Can birth control make you pee more
How Oral Contraceptives Wreak Havoc on the Female Body
By Joshua Gonzalez, MD
The advent of oral birth control pills in the 1960s was heralded as a huge victory for women’s rights. Finally, women could take control of their bodies and their fertility. Since then, oral contraceptive pills (OCPs) have become ubiquitous in reproductive aged women with nearly 10 million women today using The Pill as their primary means of contraception (Guttmacher).
Unfortunately, most of those women have no idea how these medications work and often have not been told of their potential side effects. Worse yet, many women are given oral birth control pills for non-contraceptive reasons: erratic mood, recurrent migraines, irregular menses, menstrual cramping, endometriosis, and even acne. Starting in adolescence, OCPs are handed out to women like candy. Women can spend many years in their young adult lives on these medications simply because they haven’t been properly counseled on alternative forms of contraception.
So what’s the big deal? Why should you be worried if you’re on an OCP? Well, let’s talk about how these medications work. OCPs are drugs mostly comprised of synthetic hormones. That is, fake hormones. These medications trick your ovary into thinking there’s enough real hormone around by exposing it to a hormone-like compound. Consequently, ovarian production of very important sex steroid hormones stops, as does ovulation. Hence, no pregnancy!
The problem is that your body needs sex steroid hormones for lots of different things. Estrogen, progesterone, and testosterone are all important for the health of a woman’s body. Yes, I said testosterone (more on that later). These hormones are important for bone health, cardiovascular health, libido, mood, cognition, and especially the health of the genital tissues. And when the body isn’t exposed to these hormones, like when you’re on an OCP, there can be consequences.
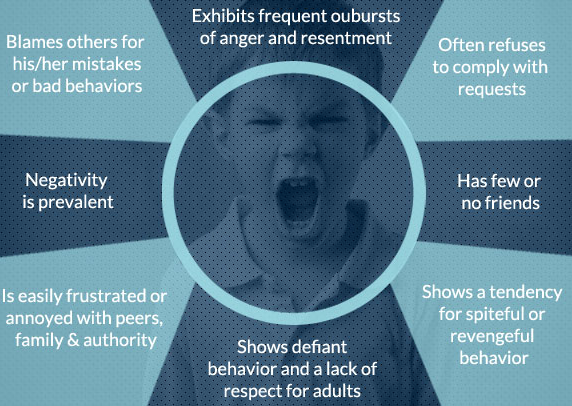
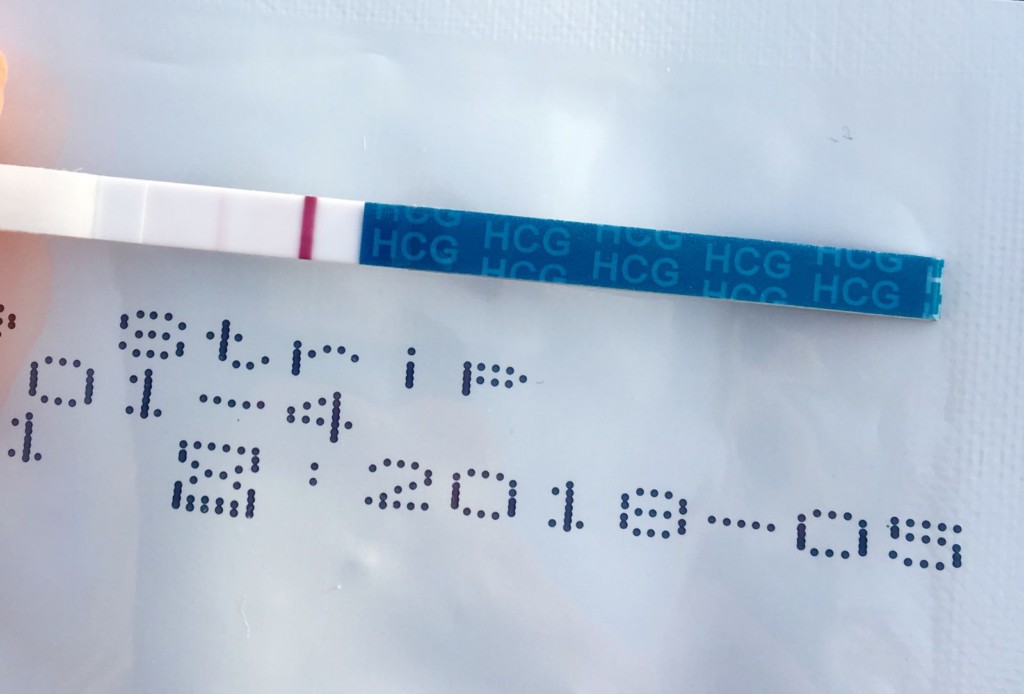
One recent study found that women using a hormonal contraceptive method experienced less frequent sexual activity, arousal, pleasure, and orgasm and more difficulty with lubrication (Smith). It is not uncommon for young women on OCPs to report pain with intercourse (called dyspareunia) as well. Some women may not experience dyspareunia but can present with other symptoms like urinary urgency, urinary frequency, recurrent urinary tract infections (UTI) or yeast infections. All of these things can happen with OCP use, but often go unrecognized or ignored.
It is not uncommon for young women on OCPs to report pain with intercourse (called dyspareunia) as well. Some women may not experience dyspareunia but can present with other symptoms like urinary urgency, urinary frequency, recurrent urinary tract infections (UTI) or yeast infections. All of these things can happen with OCP use, but often go unrecognized or ignored.
To understand why this happens, one must appreciate the anatomy of the genital tissues and how they respond differently to specific hormones. These details are not known by most patients on OCPs and often are lost on the physicians who prescribe these medications.
The female genitalia are comprised of three unique anatomic structures: the vulva, the vagina, and the vestibule. Each of these tissues arise from different embryological structures during fetal development. And each of these tissues respond uniquely to specific sex steroid hormones.
The vulva and vagina primarily rely on estrogen to maintain their health. When a woman goes through menopause and her ovary stops producing estrogen, these tissues can become dry, inflamed, chronically irritated, and literally shrink (atrophy). Similar things can happen to younger women on an OCP. When these tissues are chronically irritated they become a breeding ground for bacteria and yeast and can lead to recurrent infections. The lack of estrogen can also cause less vaginal lubrication, which can lead to pain with sexual activity.
