Are birth defects genetic
What are Birth Defects? | CDC
Birth defects are common, costly, and critical conditions that affect 1 in every 33 babies born in the United States each year.1 Read more about what we have learned about birth defects and how women can improve their chances of having a baby born without a birth defect.
Birth Defects Are Common
Every 4 ½ minutes, a baby is born with a birth defect in the United States. That means nearly 120,000 babies are affected by birth defects each year.1
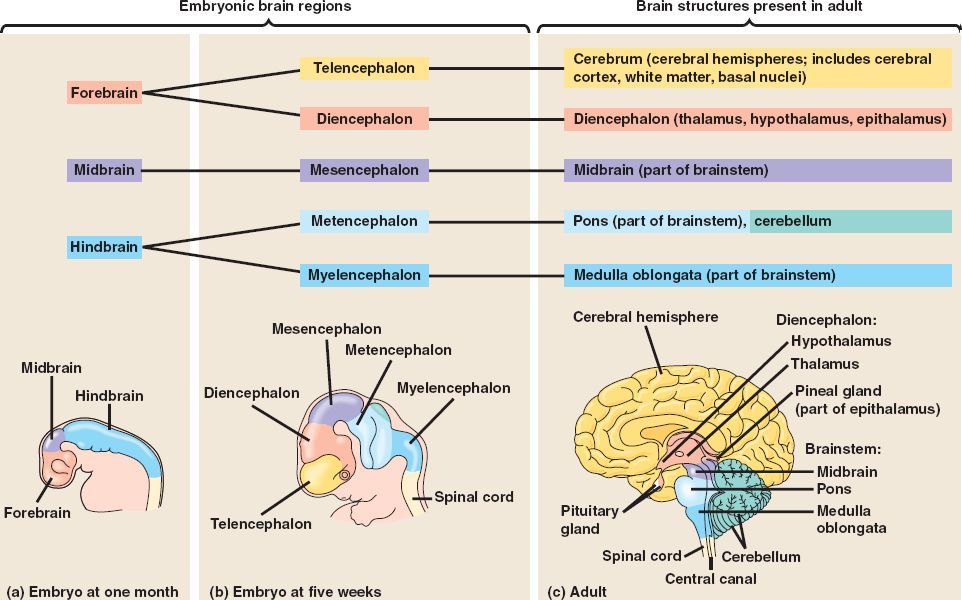
Birth defects are structural changes present at birth that can affect almost any part or parts of the body (e.g., heart, brain, foot). They may affect how the body looks, works, or both. Birth defects can vary from mild to severe. The well-being of each child affected with a birth defect depends mostly on which organ or body part is involved and how much it is affected. Depending on the severity of the defect and what body part is affected, the expected lifespan of a person with a birth defect may or may not be affected.
Identifying Birth Defects
A birth defect can be found before birth, at birth, or any time after birth. Most birth defects are found within the first year of life. Some birth defects (such as cleft lip) are easy to see, but others (such as heart defects or hearing loss) are found using special tests, such as echocardiograms (an ultrasound picture of the heart), x-rays or hearing tests.
Learn more about diagnosing birth defects »
Causes
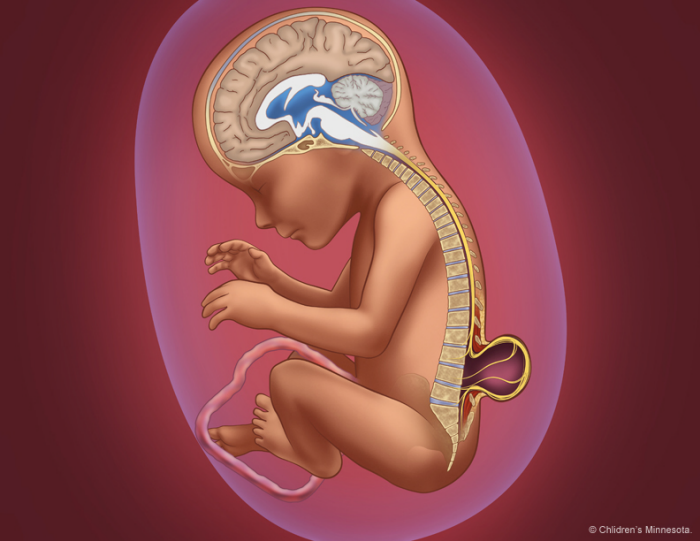
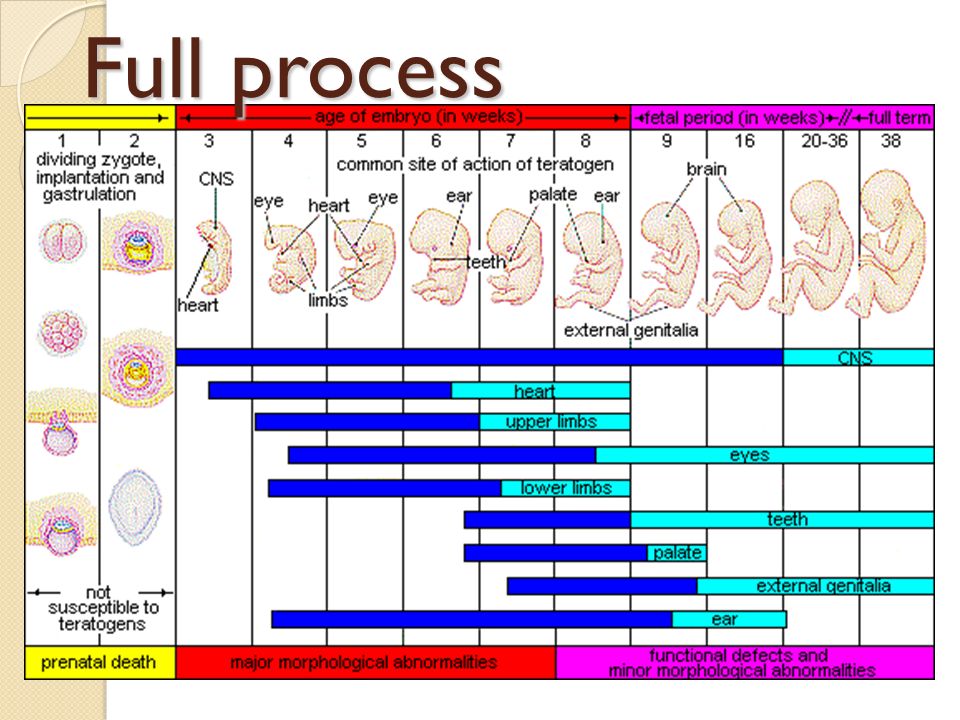
Birth defects can occur during any stage of pregnancy. Most birth defects occur in the first 3 months of pregnancy, when the organs of the baby are forming. This is a very important stage of development. However, some birth defects occur later in pregnancy. During the last six months of pregnancy, the tissues and organs continue to grow and develop.
For some birth defects, like fetal alcohol syndrome, we know the cause. But for most birth defects, we don’t know what causes them. For most birth defects, we think they are caused by a complex mix of factors.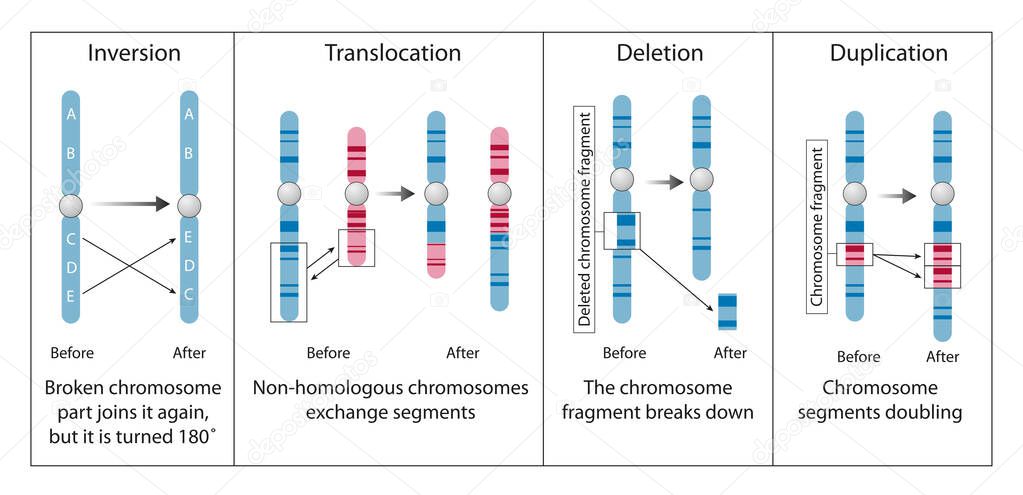 These factors include our genes (information inherited from our parents), our behaviors, and things in the environment. But, we don’t fully understand how these factors might work together to cause birth defects.
These factors include our genes (information inherited from our parents), our behaviors, and things in the environment. But, we don’t fully understand how these factors might work together to cause birth defects.
While we still have more work to do, we have learned a lot about birth defects through past research. For example, some things might increase the chances of having a baby with a birth defect, such as:
- Smoking, drinking alcohol, or taking certain drugs during pregnancy.
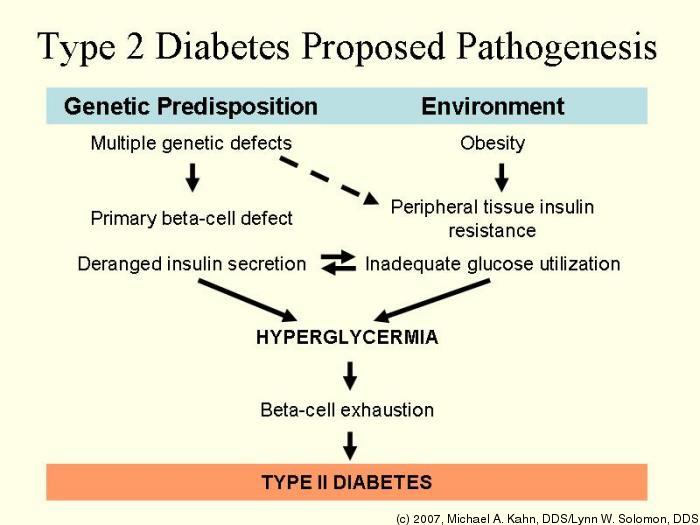
- Having certain medical conditions, such as being obese or having uncontrolled diabetes before and during pregnancy.
- Taking certain medications, such as isotretinoin (a drug used to treat severe acne).
- Having someone in your family with a birth defect. To learn more about your risk of having a baby with a birth defect, you can talk with a clinical geneticist or a genetic counselor.
- Having certain infections during pregnancy such as Zika virus and cytomegalovirus.
- Experiencing fever greater than 101oF or having an elevated body temperature due to heat exposure.
- Being an older mother, as the risk of chromosomal abnormalities increases with age.
Having one or more of these risks doesn’t mean you’ll have a pregnancy affected by a birth defect. Also, women can have a baby born with a birth defect even when they don’t have any of these risks. It is important to talk to your doctor about what you can do to lower your risk.
Learn about CDC’s research on causes and risk factors »
Top of Page
Prevention
Not all birth defects can be prevented. But, there are things that a woman can do before and during pregnancy to increase her chance of having a healthy baby:
- Be sure to see your healthcare provider regularly and start prenatal care as soon as you think you might be pregnant.
- Get 400 micrograms (mcg) of folic acid every day, starting at least one month before getting pregnant.

- Don’t drink alcohol or smoke.
