Can chlamydia cause you not to get pregnant
Is an STD the Reason You Are Not Getting Pregnant?
Sexually transmitted diseases are running rampant, causing infertility in the process. This may seem scary, but we are specially equipped to find and address STD-related infertility, even if it happened a long time ago.
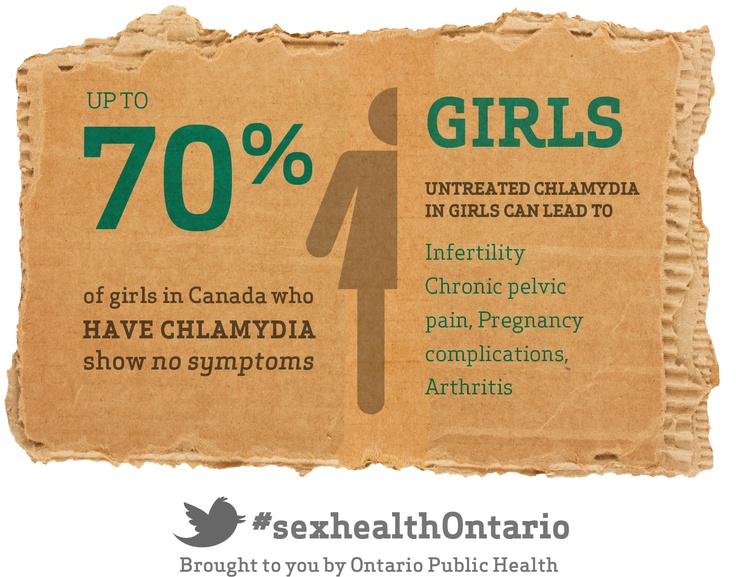
It is ironic that the more you’ve had sex in your past, the less fertile you may be, particularly if condoms weren’t used. Sexually transmitted diseases (STDs) can make both women and men infertile, though it seems to affect women more. Up to 85 percent of women that have had chlamydia don’t realize they’ve had it.
Moreover, the South (particularly Mississippi) has some of the highest rates of STDs in the United States. Other areas of the U.S. with high rates of infections include Alaska, Washington, D.C. and the U.S. Virgin Islands (which may need a new name based on these statistics).
STDs can not only affect mothers and fathers, but even their children (e.g. chlamydial conjunctivitis). A single event of pelvic inflammatory disease (PID) can cause 20 percent of women to have blocked fallopian tubes, as well as a 20 percent rate of chronic pelvic pain. Even if the fallopian tubes aren’t completely closed, they can still have damage that can be missed. We’re fortunate at Positive Steps Fertility to provide our Parryscope™ fertility evaluation that thoroughly examines the fallopian tubes, as well as uterine health and ovarian reserve, often picking up problems other doctors have missed.
Related information: Having trouble getting pregnant? Whether due to STDs or other causes, we can help. So please make an appointment.
There are three basics to understanding how STDs and fertility overlap: what STDs are, how they cause infertility and how to fix problems.
What are sexually transmitted diseases?
An STD is one that is passed from one person to another mainly through intimate sexual contact, which can be “heavy petting,” vaginal or anal sexual intercourse, and oral sex. There are dozens of STDs including syphilis, gonorrhea, chlamydia, herpes, human papillomavirus (HPV) and others. But gonorrhea and chlamydia are the ones most likely to cause subfertility (reduced fertility).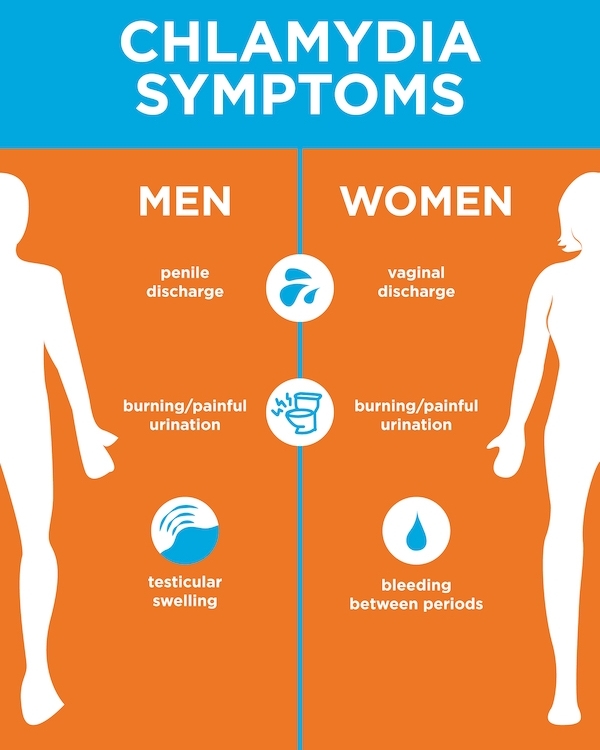
Most sexually active people are familiar with the term STD, and probably STI (sexually transmitted infection). The terms are often used interchangeably. But technically the sexually transmitted infection occurs before the sexually transmitted disease, which follows from the infection. STI or STD, you don’t want either one.
About 20 million new cases of STDs occur every year, according to the Centers for Disease Control and Prevention (CDC). And roughly 75 percent of women will get some type of STD in their lifetime (over 90 percent if you include HPV). STDs are most common in women under age 25, and up to 80 percent of women with chlamydia get it between age 15 and 25.
