Painful urethra after birth
Problems With Urethra After Childbirth? – Knix
TEAM KNIX / FERTILITY PREGNANCY
Giving birth is a major physical trauma and it has impacts on your body beyond your reproductive system.
It is very common for women to experience “urinary retention” or difficulty passing urine following childbirth. But it is important to pee within 6 to 8 hours of delivery to prevent urinary tract infections (UTIs) and keep the bladder healthy.
The good news is that urinary retention is usually temporary and passes once you recover.
How Childbirth Affects the Bladder
Your bladder can be a little traumatized by you giving birth. The pressure exerted by an exiting baby might force it to shut down temporarily. Or any anesthesia you were administered may have decreased its sensitivity, effectively “numbing” it.
As with any abdominal surgery, swelling and pain can also impact your body’s basic functions. Basically, it can take a while for your body to “reboot” after any kind of trauma.
There’s also a psychological effect; you yourself may be nervous to pee. Peeing after childbirth can sting (in part due to tears and incisions) and this may also fill you with dread that inhibits your ability to urinate.
What to Expect After Childbirth
Expect your nurses to be very interested in when you’re ready to pee and how much urine you pass when you do use the bathroom. They want to feel like your body’s basic functions are returning to normal before they release you.
Again, this is similar to any surgery; they want you to pee, or they want to hear you’ve got gas or your tummy’s rumbling, that your appetite is returning etc.
Your nurses or doctors will want you to pee within 6 to 8 hours of delivery and after you go, they’ll want to see how much urine you’ve passed. They may also measure the bladder for distension (a.k.a. fullness).
If you do not manage to urinate within the designated time frame, your healthcare providers may use a catheter to drain your bladder of urine.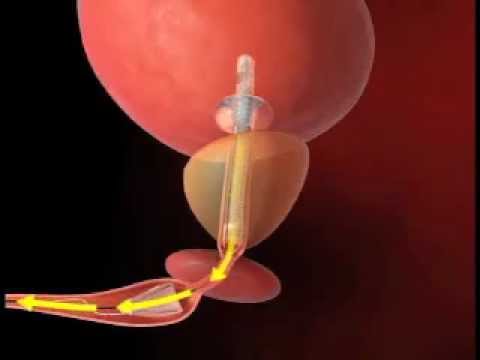 They’ll be on the lookout for signs of a urinary tract infection (UTI) as this is sometimes the reason new mothers cannot pee postpartum.
They’ll be on the lookout for signs of a urinary tract infection (UTI) as this is sometimes the reason new mothers cannot pee postpartum.
Even if you manage to pee and are cleared for release, continue to pay attention to urination and any unusual sensations as your body heals. You should feel that you are making a sure return to normal.
If you’re only able to pee small amounts, if there’s pain or a burning sensation, or if you experience a fever, make sure to book an appointment to see your doctor.
Similarly, if you feel you can’t control leakages and are experiencing incontinence, chat with your doctor.
Urethral Prolapse
While the urethra itself can be bruised during childbirth, this usually heals as swelling is reduced. Other than bruising, no significant sources speak to postpartum urethral damage.
Urethral prolapse (urethrocele) is when the urethra pushes into the vaginal canal or protrudes out of the urethral opening.
Urethral prolapse in female patients is a rare event. It usually occurs in much older women. While pregnancy and childbirth may be precursors to urethral prolapse in later life, there have only been 2 documented cases of postpartum urethral prolapse (source).
How Common Is Postpartum Urinary Retention?
Postpartum urinary retention (PPUR) affects roughly 8% of women who give birth (source). Risk factors for experiencing urinary retention include:
- Being catheterized during labor
- Prolonged labor
- An episiotomy, which is an incision made in the perineum—the tissue between the vaginal opening and the anus—during childbirth
- Epidural analgesia (having regional epidural administered during labor)
- Perineal tear and sphincter rupture can cause urinary retention
How to Help Your Bladder Recover Immediately Postpartum
There are some steps you can take to help your bladder recover after childbirth.
Sip, Don’t Gulp
Drinking fluids helps kick your systems back into action. Rather than gulping vast quantities of water, sip water continually.
Rather than gulping vast quantities of water, sip water continually.
Get Moving (Gently Does It)
Moving around similarly helps your body wake back up. While you may be weak still, begin as soon as you can, even if it’s with short, accompanied walks up and down the ward.
Take it easy and listen to your body (don’t push through unusual pain). But as you gain strength, your body will respond and your systems will find their rhythm again.
If You’re Shy, Ask for a Little Space
It can be difficult to pee with an audience, so if your nurses are hovering and you’re finding it gives you performance anxiety, don’t feel shy to politely ask for a little space.
Try Sitz Baths or Ice Packs
If swelling and bruising has caused pain that is making it psychologically difficult for you to urinate, try ice packs or ask your nurse if a sitz bath would help relieve that pain.