- Talk to a healthcare provider about any medications you are taking or thinking about taking. This includes prescription and over-the-counter medications and dietary or herbal supplements. Don’t stop or start taking any type of medication without first talking with a doctor.
- Know how to prevent infections during pregnancy.
- Be proactive in identifying and treating fever when ill or after getting a vaccine. Treat fevers higher than 101oF with Tylenol® (or store brand acetaminophen), and avoid hot tubs, saunas, or other environments that might cause overheating.
- If possible, be sure any medical conditions are under control, before becoming pregnant. Some conditions, such as diabetes, can increase the risk for birth defects.
More tips to prevent birth defects »
Top of Page
Living with a Birth Defect
Babies who have birth defects often need special care and interventions to survive and to thrive developmentally.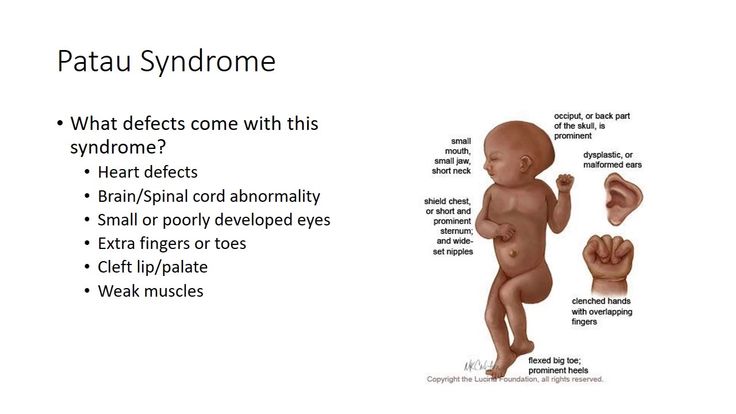 State birth defects tracking programs provide one way to identify and refer children as early as possible for services they need. Early intervention is vital to improving outcomes for these babies. If your child has a birth defect, you should ask his or her doctor about local resources and treatment. Geneticists, genetic counselors, and other specialists are another resource.
State birth defects tracking programs provide one way to identify and refer children as early as possible for services they need. Early intervention is vital to improving outcomes for these babies. If your child has a birth defect, you should ask his or her doctor about local resources and treatment. Geneticists, genetic counselors, and other specialists are another resource.
Find more information for families who have a child with a birth defect »
Top of Page
References
- Centers for Disease Control and Prevention. Update on Overall Prevalence of Major Birth Defects–Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5.
Genetic and chromosomal conditions | March of Dimes
Genes and chromosomes sometimes change or have missing or extra parts. This can cause serious health conditions and birth defects in your baby.
You can decide whether to have tests before and during pregnancy to find out if your baby is at increased risk for or has certain genetic conditions and birth defects.
Your provider or a genetic counselor can help you understand the benefits and risks of testing.
A genetic counselor can also help you understand test results and how genetics, birth defects and other medical conditions run in families.
Your family health history can help you, your provider and your genetic counselor identify genetic conditions that run in your family.
What are genes and chromosomes?
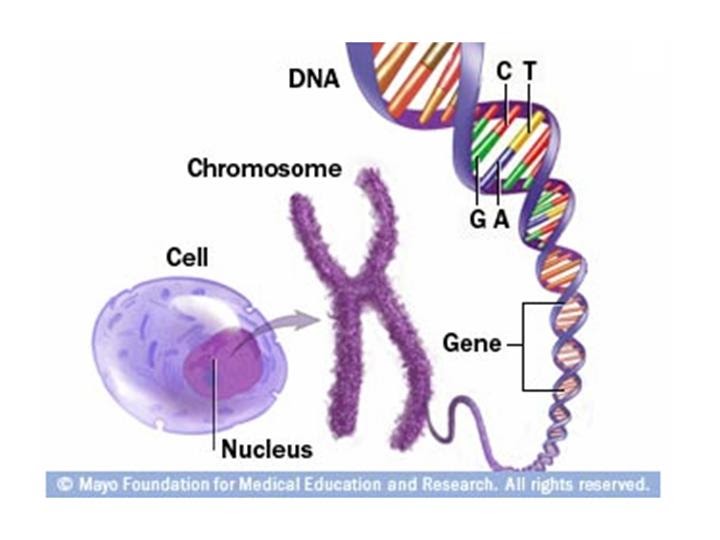
Genes are part of your body’s cells that store instructions for the way your body grows and works. Genes are passed from parents to children. Each person has more than 20,000 genes. Your genes make you the way you are — they help control things like your height, the curliness of your hair and the color of your eyes.
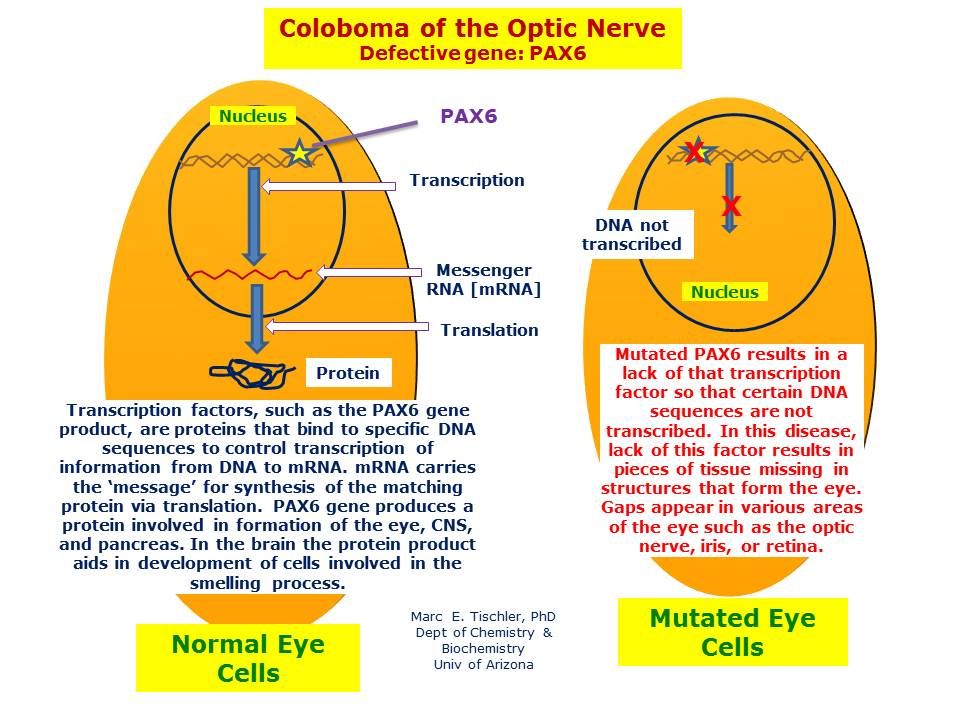
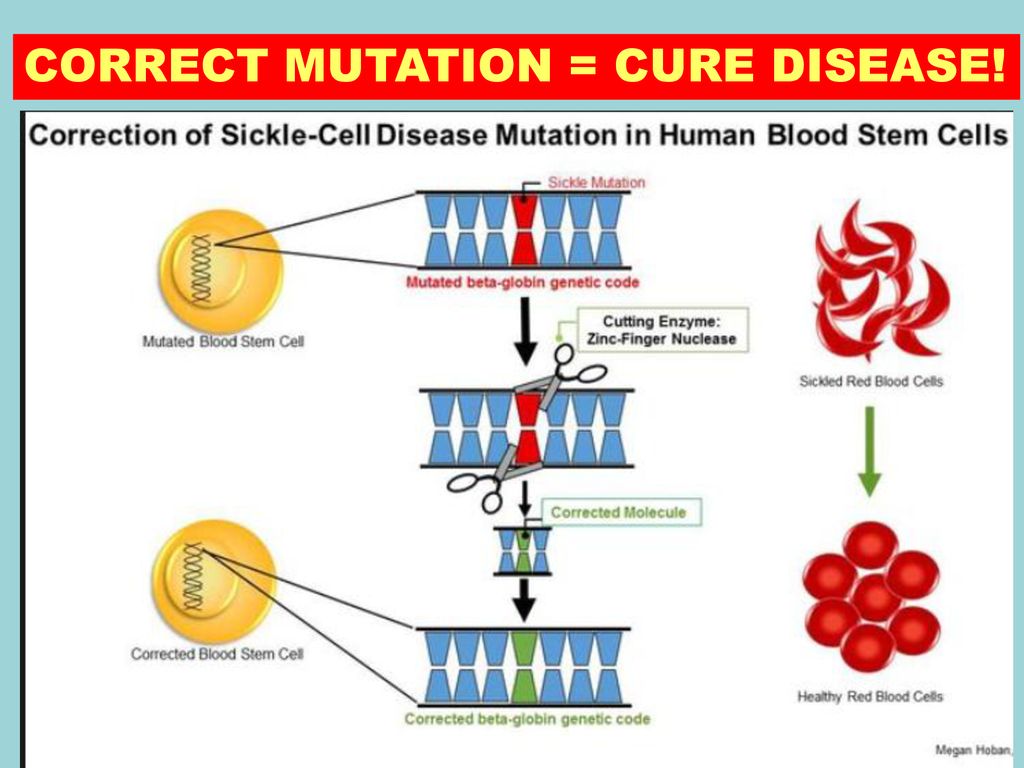
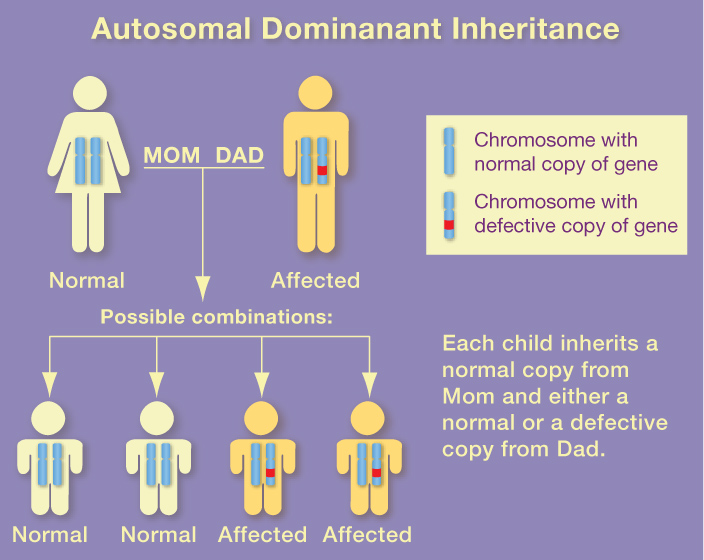
Sometimes the instructions that are stored in a gene change. This is called a gene change or a mutation. A gene can change on its own, or it can be passed from parents to children.
