Milk allergy poop in babies
Milk allergy and baby poop: Pictures, symptoms, and treatment
Baby poop can vary greatly. If poop is more watery and frequent than usual and the baby has other symptoms, such as vomiting or refusing to feed, a parent or caregiver may need to consult a doctor. A cow’s milk allergy may be the cause.
Cow’s milk allergy is the most common food allergy in infants. It affects up to 3% of babies in developed countries by the time they turn 1 year of age.
This article discusses milk allergy in babies, how it affects their poop, other symptoms, and how to manage it.
Typical baby poop varies in appearance according to what the baby eats and their age.
When babies are newborn, their poop is thick and black. This is called meconium, which consists of amniotic fluid, skin cells, and other substances the fetus swallowed while in the uterus.
After the first few days, a baby’s poop will transition. The transitional stool will be more of a yellowish-green color and not as thick as meconium.
Once the baby is a few days older, their poop will depend largely on whether they drink breastmilk or formula.
A typical poop from a breastfed baby is usually yellow, green, or brown and seedy. Their stool may be quite soft or runny, but that does not necessarily mean they have diarrhea.
Babies who drink breast milk often need more nappy changes than formula-fed babies, as they digest breast milk faster.
A typical poop from a formula-fed baby is often thicker than that of a breast milk-fed baby. It will be yellow or brown and similar to the texture of peanut butter.
After around 6 months, babies begin eating solid foods. At this time, their poop often becomes firmer and the color may reflect what they eat. For example, babies who eat carrots, sweet potatoes, and pumpkin may have orange poop.
Learn more about baby poop color.
The most common sign that a baby is allergic to milk is blood in their stool. A baby’s poop may also become more runny and frequent, similar to diarrhea. It may also contain mucus.
It may also contain mucus.
Learn more about blood in a baby’s stool.
A milk allergy, sometimes called a cow’s milk protein allergy, occurs when the baby’s immune system overreacts to milk protein. It generally occurs with cow’s milk, but it can also occur with sheep and goat milk.
Although babies younger than 6 months do not usually eat solid foods, they may react to dairy proteins in formula or breast milk.
When this happens, the baby’s body will produce histamines to “attack” the milk. It is different from lactose intolerance, which occurs when a person can not digest the sugar in the milk, called lactose.
About 80% of children will outgrow the allergy by the time they reach 16 years.
The allergic reaction can cause various symptoms aside from a change in the baby’s stools.
Like other food allergies, symptoms of a cow’s milk allergy can range from mild to severe. These symptoms can include:
- hives or a red, itchy rash — though there may be no redness on darker skin
- upset stomach
- vomiting
- colic
- coughing
- wheezing
- congestion
Symptoms often start within 2 hours of coming into contact with milk but can also be immediate. They may also appear many hours later.
They may also appear many hours later.
Delayed reactions
Most reactions to milk appear soon after a baby comes into contact with milk. However, in some, a reaction can occur more than 20 hours after contact. Doctors call this delayed type hypersensitivity.
Symptoms of these delayed reactions are mainly gastrointestinal. A parent or caregiver may notice:
- changes in stool
- bloody diarrhea
- weight loss
- vomiting
- pale skin
- lethargy
Serious reactions
In rare cases, a baby may have a serious allergic reaction to milk, resulting in anaphylaxis, which can be life threatening.
