How to tell if your child has lead poisoning
Lead poisoning - Symptoms and causes
Overview
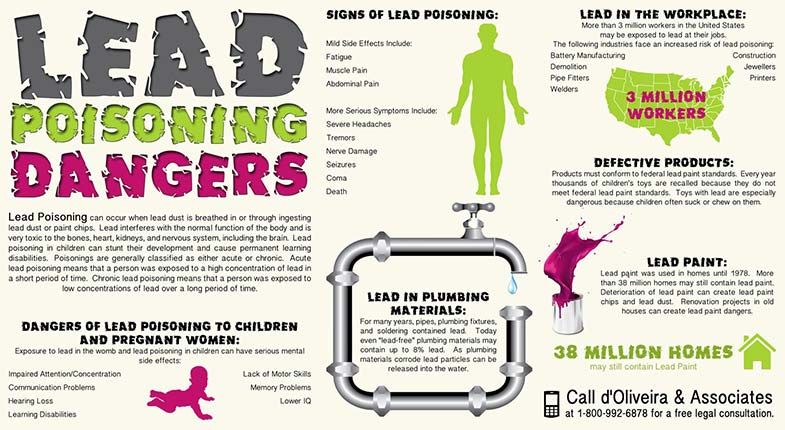
Lead poisoning occurs when lead builds up in the body, often over months or years. Even small amounts of lead can cause serious health problems. Children younger than 6 years are especially vulnerable to lead poisoning, which can severely affect mental and physical development. At very high levels, lead poisoning can be fatal.
Lead-based paint and lead-contaminated dust in older buildings are common sources of lead poisoning in children. Other sources include contaminated air, water and soil. Adults who work with batteries, do home renovations or work in auto repair shops also might be exposed to lead.
There is treatment for lead poisoning, but taking some simple precautions can help protect you and your family from lead exposure before harm is done.
Symptoms
Initially, lead poisoning can be hard to detect — even people who seem healthy can have high blood levels of lead. Signs and symptoms usually don't appear until dangerous amounts have accumulated.
Lead poisoning symptoms in children
Signs and symptoms of lead poisoning in children include:
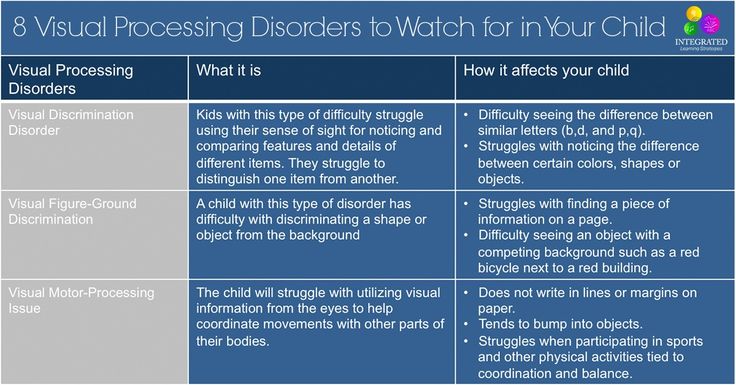
- Developmental delay
- Learning difficulties
- Irritability
- Loss of appetite
- Weight loss
- Sluggishness and fatigue
- Abdominal pain
- Vomiting
- Constipation
- Hearing loss
- Seizures
- Eating things, such as paint chips, that aren't food (pica)
Lead poisoning symptoms in newborns
Babies exposed to lead before birth might:
- Be born prematurely
- Have lower birth weight
- Have slowed growth
Lead poisoning symptoms in adults
Although children are primarily at risk, lead poisoning is also dangerous for adults. Signs and symptoms in adults might include:
- High blood pressure
- Joint and muscle pain
- Difficulties with memory or concentration
- Headache
- Abdominal pain
- Mood disorders
- Reduced sperm count and abnormal sperm
- Miscarriage, stillbirth or premature birth in pregnant women
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
Lead is a metal that occurs naturally in the earth's crust, but human activity — mining, burning fossil fuels and manufacturing — has caused it to become more widespread.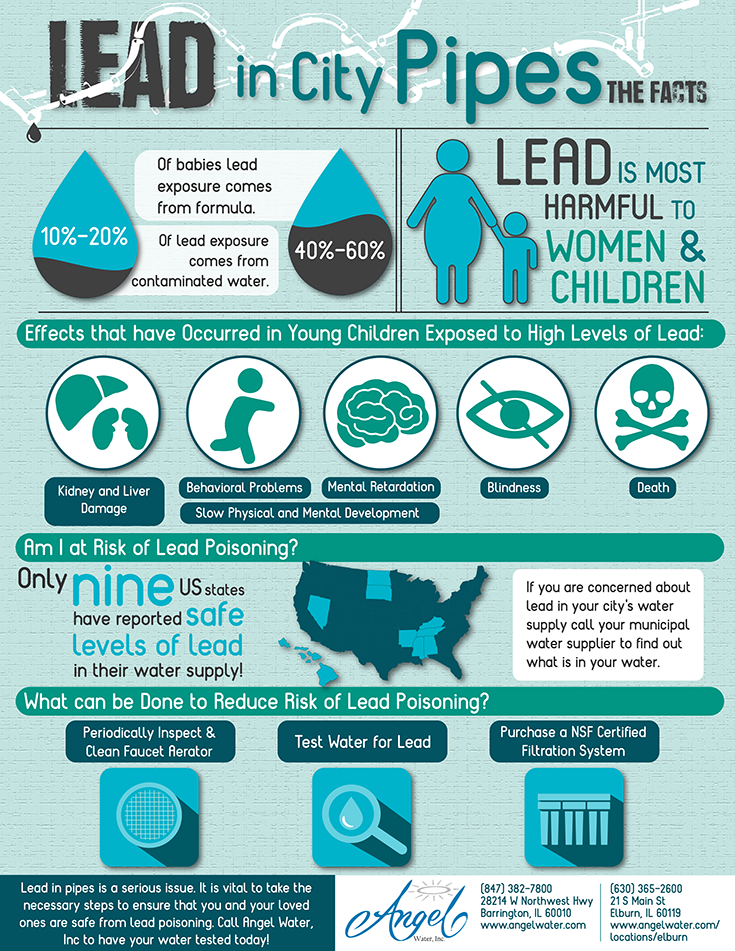 Lead was also once used in paint and gasoline and is still used in batteries, solder, pipes, pottery, roofing materials and some cosmetics.