According to the CDC, there were a record number of cases in 2016 for gonorrhea, chlamydia and syphilis. Though we hope for these numbers to drop for subsequent years (there’s a delay in release of data due to analysis), decreased government funding for health centers has already led to increased costs for testing in several areas, resulting in fewer people getting evaluated.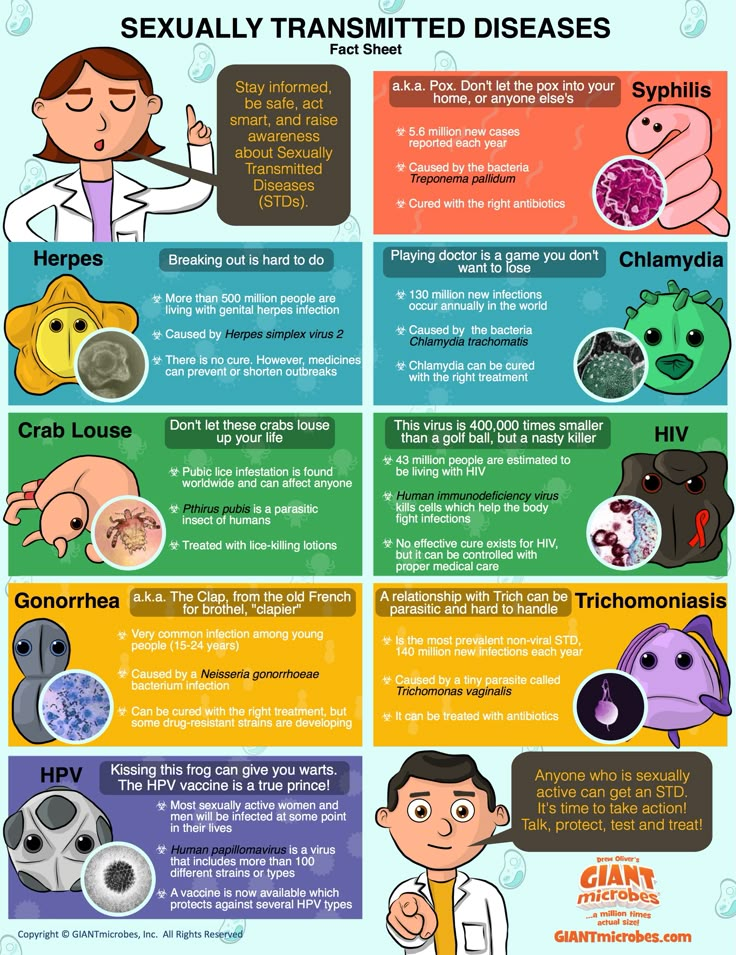
This means more people with infections won’t know they have one, and a greater likelihood of STDs being spread. Based on past parallels, we expect more women to have STIs in the future, particularly in areas with limited investment in public health.
The best practice, particularly for people trying to get pregnant, is to be tested for STDs (CDC guidelines for testing) and get treated if an STD is present. Mississippians particularly should be on guard for STDs. According to the CDC, the state ranks #1 in gonorrhea, #3 in chlamydia and #7 in primary and secondary syphilis.
How STDs cause infertility
Gonorrhea and chlamydia, which are preventable, are the two STDs most likely to result in infertility because they can cause PID in women. This can inflame and scar the fallopian tubes, making it hard for sperm and eggs to find each other, blocking pregnancy. Chlamydia and gonorrhea can also cause inflammation of the cervix and inflammation of the urethra in the lower part of the urinary tract.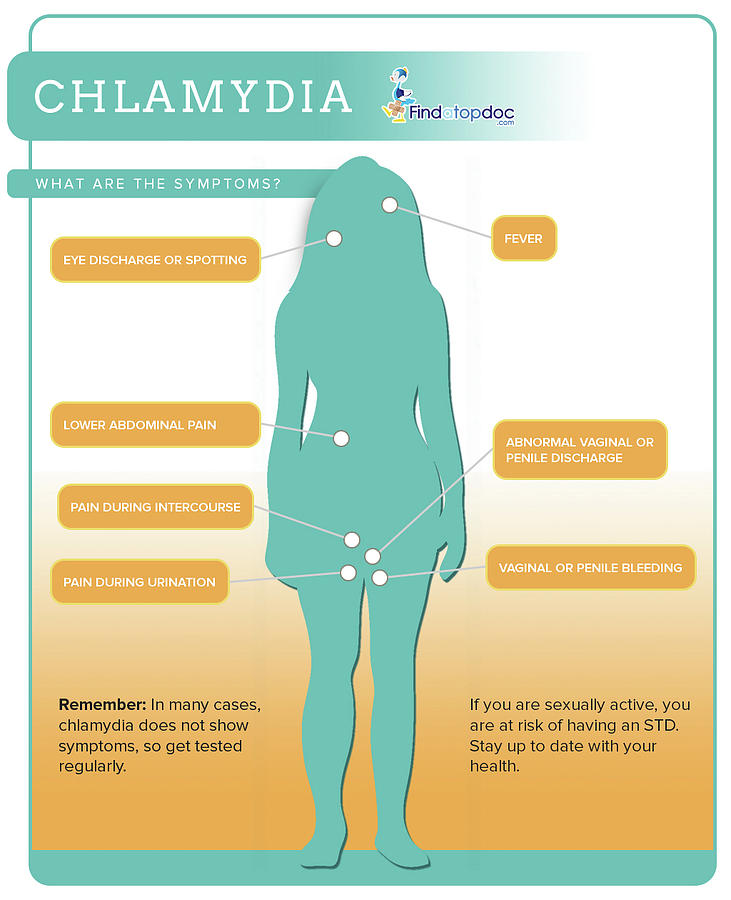
Gonorrhea and chlamydia often show no symptoms, so that’s another concern and reason to be tested. If untreated, about 15 percent of women with chlamydia will develop PID, which occurs in the upper part of the genital tract affecting the uterus, fallopian tubes and surrounding tissues in those areas. This can cause infertility, with cases of acute PID being particularly damaging to fertility.
