Pain in pelvis when standing up
18 Possible Causes of Pelvic Pain in Women
If you have pain below your belly button and above your legs, it counts as pelvic pain. It can be caused by a lot of things. It may be a harmless sign that you’re fertile, a digestive disorder, or a red flag that you need to go to the hospital.
If you have a sharp pain in the lower right part of your belly, are vomiting, and have a fever, it could be appendicitis. If you have these symptoms, go to the ER. An infected appendix may need surgery. If it bursts, it can spread the infection inside your body. This can cause serious complications.
Do you have belly pain, cramps, bloating, and diarrhea or constipation that keeps coming back? Talk to your doctor to figure out the problem. It could be IBS, sometimes called spastic colon. Doctors aren’t sure what causes it. Diet changes, stress management, and medications may help.
Ever feel a painful twinge between periods? You may be feeling your body ovulate. When you do, the ovary releases an egg along with some fluid and blood. It can cause irritation. This feeling is called mittelschmerz -- German for "middle" and "pain." That’s because it happens midway through your monthly cycle. The pain may switch sides from month to month. It isn't harmful and usually goes away in a few hours.
You can usually feel these cramps in your lower belly or back. They typically last 1 to 3 days. Why the pain? Every month, your uterus builds up a lining of tissue. That’s where an embryo can implant and grow. If you don't get pregnant, the lining breaks down and is shed during your period. When the uterus tightens to push it out, you get a cramp. Try a heating pad and over-the-counter pain relievers to ease pain. Exercise and de-stressing can help, too. You can also talk to your doctor about PMS pain. Certain birth control pills or antidepressants may help.
This happens when an embryo implants somewhere outside of the uterus and begins to grow. This usually happens in the fallopian tubes. Sharp pelvic pain or cramps (particularly on one side), vaginal bleeding, nausea, and dizziness are symptoms. Get medical help right away. This is a life-threatening emergency.
Get medical help right away. This is a life-threatening emergency.
Pelvic pain is a warning sign of some STDs. Two of the most common are chlamydia and gonorrhea (shown here through a microscope). You often get both at the same time. They don't always cause symptoms. But when they do, you may have pain when you pee, bleeding between periods, and abnormal vaginal discharge. See your doctor. It’s also important to get partners checked and treated, too, so you don’t pass the infection back and forth.
This is a complication of sexually transmitted diseases. It's the No. 1 preventable cause of infertility in women. It can cause permanent damage to the uterus, ovaries, and fallopian tubes. Belly pain, fever, abnormal vaginal discharge, and pain during sex or urination can be symptoms. Get it treated right away to avoid damage. It is treated with antibiotics. In severe cases, you may need to be hospitalized. Get your partner treated, too.
Ovaries release eggs when you ovulate. Sometimes a follicle doesn't open to release the egg. Or it recloses after it does and swells with fluid. This causes an ovarian cyst. They’re usually harmless and go away on their own. But they may cause pelvic pain, pressure, swelling, and bloating. And if a cyst bursts or twists, it can cause sudden, severe pain, sending you to the emergency room. Doctors can spot them during a pelvic exam or ultrasound.
Sometimes a follicle doesn't open to release the egg. Or it recloses after it does and swells with fluid. This causes an ovarian cyst. They’re usually harmless and go away on their own. But they may cause pelvic pain, pressure, swelling, and bloating. And if a cyst bursts or twists, it can cause sudden, severe pain, sending you to the emergency room. Doctors can spot them during a pelvic exam or ultrasound.
These grow on or in the wall of the uterus. While they’re sometimes called fibroid tumors, they are not cancerous. Fibroids are common in women in their 30s and 40s. They usually don’t cause problems. But some women may have pressure in the belly, low back pain, heavy periods, painful sex, or trouble getting pregnant. Talk with your doctor if you need treatments to shrink or remove them.