Lead was also once used in paint and gasoline and is still used in batteries, solder, pipes, pottery, roofing materials and some cosmetics.
Lead in paint
Lead-based paints for homes, children's toys and household furniture have been banned in the United States since 1978. But lead-based paint is still on walls and woodwork in many older homes and apartments. Most lead poisoning in children results from eating chips of deteriorating lead-based paint.
Water pipes and imported canned goods
Lead pipes, brass plumbing fixtures and copper pipes soldered with lead can release lead particles into tap water. Lead solder in food cans, banned in the United States, is still used in some countries.
Other sources of lead exposure
Lead sometimes can also be found in:
- Soil. Lead particles from leaded gasoline or paint settle on soil and can last years. Lead-contaminated soil is still a major problem around highways and in some urban settings.
 Some soil close to walls of older houses contains lead.
Some soil close to walls of older houses contains lead. - Household dust. Household dust can contain lead from lead paint chips or from contaminated soil brought in from outside.
- Pottery. Glazes found on some ceramics, china and porcelain can contain lead that can leach into food served or stored in the pottery.
- Toys. Lead is sometimes found in toys and other products produced abroad.
- Cosmetics. Tiro, an eye cosmetic from Nigeria, has been linked to lead poisoning. Kohl is another eye makeup that may contain lead.
- Herbal or folk remedies. Lead poisoning has been linked to greta and azarcon, traditional Hispanic medicines, as well as some from India, China and other countries.
- Mexican candy. Tamarind, an ingredient used in some candies made in Mexico, might contain lead.
- Lead bullets. Time spent at firing ranges can lead to exposure.

- Occupations. People are exposed to lead and can bring it home on their clothes when they work in auto repair, mining, pipe fitting, battery manufacturing, painting, construction and certain other fields.
Risk factors
Factors that may increase your risk of lead poisoning include:
- Age. Infants and young children are more likely to be exposed to lead than are older children. They might chew paint that flakes off walls and woodwork, and their hands can be contaminated with lead dust. Young children also absorb lead more easily, and it's more harmful for them than it is for adults and older children.
- Living in an older home. Although the use of lead-based paints has been banned since the 1970s, older homes and buildings often retain remnants of this paint. People renovating an older home are at even higher risk.
- Certain hobbies. Making stained glass and some jewelry requires the use of lead solder.
 Refinishing old furniture might put you in contact with layers of lead paint.
Refinishing old furniture might put you in contact with layers of lead paint. - Living in developing countries. Developing countries often have less strict rules regarding exposure to lead than do developed countries. American families who adopt a child from another country might want to have the child's blood tested for lead poisoning. Immigrant and refugee children also should be tested.
Lead can harm an unborn child. If you're pregnant or planning a pregnancy, be especially careful to avoid exposure to lead.
Complications
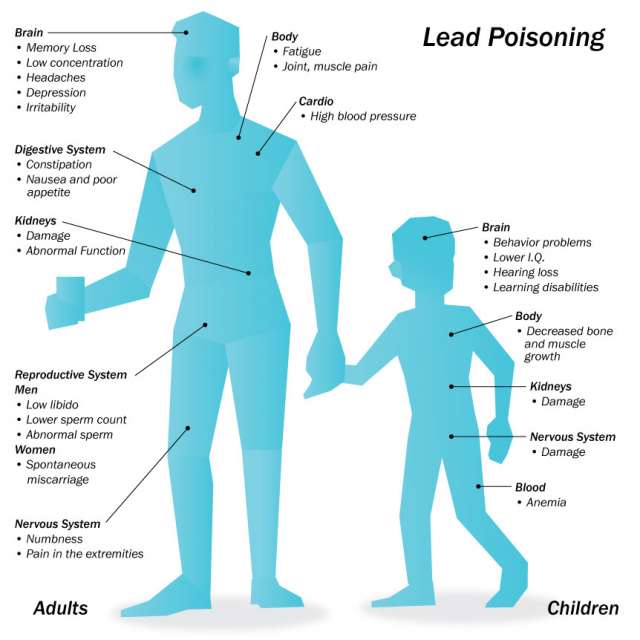
Exposure to even low levels of lead can cause damage over time, especially in children. The greatest risk is to brain development, where irreversible damage can occur. Higher levels can damage the kidneys and nervous system in both children and adults. Very high lead levels may cause seizures, unconsciousness and death.
