Baby with cold sleeping more
Do Babies Sleep More When They're Sick? Here's What To Expect
Life
Shutterstock
by Grace Gallagher
You can probably tell pretty quickly when your kiddos are getting sick: They get that telltale glassy-eyed look, they don’t want to eat even their favorite foods, and their energy level dips. While you’d usually rejoice at the sound of a quiet house, it's actually pretty awful to realize your kids aren’t feeling their best, especially when they’re babies and can’t articulate how they feel. One of the first signs of sickness in your baby can be a change in sleep. But do babies sleep more when they’re sick?
“During sleep, our bodies heal, so it's drastically important that we give babies and infants a chance to do just that,” pediatrician Dr. Tanya Altmann tells Romper. “If they wake up in the middle of the night, feel free to go in and comfort them and encourage them to sleep; that will help them get better soon and fight off the illness. ” She adds that while schedules are usually great, it's ok to break from routine while the child is sick.
Just like you probably crave sleep when you’re under the weather (or when you’re caring for kids during flu season) babies will likely sleep more when they’re sick, but unfortunately that extra snoozing might not happen during the night.
Your baby may actually sleep less when they’re in the midst of sickness because they’re uncomfortable (sorry to break the bad news), but an uptick in sleep can mean your baby is on the mend. “Often when the illness is subsiding and symptoms such as fever are lessening, then you will see babies sleep more,” pediatric hospitalist Dr. Cindy Holt tells Romper. “Some parents are concerned when this happens, but it is just the body’s natural response to the recovery process.”
Sick children will give you signs when they’re tired so you can follow their cues to figure out when they need the extra shuteye. You might be tempted to put them to bed earlier, which does work in some cases, but they could really just need an extra nap instead.
“When babies are sick, they usually will sleep when they need to, which often tends to be during the day,” Altmann tells Romper. “Sometimes though they are so uncomfortable it will be hard for them to settle down, so usually comforting measures like rocking may help. If they seem tired, then go for an earlier bedtime and keep your fingers crossed [that] they sleep all night!”
It can seem like your baby is sleeping a staggering amount (even when they’re not sick). “The first few months of life, babies need about 14 to 17 hours of sleep in a 24-hour period and will usually wake up every two or three hours on their own to feed," Altmann says. As they get older, they'll sleep less overall, but will begin sleeping longer stretches at night. You may also feel like they're sick all the time, but that doesn't mean you're doing anything wrong. In fact, "most healthy babies will get six to eight colds before their first birthday," per Parents. Fun.
During a cold or flu, you might think your little one is having a sleep regression, especially if they’re waking up during the night or taking more naps than usual, but it’s nothing to worry about. “Too much sleep is only a concern if it is in association with continued illness, [or] the illness seems to not be getting better,” Holt says. “Always call your physician if you're concerned.”
“Too much sleep is only a concern if it is in association with continued illness, [or] the illness seems to not be getting better,” Holt says. “Always call your physician if you're concerned.”
Babies heal through sleep so it's important they get enough of it, but “in general, it doesn't really matter when they get extra sleep,” Holt says. So if they’re acting tired way before bedtime, it’s totally fine to put them to bed early, or to incorporate an extra nap into the day. Who knows, maybe you can get a snooze in too, or more likely, some uninterrupted time to sanitize every surface in your home.
Experts:
Tanya Altmann, M.D., pediatrician
Cindy Holt, M.D., Pediatric Hospitalist, Sierra Vista Regional Medical Center in San Luis Obispo, Calif.
Common cold in babies - BabyCentre UK
In this article
- What causes colds?
- How do colds affect babies?
- How do I treat a cold?
- When should I take my baby to the doctor?
- Can I help prevent my baby from getting colds?
It’s upsetting to watch your baby suffer his first cold. He will be uncomfortable, snuffling and may have trouble feeding. But there’s a lot you can do to ease your baby’s discomfort.
He will be uncomfortable, snuffling and may have trouble feeding. But there’s a lot you can do to ease your baby’s discomfort.