When a woman goes through menopause and her ovary stops producing estrogen, these tissues can become dry, inflamed, chronically irritated, and literally shrink (atrophy). Similar things can happen to younger women on an OCP. When these tissues are chronically irritated they become a breeding ground for bacteria and yeast and can lead to recurrent infections. The lack of estrogen can also cause less vaginal lubrication, which can lead to pain with sexual activity.
The vestibule is a thin rim of tissue at the opening of the vagina. If you’ve never heard of it, you’re not alone. It is often ignored and easily missed during routine pelvic exams. Your gynecologist probably went right by it when she inserted that speculum. But it can cause even more problems than the vulva and vagina combined. The vestibule is an area responsible for mucus secretion, which provides lubrication during sexual activity. It is an area also intimately related to the urethra, the opening to the bladder that you urinate from.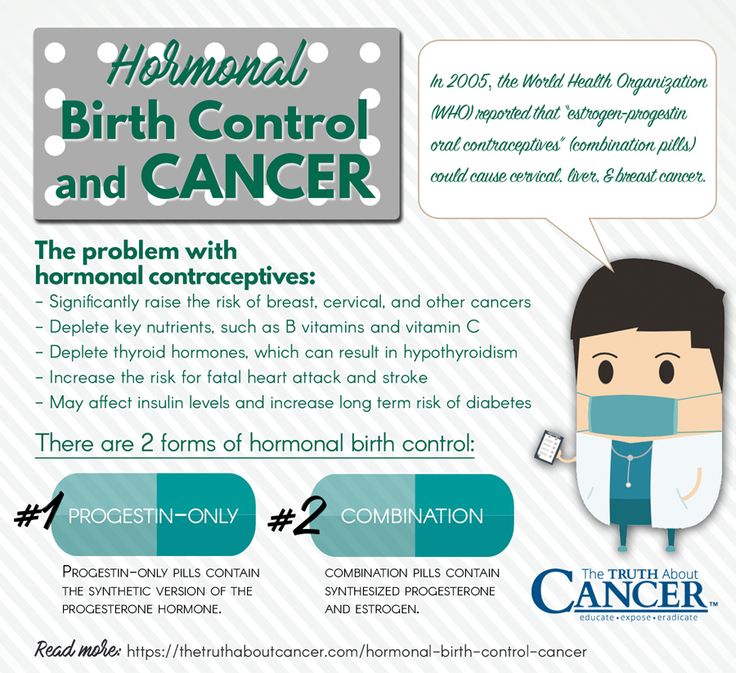 And unlike the vulva and vagina it is an area rich in testosterone receptors. When vestibular tissue is unhealthy, like when there are low levels of circulating testosterone caused by OCP use, it too becomes chronically inflamed or irritated. This can lead to pain with penetration and/or urinary symptoms that can be incorrectly assumed to be a UTI or yeast infection.
And unlike the vulva and vagina it is an area rich in testosterone receptors. When vestibular tissue is unhealthy, like when there are low levels of circulating testosterone caused by OCP use, it too becomes chronically inflamed or irritated. This can lead to pain with penetration and/or urinary symptoms that can be incorrectly assumed to be a UTI or yeast infection.
But the real damage of OCPs is their effect on a naturally occurring protein in your body called sex hormone binding globulin (SHBG). SHBG is a protein in the blood that binds testosterone and renders it inactive. Only a small amount of the testosterone your ovary makes then is actually used by the body. The rest is bound to SHBG. When women take OCPs, their SHBG skyrockets! Many physicians who prescribe these medications do not appreciate this point. With higher SHBG levels, more testosterone is bound and not usable by the body. OCPs already decrease ovarian testosterone production and now most of what’s left of your testosterone is being gobbled up by all the SHBG floating around. Worse yet, SHBG levels often remain elevated even after OCP discontinuation.
Worse yet, SHBG levels often remain elevated even after OCP discontinuation.
Many women I’ve treated have been misdiagnosed for years, told they have recurrent UTI or yeast infections or interstitial cystitis. Their physicians failed to appreciate that their symptoms were primarily a hormonal deficiency and that their OCP use was to blame. If you’re on The Pill now or were at one time you could be at risk. If you recognize or have experienced any of the symptoms I’ve mentioned, it’s worth discussing this with your health care provider. If they don’t believe you or have never heard of these potential adverse effects from OCPs, then maybe it’s time to find a new provider.
Case Example:
One particular patient stands out in my mind. When we first met, CL was 24 years old and had already been struggling with the effects of her birth control for more than two years. She first noticed pain in her vulva and vestibule (termed vulvodynia and vestibulodynia, respectively) during and after sexual intercourse. The pain was mild at first, but then intensified and lasted for longer periods as time went on. Soon she could barely sit more than a few minutes before a similar raw, burning pain would suddenly flare. She started avoiding sex and noticed a significant decrease in her libido. She began experiencing urinary frequency and urgency too. She was told by numerous physicians that she had recurrent urinary tract and yeast infections, prescribed countless rounds of antibiotics and fluconazole. She was even diagnosed and treated for interstitial cystitis. Despite being dismissed by many, she knew all the while the problem had not been addressed. This problem wasn’t in her head and it certainly wasn’t an infectious issue. Her problem was The Pill. When I first explained the real cause of her symptoms, CL cried both tears of sadness and relief.
The pain was mild at first, but then intensified and lasted for longer periods as time went on. Soon she could barely sit more than a few minutes before a similar raw, burning pain would suddenly flare. She started avoiding sex and noticed a significant decrease in her libido. She began experiencing urinary frequency and urgency too. She was told by numerous physicians that she had recurrent urinary tract and yeast infections, prescribed countless rounds of antibiotics and fluconazole. She was even diagnosed and treated for interstitial cystitis. Despite being dismissed by many, she knew all the while the problem had not been addressed. This problem wasn’t in her head and it certainly wasn’t an infectious issue. Her problem was The Pill. When I first explained the real cause of her symptoms, CL cried both tears of sadness and relief.