Symptoms of a serious reaction include:
- difficulty breathing
- swelling of the tongue
- shock
- drop in blood pressure
Infants may also experience nonclassical signs of anaphylaxis, including:
- ear pulling
- tongue thrusting
- fussiness
- increased clinginess to the caregiver
Serious reactions generally occur within minutes of consuming milk or foods containing milk.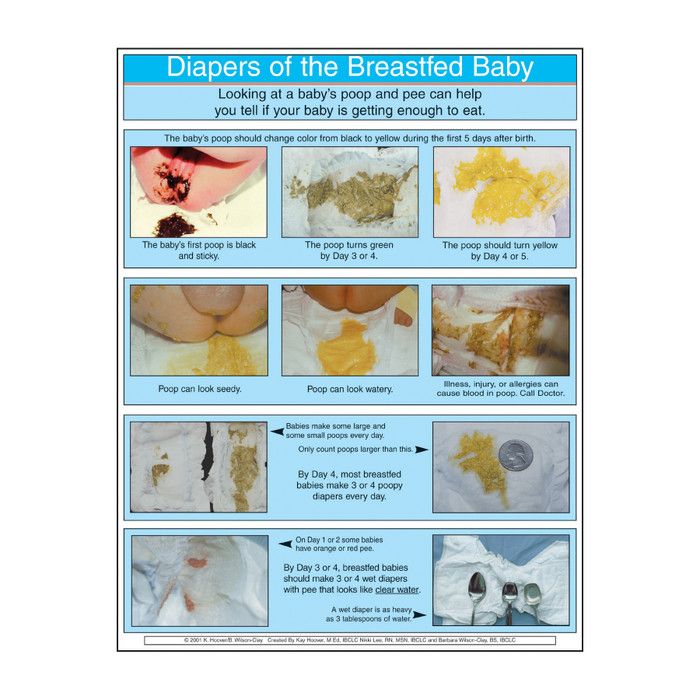
If they suspect a milk allergy, caregivers can take a baby to a pediatrician for a diagnosis. The pediatrician may recommend an appointment with an allergist.
An allergist will conduct a medical review and discuss the baby’s symptoms, including when they occur and their severity. They may also ask about the parents’ medical history.
During the exam, the doctor may recommend using a skin prick test. In this test, the doctor makes a scratch with a small milk sample on the skin. They will then wait 15–20 minutes to see if a rash or welt appears. They will likely diagnose the baby with a milk allergy if it does.
However, around half of milk allergies in babies are “nonimmunoglobulin E (IgE)-mediated.” This means they occur from a reaction involving components of the immune system other than IgE antibodies. These allergies typically take longer to present with symptoms, making them difficult to recognize. Skin testing does not help in diagnosis. In these cases, an allergist will recommend excluding milk from the diet and then reintroducing it to see if a reaction occurs. This will help confirm a cow’s milk allergy.
This will help confirm a cow’s milk allergy.
Learn more about allergy testing.
Unless the baby experiences a severe, life threatening reaction, the best treatment for a milk allergy is to avoid milk and foods containing it.
If the baby drinks formula, a doctor will recommend switching to a soy or dairy-free formula option.
Breastfed babies can react to milk proteins if the person producing breast milk consumes dairy. In these cases, the nursing individual should avoid dairy products.
For children with a food allergy, doctors may advise caregivers to carry an auto-injector containing epinephrine, which treats anaphylactic shock.
Learn about dairy milk substitutes.
At around 6 months, babies begin trying solid foods, although their main source of nutrition remains either formula or breast milk.
When introducing new foods, parents and caregivers should pay attention to food labeling. It is best to avoid all products that contain milk or dairy.
Labels may help people avoid potential exposure, but a person can also benefit from knowing which foods to avoid. Some products that contain dairy include:
- butter
- yogurt
- custard
- pudding
- milk
- some baked goods
- cheese
- cream
- ice cream
If in doubt, a parent and caregiver can talk with a health professional about foods that may cause a reaction in a baby.
A parent or caregiver should contact a doctor immediately if they notice blood in a baby’s poop. This is the most common sign of a milk allergy.
A caregiver may also want to contact a doctor if they notice any unusual digestive symptoms in their baby. A doctor can help diagnose the issue.
Babies with a milk allergy may outgrow it as they get older. About 80% of children will outgrow the allergy when they are 16 years of age.
Children who have high levels of cow’s milk antibodies in their blood are the least likely to outgrow their allergy. An allergist can use blood tests to measure a child’s antibodies.