Remember too, it’s called the common cold for a reason. Your little one may get seven or more colds before his first birthday (Brennan 2016, Whelan and Gill 2017). Colds can come on quickly and the symptoms are often at their worst in the first two or three days (NICE 2016).
Colds tend to hang around longer in babies than adults, but your little one's symptoms should clear up within about two weeks (NICE 2016). A mild cough may go on for up to three weeks (NICE 2016). It’s not a serious illness, but it may mean a lot of tissues and a few long nights for you and your partner (NICE 2015).
What causes colds?
A cold is an infection of the mouth, nose and throat (upper respiratory tract). It can be caused by one of many different viruses (NICE 2016). Babies tend to get a lot of colds because their immune systems are still developing (NHS 2015a).
Colds can be spread when someone with a cold sneezes or coughs, transmitting a virus into the air to be inhaled by someone else. Colds are also spread through contact, especially hand-to-hand contact (NICE 2015). So always cover your mouth when you cough, and wash your hands after blowing your nose.
If you’re at a playdate with another baby who has a cold, avoid sharing toys. This will help to prevent spreading a cold virus (NICE 2016).
Experts aren't really sure why colds are so much more common in winter than in summer. One theory is that being cold and breathing in cold air makes it easier for the common cold to develop, but we need more research to be sure (NICE 2016).
How do colds affect babies?
If your baby has a common cold, you may notice some of the following symptoms:
- general restlessness and irritability
- a runny or stuffy nose (congestion)
- sneezing
- coughing
- fever
(NICE 2016)
Your baby may be having trouble breathing through his nose if he’s all stuffed up, so feeding may be difficult (NICE 2016).
If your baby has previously been sleeping through the night, you’ll be reminded of those first few weeks of his life. He may wake up several times because his nose is stuffy (NICE 2016). Giving him plenty of cuddles will help him feel better.
Sometimes, a bad fit of coughing may make your baby throw up (NICE 2016). Although this can be distressing to see, it's usually nothing to worry about (Sambrook 2017). If it happens a lot, or if you have any concerns about this or any other symptoms, speak to your health visitor or GP.
Sometimes, colds can cause ear infections in young children (NICE 2016). Find out what to do if your baby gets an ear infection.
How do I treat a cold?
There's no cure for the common cold, but it should go away on its own within a few weeks (NICE 2016). In the meantime, there are a few things you can do to ease your baby's discomfort:
- Make sure your little one gets plenty of rest.

- Sit your baby upright when you can, as this helps him to breathe more easily (Whelan and Gill 2017).
- Offer your baby extra breastfeeds to keep his fluids up (NHS 2015a, NICE 2016). If he's formula-fed, offer extra drinks of water instead – just be sure to boil it first then let it cool if he's under six months (NHS 2015b).
- Infant paracetamol or infant ibuprofen can help relieve fever and pain. You can give your baby paracetamol from two months if he was born after 37 weeks and weighs more than 4kg (9lb) (MHRA 2011). You can give him ibuprofen if he is three months or older, and weighs at least 5kg (11lb) (MHRA 2016). Ask your pharmacist or GP if you’re unsure about the correct dose to give your baby.
- Your baby is too young to blow his own nose, so help him to breathe more easily by wiping his nose for him. If your baby is having trouble feeding because of a stuffy nose, nasal saline drops (sterile salt water) may help to unblock his nose. You can buy these from your pharmacy.
 Apply one or two drops to each nostril 15 minutes before a feed (NICE 2016).
Apply one or two drops to each nostril 15 minutes before a feed (NICE 2016). - A vapour rub may help your baby to breathe more easily (NICE 2016). You can buy one from your pharmacy, but make sure you follow the manufacturer’s age guidelines as they are often only suitable from three months. Apply it to your little one's chest and back, but don’t put it on his nostrils, as this isn't safe, and will sting.
- If the skin around your baby's nose is starting to become irritated, you can dab a little petroleum jelly on to soothe and protect it (Alli 2017). Use it sparingly, though, so your baby doesn't breathe it in or eat it.