Women have stayed quiet about these issues for far too long because they think painful sex or recurrent infections are “normal. ” They’re not. I have no doubt that The Pill did a great deal for women’s reproductive rights, but at what cost? With alternative methods of contraception—non-hormonal, often more reliable methods—why are we still so quick to prescribe these jagged little pills. They may be easy for women to take, but the consequences may be ultimately too hard to swallow.
” They’re not. I have no doubt that The Pill did a great deal for women’s reproductive rights, but at what cost? With alternative methods of contraception—non-hormonal, often more reliable methods—why are we still so quick to prescribe these jagged little pills. They may be easy for women to take, but the consequences may be ultimately too hard to swallow.
Continue on to Part Two: Treatment solutions and alternative birth control options here.
Additional reading:
In 2015 an International Consensus Conference on Vulvar Pain was held to examine levels of evidence surrounding causes of vulvar pain and associated factors. During this meeting, it was decided that hormonal insufficiencies can cause vulvar pain. The details and resource list have been published in three locations, the references are listed below.
http://www.nva.org/wp-content/uploads/2015/01/2015_ISSVD_ISSWSH_and_IPPS_Consensus_Terminology.2.pdf
http://www.sophiebergeron.ca/images/publications/Pukall_2016_Vulvodynia. pdf
pdf
American College of Obstetrics and Gynecology: http://www.sophiebergeron.ca/images/publications/Bornstein_2015_ISSVD.pdf
References.
- https://www.guttmacher.org/united-states/contraception
- Smith NK, Jozkowski KN, Sanders SA. Hormonal contraception and female pain, orgasm and sexual pleasure. J Sex Med. 2014 Feb;11(2):462-70.
Frequent Urination, Overactive Bladder Problems
Illustrated by Mary Galloway.
This article was originally published on April 12, 2016.
As normal as it is to pee, anxiety about passing the same coworkers several times per day, every day on your way to the bathroom can build up fast. Is there such a thing as peeing too much?
Yes there is, says Raquel B. Dardik, MD, a gynecologist at NYU Langone Medical Center. But usually, frequent peeing isn't a major cause for alarm.
If you're concerned about how often you're feeling the need to go, the first thing to figure out is what "frequent" means for you, Dr. Dardik says: "Some people really do pee more often than others, but there's no specific quantity of how many times per hour or day is too much." Instead, she says a sudden change in your bathroom patterns is a more reliable sign that something is off.
But even then, the urge to urinate is a surprisingly complex process, and it may just be that you've upped your water intake. Here, we cover a few of the possible reasons you have to pee so much — plus what to do about each.
Constant Sipping
Dardik says: "Some people really do pee more often than others, but there's no specific quantity of how many times per hour or day is too much." Instead, she says a sudden change in your bathroom patterns is a more reliable sign that something is off.
But even then, the urge to urinate is a surprisingly complex process, and it may just be that you've upped your water intake. Here, we cover a few of the possible reasons you have to pee so much — plus what to do about each.
Constant Sipping
If you carry a water bottle with you everywhere out of habit (and you drink coffee, and you have a cocktail or two at happy hour), you might not realize just how often you're filling your tank. "One of the biggest culprits is actually a good, healthy habit: drinking water," says Dr. Dardik. "Young women have healthy kidneys that filter water very well." There's nothing wrong with constant sipping, but you do have to accept that frequent bathroom trips are the price. Think of it as your reminder to get up from your desk every once in awhile.
Think of it as your reminder to get up from your desk every once in awhile.
An Infection
What if you're dealing with that dreaded sudden increase in bathroom trips? The most likely culprit, especially among sexually active women in their teens and 20s, is a urinary tract infection (also called a bladder infection), Dr. Dardik explains. These usually come with other telltale signs, such as pain or burning during urination, so most women seek treatment fairly quickly.
"But if you have a mild bladder infection," Dr. Dardik explains, "you might [only] feel like you have to go to the bathroom a lot more than you used to, and not quite realize that it's because bacteria are irritating the lining of your bladder."
Luckily, mild or severe, these infections are usually easily treated with a round of antibiotics. You can also help prevent them by remembering to pee right after sex.
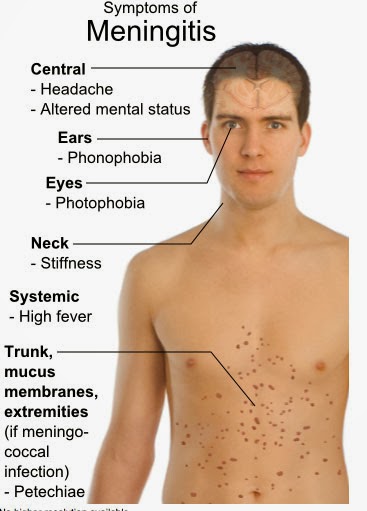
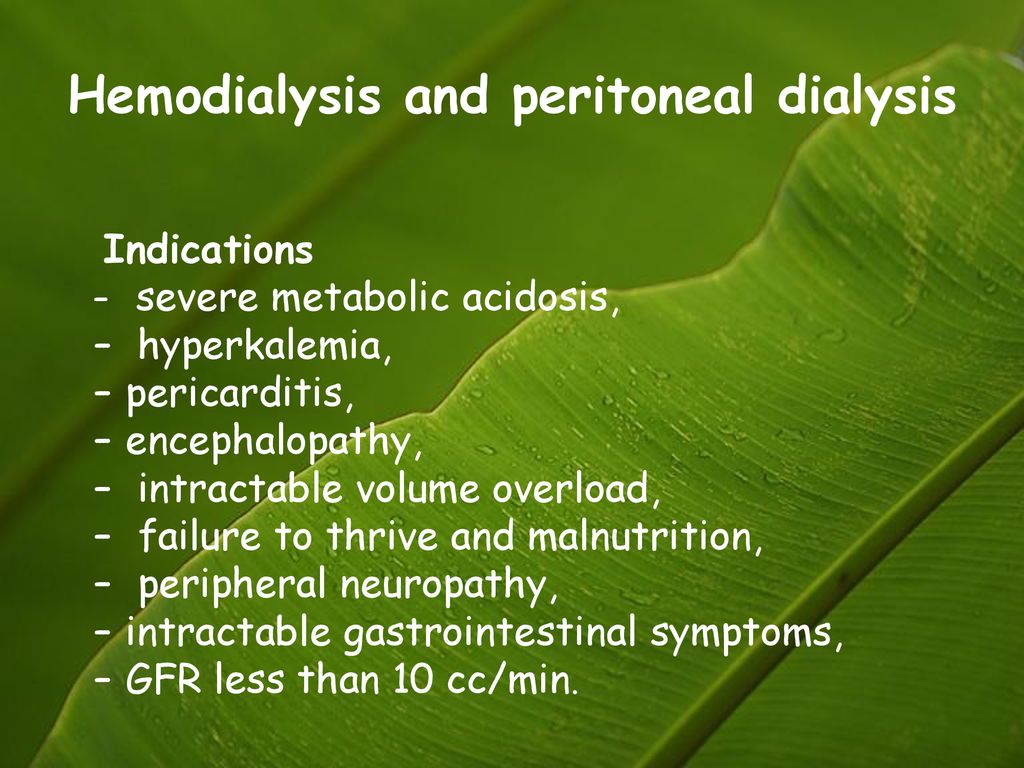
Overactive Bladder
Normally, when your bladder gets full, the muscles get stretched, and receptors in the muscle signal your brain that you need to pee. But in an overactive bladder, those receptors initiate the signal in response to the smallest stretch, even if your bladder is nowhere near full, Dr. Dardik explains. And it's extra frustrating because "a lot of times, you'll feel like you have to go that second," she adds.