An allergist can use blood tests to measure a child’s antibodies.
Those who do not outgrow the allergy usually need to avoid milk and dairy products. However, allergy experts suggest that consuming dairy in baked goods may help build up a tolerance. Caregivers should talk about this with an allergist before trying it at home.
Babies can react to milk proteins in formula, breast milk, or solid foods. The most common sign is blood in the stool.
Allergic reactions range from mild to severe. Mild reactions cause symptoms such as changes in the stool and vomiting. A severe reaction can cause difficulty breathing and may be life threatening. In these cases, people should seek immediate emergency help.
Most babies eventually outgrow a milk allergy. Until they do, parents and caregivers should avoid giving them dairy products. They may also need to keep an emergency epinephrine auto-injector in case of accidental exposure and a severe reaction.
Lactose Intolerant Baby Poop: Causes, Treatment, and More
Poop is a big part of parenthood, especially in those newborn and infant days. (Nod “yes” if you’re elbow deep in dirty diapers!)
(Nod “yes” if you’re elbow deep in dirty diapers!)
You may even be startled at what you find sometimes. Different colors, consistencies, and — gulp — even blood or mucus. You’re in good company, though. The good news is that most poop you see — even the really weird-looking stuff — can be totally normal.
There are a few times when you may have reason for concern, however. Take lactose, for example. It’s a sugar that’s found in both breast milk and formula. While very rare, some babies are intolerant to lactose because their bodies lack the enzyme (lactase) that digests it. With intolerance comes watery, loose stools and other digestive issues.
But loose stools can mean other things, too. So how can you tell the difference between lactose intolerance and more common issues? Let’s take a closer look.
Related: What does your baby’s poop color say about their health?
It’s important to understand that lactose intolerance is really uncommon in children under ages 2 to 3 years old. In fact, it tends to appear more often in adolescents and adults, when it’s usually known as primary lactose intolerance.
In fact, it tends to appear more often in adolescents and adults, when it’s usually known as primary lactose intolerance.
People with this condition begin life with a good supply of lactase, the enzyme that breaks down lactose. As they get older, their lactase levels may decrease dramatically and make digesting even small amounts of milk products difficult.
Primary lactase deficiency impacts up to 70 percent of people and is determined in part by genetics. It also happens to be more common in individuals of Asian, African, Hispanic, American Indian, Mediterranean, and Southern European descent. Not all people with lactase deficiency will have symptoms.
Congenital lactose intolerance
This isn’t to say that babies can’t be born with lactose intolerance. This condition is called congenital lactose intolerance, and it’s passed down genetically — in families — through what’s called autosomal recessive inheritance. This means that a baby has received the gene from both the mother and father at conception.
In a way, it’s like winning the genetic lottery, and studies consistently report that lactose intolerance is extremely rare in babies.
Infants with congenital lactose intolerance show signs right away, with the first few feedings up to 10 days old. Symptoms, like watery diarrhea, don’t take much time to develop because — unlike with primary lactose intolerance — the enzyme lactase is either deficient or simply absent from birth. You may also see this condition called:
- alactasia
- hypolactasia
- lactose malabsorption
- milk sugar intolerance
- congenital lactase deficiency
Galactosemia is another congenital condition that isn’t lactose intolerance, but may similarly affect your baby’s ability to process lactose in formula or breastmilk.
It’s a rare metabolic condition where the body either doesn’t produce any or doesn’t produce enough GALT, the liver enzyme needed to break down galactose.
Galactose is a part of the lactose sugar, but having galactosemia isn’t the same thing as being lactose intolerant. With this condition, babies may have similar symptoms, however, like diarrhea. These symptoms generally appear within a few days after birth.
With this condition, babies may have similar symptoms, however, like diarrhea. These symptoms generally appear within a few days after birth.
Galactosemia can be life-threatening if not detected early. Fortunately, the most common form is part of the standard newborn screen done in the United States.
