Normal bmi pregnancy
Body Mass Index, Weight Gain during Pregnancy and Obstetric Outcomes
Ghana Med J. 2010 Jun; 44(2): 64–69.
doi: 10.4314/gmj.v44i2.68886
Author information Copyright and License information Disclaimer
Objectives
To find out the effects of pregnancy weight gain in different body mass index (BMI) groups on maternal and neonatal outcomes in women delivering singletons at term.
Design
Retrospective analysis of clinical records of patients attending antenatal clinics and delivering in hospital from January 1st 1992 to December 31st 2009.
Setting
A private specialist hospital.
Methods
The records of patients starting antenatal care in the first trimester, attending at least four clinics and delivering singletons from 37 completed weeks up to 42 weeks gestation were analysed. Patients' booking gestational age, height, weight and obstetric and neonatal outcomes at delivery were noted.
Results
The total number of deliveries was 2,391 out of which 1755 (72. 4%) were analysed. The overweight and obese group compared to the normal were significantly older, shorter, weighed more at booking and gained more weight during pregnancy. The overweight or obese were significantly more likely to have induction of labour and be delivered by caesarean section compared to the normal. Maternal and neonatal outcomes which were more significant in the overweight and obese were macrosomia, stillbirth, perineal trauma, post-partum haemorrhage and retained placenta.
Conclusions
Most deliveries in the two BMI groups resulted in normal weight babies. Overweight and Obesity is associated with significantly increased incidence of adverse maternal and neonatal outcomes. It is recommended that further studies involving larger samples comparable to those done in western countries are carried out.
Keywords: body mass index, gestational weight gain, obstetric outcomes, neonatal outcomes, Ghana
Maternal weight gain in pregnancy can offer a good means of assessing the wellbeing of the pregnant mother and, by inference of her baby.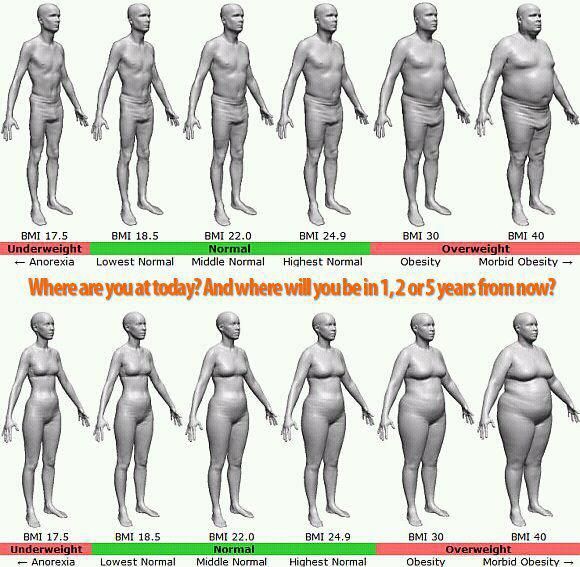 1 Inadequate prenatal weight gain is a significant risk factor for intra-uterine growth restriction, pre-term delivery and low birth weight in infants.2,3,4,5 Obesity and excessive weight gain on the other hand can lead to adverse maternal and foetal outcomes.6,7 These have led to suggestions for optimal weight gain to ensure the best outcomes.8,9,10 The Institute of Medicine (IOM) published recommended weight gains by pre-pregnancy BMI which have been the standard for subsequent research.11 These recommendations are for BMI < 19.8 kg/m2 total weight gain between 12.5 to 18 kg; BMI =19.8 to 26.0 kg/m2 total weight gain between 11.5 to 16 kg; BMI > 26.0 to 29.0 kg/m2 total weight gain between 7.0 to 11.5kg. and for BMI > 29.0 kg/m2 total weight gain of 7.
1 Inadequate prenatal weight gain is a significant risk factor for intra-uterine growth restriction, pre-term delivery and low birth weight in infants.2,3,4,5 Obesity and excessive weight gain on the other hand can lead to adverse maternal and foetal outcomes.6,7 These have led to suggestions for optimal weight gain to ensure the best outcomes.8,9,10 The Institute of Medicine (IOM) published recommended weight gains by pre-pregnancy BMI which have been the standard for subsequent research.11 These recommendations are for BMI < 19.8 kg/m2 total weight gain between 12.5 to 18 kg; BMI =19.8 to 26.0 kg/m2 total weight gain between 11.5 to 16 kg; BMI > 26.0 to 29.0 kg/m2 total weight gain between 7.0 to 11.5kg. and for BMI > 29.0 kg/m2 total weight gain of 7. 0kg.
0kg.
In earlier research the relationships between maternal height and weight with pregnancy complications were extensively explored, but in recent times, BMI is widely accepted as a better measure of over or underweight.12 More recently, the waist-hip ratio has been used to study the effects of obesity on pregnancy, but data relating to this parameter are seldom available.13 The studies conducted so far are from Western developed countries and there is a paucity of data from developing countries.14 This study was done to find out the effects of pregnancy weight gain in different BMI groups on maternal and neonatal outcomes in women delivering singleton babies at term.
The records of all patients who started their antenatal care in the first trimester, attended for antenatal care on at least four occasions and delivered in the hospital between 1st January, 1992 and 31st December, 2009 were retrieved. Using a population parameter of 34% for overweight and obese pregnant women, a sample size of 1755 was estimated at 95% confidence interval with 5% error margin and 80% power.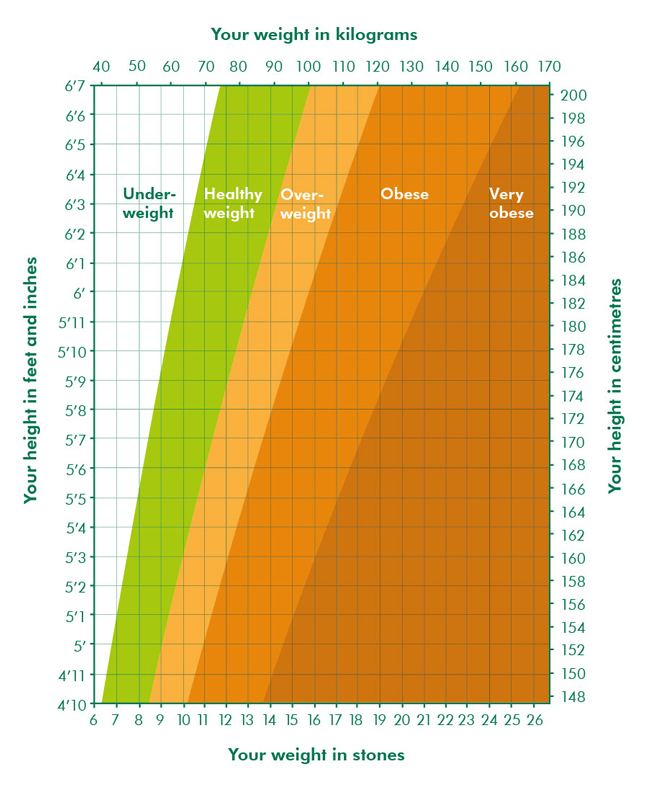 14
14
This study was conducted in Bomso Specialist Hospital in Kumasi, Ghana. This private hospital is situated in a busy cosmopolitan area close to the Kwame Nkrumah University of Science and Technology campus. Patients come from various private enterprises including mining companies, financial institutions and non-governmental organizations as well as local residents.
