Newborn sore nipples
Sore Nipples | Breastfeeding Challenges
There may be times when breastfeeding is challenging. Never ignore any issues you may have – talk to your health visitor, midwife, GP or breastfeeding specialist as soon as possible, they will be able to help you sort it out quickly.
Here are some common breastfeeding issues, and tips on what to do.
- Colic
- Constipation
- Mastitis
- Milk supply
- Reflux
- Sore nipples
- Thrush
- Tongue-tie
Sore nipples
When you first start breastfeeding, you may have sore or sensitive nipples. This is very common in the first week of breastfeeding, and is usually because your baby is not latching on (positioned or attached) properly. If you do have nipple pain, speak to your midwife, health visitor or breastfeeding specialist as soon as possible – breastfeeding should not be painful!
What causes sore nipples?
The most common cause of nipple pain is when your baby does not latch on properly. It's very important that you correct this as soon as possible – ask your midwife, health visitor or breastfeeding specialist for help, they can show you how your baby needs to be positioned when feeding. Have a look at our step-by-step guide to latching on
Whatever you do – do not stop breastfeeding! Breast milk is created on a supply and demand system, so the less you feed, the less you produce. If you are finding it really painful to breastfeed try expressing your breast milk to keep up the supply.
Breastfeeding Friend from Start for Life
The Breastfeeding Friend, a digital tool from Start for Life, has lots of useful information and expert advice to share with you – and because it's a digital tool, you can access it 24 / 7.
Other possible causes for sore nipples
Tongue tie
When the strip of tissue under your baby's tongue (attaching the tongue to the floor of the mouth) is shorter than normal – this can prevent them from latching on properly.
Thrush
Thrush (or 'candida') is an infection that can occur when your nipples become cracked or damaged. Symptoms are usually severe pain in your nipples after breastfeeding (it's described as burning or shooting pains) lasting up to an hour. Your doctor can prescribe treatment for you and your baby.
Tips for soothing sore nipples
- Some women find rubbing breast milk onto their nipples can be soothing.
- Products like Vaseline or lanolin can help with dry or cracked nipples (although there's little evidence to show what really works well).
- After each feed, let your nipples dry before getting dressed – change your breast pads after every feed.
- Avoid using soap, as this can dry out your skin.
- If possible, only wear cotton, non-underwired bras.
- It's best to avoid using nipple shields and breast shells – these will not improve your baby's attachment to the breast.
- Try not to shorten feeds – doing so will not ease the pain and may reduce your milk supply.
Videos
What can I do about sore nipples??
How do I know if my baby is properly latched on?
6 breastfeeding problems in the first week – solved
Having trouble breastfeeding your newborn? Read our expert tips and watch videos to solve common breastfeeding problems in the first week.
Share this content
Cathy Garbin, child health nurse, midwife and lactation consultant:
For seven years, Cathy was a Research Associate with the renowned Hartmann Human Lactation Research Group, while supporting breastfeeding mothers in their homes and in hospitals. The mum of two still works with families, and also conducts study days for healthcare professionals and speaks at international conferences.
Breastfeeding isn’t always easy and if you’re experiencing difficulties you’re not alone. In fact a US study of more than 500 mums found that 92% reported breastfeeding challenges by day three1. Thankfully, many early breastfeeding difficulties are simple to deal with – here are my solutions to the most common problems mums experience in the first week.
Thankfully, many early breastfeeding difficulties are simple to deal with – here are my solutions to the most common problems mums experience in the first week.
I have sore nipples what should I do?
Problem 1: Breastfeeding hurts!
Pain while breastfeeding is usually down to sore, tender nipples, especially once your milk ‘comes in’ around two to four days after giving birth.2 Your baby will be feeding every couple of hours, which means the problem can worsen quickly, with some mums finding their nipples crack, bleed or become blistered. Ouch!