Prevention
Simple measures can help protect you and your family from lead poisoning:
- Wash hands and toys.
 To help reduce hand-to-mouth transfer of contaminated dust or soil, wash your children's hands after outdoor play, before eating and at bedtime. Wash their toys regularly.
To help reduce hand-to-mouth transfer of contaminated dust or soil, wash your children's hands after outdoor play, before eating and at bedtime. Wash their toys regularly. - Clean dusty surfaces. Clean your floors with a wet mop and wipe furniture, windowsills and other dusty surfaces with a damp cloth.
- Remove shoes before entering the house. This will help keep lead-based soil outside.
- Run cold water. If you have older plumbing containing lead pipes or fittings, run your cold water for at least a minute before using. Don't use hot tap water to make baby formula or for cooking.
- Prevent children from playing on soil. Provide them with a sandbox that's covered when not in use. Plant grass or cover bare soil with mulch.
- Eat a healthy diet. Regular meals and good nutrition might help lower lead absorption. Children especially need enough calcium, vitamin C and iron in their diets to help keep lead from being absorbed.

- Keep your home well maintained. If your home has lead-based paint, check regularly for peeling paint and fix problems promptly. Try not to sand, which generates dust particles that contain lead.
By Mayo Clinic Staff
Lead Poisoning (for Parents) - Nemours KidsHealth
What Is Lead Poisoning?
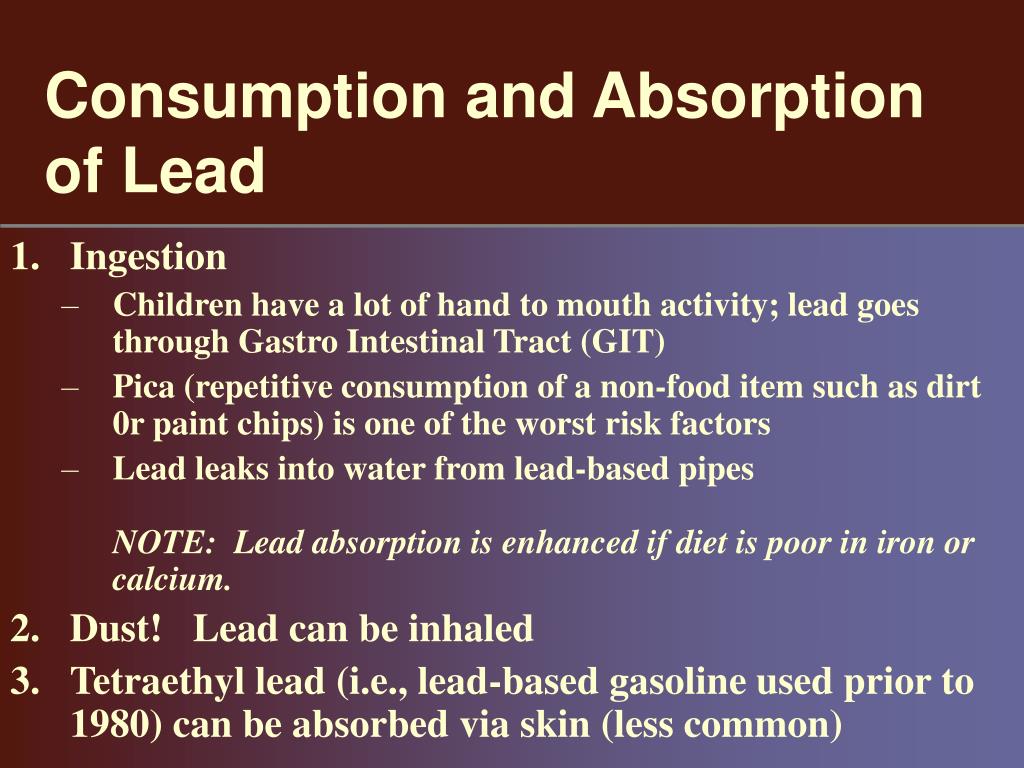
Lead poisoning happens when too much lead gets into the body. Lead can enter through the skin, or when a person breathes it in or eats or drinks something contaminated by lead. Lead in the body can hurt the brain, kidneys, and other organs.
Who Is at Risk for Lead Poisoning?