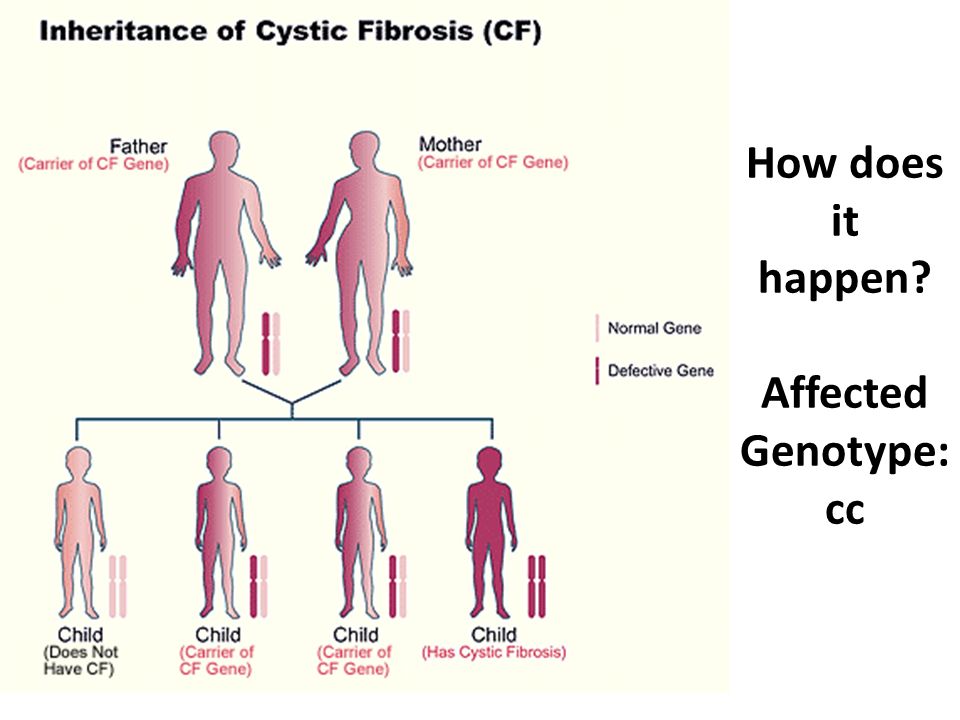
A gene change can sometimes cause health conditions, like cystic fibrosis and sickle cell disease.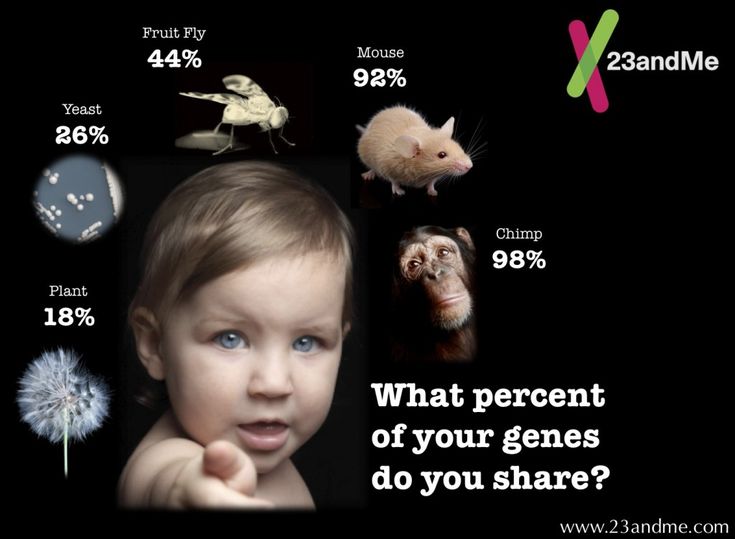 A gene change also can cause birth defects, like heart defects. Birth defects are structural changes present at birth that can affect almost any part of the body. They may affect how the body looks, works or both. Birth defects can cause problems in overall health, how the body develops or how the body works.
A gene change also can cause birth defects, like heart defects. Birth defects are structural changes present at birth that can affect almost any part of the body. They may affect how the body looks, works or both. Birth defects can cause problems in overall health, how the body develops or how the body works.
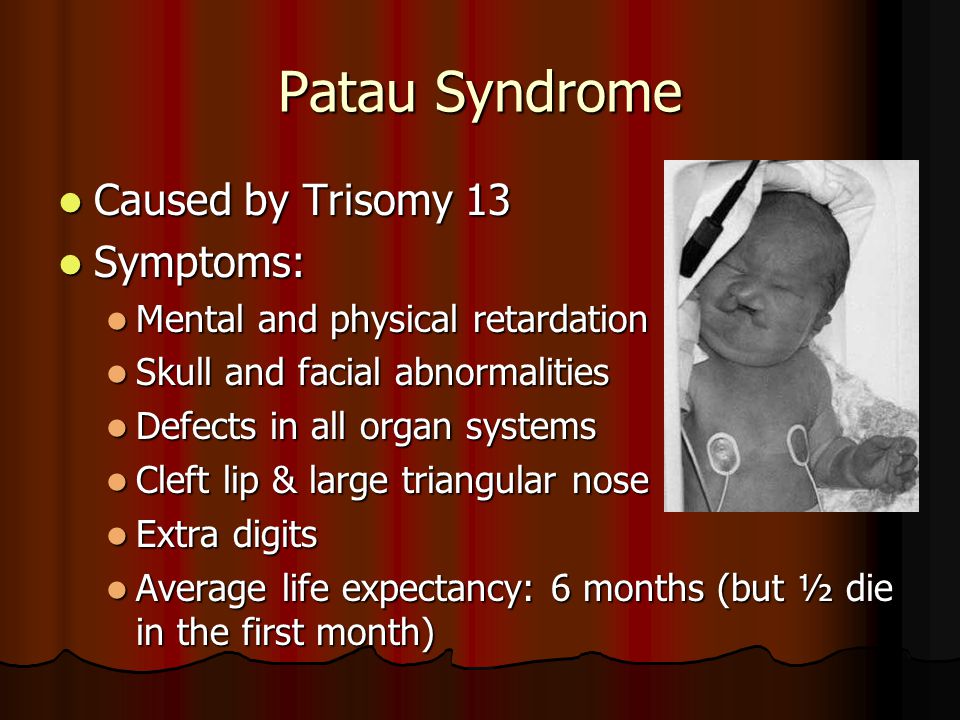
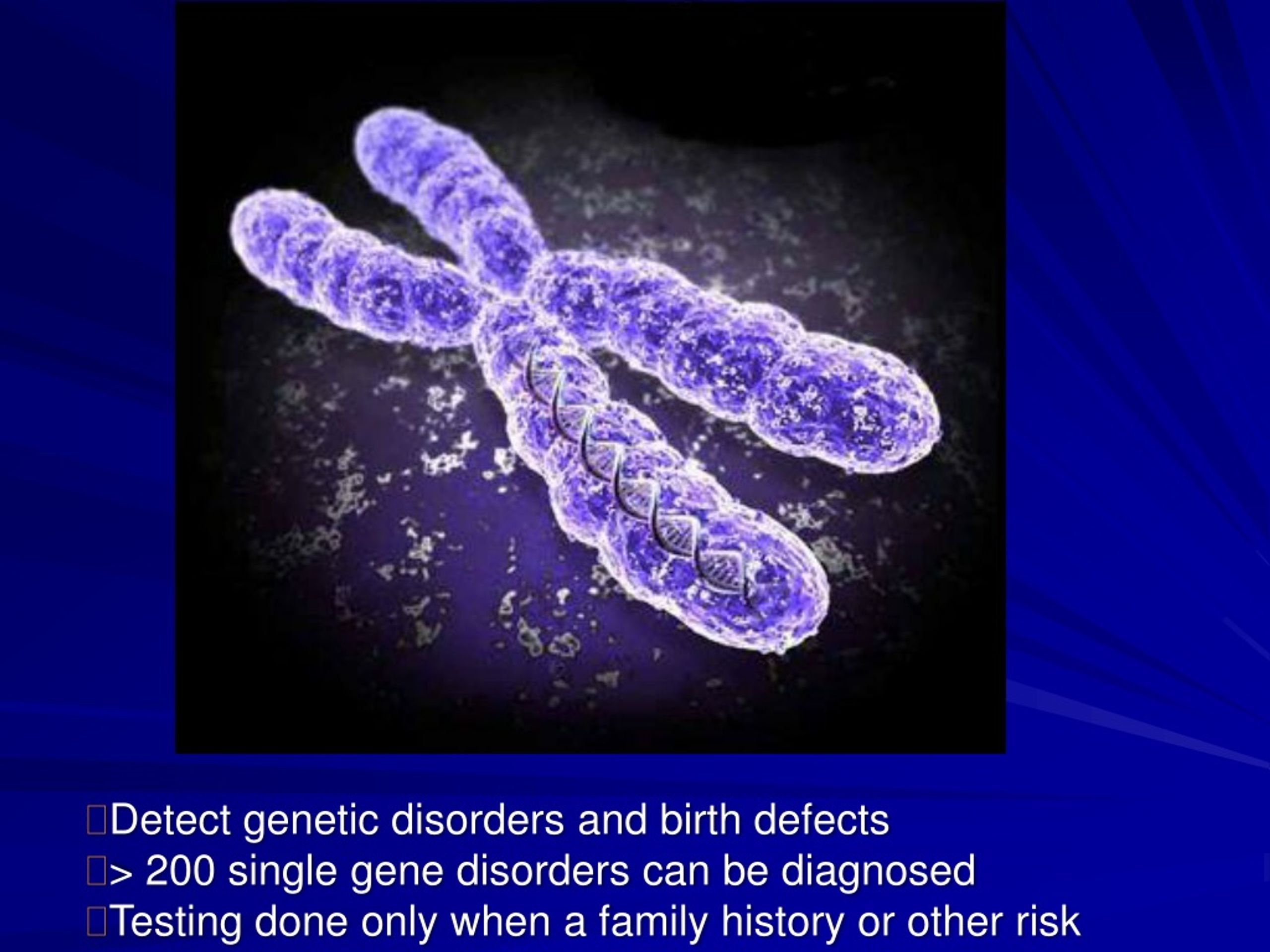
Any condition caused by a gene change is called a genetic condition (also called a genetic disorder). Some types of genetic conditions are caused by problems in one or more chromosomes. Chromosomes are the structures that hold genes. Each person has 23 pairs of chromosomes, or 46 in all. For each pair, you get one chromosome from your mother and one from your father.