In some women, there is tissue growing outside the uterus that is similar to tissue that lines the uterus. It can happen on the ovaries, fallopian tubes, bladder, intestines, and other parts of the body.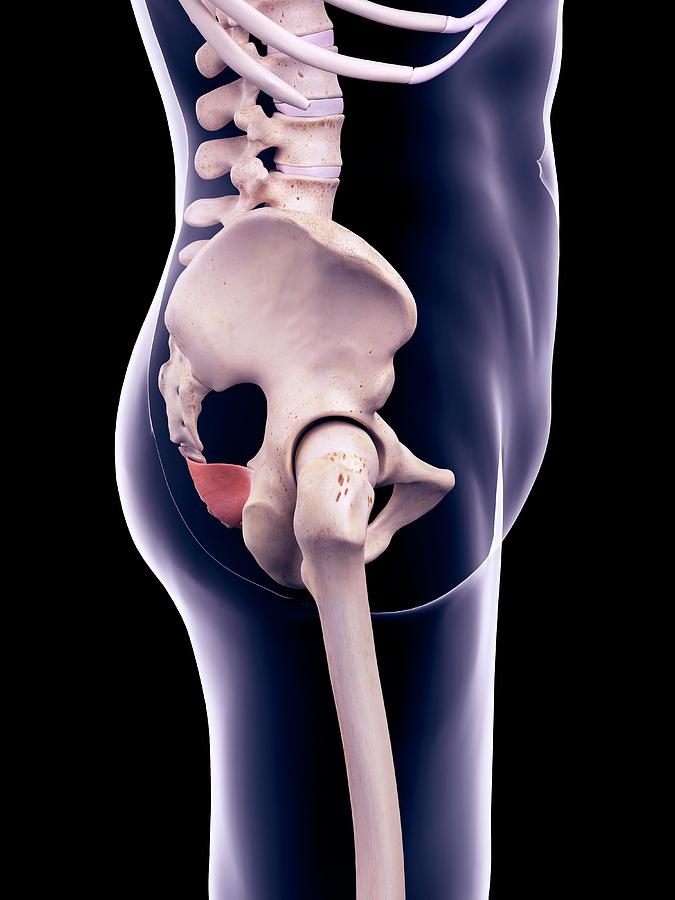 When it's time for your period, these clumps of tissue break down. But the tissue has no way to leave the body. While this is rarely dangerous, it can cause pain and form scar tissue that may make it tough to get pregnant. There are several treatment options. Pain medications, birth control pills, hormones to stop periods, surgery with small incisions, and even a hysterectomy (taking out your uterus) are options.
When it's time for your period, these clumps of tissue break down. But the tissue has no way to leave the body. While this is rarely dangerous, it can cause pain and form scar tissue that may make it tough to get pregnant. There are several treatment options. Pain medications, birth control pills, hormones to stop periods, surgery with small incisions, and even a hysterectomy (taking out your uterus) are options.
Do you have to pee often, or does it hurt when you do? Or do you feel like your bladder is full? It could be a UTI. This happens when germs get into your urinary tract. Treating it quickly can keep it from it getting serious. But if it spreads to the kidneys, it can cause serious damage. Signs of a kidney infection include fever, nausea, vomiting, and pain in one side of the lower back.
These are globs of salt and minerals that your body tries to get rid of in urine. They can be as tiny as a grain of sand or as large as a golf ball. And boy can they hurt! Your urine may turn pink or red from blood.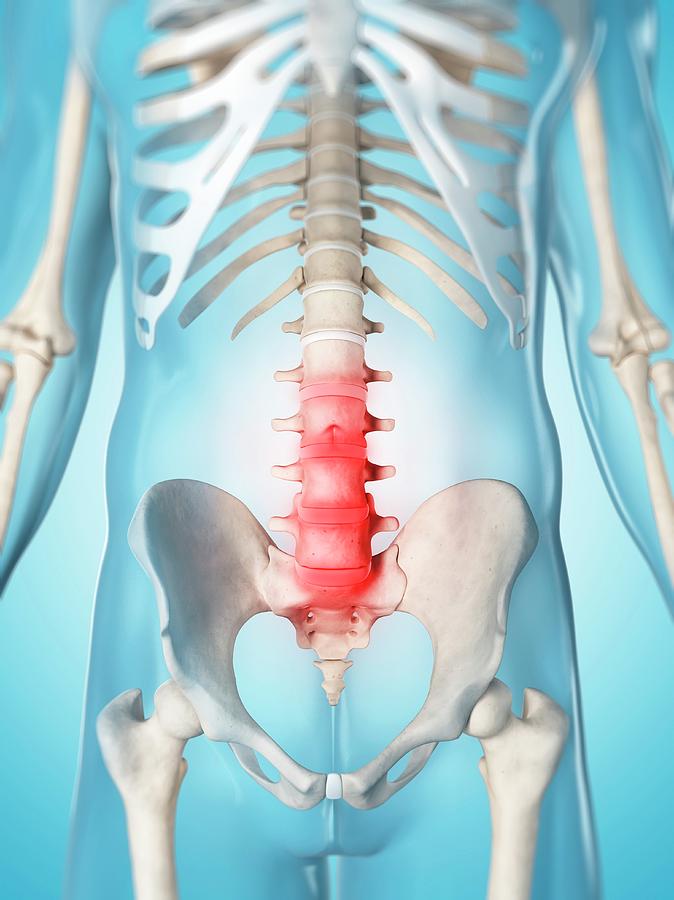 See your doctor if you think you have a kidney stone. Most will pass out of your system on their own, but some need treatment. Even if they can pass on their own, your doctor can help with pain medication and will tell you to drink lots of water.
See your doctor if you think you have a kidney stone. Most will pass out of your system on their own, but some need treatment. Even if they can pass on their own, your doctor can help with pain medication and will tell you to drink lots of water.
