want to see
You know the service you want to sign up for
Service selection
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
The choice of a specialist
Service selected:
Choosing a specialist service
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
Address selection:
st. Vikulova, 33, building 2 st. Bolshakova, d. 68
Date selection:
Time of receipt:
Password
Password
Register Can't login? account activation
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for password recovery
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for reactivating your account
Your application has been accepted, our specialists will answer your question as soon as possible!
Telephone
Comment
Dear patients!
Multidisciplinary Clinic and Maternity Hospital "Paracelsus" informs you, according to the Letter of the Ministry of Finance of the Russian Federation to the Federal Tax Service dated March 25, 2022. N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
Joint order of the Ministry of Taxation of Russia and the Ministry of Health of Russia of July 25, 2001 N 289 / BG-3-04 / 256 (hereinafter - the order of July 25, 2001) approved the form of the Certificate of payment for medical services for submission to the tax authorities of the Russian Federation (hereinafter - the Certificate payment for medical services).
This certificate certifies the fact of receiving a medical service and its payment through the cash desk of a healthcare institution at the expense of the taxpayer.
Thus, if the taxpayer submits to the tax authority a Certificate of payment for medical services, the taxpayer's failure to submit the relevant contract for the provision of medical services and (or) documents confirming payment cannot be grounds for refusing to provide such a deduction.
The amounts are based on payment data. Therefore, checks, an agreement and a clinic license are not needed to make a deduction.
Sample certificate attached.
Help Sample
Your application has been accepted, our specialists will contact you shortly!
Telephone
Comment
Error 404 | Regional perinatal center
Dear patients!!!
⚡⚡⚡ Closing for planned disinfection of obstetric hospitals of the Regional Perinatal Center is scheduled for the period from 08:00 October 17 to 08:00 October 31, 2022.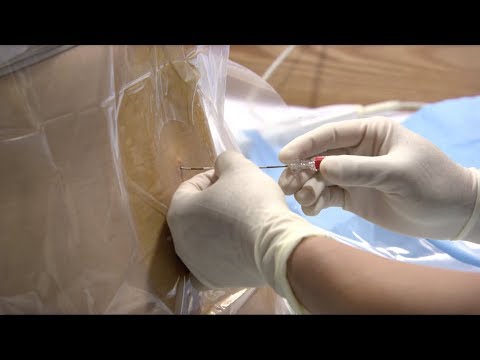
During the closing period, the following will be admitted:
- pregnant women and women in labor up to 33 weeks 6 days inclusive,
- gynecological patients for planned surgical interventions.
High-risk pregnant women in terms of 34 weeks or more, as well as gynecological patients for emergency care, during the specified period, are hospitalized at Clinical Hospital No. 9.
Reason: order of the Department of Health and Pharmacy of the Yaroslavl Region dated 10/11/2022 No. 1277.
P.S. In December 2022, there will be no closure for disinfection.
⚡⚡⚡
Given the epidemiological situation, there is currently a restriction on visits to inpatient departments of the Perinatal Center.
. dated November 25, 2021 No. 12752p-P12, regular meetings of citizens with experts on problematic issues of reproductive health continue.
Meetings are held every Saturday on the Reproductive Health channel, which is available at the links:
https://rutube. ru/channel/25385590/
ru/channel/25385590/
https://www.youtube.com/channel/UCpEP5EFRcqul2Ae6Y6RbGuA
https ://vk.com/popsovet.
Questions to experts are accepted by e-mail: [email protected].
Schedule of the educational project "Reproductive Health" for August - December 2022
| No. | Date
| Time | Expert | Subject name |
| 1. | 13.08 | 10-00 | O.M. Drapkina A. | Obesity as an interdisciplinary problem. Prevention and correction of eating disorders. Proper nutrition and psychological aspects of women's health disorders. |
| 2. | 20.08 | 10-00 | O.I. Apolikhin | Modern possibilities of drug and surgical treatment of disorders of male reproductive health. Assisted reproductive technologies for male infertility. |
| 3. | 27.08 | 10-00 | M.F. Ippolitova | Pregnancy, childbirth and abortion in adolescents. Features of preventive examination of minors. Modern methods of contraception for adolescents and youth. |
| 4. | 3.09
| 9-00 | L.V. Adamyan
| Uterine fibroids: asymptomatic, symptomatic. family forms. Possible options for examination and treatment. |
| 5. | 10.09
| 10-00 | A.B. Hecht (R.G. Akzhigitov) | Sequelae of COVID-19 in women (post-COVID syndrome). |
| 6. | 17.09 | 10-00 | A.D. Kaprin | Prostate cancer and stereotypes of male reproductive health. The possibilities of modern medicine and the right attitude to one's health. |
| 7. | 24.09 | 10-00 | E.E. Voronin L.Yu. Afonina | HIV, hepatitis and pregnancy. Prevention of HIV and hepatitis among young people. |
| 8. | 1.10 | 10-00 | I.V. Soldiers | Benign dysplasia of the mammary glands. Precancerous diseases and risk factors for the development of malignant neoplasms of the breast. What you need to know: simple answers to women's questions. |
| 9. | 8.10 | 10-00 | N.V. Mokrysheva | “Letters to my son”: what endocrine aspects of reproductive health do we need to tell teenagers about |
10. | 15.10
| 10-00 | A.D. Kaprin M.V. Kiseleva | Reproductive health of cancer patients: opportunities to become parents are real. |
| 11. | 10/22 | 10-00 | A.B. Hecht
| Prevention of postpartum depression, including during periods of limited social contact. Postcovid syndrome. |
| 12. | 29.10 | 10-00 | N.V. Mokrysheva
| Family planning for diabetes and thyroid disease: what to look for. |
13. | 5.11 | 10-00 | A.A. Steam horse | Oncology and pregnancy: preservation of reproductive function, preparation and management of pregnancy in oncological diseases. |
| 14. | 11/12 | 10-00 | A.A. Olina E.V. Uvarova | Teenage pregnancy: abortion cannot be delivered. Where to put a punctuation mark or what to do in a difficult situation? |
| 15. | 11/19 | 10-00 | L.V. Adamyan | Modern aesthetic and plastic gynecology. The unity of beauty, sexuality and psychological comfort. |
| 16. | 11/26 | 10-00 | O.I. Apolikhin | We are what we eat. Nutrition and male fertility. What and how to eat, drink to maintain fertility? |
| 17.