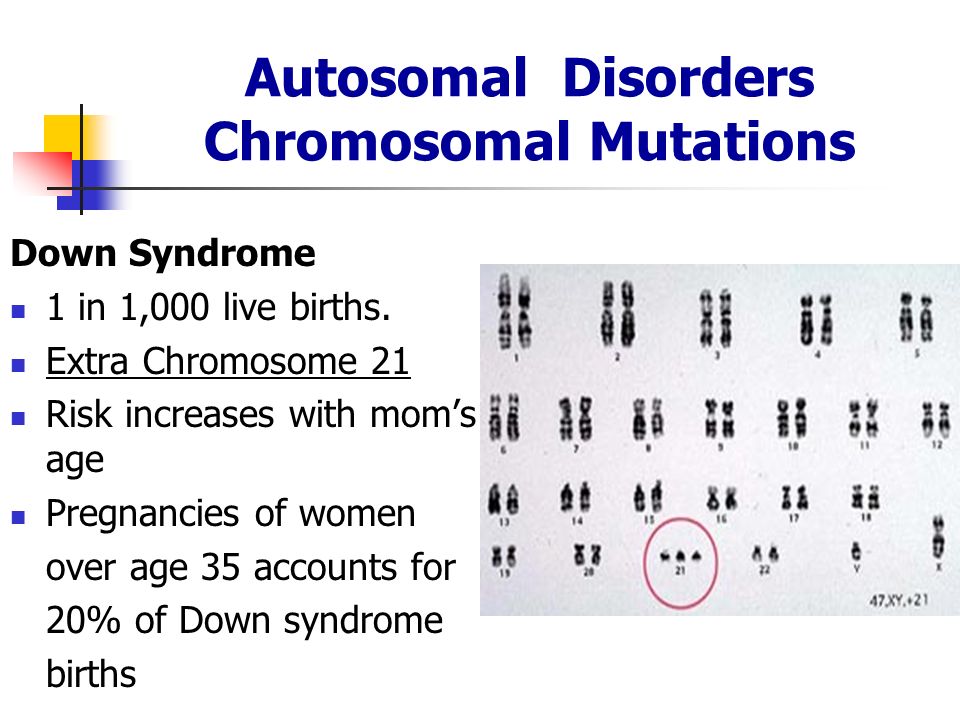
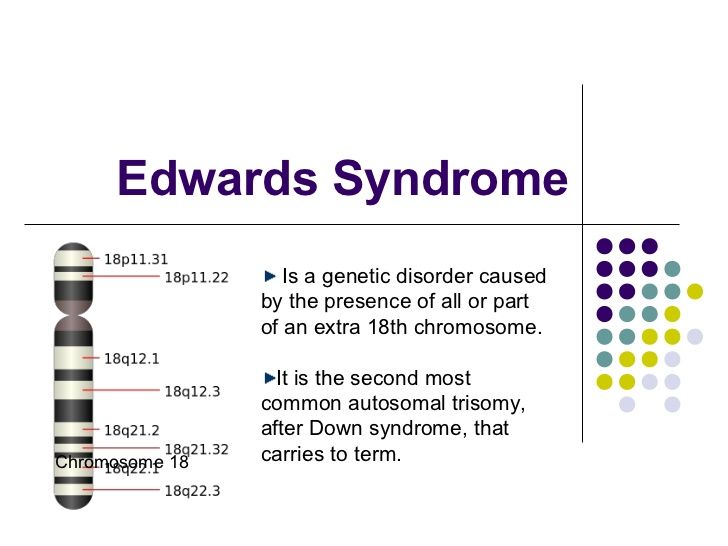
Just like genes, sometimes chromosomes change. There may be too many or too few chromosomes, or part of a chromosome may be missing. These changes can cause chromosomal conditions (also called chromosomal disorders) in a baby. One of the most common chromosomal conditions is Down syndrome (when there are three copies of chromosome 21 instead of two).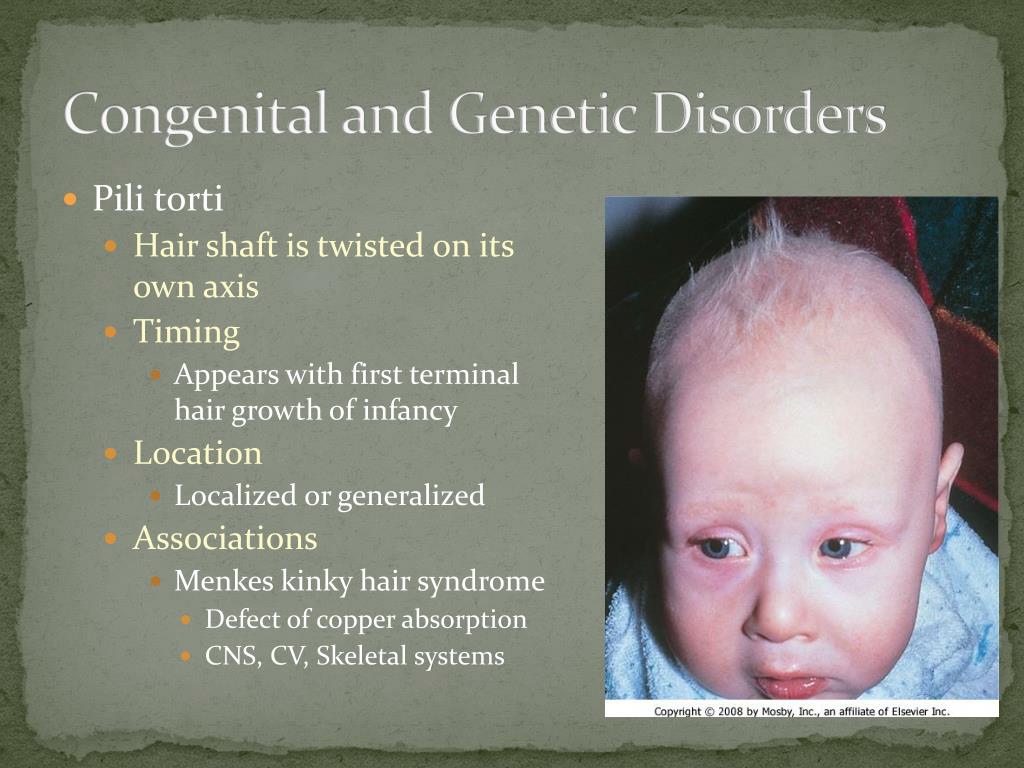 Parents can pass chromosome changes to their children, or they can happen on their own as cells develop.
Parents can pass chromosome changes to their children, or they can happen on their own as cells develop.
What is genetic counseling?
Genetic counseling helps you understand how genes, birth defects and other medical conditions run in families, and how they can affect your health and your baby's health. You get genetic counseling from a genetic counselor. This is a person who is trained to help you understand about genes, birth defects and other medical conditions that run in families, and how they can affect your health and your baby’s health. A genetic counselor can help you understand the causes of genetic conditions, what kind of testing is available, and your chances of having a baby with a genetic condition. To find a genetic counselor in your area, talk to your health care provider or contact the National Society of Genetic Counselors.
How can you find out if your baby is at risk for a genetic condition?
Your baby may be at increased risk of having a genetic condition if:
- You or your partner has a genetic condition.
- You have a child with a genetic condition.
- A genetic condition runs in your or your partner’s family or ethnic group. An ethnic group is a group of people, often from the same country, who share language or culture.
Your provider and genetic counselor use your family health history to learn more about genes, chromosomes and things in your life that may affect your health and your baby’s health. A family health history is a record of any health conditions and treatments that you, your partner and everyone in your families have had. Use our family health history form and share it with your provider.
What tests can you get before pregnancy to help you find out about genetic conditions that may affect your baby?
Carrier screening. Before pregnancy, you can have carrier screening tests that check your blood, saliva or tissue from inside your cheek to see if you’re a carrier of certain genetic conditions. If you’re a carrier, you don’t have the condition yourself, but you have a gene change for it that you can pass to your baby.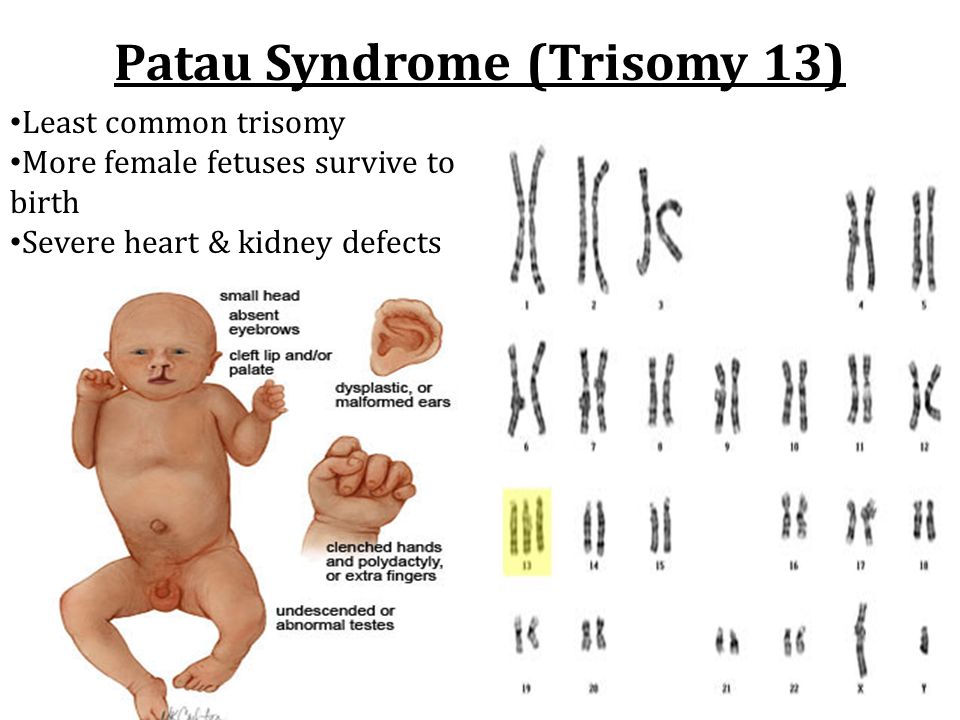
Your partner can get tested, too. If both you and your partner are carriers of the same condition, the risk that your baby has the condition increases. Getting tested before pregnancy can help you and your partner look at your baby’s risk and make decisions about getting pregnant. Carrier screening is your choice. You don’t have to have it if you don’t want it, even if your provider recommends it.
All women who are thinking about getting pregnant can get carrier screening for:
- Cystic fibrosis (also called CF). CF is a condition that affects breathing and digestion. Digestion is the process of how your body breaks down food after you eat.
- Spinal muscular atrophy (also called SMA). SMA is a group of conditions that causes muscle damage and weakness. It eventually leads to death.
- Hemoglobinopathies. These conditions affect red blood cells in the body. Types of hemogloinopathies include:
- Thalassemias. These are blood conditions that cause the body to make fewer healthy red blood cells and less hemoglobin than normal.
 Hemoglobin is a protein in red blood cells.
Hemoglobin is a protein in red blood cells. - Sickle cell disease. This is a blood condition that causes red blood cells to be shaped like a “C.”
- Thalassemias. These are blood conditions that cause the body to make fewer healthy red blood cells and less hemoglobin than normal.
Targeted carrier screening. Some women get carrier screening for certain conditions that run in families or ethnic groups. This is called targeted carrier screening or ethnic-based carrier screening. Your provider may recommend targeted carrier screening for conditions based on your family history or ethnic group, including:
- Fragile X syndrome (also called FXS). This condition happens when the body can’t make enough of a protein it needs for the brain to grow and develop. If Fragile X syndrome runs in your family, your provider may recommend carrier testing for this genetic condition.
- Tay Sachs disease. This is a condition that causes nerve cells in the brain and spine to die. It’s more common in people who are Eastern and Central European Jewish (also called Ashkenazi Jews), French-Canadian, Louisiana Cajun or Old Order Amish of Pennsylvania.
Preimplantation genetic testing. If testing shows that you or your partner is a carrier of a genetic condition and you’re having fertility treatment called in vitro fertilization (also called IVF), another testing option is preimplantation genetic testing (also called preimplantation genetic diagnosis). IVF is when an egg and sperm are combined in a lab to create an embryo (fertilized egg) which is then put in your uterus. This test checks cells from the embryo for gene changes before they’re put in your uterus. Your IVF provider can then choose embryos that don’t test positive for a gene change. Your provider or genetic counselor can help you understand your test results and the chances of passing a genetic condition to your baby.