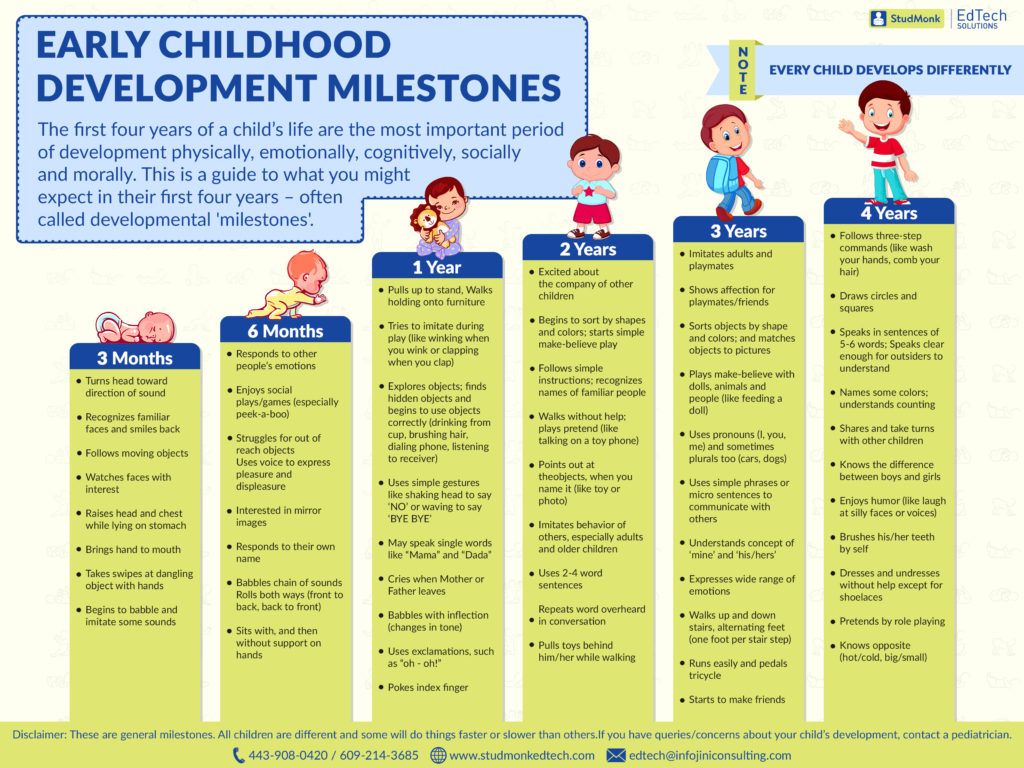
Lead is toxic to everyone, but children younger than 6 years are at greatest risk for problems from it. Their bodies absorb lead more easily than those of older kids and adults. Children 9 months to 2 years are more likely to have higher lead levels because they crawl around and put their hands and other things in their mouth.
Kids are especially at risk if they:
- live in homes built before 1978
- live in low-income households
- come from a foreign country that doesn’t regulate the use of lead
- have pica (eat things like dirt and paint chips)
Lead can pass from a mother to her unborn baby. If you are pregnant and think you have been exposed to lead or were exposed in the past, talk to your doctor about getting a blood test to check lead levels.
If you are pregnant and think you have been exposed to lead or were exposed in the past, talk to your doctor about getting a blood test to check lead levels.
How Do Children Get Lead Poisoning?
The most common way that kids get lead poisoning is from lead-based paint in older homes. Lead paint was banned in the United states in the late 1970s. Gasoline also contained lead, which was released into the air in car exhaust. Kids are exposed to lead from chipping paint; house dust; and contaminated soil around older homes, streets, airports, and industrial areas.
Kids also can come into contact with lead through:
- water that flows through old lead pipes or lead solder
- food stored in bowls glazed or painted with lead
- some old or imported toys, jewelry, pottery, and cosmetics. Lead has also been found in some imported candies and herbs.
- some jobs (like welding, auto repair, and construction) or hobbies (like stained glass, home remodeling, lead soldering)
- some traditional medicines, such as greta and azarcon (used to treat an upset stomach)
What Are the Signs & Symptoms of Lead Poisoning?
