How does baby get eczema
Eczema
Is this your child's symptom?
- An itchy rash that your doctor told you was eczema
- Eczema is a chronic skin disease
- Recurrent flare-ups of severe itching occur
- The medical name for eczema is atopic dermatitis
Symptoms of Eczema
- The main symptom is itching. If it doesn't itch, it's not eczema.
- With flare-ups (itching attacks), the rash becomes red or even raw and weepy.
- Onset: Average onset at 3 months old. Range: 1-6 months old. Usually begins by 2 years old.
- Location: Classic eczema starts on the cheeks at 1 to 6 months of age. It can spread to the rest of the face. In infants, the outer surfaces of the arms and legs also become involved.
- In older children, eczema is found in the joint creases. The elbows, wrists, and knees are the most common places.
- The rash is usually the same on both sides of the body.
Cause of Eczema
- A type of dry, sensitive skin that children inherit.
- Flare-ups are from skin contact with soap, shampoo, pollen or other irritating substances.
- About 30% of babies with severe eczema also have food allergies. The most common is cow's milk.
- Over 10% of children have eczema. It's the most common skin condition of the first 10 years.
Triggers of Eczema Flare-Ups
- Soaps. Never use bubble bath. It can cause a major flare-up.
- Pollens. Keep your child from lying on the grass during grass pollen season.
- Animals. Avoid any animals that make the rash worse.
- Foods. If certain foods cause severe itching (flares), avoid them.
- Wool. Avoid wool fibers and clothes made of other scratchy, rough materials.
- Dry Air. Use a humidifier if the air in your home is dry.
- Herpes Virus Infection (Serious). Keep your child away from anyone with fever blisters (cold sores).
 The herpes virus can cause a serious skin infection in children with eczema.
The herpes virus can cause a serious skin infection in children with eczema. - Eczema is not caused by laundry soap you use to wash clothing.
Itching Scale
- Mild: doesn't interfere with normal activities
- Moderate: interferes with child care or school, sleep, or other normal activities
- Severe: constant itching that can't be controlled
Food Allergy and Eczema Flare-Ups
- Food allergies are a factor in 30% of young children with severe eczema. This factor is mainly seen in babies.
- The main allergic foods are cow's milk and eggs.
- The main symptoms are increased skin redness and itching. Some parents report these symptoms start during or soon after the feeding.
- The eczema becomes easier to control if you avoid the allergic food.
Diagnosing Food Allergy and Eczema Flare-Ups
- Your child's doctor may suggest the steps listed below:
- Remove the suspected food or foods from your child's diet for 2 weeks.
 The eczema should greatly improve.
The eczema should greatly improve. - Then give your child that food when the eczema is under good control. This is called a "challenge."
- If the food is causing flare-ups, the eczema should become itchy and red. The flare-up should occur quickly within 2 hours of eating the food.
- If this occurs, avoid giving this food to your child. Talk to your child's doctor about the need for any food substitutes.
- If the eczema does not flare-up, your child isn't allergic to that food.
When to Call for Eczema
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Looks infected (spreading redness, pus, soft oozing scabs) and fever
- Many small blisters or punched-out sores occur
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Eczema is very painful to touch
- Looks infected but no fever
- Itching is severe after using steroid cream for more than 48 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Itching flare-ups occur often
- Eczema diagnosis was never confirmed by a doctor
- You have other questions or concerns
Self Care at Home
- Eczema with no other problems
- Questions about prevention of eczema flare-ups
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.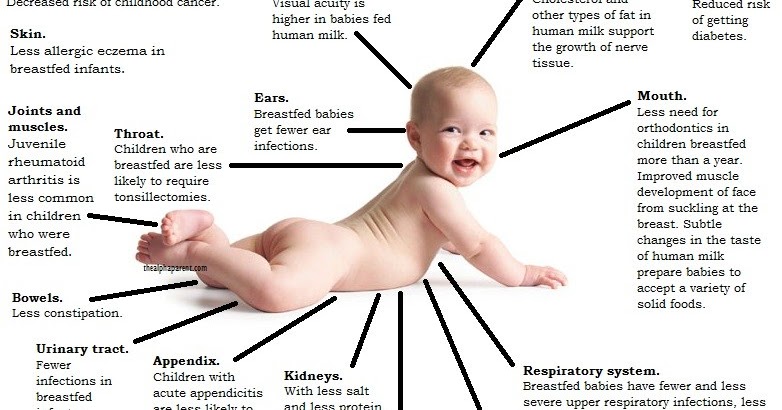
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice
Treatment for Eczema
- What You Should Know About Eczema:
- Eczema is a chronic skin disease. So, you need to learn how to control it.
- Itching attacks (flare-ups) are to be expected.
- The goal is to treat all flare-ups quickly. Reason: To prevent skin damage.
- Here is some care advice that should help.
- Treatment is Based on Severity of Eczema:
- Mild Eczema.
 Just need to use a moisturizing cream and to avoid flare-up triggers.
Just need to use a moisturizing cream and to avoid flare-up triggers. - Moderate Eczema. Also need to use a steroid cream and bedtime allergy medicine.
- Severe Eczema. Also may need antibiotics for a skin infection caused by Staph bacteria. This infection starts in open skin from severe itching.
- Mild Eczema.
- Moisturizing Cream or Ointment for Dry Skin:
- All children with eczema have dry sensitive skin.