This condition causes ongoing pain and is related to inflammation of the bladder (illustrated here). It’s most common in women in their 30s and 40s. Doctors aren’t sure why it happens. People with severe IC may need to pee several times an hour. You might also feel pressure above the pubic area, pain when you urinate, and pain during sex. Although this can be a long-term condition, there are ways to ease the symptoms and avoid flares.
As you get older, this may happen. Your bladder or uterus drops into a lower position. It usually isn't a serious health problem, but it can be uncomfortable. You may feel pressure against the vaginal wall, or your lower belly may feel full. It may also give you an uncomfortable feeling in the groin or lower back and make sex hurt.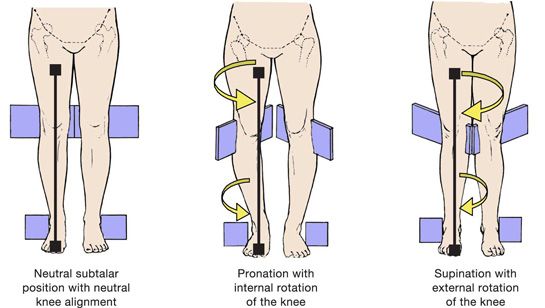 Special exercises like Kegel’s or surgery may help.
Special exercises like Kegel’s or surgery may help.
We’ve all seen varicose veins in legs. (This is a picture of one in the upper thigh.) They can sometimes happen in the pelvis, too. When blood backs up in veins, they become swollen and painful. This is known as pelvic congestion syndrome. This is a condition that's difficult to diagnose and treat. It tends to hurt worse when you sit or stand. Lying down may feel better. But because the best treatment is still unclear, you need to work with your doctor to learn what the options are and to find what works well for you.
If you've had surgery or an infection, you could have ongoing pain from this. Adhesions are a type of scar tissue inside your body. They form between organs or structures that aren’t meant to be connected. Adhesions in your belly can cause pain and other problems, depending on where they are. In some cases, you may need a procedure or surgery to get rid of them.
Does it hurt when you ride a bike or have sex? If it burns, stings, or throbs around the opening of your vagina, it could be this. The feelings can be ongoing or come and go. Before you’re diagnosed with this, your doctor will rule out other causes. This isn’t caused by an infection. Treatment options range from medication to physical therapy.
The feelings can be ongoing or come and go. Before you’re diagnosed with this, your doctor will rule out other causes. This isn’t caused by an infection. Treatment options range from medication to physical therapy.
This can be caused by many things. Most are treatable. It could be a vaginal infection, or you just may need more lubrication. The medical name is dyspareunia. Sometimes the pain gets better after sexual therapy. This type of talk therapy can focus on inner conflicts about sex or past abuse.
If you have pain that lasts at least 6 months, it’s considered chronic. It may be so bad it messes with your sleep, career, or relationships. See your doctor. Most of the conditions we've covered get better with treatment. Sometimes, even after a lot of testing, the cause of pelvic pain remains a mystery. But your doctor can still help you find ways to feel better.
Causes of Chronic Pelvic Pain and Symptoms of Each
Written by WebMD Editorial Contributors
Many conditions can cause chronic pelvic pain.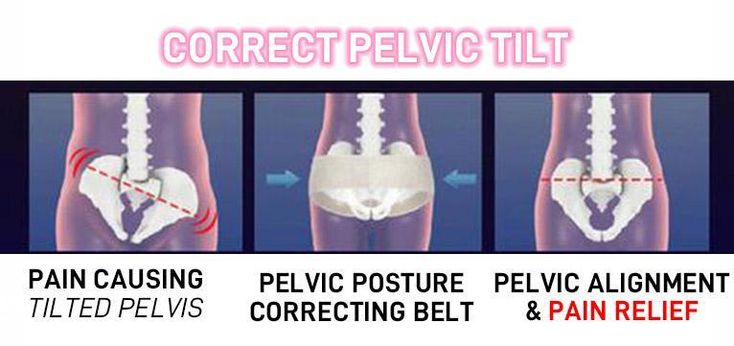 All can have similar symptoms, and that often makes it hard to figure out the source of the pain. The main symptom is pain that lasts for more than 6 months, but there are usually other symptoms as well. Understanding your symptoms can help you and your doctor begin to pinpoint the cause or causes of your chronic pelvic pain. Here are some of the causes and the related symptoms:
All can have similar symptoms, and that often makes it hard to figure out the source of the pain. The main symptom is pain that lasts for more than 6 months, but there are usually other symptoms as well. Understanding your symptoms can help you and your doctor begin to pinpoint the cause or causes of your chronic pelvic pain. Here are some of the causes and the related symptoms:
Endometriosis
In endometriosis, cells that normally line the inside of the uterus (the endometrium) grow outside on organs such as the ovaries, bladder, or rectum.