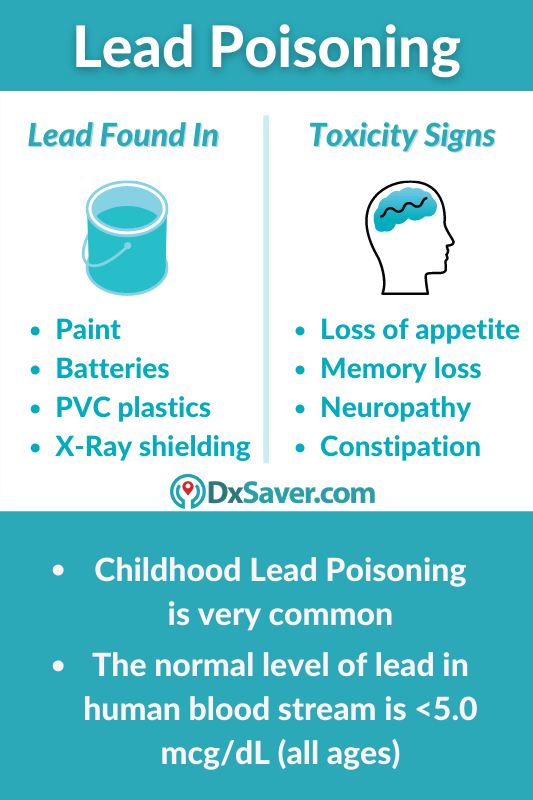
Many children with lead poisoning have no symptoms.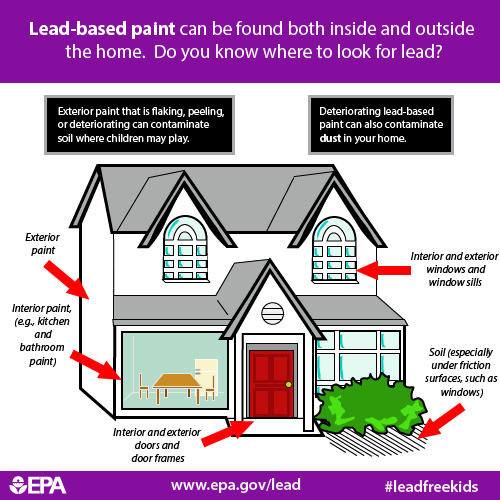 But even low-level lead exposure can lead to learning and behavior problems, like trouble paying attention. Symptoms of lead poisoning include:
But even low-level lead exposure can lead to learning and behavior problems, like trouble paying attention. Symptoms of lead poisoning include:
- loss of appetite
- feeling tired or irritable
- poor growth
- nausea and vomiting
- constipation
- stomach pain
- joint pain and muscle weakness
- headaches
Rarely, very high lead levels can cause confusion, seizures, coma, and death.
How Is Lead Poisoning Diagnosed?
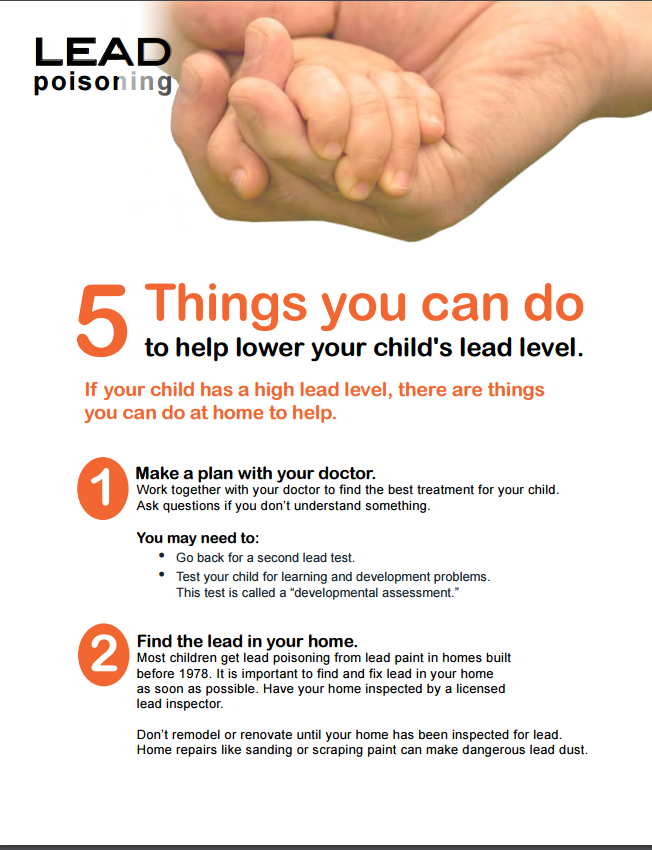
A simple blood test can diagnose lead poisoning. Doctors recommend checking kids for lead at 1 and 2 years old, when they’re most at risk for high lead levels.
Lead testing is also recommended for kids who live in an older home or whose parent has a hobby or job that involves being around lead. Any child who might have been exposed to lead should get tested.
How Is Lead Poisoning Treated?
The most important part of treatment is preventing more exposure to lead. The doctor will ask about the home to try to identify possible sources of lead. If a child has lead poisoning, all siblings should be tested.
The doctor will ask about the home to try to identify possible sources of lead. If a child has lead poisoning, all siblings should be tested.
Calcium, iron, and vitamin C are important parts of a healthy diet and also help decrease how much lead the body absorbs. The doctor may recommend a multivitamin with iron for a child who doesn’t get enough of these important nutrients in their diet.
Kids with high lead levels and symptoms of lead poisoning may need care in a hospital to get a medicine called a chelator (KEE-lay-ter). The chelator helps remove the lead from the body.
The effects of lead on development may not show up for years. Doctors will closely follow the development of children with lead exposure at all regular checkups.
How Can We Prevent Lead Poisoning?
Because there is no safe level for lead, try to protect kids from it. To help prevent lead poisoning:
- Ask your doctor about having your kids tested for lead exposure.