- The skin needs a moisturizing cream (such as Eucerin) Apply once or twice daily.
- Apply the cream after a 5 or 10-minute bath. To trap moisture in the skin, apply the cream while skin is still damp. Do this within 3 minutes of leaving the bath or shower.
- The steroid cream should be applied to any itchy spots first. Then use the moisturizing cream as the top layer.
- While most parents prefer creams, moisturizing ointments are sometimes needed in the winter. An example is Vaseline.
- Caution: Never stop the moisturizing cream.
 Reason: The rash will come back.
Reason: The rash will come back.
- Steroid Cream or Ointment for Itching:
- Itchy skin is the main symptom of eczema.
- Steroid creams or ointments are essential for controlling red, itchy skin.
- Apply steroid creams only to itchy or red spots (not to the normal skin).
- Most children have 2 types of steroid creams. (1) A mild steroid cream is used to treat any pink spots or mild itching. This is often 1% hydrocortisone cream (such as Cortaid). No prescription is needed. (2) Another stronger steroid cream is needed to treat any spots with severe itching. This is a prescription steroid cream such as Synalar. Never apply this stronger cream to the face.
- Apply these creams as directed or 2 times per day.
- After the rash quiets down, apply it once per day. After 1 good week just use moisturizing cream.
- Bathing - Avoid Soaps:
- Give one bath a day for 10 minutes in lukewarm water.
 Reason: Water-soaked skin feels less itchy. Follow the bath with a moisturizing cream (such as Eucerin) to all the skin.
Reason: Water-soaked skin feels less itchy. Follow the bath with a moisturizing cream (such as Eucerin) to all the skin. - Avoid all soaps. Reason: Eczema is very sensitive to soaps, especially bubble bath. There is no safe soap for young children with eczema. They can be cleaned using warm water.
- Give one bath a day for 10 minutes in lukewarm water.
- Allergy Medicine for Itching at Bedtime:
- Some children with eczema need an allergy medicine by mouth at bedtime.
- Reason: Scratching in bed can cause severe skin breakdown. It may also interfere with falling sleep.
- Give the med your child's doctor wanted you to use for itching.
- If none was suggested, you can try Benadryl at bedtime until you talk with your doctor. No prescription is needed. Age limit: 1 and older.
- Caution: do not use Benadryl for more than a few days.
- Itching Attack - Shower to Remove Irritants:
- Playing in the grass, being around animals, or swimming can cause increased itching.

- For itching from these causes, give your child a quick shampoo and shower.
- Playing in the grass, being around animals, or swimming can cause increased itching.
- Itching Attack - Treatment:
- At the first sign of any itching, use the steroid cream. Put it on the areas that itch. If unsure, apply 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Keep your child's fingernails cut short and smooth.
- Ask older children to try not to itch, but never punish for itching.
- For constant itching in young children, cover the hands with socks or gloves. Use for a day or until the itching is brought under control. Provide extra cuddling during this time.
- Return to School:
- Eczema cannot be spread to others.
- Children with eczema do not need to miss any child care or school.
- What to Expect:
- Eczema is a chronic condition. Around the teen years, about half get over their eczema.
- Many children who have severe eczema as babies develop asthma and nasal allergies.

- Call Your Doctor If:
- Itching is not under control after 2 days of steroid cream
- Rash looks infected (spreading redness, yellow scabs or pus)
- You think your child needs to be seen
- Your child becomes worse
Prevention of Eczema Flare-Ups
- Tips to Help Prevent Flare-Ups:
- Some flare-ups of eczema cannot be explained. But others are triggered by things that can be avoided.
- Avoid chlorine in swimming pools and spas, harsh chemicals, and soaps.
- Never use bubble bath. It can cause a major flare.
- Keep your child off the grass during grass pollen season.
- Avoid any animals that make the rash worse.
- If certain foods cause severe itching (flares), avoid them.
- Wear clothes made of cotton or cotton blends as much as possible. Avoid wool fibers and clothes made of other scratchy, rough materials. They make eczema worse.

- Try to avoid excess heat, excess cold and dry air (use a humidifier). Avoid over-dressing. Heat can make the rash worse.
- Caution: Keep your child away from anyone with fever blisters (cold sores). The herpes virus can cause a serious skin infection in children with eczema.
- Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/25/2022
Last Revised: 01/13/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Baby Eczema Symptoms, Causes, Treatments, Creams, and More
Series Eczema in Babies
Written by WebMD Editorial Contributors
Eczema can show up as crusty, flaky patches on your baby's skin, often during their first few months. It’s common and treatable. Many infants outgrow it.
It’s common and treatable. Many infants outgrow it.
Not sure if your baby's itchy, irritated rash is eczema? Your doctor can tell you for sure. These questions and answers can help you understand what to look for.
What Does Baby Eczema Look Like?
Eczema doesn't look the same on every baby. In babies with light skin, it usually shows up as patches of red skin. In darker-skinned babies, the rash might look purplish, brownish, or grayish. Eczema can be harder to see on babies with dark skin.
These patches are almost always dry, itchy, and rough.
Babies can get the condition just about anywhere on their body. Most often, it affects their cheeks and the joints of their arms and legs.
It’s easy to confuse baby eczema (also called infant eczema or atopic dermatitis) with cradle cap. But there are some key differences.