- Breathing in steam may help to loosen your baby’s blocked airways and relieve his cough. You could try sitting in a steamy bathroom for a few minutes, with the shower on, while holding your baby. But don’t put your baby too close to hot, steamy water, as it could scald him (NICE 2016).
Don’t give your baby any over-the-counter cough and cold medicines. They are not suitable for children under seven years because of the risk of side-effects, and there’s little evidence that they work (NICE 2016). Also avoid home remedies containing honey, which isn't safe for babies under one year (Sambrook 2017).
They are not suitable for children under seven years because of the risk of side-effects, and there’s little evidence that they work (NICE 2016). Also avoid home remedies containing honey, which isn't safe for babies under one year (Sambrook 2017).
Does your baby need antibiotics?
GP Claire Kaye discusses whether your doctor should give your child antibiotics.More baby videos
When should I take my baby to the doctor?
It's always worth having a word with your health visitor or taking your baby to the GP if you have any concerns about his health. If nothing else, they can help to put your mind at rest and give you more tips for caring for your baby at home.
When your baby has a cold, you should take him to the GP if:
- He's under three months old with a temperature of 38 degrees C or more, or he's three to six months old with a temperature of 39 degrees C or more (NHS 2016).
- His symptoms are getting worse rather than better after about five days (Sambrook 2017).

- He has had a cough for three or four weeks (NHS 2015a, Sambrook 2017).
- He is rubbing his ears and seems irritated. This could signal an ear infection (NHS 2015a).
- He's been producing green, yellow or brown mucus for 10 days or more (Sambrook 2017).
If at any point your little one seems to be having trouble breathing, take him straight to your nearest accident and emergency (A&E) unit (NHS 2015a).
Can I help prevent my baby from getting colds?
If you’re breastfeeding, try to continue as this is one of the best ways to protect your baby’s health. It passes antibodies to your baby that will help him fight infections. It isn’t a foolproof way to protect your baby’s health, but breastfed babies are better at fending off colds and other infections (NHS 2017).
You can also protect your baby by trying to keep him away from anyone with a cough or a cold. Or ask them to wash their hands thoroughly before holding your baby (NICE 2016). When your baby does have a cold, make sure everyone in the family washes their hands often to reduce the risk of it spreading (NHS 2015a, NICE 2016).
When your baby does have a cold, make sure everyone in the family washes their hands often to reduce the risk of it spreading (NHS 2015a, NICE 2016).
It's never fun to see your little one under the weather, but a few extra cuddles and plenty of rest should have him back to normal in no time. Just keep those tissues handy!
You might also like:
- Learn the difference between the common cold and flu.
- How long will your baby's cold be contagious? Find out.
- Think you know how to identify and treat a cold? Test your knowledge with our common cold quiz.