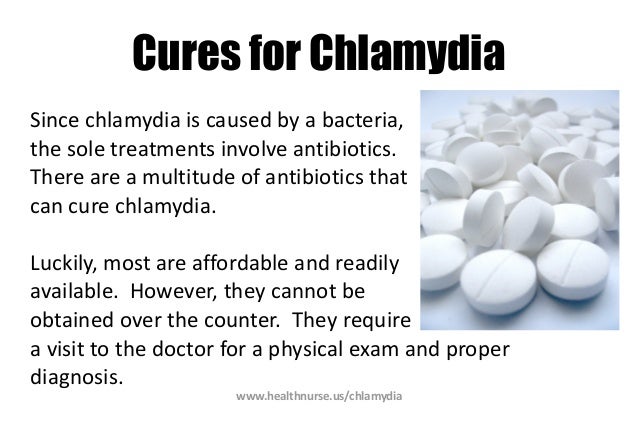
Screening for gonorrhea and chlamydia is simple and inexpensive, involving a urine sample. Treatment is also relatively easy. The CDC recommends dual therapy of two drugs, one an injection, the other an oral medication. Because gonorrhea and chlamydia often occur at the same time, this dual approach can cure both.
HPV and herpes simplex virus (HSV) don’t directly cause infertility, but HSV can make you more vulnerable to other infections. Couples with HSV must abstain from sex until the sores have healed, and HPV can progress to cervical (and other) cancer, and the treatments can sometimes make you less fertile.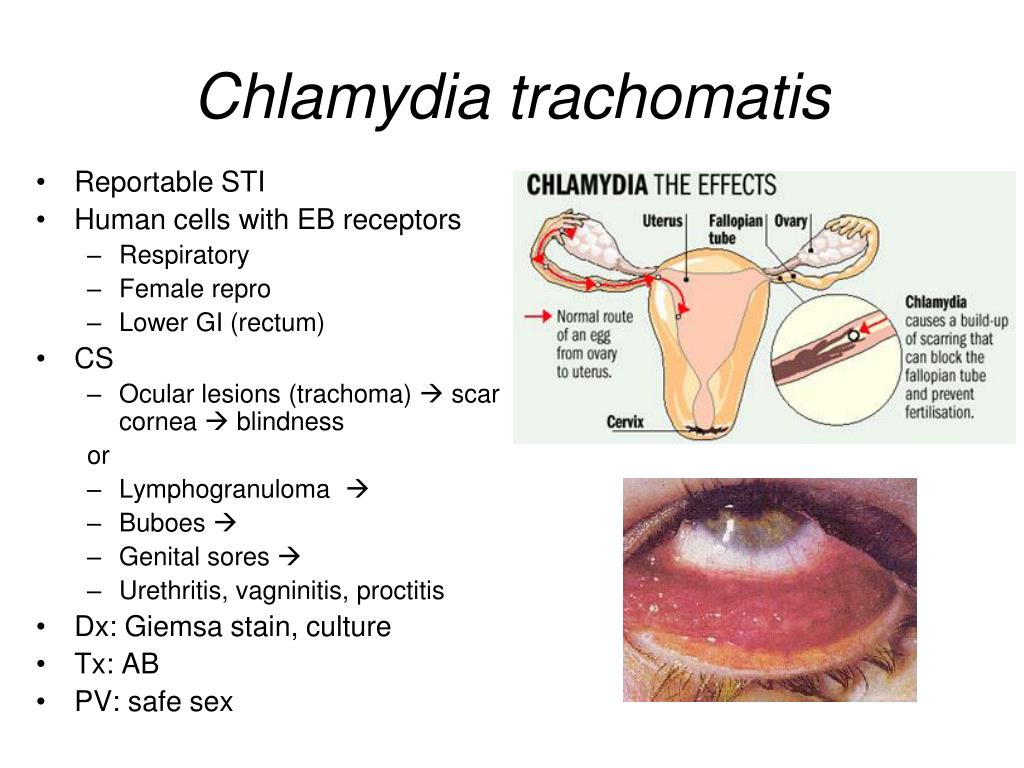
STDs in men
Though STDs are more detrimental to female fertility, if the male has gonorrhea or chlamydia, it can render him infertile because the infection can block the epididymis. These are the long, coiled tubes at the back of the testicles that store and then carry sperm during ejaculation. A blocked epididymis can mean that no sperm gets to the female’s eggs during intercourse. Men who suspect they are having trouble should come to us and have their fertility assessed.
But the most likely way that a male STD can cause infertility is that he passes the disease to his female partner. Then she becomes infertile, as described above. The male partner’s STD could also affect fertility by causing the couple to abstain from sex in order to heal and not spread the disease.
Working around STD-caused infertility
For men and women seeking to have children, the biggest issue with STDs is damage to the woman’s fallopian tubes and potentially even the uterus. The two fallopian tubes pick up eggs from the ovaries, so if the tubes are closed at that end from a previous infection, there won’t be many (or any) eggs for the sperm to find and fertilize in order to make an embryo.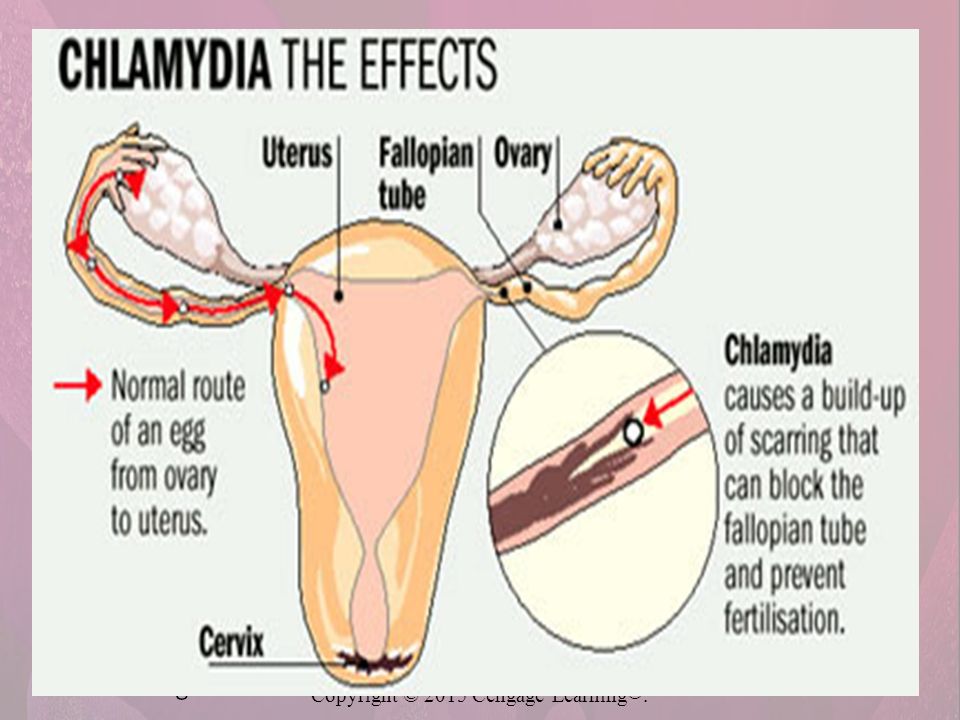
Also, even if the tubes are only partially blocked, and sperm and egg “get lucky” finding each other, the damage can still prevent an embryo from making it back to the uterus, resulting in an ectopic pregnancy, which is a dangerous condition, and the pregnancy must be ended. Additionally, very bad pelvic infections can scar the uterus, resulting in Asherman’s syndrome, making it difficult for an embryo to attach or develop.