Symptoms you may have:
- Pelvic pain or cramps before or during your period
- Pain during or after sex
- Pain when you ovulate
- Painful bowel movements
- Rectal bleeding during your period
- Pain when you urinate
- Lower back pain
- Infertility
- Spotting between periods
- Bloating in your abdomen
Adenomyosis
This condition is similar to endometriosis. Cells that normally line your uterus (the endometrium) invade the muscle tissue of the uterus wall (the myometrium). Many women with adenomyosis don't have any symptoms.
Cells that normally line your uterus (the endometrium) invade the muscle tissue of the uterus wall (the myometrium). Many women with adenomyosis don't have any symptoms.
Symptoms you may have:
- Pain during your period
- Feeling of pressure on your bladder or rectum
- Heavy periods
- Periods that last longer than usual
- Spotting between periods
Interstitial Cystitis
Women with interstitial cystitis have an inflamed bladder. The inflammation is not caused by an infection. This condition tends to affect women in their 30s and 40s.
Symptoms you may have:
- You need to urinate very often
- Often feeling an urgent need to urinate
- Discomfort when you urinate
- Pain during sex
Urinary Tract Infection
Bacteria are usually the cause of urinary tract infections. Infections can involve any part of the urinary tract, including the kidneys, bladder, and urethra. Urinary tract infections are much more common in women than in men.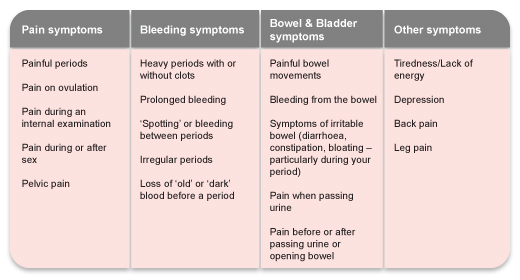
Symptoms you may have:
- Feeling pressure in your lower pelvis
- Pain or a burning sensation when you urinate
- Needing to urinate often
- Often feeling an urgent need to urinate
- Needing to get up at night to urinate
- Cloudy urine
- Blood in urine
- Urine has strong or bad smell
- Only a trickle of urine comes out
- Lower back pain
Pelvic Inflammatory Disease
This is an infection of the uterus, fallopian tubes, or ovaries that causes them to become inflamed and infected. Most often, it is a sexually transmitted bacterial infection, like gonorrhea or chlamydia. These bacteria enter the uterus through the vagina and leave the fallopian tubes to infect surrounding organs like the ovaries. Scars left by the infection may cause chronic pelvic pain, but more commonly, the pain is acute.
Symptoms you may have:
- Vaginal discharge having an unusual color, texture, or odor
- Abdominal or pelvic pain in a specific area or more widespread
- Pain during sex
- Irregular or missed periods
- Menstrual cramps that are worse than usual
- Frequent need to urinate
- Pain when you urinate
- Pain when you ovulate
- It hurts when you press on certain areas of your pelvis
- Lower back pain
- Fatigue
- Fever
- Nausea
Pelvic Congestion Syndrome
Pelvic congestion is just like the varicose veins that some women have in their legs, but it affects the veins of the pelvis.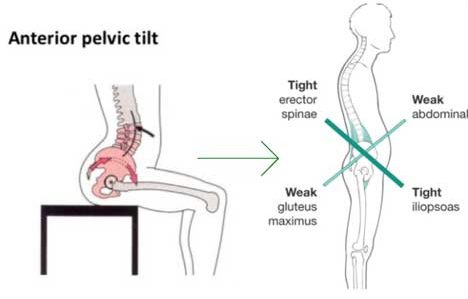 Blood backs up in the veins, making them become enlarged and engorged. Pelvic congestion causes chronic pelvic pain in some women.
Blood backs up in the veins, making them become enlarged and engorged. Pelvic congestion causes chronic pelvic pain in some women.
Symptoms you may have:
- Pain starts 7-10 days before your period
- Pelvic pain is worse when you sit or stand
- Lying down relieves pelvic pain
- Lower back pain
- Aches in your legs
- Pain during sex
Irritable Bowel Syndrome
Chronic pelvic pain sometimes isn't only due to problems with reproductive organs or the urinary tract; other organs in the pelvic area, if "diseased," can present as pelvic pain. Irritable bowel syndrome, an intestinal condition that often causes pain, may be the cause.
Symptoms you may have:
- Diarrhea
- Constipation
- Incontinence
- Flatulence
- Bloating
- Pain relieved by a bowel movement
Uterine Fibroids
Fibroids are noncancerous tumors that grow in, and on, the wall of the uterus. Not all women who have them notice symptoms, but for some, fibroids can be painful.
Symptoms you may have:
- Heavy periods
- Feeling pressure or fullness in your abdomen
- Need to urinate frequently
- Pain or cramps during your period
- Constipation
- Hemorrhoids
Levator Syndrome
Sometimes, spasms of a pelvic muscle called the "levator ani" cause pelvic pain.