References
Alli RA. 2017. Treating colds in children. WebMD, Children's Health. www.webmd.com [Accessed April 2018]
Brennan D. 2016. When your baby has a cold. WebMD, Children's Health. www.webmd.com [Accessed April 2018]
MHRA. 2011. Liquid paracetamol for children: revised UK dosing instructions have been introduced. Medicines & Healthcare products Regulatory Agency, UK Public assessment report. www.mhra.gov.uk [Accessed April 2018]
www.mhra.gov.uk [Accessed April 2018]
MHRA. 2016. Ibuprofen 100 mg/5 ml oral suspension. Medicines and Healthcare products Regulatory Agency, UK Public assessment report. www.mhra.gov.uk [Accessed April 2018]
NHS. 2015a. Colds, coughs and ear infections in children. NHS Choices, Health A-Z. www.nhs.uk [Accessed April 2018]
NHS. 2015b. Drinks and cups for babies and toddlers. NHS Choices, Health A-Z. www.nhs.uk [Accessed April 2018]
NHS. 2016. Treating a fever (high temperature) in children. NHS Choices, Health A-Z. www.nhs.uk [Accessed April 2018]
NHS. 2017. Benefits of breastfeeding. NHS Choices, Health A-Z. www.nhs.uk [Accessed April 2018]
NICE. 2016. Common cold. National Institute for Health and Care Excellence, Clinical Knowledge Summaries. cks.nice.org.uk [Accessed April 2018]
Sambrook J. 2017. Coughs and colds in children. Patient, Child Health. patient.info [Accessed April 2018]
Whelan C and Gill K.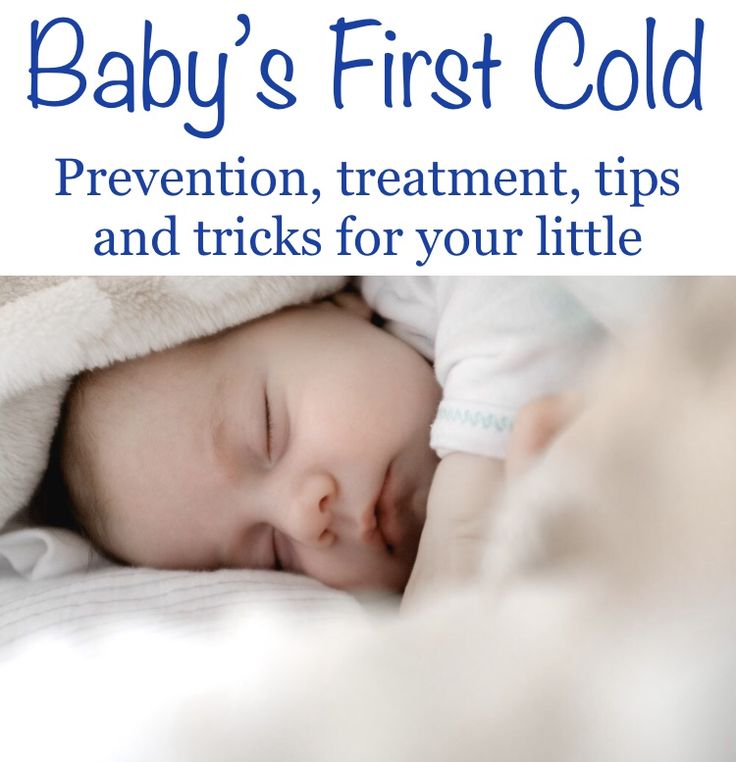 2017. What you should know about colds in newborn babies. Healthline. www.healthline.com [Accessed April 2018]
2017. What you should know about colds in newborn babies. Healthline. www.healthline.com [Accessed April 2018]
Show references Hide references
90,000 child During illness05/18/2016
71403
52
Why doesn’t sleep at night
Author
Natalya Trofimova
Natalya Trofimova
Senior Snow Consultant, Pediatrician
Mom of two daughters
222 By disrupting sleep, our body can respond to a deviation in the state of health. In medical reference books, sleep disorders are listed as a symptom of many diseases. We will analyze when a doctor’s consultation is needed before establishing a child’s sleep.
Child's crisis calendar
Conditions that often affect sleep
Viral infections
Fever, runny nose, cough, change in voice, appetite . Sleep disturbance may appear 1-2 days before fever. Children under one year of age with an increase in temperature need to be examined by a pediatrician, although treatment for uncomplicated SARS is minimal. According to modern recommendations - only antipyretic, nasal cleansing, drinking plenty of water. Antiviral and expectorant drugs have not been proven effective.
According to modern recommendations - only antipyretic, nasal cleansing, drinking plenty of water. Antiviral and expectorant drugs have not been proven effective.
Sleep will return to normal after recovery, in the first days the baby can even sleep more than usual, get enough sleep. And during illness, it is recommended to help the child in every possible way to fall asleep and sleep more. Sleep helps immune cells and liver cells to recover faster, which copes with the consequences of a storm of chemical reactions, intoxication and synthesizes building proteins for new cells to replace the affected ones.
