Can a miscarriage last 3 days
How Long Does a Miscarriage Last?
How Long Does a Miscarriage Last?Medically reviewed by Holly Ernst, PA-C — By Valencia Higuera on June 13, 2018
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Overview
A miscarriage is the loss of a pregnancy before week 20. About 10 to 20 percent of pregnancies end in miscarriage, though the actual percentage is likely higher because some pregnancies are lost very early, before a woman realizes she is pregnant.
How long a miscarriage lasts can vary, depending on several factors. Read on to learn more about miscarriages.
Risks of having a miscarriage
The risk of a miscarriage increases with age. Women under age 35 have about a 15 percent chance of miscarriage. Women between the ages of 35 and 45 have a 20–35 percent chance.
If you become pregnant after the age of 45, your chance of miscarriage increases to 80 percent.
A miscarriage can happen to anyone, but the risk is higher if you’ve had prior miscarriages, have a chronic condition such as diabetes, or have uterine or cervical problems.
Other contributing factors include being:
- smoking
- alcohol abuse
- being underweight
- being overweight
How long does a miscarriage last?
If you experience a miscarriage before realizing you’re pregnant, you may think the bleeding and cramping are due to your menstrual cycle. So, some women have miscarriages and never realize it.
The length of a miscarriage differs for every woman, and it depends on different factors, including:
- how far along you are in the pregnancy
- whether you were carrying multiples
- how long it takes your body to expel the fetal tissue and placenta
A woman early in her pregnancy may have a miscarriage and only experience bleeding and cramping for a few hours. But another woman may have miscarriage bleeding for up to a week.
The bleeding can be heavy with clots, but it slowly tapers off over days before stopping, usually within two weeks.
Symptoms of a miscarriage
A miscarriage is the spontaneous loss of a fetus. Most miscarriages take place before week 12 of pregnancy.
Symptoms of a miscarriage may include:
- vaginal spotting or bleeding
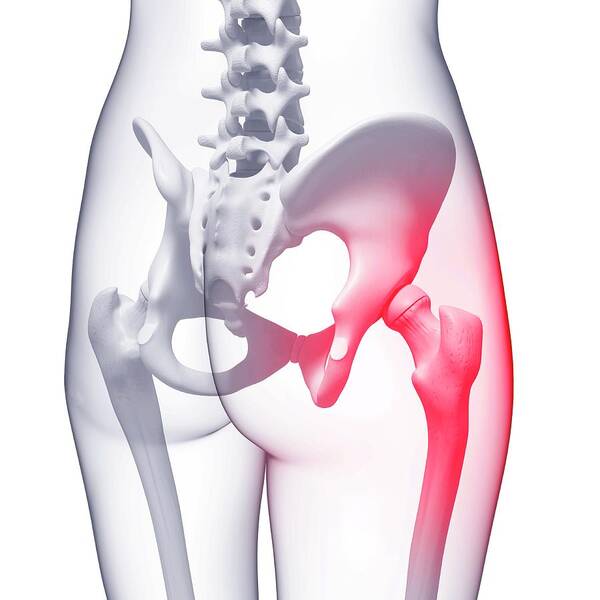
- abdominal or pelvic pain
- cramping in the lower back
- fluid or discharge from the vagina
What are the causes of a miscarriage?
Miscarriages can be caused by many things. Some miscarriages occur because of abnormalities with a developing fetus, such as:
- blighted ovum
- molar pregnancy, a noncancerous tumor in the uterus that in rare cases develops into cancer
Chromosomal abnormalities caused by an abnormal egg or sperm account for about half of all miscarriages. Another potential cause is trauma to the stomach due to invasive procedures, such as chorionic villus sampling. Early in pregnancy, it would be unlikely that an accident or fall could result in miscarriage, since the uterus is so small and well protected within the bony pelvis.
Early in pregnancy, it would be unlikely that an accident or fall could result in miscarriage, since the uterus is so small and well protected within the bony pelvis.
Other causes include certain maternal diseases that put pregnancies at risk. Some miscarriages are unexplained with no cause known.
Daily activities do not typically cause a pregnancy loss. These include activities like exercise (once your doctor says it’s OK) and sex.
What to do if you have a miscarriage
If you think you’re having a miscarriage, seek medical help immediately. Any vaginal bleeding or pelvic pain should be evaluated. There are different tests your doctor can run to determine a miscarriage.