After any testing, you and your partner talk with your provider and genetic counselor to understand results and how they may affect you, your baby and your family. Knowing whether or not your baby is at risk for a genetic condition can help you make decisions about your baby’s future and make plans to care for and get treatment for your baby after birth.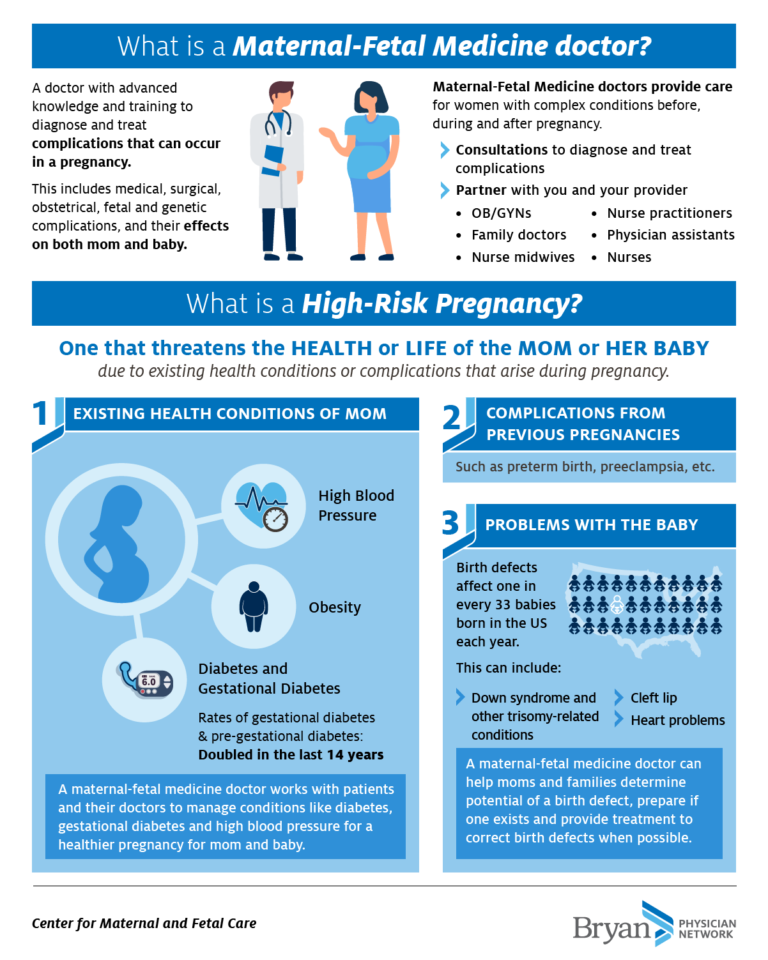
What tests can you get during pregnancy to find out about genetic conditions that may affect your baby?
Tests you can get during pregnancy include:
- Screening tests, including first-trimester screening, maternal blood screening (also called a quad screen) and cell-free DNA testing. These tests have some limitations. They tell you if your baby may be at risk for certain genetic conditions. But they do not tell you if your baby definitely has a condition. Sometimes these tests can have incorrect results. You can have screening tests as part of your prenatal tests in the first or second trimester of pregnancy.
- Diagnostic tests, including amniocentesis (also called amnio) and chorionic villus sampling (also called CVS). A diagnostic test is a test to see if you or your baby has or doesn’t have a health condition. If a screening test shows that your baby may be at risk for a condition, you can get a diagnostic test, like amnio or CVS, to find out for sure.
 The decision is up to you. Your provider also can check your baby’s blood for certain genetic conditions after he’s born.
The decision is up to you. Your provider also can check your baby’s blood for certain genetic conditions after he’s born.
The American College of Obstetricians and Gynecologists (ACOG) recommends that health care providers offer all pregnant women prenatal screening and diagnostic tests. ACOG recommends that providers give clear information about these tests so that you can make a decision that’s right for you. Before and after any testing, you and your partner can talk with your provider, a genetic counselor or both about how test results may affect you, your baby and your family.
What are the benefits and risks of testing?
Benefits of testing are learning and knowing about your baby’s condition include:
- You may learn that your baby isn’t at risk for or doesn’t have the genetic conditions you tested for.
- If you find out your baby may be at higher risk for a condition, you can find out about more testing.
- If you find out your baby does have a condition, you can find out if treatment is available during pregnancy or right after birth and make decisions about his care.
 You may want to give birth in a hospital that has the best providers and equipment to treat and care for your baby. You can find out about support services available for you and your partner. And you can learn about treatment and services available after you take your baby home.
You may want to give birth in a hospital that has the best providers and equipment to treat and care for your baby. You can find out about support services available for you and your partner. And you can learn about treatment and services available after you take your baby home.
Risks of testing include:
- Testing may affect your feelings. You may feel angry, sad or nervous about test results.
- Testing may affect family members. You may find out about a health condition that runs in your family, and not everyone in your family may want to know about or talk about the condition. Not everyone in your family may want to share health information.
- Testing may not tell you everything you need to know about your baby’s condition. For example, it may not tell you how severe a condition is or if it may get worse over time. Or the test may be inconclusive. This means it doesn’t give enough information about your baby’s condition. If results are inconclusive, you may need to decide whether to get more testing.
- Even if you know about your baby’s condition, there may be no treatment or limited treatment for it.
Physical risks of testing are small. Many tests use just a blood or saliva sample. Diagnostic tests like amnio and CVS have a small risk of miscarriage because they take a sample of fluid or tissue from around the baby.
What problems can genetic conditions cause during and after pregnancy?
Sometimes genetic conditions can cause miscarriage or stillbirth. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy. More than half of miscarriages are caused by chromosomal conditions. Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy. Sometimes babies with certain genetic conditions do not survive long after birth.
Each child born with a genetic condition is different. Problems depend on which genes or chromosomes are affected. Some children don’t have serious problems. Some may have birth defects or intellectual and developmental disabilities or both.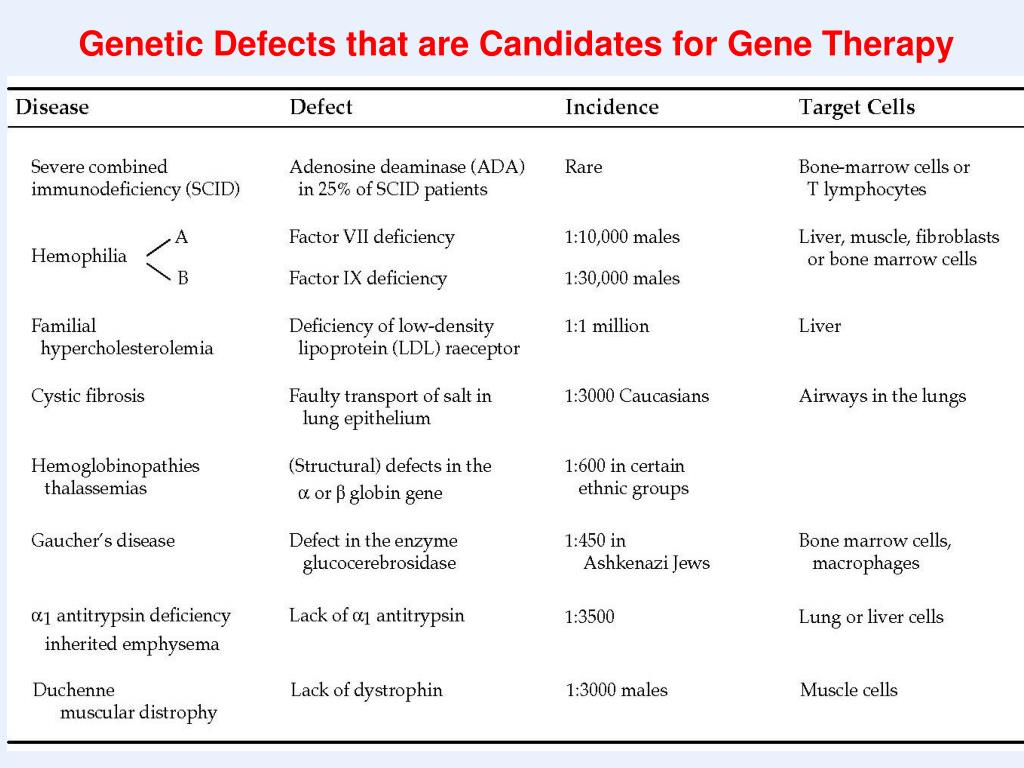 Intellectual and developmental disabilities are problems with how the brain works that can cause a person to have trouble or delays in physical development, learning, communicating, taking care of himself or getting along with others.
Intellectual and developmental disabilities are problems with how the brain works that can cause a person to have trouble or delays in physical development, learning, communicating, taking care of himself or getting along with others.
Do genes and chromosomes cause all health conditions and birth defects?
No. They cause some, but not all. We don’t know all the causes, but these things may increase the risk of your baby being born with a health condition or birth defect:
- Smoking, drinking alcohol or taking street drugs during pregnancy
- Taking certain medicines before or during pregnancy
- Getting certain infections during pregnancy
- Having certain health conditions that are not managed well
- Being in contact with harmful chemicals
More information
Centers for Disease Control and Prevention (CDC)
CDC Show Your Love Campaign
Einstein Victor Center for the Prevention of Jewish Genetic Diseases
Genetic Alliance
JScreen at Emory University
National Center for Education on Maternal and Child Health
National Organization for Rare Disorders (NORD)
National Society of Genetic Counselors
Last reviewed: April, 2022
Malformations
Malformations- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 O
- M
- R
- S
- T
- Y
- F
- X
- C
- W 0005
- B
- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- A
- B
- in
- g
- d
- E
- С
- and
- L
- m
- N 9000
- t
- in
- x
- 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Malformations
\n
- \n
- development and strengthening of registration and surveillance systems; \n
- experience and capacity building; \n
- strengthening research and scientific work in the field of etiology, diagnosis and prevention; \n
- strengthening international cooperation.
 \n
\n
\n
Definition
\n
\nCongenital malformations are also referred to as congenital malformations, congenital disorders, or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life.