In 2019, The Journal of Experimental Medicine published a study by German scientists that showed that sleep positively affects the expression of integrin receptors by T-cells of the immune system. These are special protein molecules on the surface of the immune cell, with the help of which it attaches to virus-infected cells and destroys them. An increase in stress hormones during sleep deprivation interferes with this mechanism.
Itchy skin
This is a serious enemy of healthy sleep. During severe itching, the proportion of deep sleep decreases. At night, itching intensifies for several reasons: transepidermal water loss and skin dryness increase, the level of corticosteroids in the body decreases, their anti-inflammatory effect weakens, parasympathetic activity and a number of other circadian mechanisms increase.
If you yourself have suffered from atopic diseases, you know how unpleasant it is. And in a baby, even a small speck of dermatitis can lead to anxiety. After all, the size of this speck in relation to the surface area of \u200b\u200bhis body is not at all the same as that of an adult. It is necessary to understand the causes of the rash and treat it together with a pediatrician and a dermatologist. Keep a food diary and take it with you to your doctor's appointment.
A polysomnographic study of a group of children in remission of atopic dermatitis showed that they had more nocturnal awakenings than the control group, with only 15% of awakenings due to scratching. Scientists suggest that chronic itching alters the neurochemical environment in such a way that the processes involved in the mechanisms of sleep maintenance are affected.
Scientists suggest that chronic itching alters the neurochemical environment in such a way that the processes involved in the mechanisms of sleep maintenance are affected.
When the symptoms of dermatitis subside, it is important not to forget about the basic care of dry sensitive skin. Hydration and more moisture. Cream, lotion or ointment for therapeutic care are selected individually, applied to the skin regularly, as often as necessary. After bathing, use emollient directly on damp skin to retain more moisture in the epidermis. This is especially important during the heating season.
Emollients change the quality of a child's life by eliminating dryness and itching, reduce the frequency of dermatitis relapses and the cost of treating exacerbations. The most famous are: Emolium, Locobase RIPEA, Atopic, Perfectoin, Atoderm, Topicrem, Avene, CeraVe, Uriage, Lipikar LaRoche-Posay. More budgetary: Lipobase, Crumb Cream, La Cree, CudoCell, Aveeno, Bepanthen Cream, Vaseline (yes, yes).
Abdominal pains
They also affect sleep. We will not consider acute surgical conditions and intestinal infections. Let's talk about the most common causes of abdominal pain in babies.
The famous colic is actually not as common as people think. Much more often, babies cry from simple overwork. According to various researchers, colic occurs in 5–19%, at most 40% of newborns, by 4–6 months their number decreases to 7–11% [1]. The data differ so much because the condition of the baby is assessed subjectively and it is possible to say for sure that these are colic only when they have passed. How to understand that the child really has colic? Read this article. In short, the rule of threes applies: daily crying for at least 3 hours, at least 3 days a week, at least 3 weeks in a row.
Simethicone preparations may temporarily help with increased flatulence, but they do not act on the causes of flatulence. In the first months of life, the child's intestines gradually adapt to a new type of nutrition. Indeed, before birth, the gastrointestinal tract "rested", the baby ate without his participation.
Indeed, before birth, the gastrointestinal tract "rested", the baby ate without his participation.
A dairy-free diet for breastfeeding mothers may be effective in cases of increased gas production if it is associated with cow's milk protein intolerance. If after a week or two there is no result of the diet, the allergy has nothing to do with it, you should not limit yourself in nutrition for a long time.
Feeding problems also affect excessive gas production:
- Incorrect nipple latch leads to air swallowing.
- Imbalance of "front" and "hind" milk, when the baby is applied infrequently, the mother offers the second breast too quickly when feeding, or the baby is weak and cannot effectively suck out the "hind" milk. With such feedings, gas formation increases.
- When formula-fed, the baby may not be suitable for formula or the nipple on the bottle, or the hole in the nipple is too large.
Poll
What does your baby need to fall asleep?