Cradle cap is much less itchy and irritated. It generally clears up by age 8 months and usually appears on the scalp, sides of the nose, eyelids and eyebrows, and behind the ears. See a photo of what cradle cap looks like.
See a photo of what cradle cap looks like.
Causes
It can run in families. If a parent has eczema, a baby is a lot more likely to get it, too.
Problems in the skin barrier, allowing moisture out and germs in, could also be a cause.
Eczema happens when the body makes too few fatty cells called ceramides. If you don’t have enough of them, your skin will lose water and become very dry. Read more on what causes eczema.
Does Baby Eczema Go Away by Itself?
It often does. Most children outgrow it before they start school.
It’s not common, but some kids will have eczema into adulthood. They may have times -- even years -- without the symptoms. But they may still tend to have dry skin. Get more information on kids, allergies, and eczema.
What Can Make It Worse
Each baby is different. But there are some common eczema triggers to avoid, including:
Dry skin. It can make a baby's skin itchier. Low humidity, especially during winter when homes are well-heated and the air is dry, is a cause.
Irritants. Think scratchy wool clothes, polyester, perfumes, body soaps, and laundry soaps. These can all trigger symptoms.
Stress. Children with eczema may react to stress by flushing. That can lead to itchy, irritated skin. And that, in turn, ramps up their eczema symptoms.
Heat and sweat. Both can make the itch of infant eczema worse.
Allergens. It’s not certain, but some experts believe that removing cow’s milk, peanuts, eggs, or certain fruits from a child’s food may help control eczema symptoms. Remember that your baby can get exposed to these foods if their mother eats them before they breastfeed. Find out the connection between food and eczema flares.
Home Treatment
Give your little one's skin some TLC. That’s the first step in treating their eczema. Try:
Moisturizers. One with ceramides is the best option. These are available over the counter and by prescription. Otherwise, a good moisturizer, fragrance-free cream, or ointment such as petroleum jelly, when used several times daily, will help your baby's skin retain its natural moisture. Apply immediately after a bath.
Otherwise, a good moisturizer, fragrance-free cream, or ointment such as petroleum jelly, when used several times daily, will help your baby's skin retain its natural moisture. Apply immediately after a bath.
A lukewarm bath. This hydrates and cools the skin. It may also ease itching. Make sure the water isn’t too hot! Keep the bath short -- no more than 10 minutes. To soothe itchiness even more, try adding oatmeal soaking products to your baby's tub.
Use mild, unscented body and laundry soaps. Perfumed, deodorant, and antibacterial soaps can be rough on a baby's sensitive skin.
Clean carefully. Use soap only where your baby may be dirty, such as the genitals, hands, and feet. Simply rinse off the rest of your child's body.
Dry off. Pat skin dry. Don't rub.
Dress for comfy days. To avoid the irritation of clothing rubbing on the skin, your child should wear loose clothes made of cotton.
Always wash new clothes before you put them on your baby. Use a mild, fragrance-free detergent.
To keep your little one comfy, don’t overdress them or use too many blankets. If they get hot and sweaty, that can trigger an eczema flare. Learn more about natural skin care for babies.
What to Do About Itching
Try to keep your baby from scratching their itchy skin. Scratching can make the rash worse, lead to an infection, and cause the irritated skin to get thicker and more leathery.
Trim their nails often, and then take the edge off of them with a file if you can. Some parents also slip "scratch mittens" onto their little one's hands. Others try long socks, tucked in under a long-sleeved shirt, so they're harder for a baby to remove. View a slideshow to get more eczema skin care tips.
Medicines
Some over-the-counter products, such as hydrocortisone creams and ointments, target itching and inflammation. Check the instructions and don’t use them too long, or they can thin the skin in the affected area.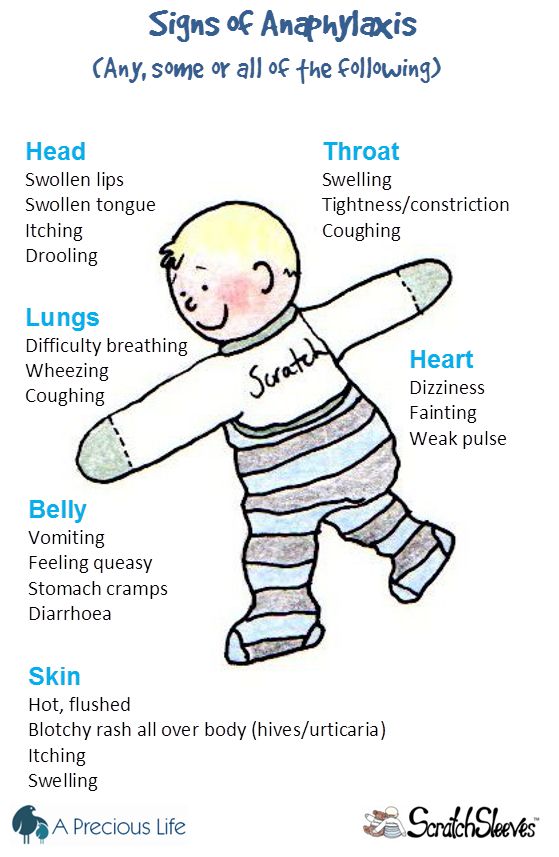
There are also medicines that need a doctor’s prescription, if other treatments don’t work.