Picture a Waterfall…
It may be a little silly (and it’s more a way of overcoming a psychological hurdle) but picturing running water can sometimes help if you’re trying to stimulate your urge to urinate.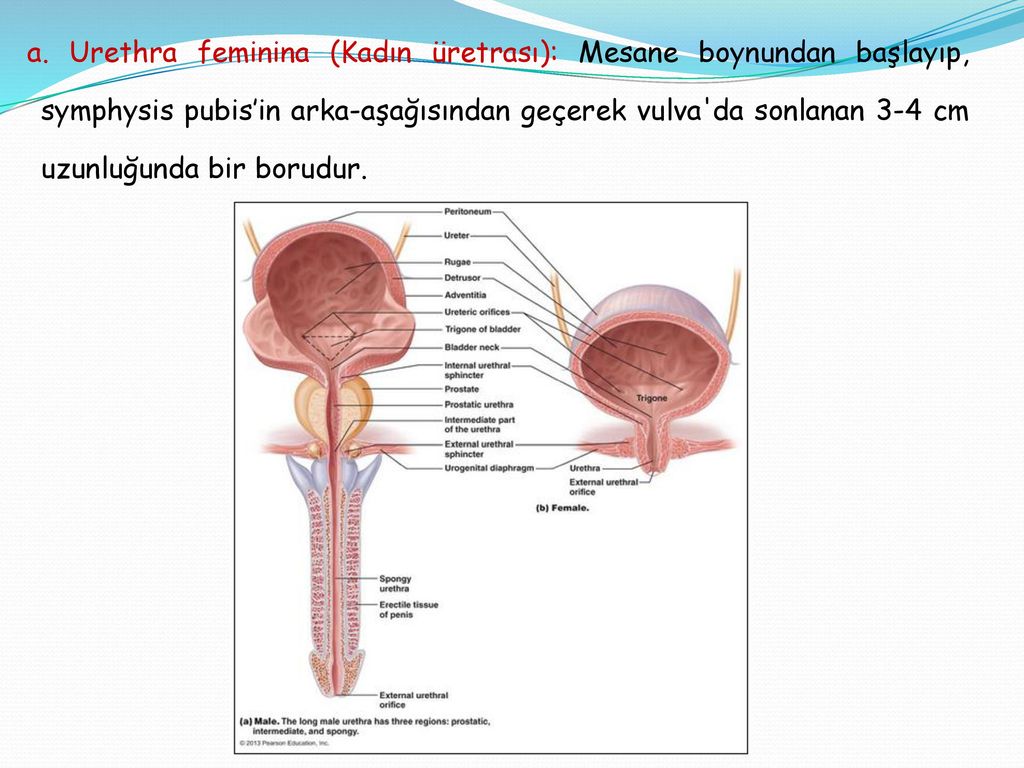 You can also run a tap.
You can also run a tap.
Timed Voiding
Urinating on a schedule or double-voiding (where you urinate and then go again 10–15 minutes later) can help make sure your bladder empties.
What About Postpartum Urinary Incontinence?
It is common to experience a little incontinence during pregnancy, due to:
- Increased pressure on the bladder: Your growing baby puts pressure on the bladder and surrounding organs, which can lead to loss of urine or an increased need to urinate in women during pregnancy.
- Extra fluids in your body: During pregnancy, you should drink between 2 and 3 liters of water per day. More fluids make it easier to leak urine.
- Hormonal changes: Hormonal changes during pregnancy cause your pelvic floor muscles to relax, which can lead to incontinence. (Pelvic floor exercises can help strengthen muscles both during pregnancy and postpartum, after delivery.)
This experience can continue after childbirth (i. e., postpartum urinary incontinence) and depending on your delivery, may become worse or begin to dissipate. If postpartum urinary incontinence worsens after childbirth, talk to your doctor as there may have been damage to your pelvic floor muscles.
e., postpartum urinary incontinence) and depending on your delivery, may become worse or begin to dissipate. If postpartum urinary incontinence worsens after childbirth, talk to your doctor as there may have been damage to your pelvic floor muscles.
It’s also recommended to do (or continue) doing Kegel exercises after childbirth to help your pelvic floor muscles regain their strength after a vaginal delivery.
Do Kegel Exercises to Strengthen Your Pelvic Floor Muscles
These exercises strengthen the pelvic floor muscles, which support the uterus, bladder, small intestine, and rectum and will help you manage bladder control problems.
Good news: Kegel exercises or pelvic floor muscle exercises can be done any time, either sitting or lying down. You can even do Kegel exercises when you are eating, sitting at your desk, or when you are resting.
How Are Kegel Exercises Done?If you’re unsure how to do pelvic floor or Kegel exercises, your doctor or physiotherapist can help you. But basically it’s like pretending you have to urinate and then holding it. You relax and tighten the muscles that control urine flow.
But basically it’s like pretending you have to urinate and then holding it. You relax and tighten the muscles that control urine flow.