(you can choose one or more options)
- Singing
- Breast
- Bottle
- Nipple
- Mommy
- Favorite toy
Vooked In addition to anxiety from pain, the baby alternates constipation and profuse, frothy, green stools with a sour smell, there may be regurgitation. This situation is usually temporary and in mild cases does not require drug correction, but it is worth contacting a pediatrician. The lactase enzyme is prescribed if such a condition is prolonged, the child does not gain weight, dermatitis appears on the skin. Breastfeeding is not canceled!
This situation is usually temporary and in mild cases does not require drug correction, but it is worth contacting a pediatrician. The lactase enzyme is prescribed if such a condition is prolonged, the child does not gain weight, dermatitis appears on the skin. Breastfeeding is not canceled!
Gastroesophageal reflux (GER) — reflux of stomach contents into the esophagus. It differs from ordinary regurgitation: the volume is more than 1-2 tablespoons, an hour or more after feeding, crying after regurgitation, the contents may contain bile, an admixture of blood.
A child with reflux gains weight poorly, urinates little, has a hoarse voice when crying, often has acute respiratory infections, otitis, sleep apnea. GER is often combined with prematurity, lactase deficiency, birth injuries of the cervical spine, hernias.
Constipation . This is not only a delay in stool for several days, followed by painful bowel movements, but also daily, but hard stools, which is also unpleasant. It is not necessary to consider constipation the absence of stool in infants (even for a week), which does not bother them at all. There are many possible causes of constipation, from too much complementary food to Hirschsprung's disease and hypothyroidism.
It is not necessary to consider constipation the absence of stool in infants (even for a week), which does not bother them at all. There are many possible causes of constipation, from too much complementary food to Hirschsprung's disease and hypothyroidism.
These are the most common causes of gastrointestinal sleep disorders, when a child sleep consultant cannot help and a pediatrician should be consulted.
Teething (dentation) .
For many children, this process affects the quality of sleep and the duration of bedtime. Read more in this article. General manifestations during teething are short-lived and almost do not require treatment. When in doubt, take your child to the doctor. Sleep disturbances during dentition are short-lived and last only a few days at the peak of eruption.
A large study has been carried out in order to establish the most characteristic symptoms of teething. It was found that increased salivation, swelling of the gums, anxiety, sleep disturbance, reddening of the cheeks, decreased appetite and a slight increase in body temperature were statistically significantly associated with the process of dentition. At the same time, significant differences were recorded only for 8 days (4 days before, on the day of eruption and 3 days after eruption), so scientists called this period the “eight-day window of teething”.
At the same time, significant differences were recorded only for 8 days (4 days before, on the day of eruption and 3 days after eruption), so scientists called this period the “eight-day window of teething”.
How sleep changes when feeling worse
- The child wakes up more often at night due to fever, pain (in the gums, in the throat), skin itching, coughing, runny nose and nasal congestion, and chaotic daytime sleep.
- Children may sleep unusually long during fever.
- Laying is delayed in case of discomfort in the gums, exacerbation of dermatitis and itching. With difficulty in nasal breathing and coughing in a horizontal position, it is difficult for a child to relax and fall asleep.
Illness while working on sleep
If you are working on improving your baby's sleep and suddenly he gets sick or teething, it will complicate the situation. Regardless of whether you are acting alone or accompanied by a consultant, it is necessary to assess the well-being of the child.
With mild symptoms, not disturbed appetite and normal behavior, you can continue to work, if necessary, stay longer at one stage or another. With an increase in temperature and a clear malaise, work according to the method is suspended at the reached stage or, if necessary, steps are taken back, for a while it is even possible to return to the previous association to sleep. When a child feels bad, he is not up to learning, you need to comfort the baby and help him, we pause in working on sleep. We help to fall asleep, we prolong sleep, we do not wake up from daytime dreams, we put them to bed earlier with short daytime dreams. This is necessary so that the baby recovers and recovers faster.
When you feel better, it is important to start returning to your usual routine in time and continue working on improving sleep. In the event of a regression, the passed stages of the methodology must be repeated, but this is easier and takes less time than the first time.