The Hospital offers specialist services in Medicine, Surgery, Paediatrics and Obstetrics and Gynaecology. The current delivery averages 100 annually. Only women carrying singleton pregnancies who delivered between 37 and 42 completed weeks were included. Data collected included demographic details, height and the weight at booking and at every visit. Body mass index (BMI) was calculated using the formula:
Weight in kilograms/ (height in metres) 2
Booking BMI was categorised as underweight (BMI ≤ 18.5), normal (BMI = 18.6–25.0), overweight (BMI = 25.1–30.0), and obese (BMI ≥ 30.1).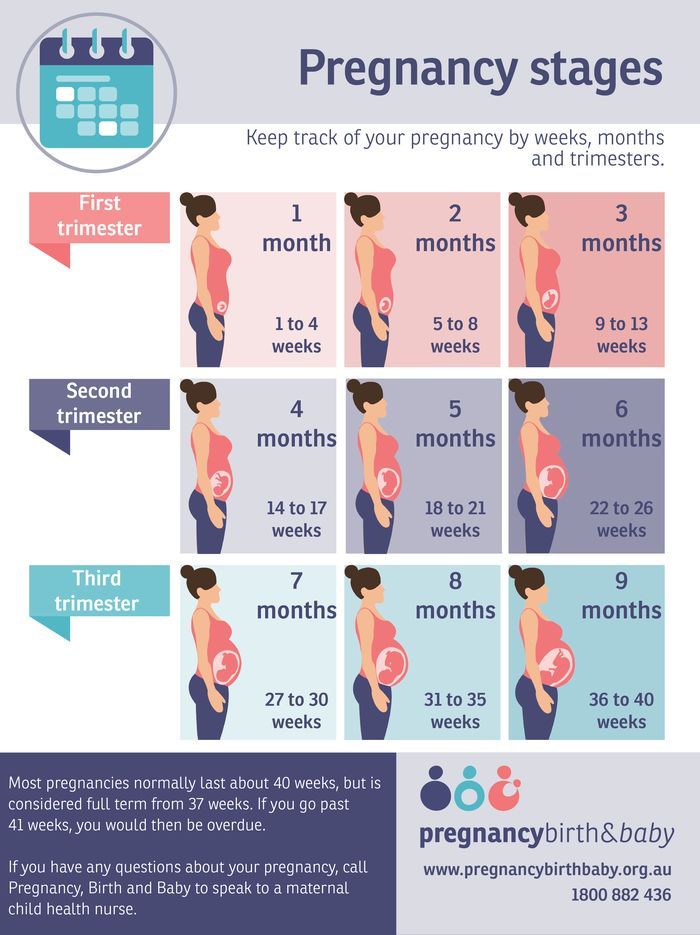 15 Gestational age (GA) was recorded according to the first day of the last normal menstrual period (LMP). Ultrasound scan-dating was performed at the first visit. If the two were in agreement, the LMP GA was used. The LMP and scan date were not to differ by more than ten days. If the difference was more than ten days then the booking scan GA was taken as the gestational age. The dating scans were performed between 10 and 13 weeks using the crown-rump length to determine gestational age.16
15 Gestational age (GA) was recorded according to the first day of the last normal menstrual period (LMP). Ultrasound scan-dating was performed at the first visit. If the two were in agreement, the LMP GA was used. The LMP and scan date were not to differ by more than ten days. If the difference was more than ten days then the booking scan GA was taken as the gestational age. The dating scans were performed between 10 and 13 weeks using the crown-rump length to determine gestational age.16
Gestational weight gain was defined as the difference between the maternal weight measured within one week prior to delivery and the maternal weight recorded at the first visit to the hospital. Gestational weight gains were grouped into three categories as low weight gain (≤ 8.0 kg), normal weight gain (8.1–16.0 kg) and high weight gain (≥ 16.1 kg).17 Labour and delivery outcomes analyzed were onset of labour (spontaneous or induced), and route of delivery-vaginal (spontaneous or vacuum extraction/forceps delivery) or caesarean section.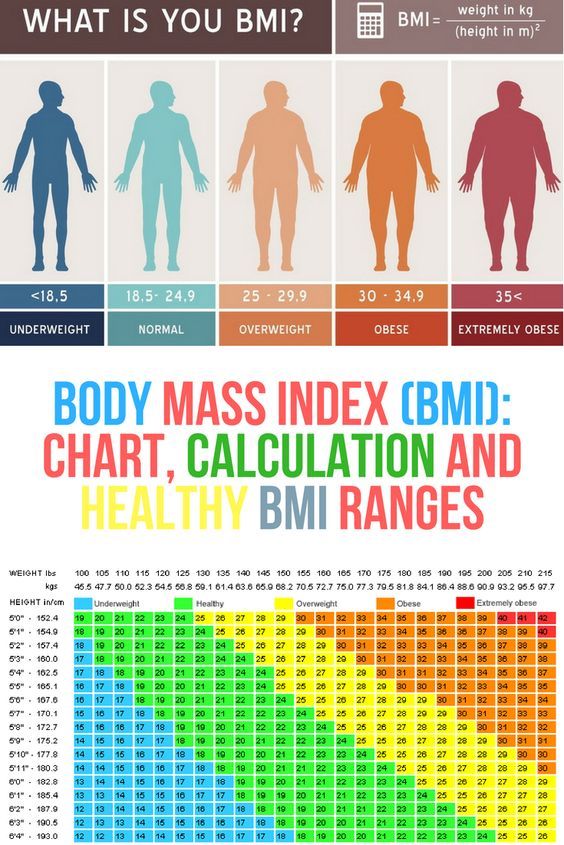 Maternal postpartum outcomes were postpartum haemorrhage, retained placenta and perineal trauma. Neonatal outcomes were birthweights, admission to neonatal intensive care unit (NICU) and stillbirths. Infant birth weights were characterized as low birthweight (LBW) ≤ 2.50kg, normal birthweight (NBW) = 2.51–3.99kg, and macrosomia ≥ 4.00kg. Data were coded and analyzed using SPSS, version 15 (SPSS, Chicago, IL, USA) and the Epidemiological Calculator, version 2.7.0 (EpiCALC).
Maternal postpartum outcomes were postpartum haemorrhage, retained placenta and perineal trauma. Neonatal outcomes were birthweights, admission to neonatal intensive care unit (NICU) and stillbirths. Infant birth weights were characterized as low birthweight (LBW) ≤ 2.50kg, normal birthweight (NBW) = 2.51–3.99kg, and macrosomia ≥ 4.00kg. Data were coded and analyzed using SPSS, version 15 (SPSS, Chicago, IL, USA) and the Epidemiological Calculator, version 2.7.0 (EpiCALC).
Frequency and proportional distribution were made to assess the distribution of observations under the three categories - obesity, overweight and underweight). For the purposes of inferential statistics, the chi square test or Fisher's exact test was used for data categorised in nominal terms to determine whether there is an association or otherwise between the variables. Student t test was used for numerical data for purposes of determining significant relationship or otherwise of observations about the three categories. The significance of an association was considered at p-value less than 0.05.
The significance of an association was considered at p-value less than 0.05.
An Odds ratio (OR) was used to determine the effects of difference among the three groups using Normal BMI as reference. The 95% confidence interval (C.I.) of an OR estimate was also determined.
The total number of deliveries during the study period was 2,391 out of which 1755 (73.4%) satisfied the study criteria. The BMI at booking classified 77/1755 (4.4%) women as underweight, 832/1755 (47.4%) as normal weight, 609/1755 (34.7%) as overweight and 314/1755 (17.9%) as obese. Parity ranged from 0 to 6 (median = 2). None of the patients smoked cigarettes nor drank alcohol and enjoyed good support from their spouses. The results of women with normal BMI are compared to those of women in the overweight and obese groups. The number of women in the underweight group was small (4.4% of the total study population) and was excluded from analysis.
shows that women in the overweight and obese group were significantly older, shorter and had higher booking weight than those in the normal group.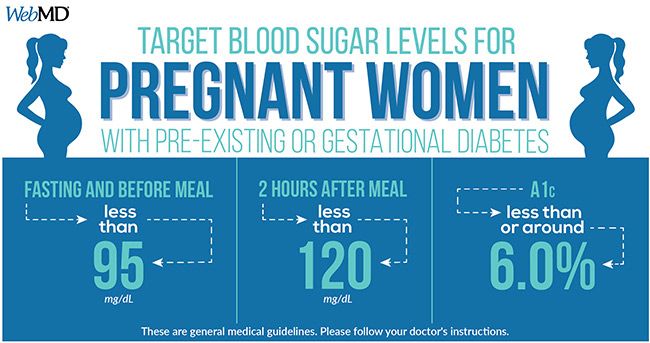 The mean weight gain between the two groups was not statistically significant (p = 0.37; [95% C.I. – 0.31, 0.11]).
The mean weight gain between the two groups was not statistically significant (p = 0.37; [95% C.I. – 0.31, 0.11]).