- Get your home checked for lead if it was built before 1978.

- Get your water tested. Call your local water department to find a laboratory that will test your water for lead.
- Regularly clean floors, windowsills, and dusty surfaces clean with a wet cloth or mop.
- Wash your kids' hands and toys often.
- Remove or wipe shoes before coming into the house.
- Keep kids away from soil around old homes and busy roads.
- Fix areas with peeling or chipped paint, such as windows and porches.
- Follow safe practices when removing lead-based paint hazards. Find a lead-safe certified contractor for home renovations.
- Serve a variety of healthy foods, such as dairy products, lean meat and beans, and fruit and vegetables.
Reviewed by: Mary L. Gavin, MD
Date reviewed: July 2021
Lead poisoning | Symptoms, complications, diagnosis and treatment
Lead poisoning occurs when lead accumulates in the body, often over several months or years. Even small amounts of lead can cause serious health problems. Children under the age of 6 are particularly vulnerable to lead poisoning, which can seriously affect mental and physical development. At very high levels, lead poisoning can be fatal.
Even small amounts of lead can cause serious health problems. Children under the age of 6 are particularly vulnerable to lead poisoning, which can seriously affect mental and physical development. At very high levels, lead poisoning can be fatal.
Paint and lead-contaminated dust in older buildings are the most common sources of lead poisoning in children. Other sources include polluted air, water and soil. Adults who work with batteries, do home repairs, or work in auto repair shops can also be exposed to lead.
There is treatment for lead poisoning, but taking some simple precautions can help protect you and your family from lead exposure before harm occurs.
Symptoms
Initially, lead poisoning can be difficult to detect - even people who appear healthy may have high levels of lead in their blood. Signs and symptoms usually do not appear until dangerous amounts of the substance have accumulated in the body.
Signs and symptoms of lead poisoning in children include:
- Developmental delay
- Learning problems
- Irritability
- Loss of appetite
- Weight Loss
- Lethargy and fatigue
- Abdominal pain
- Vomiting
- Constipation
- Hearing loss
- Seizures
Symptoms of lead poisoning in adults
Although children are primarily at risk, lead poisoning is also dangerous for adults. Signs and symptoms in adults may include:
Signs and symptoms in adults may include:
- High blood pressure
- Muscle pain
- Difficulties with memory or concentration
- Headache
- Abdominal pain
- Mood disorders
- Reduction in sperm count and abnormal semen
- Miscarriage, stillbirth or premature birth in pregnant women
Causes
Lead is a metal that occurs naturally in the earth's crust, but human activities - mining, burning fossil fuels and manufacturing - have caused it to become more widespread. Lead was also once used in paint and gasoline, and is still used in batteries, solder, pipes, ceramics, roofing materials, and some cosmetics.
Lead in paint
Lead-based home paint, children's toys, and home furniture have been banned in the United States since 1978. But lead-based paint is still found on walls and woodwork in many older homes and apartments. Most lead poisoning in children is the result of ingestion of deteriorating lead-based paint chips.
Most lead poisoning in children is the result of ingestion of deteriorating lead-based paint chips.
Lead can sometimes also be found in:
- Soil. Lead particles from leaded gasoline or paint are deposited on the soil and can last for years. Lead-contaminated soil continues to be a major problem on highways and in some urban environments. Some soils near the walls of old houses contain lead.
- Household dust. Household dust may contain lead from lead paint chips or contaminated soil from outside.
- Ceramic. Glazes found on some pottery, china may contain lead, which can leach into food served or stored in the pottery.
- Toys. Lead is sometimes found in toys and other products made abroad.
- Cosmetics. Tiro, an eye cosmetic from Nigeria, has been linked to lead poisoning.
- Herbal or folk remedies.
 Lead poisoning is associated with grita and azarkon, traditional Latin American medicines, as well as some from India, China and other countries.
Lead poisoning is associated with grita and azarkon, traditional Latin American medicines, as well as some from India, China and other countries. - Sweets. Tamarind, an ingredient used in some sweets, may contain lead.
- Professions . People are exposed to lead and can bring it home on their clothes when they work in auto repair, mining, pipe fittings, battery manufacturing, painting, construction, and some other areas.
Factors that may increase the risk of lead poisoning include:
- Age . Infants and young children are more likely to be exposed to lead than older children. They may chew on paint that has peeled off walls and woodwork, and their hands may become contaminated with lead dust. Young children also absorb lead more easily and are more harmful than adults and older children.
- Life in an old house. Although the use of lead-based paint has been banned since the 1970s, old houses and buildings often retain traces of this paint.
 People renovating an old home are at even greater risk.
People renovating an old home are at even greater risk. - Some hobbies. Stained glass and some decorations require the use of lead solder. Refinishing old furniture can result in contact with layers of lead paint.
- Life in developing countries. Developing countries often have less stringent regulations regarding lead exposure than developed countries. American families who are adopting a child from another country may want to have the child's blood tested for lead poisoning. Immigrant and refugee children should also be screened.