Developmental lactose intolerance
Developmental lactose intolerance is also present at birth. It’s a result of a baby being born prematurely (before 34 weeks’ gestation). Babies born early may have lower lactase levels because this enzyme is typically produced late in the third trimester.
This form of intolerance may not last terribly long. Babies may quickly outgrow it as their small intestine matures.
Secondary lactose intolerance
Secondary lactose intolerance can affect babies, children, and adults. With this form, the small intestine lowers its lactase production in response to illness or injury.
Common offenders include things like Crohn’s disease, celiac disease, and bacterial overgrowths. With babies, this intolerance may develop after a bought of severe diarrhea, malnutrition, or other illness.
With babies, this intolerance may develop after a bought of severe diarrhea, malnutrition, or other illness.
With time, the body may be able to process lactose after receiving treatment for the underlying condition.
Related: Everything you need to know about lactose intolerance
Again, signs and symptoms of lactose intolerance in babies usually begin within a few days after birth. If your baby is fine for several months and then shows these signs, the culprit is likely not lactose intolerance — unless your little one’s been ill and develops the secondary form.
Symptoms include:
- diarrhea
- bloating, gas, and nausea
- abdominal pain and cramping
- malnutrition/failure to thrive
Since babies can’t tell you what’s bothering them, you may notice your baby is fussy or crying after feedings. Their abdomen may be swollen or firm. They may also cry when passing gas or pooping.
Diaper contents may be the clearest indicator here. Your baby’s stools may be loose and watery. They may also appear bulky or frothy. They can even be acidic, which means you may notice diaper rash from your baby’s skin becoming irritated. (Ouch!)
Your baby’s stools may be loose and watery. They may also appear bulky or frothy. They can even be acidic, which means you may notice diaper rash from your baby’s skin becoming irritated. (Ouch!)
It’s important to speak with your doctor to receive a correct diagnosis before changing formula or trying other treatments.
The rare baby with congenital lactose intolerance should be given a lactose-free formula. Without making this switch, babies may experience weight loss and dehydration. This condition can even be life-threatening if not treated promptly.
Once your baby is old enough to eat food, try focusing on calcium-rich foods to bridge that nutrition gap. These include foods like:
- broccoli
- pinto beans
- calcium-fortified soy or other milk substitutes
- calcium-fortified breads and juices
- spinach
You may also want to talk to your pediatrician about supplements to support your baby’s vitamin D levels.
There are a few other possibilities for your baby’s strange diapers. Check in with your pediatrician to make an accurate diagnosis and treatment plan.
Check in with your pediatrician to make an accurate diagnosis and treatment plan.
Milk allergy
Some babies may be allergic to cow’s milk — it’s actually one of the morecommon food allergies among children, though it is less common in younger infants.
After drinking milk, the immune system responds, causing a range of symptoms from mild to severe. This might include things like:
- wheezing
- throwing up
- getting a skin rash or hives
- having tummy troubles
Your baby may experience bouts of diarrhea or loose stools with or without blood.
Many children outgrow a milk allergy in time. Otherwise, treatment is simply avoiding formula and other foods containing milk from cows and other mammals.
There is a small risk of anaphylaxis with milk allergy, so it’s truly key to determine if your child is intolerant or allergic.
Cow milk protein intolerance
Some babies have trouble breaking down the proteins in cow’s milk. If your little one is sensitive to milk proteins, you may see diarrhea — even bloody diarrhea — and mucus in the stool. Your baby may also experience a rash, eczema, abdominal pain, or vomiting.
If your little one is sensitive to milk proteins, you may see diarrhea — even bloody diarrhea — and mucus in the stool. Your baby may also experience a rash, eczema, abdominal pain, or vomiting.
Symptoms of this intolerance tend to develop within the first week of exposure. This condition affects formula-fed babies, but milk proteins can also pass through breastmilk if a mother consumes dairy.