Table 1
Characteristics of patients in the different BMI groups
| Characteristics | Normal | Overweight + Obese | t-test | p-value | 95% CI of Mean |
| (BMI = 18.6–25.0) | (BMI ≥ 25.1) | difference | |||
| Mean (SD) | Mean (SD) | ||||
Age at delivery(yrs.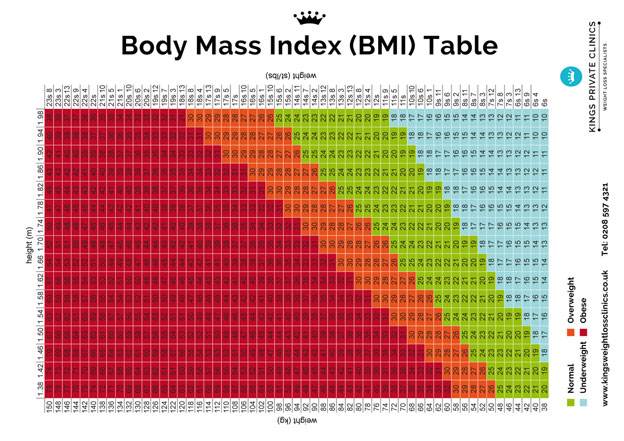 ) ) | 28.1 (5.1) | 30.2 (4.8) | 8.88 | <0.01 | [1.63, 2.56] |
| Height (m.) | 1.62 (0.07) | 1.59 (10.1) | −8.96 | <0.01 | [−0.03, −0.02] |
| Booking weight (kg.) | 57.4 (7.9) | 77.2 (9.98) | 45.74 | <0.01 | [18.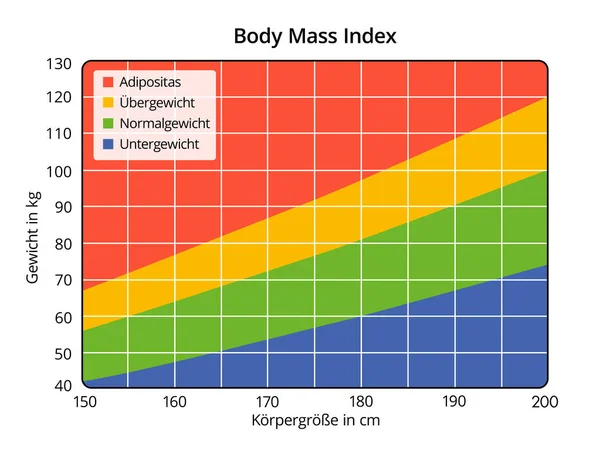 95, 20.64] 95, 20.64] |
| Mean weight gain(Kg.) | 10.0 (2.0) | 9.9 (2.6) | −0.89 | 0.37 | [−0.31, 0.11] |
| Number of subjects | 832 (47.4%) | 923 (52.6%) | |||
| (% of total 1755) | |||||
Open in a separate window
shows total weight gain by booking BMI. Total weight gain was normal in 1385/1755 (78.8%) of the patients. There was a statistically significant total weight gain in the overweight and obese compared to the normal. (p< 0.01, 95% CI= [6.41(3.63, 12.0]).
Total weight gain was normal in 1385/1755 (78.8%) of the patients. There was a statistically significant total weight gain in the overweight and obese compared to the normal. (p< 0.01, 95% CI= [6.41(3.63, 12.0]).
Table 2
Total weight gain by booking BMI
| Characteristics | Normal (BMI ≥ 18.6– 25.0) N = 832 (47.4%) | Overweight + Obese (BMI ≥ 25.1) N = 923 (52.6%) | Chi square | p-value | Odds Ratio, 95% CI of OR |
| Low weight gain ≤ 8.0 Kg. N = 259 | 124 (14. 9) 9) | 135 (14.6) | 0.41 | 0.52 | 1.09 [0.82, 1.44] |
| Normal weight gain¶ (8.1 – 16.0 Kg) N = 1385 | 693 (83.3) | 692 (75.0) | |||
| High weight gain ≥16.1Kg, N = 111 | 15 (1.8) | 96 (9.4) | 54. 99 99 | <0.01 | 6.41 [3.65, 12.0] |
Open in a separate window
¶= Reference group
shows labour and delivery outcomes. Induction of labour and delivery by caesarean section were statistically more significant in the overweight and obese group.
Table 3
Labour and delivery outcomes
| Normal (BMI = 18.6– 25.0) N = 832 (47.4%) | Overweight + Obese (BMI ≥ 25.1) N = 923 (52.6%) | Chi square | p-value | Odds Ratio, 95% CI of OR | |
| Labour and delivery outcomes | |||||
| Labour | |||||
| Spontaneous | 799 (96. 0) 0) | 859 (93.1) | |||
| Induced | 33 (4.0) | 64 (6.9) | 7.38 | <0.01 | 1.80[1.15, 2.87] |
| Delivery | |||||
| ¶Spont.Vaginal | 738 (88.7) | 695 (75.3) | |||
| Caesarean section | 84 (10. 1) 1) | 217 (23.5) | 55.54 | <0.01 | |
| 2.74[2.07,3.64] | |||||
| Vacuum/forceps | 10 (1.2) | 11 (1.2) | 0.12 | <0.72 | 1.16[0,45,3.08] |
Open in a separate window
Spont = spontaneous
¶Reference: group
Neonatal and maternal post-partum outcomes are shown in . In both BMI groups most of the newborns were of normal weight. Outcomes which were statistically significant in the overweight and obese were macrosomia, stillbirth, perineal trauma, post-partum haemorrhage and retained placenta. Outcomes which did not show significant associations were LBW babies and admission to NICU.
Outcomes which did not show significant associations were LBW babies and admission to NICU.
Table 4
Neonatal and maternal postpartum outcomes
| Outcome | Normal | Overweight + obese | Chi | p-value | Odds Ratio, |
| (BMI = 18.6–25.0) | (BMI ≥ 25.1) | square | 95% CI of OR | ||
| N = 832 (47.4%) | N = 923 (52.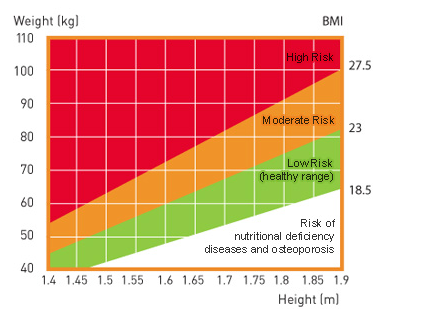 6%) 6%) | ||||
| LBW ≤ 2.50 Kg | 44 (5.3) | 36 ( 3.9) | 0.47 | 0.49 | 0.85[0.53,1.37] |
| Normal BW¶ (2.51–3.99 Kg.) | 790 (95.0) | 757 (82.0) | |||
| Macrosomia | |||||
≥ 4. 00Kg. 00Kg. | 12 (1.3) | 101 (10.9) | 68.99 | <0.01 | 8.78[4.75,17.69] |
| NICU* | 34 (4.1) | 47 (5.1) | 2.03 | 0.15 | 1.39[0.86,2.25] |
| Stillbirth | 9 (1.1) | 28 (3.0) | 9.59 | <0.01 | 3. 12[1.42, 7.57] 12[1.42, 7.57] |
| Perineal trauma | 16 (1.9) | 32 (3.4) | 5.23 | <0.01 | 2.00[1.05, 3.95] |
| Postpartum Haemorrhage | 25 (3.0) | 45 (4.9) | 5.53 | 0.02 | 1.81[1.07, 3.11 |
| Retained placenta | 9 (1.1) | 35 (3. 8) 8) | 15.02 | <0.01 | 3.90[1.82, 9.29] |
Open in a separate window
¶= reference group
*NICU = neonatal intensive care unit
Maternal weight is recorded at almost all antenatal attendances and weight gain is considered to be a significant clinical test in antenatal care. Maternal weight gain is also a measurement frequently discussed by the patient in consultation with her doctor or midwife. Concern is often expressed if the patient does not gain weight as the pregnancy progresses. The amount of maternal weight gain that is compatible with a normal outcome has been the matter of debate since the 1940s.18,19,20 These have led to studies resulting in recommended weight gains in pregnancy.21 While most reports define obesity as an increased body mass index of greater than or equal to 30 kg/m2 (IOM),others have defined it as increased waist circumference, increased waist - hip ratio or body weight of more than 90 Kg.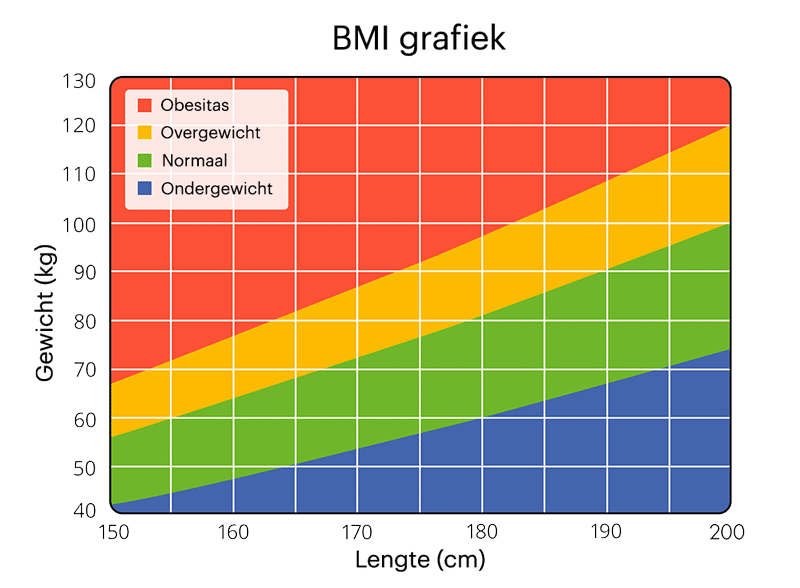 This makes comparison of studies difficult and may have implications in the management of normal pregnancy.