Solutions3
- Check your baby’s latch. Your baby not latching correctly is the most likely cause of breastfeeding pain. Your newborn should have a large portion of the lower part of the areola (the dark skin around your nipple) in her mouth when she feeds, with your nipple against the roof of her mouth, cupped gently underneath by her tongue.

- See a lactation consultant or breastfeeding specialist to make sure your baby’s mouth and body are positioned correctly and that there are no other latching problems. They can also check inside your baby’s mouth to see if there is a physical problem.
- Try different breastfeeding positions. A laid-back, cross-cradle, underarm (‘rugby ball’) or lying-down hold may take the pressure off the most painful areas of your breast.
- Wipe damaged nipples gently with several pieces of water-moistened cotton wool after feeding to remove any debris that could lead to infection.
- Air-dry nipples or dab with a very clean, soft muslin or flannel, as infection can flourish in damp conditions. Use either disposable or washable nursing pads to absorb any milk leakage, remembering to change them regularly.
- Soothe your nipples. Relieve soreness and any dry skin with ultra-pure lanolin cream or gently apply a few drops of your own breast milk – you won’t have to remove either before the next feed.
 You could also try hydrogel pads straight from the fridge. These nipple dressings cool and provide instant breastfeeding pain relief, while creating ideal conditions for healing.
You could also try hydrogel pads straight from the fridge. These nipple dressings cool and provide instant breastfeeding pain relief, while creating ideal conditions for healing. - Protect your nipples. Breast shells prevent your clothes from rubbing against sore areas.
- Be patient. Soreness normally settles down after a few days as your body gets used to breastfeeding and your baby’s sucking becomes more efficient.
- Consult a healthcare professional, lactation consultant or breastfeeding specialist if the pain while breastfeeding doesn’t subside after a few days. Ongoing nipple soreness can be a sign of an infection that may require medication.
Problem 2: My baby is not latching properly
Some newborns just don’t seem to manage to get a great latch – perhaps because you both need a little more time to get breastfeeding coordinated, or because they were born prematurely, are uncomfortable after a difficult birth, or their mum has flat or inverted nipples.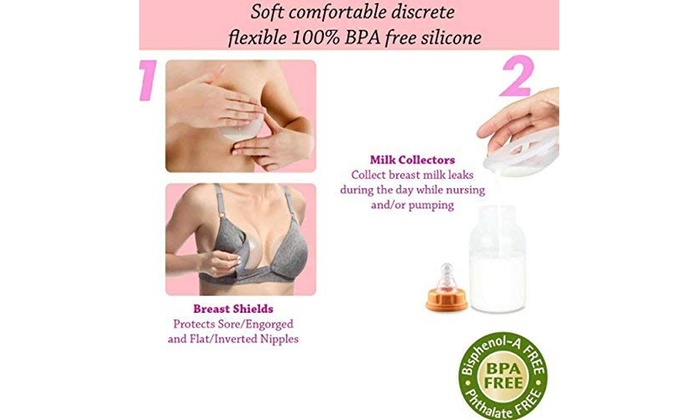
Solutions
- Get support from a lactation consultant or breastfeeding specialist who can diagnose the cause of the problem and develop a plan to help you overcome it.
- Draw out inverted or flat nipples. Nipple formers fit comfortably inside your bra, and apply a gentle pressure that can help draw out your nipples to support breastfeeding.
- Adopt different holds to make things easier for your newborn. She needs to feel supported, comfortable, and able to breathe in order to feed effectively. Make sure you’re not holding her head or pushing it. A laid-back, baby-led feeding style encourages your baby to use her innate reflexes, making it easier for her to reach your breast and latch on.4
- Make tiny adjustments while feeding. Rather than take your baby on and off the breast, creating frustration for you both, try ensuring she’s well positioned and comfortable.
 Keep her body and bottom close to you, support her across her shoulder girth, and hold her firmly so she feels secure. Let her head rest on your wrist so it can tilt back slightly and allow more space for her nose to breathe. Her chin should be close to your breast. If minor adjustments don’t seem to be improving your baby’s comfort, seek support from a lactation consultant or breastfeeding specialist.