One way to learn the pelvic floor muscles you should activate is to pay attention when you pee: Start to pee and then stop. You should feel the muscles in your vagina, bladder, and anus get tight and move up. These are the pelvic floor muscles.
Wear Leakproof Underwear While You’re Recovering from Giving Birth
Pregnancy and childbirth are not casual undertakings and it’s only natural that your body would feel a little worse for wear after giving birth to a baby. While the media has normalized an expectation that you can bounce back to normal in no time and be “red carpet ready,” it’s not really the case for many women.
Instead, allow yourself time to recover and provide yourself tools to ease that recovery time. Soreness, tenderness, and light bladder leaks will likely be part of that recovery. Leakproof underwear will offer you protection from any involuntary urine leakage and help minimize the embarrassment and inconvenience of postpartum urinary incontinence.
Do keep your doctor abreast of what’s happening and always be alert to signs of more serious medical concerns. In particular, don’t ignore unusual or persistent pain or bleeding. Other than that, be kind to yourself—you just gave birth!
Written by Jane Flanagan — Updated on March 1, 2022.
After Giving Birth, I Had a UTI From Hell. My Doctor Didn't Believe Me.
“You just had a baby. Of course you’re in pain,” a doctor informed me three days after giving birth. In the midst of the hazy confusion of taking care of a very tiny human, I had managed to make an appointment for what I was certain was the worst UTI of my life.
“This isn’t normal,” I insisted. “I’m bleeding from where I pee.”
“You’re bleeding from your vagina." He didn't even look. "You just had a baby.” This old-man doctor with a grizzled beard and unkind eyes seemed more confident in his statement the second time he said it, his words and expression informing me he thought my complaints were unwarranted and, frankly, taking up his precious time.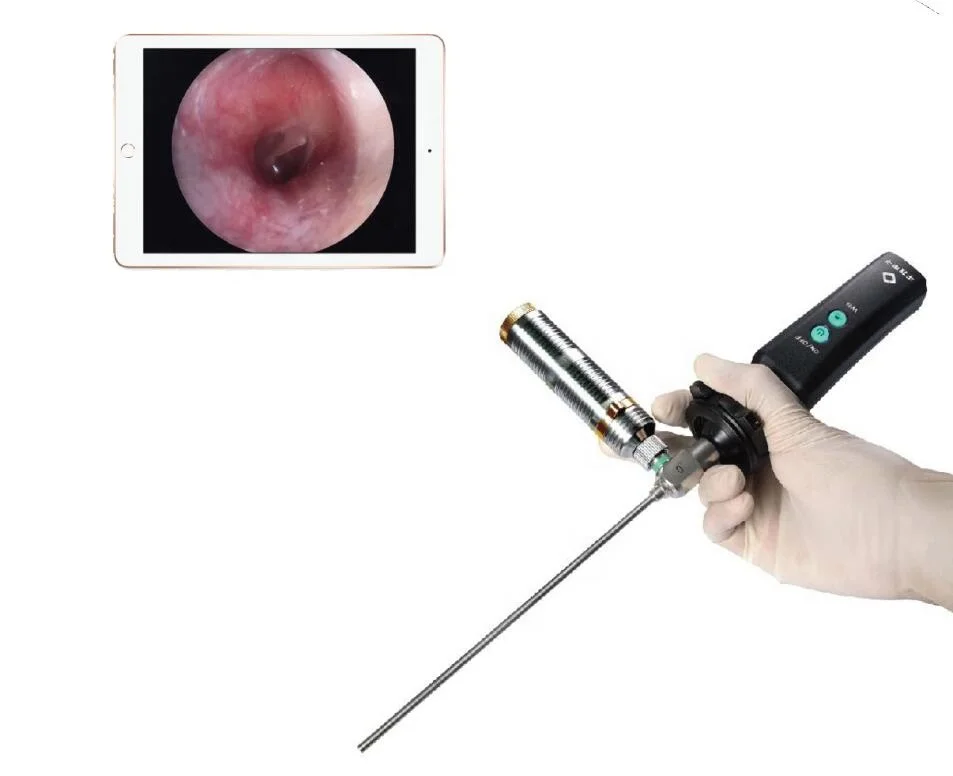
Because my UTI had come on so suddenly, I was forced to see the first doctor available. But I had been shuffled through various physicians in the system throughout my pregnancy so I didn't even have a regular ob-gyn I could ask for advice.
“I know the difference between my urethra and vagina,” I said. “If I’m wrong then I’ve been putting tampons, not to mention other things, in the wrong hole for 20 years.” The doctor didn’t think I was funny, and when he tested my urine, at my insistence, he discovered what I knew would be there — a nasty UTI, likely caused by the catheter inserted when I was given an epidural. One in 3 new moms report having urinary or bowel problems after giving birth, according to a 2013 survey by the nonprofit Childbirth Connection.
I've had both.