This makes comparison of studies difficult and may have implications in the management of normal pregnancy.
Obesity in Ghana is increasing especially among females.22,23 Maternal obesity has long been correlated with an increased risk of chronic hypertension and diabetes prior to pregnancy and adverse pregnancy outcomes including pre-eclampsia, gestational diabetes, fetal macrosomia and caesarean deliveries.24,25 The perinatal problems that have been identified with maternal obesity and pregnancy include an increased risk of birth asphyxia, birth trauma, and neonatal hypoglycaemia.26 In this study, risk factors associated with overweight and obesity were increased induction of labour, caesarean sections, macrosomic babies, stillbirths, perineal trauma, post-partum haemorrhage and retained placenta.
The limitations of this study were the relatively small sample size and that it was conducted in a private clinic. The low ratio of underweight patients may be a reflection of the generally good nutritional status of these patients and also the general notion among Ghanaians that being plump is a reflection of well-being. It is likely that if the sample size were larger or if the study were done in a public hospital other significant obstetric and neonatal complications would have been found.
The low ratio of underweight patients may be a reflection of the generally good nutritional status of these patients and also the general notion among Ghanaians that being plump is a reflection of well-being. It is likely that if the sample size were larger or if the study were done in a public hospital other significant obstetric and neonatal complications would have been found.
This study, though involving relatively small numbers, adds to the increasing body of evidence which suggests that obesity, measured by BMI, predisposes women to complicated pregnancies and increased obstetric interventions. Obstetrically, obese women may benefit from low gestational weight gain. In developing countries the paucity of research on weight gain in pregnancy and obstetric and neonatal outcomes gives cause for concern. Anaemia and low birth weight is relatively common and poor weight gain has been found to contribute to these.14 Pregnant women in these countries generally start antenatal care late and early BMI will be difficult to determine.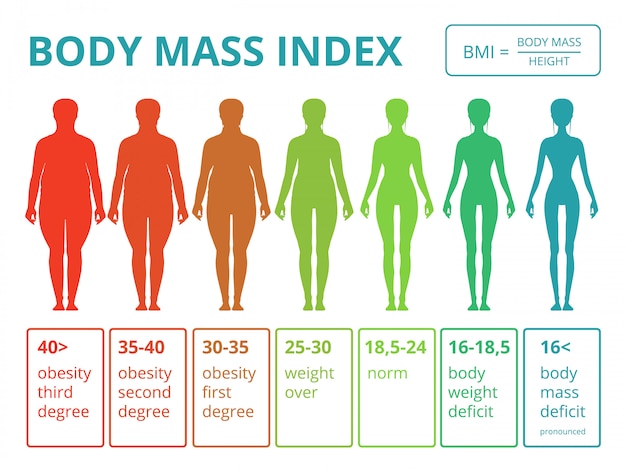 In addition weight gain will be influenced by seasonal availability of food especially in rural areas as well as high parity and breast feeding patterns.27
In addition weight gain will be influenced by seasonal availability of food especially in rural areas as well as high parity and breast feeding patterns.27
A proposal from South Africa in which monitoring of pregnant women can be done with measurements of height, weight and mid-upper arm circumference (MUAC) to classify them into various risk categories is worth exploring.28
This study has shown an association between maternal overweight and obesity and adverse pregnancy outcomes including higher caesarean section rates, stillbirths, fetal macrosomia, post-partum haemorrhage and retained placenta. Normal fetal outcome is possible throughout the range of BMI and weight gain.
It is recommended that studies enrolling larger sample sizes such as in hospitals delivering over 5,000 women per year are carried out as these are more likely to yield results comparable to those found in the large population based studies in the developed countries and add to data which is currently lacking in developing countries.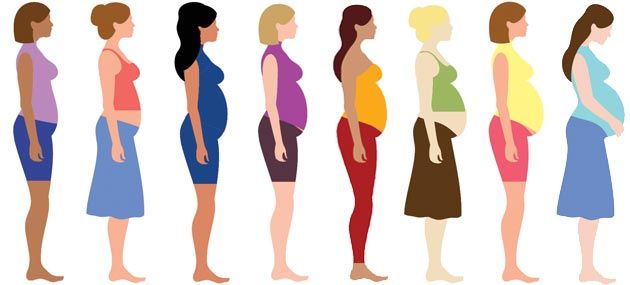 There is also the need to develop guidelines on weight gains to optimize pregnancy and neonatal outcomes.
There is also the need to develop guidelines on weight gains to optimize pregnancy and neonatal outcomes.