Researchers are still working out what, specifically, causes the bladder to react this way, and the confusion stems partly from the fact that the condition can be so individual. "For some people, it's an 'all the time' type of problem," says Dr. Dardik. "But for other people, it's a milder problem that gets exacerbated by other things, such as stress."
If your doc thinks you might have overactive bladder, she may order tests to rule out other causes. If it turns out you do have it, she can prescribe treatments, including medications or behavioral changes such as monitoring your fluid intake and doing kegel exercises (a stronger pelvic floor seems to help), depending on the severity of your symptoms.
But in an overactive bladder, those receptors initiate the signal in response to the smallest stretch, even if your bladder is nowhere near full, Dr. Dardik explains. And it's extra frustrating because "a lot of times, you'll feel like you have to go that second," she adds.
Researchers are still working out what, specifically, causes the bladder to react this way, and the confusion stems partly from the fact that the condition can be so individual. "For some people, it's an 'all the time' type of problem," says Dr. Dardik. "But for other people, it's a milder problem that gets exacerbated by other things, such as stress."
If your doc thinks you might have overactive bladder, she may order tests to rule out other causes. If it turns out you do have it, she can prescribe treatments, including medications or behavioral changes such as monitoring your fluid intake and doing kegel exercises (a stronger pelvic floor seems to help), depending on the severity of your symptoms.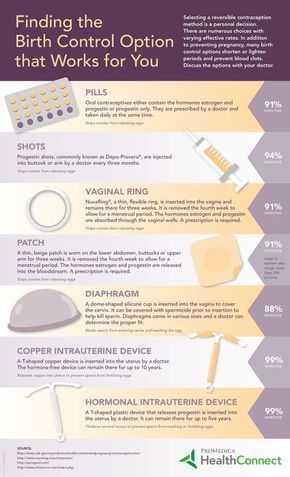 If needed, you might be referred to a specialist.
If needed, you might be referred to a specialist.
Advertisement
“
One of the biggest culprits is a good, healthy habit: drinking water.
”
Hormones
Ah, another thing your lovely hormones can do for you! The natural ebb and flow in your reproductive hormones may also affect your bladder. That could show up as a change in your bathroom habits around your period, as you head into menopause, or only when you're pregnant. Dr. Dardik says researchers still aren't sure why hormones do this, but it does seem to be the case for some women.
More Rare Causes
Less commonly, things such as fibroids (benign uterine tumors) may press on the bladder from the outside, causing you to feel like you have to pee. Most of the time, fibroids cause no symptoms and shrink on their own. But if you have one large enough to cause issues, treatment options include hormonal birth control pills to shrink it or surgery to remove it. Frequent urination can also be a symptom of other more serious conditions, such as diabetes or multiple sclerosis — which is why a constant need to pee shouldn't be ignored. (But again, these culprits are much less likely.)
Frequent urination can also be a symptom of other more serious conditions, such as diabetes or multiple sclerosis — which is why a constant need to pee shouldn't be ignored. (But again, these culprits are much less likely.)
What To Do
If you're concerned, Dr. Dardik suggests keeping a pee diary for two or three days. That'll help you pick up on patterns that might otherwise go unnoticed: Are you peeing between 10 a.m. and 1 p.m. along with your second and third cups of coffee? Or does the issue go away completely during the night and on the weekends, when you're not around a stressful work situation?
All of these clues can help pinpoint whether the issue is related to your bladder, a specific environment, or something else entirely. And that data can help your doctor immensely. Looking for these patterns is probably the first thing your doctor will ask you to do anyways, Dr. Dardik says. So coming into your appointment armed with that info will only help speed things along.
Fomin's clinic - a network of multidisciplinary clinics
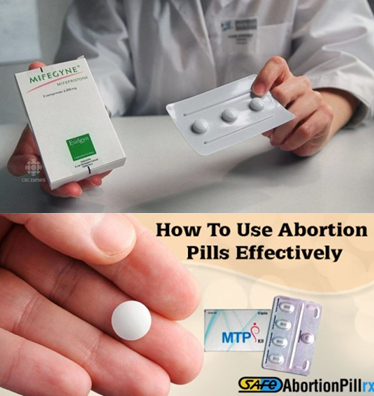
There are many methods of hormonal contraception, it is not easy to understand them. In this article, we answer the most common questions and take a closer look at the pros, cons, and subtleties of using hormonal birth control.
All processes associated with childbirth in the female body are controlled by hormones. With the help of drugs that contain synthetic analogues of female hormones, pregnancy can be prevented even at the stage of egg maturation.