With the Parryscope™ technique I invented and for which I have a patent and trademark pending, we can quickly, gently and accurately look at whether the fallopian tubes are open or whether STDs (or other factors) may have resulted in scarring. At the same time we can also look at ovarian and uterine factors, so as to cover the core factors in female fertility.
If there is a blockage in the fallopian tubes or other problems are found, additional evaluation and treatment may be necessary. Though the Parryscope™ technique is a minimally invasive surgical service through hysteroscopy, the focus is on diagnostic evaluation.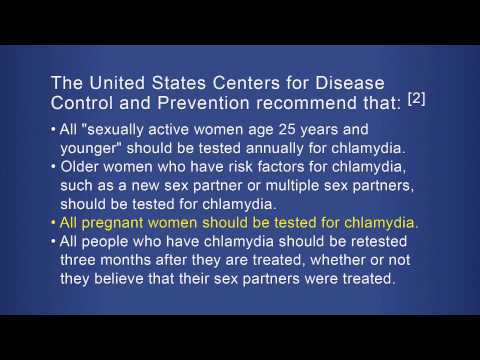 Other minimally invasive surgeries such as laparoscopy may be necessary to repair the tubes.
Other minimally invasive surgeries such as laparoscopy may be necessary to repair the tubes.
We perform such surgeries at Positive Steps Fertility. These therapies can include a salpingostomy procedure that can clear a new opening in a blocked fallopian tube near the ovary. Another option is a fimbrioplasty operation, which can rebuild the fringe-like ends of the fallopian tube by the ovary that serve to sweep the egg into the tube from the ovary. For blockages of the tubes near the uterus, we can attempt to clear them with tubal cannulation, in which we use a catheter through the cervix and uterus to try to clear the blockage
If these aren’t options or are not successful, we have to bypass the fallopian tubes to achieve pregnancy. This is where assisted reproductive technologies come into play, and in vitro fertilization (IVF) is often the best choice.
If only one fallopian tube is blocked, pregnancy is still possible. We may be able to assist it with intrauterine insemination (IUI).
Three closing thoughts on STDs and infertility for people trying to have children
- You should try your best to prevent getting an STD.
- If you think it’s possible you have an STD, be tested and have it treated.
- If you suspect an STD – or anything – is preventing you from getting pregnant, get in touch with me: We’ll find out the problem and work around it the best way possible.
Chlamydia - Complications - NHS
If chlamydia isn't treated, it can sometimes spread and cause potentially serious problems.
Complications in women
Pelvic inflammatory disease (PID)
In women, chlamydia can spread to the womb, ovaries or fallopian tubes. This can cause a condition called pelvic inflammatory disease (PID).
PID can cause a number of serious problems, such as:
- difficulty getting pregnant or infertility
- persistent (chronic) pelvic pain
- an increased risk of ectopic pregnancy (where a fertilised egg implants itself outside the womb)
The symptoms of PID are generally similar to the symptoms of chlamydia, including discomfort or pain during sex, pain during urination, and bleeding between periods and after sex.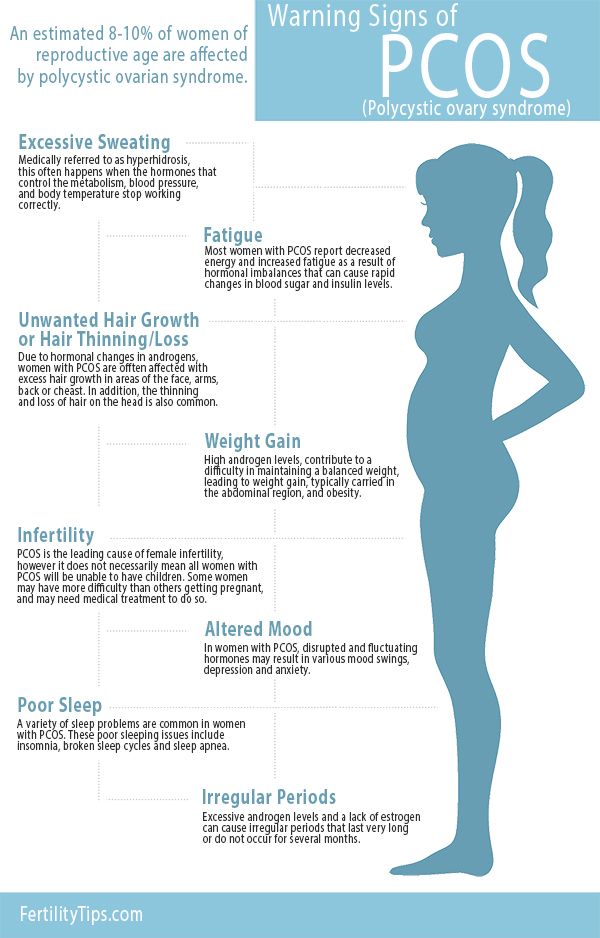
PID is usually treated with a 2-week course of antibiotics. The risk of experiencing problems such as infertility is lower if it's treated early, so it's important to seek medical advice as soon as possible if you have symptoms of the condition.