1. Varma TR. Maternal weight and weight gain in pregnancy and obstetric outcome. Int J Gynaecol Obstet. 1984 Apr;22(2):161–166. [PubMed] [Google Scholar]
2. Lawoyin TO. Maternal Weight and Weight Gain in Africans. Its relationship to Birth Weight. Journal of Tropical Pediatrics. 1991;37(4):166–171. [PubMed] [Google Scholar]
3. Tulman L, Morin KH, Fawcett J. Prepregnant Weight and Weight Gain During Pregnancy: Relationship to Functional Status, Symptoms, and Energy [PubMed] [Google Scholar]
4. Suitor CW. Maternal Weight Gain: A Report of an Expert Work Group. Arlington, VA: National Center for Education in Maternal and Child Health; 1997. [Google Scholar]
5. Marsoosi V, Jamal A, Eslamian L. Pre-pregnancy weight, low pregnancy weight gain, and preterm delivery. Int J Gynaecol Obstet. 2004;87:36–37. [PubMed] [Google Scholar]
6. Kumari AS. Pregnancy outcome in women with morbid obesity.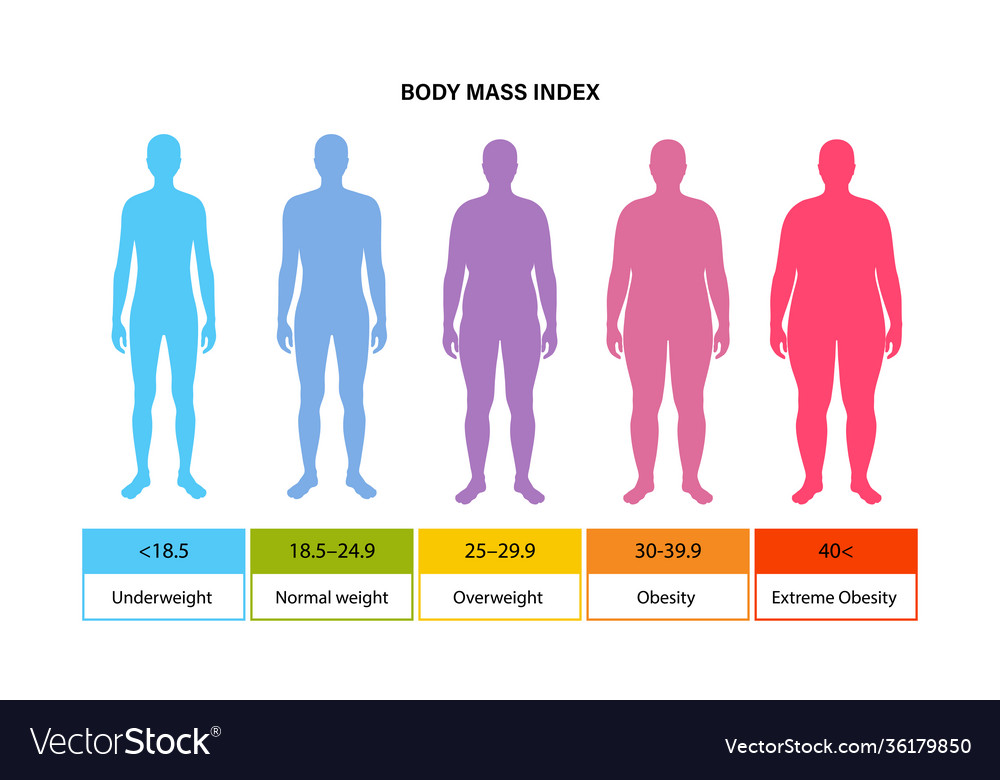 Int J Gynaecol Obstet. 2001;73:101–107. [PubMed] [Google Scholar]
Int J Gynaecol Obstet. 2001;73:101–107. [PubMed] [Google Scholar]
7. Ekblad U, Grenman S. Maternal weight, weight gain during pregnancy and pregnancy outcome. Int J Gynae Obstet. 1992;39(4):277–283. [PubMed] [Google Scholar]
8. Wells C, Murra EK. Weight Gain During Pregnancy: Colorado Pregnancy Risk Assessment Monitoring System (PRAMS) Colorado department of public Health and environment; 1997–2000. [Google Scholar]
9. Abrams B, Altman SL, Pickett KE. Pregnancy weight gain: still controversial 1–4. Am J Clin Nutr. 2000;71(suppl):1233S–1241S. [PubMed] [Google Scholar]
10. Bracero LA, Byrne DW. Optimal Maternal Weight Gain during Singleton. Pregnancy Gynecologic and Obstetric Investigation. 1998;46:9–16. [PubMed] [Google Scholar]
11. Carmichael S, Abrams B, Selvin S. The Pattern of Maternal Weight Gain in Women with Good Pregnancy Outcomes. Am J Public Health. 1997;87:1984–1988. [PMC free article] [PubMed] [Google Scholar]
12. Bhattacharya S, Campbell DM, Liston WA, Bhattacharya S. Effect of Body Mass Index on pregnancy outcomes in nulliparous women delivering singleton babies. BMC Public Health. 2007;7:168. doi: 10.1186/1471-2458-7-168. http://www.biomedcentral.com/1471-2458/7/168. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
13. Wood L. Obesity, waist-hip ratio and hunter-gatherers. BJOG. 2006;113:1110–1116. [PubMed] [Google Scholar]
14. Sahu MT, Agarwal A, Das V, Pandey A. Impact of maternal body mass index on obstetric outcome. J Obstet Gynaecol Res. 2007 Oct;33(5):655–659. [PubMed] [Google Scholar]
15. Doherty DA, Magan EF, Francis J, Morrison JC, Newnham JP. Pre-pregnancy body mass index and pregnancy outcomes. Int J Gynaecol Obstet. 2006;95:242–247. [PubMed] [Google Scholar]
16. National collaborating centre for women's and children's health, author. Antenatal care routine care for the healthy pregnant woman. NICE/RCOG press; 2008. [Google Scholar]
17. Cedergren M. Effects of gestational weight gain and body mass index on obstetric outcome in Sweden. Int J Gynaecol Obstet. 2006;93:269–274. [PubMed] [Google Scholar]
Int J Gynaecol Obstet. 2006;93:269–274. [PubMed] [Google Scholar]
18. Beilly JS, Kurland I. Relationship of maternal weight gain and weight of the newborn infant. Am J Obstet Gynecol. 1945;150:202–206. [Google Scholar]
19. Hytten FE, Leitch I. The Physiology of Human Pregnancy. 2nd ed. Oxford: Blackwell Scientific Publications; 1971. pp. 265–285. [Google Scholar]
20. Rosso P. A new chart to monitor weight gain during pregnancy. Am J Clin Nutr. 1985;41:644–652. [PubMed] [Google Scholar]
21. National Academy of Sciences, Institute of Medicine, Food and Nutrition Board, author. Nutrition During Pregnancy Part I—Weight Gain. Part II—Nutrient Supplements, Committee on Nutritional Status During Pregnancy and Lactation, Subcommittee on Dietary Intake and Nutrient Supplements During Pregnancy, Subcommittee on Nutritional Status and Weight Gain During Pregnancy. Washington, DC: National Academy Press; 1990. [Google Scholar]
22. Biritwum RB, Gyapong J, Mensah G. The epidemiology of obesity in Ghana.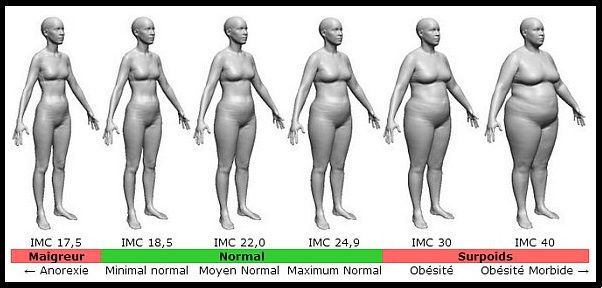 Ghana Med J. 2003;39(3):82–85. [PMC free article] [PubMed] [Google Scholar]
Ghana Med J. 2003;39(3):82–85. [PMC free article] [PubMed] [Google Scholar]
23. Ofei F. Obesity-a preventable disease. Ghana Med J. 2003;39(3):98–101. [PMC free article] [PubMed] [Google Scholar]
24. Cnattingius S, Bergstrom R, Lipworth L, Kramer MS. Prepregnancy weight and the risk of adverse pregnancy outcomes. N Engl J Med. 1998;338:147–152. [PubMed] [Google Scholar]
25. Sebire NJ, Jolly M, Harris JP, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord. 2001;25:1175–1182. [PubMed] [Google Scholar]
26. Edwards LE, Hellerstedt WL, Alton IR, et al. Pregnancy complications and birth outcomes in obese and normal-weight women: effects of gestational weight change. Obstet Gynecol. 1996;87:389–394. [PubMed] [Google Scholar]
27. Hartikainen H, Maleta KH, Kulmala T, Ashorn P. Seasonality of gestational weight gain and foetal growth in rural Malawi. East African Medical Journal. 2005;82(6):294–299. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
28. Kruger HS. Maternal anthropometry and pregnancy outcomes: a proposal for the monitoring of pregnancy weight gain in outpatient clinics in South Africa. Acta Obstet Gynecol Scand. 2007;86(1):26–32. [PubMed] [Google Scholar]
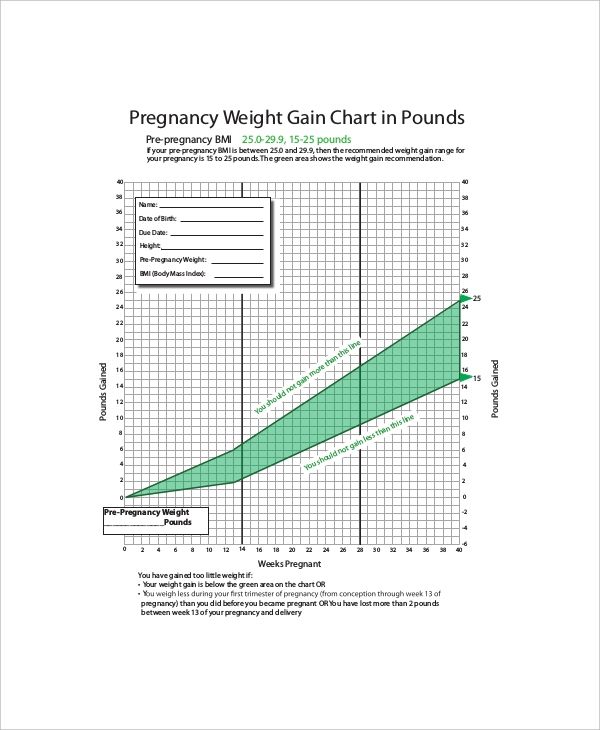
Weight Gain During Pregnancy
What you eat and how much of it is more important than ever while you are pregnant. The amount of weight you gain during your pregnancy is as essential to your health as it is to the health of your baby. While you’re pregnant, you should work closely with your doctor to make sure you keep your pregnancy weight on target.