I was in one of the best medical systems in one of the most progressive cities in America and I have top-notch health insurance. But I would soon discover, on my own and through discussions with other women, that this lack of postpartum care is too often the norm in the United States, a country where more women die due to pregnancy-related complications than any other developed nation and where childbirth injuries can go undiagnosed for years.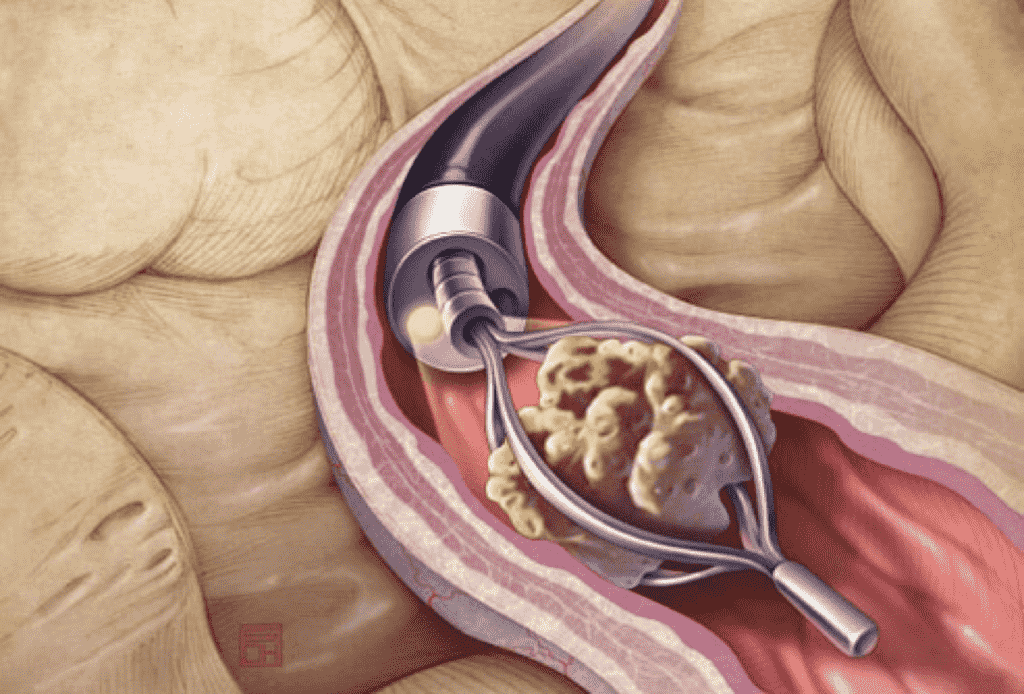
I’ve spoken to many women about their own postpartum horror stories — untreated cracked ribs and pelvic bones, persistent incontinence, spinal fluid leakage leading to throbbing headaches, uterine infections, and swollen labias that make sitting impossible. The common thread was that doctors initially waved away these concerns when the women informed them they knew something wasn’t right with their bodies — until they forcefully advocated for themselves.
I assumed, incorrectly, that the doctors would let me know what to expect and how to take care of myself.
Before I was released from the hospital, about 36 hours after giving birth, no one talked to me about the many symptoms I might experience when I went home, including the possibility of a UTI. This was my first baby. I didn't know what to ask for. I assumed, incorrectly, that the doctors would let me know what to expect and how to take care of myself.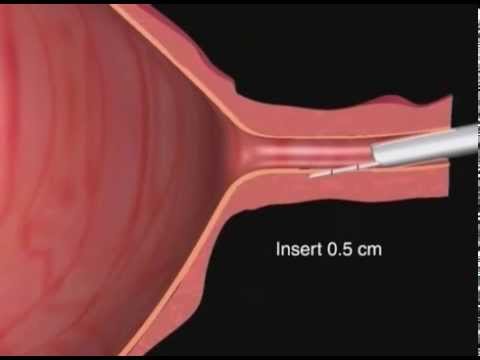 We didn’t talk about hemorrhoids, contractions while breastfeeding that would cause my uterus and vagina to ache constantly, or bleeding nipples due to breastfeeding. These are all common postpartum symptoms, according to a study out of UNC Chapel Hill, the 4th Trimester Project, which for two years has been tracking the care new moms get in the United States. The study found that around half of new moms are still in pain weeks after giving birth.
We didn’t talk about hemorrhoids, contractions while breastfeeding that would cause my uterus and vagina to ache constantly, or bleeding nipples due to breastfeeding. These are all common postpartum symptoms, according to a study out of UNC Chapel Hill, the 4th Trimester Project, which for two years has been tracking the care new moms get in the United States. The study found that around half of new moms are still in pain weeks after giving birth.
The one thing I was told about my postpartum care was to call a doctor if I had blood clots the size of golf balls, a possible sign of postpartum hemorrhaging, either in the toilet when I peed or on the giant maxi-pads that would become my new must-have accessory.
How big was a golf ball again? It’s been a while since I’ve been out on the links, what with the pregnancy and all. Everything else — blood clots smaller than golf balls, pus, throbbing pain, burning, itching — I was led to believe was par for the course.