Your doctor will check your cervix during a pelvic examination. Your doctor might perform an ultrasound to check the fetal heartbeat. A blood test can look for the pregnancy hormone.
If you’ve passed pregnancy tissue, bring a sample of the tissue to your appointment so your doctor can confirm the miscarriage.
Types of miscarriage
There are different types of miscarriages. These include:
Threatened miscarriage
During a threatened miscarriage your cervix isn’t dilated, but you do experience bleeding. There is still a viable pregnancy present. There’s a risk of miscarriage, but with observation and medical intervention, you may be able to continue the pregnancy.
Inevitable miscarriage
An inevitable miscarriage is when your cervix is dilated and your uterus is contracting. You may already be passing some of the pregnancy tissue vaginally. This is a miscarriage already in progress.
Incomplete miscarriage
Your body releases some fetal tissue, but some of the tissue remains in your uterus.
Missed miscarriage
During a missed miscarriage, the embryo has died, but the placenta and embryonic tissue remain in your uterus. You may not have any symptoms, and the diagnosis is made incidentally on an ultrasound exam.
Complete miscarriage
During a complete miscarriage your body passes all the pregnancy tissue.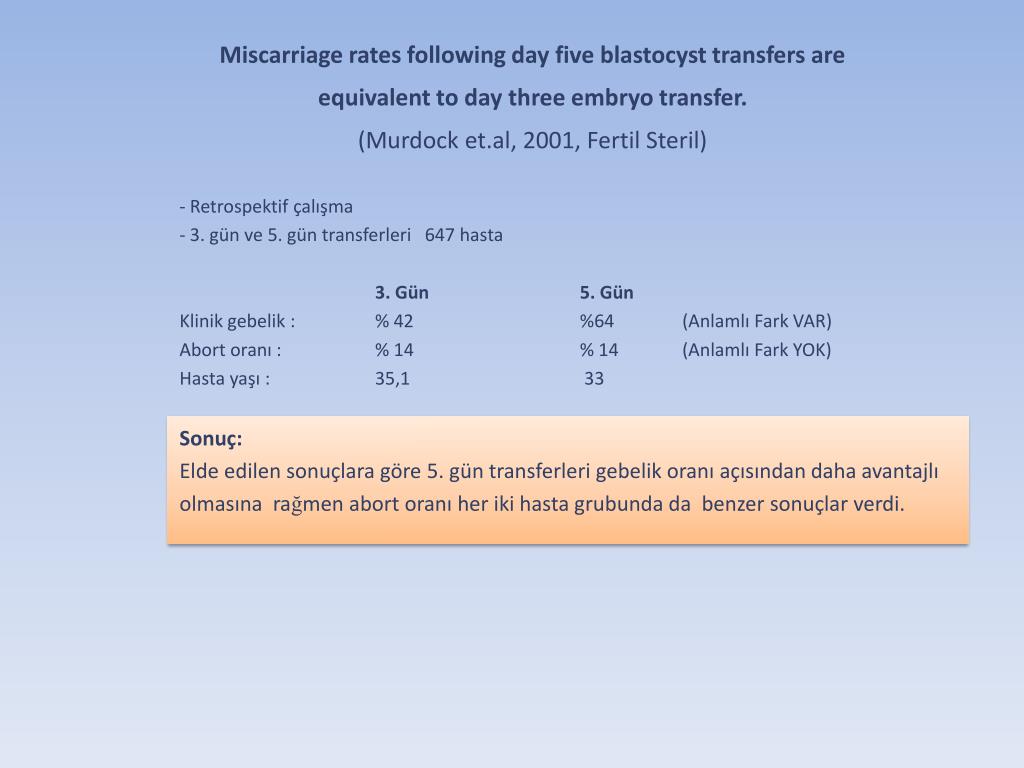
If you ignore a possible miscarriage, you could develop septic miscarriage, which is a rare but serious uterine infection. Symptoms of this complication include a fever, chills, abdominal tenderness, and foul-smelling vaginal discharge.
Ways to treat a miscarriage
Treatments vary according to the type of miscarriage. With a threatened miscarriage, your doctor may recommend you rest and limit activity until the pain and bleeding stop. If there’s a continued risk for a miscarriage, you may have to remain on bed rest until labor and delivery.