Not gaining enough weight can jeopardize your baby’s growth and development. Gaining too much weight can cause complications during your pregnancy and make it difficult for you to lose the extra pounds after your delivery.
“Eating for two” doesn’t mean you should double-up on the food you consume. If you are a healthy weight before your pregnancy, you only need to eat an average of an extra 300 calories a day during your pregnancy — that’s a glass of skim milk and half a sandwich.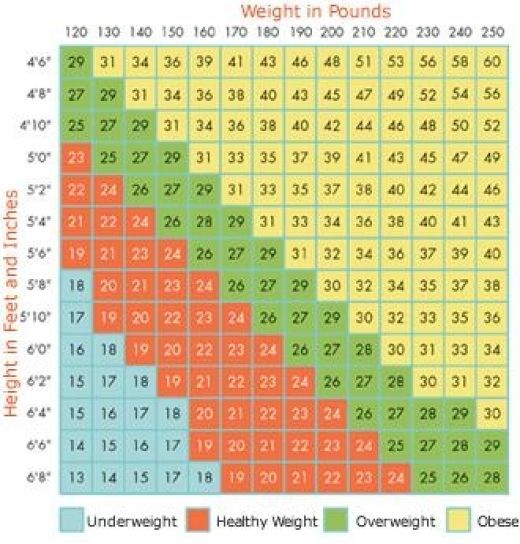
Eat a nutritious, well-rounded diet. According to the American College of Obstetricians and Gynecologists, pregnant women should have three cups of dairy, 5-6.5 ounces of protein, 1 ½-2 cups of fruits, 2 ½-3 cups of vegetables, and 6-8 ounces of whole grains every day.
How Much You Should Gain
The amount of weight you need to gain during your pregnancy depends on a number of different factors, including if you are having twins or multiples, your pre-pregnancy weight, your body mass index (BMI), and your and your baby’s overall health.
Pregnancy Weight Guidelines
| Underweight (BMI <18.5) | Healthy Weight (BMI 18.5-24.9) | Overweight (BMI 25-29.9) | Obese (BMI >30) |
|---|---|---|---|
| <80 | 80-107 | 108-128 | >128 |
| <83 | 83-111 | 112-133 | >133 |
| <86 | 86-115 | 116-138 | >138 |
| <89 | 89-110 | 120-143 | >143 |
| <92 | 92-123 | 124-148 | >148 |
| <95 | 95-127 | 128-153 | >153 |
| <98 | 98-132 | 133=158 | >158 |
| <101 | 101-136 | 137-163 | >163 |
| <105 | 105-140 | 141-169 | >169 |
| <108 | 108-145 | 146-174 | >174 |
| <111 | 111-149 | 150-179 | >179 |
| <115 | 115-154 | 155-185 | >185 |
| <118 | 118-159 | 160-191 | >191 |
| <122 | 122-164 | 165-196 | >196 |
| <125 | 125-168 | 169-202 | >202 |
| <129 | 129-173 | 174-208 | >208 |
| <133 | 133-178 | 179-214 | >214 |
| <137 | 137-183 | 184-220 | >220 |
| <140 | 140-189 | 190-227 | >227 |
| <143 | 143-194 | 195-233 | >233 |
| <148 | 149-199 | 200-239 | >239 |
Weight during pregnancy.
 What increase is considered optimal?
What increase is considered optimal? Why is excessive weight gain during pregnancy particularly harmful? What should be the calorie content of the diet? How to build your diet so that you can eat varied (and tasty), but at the same time not gain too much? Let's figure it out.
What makes up weight gain during pregnancy?
An increase in the subcutaneous fat layer during pregnancy is a normal and natural process.
While the baby is growing inside you, he needs energy and external protection. But during pregnancy, weight increases not only and not so much due to the adipose tissue of the mother: there is more fluid in the body, the uterus grows, the fetus and placenta develop, and the breasts increase in preparation for the feeding process.
Interestingly, weight loss during the period of toxicosis can later provoke its increase: the body will try to regain what was lost.
Expectant mothers especially actively gain weight in the second trimester and the beginning of the third, but closer to childbirth, a pregnant woman can even lose 1-2 kilograms.
As long as the weight increases more or less evenly and does not go beyond the upper limit of the norm, there is nothing to worry about. But if your weight is rapidly going up, you should be wary.
How to correctly calculate the weight, and what increase is considered optimal?
In Russian obstetric practice, it is generally accepted that the total gain should not exceed 12 kg. for the entire pregnancy. Of these 12 kg. 5-6 accounts for the fetus, placenta, amniotic fluid, another 1.5-2 - for an increase in the uterus and mammary glands, and only 3-3.5 - for the fat mass of a woman.
But this is a general indicator, a kind of "average temperature in the hospital." The optimal increase is calculated individually and depends on the initial weight of the pregnant woman, her age, the number of fetuses and the size of the child (children), physical activity.
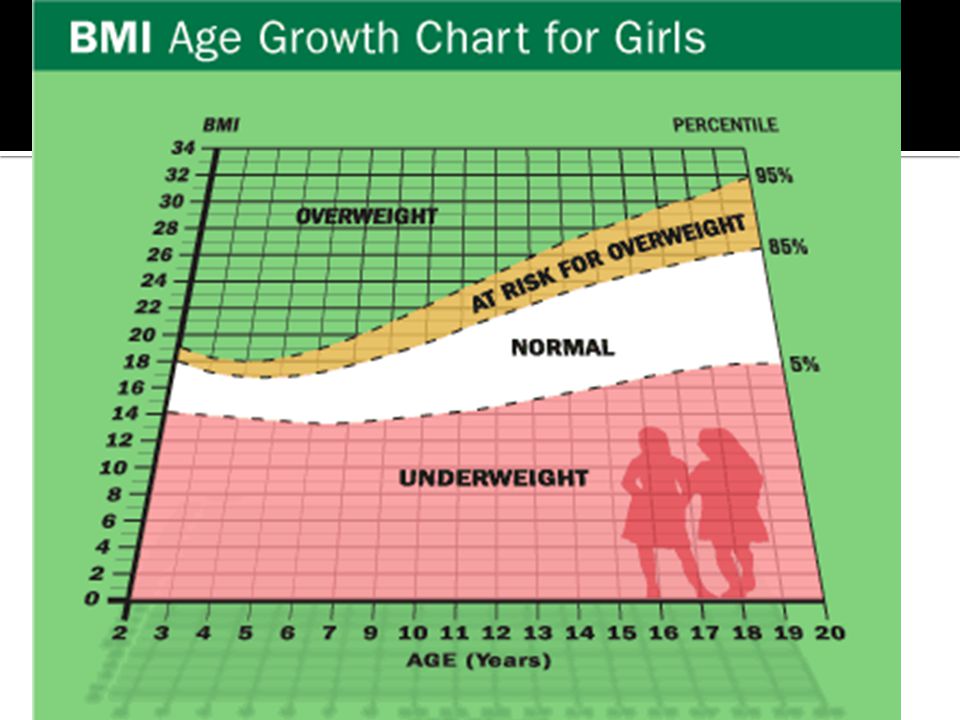
WHO recommends that optimal weight gain be calculated based on Body Mass Index (BMI).
It is determined by the formula: body weight (kg) / height squared (m).
| BMI | Recommended weight gain |
|---|---|
| 19.8-26 (normal body weight) | 12.5-15 kg |
| 26.1-29 (overweight) | 11.5 - 14 kg |
| over 29 (obese) | 7-9 kg |
How to calculate the optimal weight gain?
To do this, use the following chart:
- Calculate your BMI: divide your initial weight in kg. for height in meters squared.
For example, your "pre-pregnancy" weight was 60 kg with a height of 170 cm.
BMI = 60: (170 x 170) = 20.76.
- A BMI of less than 18.5 indicates underweight. Indicators from 18.5 to 25 are within the norm, from 25 to 30 are above the norm, and a figure greater than 30 indicates obesity.