\n
Causes and risk factors
\n
\nApproximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
\n
Socio-economic factors
\n
\nAlthough low income may be an indirect determinant, malformations are more likely to occur in families and countries with insufficient resources. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development.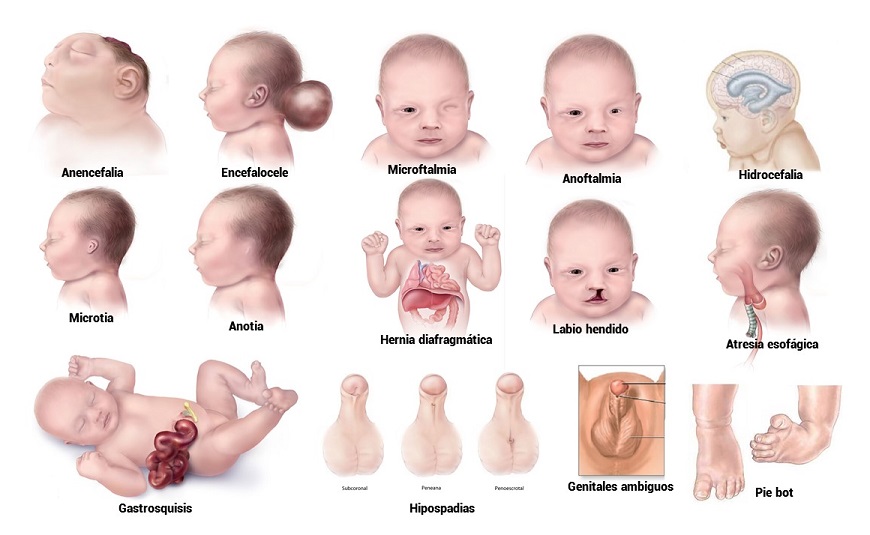 Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
\n
Genetic factors
\n
\nIncest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins . Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.\n
\n
Infections
\n
\nMaternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
\n
Maternal nutrition
\n
\nDeficiencies in iodine, folate, obesity, or conditions such as diabetes mellitus are associated with some malformations.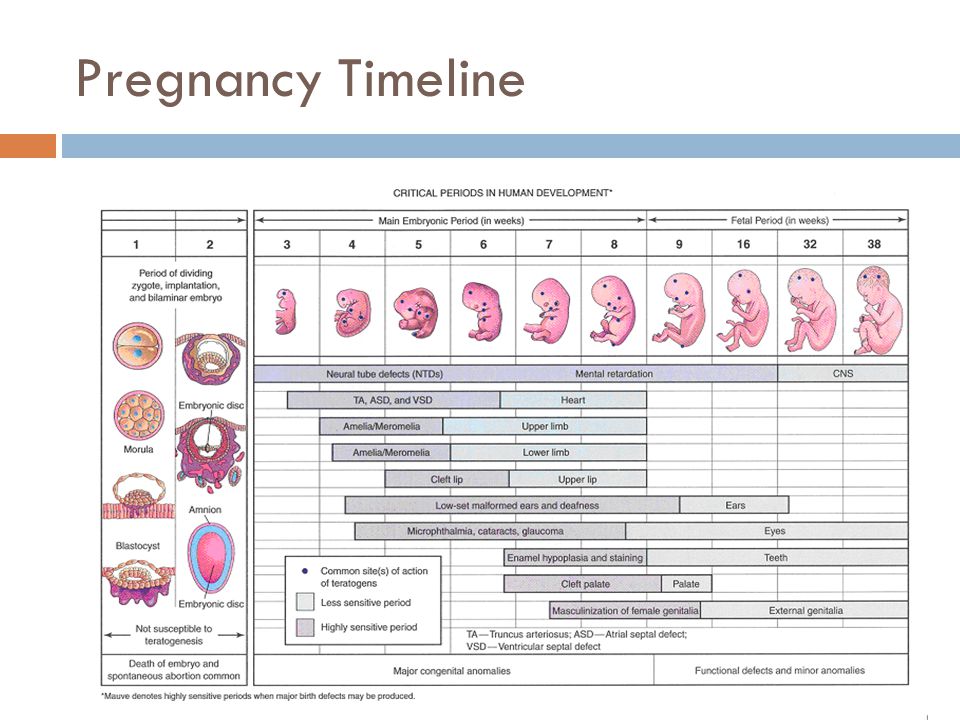 For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
\n
Environmental factors
\n
\nMaternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of developing the fetus or a newborn baby with birth defects. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition.
\n
Prevention
\n
\nPregnancy and conception preventive health care, and prenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures:
\n
- \n
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, as a result of daily oral supplementation or fortification of staple foods, such as wheat or corn flour.
 \n
\n - Supervise that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol. \n
- Pre-pregnancy and pregnancy prevention of diabetes through counseling, weight management, proper nutrition, and, if necessary, insulin administration. \n
- Prevention of exposure to environmental hazardous substances (eg, heavy metals, pesticides, certain drugs) during pregnancy. \n
- Ensuring that any exposure of a pregnant woman to drugs or medical exposures (such as x-rays) is justified and based on a careful analysis of the health risks and benefits. \n
- Increase vaccination coverage for women and children, especially against rubella. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood. \n
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n - Scaling up and intensifying training for health professionals and other staff involved in strengthening malformation prevention. \n
\n
Identification
\n
\nPre-conception (pre-conception) and near conception (peri-conception) health care includes basic reproductive health care as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
\n
- \n
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or at risk of passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
 \n
\n - Preconception screening: Maternal characteristics may increase risk, and screening results should be used to provide appropriate care based on risk. During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. \n
- Newborn screening includes a clinical examination and screening for hematological, metabolic, and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability.
 In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. \n
In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. \n
\n
Treatment and care
\n
\nIn countries with adequate health services, structural congenital malformations can be corrected with pediatric surgery and children with functional problems such as thalassemia (inherited by recessive blood disease), sickle cell disorders, and congenital hypothyroidism.
\n
WHO activities
\n
\nIn 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.
\n
\nThe Global Strategy for Women's and Children's Health, announced in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in implementing efficient and cost-effective action to promote newborn and child health.\n
\n
\nWHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy to fortify foods with salt folic acid at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.
\n
\nThe International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit, international organization in official relations with WHO.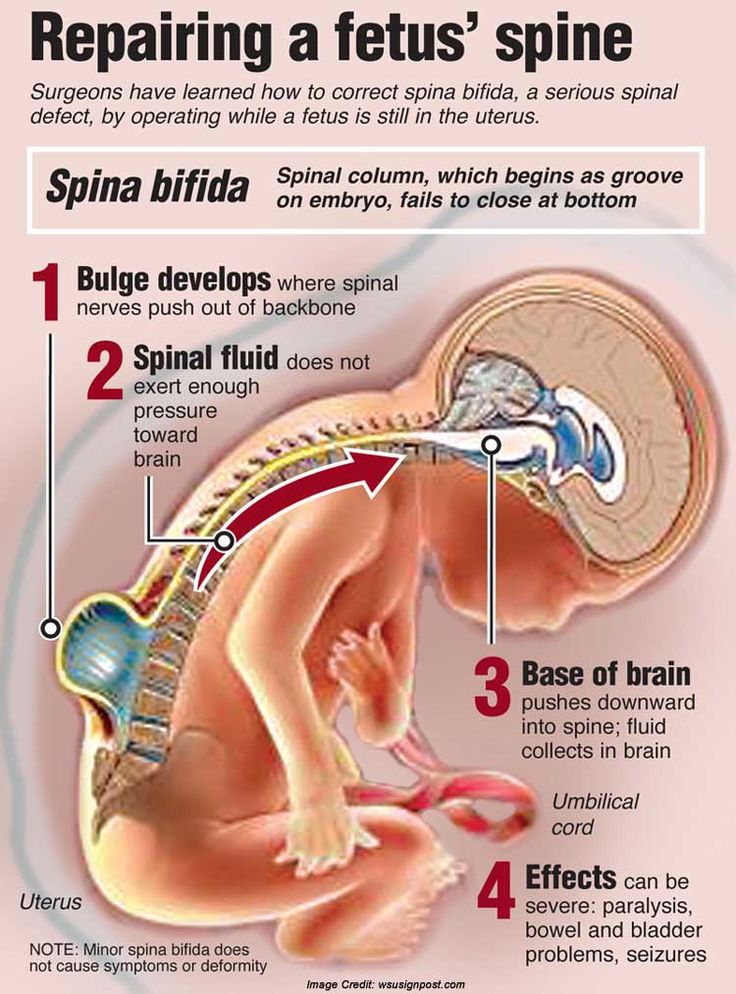 This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
\n
\nThe WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual seminars on surveillance and prevention of birth defects and preterm birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs.
\n
\nThe GAVI Alliance, partnered with WHO, is helping developing countries to increase the control and elimination of rubella and congenital rubella syndrome through immunization.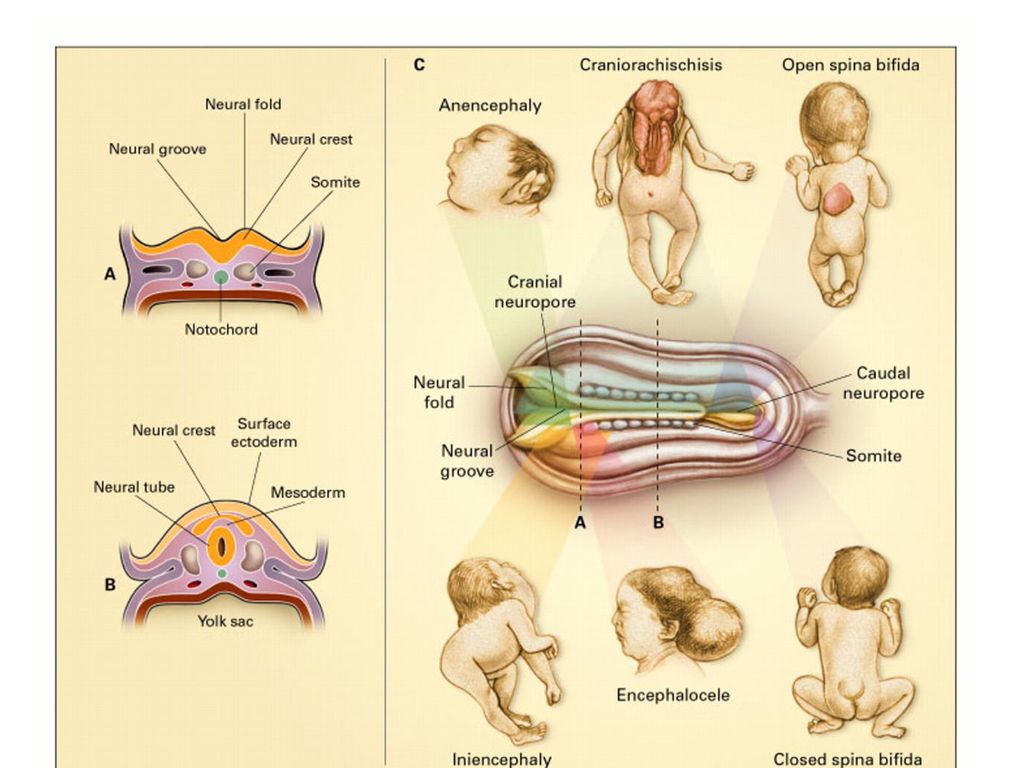
\n
\nWHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers.
\n
United Nations Convention on the Rights of Persons with Disabilities
\n
\nThe WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).
\n
","datePublished":"2022-02-28T22:52:00.0000000+00:00","image":"https://cdn.who.int/media/images/default -source/imported/preterm-birth-mother-jpg.jpg?sfvrsn=c5c1adf1_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo": {"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified ":"2022-02-28T22:52:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/congenital-anomalies", "@context":"http://schema.org","@type":"Article"};
Key Facts
- It is estimated that 303,000 children die every year from malformations during the first 4 weeks of life.
- Developmental disabilities can lead to long-term disability, with significant impacts on individuals, their families, health systems and society.
- The most severe malformations include heart defects, neural tube defects and Down's syndrome.

- Although malformations may be genetic, infectious or environmental in origin, the exact cause is often difficult to establish.
- Some birth defects can be prevented. The main elements of prevention are, inter alia, vaccination, adequate intake of folic acid or iodine through fortification of staple foods or provision of nutritional supplements, and proper prenatal care.
Malformations and preterm birth are major causes of childhood death, chronic disease and disability in many countries. In 2010, the World Health Assembly adopted a resolution calling on all Member States to promote primary prevention and health promotion for children with developmental disabilities through:
- development and strengthening of registration and surveillance systems;
- experience and capacity building;
- strengthening research and scientific work in the field of etiology, diagnosis and prevention;
- strengthening international cooperation.
Definition
Congenital malformations are also referred to as congenital malformations, congenital disorders or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life.
Causes and risk factors
Approximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
Socio-economic factors
While low income may be an indirect determinant, malformations are more likely to occur in under-resourced families and countries. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development. Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Genetic factors
Incest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins. Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.
Infections
Maternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
Maternal nutrition
Deficiency of iodine, folic acid salts, obesity, or conditions such as diabetes mellitus are associated with some malformations. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
Environmental factors
Maternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of birth defects in the fetus or newborn. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition.
Prevention
Preventive health care during pregnancy and conception, as well as antenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following:
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, through daily oral supplementation or fortification of staple foods such as wheat or corn flour .

- Supervise that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol.
- Prevention of diabetes in pregnancy and during pregnancy through counseling, weight management, proper nutrition and, if necessary, insulin administration.