Symptoms you may have:
- Pain is related to sitting.
- Pain doesn't seem to be related to bowel movements.
- You wake up at night in pain.
- Pain usually lasts less than 20 minutes at a time.
Pelvic Support Problems
Sometimes women have pelvic pain when the muscles and ligaments that hold organs in place weaken. This causes organs like the uterus, the bladder, or the rectum to move from their normal places and herniate into the vagina. The vagina may also change shape. Pregnancy and giving birth may cause these kinds of problems.
Symptoms you may have:
- Leaking urine
- Feeling like something is falling out of your vagina
- Difficulty with bowel movements
- Lower back pain
- Pain during sex
- Pelvic organs bulge into the vagina, or even stick out the vaginal opening, in severe cases
Vulvodynia
Vulvodynia is pain that affects the vulva for no apparent reason.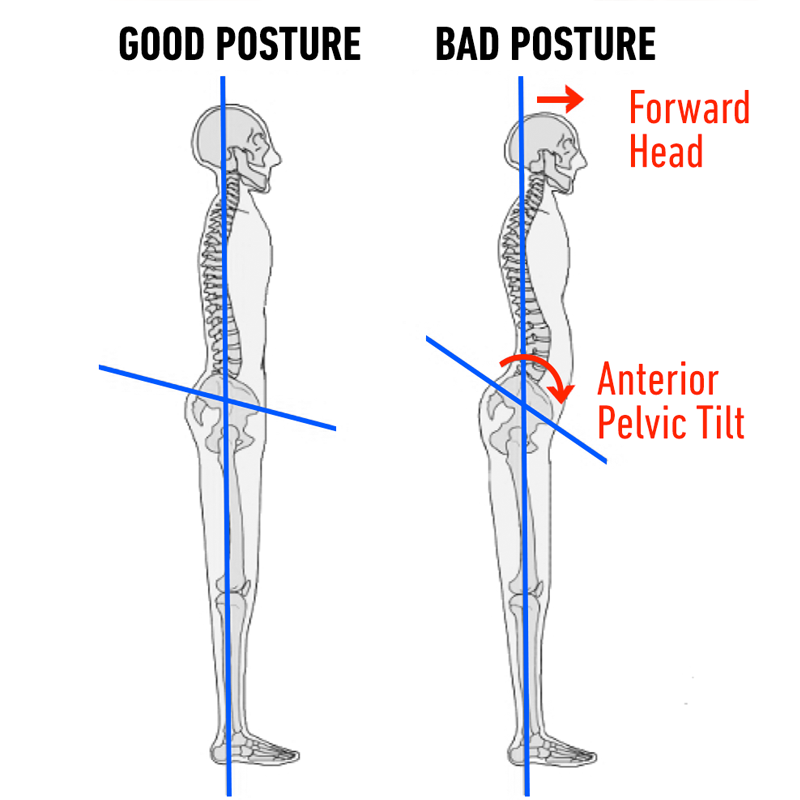 The pain of vulvodynia may be constant or it may come and go.
The pain of vulvodynia may be constant or it may come and go.
Symptoms you may have:
- Burning or stinging sensations in the vulva
- Pain when something presses on the vulva, like during sex or when you straddle a seat
- Pain in your inner thighs
Psychological Causes
For some women, the root of pelvic pain is psychological. That's not to say that the pain isn't real. There just isn't an identifiable physical cause. Some people have emotional problems that only show up as physical symptoms. Women who have suffered sexual abuse or assault often have chronic pelvic pain afterward.
Symptoms you may have:
- Depression
- Anxiety
- Substance abuse
- Stress
Other Causes
Less common causes of pelvic pain include:
Ovarian remnant. Sometimes, when you have surgery to remove your ovaries, a small part of an ovary is left behind. If this happens, the leftover piece can get cysts that can be painful.
Cervical cancer. Continuous pelvic pain is a sign of cervical cancer. You could feel it near your appendix if the cancer is advanced. If the discomfort is due to cancer, it'll usually come with other symptoms like:
- Abnormal vaginal bleeding, like bleeding between periods, heavy bleeding during your period, or bleeding after sex
- Vaginal discharge
- Painful sex
- Leg pain
- Unexplained weight loss
Ovarian cancer. Pelvic pain can be one of many signs of ovarian cancer. If yours is, what you feel can be persistent and severe. It might come with:
- Bloating
- Belly pain
- Trouble eating
- Urinary issues like always feeling like you need to pee or having to pee often
Vaginal cancer. One symptom is pelvic pain. Others include:
- Bleeding after sex or menopause
- A lump of mass in your vagina
- Watery discharge
- Frequent, painful peeing
- Constipation
Endometrial cancer. Pain in your pelvis is a sign of late-stage endometrial cancer. You might also have:
Pain in your pelvis is a sign of late-stage endometrial cancer. You might also have:
- Unusual bleeding or discharge in your vagina
- Unexplained weight loss
- Feeling a mass
Radiation treatment. Radiation treatment for cancer can damage healthy cells and tissue. That damage can lead to scar tissue that can bring pain.