When to Call a Doctor
Make the call if your baby’s eczema doesn’t begin to get better within a week of starting over-the-counter hydrocortisone creams. It may be time for a prescription medicine.
Also check with your doctor if yellow or light brown crust or pus-filled blisters appear on top of the eczema. This could be the sign of a bacterial infection that needs antibiotics.
You should call your doctor if your baby is around anyone who has cold sores or genital herpes. Eczema can make your little one more likely to pick up those germs.
Eczema in children - what is eczema, photo, treatment
The disease is treated by:
Pediatric dermatologist
Last update date: 10/22/2021
Article content
- Symptoms of eczema in children
- Reasons for the appearance of
- Varieties of eczema
- Viral (exanthema)
- Seborrheic
- Atopic
- Microbial
- Mycotic ec
- Diagnosis of disease
- Treatment
Eczema is a skin disease characterized by a rash with redness, burning, and itching. Occurs from the first months of life. Has a relapsing form, is practically incurable. That is, after the symptoms disappear, they may reappear.
Occurs from the first months of life. Has a relapsing form, is practically incurable. That is, after the symptoms disappear, they may reappear.
Symptoms of eczema in children
Characteristics of the disease:
- rash;
- reddening of the skin in areas that are slightly inflamed and have signs of swelling, with clear contours;
- peeling of the skin;
- itching, worse in the evening;
- bubbles, in place of which crusts then form;
- decreased appetite;
- weakness;
- irritability.
The manifestation of these symptoms depends on the stage of the disease. In the acute period, the skin intensely reddens, swells and becomes hot to the touch. Weeping bubbles form on it. In case of infection, secondary symptoms are added to the primary symptoms - high fever, headache and muscle pain, weakness, etc.
If the pathology is not stopped within 1.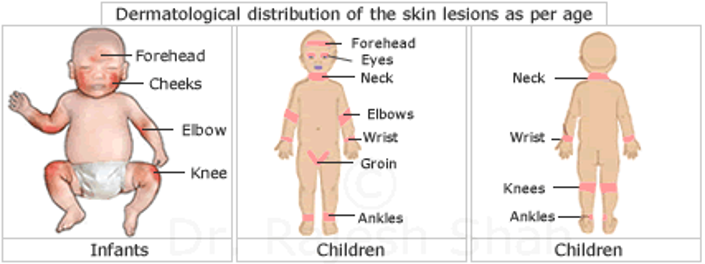 5-2 months, it passes into the subacute stage. The symptoms of the acute period become less pronounced, while the skin thickens in the affected areas. If recovery does not occur within six months, the disease passes into the chronic stage. Thickened skin in the affected areas becomes covered with scales, becomes less red and dry to the touch. Source:
5-2 months, it passes into the subacute stage. The symptoms of the acute period become less pronounced, while the skin thickens in the affected areas. If recovery does not occur within six months, the disease passes into the chronic stage. Thickened skin in the affected areas becomes covered with scales, becomes less red and dry to the touch. Source:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1199031/
Miriam Santer, Sue Lewis-Jones, Tom Fahey
Childhood eczema
// BMJ. 2005 Sep 3; 331(7515): 497
Eczema in children is relatively severe. It is characterized by increased sensitivity of the skin and mucous membranes, a decrease in resistance to infections, inflammatory foci often suppurate.
Reasons for the appearance of
One of the main reasons is heredity . In order for the disease to manifest itself, a stimulus is needed for this, which can be an allergic reaction (to children's cosmetics, household chemicals, animal hair, etc.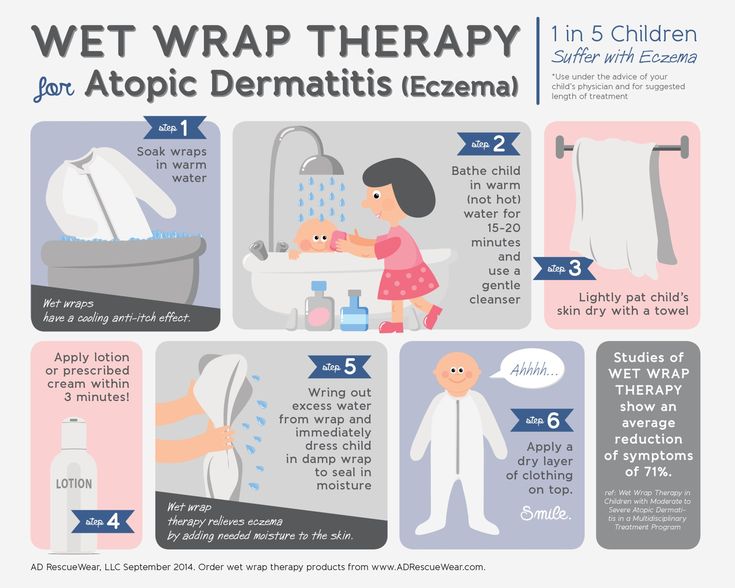 ), stress against the background of a general weakness of the body. Also the disease is caused by:
), stress against the background of a general weakness of the body. Also the disease is caused by:
- endocrine pathologies;
- infection with worms;
- viruses;
- dysbacteriosis;
- infections;
- some foods and drugs that the mother consumes if the child is breastfed.
Each of these factors alone does not cause disease. Several equivalent reasons are involved in the development of "weeping lichen". As a result, an unusual response of the body to internal and external influences is formed.