- Prevention during pregnancy of exposure to hazardous environmental substances (eg, heavy metals, pesticides, certain drugs).
- Ensuring that any exposure of a pregnant woman to drugs or radiation for medical purposes (eg x-rays) is justified and based on a careful analysis of the health risks and benefits.
- Increase vaccination coverage for women and children, especially against rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood.
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy.
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. - Scaling up and intensifying training for health professionals and other staff involved in strengthening the prevention of malformations.
Identification
Medical care before conception (in the preconception period) and around the time of conception (in the periconceptional period) includes basic reproductive health care, as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
- Preconception screening: Maternal characteristics may increase risk and screening results should be used to provide appropriate care based on risk.
 During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy.
During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. - Newborn screening includes a clinical examination, as well as screening for hematological, metabolic and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability. In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward.
Treatment and medical care
In countries with adequate health services, structural birth defects can be corrected with pediatric surgery and timely treatment can be provided for children with functional problems such as thalassemia (a recessive blood disorder), sickle cell disorders, and congenital hypothyroidism.
WHO activities
In 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.
The Global Strategy for Women's and Children's Health, launched in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in achieving effective and cost-effective action to improve newborn health and children.
WHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy for folic acid fortification at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.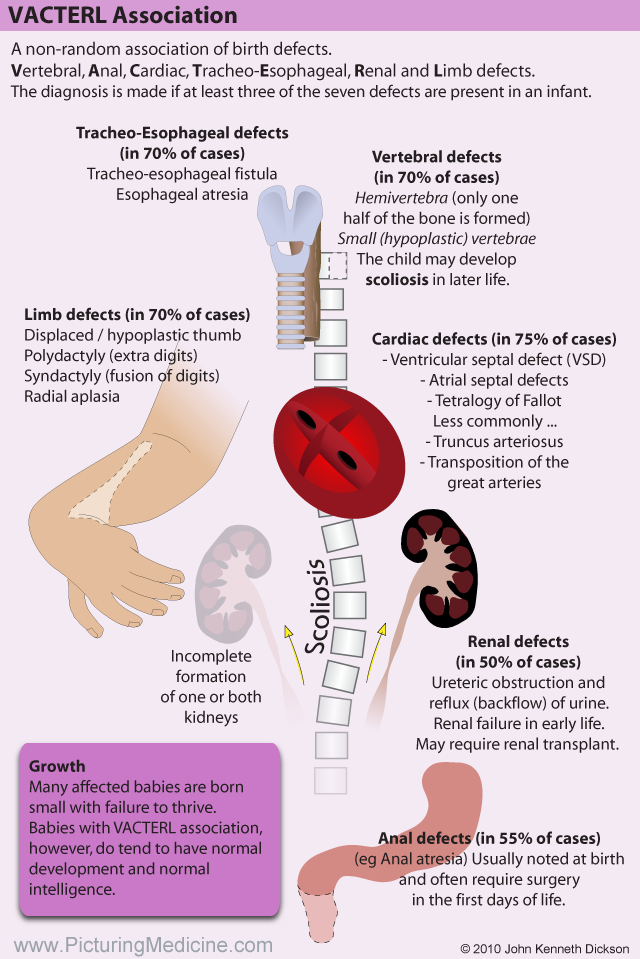
The International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit international organization in official relations with WHO. This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
The WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual workshops on surveillance and prevention of birth defects and premature birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs.
The GAVI Alliance, with WHO among its partners, is helping developing countries to accelerate the control and elimination of rubella and congenital rubella syndrome through immunization.
WHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers.
UN Convention on the Rights of Persons with Disabilities
The WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).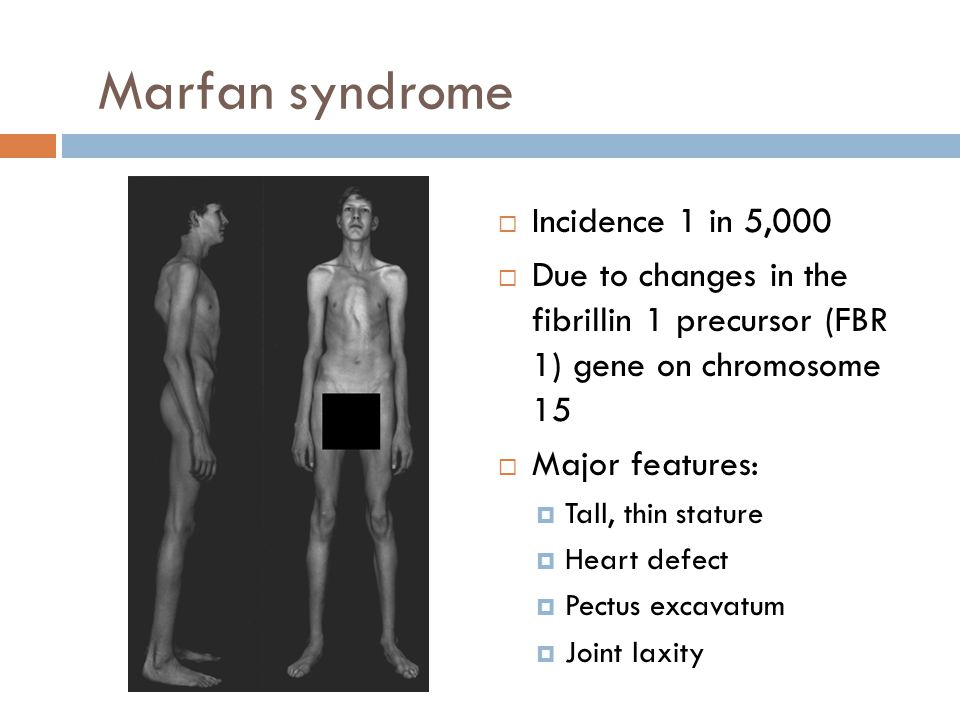
Congenital genetic anomalies
Home / Congenital genetic anomalies
Genetic are diseases that occur due to defects in genes, chromosomal abnormalities. Every healthy person has 6-8 damaged genes, but they do not disrupt cell functions and do not lead to disease, because they are recessive (non-manifested). If a person inherits two similar abnormal genes from his mother and father, he becomes ill. The probability of such a coincidence is extremely small, but it increases dramatically if the parents are relatives (that is, they have a similar genotype). For this reason, the frequency of genetic abnormalities is high in closed populations.
Each gene in the human body is responsible for the production of a specific protein. Due to the manifestation of a damaged gene, the synthesis of an abnormal protein begins, which leads to cell dysfunction and developmental defects.
A doctor can establish the risk of a possible genetic anomaly by asking you about the diseases of relatives “up to the third knee”, both on your part and on the part of your husband.
Currently, the problem of congenital malformations is relevant in many branches of medicine. According to long-term observation, more than 5.5% of children with congenital malformations are born in the world, mortality among newborns from congenital malformations is about 30% (up to 270 thousand children die annually under the age of 28 days of life). In the structure of perinatal mortality, congenital malformations in full-term children occupy the first place. About 10% of conceptions in the human population are accompanied by congenital anomalies in the development of the fetus. Approximately 0.5% of cases are chromosomal diseases, 0.7% are molecular pathologies, 1.8% are hereditary polygenic diseases, and about 7% are hereditary predispositions.
The viability of children with combined congenital malformations is increasingly considered as the main criterion in assessing the state of health. Despite the progress made in improving the quality of modern surgical care and intensive care for young children, the results of treatment, unfortunately, are not always encouraging.
When analyzing a diagnostic study of a detected birth defect in a newborn, a neonatologist must highlight the type of this pathology, its causes, belonging to a particular syndrome, and how often this defect is accompanied by other congenital diseases.
Congenital anomalies in the development of a child can be hereditary (due to gene mutations and chromosomal pathologies), teratogenic (acquired during pregnancy) and multifactorial (a combination of the first two factors). Of the various hereditary defects, a fairly common chromosomal disease should be distinguished - Down syndrome , in which the characteristic appearance of the child indicates his physical and mental retardation. Endocrine and hormonal pathologies of a pregnant woman, injuries during childbearing, oligohydramnios, viral diseases (rubella, influenza), intoxication of the body with chemicals, the intake of antidepressants, antibiotics, anticonvulsants by the expectant mother lead to deviations in the intrauterine development of the fetus.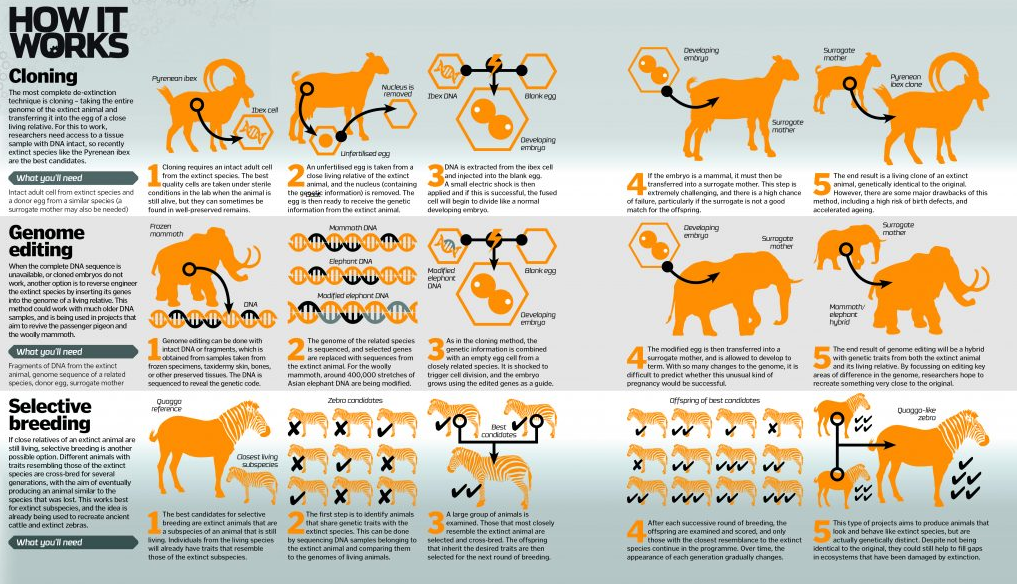 And sometimes the true causes of congenital anomalies are not possible for embryologists, geneticists and neonatologists to establish at all.
And sometimes the true causes of congenital anomalies are not possible for embryologists, geneticists and neonatologists to establish at all.
There are a great many pathological deviations in the development of children, since absolutely any organ of a child can undergo an abnormal anatomical structure or a degenerative-dystrophic condition. A common anomaly is congenital heart disease, accompanied by defects in the interventricular and interatrial septum, stenosis (narrowing) of the aortic valve, which lead to a change in intracardiac hemodynamics. Renal congenital pathologies are also common: fusion, absence of one kidney ( agenesis ), or the appearance of a third. There are known cases of abnormal elongation and thickening of the large intestine ( Hirschsprung's disease ), the occurrence of diaphragmatic hernia, the absence of testicles in the scrotum ( cryptorchidism ).