Some 2 to 5 percent of babies have this sensitivity, but it generally resolves by the time they reach their first birthdays. So an ice cream cake may still be an option for the big day. Ready the camera!
Foremilk/hindmilk imbalance
If you breastfeed, you may have heard that your milk is divided into two types. Foremilk may be lighter, like skim milk. Hindmilk may appear fattier, like whole milk. More foremilk is produced at the start of a nursing session. The more time your baby nurses, the more hindmilk they’ll get.
With some babies, if there’s an imbalance and baby gets too much foremilk, it may cause anything from gas to irritability. Your baby’s poop may be explosive at times. And it can look green, watery, or foamy.
Your baby’s poop may be explosive at times. And it can look green, watery, or foamy.
Related: Does my baby have a foremilk/hindmilk imbalance?
You may want to switch formulas with the guidance of your doctor if your child is allergic to milk or if they show a protein sensitivity. There are a variety of choices on the market, including soy and hypoallergenic formulas that you can purchase both over the counter and by prescription.
Breastfeeding mamas may need to modify their own diets to ensure that milk and its protein isn’t passed through down to their baby. This means avoiding obvious foods like milk, cheese, yogurt, and other dairy products.
You’ll also need to read labels carefully to look for things like dry milk solids, buttermilk, casein, and other products found in processed foods. Talk to your doctor before following any strict elimination diet, as you may be missing out on important nutrients.
If you suspect foremilk/hindmilk imbalance, a visit to a certified lactation consultant may be helpful. You may want to try feeding more frequently or feeding baby fully on one breast before changing to the next.
You may want to try feeding more frequently or feeding baby fully on one breast before changing to the next.
Related: Milk protein allergy: What are my formula options?
Poop of all colors and textures may be normal in babies. If weird-looking poop is accompanied by excessive crying, gas, blood in the stool or other symptoms, visit your pediatrician.
Lactose intolerance is rare in infants, but there are a range of other conditions and situations that may require switching formulas or trying different feeding methods to make baby happier and healthier.
Allergy to cow's milk protein in children
Food allergy is a food-induced adverse (pathological) reaction based on immune mechanisms. In children under one year of age, the most common cause of food allergy is cow's milk protein (CMP).
A distinction is made between cow's milk protein allergy and cow's milk protein intolerance. In the first case immune mechanisms are involved, in the second - the baby simply does not have enough enzymes to digest cow's milk protein (for example, lactase deficiency).
There are only 36 cow's milk protein allergens, but 4 of them most often cause food allergies.
Casein is 80% BCM, it is heat stable (does not break down when boiled) and is not a species-specific protein. This means that if you are allergic to it, you may be allergic to the milk of other animal species.
β - lactoglobulin has the highest allergenic activity, species-specific, does not break down when boiled. This protein is not found in human milk.
α - lactalbumin is destroyed by boiling, species-specific.
Bovine serum albumin is not destroyed by boiling If an allergy to this cow's milk protein is detected, the child may also react to beef and veal meat.
It should be noted that mainly children who are bottle-fed with mixtures based on cow's milk protein suffer from cow's milk protein allergy.
This type of allergy can also develop in children who are breastfed - if the diet of a nursing mother contains products containing cow's milk protein (milk, cheese, cottage cheese, sour cream, butter, fermented milk products), especially in large quantities.
What symptoms suggest that the baby may be allergic to CMP:
- Skin manifestations (dry skin, dry nummular rashes, skin itching).
- Gastrointestinal manifestations (bloating, regurgitation, vomiting, loose stools, possibly stools with mucus and blood streaks).
- Respiratory manifestations (itchy eyes, cough, nasal congestion and even urticaria and Quincke's edema). These symptoms are rare in toddlers, but still possible.
Diagnosis
I must say that if the first manifestations of a food allergy in a baby appeared after switching to artificial feeding with a "regular" adapted formula based on cow's milk, then this is a reason to suspect cow's milk proteins as an allergen.