- Now that you know your BMI, find the optimal weekly increase in the table and compare it with yours.

| Week of pregnancy | Underweight before pregnancy (BMI less than 18.5) | Normal pre-pregnancy weight (BMI 18.5 to 24.9) | Overweight before pregnancy (BMI over 30) |
|---|---|---|---|
| 4 | 0-0.9 kg | 0-0.7 kg | 0-0.5 kg |
| 6 | 0-1.4 kg | 0-1 kg | 0-0.6 kg |
| 8 | 0-1.6 kg | 0-1.2 kg | 0-0.7 kg |
| 10 | 0-1.8 kg | 0-1.3 kg | 0-0.8 kg |
| 12 | 0-2 kg | 0-1.5 kg | 0-1 kg |
| 14 | 0.5-2.7 kg | 0.5-2 kg | 0.5-1.2 kg |
| 16 | up to 3.6 kg | up to 3 kg | up to 1.4 kg |
| 18 | up to 4.6 kg | up to 4 kg | up to 2.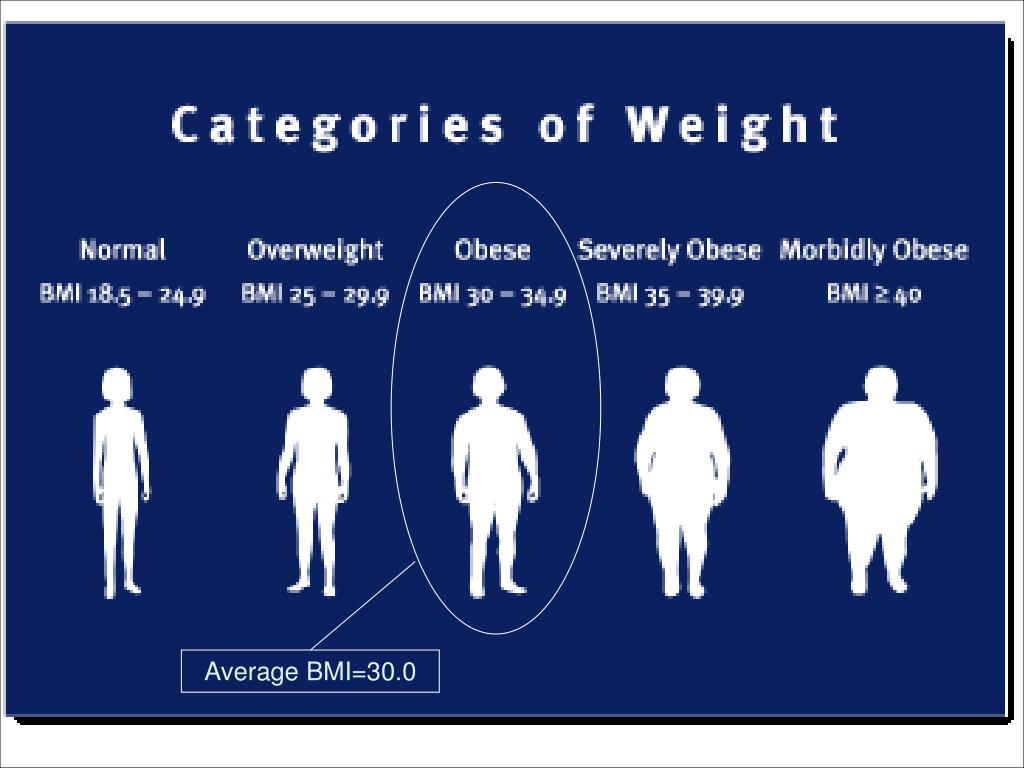 3 kg 3 kg |
| 20 | up to 6 kg | up to 5.9 kg | up to 2.9 kg |
| 22 | up to 7.2 kg | up to 7 kg | up to 3.4 kg |
| 24 | up to 8.6 kg | up to 8.5 kg | up to 3.9 kg |
| 26 | up to 10 kg | up to 10 kg | up to 5 kg |
| 28 | up to 13 kg | up to 11 kg | up to 5.4 kg |
| 30 | up to 14 kg | up to 12 kg | up to 5.9 kg |
| 32 | up to 15 kg | up to 13 kg | up to 6.4 kg |
| 34 | up to 16 kg | up to 14 kg | up to 7.3 kg |
| 36 | up to 17 kg | up to 15 kg | up to 7.9 kg |
| 38 | up to 18 kg | up to 16 kg | up to 8.6 kg |
| 40 | up to 18 kg | up to 16 kg | up to 9.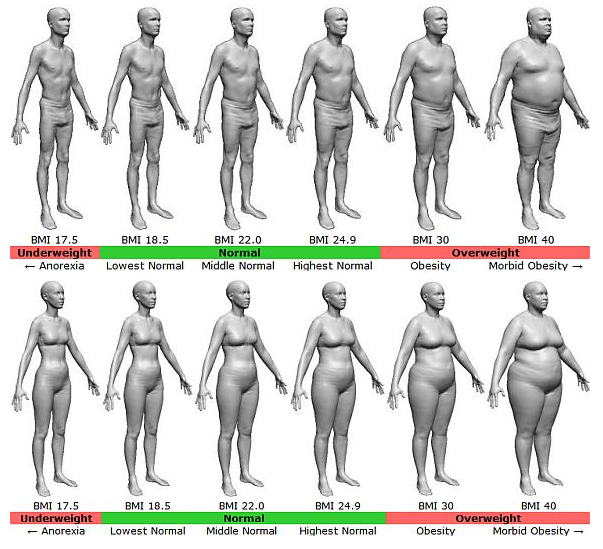 1 kg 1 kg |
Recently, doctors are increasingly talking about an individual approach and urge not to panic if the increase is slightly beyond the normal range. When assessing the state of health of a pregnant woman, the doctor focuses not only on weight, but also takes into account the results of tests and examinations and other important indicators.
Why is excessive weight gain dangerous?
Gaining extra pounds can lead to gestational diabetes, hypertension, preeclampsia, or cause a caesarean section.
In addition, excessive weight gain during pregnancy may increase the risk of obesity and associated cardiovascular disease.
What can I do to keep my weight within normal limits during pregnancy?
First of all, consult a nutritionist. If there is no such doctor in the antenatal clinic, it makes sense to contact a specialist on a commercial basis. He will develop an individual diet, which will contain all the useful elements, and will offer to keep a food diary. It will also tell you how to eat right and weigh yourself.
It will also tell you how to eat right and weigh yourself.
To prevent excessive weight gain during pregnancy, it is enough to follow simple rules of a healthy diet:
- Eat often and in small portions;
- Always keep a “healthy snack” on hand: fresh apple wedges, unsweetened crackers, dried fruit, or sugar-free yogurt;
- Refuse soda, chips, sausages and sausages;
- Minimize sweets;
- Avoid fast food;
- Limit the use of condiments, especially salt, which retains water in the body;
- Choose steamed dishes;
- Eat more fiber-rich foods such as whole grain bread, bran, vegetables;
The diet of a pregnant woman should be varied. Include grains, vegetables, fruits, dairy products, meat and fish, legumes, or nuts.
It must be remembered that expectant mothers should never starve and adhere to extreme diets.
How many calories per day do you need during pregnancy?
It is difficult to calculate the energy value per day on your own, and then strictly adhere to a certain number of calories, and it is not necessary, unless it is recommended by a nutritionist or endocrinologist. On average, you can aim for 2000-2500 calories per day, but it is important to understand that the need for calories depends on many factors: age, initial weight, health status and level of physical activity.
On average, you can aim for 2000-2500 calories per day, but it is important to understand that the need for calories depends on many factors: age, initial weight, health status and level of physical activity.
When should I be on the alert?
Strictly speaking, it is better for a pregnant woman not to worry and entrust her condition to a doctor who will control the development of pregnancy, analyzes and monitor weight. It is important to take tests to determine the level of fasting blood glucose once a trimester. The appearance of glucosuria, an increase in fasting blood glucose (more than 5.5 mmol / l) or an hour after a meal (more than 7.7 mmol / l) indicate the possible development of "diabetes in pregnancy", in connection with which the doctor will prescribe appropriate treatment . In addition, a sharp increase in body weight can cause preeclampsia.