In some cases, you can let a miscarriage progress naturally. This process can take up to a couple of weeks. Your doctor will review bleeding precautions with you and what to expect. A second option is for your doctor to give you medication to help you pass the pregnancy tissue and placenta faster. This medication can be taken orally or vaginally.
Treatment is usually effective within 24 hours. If your body doesn’t expel all the tissue or placenta, your doctor can perform a procedure called dilation and curettage (D and C). This involves dilating the cervix and removing any remaining tissue. You could also discuss having a D and C with your doctor as first-line treatment, without using medication or letting your body pass the tissue on its own.
This involves dilating the cervix and removing any remaining tissue. You could also discuss having a D and C with your doctor as first-line treatment, without using medication or letting your body pass the tissue on its own.
Next steps
A pregnancy loss can occur even if you do eliminate risk factors like smoking and drinking. Sometimes, there’s nothing you can do to prevent a miscarriage.
After a miscarriage, you can expect a menstrual cycle within about four to six weeks. After this point, you can conceive again. You can also take precautions against having a miscarriage. These include:
- taking prenatal vitamins
- limiting your caffeine intake to 200 milligrams per day
- managing other medical conditions you may have, such as diabetes or high blood pressure
Shop for prenatal vitamins.
Having a miscarriage doesn’t mean you can’t have a baby. But if you have multiple miscarriages, your doctor may suggest testing to determine if there is an underlying cause.
Last medically reviewed on June 13, 2018
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- American College of Obstetricians and Gynecologists. (2010). ACOG Committee Opinion No. 462: Moderate caffeine consumption during pregnancy. DOI:
10.1097/AOG.0b013e3181eeb2a1 - Andersen N, et al. (2000). Maternal age and fetal loss: population based register linkage study.
ncbi.nlm.nih.gov/pubmed?term=10864550 - Management of miscarriage: Your options. (2016).
miscarriageassociation.org.uk/wp/wp-content/leaflets/Management-of-miscarriage. pdf
pdf - Mayo Clinic Staff. (2016). Miscarriage.
mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/basics/causes/con-20033827 - Miscarriage. (2017).
americanpregnancy.org/pregnancy-complications/miscarriage/ - Nelson DB, et al. (2003). Violence does not influence early pregnancy loss.
ncbi.nlm.nih.gov/pubmed?term=14607576 - Hirsch L. (2015). Understanding miscarriage.
kidshealth.org/en/parents/miscarriage.html
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Jun 13, 2018
By
Valencia Higuera
Edited By
Frank Crooks
Medically Reviewed By
Holly Ernst, PA-C
Share this article
Medically reviewed by Holly Ernst, PA-C — By Valencia Higuera on June 13, 2018
related stories
What Does a Miscarriage Look Like?
What to Know About Your First Period After a Miscarriage
How Soon Can You Ovulate After Miscarriage?
How to Tell if You’re Having a Miscarriage Without Bleeding
Am I Having a Miscarriage? What It May Feel Like
Read this next
What Does a Miscarriage Look Like?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Bleeding in pregnancy could be a sign of miscarriage.
 Learn what miscarriage bleeding looks like, plus other signs of pregnancy loss, including how…
Learn what miscarriage bleeding looks like, plus other signs of pregnancy loss, including how…READ MORE
What to Know About Your First Period After a Miscarriage
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
After a miscarriage, your period will likely take four to six weeks to come back. This depends on how long you were pregnant before the miscarriage…
READ MORE
How Soon Can You Ovulate After Miscarriage?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
It’s possible to ovulate as early as two weeks following a miscarriage. That means you could become pregnant again before having a period. Talk to…
READ MORE
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.
 D., MSN, R.N., CNE, COI
D., MSN, R.N., CNE, COIA miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
Am I Having a Miscarriage? What It May Feel Like
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Every woman and every pregnancy is different when it comes to what a miscarriage feels like. Signs and symptoms may also vary depending on your stage…
READ MORE
Depression After a Miscarriage
Medically reviewed by Janine Kelbach, RNC-OB
It’s not uncommon to experience depression after the sudden loss of a pregnancy. Learn how to cope with the depression associated with miscarriage.
READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
Maintaining a Healthy Pregnancy
Medically reviewed by Stacy Sampson, D.O.
Pregnant people who eat well and exercise regularly along with regular prenatal care are less likely to have complications during pregnancy.