Women's Health Guide
- Screening & Tests
- Diet & Exercise
- Rest & Relaxation
- Reproductive Health
- Head to Toe
CAUSES OF PAIN IN THE HIP JOINT
Osteoarthritis of the hip joint. Osteoarthritis is a degenerative disease of the hip joint that is associated with general aging of the body and usually occurs in people over 50 years of age. When the cartilage of the joint wears out, they no longer adequately protect the bones of the joint from direct contact between the bones. Direct bone contact causes pain and inflammation. On an x-ray, a healthy joint has a narrow band between the bones that appears to be empty. This strip is cartilage. In an osteoarthritis-damaged joint, the bones appear side by side on an x-ray, and there is no "blank" band between them.
Direct bone contact causes pain and inflammation. On an x-ray, a healthy joint has a narrow band between the bones that appears to be empty. This strip is cartilage. In an osteoarthritis-damaged joint, the bones appear side by side on an x-ray, and there is no "blank" band between them.
Osteoarthritis can be caused not only by the natural aging process, but also by overloading the joints (at work, during sports or due to being overweight), arthritis and genetic predisposition.
One of the first signs of osteoarthritis is the loss of the ability to rotate the hip joint. Symptoms include pain on movement, stiffness in the hip joint, and lameness. The intensity of the symptoms can vary, sometimes there is a feeling of complete recovery, and at times very pronounced disturbances.
Osteoarthritis does not improve, but it is possible to limit the development of this disease and maximize the quality of life. To do this, you need to take care of your weight, study and regularly do a set of exercises to strengthen the ligaments and muscles of the hip joint under the supervision of a physiotherapist, protect the hip joint from a heavy load, and also take anti-inflammatory and pain medications after consulting a doctor. In some cases, hip arthroplasty is required.
In some cases, hip arthroplasty is required.
Femoroacetabular syndrome - bone processes (osteophytes) on the bones forming the joint. Recoil syndrome, limitation of movement in the joint and pain gradually develop. The cause of the disease may be an injury to the joint. This disease causes osteoarthritis. Sharp (sometimes dull) pain occurs when a person turns and crouches. Osteophytes can be removed surgically, but over time they form again, damaging the joint.
Hip bursitis - inflammation that occurs in the bag of the hip joint (mucous bag). Signs of inflammation: pain in the hip joint from the buttocks or in the sciatic muscle, pain when trying to lie on the inflamed hip joint, when pressing on the hip joint, getting up from a sitting position, going up or down the stairs. Inflammation can be caused by various causes, for example, a bruised hip, overloading the hip joint while running, jumping or standing for a long time, and poor posture.
To pinpoint the cause of the pain, an injection of pain medication into the mucosal sac is used to ensure that when the pain caused by the bursitis is relieved, there is no other pain that needs to be investigated.
Non-steroidal anti-inflammatory drugs, pain relievers, and injections of corticosteroids and growth factor into the hip joint are used to treat inflammation of the hip joint.
They quickly reduce pain and swelling, so they are often given when non-steroidal anti-inflammatory drugs are not working or the person has an intolerance to these drugs. After consultation with an orthopedic traumatologist, physiotherapy is recommended.
Fracture of the bones that make up the hip joint is more common in older people with osteoporosis. Because of the brittle bones characteristic of the disease, a fracture can cause a seemingly unimportant fall or bruise. In young people, the bones of the hip joint break as a result of severe injuries, such as a traffic accident.
A hip fracture is indicated by pain in the hip and groin, especially on movement.
Hip fractures are treated both conservatively and surgically. The surgeon, having assessed the type and extent of the fracture, will decide on the most appropriate method of treatment.
If surgery is necessary, during surgery the broken bone is replaced or the fracture site is fixed with a metal plate or screw to ensure proper healing of the bone.
Hip dysplasia - developmental disorders of the hip joint, under the influence of which the bones of the hip joint form a mutual discrepancy, which gradually damages this joint. Joint instability develops, subluxations or complete dislocations. In their youth, such people have excessive elasticity of the hip joint - without preparation they can sit on the twine and perform other acrobatic exercises. Such abilities indicate problems in the hip joint.
If hip dysplasia is left untreated, osteoarthritis develops. There are several non-surgical solutions that are applied to keep the lifespan of the hip joint as long as possible. However, anti-inflammatory medications, maintaining optimal body weight, physical therapy exercises, or using a cane while walking are temporary solutions, as they cannot eliminate the cause - a malformed hip joint that causes damage to itself. Depending on the pathology of the hip joint, the disease gradually progresses and surgery is necessary. As a final solution, a hip replacement is used - arthroplasty or endoprosthetics.