Keep her body and bottom close to you, support her across her shoulder girth, and hold her firmly so she feels secure. Let her head rest on your wrist so it can tilt back slightly and allow more space for her nose to breathe. Her chin should be close to your breast. If minor adjustments don’t seem to be improving your baby’s comfort, seek support from a lactation consultant or breastfeeding specialist. - Feed through nipple shields. If your baby will not latch on, a lactation consultant or breastfeeding specialist may recommend using nipple shields to give your baby a larger, firmer target to attach to. In general, nipple shields should be considered a short-term solution.
The top 8 tips if your baby has lost too much weight
Problem 3: I do not have enough breast milk
Initially you’ll make a small amount of breast milk because the hormonal changes that trigger your milk production happen slowly, and won’t be finished until around day two to four. 2 This may cause you to worry your baby isn’t getting enough, but as her stomach is only tiny at first and she feeds frequently, it’s not a problem. During the first few days you only need to be concerned if your baby is losing more weight than expected and producing too few wet and dirty nappies, or is showing signs of dehydration. For a full explanation of how often your newborn should be weeing and pooing, read breastfeeding a newborn: what to expect in the first week.
2 This may cause you to worry your baby isn’t getting enough, but as her stomach is only tiny at first and she feeds frequently, it’s not a problem. During the first few days you only need to be concerned if your baby is losing more weight than expected and producing too few wet and dirty nappies, or is showing signs of dehydration. For a full explanation of how often your newborn should be weeing and pooing, read breastfeeding a newborn: what to expect in the first week.
Solutions
- Seek support from a lactation consultant, breastfeeding specialist or healthcare professional, who’ll be able to assess if you have a milk supply problem. The earlier you get help, the better.
- Feed on demand, not to a schedule. In the first week after birth your newborn will want to feed at least every two to three hours (maybe more!) throughout the day and night. This frequency helps to build your milk production.
- Look after yourself.
 It’s not always easy with a newborn, but try to rest when you can, eat well, and get as much help as possible with chores and any older children so you can focus on breastfeeding.
It’s not always easy with a newborn, but try to rest when you can, eat well, and get as much help as possible with chores and any older children so you can focus on breastfeeding. - Try expressing. If your baby is feeding often and still not putting on weight, a lactation consultant or breastfeeding specialist may recommend pumping to build your milk supply. If your milk hasn’t come in yet, the Medela Symphony hospital-grade double electric breast pump has an ‘Initiate’ program that mimics the way a newborn feeds in the first few days.
Problem 4: My breasts are really full and hard
When your milk comes in, your breasts will become fuller and firmer. If your baby is feeding well and frequently, this should pass without problems. However, some women’s breasts become rock hard, and they may also be tender, uncomfortable, even painful – a condition called breast engorgement. Engorged breasts may also feel fairly hot due to all the activity inside – it’s like a traffic jam in there! Although it’s only temporary, often lasting 24 to 48 hours, engorgement can also make it difficult for your baby to latch, as your nipples may become flattened. 5
5
Solutions
- Feed your baby frequently. Aim to feed at least eight to 12 times every 24 hours. This is the primary treatment for this condition – for more tips and advice read our article on breast engorgement.6,7
- See a healthcare professional, lactation consultant or breastfeeding specialist if the symptoms last more than 48 hours, you have a fever, or your baby is unable to breastfeed because of the engorgement.
Problem 5: My breasts are leaking
Leaky breasts are very common in the early days of breastfeeding, once your milk has come in. You may leak from one breast when you’re feeding your baby from the other, when lying on your front while sleeping, or when something stimulates your let-down reflex unexpectedly – like another baby crying in the supermarket. Leaking usually settles down after six weeks or so.
Solutions
- Protect your clothes by wearing disposable or washable nursing pads inside your bra day and night.

