Pregnancy miscarriage types
Miscarriage | Pregnancy Birth and Baby
The loss of a baby through miscarriage can be very distressing. A miscarriage generally occurs for reasons outside your control and nothing can be done to prevent or stop it from happening. Most women who have had a miscarriage will go on to have a healthy pregnancy in the future.
What is a miscarriage?
A miscarriage is the loss of your baby before 20 weeks of pregnancy. The loss of a baby after 20 weeks is called a stillbirth.
Up to 1 in 5 confirmed pregnancies end in miscarriage before 20 weeks, but many other women miscarry without having realised they are pregnant.
Common signs of miscarriage include:
- cramping tummy pain, similar to period pain
- vaginal bleeding
If you think you are having a miscarriage, see your doctor or go to your local emergency department.
Many women experience vaginal spotting in the first trimester that does not result in pregnancy loss.
What are the types of miscarriage?
There are several types of miscarriage — threatened, inevitable, complete, incomplete or missed.
Other types of pregnancy loss include an ectopic pregnancy, molar pregnancy and a blighted ovum.
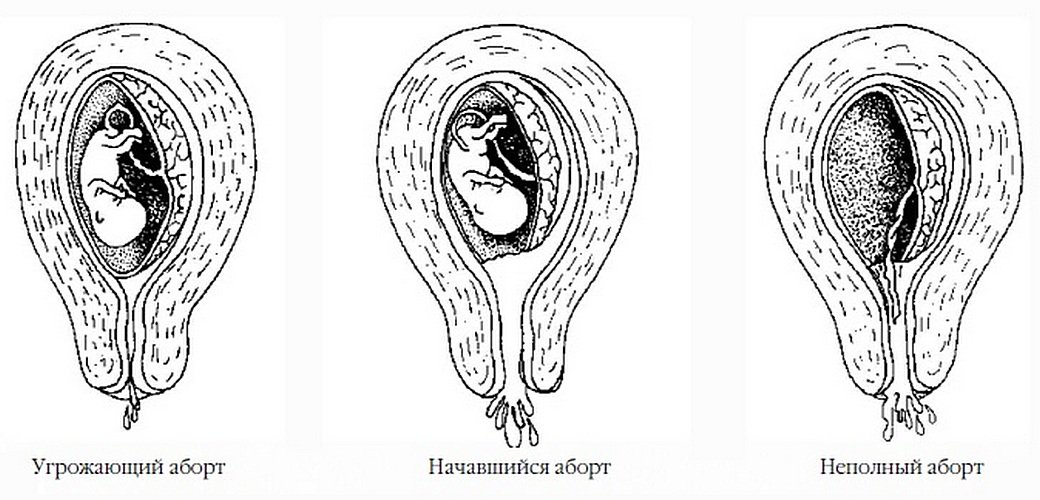
Threatened miscarriage
When your body is showing signs that you might miscarry, that is called a 'threatened miscarriage'. You may have light vaginal bleeding or lower abdominal pain. It can last days or weeks and the cervix is still closed.
The pain and bleeding may resolve and you can go on to have a healthy pregnancy and baby. Or things may get worse and you go on to have a miscarriage.
There is rarely anything a doctor, midwife or you can do to prevent a miscarriage. In the past bed rest was recommended, but there is no scientific proof that this helps at this stage.
Inevitable miscarriage
Inevitable miscarriages can come after a threatened miscarriage or without warning. There is usually a lot more vaginal bleeding and strong lower stomach cramps. During the miscarriage your cervix opens and the developing fetus will come away in the bleeding.
Complete miscarriage
A complete miscarriage has taken place when all the pregnancy tissue has left your uterus. Vaginal bleeding may continue for several days. Cramping pain much like labour or strong period pain is common — this is the uterus contracting to empty.
If you have miscarried at home or somewhere else with no health workers present, you should have a check-up with a doctor or midwife to make sure the miscarriage is complete.
Incomplete miscarriage
Sometimes, some pregnancy tissue will remain in the uterus. Vaginal bleeding and lower abdominal cramping may continue as the uterus continues trying to empty itself. This is known as an 'incomplete miscarriage'.
Your doctor or midwife will need to assess whether or not a short procedure called a ‘dilatation of the cervix and curettage of the uterus’ (often known as a ‘D&C’) is necessary to remove any remaining pregnancy tissue. This is an important medical procedure done in an operating theatre.
Missed miscarriage
Sometimes, the fetus has died but stayed in the uterus. This is known as a 'missed miscarriage'.