Eczema in a child can occur on the body, legs, arms, face, head, fingers, behind the ears, on the elbows.
"Weeping lichen" manifests itself on the legs rash, burning, itching early in life or during adolescence. The likelihood of its occurrence increases when the legs sweat a lot, immunity is reduced, the diet is disturbed, and the rules of personal hygiene are not observed. The skin is very dry, cracks form, causing pain.
The skin is very dry, cracks form, causing pain.
Eczema on the hands causes psychological discomfort if the child is already adapting to society, imposes restrictions on habitual actions. It arises from: prolonged contact with detergents, allergies to cat hair, certain foods, pollen, excessive sweating of the hands, excessive dryness of the skin, suppuration.
This disease is very common, localized on the elbows. With it, the skin is very dry, cracks form, the child feels itchy, the skin flakes and turns red.
Also common type of eczema is its dry form . Localization - fingers . It usually starts with one finger and spreads without treatment up to the entire hand. Clinical picture: cracks, dryness and roughness of the skin, a decrease in its elasticity, peeling, rash. Itching appears rarely, it is mild. Variety - localization between the fingers. Manifested by small bubbles, severe itching. When the bubbles burst, weeping areas form, which then coarsen, peel off, become covered with pigmentation and cracks.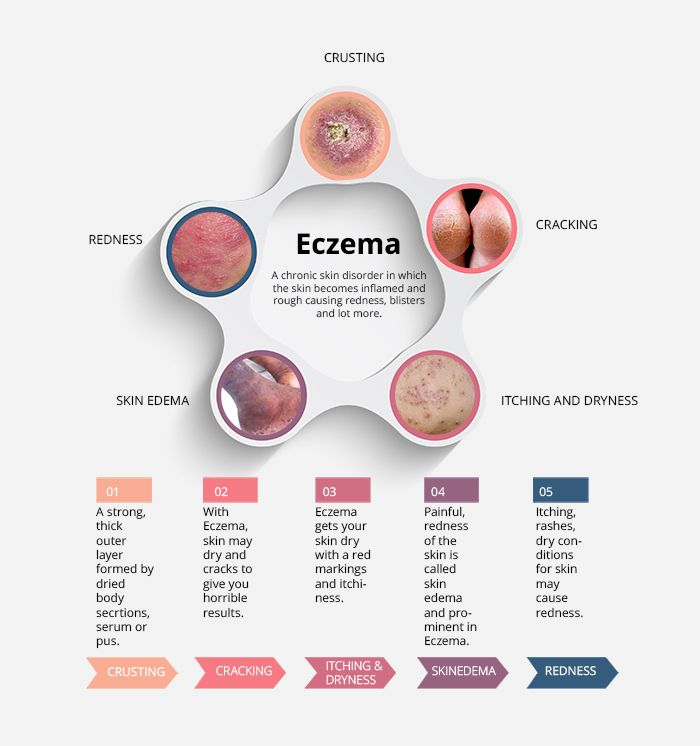
An ailment may develop on the body . In this case, an itchy rash, inflammation, vesicles and vesicles (watery cavities protruding above the surface of the skin), erosion, red spots appear. May appear in the first weeks of life.
On the head, the disease very often appears in infants as early as the 2nd week of life, when the hormonal background has not yet settled. Usually it does not bother the child, it looks like peeling.
Eczema on the face causes great discomfort because it spoils the appearance of the child. Other children shun such patients. The disease is most often acute accompanied by swelling, redness, blisters with clear liquid, itching and pain. When the bubble opens, erosion is visible in its place, then a crust forms. This cycle is repeated many times, so the face actually “blooms”: it simultaneously has erosion, bubbles, and dried areas. At the same time, the skin on the eyelids thickens and flakes off strongly, the cheeks and eyebrows give out symptoms symmetrically, the lips dry very much, they can crack and bleed, whitish scales separate from them.
The disease can be localized behind the ears. Weeping areas are formed, which then dry out, cracks form. Accompanied by itching, swelling of the skin.
Varieties of eczema
Eczema is divided into several types - true, viral, seborrheic, atopic, microbial and mycotic.
True (idiopathic) eczema
This is the most common. In the acute form, it is manifested by many microvesicles - the smallest bubbles filled with liquid. They quickly open up, forming microerosions, which are covered with granulations - crusts. The lesions begin on the face and hands, and then cover the entire body. They cause intense itching. Foci - without clear boundaries. In the chronic stage, infiltrates are formed, usually symmetrical with respect to each other.
Variety true eczema - dyshidrotic . It is localized mainly on the palms, soles, lateral surfaces of the toes and hands. Multiple vesicles are arranged in groups. Contact eczema, which occurs on open areas of the skin after contact with an allergen, is also considered true.
Contact eczema, which occurs on open areas of the skin after contact with an allergen, is also considered true.
Viral eczema (exanthema)
It develops due to the ingestion of pathogens of viral infections that affect the skin - herpes viruses, chickenpox, hepatitis B and C, Epstein-Bar and Coxsackie, enteroviruses and cytomegalovirus, adenovirus and parvovirus B19. It runs especially hard. Symptoms appear abruptly, accompanied by swelling of the skin, fever and nausea. Source:
E.O. Utenkova
Infectious exanthems in children
// Children's infections, 2018, No. 17(3)
Seborrheic
Comes after seborrhea as a complication. It is characterized by severe itching and flaking in the scalp, behind the ears and on the neck, as well as in areas where there are many sebaceous glands - between the shoulder blades, on the shoulders and in the décolleté. Accompanied by the formation of yellow-gray crusts.