There are several non-surgical solutions that are applied to keep the lifespan of the hip joint as long as possible. However, anti-inflammatory medications, maintaining optimal body weight, physical therapy exercises, or using a cane while walking are temporary solutions, as they cannot eliminate the cause - a malformed hip joint that causes damage to itself. Depending on the pathology of the hip joint, the disease gradually progresses and surgery is necessary. As a final solution, a hip replacement is used - arthroplasty or endoprosthetics.
Osteonecrosis of the hip occurs when the blood circulation is interrupted in the bone and it does not receive nutrients. As a result, cells and parts of the bone die. The most common factors that can cause osteonecrosis are:
- serious injury resulting in impaired blood supply to the bone,
- prolonged or excessive use of corticosteroids,
- excessive alcohol consumption.
However, sometimes the causes of osteonecrosis are unclear.
Bone necrosis causes pain and restriction in the affected joint. If osteonecrosis is detected in a timely manner and has affected small areas of the bone, pain medication and reduced exercise (including walking) can give good results. With the development of the disease, surgical intervention is required. For the treatment of osteonecrosis, operations of various types and degrees of complexity are used, up to a complete replacement of the hip joint - arthroplasty or arthroplasty.
Hip pain when sitting: causes, treatment
Pain in the hip joint when sitting can signal various pathological conditions and injuries. Therefore, before visiting a doctor, it is necessary to understand their features in order to begin the correct treatment.
Causes of pain
Due to the characteristics of the innervation of the hip joint (hip joint), pain in this area may not give a clear picture of its dislocation. It can be difficult to determine the point at which the discomfort is greatest. Aching pain can come from the lower back, while accumulating in the groin or buttock. There can be many reasons for the development of such a condition.
Aching pain can come from the lower back, while accumulating in the groin or buttock. There can be many reasons for the development of such a condition.
Pain when sitting can be associated with such phenomena as:
- stretching of the muscles of the buttocks or thighs due to awkward movement;
- injuries of the pelvic bones;
- dislocations of joints;
- inflammation in the joint and surrounding tissues;
- degenerative changes in the musculoskeletal system;
- pediatric pathologies of the hip joint;
- infectious diseases;
- sciatic neuralgia, etc.
Determining the true cause of pain can be difficult. To do this, you need to go through a full diagnosis.
Possible diseases
The most common causes of pain in the hip joint, except for banal bruises and dislocations, are such pathological processes as:
- arthritis of various origins;
- tendovaginitis;
- bursitis;
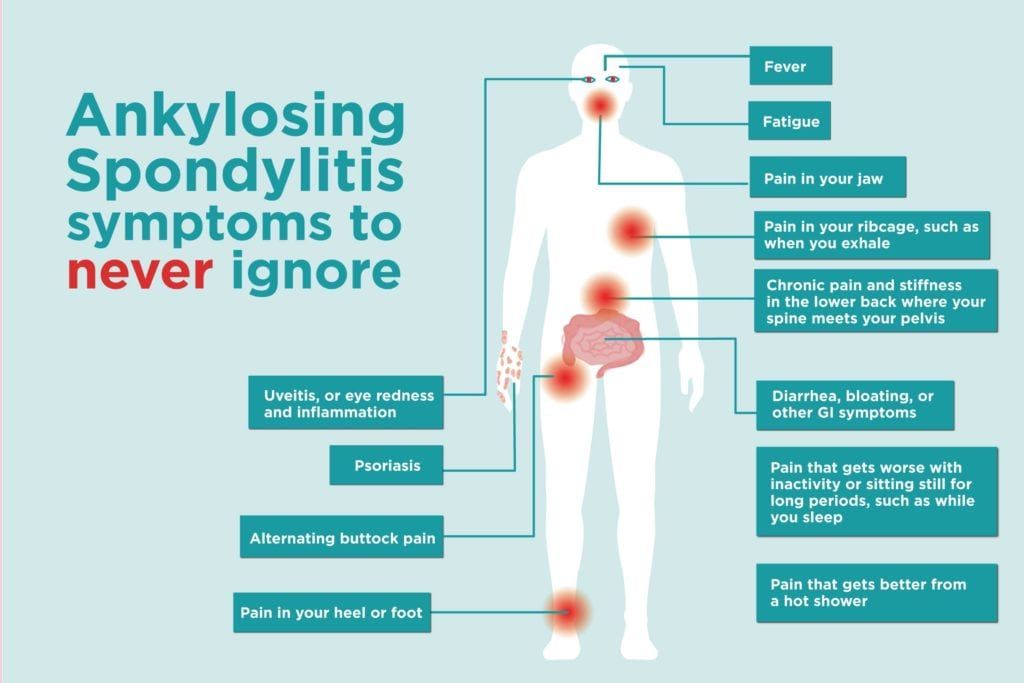
- ankylosing spondylitis;
- osteoarthritis;
- osteochondrosis;
- spondylolisthesis;
- dysplasia;
- epiphyseolysis;
- osteochondropathy;
- neoplasms of bones and soft tissues and other conditions.