Of course, the external manifestations of childhood malformations look very unsightly.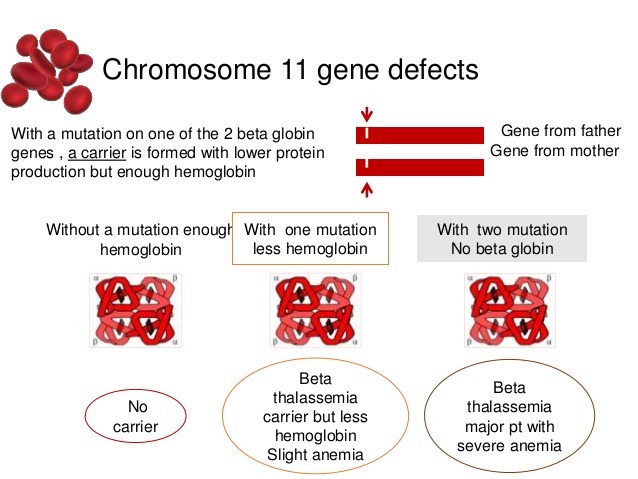 A child can be born with deformed or abnormally short upper and lower limbs ( clubfoot, lameness ), congenital dislocation of the hip, cleft lip, cleft palate, protruding chest, pathological curves of the spine. Often, melanin pigment is completely absent in the skin ( albinism ), so the child is contraindicated in sun exposure. Sometimes there is an increased number ( polydactyly ) of fingers and toes or their fusion ( syndactyly ), the absence of an anus opening ( atresia ), a decrease in the size of the skull ( microcephaly ), drooping of the upper eyelid ( itosis ) .
A child can be born with deformed or abnormally short upper and lower limbs ( clubfoot, lameness ), congenital dislocation of the hip, cleft lip, cleft palate, protruding chest, pathological curves of the spine. Often, melanin pigment is completely absent in the skin ( albinism ), so the child is contraindicated in sun exposure. Sometimes there is an increased number ( polydactyly ) of fingers and toes or their fusion ( syndactyly ), the absence of an anus opening ( atresia ), a decrease in the size of the skull ( microcephaly ), drooping of the upper eyelid ( itosis ) .
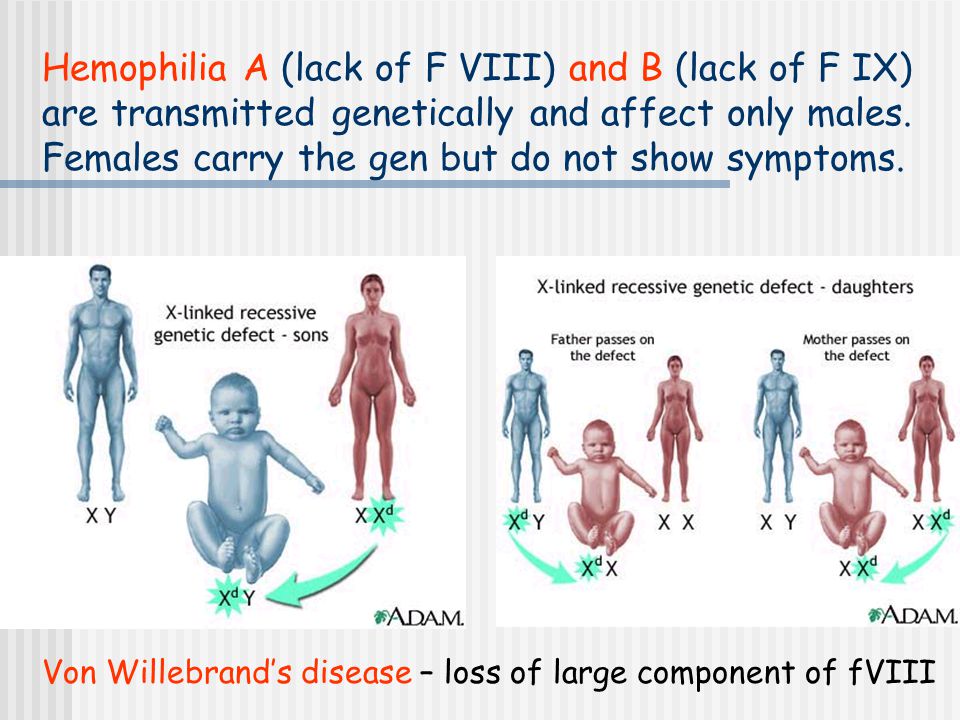
It should be noted that the numerous list of congenital malformations includes such diseases as a violation of the blood clotting factor ( hemophilia ), color blindness ( color blindness ), spina bifida ( spina bifida ). Many of these pathologies are treatable, some of them lead to lifelong disability, but, unfortunately, there are defects in which the child is not viable. These include the complete absence of lungs or kidneys, skin ( acrania ), or cerebral hemispheres (anencephaly ).
These include the complete absence of lungs or kidneys, skin ( acrania ), or cerebral hemispheres (anencephaly ).
Congenital malformations in children can develop immediately after fertilization, occur in the first weeks of pregnancy, or at later stages of bearing a child. In this regard, pregnancy planning and prenatal diagnosis (medical genetic counseling), which involves a comprehensive examination of the health status of both spouses, are of great importance. This is especially true of persons in whose families people with abnormal deviations were previously born. Of course, today medicine has reached unprecedented heights, but it is better not to tempt fate and take care of the health of the unborn child long before pregnancy.
Each gene in the human body is responsible for the production of a specific protein. Due to the manifestation of a damaged gene, the synthesis of an abnormal protein begins, which leads to cell dysfunction and developmental defects.
A doctor can determine the risk of a possible genetic anomaly by asking you about the diseases of relatives “up to the third generation”, both on your side and on the side of your husband.
Turner Syndrome is a disorder affecting girls characterized by the partial or complete absence of one or two X chromosomes. The disease occurs in one in 3,000 girls. Girls with this disease are usually very small and their ovaries do not function.
Trisomy X Syndrome is a condition in which a girl is born with three X chromosomes. This disease occurs in an average of one in 1000 girls. The X-trisomy syndrome is characterized by a slight mental retardation and, in some cases, infertility.
Klinefelter's syndrome is a condition in which a boy has one extra chromosome. The disease occurs in one boy out of 700. Patients with Klinefelter's syndrome, as a rule, are tall, there are no noticeable external developmental anomalies (after puberty, facial hair growth is difficult and the mammary glands are somewhat enlarged).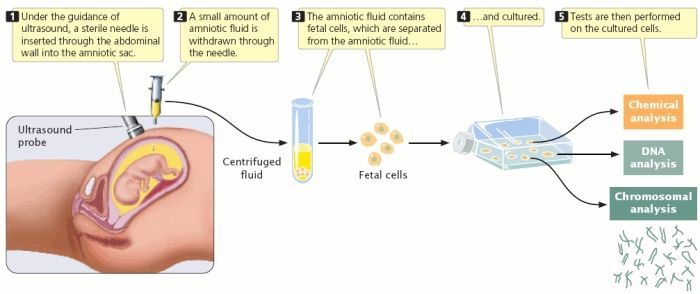 Intellect in patients is usually normal, but speech disorders are common. Men with Klinefelter syndrome are usually infertile.
Intellect in patients is usually normal, but speech disorders are common. Men with Klinefelter syndrome are usually infertile.
Cystic fibrosis is a genetic disease in which the functions of many glands are impaired. Cystic fibrosis only affects Caucasians. Approximately one in 20 white people has one damaged gene that, if manifested, can cause cystic fibrosis. The disease occurs when a person receives two of these genes (from the father and from the mother). In Russia, cystic fibrosis, according to various sources, occurs in one newborn out of 3500-5400, in the USA - in one out of 2500. With this disease, the gene responsible for the production of a protein that regulates the movement of sodium and chlorine through cell membranes is damaged. There is dehydration and an increase in the viscosity of the secretion of the glands. As a result, a thick secret blocks their activity. In patients with cystic fibrosis, protein and fat are poorly absorbed, as a result, growth and weight gain are greatly slowed down.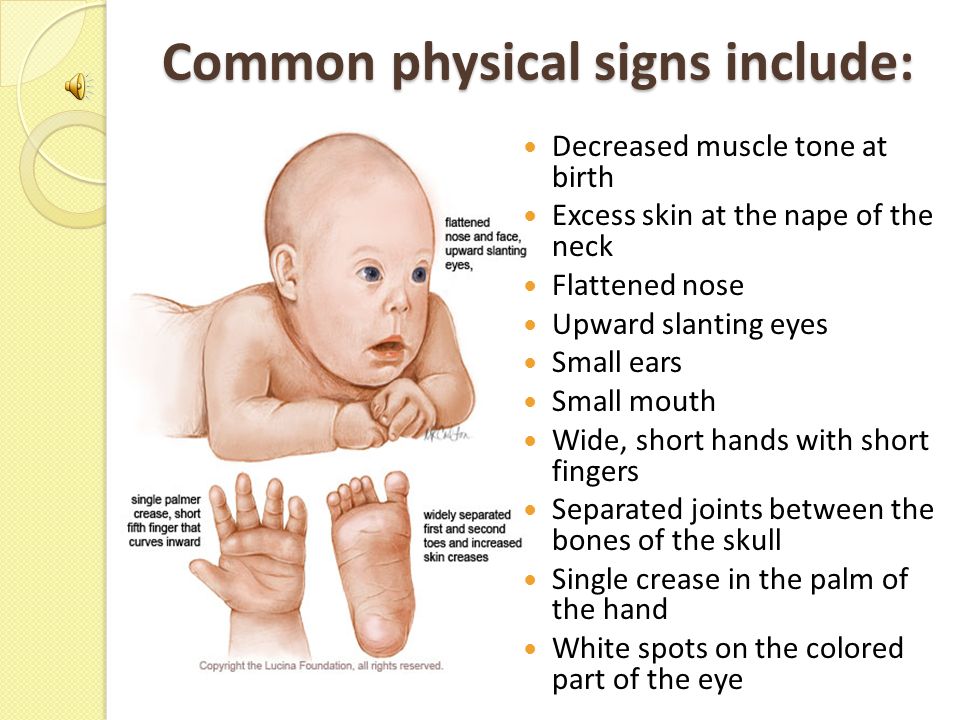 Modern methods of treatment (taking enzymes, vitamins and a special diet) allow half of the patients with cystic fibrosis to live more than 28 years.
Modern methods of treatment (taking enzymes, vitamins and a special diet) allow half of the patients with cystic fibrosis to live more than 28 years.
Hemophilia is a genetic disease characterized by increased bleeding due to a deficiency of one of the blood coagulation factors. The disease is inherited through the female line, while it affects the vast majority of boys (an average of one in 8500). Hemophilia occurs when the genes responsible for the activity of blood clotting factors are damaged. With hemophilia, frequent hemorrhages in the joints and muscles are observed, which can ultimately lead to their significant deformation (that is, to a person's disability). People with hemophilia should avoid situations that could lead to bleeding. Patients with hemophilia should not take drugs that reduce blood clotting (for example, aspirin, heparin, and some painkillers). To prevent or stop bleeding, the patient is given a plasma concentrate containing a large amount of the missing clotting factor.![]()
Tay Sachs disease is a genetic disease characterized by the accumulation of phytanic acid (a product of the breakdown of fats) in tissues. The disease occurs mainly among Ashkenazi Jews and Canadians of French origin (in one newborn in 3600). Children with Tay-Sachs disease are retarded from an early age, then they become paralyzed and blind. As a rule, patients live up to 3-4 years. There are no treatments for this disease.
It is believed that the probability of having a baby with a congenital or hereditary pathology, the so-called population or general statistical risk, is approximately 3-5% for each pregnant woman. In rare cases, the probability of the birth of a child with a genetic disease can be predicted and the pathology can be diagnosed already in the period of intrauterine development of the child. Certain congenital malformations and diseases are established using laboratory biochemical, cytogenetic and molecular genetic methods even in the fetus, since some diseases are detected during a complex of prenatal (prenatal) diagnostic methods.