| 03.12 | 10-00 | N.V. Dolgushin O.I. Apolikhin A.A. Olina | Medical genetic counseling for pregnancy planning. Assisted reproductive technologies, family assistance programs. Inefficiency of ART and ways to overcome it. |
| 18. | 10.12 | 10-00 | N.G. Mokrysheva
| Beyond genes: the role of parents in childhood obesity. |
| 19. | 17.12 | 10-00 | Final event | New opportunities in medicine and reproduction ( genetics, immunology, cell technology, endocrinology, reproductive surgery, gynecology, urology, oncology ). |
⚡⚡⚡ Partner birth has resumed.
GBUZ YaO "Regional Perinatal Center", based on letters from the Head of the Rospotrebnadzor Administration for the Yaroslavl Region dated March 21, 2022 No. 76-00-04 / 41-1099-2022, dated 04.20.2022 No. 76-00-04 / 48-1632-2022 and dated 07.01.2022 No. 76-00-04 / 41-2515-2022, informs about the possibility of partner childbirth from 03.23.2022, subject to the following conditions: the partner has a QR code about vaccination, as well as a PCR test made no later than 48 hours before delivery (!!!express test is not accepted).
On the basis of clause 811. Decree of the Chief State Sanitary Doctor of the Russian Federation dated January 28, 2021 No. 4 “On Approval of Sanitary Rules and Norms SanPiN 3.3686-21 “Sanitary and Epidemiological Requirements for the Prevention of Infectious Diseases”, who is present at partner childbirth, is obliged to provide the result of an examination for tuberculosis (fluorography of the chest organs) not older than 1 year.
In addition, the future father needs to have a passport, a change of shoes (clean rubber slippers), a change of clean clothes (t-shirt and pants), a pair of clean handkerchiefs, a pack of wet antibacterial wipes and a small bottle of drinking water.
⚡⚡⚡ Instruction for citizens on actions in case of asymptomatic or mild novel coronavirus infection and acute respiratory viral infection (Download full memo, download short memo)
⚡⚡⚡Information for accompanying persons
Due to the increased risk of the spread of COVID-19, persons accompanying patients in outpatient departments are not allowed in the building of the Perinatal Center.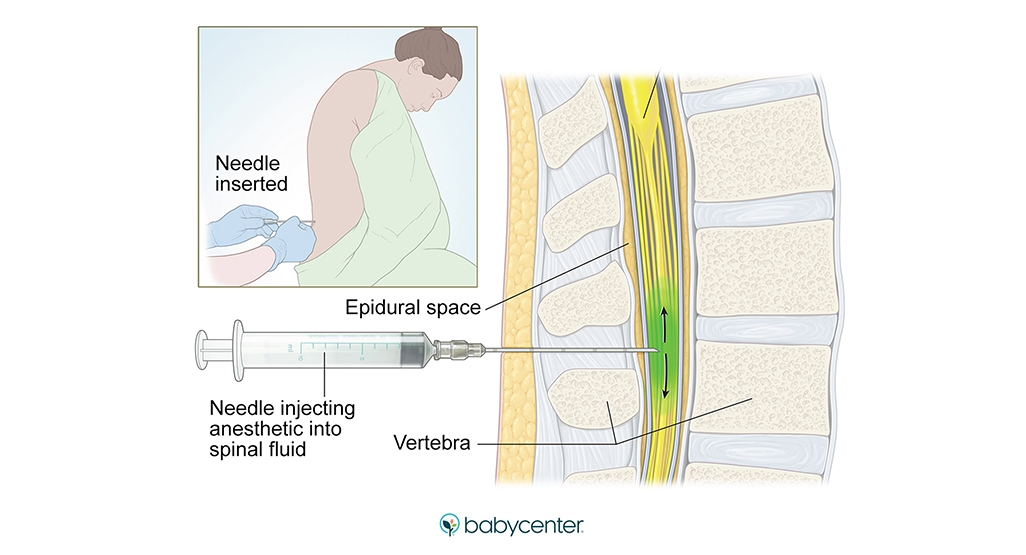
 B. Hecht
B. Hecht 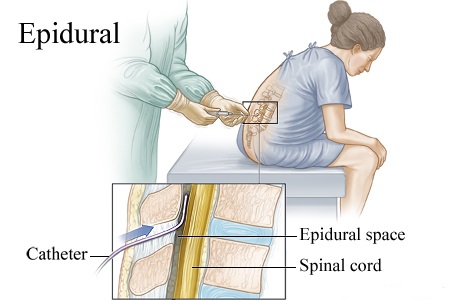

 The impact of obesity on the somatic, psychological and social well-being of children and adolescents.
The impact of obesity on the somatic, psychological and social well-being of children and adolescents.