Modern hormonal contraceptives can do three things:
-
do not allow the egg to leave the ovaries - that is, they stop ovulation;
-
make the mucus in the cervix thick and sticky so that sperm cannot reach the egg and fertilize it;
-
interfere with the growth of the lining of the uterus (endometrium) - as a result, a fertilized egg cannot be fixed in the uterus.
This is usually enough to prevent pregnancy. Women who use hormonal contraceptives do not need a condom "for insurance", but to protect themselves from sexually transmitted infections. Hormonal contraceptives do not protect against germs.
The British Ministry of Health estimates that when used correctly, hormonal contraceptives are more than 99% effective. But even if you use them not quite according to the instructions (for example, take a pill at the wrong time, or skip taking one pill altogether), the result will still be quite reliable: about 91% efficiency.
It is important to understand that there is no 100% reliable method of contraception. Employees of the World Health Organization (WHO) calculated the proportion of couples who used hormonal contraceptives for a whole year in full accordance with existing recommendations - that is, according to instructions and regularly. Even in this case, 0.05-0.3% of women still became pregnant.
And this is a wonderful result. In comparison, the proportion of women who became pregnant while using a male condom was 2%. Sperm-killing vaginal suppositories and gels failed the owners in 18% of cases, and vaginal diaphragms, which were used together with gels, failed in 6% of cases.
As with any drug, hormonal contraceptives have side effects, but the benefits far outweigh the harms in most cases. For example, it has recently been found that birth control pills protect women from ovarian and endometrial cancer.
It is interesting that even a complete "cancellation of menstruation" does not harm the female body. It is even useful - if a woman suffered from endometriosis before taking contraceptives, hormonal contraceptives will help relieve symptoms.
But in order for contraception to be useful, an important condition must be observed: the drug must be chosen correctly. This should be done by a doctor.
No. For most women, the ability to have children is restored in the first month after giving up hormonal contraception.
For most women, the ability to have children is restored in the first month after giving up hormonal contraception.
The only exception is injectable contraception, which lasts 3-6 months. In order for the probability of conception to be higher, it is worth waiting 6-10 months from the moment of the last injection.
Hormonal contraceptives are divided into two large groups: progestin and combined, the latter include progestins and estrogens. Although drugs from both groups prevent pregnancy, they work in slightly different ways and have different side effects.
For example, in addition to protecting against unplanned pregnancy, combined drugs treat acne and reduce menstrual pain - but more often than progestin drugs cause headaches, and they should not be used by smokers.
In addition, the difference in composition allows you to select a contraceptive for the needs of a particular woman. The drug needed by a teenager may be different from the drug needed by a forty-year-old mother of two children.
What are they. Progestin contraceptives are available in the form of tablets, subcutaneous implants, and injections.
Who suits. Universal tool, suitable for almost everyone. It is most often recommended for patients who have contraindications for combined contraceptives: nursing mothers and women who have contraindications for taking combined contraceptives.
Common side effects. Acne, breast tenderness, headaches. Sometimes spotting occurs, or these contraceptives lead to a complete absence of menstruation, which does not suit everyone.
Nuances:
If a woman has chosen pills, and more than 5 days have passed since the last menstruation, 2 more days after taking the first pill, you need to use additional methods of contraception. If less than 5 days have passed, additional contraception is not needed.
If a woman does not have a menstrual cycle and she is not pregnant, you can start taking the drug on any day of the cycle. Just in case, you need to use additional means of protection for another 2 days.
Tablets can be taken immediately after the birth of the baby, but it is better to start one month after the birth. This reduces the risk of thromboembolism - blockage of a vein by a blood clot.
If a woman chooses an injection or an implant and more than 7 days have passed since her last menstrual period, additional contraception must be used for another week. If less than 7 days have passed, additional contraception is not needed.
How to take. You can start taking pills on any day of the cycle. Stop taking - too, it is not necessary to “drink up” the package to the end.
Pros:
- Suitable for women of any age
- are suitable for both giving birth and women
- before taking the drug, you do not need to be examined by a gynecologist
Minures
- must be taken every day
9
How to use. Under local anesthesia, it is injected under the skin once every 3 years on any day of the cycle. You can extract at any time.
Pros:
- The most reliable method (less than 0.5 pregnancies per 100 women per year of use)
- The longest possible term for hormonal contraceptives is valid: 3 years
- Suitable for both women who have given birth and for women who have not given birth
- Reduce amount of menstrual flow
Cons
- Can be painful when inserting and removing the implant
How to use. Depending on the drug, once every 2-3 months on any day of the cycle, an injection is made into the gluteal muscle or into the deltoid muscle of the shoulder.
Pros:
- Convenient compared to pills: you need to think about contraception only once every 2-3 months
- Suitable for women of any age
- Suitable for women who have given birth and have not given birth
What are. Combined contraceptives come in the form of tablets, vaginal rings, and patches.
Suitable for. Most healthy non-smokers before menopause. However, all people (and drugs) are different, so you need to select pills together with a gynecologist.
Who is not suitable. Nursing mothers, women over 35 years of age who smoke more than 15 cigarettes a day, and women suffering from cardiovascular diseases, cancer, blood clotting disorders, migraine with aura, complicated diabetes mellitus and liver disease.
Nuances:
Before prescribing a combined contraceptive, the doctor should ask the patient in detail about her well-being and measure her blood pressure. The drug is not suitable for women with arterial hypertension. If the pressure is below 140/90 mm Hg. Art., the medicine can be used.
If more than 5 days have passed since the last menstruation, in order not to become pregnant, you need to use additional methods of contraception for another week. If less than 5 days have passed since the last menstruation, additional contraception is not needed. If a woman does not have a menstrual cycle, and she is not pregnant, you can start drinking the drug on any day of the cycle. Just in case, you need to use additional methods of contraception for another week.
If a woman does not have a menstrual cycle, and she is not pregnant, you can start drinking the drug on any day of the cycle. Just in case, you need to use additional methods of contraception for another week.
Combined contraceptives are not recommended for the first 3-6 weeks after birth. This will reduce the risk of thromboembolism.
How to take. Tablets should be taken one at a time, at the same time each day. If you miss even one day, there is a small risk of getting pregnant.