Pregnancy complications
If you have chlamydia that's not treated while you're pregnant, there's a chance you could pass the infection on to your baby. If this happens, your baby may develop an eye infection (conjunctivitis) and lung infection (pneumonia).
If your baby has symptoms of these conditions, your midwife or GP can arrange for a test to check for chlamydia, and antibiotics can be used to treat the infection.
Untreated chlamydia in pregnancy may also increase the risk of problems such as premature labour and birth (before 37 weeks of pregnancy) or your baby being born with a low birthweight.
Complications in men
Inflammation of the testicles
In men, chlamydia can spread to the testicles and epididymis (tubes that carry sperm from the testicles), causing them to become painful and swollen.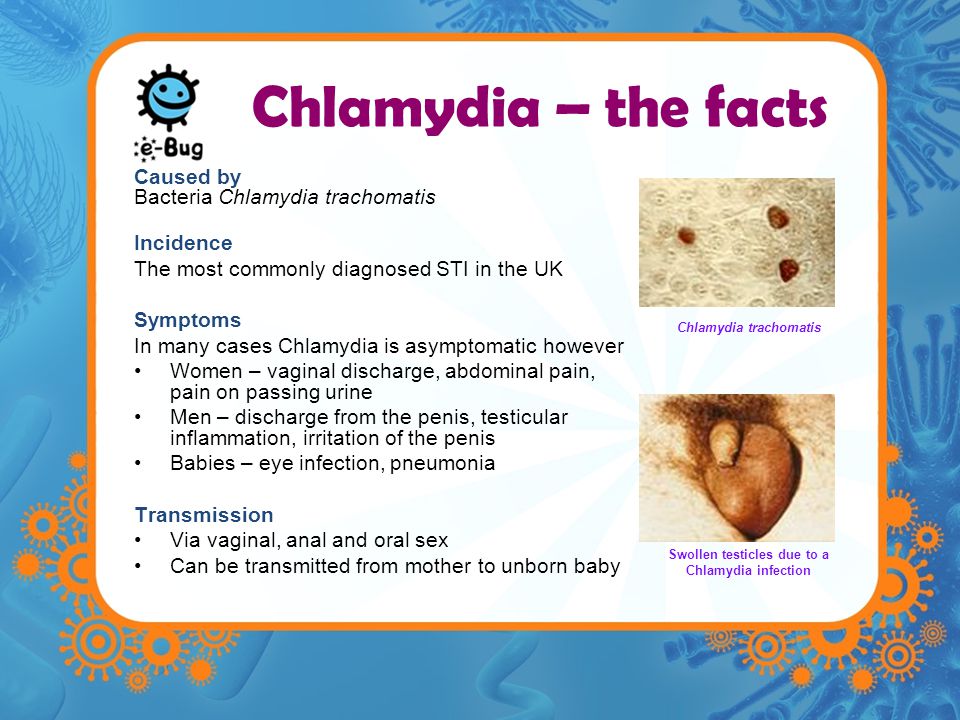 This is known as epididymitis or epididymo-orchitis. This is very rare.
This is known as epididymitis or epididymo-orchitis. This is very rare.
The inflammation is usually treated with antibiotics. If it's not treated, there's a possibility it could affect your fertility.
Reactive arthritis
Chlamydia is the most common cause of sexually acquired reactive arthritis (SARA). This is where your joints, eyes or urethra (the tube that passes urine out of the body) become inflamed, usually within the first few weeks after having chlamydia.
It can affect women who have had chlamydia but is more common in men.
There's currently no cure for SARA, but most people get better in a few months. In the meantime, treatment with non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help relieve the symptoms.
Page last reviewed: 01 September 2021
Next review due: 01 September 2024
Chlamydia - KVD №2
What is chlamydia?
Chlamydia is a common sexually transmitted infection (STI). The disease is caused by the bacterium Chlamydia trachomatis (Chlamydia trachomatis), which affects the female genital area and is the cause of non-gonococcal urethritis in men. Manifestations of chlamydia are usually minor or absent, but serious complications develop. Complications can cause irreparable damage to the body, including infertility - all this proceeds very secretly.
The disease is caused by the bacterium Chlamydia trachomatis (Chlamydia trachomatis), which affects the female genital area and is the cause of non-gonococcal urethritis in men. Manifestations of chlamydia are usually minor or absent, but serious complications develop. Complications can cause irreparable damage to the body, including infertility - all this proceeds very secretly.
Chlamydia also causes penile discharge in infected men.
Chlamydia transmission routes
Chlamydia can be transmitted through:
- vaginal or anal contact with an infected partner;
- less common with oral sex;
- use of sex toys with an infected partner;
- infection of a newborn during childbirth from a sick mother.
Absolutely all sexually active people can get chlamydia. The greater the number of sexual partners, the greater the risk of infection. The risk of infection is especially high in girls, because their cervix is not fully formed. About 75% of new cases occur in women under 25 years of age. By the age of 30, approximately 50% of sexually active women have had chlamydia. In sexually active men, the risk of infection is highest between the ages of 20 and 24.
About 75% of new cases occur in women under 25 years of age. By the age of 30, approximately 50% of sexually active women have had chlamydia. In sexually active men, the risk of infection is highest between the ages of 20 and 24.
You cannot get chlamydia through kisses, hugs, dishes, baths, towels.
Manifestations of chlamydia
Chlamydia is very secretive. About 75% of infected women and 50% of infected men are asymptomatic. If manifestations of the disease develop, then this occurs approximately 1 to 3 weeks after infection.
In women, chlamydia first affects the cervix and urethra (urinary canal).
Manifestations:
- unusual vaginal discharge;
- pain or discomfort when urinating;
If the infection penetrates to the appendages, manifestations are possible:
- pain in the lower abdomen;
- pain in the lumbar region;
- nausea;
- slight increase in temperature;
- pain during intercourse or bleeding after it;
- bleeding between periods.