Atopic
It is manifested by a reaction to external factors in the form of dryness and peeling of the skin. It is a chronic relapsing inflammation of the skin. May be complicated by fungal and microbial lesions. It often develops in infancy and, as they grow older, can go into a stage of stable remission. Source:
It is a chronic relapsing inflammation of the skin. May be complicated by fungal and microbial lesions. It often develops in infancy and, as they grow older, can go into a stage of stable remission. Source:
L.S. Namazova, Yu.G. Levina, A.G. Surkov, K.E. Efendiev, I.I. Balabolkin, T.E. Borovik, N.I. Voznesenskaya, L.F. Kaznacheeva, L.P. Mazitova, G.V. Yatsyk
Atopic dermatitis
// Pediatric pharmacology, 2006, №1, p.34-40
Microbial
These are asymmetric rashes provoked by the ingress of microbes into wounds on the skin - abrasions, scratches, fistulas. Lesions - with clear boundaries, often located on the legs and arms.
Mycotic
It develops as an allergy to a fungal infection. It is characterized by clear rounded lesions. Difficult to treat.
Disease diagnosis
The doctor makes a preliminary diagnosis based on the clinical picture and the results of the survey. To confirm it, appoint:
- general and biochemical blood tests;
- general urine analysis;
- complex allergological and immunological studies, including application skin tests.

Since the manifestations of eczema in children are sometimes similar to ringworm and scabies, histological examination of the affected tissues may be necessary for differential diagnosis.
Treatment of eczema in children
How to treat eczema in a child
The most important thing is to reliably determine the cause, then you need to exclude contact with an allergen or other provoking factor. For skin care, the doctor prescribes external medicines. It is very important not to let the baby scratch the skin, especially the baby . To do this, children cut their nails, put on special textile bags. In some cases, lotions, talc, some types of physiotherapy, hot baths, etc. are used. The doctor may prescribe oral antihistamines, anti-inflammatory and other drugs. Source:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6001985/
Simon Tso
Management of childhood eczema: reflections from secondary care
// Br J Gen Pract. Jun 2018; 68(671): 269
Jun 2018; 68(671): 269
Important! Children's allergic reactions cannot be started and treated with folk remedies. Be sure to consult a doctor for a correct diagnosis.
Sources:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1199031/
Miriam Santer, Sue Lewis-Jones, Tom Fahey. Childhood eczema // BMJ. 2005 Sep 3; 331(7515): 497. - E.O. Utenkov. Infectious exanthems in children // Children's infections, 2018, No. 17 (3).
- L.S. Namazova, Yu.G. Levina, A.G. Surkov, K.E. Efendiev, I.I. Balabolkin, T.E. Borovik, N.I. Voznesenskaya, L.F. Kaznacheeva, L.P. Mazitova, G.V. Yatsyk. Atopic dermatitis // Pediatric pharmacology, 2006, No. 1, pp. 34-40.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6001985/
Simon Tso. Management of childhood eczema: reflections from secondary care // Br J Gen Pract. Jun 2018; 68(671): 269.
Date of publication: 10/20/2017
The information in the article is provided for reference purposes and does not replace the advice of a qualified specialist. Do not self-medicate! At the first signs of the disease, you should consult a doctor.
Do not self-medicate! At the first signs of the disease, you should consult a doctor.
Eczema in children - what is eczema, photo, treatment
The disease is treated by:
Pediatric dermatologist
Last update date: 10/22/2021
Article content
- Symptoms of eczema in children
- Reasons for the appearance of
- Varieties of eczema
- Viral (exanthema)
- Seborrheic
- Atopic
- Microbial
- Mycotic ec
- Diagnosis of disease
- Treatment
Eczema is a skin disease characterized by a rash with redness, burning, and itching. Occurs from the first months of life. Has a relapsing form, is practically incurable. That is, after the symptoms disappear, they may reappear.
Symptoms of eczema in children
The disease is characterized by:
- rash;
- reddening of the skin in areas that are slightly inflamed and have signs of swelling, with clear contours;
- peeling of the skin;
- itching, worse in the evening;
- bubbles, in place of which crusts then form;
- decreased appetite;
- weakness;
- irritability.

The manifestation of these symptoms depends on the stage of the disease. In the acute period, the skin intensely reddens, swells and becomes hot to the touch. Weeping bubbles form on it. In case of infection, secondary symptoms are added to the primary symptoms - high fever, headache and muscle pain, weakness, etc.
If the pathology is not stopped within 1.5-2 months, it passes into the subacute stage. The symptoms of the acute period become less pronounced, while the skin thickens in the affected areas. If recovery does not occur within six months, the disease passes into the chronic stage. Thickened skin in the affected areas becomes covered with scales, becomes less red and dry to the touch. Source:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1199031/
Miriam Santer, Sue Lewis-Jones, Tom Fahey
Childhood eczema
// BMJ. 2005 Sep 3; 331(7515): 497
Eczema in children is relatively severe. It is characterized by increased sensitivity of the skin and mucous membranes, a decrease in resistance to infections, inflammatory foci often suppurate.