READ MORE
Pregnancy Complications
Medically reviewed by Michael Weber, MD
Sometimes a pregnant woman’s existing health conditions can contribute to problems, and other times new conditions arise because of body and hormonal…
READ MORE
Premature Birth Complications
Medically reviewed by Karen Gill, M.D.
Premature birth complications can occur when a baby is born early, usually before 37 weeks of pregnancy. Learn about short-term and long-term…
READ MORE
What Does a Miscarriage Look Like? Bleeding, Duration, and More
A miscarriage is a spontaneous pregnancy loss before 20 weeks of gestation. Some 8 to 20 percent known pregnancies end in miscarriage, with the majority happening before the 12th week.
Some 8 to 20 percent known pregnancies end in miscarriage, with the majority happening before the 12th week.
The signs and symptoms of miscarriage vary from person to person. Symptoms may also vary depending on how far along you are. For example, a fetus at 14 weeks will be much larger than a fetus at 5 weeks of gestation, so there may be more bleeding and tissue loss with a later miscarriage.
Miscarriage symptoms may include:
- spotting or bleeding from the vagina
- abdominal cramping or pain in the lower back
- passage of tissue, fluid, or other products from the vagina
Read on to learn more about identifying a miscarriage and what to do if you suspect you’re experiencing one.
Bleeding may start as light spotting, or it could be heavier and appear as a gush of blood. As the cervix dilates to empty, the bleeding becomes heavier.
The heaviest bleeding is generally over within three to five hours from the time heavy bleeding begins.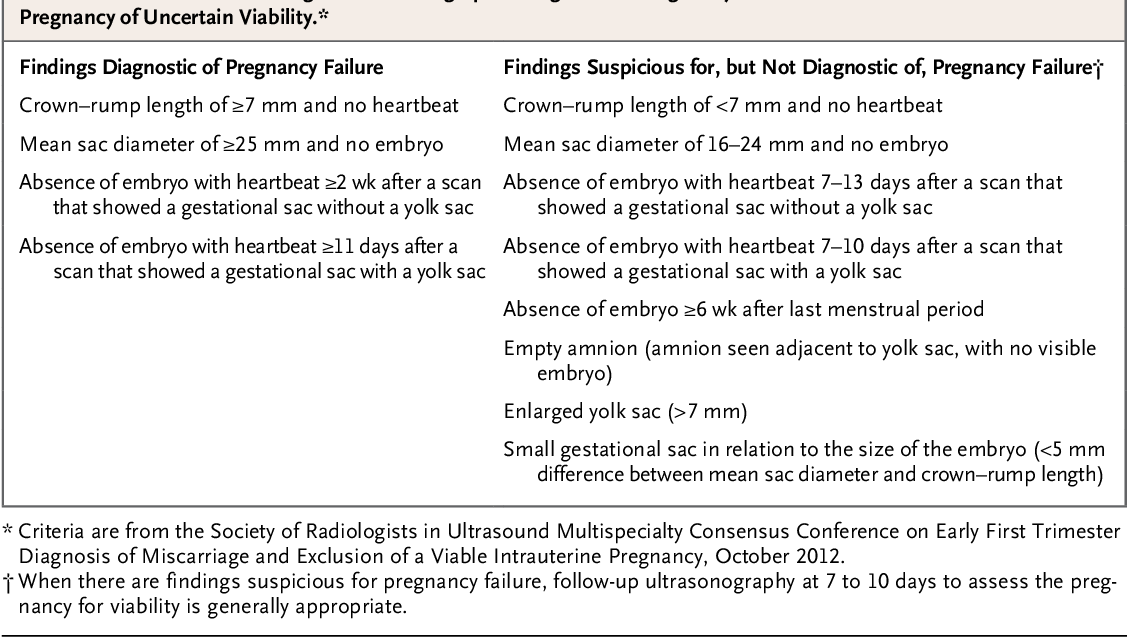 Lighter bleeding may stop and start over one to two weeks before it completely ends.
Lighter bleeding may stop and start over one to two weeks before it completely ends.
The color of the blood can range from pink to red to brown. Red blood is fresh blood that leaves the body quickly. Brown blood, on the other hand, is blood that’s been in the uterus a while. You may see discharge the color of coffee grounds, or near black, during a miscarriage.
Exactly how much bleeding you’ll experience depends on a variety of circumstances, including how far along you are and whether or not your miscarriage is progressing naturally.
While you may see a lot of blood, let your doctor know if you fill more than two sanitary pads an hour for two or more hours in a row.