Arthritis of the hip joint - there are several varieties of this pathology that occur due to different reasons. This group of diseases is characterized by inflammation of the tissues of the joint, the appearance of discomfort and swelling. Over time, if left untreated, it leads to stiffness.
Tenosynovitis is characterized by inflammatory processes in the tendons of the thigh due to injuries or regular physical exertion. A distinctive feature of this pathology is pain when getting up from a sitting position on a chair, with long walking and squatting.
When bursitis inflammatory changes occur in the bursae - "sacs" with synovial fluid that reduces bone friction. Such pathological processes are associated with prolonged physical exertion, hip injuries and diseases of the lumbosacral spine.
Ankylosing spondylitis often has a sluggish onset with gradual progression leading to complete immobility of the joint. It most often affects young people under the age of 30.
It most often affects young people under the age of 30.
With osteoarthritis (coxarthrosis) , degenerative processes occur in the interarticular cartilage, which lead to subsequent disability. Similar pathologies develop after 40 years. More often they occur due to genetic predisposition, heavy physical exertion, hip injuries and concomitant joint pathologies.
Osteochondrosis and spondylolisthesis — degenerative diseases of the lumbar spine associated with deformation and abrasion of the intervertebral discs. Such pathologies cause irradiating painful discomfort. In this case, a sharp pain can be given to the thigh, buttock or leg when coughing and while driving on rough roads.
Dysplasia is a phenomenon of unstable hip, which without appropriate therapy leads to chronic subluxations and then dislocations. This pathology is more common in girls. If dysplasia is not diagnosed in infancy, then in adolescents it causes pain, instability of the hip region and the subsequent development of arthrosis.
Epiphysiolysis appears during the growth spurt. It occurs more often in obese boys aged 8–15 years. Pain is localized in the pelvic region and can radiate to the groin and knee even at rest. It leads to severe articular pathologies, therefore, it requires immediate treatment.
Osteochondropathy is a whole complex of bone and cartilage diseases. They develop due to a genetic predisposition or a combination of hormonal disorders and infectious diseases. In this case, the appearance of unpleasant sensations in the knee is characteristic, gradually turning into the thigh or, conversely, the pain in the hip joint radiates to the leg. Discomfort occurs at rest and increases with any physical exertion.
Neoplasms of bones and soft tissues , developing in the lumbosacral region, buttocks, thigh and skeletal system of the legs, often lead to pain discomfort in the lumbar area and in the joint between the thigh and pelvis.
Watch this video on YouTube
Recommended treatments
If you experience long-term pain in the hip joint, you should consult with narrow specialists: a neurologist, traumatologist, orthopedist or rheumatologist. Only after the diagnosis and determination of the pathology, the doctor will prescribe the appropriate therapy.
The way to get rid of the pain syndrome directly depends on the cause of its occurrence. General methods in the treatment of such pathologies are:
- repositioning of bones in violation of their integrity;
- adjustment of joints when dislocations are detected;
- prescribing medications;
- use of physiotherapy techniques;
- massage treatments;
- performing a set of exercises of physiotherapy exercises and swimming;
- use of manual therapy techniques;
- folk methods of treatment.
If necessary, surgical treatment of the resulting pathology may be recommended.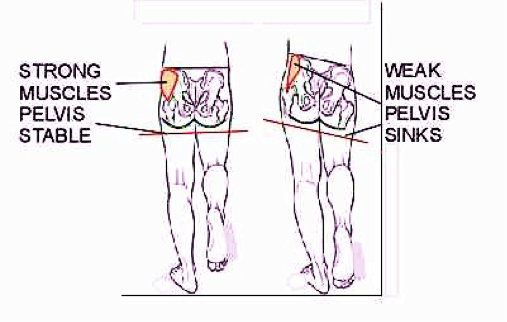
Ways of pain relief
As the main ways to eliminate pain, modern medicine offers:
- anti-inflammatory drugs;
- muscle relaxant preparations;
- diuretics;
- chondroprotective preparations (in complex therapy).
Anti-inflammatory drugs (eg Diclofenac, Ibuprofen, Nimesulide, Movalis) have a pronounced analgesic effect and reduce inflammation in all tissues of the musculoskeletal system, including the hip joint.
There are two types of anti-inflammatory drugs - nonsteroidal and steroidal. Traditionally, in the treatment of HBS diseases, dosage forms belonging to the first group of drugs are used. Steroid medicines are used only in critical situations, when non-steroidal medicines did not bring the expected effect. They are often recommended for intra-articular blockades.
Muscle relaxants help relax the hip muscles and prevent spasms.
Diuretics remove excess fluid from the tissues of the joint, relieving swelling and additional discomfort.