The only time my injuries were discussed was immediately after the actual childbirth, while my legs were still paralyzed from my epidural.
The only time my injuries were discussed was immediately after the actual childbirth, while my legs were still paralyzed from my epidural and I had my purple, wailing newborn on my chest rooting around for a nipple he had never even met. That’s when the doctor explained I had a first-degree tear. She stitched it up and never mentioned it again. I didn't know even what she meant until I Googled it a day later and learned that, in terms of birth injuries, I'd won the tearing Olympics. A first-degree tear means only the skin around my vagina was ripped apart, compared with a second-degree tear, which penetrates the muscles; or a third degree tear, which extends into the anal sphincter.
No one examined my stitches before I left the hospital, a situation familiar to many new moms I spoke to. “Shouldn’t someone look at my vagina?” I asked my husband. I felt a little ridiculous asking someone to check. Someone would look if there was a problem, wouldn’t they? I considered using the old makeup-compact-between-my-legs trick, the one I’d used to check out my labia for the first time when I was 14, but when I felt the swollen, bleeding tissue with my fingers, I was too scared to look.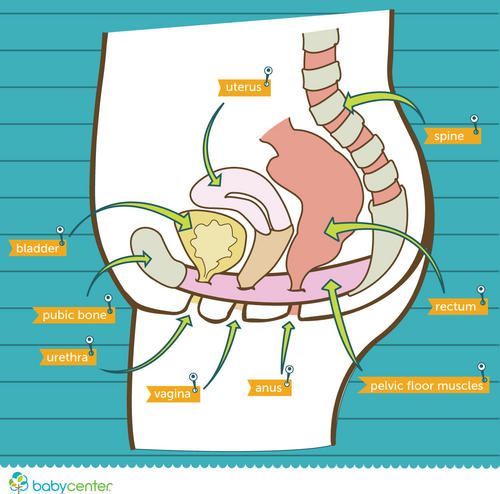
The nurses made an appointment for me to have my stitches checked out six weeks from delivery. A majority of women aren’t scheduled to see their care provider until six weeks after birth, in contrast to a newborn’s first doctor's appointment, which is typically two or three days after bringing the baby home.
When I left the hospital, I knew how to swaddle, diaper, soothe, bathe, and burp my baby. I had no clue how to take care of my own body.
When I left the hospital, I knew how to swaddle, diaper, soothe, bathe, and burp my baby. I had no clue how to take care of my own body. No one even gave me instructions on how to keep the area around my stitches clean and free from infection.
I was given a squirt bottle that looked like it should contain an off-brand version of Gatorade and told to squirt it "down there" when I peed. It was unclear which part of "down there" was being referred to. This gave me the sense from the hospital staff that I shouldn’t be worrying about myself at all, that I should be focusing on caring for my infant.
“First-time mothers, especially, have so little sense of what degree of physical and emotional upheaval is to be expected and what's cause for concern,” says author and researcher Lauren Brody, who wrote the book The Fifth Trimester and interviewed more than 700 American mothers about their physical, mental, and emotional health after giving birth. “Generally, women err on the side of dismissing our own needs.”
I cried every other day the first few weeks after my baby was born in July. The internet told me this was normal. It even has an adorable name, “the baby blues.” But my crying wasn't the result of a hormone-induced depression or a subconscious fear about my radically altered life. I cried because I felt sharp pains every time I rolled over to get my baby from the bassinet and because I'm wasn't yet physically capable of walking up and down my hallway to soothe him. Those pains made it difficult to care for my baby the way I wanted to and I felt like a bad mother. Sometimes the guilt outweighed the pain and I pushed myself to do it anyway, which wasn't good for either of us.
Sometimes the guilt outweighed the pain and I pushed myself to do it anyway, which wasn't good for either of us.
Before I had our baby, my husband Nick and I attended free classes at our hospital on childbirth and taking care of a newborn. Each of them lasted the better part of a day and covered everything from newborn acne to the amount they will likely spit up in a given day (a lot).
This content is imported from Instagram. You may be able to find the same content in another format, or you may be able to find more information, at their web site.
View On Instagram
The hospital didn't offer me a single class, before or after the birth, on caring for my postpartum body. It would have been nice to have an hour of instruction on why and how my body would feel weird, and what would be worth worrying about.
“There is a lack of lay education about the normal physiological events that are going to take place in your body postpartum. It’s not drilled into you, like so much of the other prenatal information,” says Erica Chidi Cohen, a birth and postpartum doula, the co-founder of Loom, a reproductive wellness center in Los Angeles and the author of Nurture: A Modern Guide to Pregnancy, Birth, Early Motherhood. “No one tells women they might have postpartum bleeding for eight weeks, they might have uterine cramping for up to a month, excessive sweating, urinary incontinence, the high possibility of a UTI if you had an epidural.”