What does a missed miscarriage look like?
You may not experience bleeding or other symptoms with a miscarriage, at least at first.
A missed miscarriage, also referred to as a missed abortion, happens when the fetus has died but the products of conception remain in the uterus. This type of miscarriage is usually diagnosed via ultrasound.
Just as with the amount of blood you’ll see, the duration of a miscarriage will vary from person to person and even from pregnancy to pregnancy.
In many cases, a miscarriage will take around two weeks to pass naturally. Your doctor may prescribe the medication misoprostol (Cytotec) to help a miscarriage pass more quickly. Bleeding may start within two days of beginning the medication. For others, it may take up to two weeks.
Once the miscarriage has started, the tissue and heaviest bleeding should be passed in about three to five hours. After the fetus has passed, you may still experience spotting and mild tissue loss for one to two weeks.
It may be difficult to tell a very early miscarriage from a late period. In fact, many miscarriages happen before a person even knows they’re pregnant.
In general, a miscarriage will cause more intense symptoms than a menstrual period. For example:
- Your menstrual flow may be relatively similar from month to month with heavy days and light days.
 A miscarriage can also have heavy and light days, but bleeding may be especially heavy at times and last longer than you’re used to.
A miscarriage can also have heavy and light days, but bleeding may be especially heavy at times and last longer than you’re used to. - Bleeding from a miscarriage may also contain large clots and tissue you don’t normally see during your period.
- Cramps can be a part of your normal monthly cycle, but with a miscarriage, they may be particularly painful as the cervix dilates.
- The color of blood during your period can range from pink to red to brown. If you see a color you’re not used to seeing, it may be a sign of miscarriage.
Always contact your doctor if you’re pregnant and experience bleeding. While a miscarriage can’t be stopped once it starts, you doctor can run tests to help determine if you’re experiencing the loss of your pregnancy or something else.
To diagnose a miscarriage, your doctor will likely perform an ultrasound to look for the baby’s heartbeat, if you’re far enough along to see a heartbeat. Your doctor may also order a blood test to check human chorionic gonadotropin (hcG) levels to see if they’re rising or falling.
If a miscarriage is confirmed, your doctor may suggest “expectant management” or waiting for the miscarriage to pass naturally. This generally happens within two weeks.
Incomplete miscarriage
The miscarriage may be incomplete if:
- your bleeding is particularly heavy
- you have a fever
- an ultrasound reveals there’s still tissue in your uterus
If this is the case, your doctor may suggest a dilation and curettage (D and C), which is a surgical procedure done to remove remaining tissue. The procedure is done under general or regional anesthesia, and is considered safe. D and C doesn’t usually lead to long-term complications.
Threatened miscarriage
It’s important to report any bleeding or pain you experience in your pregnancy to your doctor. In some cases, you may have what’s called a threatened miscarriage, and there may be certain treatments that can help. These include:
- hormone supplements if the bleeding is caused by low progesterone
- a cerclage (stitch in the cervix) if the issue is with the cervix opening prematurely
Speak with your healthcare provider if you’re looking to get pregnant again after a miscarriage. While it may be safe to start trying after your first normal period, you may want to schedule a checkup depending on the cause or the number of miscarriages you’ve had.
While it may be safe to start trying after your first normal period, you may want to schedule a checkup depending on the cause or the number of miscarriages you’ve had.
The reason for loss isn’t always known, but around half of miscarriages are caused by issues with the baby’s chromosomes.
Other possible causes include:
- uterine issues
- hormonal imbalances
- other health conditions, such as diabetes, autoimmune disorders, or polycystic ovary syndrome
After a miscarriage, you may have hcG in your blood for one to two months, which could lead to a false positive pregnancy test. In most cases, your period will return within four to six weeks, though you may start ovulating almost immediately following a miscarriage.