Reasons for the appearance of
One of the main reasons is heredity . In order for the disease to manifest itself, a stimulus is needed for this, which can be an allergic reaction (to children's cosmetics, household chemicals, animal hair, etc.), stress against the background of a general weakness of the body. Also the disease is caused by:
- endocrine pathologies;
- infection with worms;
- viruses;
- dysbacteriosis;
- infections;
- some foods and drugs that the mother consumes if the child is breastfed.
Each of these factors alone does not cause disease. Several equivalent reasons are involved in the development of "weeping lichen". As a result, an unusual response of the body to internal and external influences is formed.
Eczema in a child can occur on the body, legs, arms, face, head, fingers, behind the ears, on the elbows.
"Weeping lichen" manifests itself on the legs rash, burning, itching early in life or during adolescence.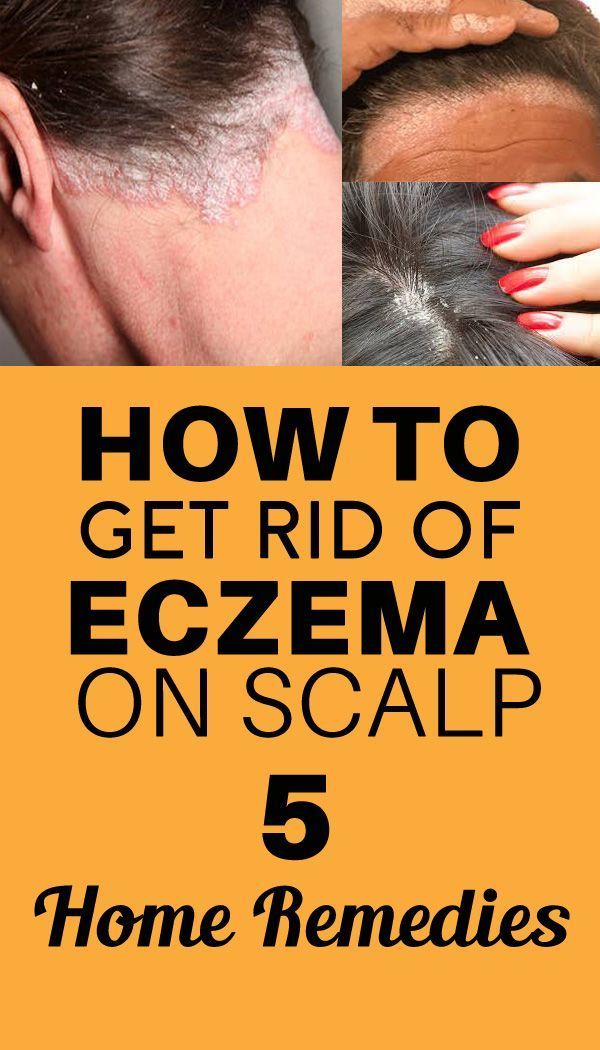 The likelihood of its occurrence increases when the legs sweat a lot, immunity is reduced, the diet is disturbed, and the rules of personal hygiene are not observed. The skin is very dry, cracks form, causing pain.
The likelihood of its occurrence increases when the legs sweat a lot, immunity is reduced, the diet is disturbed, and the rules of personal hygiene are not observed. The skin is very dry, cracks form, causing pain.
Eczema on the hands causes psychological discomfort if the child is already adapting to society, imposes restrictions on habitual actions. It arises from: prolonged contact with detergents, allergies to cat hair, certain foods, pollen, excessive sweating of the hands, excessive dryness of the skin, suppuration.
This disease is very common, localized on the elbows. With it, the skin is very dry, cracks form, the child feels itchy, the skin flakes and turns red.
Also common type of eczema is its dry form . Localization - fingers . It usually starts with one finger and spreads without treatment up to the entire hand. Clinical picture: cracks, dryness and roughness of the skin, a decrease in its elasticity, peeling, rash. Itching appears rarely, it is mild. Variety - localization between the fingers. Manifested by small bubbles, severe itching. When the bubbles burst, weeping areas form, which then coarsen, peel off, become covered with pigmentation and cracks.
Itching appears rarely, it is mild. Variety - localization between the fingers. Manifested by small bubbles, severe itching. When the bubbles burst, weeping areas form, which then coarsen, peel off, become covered with pigmentation and cracks.
An ailment may develop on the body . In this case, an itchy rash, inflammation, vesicles and vesicles (watery cavities protruding above the surface of the skin), erosion, red spots appear. May appear in the first weeks of life.
On the head, the disease very often appears in infants as early as the 2nd week of life, when the hormonal background has not yet settled. Usually it does not bother the child, it looks like peeling.
Eczema on the face causes great discomfort because it spoils the appearance of the child. Other children shun such patients. The disease is most often acute accompanied by swelling, redness, blisters with clear liquid, itching and pain. When the bubble opens, erosion is visible in its place, then a crust forms. This cycle is repeated many times, so the face actually “blooms”: it simultaneously has erosion, bubbles, and dried areas. At the same time, the skin on the eyelids thickens and flakes off strongly, the cheeks and eyebrows give out symptoms symmetrically, the lips dry very much, they can crack and bleed, whitish scales separate from them.
This cycle is repeated many times, so the face actually “blooms”: it simultaneously has erosion, bubbles, and dried areas. At the same time, the skin on the eyelids thickens and flakes off strongly, the cheeks and eyebrows give out symptoms symmetrically, the lips dry very much, they can crack and bleed, whitish scales separate from them.