Most modern combined preparations are 21 tablets, after which the woman does not take the drug for 7 days, or 24 tablets with the active ingredient and 4 "pacifiers" without the active ingredient. These tablets are more convenient because they can be taken continuously.
Pros:
- Women with irregular menstruation help to normalize the cycle
- reduce the amount of menstrual discharge by 40-50%
- reduce menstrual pain in 70-80% of patients
- can be used to treat acne
- reduce blood loss and pains with pains for blood loss and pains in case fibroids and endometriosis
- Reduce the risk of certain cancers (ovarian, endometrial and colorectal cancers)
- Strengthen bones
Cons:
- Should be taken every day at the same time
- Not recommended for breastfeeding mothers
- Not suitable for everyone: there are contraindications
- Side effects: from spotting in the first month of use to headaches and depression
- All the advantages of pills, but the ring is more convenient to use
- Compared to the plaster: invisible on the body
- Can be felt inside the vagina
- May fall out - then it must be rinsed under running water and reinserted risk of disturbances in the microflora of the vagina, symptoms may increase in people with vaginosis and candidiasis
- May interfere with sexual intercourse
- All the advantages of tablets, but the patch is more convenient to use
- Compared to the vaginal ring: no problems with unpleasant sensations and with the microflora of the vagina
- The right method of hormonal contraception is a reliable and safe way to avoid an unplanned pregnancy.
- Hormonal contraceptives have contraindications, limitations and side effects. You need to choose a contraceptive with your doctor.
- If the absence of menstruation does not bother you, it is not necessary to take a break from taking contraceptives. There is no need to endure menstruation to maintain health.
- If side effects from contraceptives do not go away after 2-3 months, you need to see a doctor to help you choose a more suitable contraceptive.
- Combination tablets are available under many different names. They differ in dosage and ratio of estrogen and progestin.
- Progestin tablets are also different, depending on the combination of norethisterone or desogestrel in their composition.

- Many women experience individual intolerance to certain components of hormonal contraceptives.
- .
- Of these, 45% suffered from anxiety, the other 45% from depression.
- 46% said the pills reduced their sex drive.
- 58% believe the pills have had a negative impact on their mental health.
- 4% speak of the positive effect of the tablets.
1 How to use.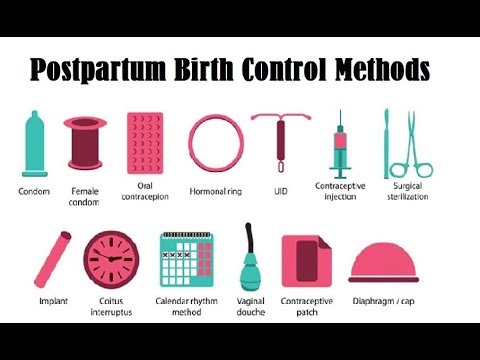 Insert into the vagina once a month, like a tampon. After 3 weeks, the ring should be removed and a week break should be taken. A week later - insert a new ring.
Insert into the vagina once a month, like a tampon. After 3 weeks, the ring should be removed and a week break should be taken. A week later - insert a new ring.
Pros:
Cons:
How to use. Stick on the stomach, thigh or shoulder. The patch should be changed once a week. After three weeks, take a break for one week.
Cons:
Gets dirty quickly and does not look aesthetically pleasing - Can often peel off, especially in summer - More often needs to be replaced than a ring - May cause skin irritation - Few options: difficult to find an alternative patch if it causes side effects
hormones, biochemistry and blood clotting is not necessary.
If the woman has had health problems, the doctor may order additional tests. This will help ensure that the contraceptive method chosen will do more good than harm.
If you are not embarrassed by the absence of menstruation, you do not need to cancel hormonal contraceptives, this will not harm your health, and will not affect your ability to have children in the future.
You can use contraceptive pills continuously to avoid periods. And if you implant an implant or regularly inject, there is a chance that your periods will pass by themselves.
Contraceptives with progestins: tablets. If you remember the missed pill within 3 hours, just take it and continue taking it as usual. Two days after that, you will have to additionally protect yourself.
If you remember the pill later, the recommendations will be the same. The only problem is that the reliability of contraception in this situation is a big question. If you keep forgetting your pills, you may be better off with another method of contraception. Contraceptives with progestins: injections. If you are less than 2 weeks late with your injection, just do it - no additional contraceptive measures are needed. If longer - too. Most importantly, make sure you're not pregnant and take extra protection for a week.
Contraceptives with progestins: injections. If you are less than 2 weeks late with your injection, just do it - no additional contraceptive measures are needed. If longer - too. Most importantly, make sure you're not pregnant and take extra protection for a week.
Combined contraceptives: tablets. If you remember the missed pill within two days, just take it, and then continue to take the pills "on schedule". It is not scary if you have to take two tablets in one day. There is no need for additional protection.
If more than two days have passed, you need to take only the last missed tablet, and continue to drink according to the "schedule". True, in this case, you will have to use additional methods of protection for a week - for example, a condom.
The risk of getting pregnant depends on which pill you forgot. If this happened at the beginning or at the end of taking the tablets with the active substance, the chance of getting pregnant is higher. In this situation, you should consult a doctor and make sure, even if less than 2 days have passed.
Combined contraceptives: ring, patch. If less than two days have passed, simply insert a new ring or apply a band-aid. Additional protection is not required. If more than 2 days have passed, use a contraceptive and additional protection for a week. It is worth consulting with your doctor: if you have had unprotected contacts, emergency methods of contraception may be required.
In this situation, doctors advise simply taking another pill, regardless of which contraceptive you used. If nausea and diarrhea persist for more than two days, act as if you missed a pill.
Side effects did not go away after 2-3 months from the start of taking the contraceptive. If spotting and nausea do not go away, you need to see a doctor to change the drug.
Bitterness in the mouth, severe dizziness and bleeding. Over time, these symptoms do not go away. If they appear, you should immediately consult a doctor to change the drug.
Follow us
"Birth control pills have made my life a nightmare"
Millions of women take birth control pills, and many are quite happy. However, there are times when these pills have a detrimental effect on the psyche.