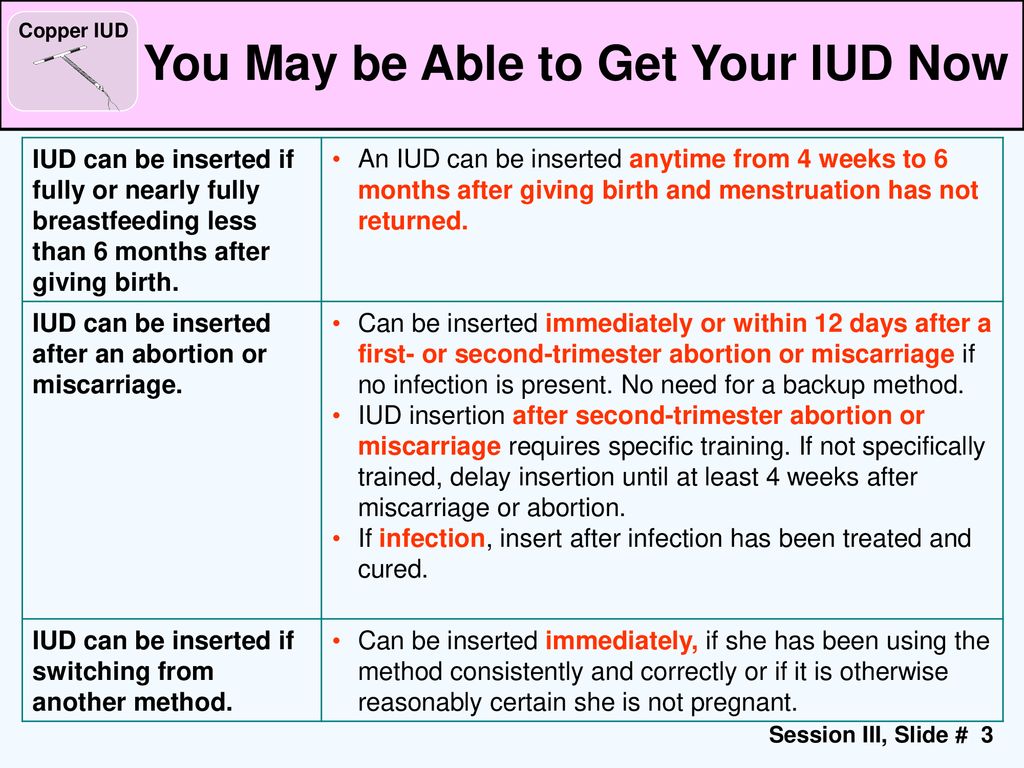
Speak with your doctor about birth control options if you don’t wish to become pregnant after a miscarriage.
Will I miscarry again?
Having one miscarriage doesn’t necessarily increases your chances of having another. The risk remains around 20 percent.
The risk remains around 20 percent.
Two or more miscarriages is referred to as recurrent pregnancy loss (RPL). The risk of miscarriage after two losses is 28 percent. After three consecutive losses, it increases to 43 percent.
Only 1 percent of people experience three or more miscarriages. About 65 percent of those with unexplained RPL go on to have successful pregnancies.
Activities like exercise, work, morning sickness, and sex don’t cause miscarriages. Even things like smoking or drinking alcohol or caffeine, which can lead to other complications, are also unlikely to lead to early pregnancy loss.
A miscarriage can be physically painful, and it may also cause a variety of emotions. While your body may recover in a few weeks, be sure to take time to process your feelings, grieve, and reach out for help when you need it.
Spontaneous miscarriage and miscarriage
Over the past 10 years, the number of spontaneous miscarriages has been growing rapidly. The International Histological Classification Organization (FIGO) has declared the situation with an increase in the frequency of miscarriages an epidemic.
The International Histological Classification Organization (FIGO) has declared the situation with an increase in the frequency of miscarriages an epidemic.
Spontaneous miscarriage is the termination of pregnancy before the fetus reaches a viable term (up to 22 weeks of pregnancy and fetal weight 500 g.).
Most miscarriages (about 80%) occur before 12 weeks of gestation. Moreover, in the early stages up to 8 weeks of pregnancy, the cause of miscarriage is chromosomal abnormalities in 50% of cases. It turns out that nature eliminates the defective product of conception. And these causes are difficult to prevent, especially in the presence of hereditary diseases. Fortunately, accidental breakdowns are much more common than genetically determined ones. Therefore, subsequent pregnancies usually end happily. But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.
What are the reasons?
- chronic diseases: inflammatory diseases of the uterus and appendages, polycystic ovary syndrome, uterine fibroids, endometriosis, malformations of the genital organs.
- infections: toxoplasmosis, listeriosis, genital tuberculosis, sexual infections - chlamydia, mycoplasma, ureaplasma, syphilis.
- antiphospholipid syndrome.
- endocrine diseases: diabetes, thyroid disease.