The next thing is correct history taking : the doctor will definitely find out if anyone in your family suffers from allergic diseases (bronchial asthma, allergic rhinitis, atopic dermatitis, hay fever). If the family has these diseases, the risk of developing allergies in the baby increases.
At the discretion of the doctor, it is possible to take blood from a child for the presence of immunoglobulin E (IgE) antibodies to cow's milk proteins, which were mentioned above. In the presence of IgE antibodies to CMP in the baby's blood, almost 100% confirms that he has an allergy. Paradoxically, the absence of these antibodies does not rule out an allergy to cow's milk proteins, but only indicates that the allergy proceeds through a different type of allergic reaction.
And the simplest, most important and affordable method is the diagnostic diet with the exclusion of products from the child's diet (or from the mother's diet during breastfeeding) containing CMP. The duration of this diet is from 1-2 to 4 weeks. If during these periods there is no improvement in the condition of the baby, then an allergy to CMP is unlikely.
The duration of this diet is from 1-2 to 4 weeks. If during these periods there is no improvement in the condition of the baby, then an allergy to CMP is unlikely.
If the child's condition improves, you may need challenge test . This means the introduction of dairy products into the child's diet again. And if the manifestations of allergies return, this will prove an allergy to BCM. This test is carried out under strict medical supervision.
In children who are fed exclusively with breast milk, it is necessary to exclude products containing CMP from the mother's diet .
There are 3 types of mixtures:
- based on the hydrolysis of whey proteins;
- based on the hydrolysis of the casein fraction;
- based on amino acids.
Allergy is possible for the first two options, the reaction is very unlikely for the third option.
If the baby is bottle-fed, then it must be transferred to amino acid blend or highly hydrolyzed blend. Most infant formulas are made with whole proteins and are therefore not suitable for babies allergic to CMP. They also do not recommend hypoallergenic mixtures, since the protein in them is not sufficiently split and mixtures in goat's milk (cross-reactions).
Most infant formulas are made with whole proteins and are therefore not suitable for babies allergic to CMP. They also do not recommend hypoallergenic mixtures, since the protein in them is not sufficiently split and mixtures in goat's milk (cross-reactions).
Usually, allergists first transfer children to mixtures based on complete hydrolysis of BCM or casein, if there is no proper effect within 2-3 weeks, it is recommended to transfer the baby to an amino acid mixture.
Perhaps, if the child has severe manifestations of food allergies, the doctor will advise you to immediately transfer the baby to an amino acid mixture. By agreement with the doctor, it is possible to transfer the child to a mixture based on soy protein isolate (from 6 months).
Amino acid mixtures are more easily tolerated by children with various forms of food allergies, as they do not have the bitter taste characteristic of mixtures with a high degree of protein hydrolysis.
Amino acid mixtures can be used both for the short term diagnosis of CMP allergy and as a dietary base for long term use in children with food allergies.
Diet duration — at least 6 months . Then the issue of transferring the baby to a hypoallergenic mixture is decided. In case of recurrence of symptoms, the introduction of dairy products is postponed for another 6 months.
The prognosis for CMP allergy in infants and young children with the correct management of patients is favorable.
Approximately 50% of children by the age of 1 year can be introduced into the diet of foods that include CMP. More than 75% of children by age 3 or older 90% of children by the age of 6 do not show allergic reactions to CMP.
Good to know about MILK ALLERGY (melk)
MILK ALLERGY
Useful information about milk allergy – Information sheet of the Norwegian Asthma and Allergy Association
What is milk allergy?
When allergic to cow's milk protein, a strong reaction of the body's immune system may be the production of antibodies (IgE), or the activation of inflammatory cells. With every meal containing milk proteins, an allergic reaction of the immune system is observed in the form of the production of mediators, such as histamine, or a T-cell inflammatory reaction. Histamine is produced in several places in the body and leads to symptoms such as diarrhea, nausea, abdominal pain, or skin lesions (urticaria, eczema).