If you have a missed miscarriage, you may have a brownish discharge. Some of the symptoms of pregnancy, such as nausea and tiredness, may have faded. You might have noticed nothing unusual. You may be shocked to have a scan and find the fetus has died.
If this happens, you should discuss treatment and support options with your doctor.
Recurrent miscarriage
A small number of women have repeated miscarriages. If this is your third or more miscarriage in a row, it’s best to discuss this with your doctor who may be able to investigate the causes, and refer you to a specialist.
A miscarriage can occur suddenly or over a number of weeks. The symptoms are usually vaginal bleeding and lower tummy pain. It is important to see your doctor or go to the emergency department if you have signs of a miscarriage.
The most common sign of a miscarriage is vaginal bleeding, which can vary from light red or brown spotting to heavy bleeding. If it is very early in the pregnancy, you may think that you have your period.
If it is very early in the pregnancy, you may think that you have your period.
Other signs may include:
- cramping pain in your lower tummy, which can vary from period-like pain to strong labour-like contractions
- passing fluid from your vagina
- passing of blood clots or pregnancy tissue from your vagina
What really happens during a miscarriage?
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
What should I do if I think I’m having a miscarriage?
If you are concerned that you are having a miscarriage, call your doctor or midwife for advice and support.
Keep in mind that many women experience vaginal spotting in the first trimester of pregnancy that does not result in a miscarriage.
If you are alone, consider calling your partner or a friend for help and support.
If you have very heavy bleeding, strong pain or feel unwell, call triple zero (000) or have someone take you to your nearest emergency department.
How is a miscarriage managed?
Unfortunately, nothing can prevent a miscarriage from happening once it has begun. What happens now depends on your own health and what is happening to you.
Each approach has benefits and risks. You should discuss these with your doctor.
Expectant or natural management
Also called ‘watch and wait’, expectant management may be recommended in early pregnancy. This involves going home and waiting until the pregnancy tissue has passed from your womb by itself. This can happen quickly, or it may take a few weeks.
Medical management
You may be offered medication that speeds up the passing of the pregnancy tissue. You may be asked to stay in hospital until the tissue has passed, or you may be advised to go home.
Surgical management
You may be advised to have a form of minor surgery called a 'dilatation and curettage' (also called a D&C or a curette). This procedure is often recommended if you have heavy bleeding, significant pain or signs of infection. It may also be recommended if expectant or medical management has failed. You may also decide that you prefer this option.
It may also be recommended if expectant or medical management has failed. You may also decide that you prefer this option.
This procedure is done under general anaesthesia in an operating theatre. It takes 5-10 minutes once you are asleep. The doctor opens the cervix and removes the remaining pregnancy tissue.
How is a miscarriage treated?
Once it is confirmed that you are having a miscarriage, your doctor may offer or recommend treatment. There are many options. All have benefits and risks — discuss these with your doctor.
If the miscarriage is complete
If it seems the miscarriage is complete, you should still see your doctor for a check-up. You may be advised to have an ultrasound to make sure your uterus is empty.
If you go to hospital
If you go to your hospital’s emergency department, you will be seen first by a triage nurse, who will assess how urgently you need to be seen by a doctor. Depending on your symptoms, you will either be taken in to see a doctor immediately, or you will be asked to wait.
If you are waiting to be seen and your symptoms become worse or you feel like you need to go to the toilet, let the staff know immediately.
What happens if I miscarry at home?
Some women miscarry at home before they have a chance to see their doctor or get to the hospital.
If this happens, then:
- use pads to manage the bleeding
- if you can, save any pregnancy tissue that you pass, as your doctor may recommend it is tested to see why your miscarriage happened
- take medications such as paracetamol if you have pain
- rest
- call your doctor or midwife
There is a chance you may see your baby in the tissue that you pass, but often the baby is too small to recognise, or may not be found at all. It is normal to want to look at the remains, but you may decide you do not want to. There is no right or wrong thing to do.
Some women miscarry while on the toilet. This can also happen if you are out and about, or in hospital. There is no right or wrong way to handle this.
There is no right or wrong way to handle this.
Why do miscarriages happen?
Many women wonder if their miscarriage was their fault. In most cases, a miscarriage has nothing to do with anything you have or have not done. There is no evidence that exercising, stress, working or having sex causes a miscarriage.
Most parents do not ever find out the exact cause. However, it is known that miscarriages often happen because the baby fails to develop properly, usually due to a chromosomal abnormality that was spontaneous, not inherited.