Symptoms in men:
- clear or cloudy discharge from the penis;
- pain or discomfort when urinating;
- there may be burning and itching in the area of the outlet of the urethra;
- rarely pain and/or swelling of the testicles.
Men or women who have anal sex with an infected partner can infect the rectum, resulting in inflammation, pain, discharge, or bleeding from the rectum.
Chlamydia can cause sore throat (pharyngitis) in men and women who have oral contact with an infected partner.
What complications can develop if chlamydia is not treated?
If the disease is not treated, serious short-term and persistent complications develop. Like the disease itself, complications often occur insidiously.
In women with untreated chlamydia, the infection can spread from the urethra to the fallopian tubes (the tubes that carry the egg from the ovaries to the uterus) - this causes (in 40% of cases) the development of pelvic inflammatory disease (PID). PID causes permanent damage to the fallopian tubes, uterus, and surrounding tissues. Chronic pelvic pain, infertility and ectopic pregnancy are the result of PID.
PID causes permanent damage to the fallopian tubes, uterus, and surrounding tissues. Chronic pelvic pain, infertility and ectopic pregnancy are the result of PID.
Women with chlamydia are more susceptible to HIV infection, the risk increases by almost 5 times.
To prevent serious consequences of chlamydia, annual chlamydia screening is required for all sexually active women 25 years of age and younger. An annual examination is necessary for women over 25 who are at risk (new sexual partner, multiple sexual partners). All pregnant women should be screened for chlamydia.
Complications of chlamydia are rare in men. The infection sometimes extends to the epididymis and causes pain, fever, and, rarely, male infertility (sterility).
Rarely, chlamydial infection can cause inflammation of the joints in combination with skin lesions, inflammation of the eyes and urinary tract - this is the so-called Reiter's syndrome.
The effect of chlamydia on a pregnant woman and her child
Chlamydia in pregnant women increases the risk of miscarriage, premature detachment of the placenta.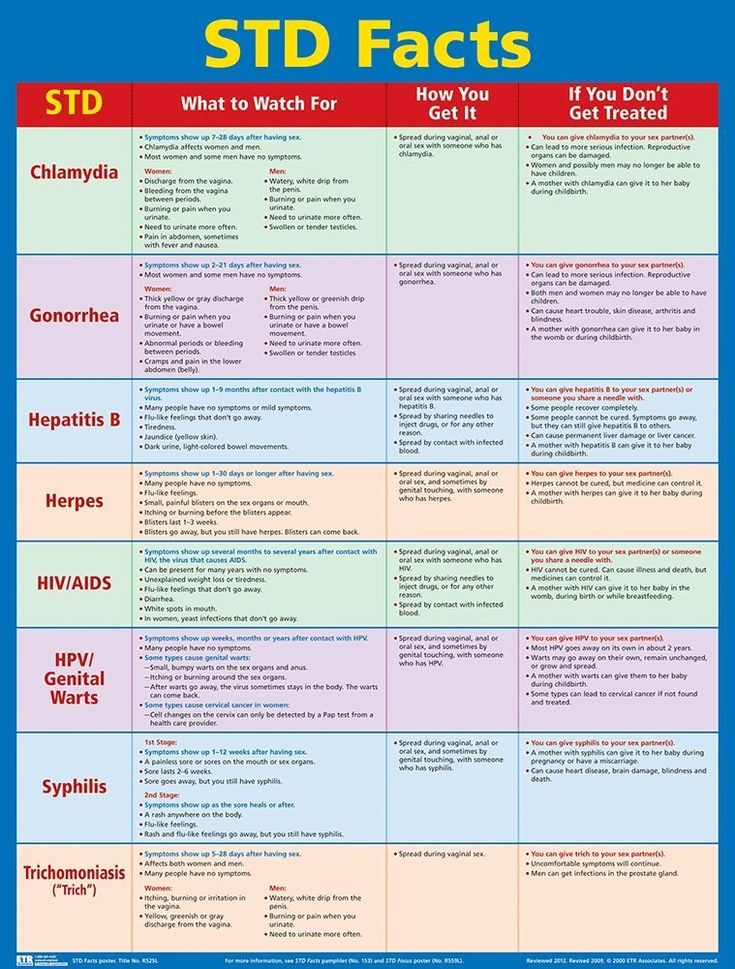 Newborns from infected mothers can get eye and lung infections. A lung infection (pneumonia) can be fatal to a newborn.
Newborns from infected mothers can get eye and lung infections. A lung infection (pneumonia) can be fatal to a newborn.
Diagnosis of chlamydia
Diagnosis includes observation of the patient's clinical symptoms, testing for chlamydia smears from the cervix, scraping from the urinary canal, the first morning urine. Most often, the study is carried out by PCR (polymerase chain reaction). Swabs and scrapings may cause minor discomfort.
In addition, a blood test by ELISA (enzyme-linked immunosorbent assay) for the presence of immunity to chlamydia is carried out, this auxiliary test often helps to establish an accurate diagnosis.
Treatment of chlamydia
Treatment of chlamydia is with oral antibiotics. To prevent re-infection, all sexual partners must be found, examined and treated. Patients with chlamydia should refrain from unprotected sex during treatment, otherwise it is possible to re-infect the sexual partner. Unfortunately, after successful treatment, re-infection with chlamydia is possible, since a strong immunity to this microorganism does not develop. Repeated infection of women with chlamydia leads to a significant increase in the risk of serious complications, including infertility. A re-examination is carried out 4 weeks after treatment.
Repeated infection of women with chlamydia leads to a significant increase in the risk of serious complications, including infertility. A re-examination is carried out 4 weeks after treatment.
Prevention of chlamydia
The best way to prevent sexually transmitted infections is through long-term sexual contact with one healthy sexual partner. Latex male condoms, when used correctly, drastically reduce the risk of transmission.