It’s not drilled into you, like so much of the other prenatal information,” says Erica Chidi Cohen, a birth and postpartum doula, the co-founder of Loom, a reproductive wellness center in Los Angeles and the author of Nurture: A Modern Guide to Pregnancy, Birth, Early Motherhood. “No one tells women they might have postpartum bleeding for eight weeks, they might have uterine cramping for up to a month, excessive sweating, urinary incontinence, the high possibility of a UTI if you had an epidural.”
It’s complete bullshit that a new mom should have to rely on the internet, with its anecdotal and potentially misleading information, to scrutinize every new ache and pain. I’ve been lucky to get advice from a village of women, some I know well, and others near-strangers on social media who have given me advice on how to create ice packs from maxi-pads and baby diapers; why I should use olive oil as nipple cream; and to squirt lidocaine on Tucks pads like toothpaste, smush it around, and stick 'em where it hurts like a poultice.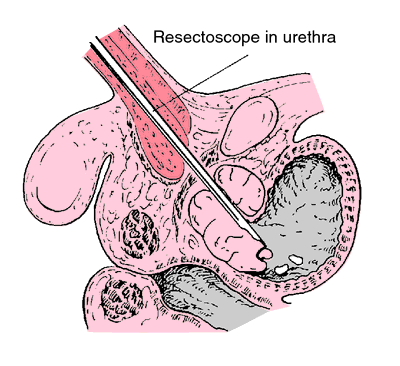 This is pure magic. Their help has been invaluable, but I should be getting advice and guidance from medical professionals. I've since reached out to friends who live across the country and are trained ob-gyns, and taken to weeding through the great morass of medical information on the internet.
This is pure magic. Their help has been invaluable, but I should be getting advice and guidance from medical professionals. I've since reached out to friends who live across the country and are trained ob-gyns, and taken to weeding through the great morass of medical information on the internet.
Giving birth is painful. Recovering from giving birth is also painful. But there’s no reason that pain should be a mystery.
Jo Piazza is the author of the memoir How to Be Married and the novel Fitness Junkie.
Jo Piazza Jo Piazza is author of seven critically acclaimed books, both fiction and non-fiction which have been translated into more than ten languages, including her most recent, Charlotte Walsh Likes to Win.
Problems with urination after childbirth: pain, cramps, burning
PreviousNext
- Problems with urination after childbirth
- How to speed up the recovery of bladder function
- It is recommended to consult a doctor
Contents:
During the postpartum period, many women have difficulty urinating.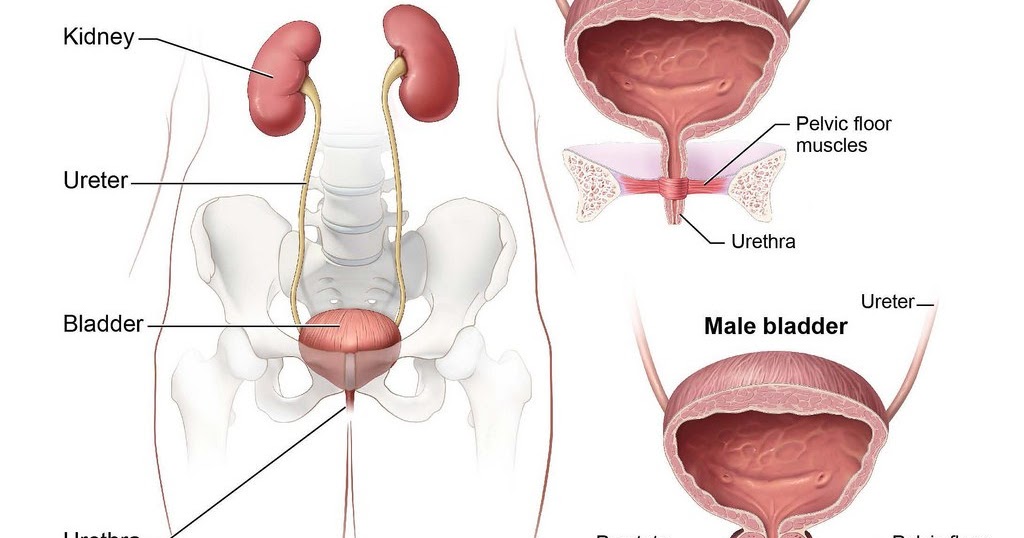 Lack of urge or, conversely, too frequent urge, pain, leakage when coughing or laughing is a consequence of stretching the muscles of the pelvic floor and reducing the tone of the bladder.
Lack of urge or, conversely, too frequent urge, pain, leakage when coughing or laughing is a consequence of stretching the muscles of the pelvic floor and reducing the tone of the bladder.
Problems with urination after childbirth
After giving birth, a woman may not feel like going to the toilet at all, even when her bladder is already full.
This is due to the fact that the pressure of the uterus on the bladder disappears, the tone of the bladder decreases, it increases in size, swells and begins to accumulate a lot of fluid. His sensitivity may decrease due to the use of painkillers in childbirth, muscle spasms, or fear of pain.