- Don’t waste a drop! Milk collection shells fit inside your bra to collect any leaked milk. They’re helpful when the leakage is too much for nursing pads, or if one nipple tends to drip while you’re feeding from the other. If you want to save the collected milk, you can, but only use milk you’ve collected during a breastfeed. Store in a sterile container and, if you’re not feeding it to your baby straight away, place in the fridge immediately and use within 24 hours. Don’t wear collection shells for more than two to three hours at a time.
Problem 6: I think I’m producing too much milk
Sometimes when your milk comes in, it really comes in! You may have a temporary oversupply for the first few weeks but it should settle down soon.7 Until then your breasts may feel painful and hard most of the time, even straight after a feed, and you might be leaking a lot of milk. Your baby may cough and splutter with the force of your let down, vomit as soon as she is moved after feeds, and have an uncomfortable tummy or explosive, frothy, greenish poos. All this suggests you may have too much milk, but this issue may resolve itself as soon as your breasts adjust to their new job.
All this suggests you may have too much milk, but this issue may resolve itself as soon as your breasts adjust to their new job.
Solutions
- Express a little milk by hand at the start of each feed to reduce the force of your let down.
- Try the laid-back breastfeeding position so your baby can better control the flow of milk. Or use the cradle position: holding her across her shoulders, ensuring your baby’s head is tilting back slightly and resting on your wrist. Her body will be resting on yours, sloping down diagonally.
- Be gentle and patient. Allow your baby to rest and digest her milk, both during and after a feed. Moving her around too much or too quickly could make her feel sick. As she grows, she’ll get better at coping with the flow, which is likely to slow in any case.
- Use a towel or muslin cloth to soak up the surge if your baby gets overwhelmed when your milk starts to flow, and put a milk collection shell on your other breast to catch any leaks.

- Seek advice from a lactation consultant or breastfeeding specialist if you’re still having difficulties after several weeks. They will assess you, and may advise on one-sided feeding or block feeding if you need to reduce your milk supply.
Read on: Breastfeeding difficulties in the next few weeks and breastfeeding challenges after the first month
References
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics. 2013:peds-2013.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching‐On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women’s Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev. 2008;84(7):441-449.
Early Hum Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208.
6 Amir LH. Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol# 4: Mastitis, revised March 2014. Breastfeed Med. 2014;9(5):239-243.
7 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol# 20: Engorgement. Breastfeed Med. 2009;4(2):111-113.
Mastitis | Morozovskaya Children's Clinical Hospital DZM
The hospital operates around the clock
The call center is open from 08:00 to 20:00 +7 (495) 959-88-00, +7 (495) 959-88-03
Appointments | examination
Online appointment
Physiological breast engorgement in newborns occurs on the 3rd-4th day of life, reaching a maximum by the 7th-8th day of life. Associated with the ingress of maternal hormones into the placental circulation. It occurs in both girls and boys.
Manifested as an increase in the mammary glands, often symmetrical. The skin over the enlarged mammary gland is not changed. A milky-white fluid may come out of the nipple. This condition does not require special treatment. As the level of maternal hormones in the blood decreases in a newborn child, physiological breast engorgement disappears.
Mastitis is a purulent-inflammatory disease of the breast. It occurs in both girls and boys in the first 2 weeks of life.
Mastitis is caused by bacteria entering the breast ducts during the period of physiological engorgement. It starts suddenly and progresses rapidly. It manifests itself in the form of an increase and redness of one breast. The gland becomes dense, sharply painful, pus may stand out from the nipple. The general condition of the child is deteriorating. The baby becomes lethargic, refuses to breastfeed, body temperature rises. In the future, the skin over the mammary gland acquires a purple-cyanotic hue, due to the underdevelopment of the capsule, inflammatory changes quickly spread beyond the mammary gland. In the absence of the necessary treatment, the process can spread in breadth and depth, causing necrotic changes in the breast itself and surrounding tissues.
In the absence of the necessary treatment, the process can spread in breadth and depth, causing necrotic changes in the breast itself and surrounding tissues.