If a child already has the ability to fall asleep on his own, he may also experience sleep regressions during colds, dental, stress, travel. If the difficult period is over, and the child still often wakes up at night, do not delay - BabySleep consultants will help you sort out the situation and improve your child's sleep.
If the difficult period is over, and the child still often wakes up at night, do not delay - BabySleep consultants will help you sort out the situation and improve your child's sleep.
Sources:
[1] Kilgour T., Wade S. 2005, Privorotsky V.F., Lupova N.E., 2012, P. Anderson 2014.
901 Pubmed AAP, Medscape, Sciencedaily
Article updated: 06/26/2021
#healthyson
', nextArrow: '', responsive: [{breakpoint: 1199, settings: {arrows: !1, infinite: !1, slidesToShow: 1}}] }) })When is a doctor urgently needed? Neuro-Clinic Medical Center.
March 4, 2019
In the state of a sick child, several zones are conditionally distinguished: green, yellow and red (similar to a traffic light). When children have a cold, they can be in a safe "green zone" even at high temperatures (up to 41 ° C, if they do not have severe neurological disorders or heart defects), because fever is a tool in the fight against viruses, it does not poses a threat. However, there are “red flags” that every parent should be able to recognize in time.
However, there are “red flags” that every parent should be able to recognize in time.
1. The child is lethargic, wants to sleep all the time
The first thing parents should pay attention to is that the child has become less active. The usually smiling, running, playing baby suddenly became lethargic. He is not interested in what is happening around, wakes up only after you wake him up, immediately falls asleep again or does not wake up at all.
2. Discoloration of the skin
If the skin is pale, this is a reason to take the child to the doctor. When it is bright red, "variegated" or ash gray, this is a signal to consult a pediatrician without delay.
3. Rapid breathing
“Crackling” is heard in the child’s chest, he “grunts”. The respiratory rate in children 6-12 months of age exceeds 50 breaths per minute, in children older than a year - 40 breaths per minute. With such symptoms, call an ambulance.
4. Tachycardia
Increased heart rate. A child up to a year has more than 160 beats per minute, 1-2 years old - more than 150 beats per minute, 2-5 years old - more than 140 beats per minute.
A child up to a year has more than 160 beats per minute, 1-2 years old - more than 150 beats per minute, 2-5 years old - more than 140 beats per minute.
5. Signs of dehydration
Even when the temperature is high, the child's skin may be normal in color and the mucous membranes may be moist. This means that the fluid that he loses through sweat, breathing and urination is replenished.
If this does not happen, the lips and mucous membranes of the child will be dry, the frequency of urination will decrease (less than 1 time in 4 hours). He will refuse liquid or be unable to swallow it. Babies will be sluggish and suck a little.
If dehydration is suspected, the skinfold release time should be checked. Grab the skin on the abdomen on the side of the navel with your thumb and forefinger. Then unclench your fingers: if the skin fold stretches for more than 3 seconds, show the child to the doctor. If it does not straighten out for more than 5 seconds, call an ambulance.
6. Discharge from the ears
Any fluid leaking from the ears - pus or bloody discharge - is most likely a sign of perforation of the eardrum, which requires urgent examination.
7. Chills, vomiting and other symptoms
It is quite common for mild viral infections for parents not to see a doctor. However, remember that the child must be examined by a doctor if he has the following symptoms.
Temperature above 39°C in a 3-6 month old child: fever persists for more than 5 days; chills - a feeling of cold, which is accompanied by muscle tremors; severe swelling/edema of the extremities or joints; weakness in an arm or leg.
Call an ambulance immediately: if the temperature is above 38°C in a child under 3 months old; the rash does not turn pale when pressed; vomiting fountain; the neck is motionless / there was a photophobia; stool with blood; pain in the abdomen, especially in the right half; swelling or hyperemia of the scrotum; unexplained persistent weight loss; increased persistent sweating for more than 6 weeks; persistent epileptic convulsions; neurological symptoms appeared: facial distortion, speech disturbance, impaired coordination of movement, recurring headaches, the child does not use one or more limbs in the game / life activity.