Annual chlamydia screening required for all sexually active women 25 years of age and younger. An annual examination is also necessary for women over 25 who are at risk (new sexual partner, multiple sexual partners). All pregnant women should be screened for chlamydia.
Any manifestations, such as pain or discomfort when urinating, unusual rash, discharge are a signal to stop sexual intercourse and immediately examine in a specialized clinic - KVD. If the patient is found to have chlamydia (or any other STI), he must inform his sexual partners so that they also undergo a full examination and appropriate treatment.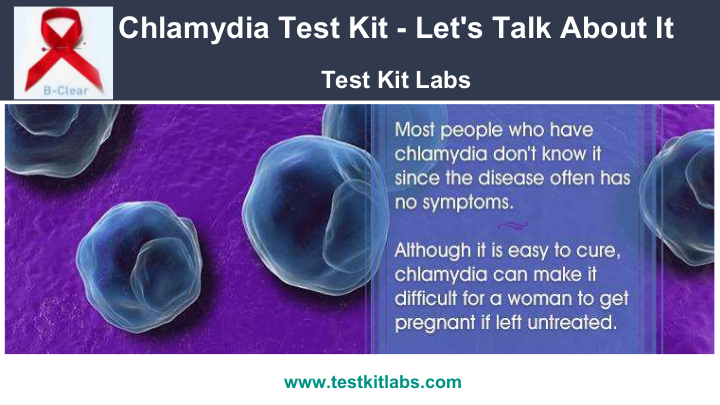 This will reduce the risk of developing serious complications and prevent the possibility of re-infection.
This will reduce the risk of developing serious complications and prevent the possibility of re-infection.
Patients with chlamydia should refrain from unprotected sex during treatment, otherwise the sexual partner may be re-infected.
Chlamydia and pregnancy
Their favorite habitat is the cervix (more precisely, the mucous membrane of the cervical canal). It is there that they are located in colonies, i.e. are not found throughout. Such frequent cases are associated with this fact, when one doctor takes a smear from the cervical canal and chlamydia is found in it, and the other one also takes a smear a day later, but chlamydia is not found again. That is why the diagnostic value of swabs for chlamydia is quite low - about 30%.
How chlamydia manifests itself
During an exacerbation of the infectious process, women's complaints may be different, depending on the level of chlamydia spread.
When chlamydia is found in the cervix, there may be slight discharge from the vagina, accompanied by moderate pulling pains in the lower abdomen, which is typical for local exacerbation of the process (there are practically no complaints in the chronic form).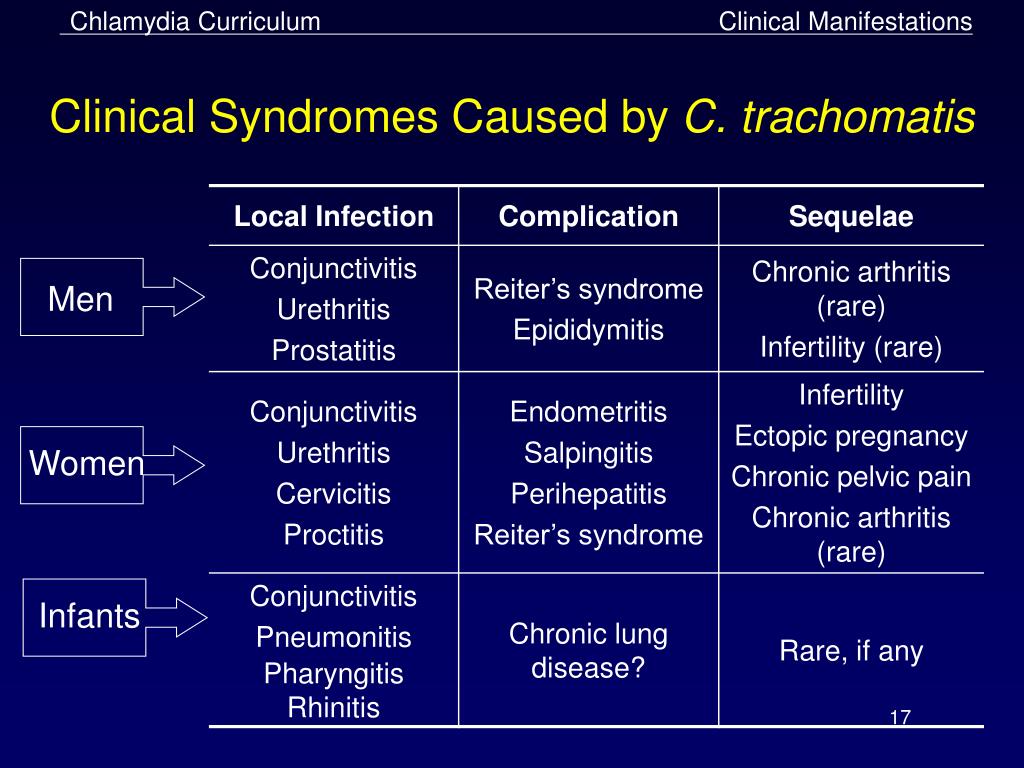 If the infection spreads higher (uterine cavity, tubes), then the complaints are more pronounced, because, for example, inflammation of the appendages may begin.
If the infection spreads higher (uterine cavity, tubes), then the complaints are more pronounced, because, for example, inflammation of the appendages may begin.
Exacerbation of chlamydial infection is especially dangerous during pregnancy, as it can lead to various complications.
Possible complications:
- early miscarriages are possible,
- late term premature amniotic fluid and preterm labor,
- in childbirth, there is a high probability of infection of the fetus (conjunctivitis, pharyngitis, otitis and even pneumonia).
Chlamydia diagnostics
The most informative method is a blood test for antibodies (immunoglobulins) to chlamydia. If a small concentration of these antibodies is detected, then they speak of a chronic carriage of chlamydia. If the concentration is high, there is an exacerbation of chlamydial infection.