Treatment of mastitis depends on the timeliness of seeking medical attention. In the early stages, at the very beginning of the disease, conservative treatment is possible. Apply warming ointment compresses, antibiotic therapy. In cases where an abscess has already formed in the region of the mammary gland, a surgical intervention is performed to open and drain the abscess cavity. From the first day, broad-spectrum antibiotics are prescribed until the postoperative wound heals and the seal resolves, which is an indication for the patient to be discharged.
The prognosis for mastitis in uncomplicated cases is favorable. In the case of late treatment and the severity of the inflammatory process, the death of the glandular tissue in girls is possible, which in the future may manifest itself in the form of a cosmetic defect and a decrease in lactation on the side of the lesion.
Version for the visually impaired
Morozov Children's City Clinical Hospital of the Moscow City Health Department
Call center from 08:00-20:00
+7 (495) 959-88-00
+7 (495) 959-88-03
Email: mdg.kbmoz. ru
MG MHIF
+7 (495) 952-93-21
Unified inquiry service
Government of Moscow
+7 (495) 777-77-77
Site map
Breast engorgement and bloody discharge from the vagina in newborns, is it dangerous - Children - tsn.ua , breast nipples and others.
Moms and dads can’t find a place for themselves from excitement and run with the child to the doctors, although in reality nothing terrible happens - we are talking about the so-called hormonal (genetic or sexual) crisis, which occurs quite often in newborns and passes without any intervention or treatment. The crisis is due to the fact that the mother passes on to her child an excessive amount of her own female sex hormones. More often, girls suffer from a hormonal crisis, but boys sometimes have its manifestations.
More often, girls suffer from a hormonal crisis, but boys sometimes have its manifestations.
Maya Smolyar, head of the department for post-intensive care of premature newborns at the Zhytomyr Regional Perinatal Center, told about the signs of a hormonal crisis and what parents should do.
Breast engorgement
Child health
The first sign of a hormonal crisis is a physiological breast engorgement or mastopathy. A whitish liquid like colostrum can sometimes even leak from the mammary glands. There is no need to be afraid of this, and physiological mastopathy should not be confused with mastitis! Mastitis is a pathological purulent process that needs treatment, while physiological mastopathy does not need treatment and goes away on its own within one to two weeks.
Breast engorgement appears 3-4 days after the birth of a child and does not cause him any discomfort at all. For the mother, the main thing is not to feel anything, not to squeeze anything out and not to strain out of the baby's breast. Keep the child's body clean. It is very important to know that new store-bought clothes for a newborn baby should be washed and ironed with a hot iron. After all, it is not known where and for how long these clothes were stored, what they came into contact with, who took them and with what hands. And another important point: clothes that are in direct contact with the child's body should only be made of natural fabric that "breathes". If the mother adheres to the elementary rules of hygiene, wash the child on time and wash her hands often, then physiological mastopathy will quietly go away without any consequences.
Keep the child's body clean. It is very important to know that new store-bought clothes for a newborn baby should be washed and ironed with a hot iron. After all, it is not known where and for how long these clothes were stored, what they came into contact with, who took them and with what hands. And another important point: clothes that are in direct contact with the child's body should only be made of natural fabric that "breathes". If the mother adheres to the elementary rules of hygiene, wash the child on time and wash her hands often, then physiological mastopathy will quietly go away without any consequences.
What is menorrhagia?