With every meal containing milk proteins, an allergic reaction of the immune system is observed in the form of the production of mediators, such as histamine, or a T-cell inflammatory reaction. Histamine is produced in several places in the body and leads to symptoms such as diarrhea, nausea, abdominal pain, or skin lesions (urticaria, eczema).
Cow's milk contains over 25 different proteins that can cause a reaction in "milk" allergy sufferers. For most people, an allergic reaction can be caused by more than one type of protein. The milk of other artiodactyls such as goat, horse and buffalo contains many of the same proteins. Therefore, allergy sufferers should not consume artiodactyl milk at all.
If a breastfeeding mother herself consumes cow's milk, some proteins may be transferred with mother's milk to the baby's body and lead to negative consequences. Therefore, a breastfeeding mother should follow a dairy-free diet.
Cow's milk allergy is not the same as lactose intolerance. The latter occurs due to the reduced ability of the body to digest milk sugar (lactose). Lactose intolerance leads to stomach pain and diarrhea as a consequence of eating large amounts of dairy products with high levels of lactose (sweet milk, brown (goat) cheese, ice cream and cream).
The latter occurs due to the reduced ability of the body to digest milk sugar (lactose). Lactose intolerance leads to stomach pain and diarrhea as a consequence of eating large amounts of dairy products with high levels of lactose (sweet milk, brown (goat) cheese, ice cream and cream).
Symptoms
The symptoms of a milk allergy are very individual. For some, they are minor and harmless, while for others, a severe allergic reaction can occur, even when drinking a small amount of milk. Gastrointestinal tract disorder is common. Not so often there is itching in the mouth and throat, swelling of the mucous membrane and breathing problems, which is especially true for young children. It is also common for them to develop eczema and hives on the skin.
Who is affected?
Milk allergy is the most common type of allergy in young children, which is explained by the early introduction of cow's milk into the diet of infants (eg cereals or mother's milk substitute). About 2-5% of Norwegian babies (0-3 years old) suffer from this type of allergy.
About 2-5% of Norwegian babies (0-3 years old) suffer from this type of allergy.
Diagnosis
In order to determine the presence of a milk allergy, the doctor must read the patient's medical history, as well as take a blood test for the presence of allergic antibodies and a Pirquet test. Not all milk allergy sufferers will show positive results from these tests. This is especially true for infants with symptoms such as vomiting, diarrhea, or blood in the stool. The only reliable way to find out if milk causes these symptoms is to eliminate milk from the diet for a period of time. When in doubt, reintroduce it back into the diet and see if symptoms return. For children who have not received milk for some time due to allergies, a control test using cow's milk should be performed to ensure that there is no allergic reaction.
Predictions
Generally, cow's milk allergy has a fairly good prognosis. Most of the children get rid of it before reaching school age. Babies who have had negative test results are often allowed to resume milk intake after half a year or a year. It is not known how many adults suffer from milk allergy, but it is estimated that this number does not exceed one percent of the population.
Babies who have had negative test results are often allowed to resume milk intake after half a year or a year. It is not known how many adults suffer from milk allergy, but it is estimated that this number does not exceed one percent of the population.
Where is milk protein found?
Milk is found in many processed and prepared industrial foods. Therefore, when buying a product, it is important to familiarize yourself with the list of substances contained in it. The goods declaration must list all ingredients containing milk. A certain group of words used in such lists indicates the content of milk protein in the product: butter, yogurt, yogurt powder.
Cocoa butter, lactic acids and group E substances do not contain milk protein.
Diet
Milk is an important source of nutrients in the Norwegian diet. 25% of the protein given to children, 70% of the iodine and about 70% of the calcium are obtained from dairy products. That is why, in cases of exclusion of dairy products from the diet, these products should be replaced with others that will provide the intake of the above nutrients.