Vicki Spratt, Associate Editor of The Debrief, tells how she battled depression, anxiety and panic attacks for years while trying to find the right medication.
How it all started o s
My mother and I came to my local doctor with a complaint that my periods had not ended for three weeks. She recommended birth control pills for me - with some reservations, of course. Pills do not protect against sexually transmitted diseases, the doctor stressed, and unprotected sex can lead to the development of cervical cancer. She was forced to say this, although I was only 14 years old, and I thought about sex last.
She recommended birth control pills for me - with some reservations, of course. Pills do not protect against sexually transmitted diseases, the doctor stressed, and unprotected sex can lead to the development of cervical cancer. She was forced to say this, although I was only 14 years old, and I thought about sex last.
Image copyright VICKY SPRATT
The nurse filled out the prescription and I ended up with a three month supply of oral contraceptives. Going to the pharmacy for green blisters with tiny yellow pills I took as a kind of rite of passage into women. These were not just pills, but a sweetened concentrate of feminism, the struggle for women's rights, medical progress.
That's how it all started. It was 14 years ago, and since then I have been "playing drug roulette" for more than ten years, testing various drugs on myself with varying success. At the same time, I began to experience anxiety, depression, and mood swings that, with minor interruptions, haunted me all my adult life.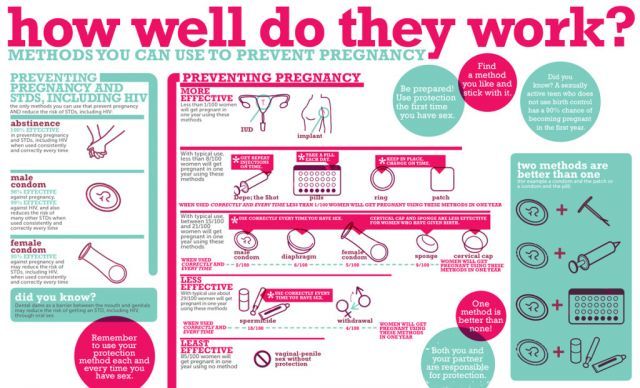
I had several failed romances and had to miss a year of university. All this I attributed to my shortcomings. Like, such a person I am: unadapted to life, insecure, unhappy. It wasn't until my 20s, when I had already graduated from university and my mental and behavioral problems could no longer be attributed to "difficult adolescence", that I first seriously thought about the side effects of pills.
Image copyright BSIP/Getty
Types of contraceptive pills
There are two main types of contraceptives: combination pills, which contain estrogen and progestin (a synthetic form of progesterone), and "pure progestin pills" or "mini pills," which contain only one hormone (progestin).
Pass the podokast
Podkast
Shcho TS BULO
TIZHNIA, Yaku explain our magazine
Kinets Once upon a result of a result of the next PANICAL ARE and started looking for information on Google. The day before, I switched to new progestin contraceptives, which I was prescribed because of a migraine. As it turned out, combination pills are contraindicated for those who suffer from migraine with aura.I searched for the name of my drug and the words "depression" and "anxiety". The Internet immediately showed me forum threads and posts by bloggers who were suffering from the same symptoms as me.
By that time, I had already gone to my local doctor several times complaining of sudden and powerful panic attacks - this had never happened before. The topic of contraceptives never came up in the conversation, despite the fact that the attacks occurred simultaneously with the transition to new pills. Instead, I was prescribed a large dose of beta-blockers - drugs that treat anxiety - and advised to take a course of cognitive-behavioral therapy.
The topic of contraceptives never came up in the conversation, despite the fact that the attacks occurred simultaneously with the transition to new pills. Instead, I was prescribed a large dose of beta-blockers - drugs that treat anxiety - and advised to take a course of cognitive-behavioral therapy.
I lived like this for about six to eight months. I can't say for sure, because this period in my memory is very blurred and accelerated, because the feeling of anxiety and danger was constantly pulsing in my veins.
Image credit, BSIP/Getty
Learn more
The Debrief conducted a survey of 1,022 female readers aged 18 to 30:
I would like to laugh when I think about it. This is how all good stories should end, right? But there was nothing funny about what I went through. It was horror. I felt fear all the time. I did not recognize myself, did not love and could not live in peace. I didn’t know what to do, who to turn to and whether this would end. In addition to anxiety, I was seized by apathy. I felt like a complete mediocrity and blamed only myself for what was happening.
Thinking I was crazy, I told my doctor that I "felt like I'm not myself, but someone else," as if my brain was moldy and shrunken.
"Don't you think it has something to do with my pills?" I asked. I remember the expression on her face: she was trying to keep a neutral look, but she could hardly contain her sarcasm. I explained that six of the seven types of pills I was taking had a negative effect on my well-being. The only exception was high estrogen pills, which made me feel like a superwoman for a year until they were discontinued (partly due to migraines, partly because long-term use of this drug increases the risk of thrombosis).
The only exception was high estrogen pills, which made me feel like a superwoman for a year until they were discontinued (partly due to migraines, partly because long-term use of this drug increases the risk of thrombosis).
Having mastered herself, the doctor said categorically "no": my problems are not related to pills.
However, I didn't listen to her or my therapist and stopped taking progestin pills.
What happened next, I can only call a gradual and careful return of my "I". After three to four weeks, I stopped taking beta-blockers. To this day, I always carry them with me in my purse in case I fall "off the high rock of my consciousness" again. However, for three and a half years they were never needed.