Lead in whole blood
A heavy toxic metal whose elevated levels in the blood reveal acute or chronic lead poisoning - saturnism.
Synonyms English
Lead (Pb), blood.
Test method
Inductively coupled plasma mass spectrometry.
Units
µg/l (micrograms per litre).
What biomaterial can be used for research?
Venous blood.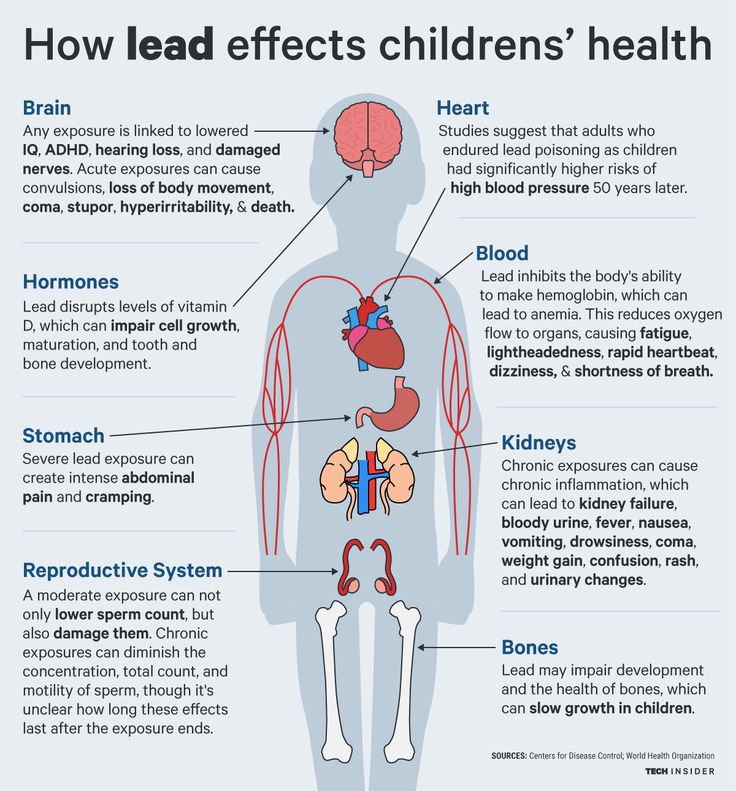
How to properly prepare for an examination?
- Do not eat for 2-3 hours before the examination, you can drink pure non-carbonated water.
- Do not smoke for 30 minutes prior to examination.
General information about the study
Among heavy toxic metals, lead is the most common cause of poisoning. It is widely used in industry and found in small amounts in the environment. For many years it has been used in the manufacture of paints, water pipes, pesticides and cans. Its content is increased in old dilapidated houses and in the territories surrounding many industrial enterprises.
Lead enters the body through the respiratory system or is absorbed in the gastrointestinal tract. The degree of absorption depends on the particle size and the chemical form of the lead. In the body of an adult, 6-10% of this metal is absorbed from the intestines and a very small amount is retained in the tissues.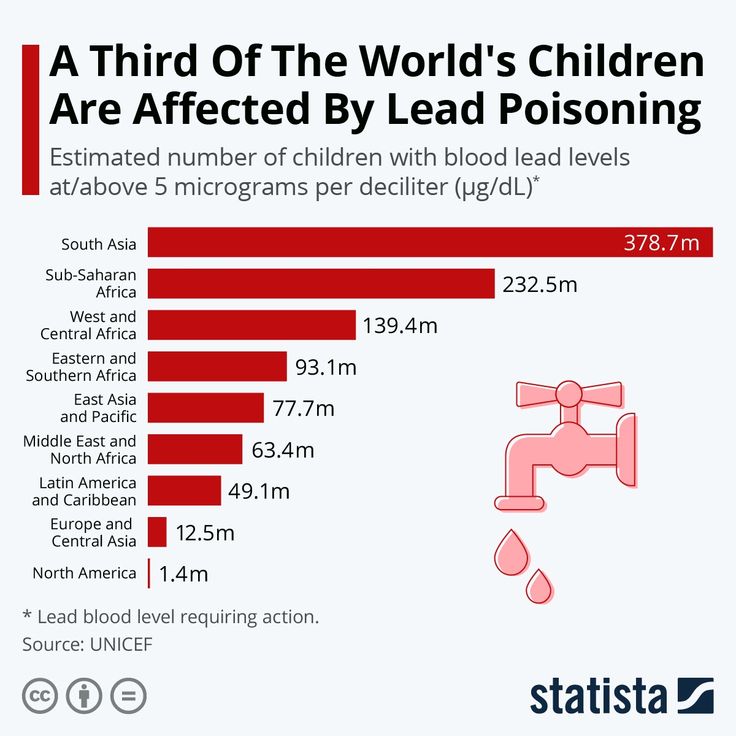 Due to intensive growth and a high degree of absorption in the intestines of a child, 40-50% of the lead ingested is absorbed, of which 20-25% accumulates in the tissues.