- metabolic disorders in the body: obesity, folic acid deficiency, iron deficiency, vitamin D deficiency.
- male factor.
Of course, these causes are identified and eliminated before the planned conception.
There are harmful factors that can affect the development of the fetus in the early stages of pregnancy and lead to miscarriage:
- alcohol consumption.
- caffeine use (4-5 cups of coffee per day).
- smoking (more than 10 cigarettes a day).
- drug use.
- taking medications with a teratogenic effect (for example: aspirin, nise and others from this group of drugs; antifungals; antidepressants; some antibiotics and a number of other drugs).
- toxins and occupational hazards: ionizing radiation, pesticides, inhalation of anesthetic gases.
What are the signs of possible pregnancy loss?
These are complaints of pain in the lower abdomen and lower back, bloody discharge from the genital tract. It is necessary to consult a doctor to rule out an ectopic pregnancy and conduct an additional examination (hCG test, blood test for progesterone, ultrasound).
In early pregnancy, with dubious ultrasound data or suspected non-developing (missing) pregnancy, expectant management is chosen with a repeat examination by a gynecologist, ultrasound, tests after 7-10 days. If a the diagnosis was made and the fact of uterine pregnancy was confirmed, with a threatened miscarriage, preservation therapy is carried out in an outpatient day hospital. A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed.
In accordance with the clinical treatment protocol approved by the Ministry of Health of the Russian Federation dated 07.06.2016. Preference is given to drug therapy aimed at terminating pregnancy with prostaglandin analogues (misoprostol) with or without prior use of an antiprogestin (mifepristone). In case of need for surgical treatment (with incomplete miscarriage with infected miscarriage), it is recommended to use aspiration curettage (with an electric vacuum source or a manual vacuum aspirator). What has a significant advantage over curettage of the uterine cavity because it is less traumatic and can be performed on an outpatient basis.
All women who have had a miscarriage need treatment to prevent complications and prevent recurrent miscarriages. Why is rehabilitation therapy necessary?
According to the decision of the XVIII World Congress of Obstetricians and Gynecologists , the diagnosis of chronic endometritis should be made to absolutely all women who have had an undeveloped pregnancy. Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
If time is lost, it is necessary to carry out additional diagnostics: a pipel biopsy of the endometrium with a histological examination and a study for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome).
In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities for a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist). Our gynecologists of the highest category Melko O.N., Novitskaya E.L., Tikhonova T.N. and urologist of the highest category Kanaev S.A. have sufficient experience in the rehabilitation and preparation of couples for the next pregnancy with a successful outcome. Treatment is carried out in a day hospital with the use of drugs, physiotherapy, gynecological massage, prostate massage.
Our gynecologists of the highest category Melko O.N., Novitskaya E.L., Tikhonova T.N. and urologist of the highest category Kanaev S.A. have sufficient experience in the rehabilitation and preparation of couples for the next pregnancy with a successful outcome. Treatment is carried out in a day hospital with the use of drugs, physiotherapy, gynecological massage, prostate massage.
WE WILL HELP YOU!
st. Yakovleva, 16 st. Kirova 47 B
tel. 244-744 tel. 46-43-57
Miscarriage during missed pregnancy
What is a miscarriage?
According to medical statistics, miscarriage is the most common complication during pregnancy. About 10-20% of all recorded pregnancies end in miscarriage. Miscarriage is a sporadic, sudden, termination of pregnancy, which is accompanied by complete or partial emptying of the uterus.
Missed pregnancy loss (MP) can be seen on ultrasound. It consists in confirming the non-viability of the fetus without bleeding. The ST can end in a miscarriage, when the body gets rid of the dead fetus on its own, or in a medical abortion, when medical or surgical manipulations are used to clean the uterine cavity.
The ST can end in a miscarriage, when the body gets rid of the dead fetus on its own, or in a medical abortion, when medical or surgical manipulations are used to clean the uterine cavity.
Causes of miscarriage and miscarriage
80% of miscarriages occur in the first trimester before 12 weeks. In 50% of cases, this occurs due to genetic defects in the fetus. The threat of miscarriage due to chromosomal abnormalities decreases with the course of pregnancy: by 20 weeks it is 10-20% versus 41-50% in the first trimester. The main cause of genetically determined early miscarriages are autonomous trisomies - when three homologous chromosomes are present in the cells instead of two. Such defects occur at the time of conception and are not subject to correction. They lead to miscarriage or to the development of severe genetic diseases. In addition to genetics, immunological, endocrine and infectious causes are distinguished.