This problem does not require special treatment: gradually the tone of the bladder increases, the swelling subsides, and urination returns to normal. It’s just worth at first regularly reminding yourself that you need to visit the toilet.
Frequent and profuse urination in the first days after childbirth indicates the removal of excess fluid from the body. If you often want to go to the toilet, and the amount of urine is scanty, it is better to consult a doctor, as this may be a sign of the onset of inflammation of the bladder or urethra.
If you often want to go to the toilet, and the amount of urine is scanty, it is better to consult a doctor, as this may be a sign of the onset of inflammation of the bladder or urethra.
Most often, burning and pain are explained by the ingress of urine on abrasions that appeared during childbirth, and unhealed sutures. To reduce discomfort, you can urinate while standing in the shower with your legs wide apart so that the stream of urine does not touch the external genitalia.
If painful urination does not go away after healing of abrasions and stitches (usually on the second or third day) or the bladder itself hurts, this may be a symptom of urethritis or cystitis.
After natural childbirth, the pelvic floor muscles stretch and lose elasticity, relieving pressure on the bladder and urethra. As a result, the bladder loses its ability to close completely, so when laughing or coughing, a few drops of urine may be released. Many women are embarrassed by this delicate problem, but in fact, it can be dealt with with the help of sanitary pads and Kegel exercises.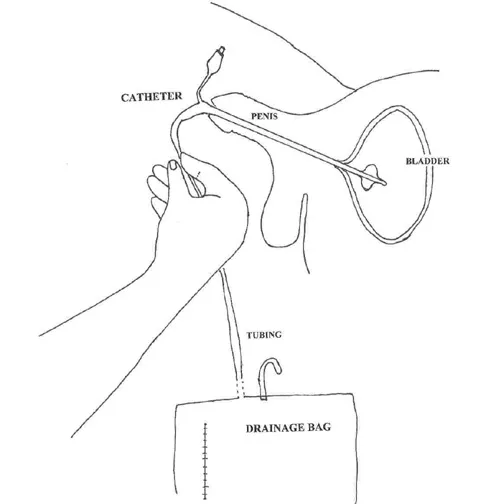
How to speed up recovery of bladder function
If you find it difficult to get up, use the vessel, but not cold, but preheated. Urination can be caused reflexively - the sound of flowing water. If you couldn’t go to the toilet on your own, inform the nurse who will put the catheter.
-
Bladder exercise: do not reduce fluid intake, especially if breastfeeding.
-
Force the bladder to work: in the first days after childbirth, go to the toilet every two hours, even if you do not feel the urge.
-
Walk more: this stimulates the normal functioning of the intestines and bladder.
-
Do special pelvic floor exercises called Kegel exercises.
In a lying or sitting position, tighten the muscles of the vagina and anus as if you are holding back urination, stay in this position for a few seconds, and then completely relax the muscles.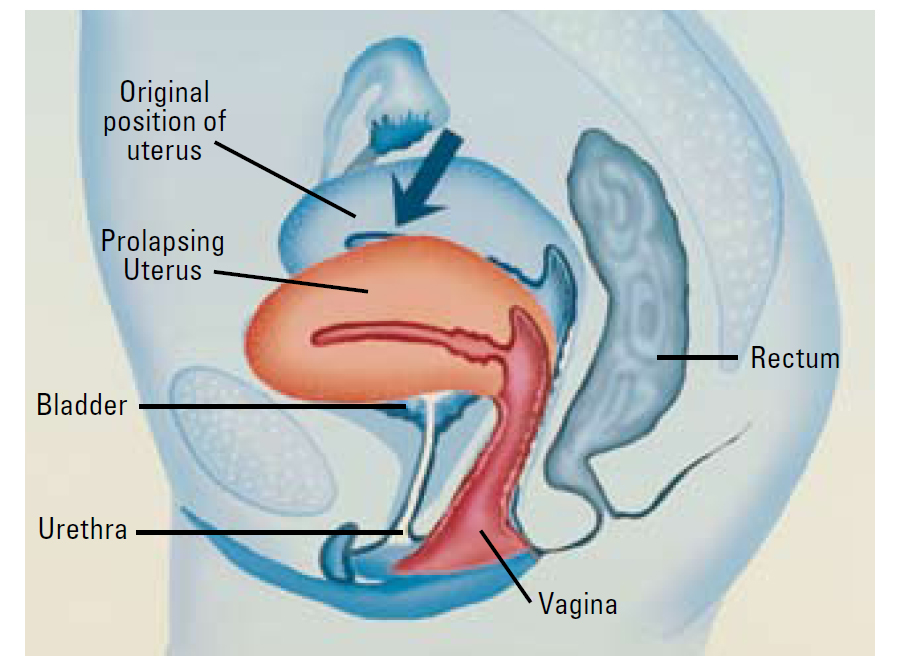 When doing the exercises, do not strain your stomach and buttocks and do not move your legs together. Kegel exercises are recommended to be done at least 3 times a day, and preferably more often. In one approach, it is optimal to perform 8–10 muscle contractions.