Of course, my problems didn't disappear overnight, but the panic attacks stopped. None have happened over the years. From time to time I experience depression, anxiety and stress, but not to the extent that when I took the progestin pills.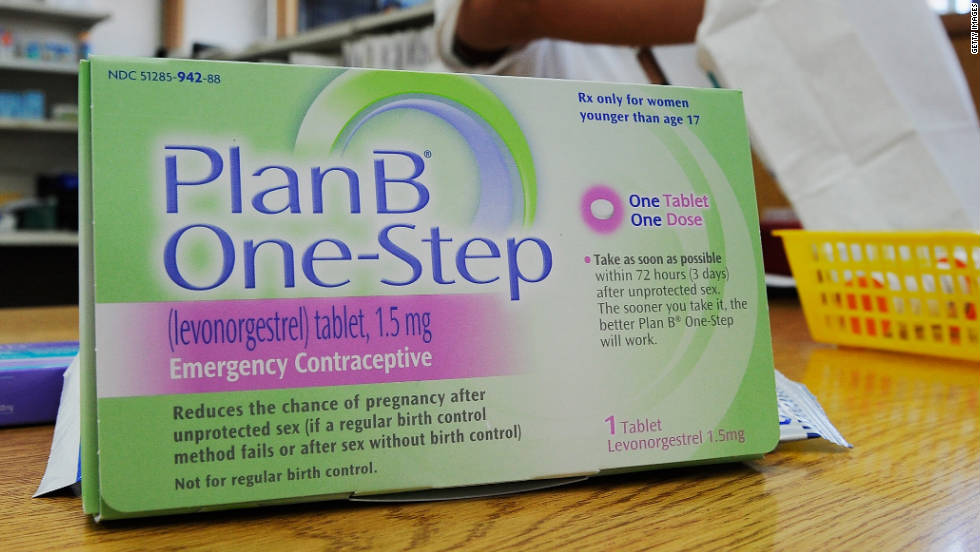 I remembered what joy is. My sex drive has returned. I stopped being afraid of everyone and everyone.
I remembered what joy is. My sex drive has returned. I stopped being afraid of everyone and everyone.
A year after the panic attacks stopped, I went on a solo trip to the other side of the world. A year earlier, this would have been unthinkable. Sitting on a distant tropical beach under a warm thunderstorm, I suddenly burst into tears of joy. What a relief it was that I became myself again, that I can control my thoughts, that I was not mistaken - I really know myself better than the doctors assured me.
I am now 28 years old and no longer take hormonal contraceptives. With the exception of mild mood swings during the day before my period, I was completely free from anxiety, depression, and panic attacks.
Image copyright VICKY SPRATT
Ever since I lost myself on progestin pills and found myself again on a South Asian beach, my problem has gradually begun to attract more and more attention. In 2013, Holly Grigg Spall's book Sweetening The Pill was published, in which the author stated the impact of hormonal contraception on women's mental health.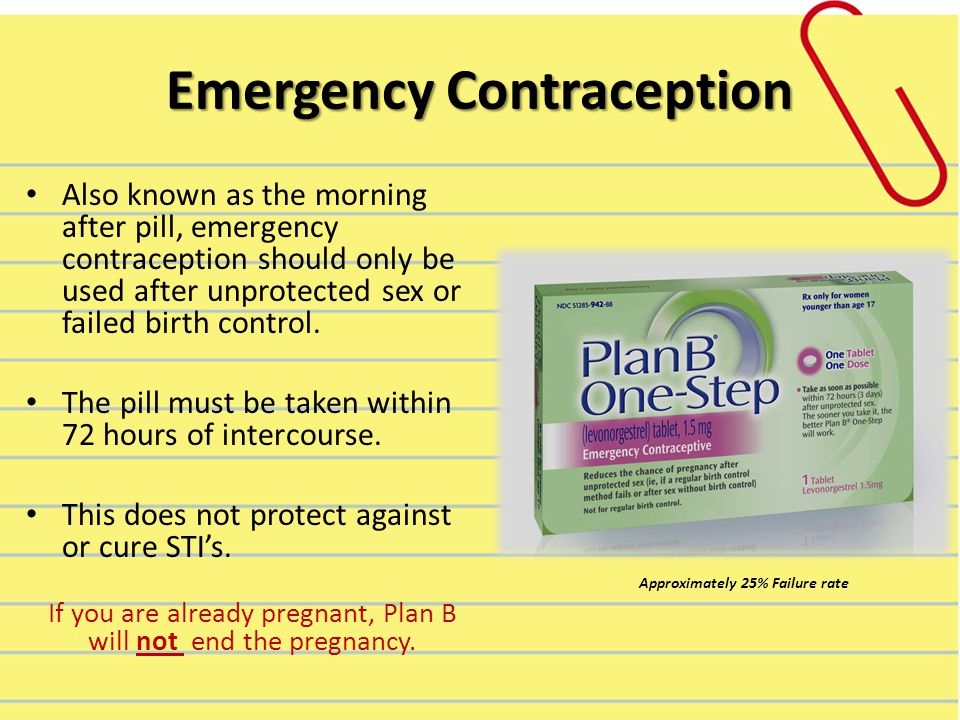
In addition, an important study was carried out: Professor Øyvind Lidegaard from the University of Copenhagen found that women who take birth control pills (both combined and progestin) are more likely to be prescribed antidepressants than others. This difference was especially noticeable among young women aged 15-19 who took the combination pill.
Lidegaard was able to carry out this study because he was given access to the health records of over a million Danish women aged 15 to 34.
After reading about this study, I sent an information request to the National Health Service. As a journalist for The Debrief, I knew that many British women also suffer from such effects of pills - our readers complained to us almost daily. I asked how many women take birth control pills along with antidepressants or beta-blockers. I was told that their system does not yet allow sampling of this data.
Pills and depression
Here's what Professor Helen Stokes-Lampard, President of the Royal College of Physicians says:
"Hormones have been proven to affect mood - both positively and negatively. For most women, reliable contraception and regulation of the menstrual cycle are undeniable the benefits outweigh the side effects, if any. In addition, many women claim that hormonal drugs improve their mood.
For most women, reliable contraception and regulation of the menstrual cycle are undeniable the benefits outweigh the side effects, if any. In addition, many women claim that hormonal drugs improve their mood.
If a woman thinks that contraceptives negatively affect her mood, she should see a doctor. "
Depression is now considered a possible but rare side effect of hormonal contraceptives, according to the instructions that come with the pills. The National Health Service website refers to "mood swings" without directly naming depression, anxiety, or panic attacks.
You don't have to give up pills, but you don't have to put up with the negative side effects that keep us from living. We need information to make a choice. We need more thorough research on the effect of hormonal contraceptives on the female psyche, monitoring the reaction of patients, more support for those who suffer from serious side effects. Women should not feel ignored or not taken seriously.