These and other diseases can be dangerous, which is why you need to carefully monitor the body weight during the gestation period, but remember that pregnancy is not the time for strict diets.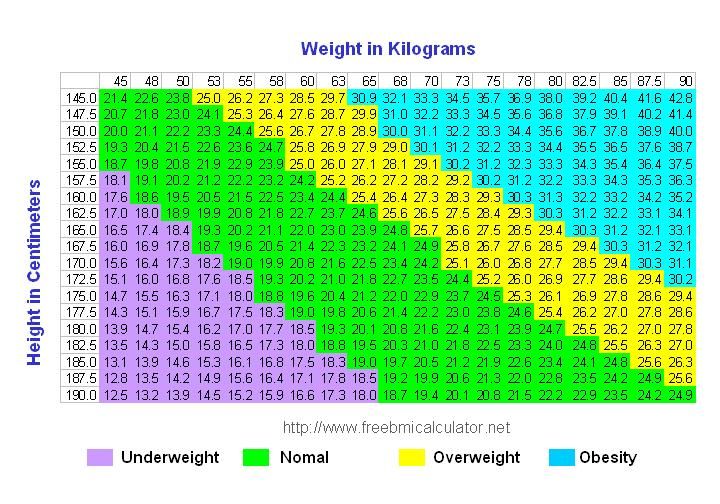
When using any materials from the site nutriclub.ru, a link to the site is required.
© Nutriclub, 2020
You will also be interested
- Nutriclub - healthy nutrition and child development
- Pregnancy
- Mom's health and well-being
- weight during pregnancy. What increase is considered optimal? - Nutriclub
Pregnancy weight gain - What is BMI?
- Contents
Every woman gains a certain amount of weight during pregnancy. But in this case, it cannot be called superfluous, since each kilogram appears for a reason. You should not be afraid of such weight gain, because often after childbirth, most women manage to quickly return to their usual form. However, one should not “launch” oneself either - too rapid weight gain at each stage of pregnancy can have negative consequences. Everything should be in moderation, and in order to control it, you need to know in advance what should be the rate of weight gain during pregnancy.
Everything should be in moderation, and in order to control it, you need to know in advance what should be the rate of weight gain during pregnancy.
What is the normal weight gain during pregnancy?
This indicator is individual. Some gain only 5-6 kg, feeling fine, having no problems with bearing a child. There are those who gain more than 20 kg, also without complaints and complications. However, in most cases, the rate of weight gain during pregnancy is average between these values - 9-14 kg when carrying one child and 16-21 kg if the pregnancy is multiple.
It is also important to remember that in the first trimester a pregnant woman may not notice weight gain. Firstly, the fetus is just being formed, and it is too early to talk about its growth. Secondly, many during this period have severe toxicosis, accompanied by a deterioration in appetite and vomiting. As a result of such conditions, a woman can, on the contrary, lose a couple of kilograms. Starting from the second trimester, weight gain becomes more noticeable. Usually it is about 1 kg per month. The sharpest jump can be seen in recent months - then a woman can recover more than 400 g per week.
Usually it is about 1 kg per month. The sharpest jump can be seen in recent months - then a woman can recover more than 400 g per week.
Keep in mind that these are only generalized data and should not be taken as a hard and fast rate of weight gain during pregnancy. Only a doctor can determine whether this or that weight gain is acceptable for a woman and her fetus. This is especially true in cases where a pregnant woman has concomitant health problems, or she bears more than three children.
What increases the weight of a pregnant woman?
In order for a pregnant woman not to be afraid of the fact that she is gaining kilograms, she needs to understand where they come from.
The main sources of weight gain are:
- Fetal weight. The child in the womb is getting bigger every day, respectively, this affects the weight indicator, adding up to 3-4 kg.
- Enlargement of the uterus and amniotic fluid. Usually, at their expense, a pregnant woman gains up to 2 kg before giving birth.
- Increased blood volume in the body. This indicator can vary greatly, but usually about 1.5 kg is assigned to it.
- The appearance of additional fluid in the body. Its weight can be from 1.5 to 3 kg.
Do not forget that in the last weeks before giving birth, a woman's mammary glands begin to increase - milk accumulates in them. This process increases the total weight by about 0.5 kg.
Regardless of how a woman eats during pregnancy, avoiding the accumulation of body fat is extremely rare. The norm can be considered a situation when their weight does not exceed 3-4 kg. This indicator can be considered the most unstable. If a woman was actively involved in sports before pregnancy, she may gain less. If a pregnant woman allows herself to eat too much, or takes hormonal drugs to preserve the fetus, this can lead to a significant increase in this indicator.
What factors influence weight gain during pregnancy?
Although the sources of weight gain are clearly identified, there are internal and external factors that can affect the amount of weight gained.
The main ones are:
- Initial weight of a woman. Of course, this factor cannot be considered decisive, but it shows that usually thin women gain more extra pounds during pregnancy than obese women.
- Growth of a pregnant woman. Tall women tend to gain more kg.
- Tendency to be overweight. If a woman has such a predisposition, she needs to be especially careful, because during pregnancy she can gain a lot of extra pounds.
- Strong increase in appetite. This factor is not common to everyone, but to the majority. Feeling a sharp increase in appetite, women can succumb to it, or vice versa - try to restrain themselves, controlling weight gain in themselves and in the fetus.
- The presence of toxicosis. If such conditions are frequent and severe, it can lead to weight loss, which is highly undesirable during pregnancy.
- Presence of comorbidities, such as diabetes. In this case, a violation of metabolic processes is possible, which will cause weight gain.

It is worth remembering that age can also affect the rate of weight gain. The older a woman is, the more difficult it is for her to control her weight gain during pregnancy. Therefore, for those who give birth in adulthood, it is important to pay special attention to this issue.
BMI when calculating weight gain
BMI is one of the basic concepts that can be used to control the process of weight gain during pregnancy. This indicator is calculated quite simply - according to the formula: the usual weight of a person must be divided by his height (m) squared.
The resulting figure can be attributed to 3 types of figure:
- up to 19.8 (Group 1) - the thinnest women
- 19.8-26 (Group 2) - women with an average build
- from 26 (3 group) - obese women
For example
With a height of 1.75 m, a woman weighs 65 kg.
1.75*1.75≈3.
65:3=21.6
It is the body mass index that is used to calculate the rate of weight gain during pregnancy by trimesters or weeks. The easiest way to do this is to use a weight gain calculator.
The easiest way to do this is to use a weight gain calculator.
The risk of being underweight during pregnancy
Severe weight loss during pregnancy or simply underweight can adversely affect the health of both the woman and the child.
Possible risks are:
- premature birth, which can be very dangerous for both the mother and the baby
- too low birth weight, which can cause health problems
- baby's weight in the first months after birth
To exclude the possibility of such unpleasant situations, it is important to notice the underweight in time and determine its cause. It may consist in malnutrition, severe toxicosis, etc. Usually, such conditions can be successfully corrected by taking special medications or diets.
Why is too rapid weight gain during pregnancy dangerous?
Rapid weight gain during pregnancy, as well as its reduction, is fraught with the following pathologies:
- development of gestational diabetes mellitus
- increased blood pressure
- risk of preeclampsia - severe deterioration of the pregnant woman in the last weeks before childbirth permanent
- pain
- premature aging of the placenta
- metabolic disorder
It is important to remember that if an expectant mother recovers rapidly, the same happens to the fetus. Its large weight can complicate the process of natural childbirth, because of which you will have to do a caesarean. It also increases the risk of preterm birth with complications.
Its large weight can complicate the process of natural childbirth, because of which you will have to do a caesarean. It also increases the risk of preterm birth with complications.
How to maintain a correct BMI during pregnancy: nutritional tips
No matter how much a woman gains weight during pregnancy, it is important for her to follow a healthy diet. In addition to the ability to maintain normal weight, it will also help maintain the health of the pregnant woman and the child.
The following recommendations can be considered universal:
- Exclusion from the diet of a large number of sweet foods, primarily flour.
- The use of fermented milk products in sufficient quantities (they will help improve metabolic processes).
- Selection of foods that contain folic acid. If this is not possible, you can take the appropriate drugs.
- Refusal of fatty, fried and smoked foods - such food can not only cause weight gain, but also negatively affect the health of the fetus, as it worsens the quality of the blood.