When doing the exercises, do not strain your stomach and buttocks and do not move your legs together. Kegel exercises are recommended to be done at least 3 times a day, and preferably more often. In one approach, it is optimal to perform 8–10 muscle contractions.
-
Refuse to use drinks and foods that irritate the bladder - coffee, hot spices, pickles, smoked meats.
It may take from several days to one and a half months to restore the normal functioning of the bladder. If during this time the incontinence does not go away, you need to inform the gynecologist about this at the scheduled examination, which usually happens six weeks after the birth.
It is recommended to see a doctor if:
-
after healing of tears or incisions in the perineum, you still experience pain or burning in the urethra or in the bladder area;
-
frequent urge to urinate, but scant amount of urine;
-
urine cloudy and with a sharp, unpleasant odor;
-
body temperature is increased, even slightly.

These symptoms may be a sign of the development of a urinary tract infection, which, if not properly treated, will cause pyelonephritis. Treatment today can be successfully combined with breastfeeding, so do not be afraid to seek medical help if your bladder does not work like clockwork after childbirth.
| Authors: | Huggies experts |
References:
-
Caring for your Bladder During and after Delivery. University of Michigan Health System.
-
Chaunie Brusie. Postpartum Incontinence Causes and Treatment. Verywell family. Updated on August 04, 2019.
-
After birth—bladder assessment. Mater Mothers' Hospital.
-
Urinary Incontinence and Pregnancy.
 WebMD.
WebMD. -
10 truths: leaking urine in pregnancy and after birth. NCT UK.
Read us on Yandex Zen
PreviousNext
Discomfort in the urethra in women
home
/
All about health
/
Urethral discomfort in women
Urethral syndrome in women is a condition that affects the urethra (the tube that carries your urine out). Urethral syndrome indicates inflammation or damage to the urethra.
Symptoms of urethral syndrome resemble urethritis, which is caused by infection and inflammation of the urethra. They include lower abdominal pain and frequent and painful urination.
Both conditions only increase the irritation of the urethra. Urethritis develops against the background of bacterial and viral infections, while the cause of urethral syndrome is often unclear.
Causes, symptoms and risk factors for urethral syndrome
Urethral syndrome can have many causes. This should also include physical anomalies in the structure of the urethra - for example, narrowing or irritation that appeared after an injury or surgery.
Urethral irritation can be caused by:
-
fragrant products, perfumery,
-
soap, bath foam or sanitary napkins,
-
diabetes mellitus or disharmony;
-
spermicidal lubricant,
-
certain drinks and foods containing caffeine,
-
chemotherapy and radiation.
Injury to the urethra can be caused by:
-
sexual activity,
-
diaphragm use,
-
use of tampons
-
cycling, horseback riding.
Urethral syndrome may also occur in postmenopausal women in whom urethral injury is promoted by estrogen deficiency (female sex hormones during the first 14 days of the cycle) and vaginal dryness.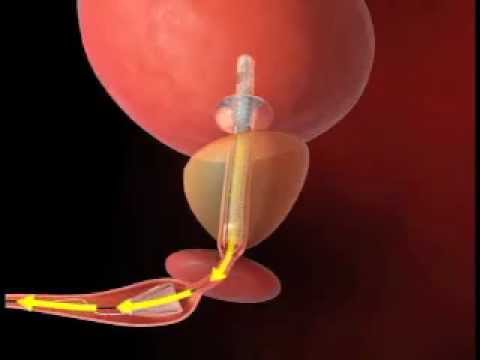
Estrogen deficiency in women is accompanied by impaired blood supply to the bladder and urethra, as well as a sharp decrease in the barrier function of the urothelium.
The formation of a barrier (protective) layer in the urethra and bladder in women is mainly a hormonally dependent process, where estrogens affect its synthesis, and progesterone affects its release by epithelial cells.
If during the examination a bacterial or viral infection was detected, then we are talking about urethritis, and not about urethral syndrome.
Symptoms of urethral syndrome in women include:
-
lower abdominal pain,
-
feeling of pressure in the abdomen
-
a recurring urge to urinate urgently
-
frequent urge to urinate
-
urinary problems,
-
pain during urination
-
discomfort in the vulva,
-
pain during sex
-
blood in the urine.
Diagnosing urethral syndrome is very difficult - for this you need to exclude other possible causes of the above symptoms, in particular - infections caused by viruses and bacteria.
Make an appointment
To make an appointment with a specialist, use the appointment form
Sign up
Modern equipment
The most modern medical equipment in the hands of our specialists turns into a perfect tool to fight for your health.
Certificates and sick leave certificates
We issue sick leave certificates, medical books, university certificates, employment certificates, driver's licenses, weapons, traffic police and others.
Convenient working hours
Our clinics are open every day, which means that medical specialists are always ready to help, even on weekends.
Home help service
Calling doctors at home, examinations and treatment procedures at home.