In the second trimester, various diseases and disorders in the mother's body become the main cause of miscarriage.
There is a list of factors that can trigger early pregnancy loss:
-
woman's age. At the age of 20-30 years, the risk of spontaneous miscarriage is 9-17%, at 35-40 years old - 20%, at 40-45 - 40%;
-
alcohol abuse;
-
abuse of caffeine;
-
smoking;
-
drug use;
-
chronic diseases of the mother;
-
maternal infections;
-
use of medications incompatible with pregnancy;
-
history of spontaneous abortion. The risk of subsequent pregnancy loss in women with one miscarriage in history is 18-20%, with two - 30%, with three - 43%.
Symptoms and signs of miscarriage
You can suspect a miscarriage by sudden spotting and sharp pain in the lower abdomen. If these symptoms appear, seek immediate medical attention. The doctor must conduct an ultrasound diagnosis. Transvaginal scanning (TVS) is considered the gold standard for diagnostics - when the sensor is inserted into the uterus through the vagina.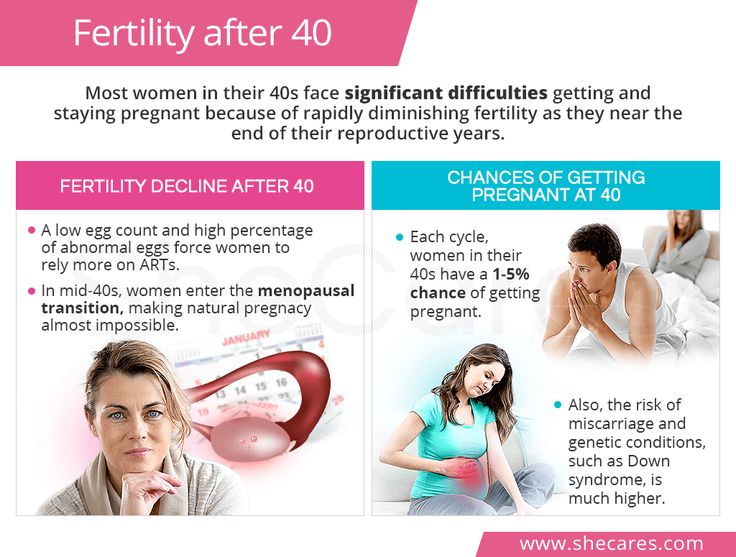 If TVS is not available, a transabdominal scan can be applied - through the anterior abdominal wall.
If TVS is not available, a transabdominal scan can be applied - through the anterior abdominal wall.
Missed pregnancy may be asymptomatic and not manifest until the next scheduled ultrasound.
How does a miscarriage happen?
The miscarriage process has four stages. This does not happen overnight and lasts from several hours to several days.
The first stage - the threat of miscarriage. Among the symptoms: pulling pains in the lower abdomen, scanty blood discharge, increased uterine tone. The process of detachment of the placenta from the place of attachment in the uterus begins. The internal os is closed. The main thing is to seek help in time, then with proper therapy if there is a chance to stop the miscarriage and save the pregnancy.
The second stage - the beginning of a miscarriage. Strong discharge, the cervical canal is ajar, the doctor diagnoses the final detachment of the placenta.
Third stage - miscarriage in progress. You can feel the regular contractions of the uterus, the outcome of the fetus, placenta and uterine contents, profuse blood discharge has begun.
You can feel the regular contractions of the uterus, the outcome of the fetus, placenta and uterine contents, profuse blood discharge has begun.
The last fourth stage is a complete miscarriage. The pregnancy is interrupted, the uterine cavity does not contain the fetus and products of conception.
How to determine ST?
It should be remembered that a miscarriage can be diagnosed only during an ultrasound examination. Home tests will not give reliable results. Ultrasound will show the presence or absence of a heartbeat in the fetus.
Treatment of miscarriage and miscarriage
Due to the fact that the vast majority of spontaneously terminated pregnancies are due to genetic abnormalities (non-viability) of the fetus, then, speaking about the treatment of miscarriage, it is worth talking about ensuring complete and safe cleansing of the uterus, preventing infection and preventing bruising. With the help of an ultrasound examination, the doctor will check whether the uterus has completely cleared.