On the 4-5th day after birth, girls may experience bloody discharge from the genital slit, resembling menstruation in women - the so-called menorrhagia. Many mothers are terrified of this. But you don't need to be afraid. This is a manifestation of a hormonal crisis, which goes away within 4-5 days, a maximum of a week. In this case, hygiene is also important.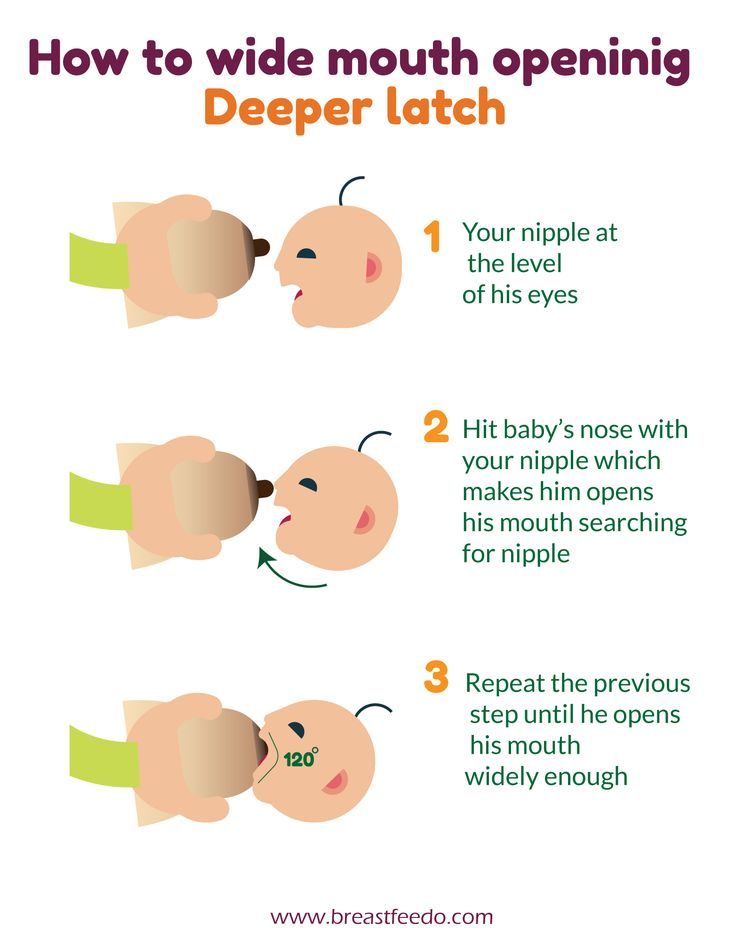 Girls should be washed in such a way that the water jet is directed from front to back. That's all the recommendations. In no case should you try to scrape off the discharge with your finger or scratch it - this way you will only injure the child.
Girls should be washed in such a way that the water jet is directed from front to back. That's all the recommendations. In no case should you try to scrape off the discharge with your finger or scratch it - this way you will only injure the child.
Vulvovaginitis. Do not be afraid
Also read
In newborn girls, whitish discharge can also come from the genital slit - this is also a manifestation of a hormonal crisis. Usually they do not bother the child in any way, and parents should not worry. No need to try to scrape off the discharge with your finger or get your finger into the genital gap, otherwise you can injure the child and cause an infection. It is necessary to properly wash the child, change diapers on time and nothing else.
Testicular dropsy - is it scary?
In boys, a hormonal crisis often manifests itself in the form of swelling of the genital organs (popularly - dropsy of the testicles). This is a purely physiological process that should take place within two months. If the parents are seriously worried, it is best to consult a specialist to calm down. Only a doctor, in this case a district pediatrician, can distinguish a physiological process from a pathological one.
If the parents are seriously worried, it is best to consult a specialist to calm down. Only a doctor, in this case a district pediatrician, can distinguish a physiological process from a pathological one.
What does a rash on a child's face mean?
Also read
Another sign of a hormonal crisis in newborns is the appearance of so-called milia - pimples that look like a pustular rash. Pimples usually appear on the nose, cheeks and under the eyes of the baby. Often parents confuse them with furunculosis. But this is not furunculosis at all, but a blockage of the sebaceous glands on the child's face. To make sure of this, parents should show the baby to the pediatrician. But you yourself do not need to do anything: do not try to tear off pimples or smear them with something. The main thing is to wash the child twice a day, it is better not with water, but with a decoction of chamomile, and gently wipe your face with a baby towel. You can not use a towel made of hard fabric, so as not to injure the delicate skin of the baby.