The diagnosis of "chlamydia" is legitimate when it is confirmed by two fundamentally different diagnostic methods: smear (microscopy) and blood for antibodies to chlamydia (biochemical method). Only when the titer (concentration) of antibodies is high and / or in the presence of complaints specific to this infection, a course of treatment is indicated.
Only when the titer (concentration) of antibodies is high and / or in the presence of complaints specific to this infection, a course of treatment is indicated.
Digits must be multiples, i.e. more or less than twice, from the previous one (IgA 1:40 and IgG 1:80). Titers of 1:5 and less are doubtful and negative. Elevated IgG numbers indicate that the process is chronic. In this case, treatment is indicated if there are certain complaints, or if before that, the person has never been treated for this infection. High numbers of IgA are mainly found in an acute process (primary infection) or during an exacerbation of a chronic one that needs treatment.
What to do if the test is positive?
It must be remembered that today there are almost no 100% reliable methods, including the ELISA method (enzymatic immunoassay) is no exception. Quite often there are “false positive” results - you have to do either repeated tests or use other, fundamentally different methods.
These can be:
- taking smears for the PIF method (examination with a luminescent microscope) - where there may also be “false positive” answers,
- PCR blood test (based on the principle of genetic engineering, the study of DNA or its fragments) - today, its reliability is very high.
In the search for the truth of the diagnosis, quite often, everything can rest either on the financial capabilities of patients, or on the insufficient equipment of a particular laboratory. The better the body's defenses, the less likely it is to contract chlamydia. In which case, only “carriage” threatens you, it is not dangerous for you (only IgG, in low titers, will be determined in the blood test).
It is considered optimal if the whole family is examined at the same time (all interested persons, including children), because in this case, it is possible to identify who is at what stage and monitor the effectiveness of treatment.
In most cases, the causative agents of ureplasmosis and mycoplasmosis do not manifest themselves in any way (latent bacteriocarrier), and only when the process is exacerbated, they cause complications of pregnancy and infection of the fetus, similar to chlamydia. Therefore, when examining women who have had the above problems in the past, swabs and blood are taken at least immediately for these three pathogens. By the way, studies have shown that taking hormonal birth control pills reduces the risk of chlamydia infection, this effect is associated with an increase in the protective properties of cervical mucus (its permeability to bacteria decreases). As mentioned above, chlamydia is dangerous for pregnant women.
By the way, studies have shown that taking hormonal birth control pills reduces the risk of chlamydia infection, this effect is associated with an increase in the protective properties of cervical mucus (its permeability to bacteria decreases). As mentioned above, chlamydia is dangerous for pregnant women.
What to do?
But what to do if, after all, the future mother has been diagnosed with chlamydia in the acute stage?
The placenta can be thought of as a mesh filter through which large molecules cannot pass (they remain in the mother's body). Therefore, in the treatment of a pregnant woman, antibiotics are used that are harmless to the fetus (i.e. those that do not pass through the placenta). These include drugs whose molecular weight is greater than the "capacity" of the capillaries. However, when taking these drugs, the effect on the fetus is still possible. The antibiotic acts primarily on the mother's body, however, during the period of treatment, it changes the metabolism in the body, which in turn affects the metabolism of the fetus. Antibiotics are always prescribed in short courses so that the effects are minimal.
References
- Zofkie AC., Fomina YY., Roberts SW., McIntire DD., Nelson DB., Adhikari EH. Effectiveness of Chlamydia Trachomatis expedited partner therapy in pregnancy. // Am J Obstet Gynecol - 2021 - Vol - NNULL - p.; PMID:33894150
- Zofkie AC., Fomina YY., Roberts SW., McIntire DD., Nelson DB., Adhikari EH. Effectiveness of Chlamydia Trachomatis expedited partner therapy in pregnancy. // Am J Obstet Gynecol - 2021 - Vol - NNULL - p.; PMID:33894147
- Shilling HS., Garland SM., Costa AM., Marceglia A., Fethers K., Danielewski J., Murray G., Bradshaw C., Vodstrcil L., Hocking JS., Kaldor J., Guy R., Machalek D.A. Chlamydia trachomatis and Mycoplasma genitalium prevalence and associated factors among women presenting to a pregnancy termination and contraception clinic, 2009-2019. // Sex Transm Infect - 2021 - Vol - NNULL - p.; PMID:33782146
- Vercruysse J.
 , Mekasha S., Stropp LM., Moroney J., He X., Liang Y., Vragovic O., Valle E., Ballard J., Pudney J., Kuohung W., Ingalls RR. Chlamydia trachomatis Infection, when Treated during Pregnancy, Is Not Associated with Preterm Birth in an Urban Safety-Net Hospital. // Infect Dis Obstet Gynecol - 2020 - Vol2020 - NNULL - p.8890619; PMID:33082702
, Mekasha S., Stropp LM., Moroney J., He X., Liang Y., Vragovic O., Valle E., Ballard J., Pudney J., Kuohung W., Ingalls RR. Chlamydia trachomatis Infection, when Treated during Pregnancy, Is Not Associated with Preterm Birth in an Urban Safety-Net Hospital. // Infect Dis Obstet Gynecol - 2020 - Vol2020 - NNULL - p.8890619; PMID:33082702 - Olaleye AO., Babah OA., Osuagwu CS., Ogunsola FT., Afolabi BB. Sexually transmitted infections in pregnancy - An update on Chlamydia trachomatis and Neisseria gonorrhoeae. // Eur J Obstet Gynecol Reprod Biol - 2020 - Vol255 - NNULL - p.1-12; PMID:33059307
- Hoenderboom BM., van Bergen JEAM., Dukers-Muijrers NHTM., Götz HM., Hoebe CJPA., de Vries HJC., van den Broek IVF., de Vries F., Land JA., van der Sande MAB., Morré SA., van Benthem BHB. Pregnancies and Time to Pregnancy in Women With and Without a Previous Chlamydia trachomatis Infection. // Sex Transm Dis - 2020 - Vol47 - N11 - p.739-747; PMID:32701764
- He W., Jin Y.