The disease can be localized behind the ears. Weeping areas are formed, which then dry out, cracks form. Accompanied by itching, swelling of the skin.
Varieties of eczema
Eczema is divided into several types - true, viral, seborrheic, atopic, microbial and mycotic.
True (idiopathic) eczema
This is the most common. In the acute form, it is manifested by many microvesicles - the smallest bubbles filled with liquid. They quickly open up, forming microerosions, which are covered with granulations - crusts. The lesions begin on the face and hands, and then cover the entire body. They cause intense itching. Foci - without clear boundaries. In the chronic stage, infiltrates are formed, usually symmetrical with respect to each other.
Foci - without clear boundaries. In the chronic stage, infiltrates are formed, usually symmetrical with respect to each other.
Variety true eczema - dyshidrotic . It is localized mainly on the palms, soles, lateral surfaces of the toes and hands. Multiple vesicles are arranged in groups. Contact eczema, which occurs on open areas of the skin after contact with an allergen, is also considered true.
Viral eczema (exanthema)
It develops due to the ingestion of pathogens of viral infections that affect the skin - herpes viruses, chickenpox, hepatitis B and C, Epstein-Bar and Coxsackie, enteroviruses and cytomegalovirus, adenovirus and parvovirus B19. It runs especially hard. Symptoms appear abruptly, accompanied by swelling of the skin, fever and nausea. Source:
E.O. Utenkova
Infectious exanthems in children
// Children's infections, 2018, No. 17(3)
Seborrheic
Comes after seborrhea as a complication. It is characterized by severe itching and flaking in the scalp, behind the ears and on the neck, as well as in areas where there are many sebaceous glands - between the shoulder blades, on the shoulders and in the décolleté. Accompanied by the formation of yellow-gray crusts.
It is characterized by severe itching and flaking in the scalp, behind the ears and on the neck, as well as in areas where there are many sebaceous glands - between the shoulder blades, on the shoulders and in the décolleté. Accompanied by the formation of yellow-gray crusts.
Atopic
It is manifested by a reaction to external factors in the form of dryness and peeling of the skin. It is a chronic relapsing inflammation of the skin. May be complicated by fungal and microbial lesions. It often develops in infancy and, as they grow older, can go into a stage of stable remission. Source:
L.S. Namazova, Yu.G. Levina, A.G. Surkov, K.E. Efendiev, I.I. Balabolkin, T.E. Borovik, N.I. Voznesenskaya, L.F. Kaznacheeva, L.P. Mazitova, G.V. Yatsyk
Atopic dermatitis
// Pediatric pharmacology, 2006, №1, p.34-40
Microbial
These are asymmetric rashes provoked by the ingress of microbes into wounds on the skin - abrasions, scratches, fistulas. Lesions - with clear boundaries, often located on the legs and arms.
Lesions - with clear boundaries, often located on the legs and arms.
Mycotic
It develops as an allergy to a fungal infection. It is characterized by clear rounded lesions. Difficult to treat.
Disease diagnosis
The doctor makes a preliminary diagnosis based on the clinical picture and the results of the survey. To confirm it, appoint:
- general and biochemical blood tests;
- general urine analysis;
- complex allergological and immunological studies, including application skin tests.
Since the manifestations of eczema in children are sometimes similar to ringworm and scabies, histological examination of the affected tissues may be necessary for differential diagnosis.
Treatment of eczema in children
How to treat eczema in a child
The most important thing is to reliably determine the cause, then you need to exclude contact with an allergen or other provoking factor.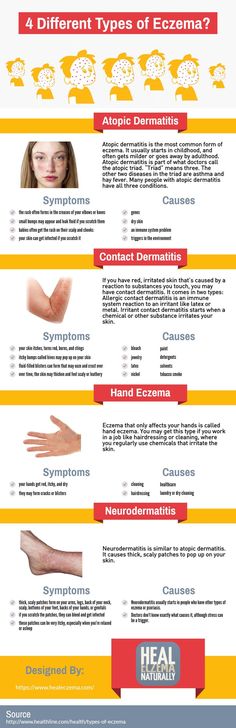 For skin care, the doctor prescribes external medicines. It is very important not to let the baby scratch the skin, especially the baby . To do this, children cut their nails, put on special textile bags. In some cases, lotions, talc, some types of physiotherapy, hot baths, etc. are used. The doctor may prescribe oral antihistamines, anti-inflammatory and other drugs. Source:
For skin care, the doctor prescribes external medicines. It is very important not to let the baby scratch the skin, especially the baby . To do this, children cut their nails, put on special textile bags. In some cases, lotions, talc, some types of physiotherapy, hot baths, etc. are used. The doctor may prescribe oral antihistamines, anti-inflammatory and other drugs. Source:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6001985/
Simon Tso
Management of childhood eczema: reflections from secondary care
// Br J Gen Pract. Jun 2018; 68(671): 269
Important! Children's allergic reactions cannot be started and treated with folk remedies. Be sure to consult a doctor for a correct diagnosis.
Sources:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1199031/
Miriam Santer, Sue Lewis-Jones, Tom Fahey. Childhood eczema // BMJ. 2005 Sep 3; 331(7515): 497. - E.O. Utenkov.