Due to intensive growth and a high degree of absorption in the intestines of a child, 40-50% of the lead ingested is absorbed, of which 20-25% accumulates in the tissues.
Even in small amounts, lead has a negative effect on many organs and tissues (there may be no symptoms of intoxication). In humans, it inhibits hemoglobin synthesis and leads to microcytic anemia at normal iron levels. Lead molecules disrupt the conduction of an impulse along the nerve fiber.
The degree of harm and severity of symptoms depends on the dose of the metal and the duration of its exposure, the age of the person, his nutritional status, the presence of concomitant diseases and pathologies. For example, malnourished people with iron deficiency have greatly increased absorption of lead from the gut. Children and pregnant women are most susceptible to the toxic effects of this metal. Lead is able to penetrate through the placenta from the mother into the fetus, which can not only affect the formation of organs and tissues of the child, but also contribute to miscarriage or premature birth.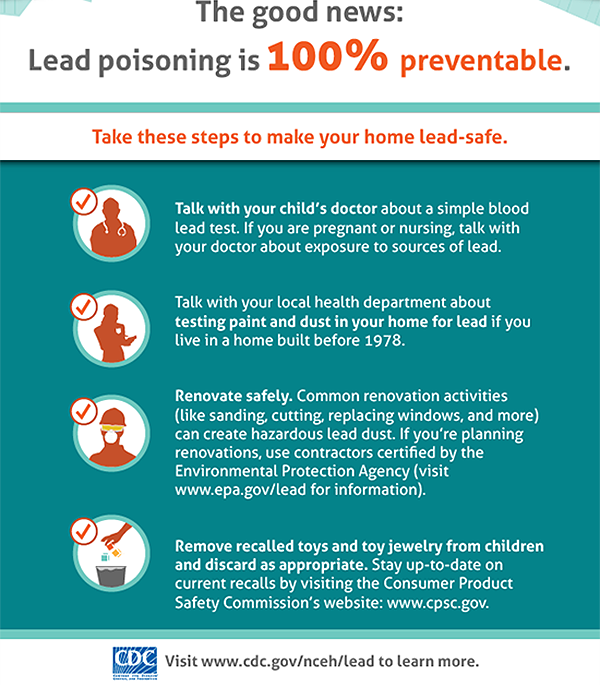
The main "target" of lead is the central nervous system. In children, due to the imperfect development of the blood-brain barrier, it penetrates into the nervous tissue much faster than in adults. Lead intoxication affects the formation of hearing and vision, causes developmental delay, persistent disorders of neuropsychic functions and behavior, and a decrease in mental abilities.
Lead poisoning in adults is most often caused by occupational contact with this metal or by the use of materials containing it in everyday life. The probability of poisoning is high among factory workers, auto repair workers, lead coating manufacturers, miners, welders, builders, steelworkers, foundry workers. Also, intoxication is possible in the manufacture of lead bullets and fishing sinkers, stained-glass windows and ceramics, soldering, drawing with paints containing lead.
Lead levels are elevated in children under 6 years of age due to their tasting habits and high intestinal absorption. In the US, the American Academy of Pediatrics recommends mandatory screening for blood lead in all children, especially in the first and second years of life.
In the US, the American Academy of Pediatrics recommends mandatory screening for blood lead in all children, especially in the first and second years of life.
Lead accumulates mainly in the bones and is excreted from the body very slowly. Acute poisoning occurs rarely and is manifested by encephalopathy, severe abdominal pain, vomiting, impaired stool, convulsions, and in some cases ends in coma and even death. Chronic lead exposure may be asymptomatic for a long time. Its signs may be a pale gray skin color, a dark border around the edges of the gums, weakness, nausea, fatigue, weight loss, anemia, headaches, cramps in the stomach, impaired function of the kidneys, nervous and reproductive systems.
The concentration of lead in the blood correlates with its content in the whole body. It can be used to determine the severity of poisoning and decide on the tactics of treatment and the appointment of antidotes, evaluate the effectiveness of therapy.
What is research used for?
- For the diagnosis of lead poisoning.
- For the differential diagnosis of probable causes of chemical poisoning (while also determining levels of other toxic metals).
- For monitoring excessive human exposure to lead in industrial settings.
- To evaluate the effectiveness of the treatment of saturnism.
When is the test scheduled?
- For symptoms of lead poisoning.
- During preventive examination of children and adults.
- When examining family members of a person working in conditions of high lead content (due to the possibility of lead entering the house with contaminated clothing).
- When examining people working in conditions of lead exposure.
- During and after poisoning therapy.
What do the results mean?
Reference values: 0 - 250 µg/l.
Causes of elevated blood lead levels:
- Acute or chronic lead poisoning.
Also recommended
- Lead in urine
- Blood mercury
- Mercury in urine
- Arsenic in blood
- Arsenic in urine
- Antimony in blood
- Antimony in urine
- Serum cadmium
- Cadmium in urine
- Complete blood count (without leukocyte formula and ESR)
Who orders the examination?
Occupational pathologist, neurologist, toxicologist, resuscitator, therapist, pediatrician.