Occasionally, miscarriage is caused by:
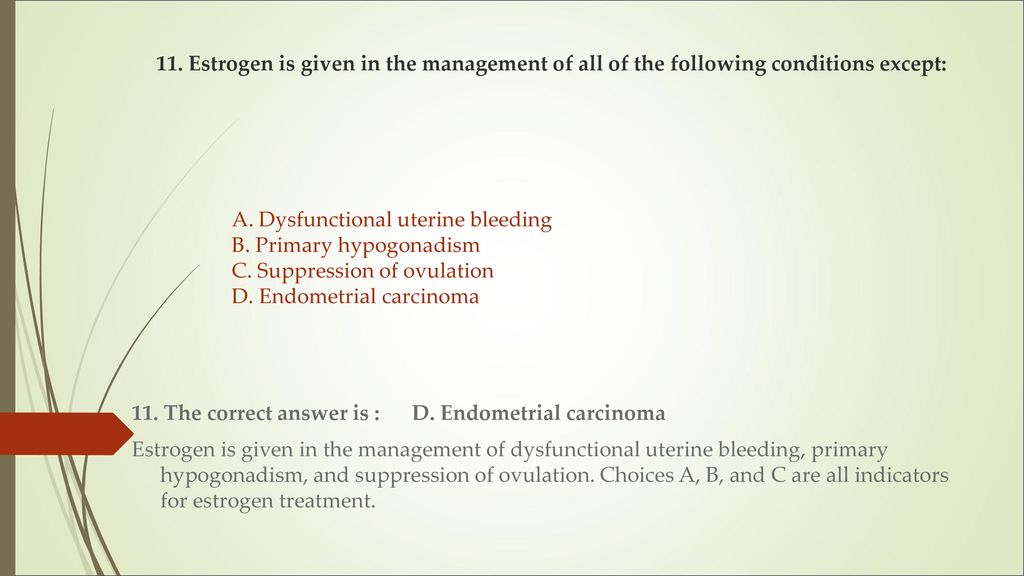
- hormonal abnormalities
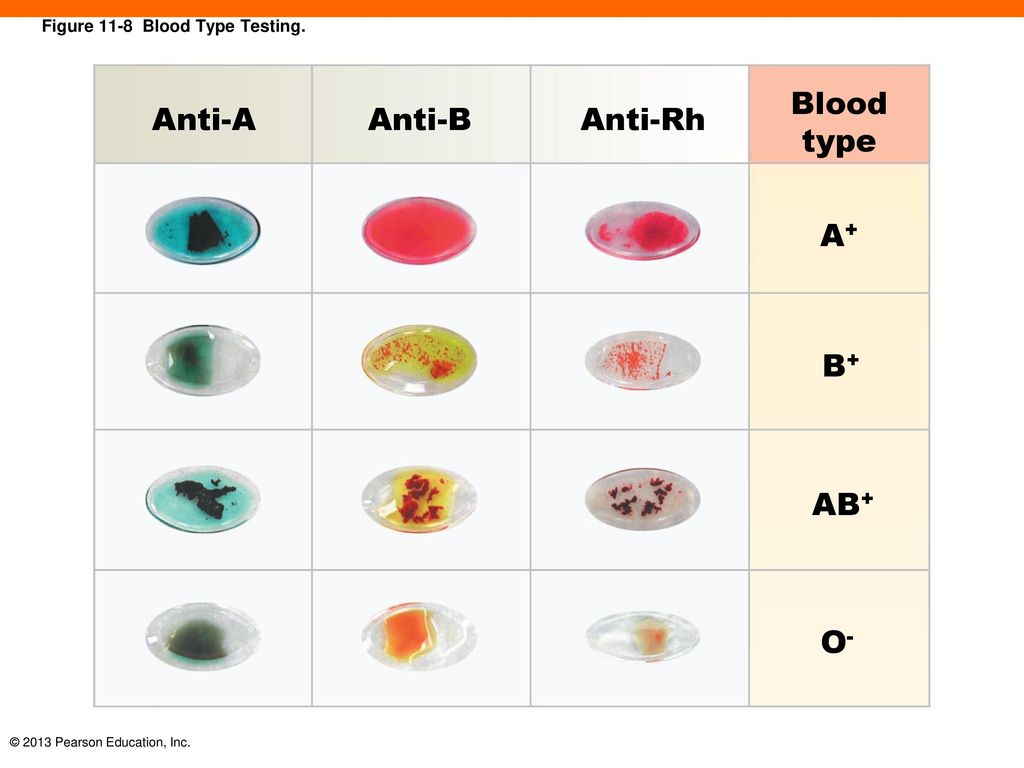
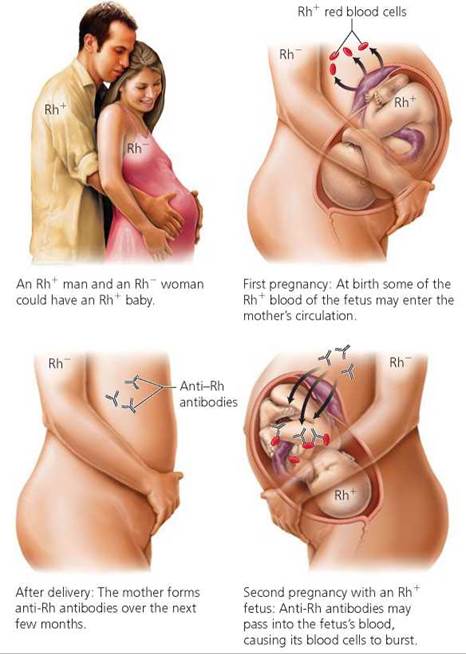
- immune system and blood clotting problems
- medical conditions such as thyroid problems or diabetes
- severe infections causing high fevers (not common colds)
- physical problems with your womb or cervix
What are the risk factors for miscarriage?
Women are more likely to have miscarriages if they:
- are older
- smoke
- drink alcohol in the first trimester
- drink too much caffeine in coffee, tea or energy drinks
- have had several previous miscarriages
Can you prevent a miscarriage?
Living healthily — no cigarettes, no alcohol and little to no caffeine — can decrease your risk of miscarriage.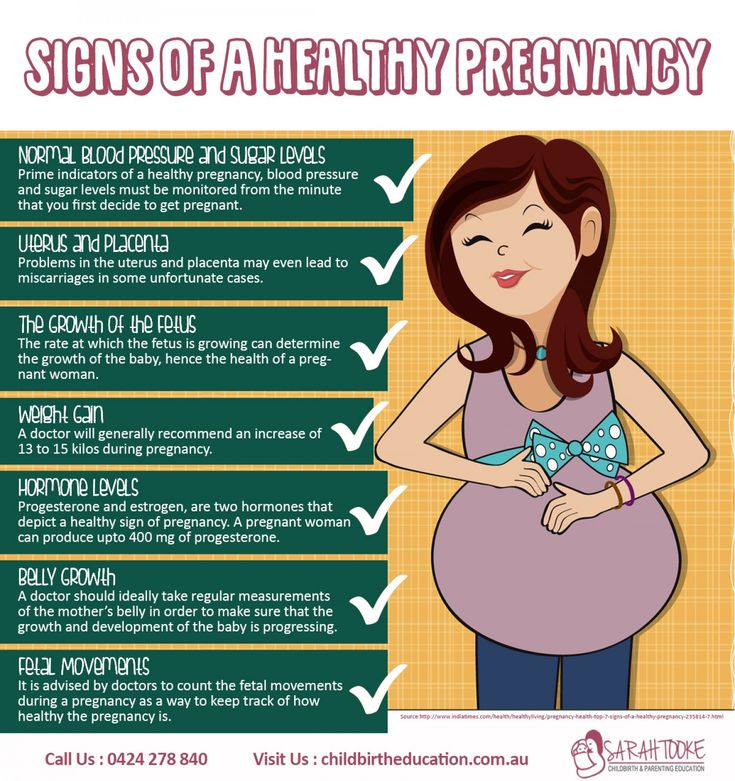 It’s a good idea to avoid contact with people who have a serious infectious illness when you’re pregnant.
It’s a good idea to avoid contact with people who have a serious infectious illness when you’re pregnant.
Who can I talk to for advice and support?
Talk to your doctor or midwife for information and advice on what do and how to look after yourself if you experience a miscarriage.
Your hospital should be able to provide details of available support services, such as bereavement support.
SANDS is an independent organisation that provides support for miscarriage, stillbirth and newborn death. You can call them on 1300 072 637 or visit www.sands.org.au.
You can also call Pregnancy, Birth and Baby on 1800 882 436, 7am to midnight (AET) to speak to a maternal child health nurse for advice and emotional support.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.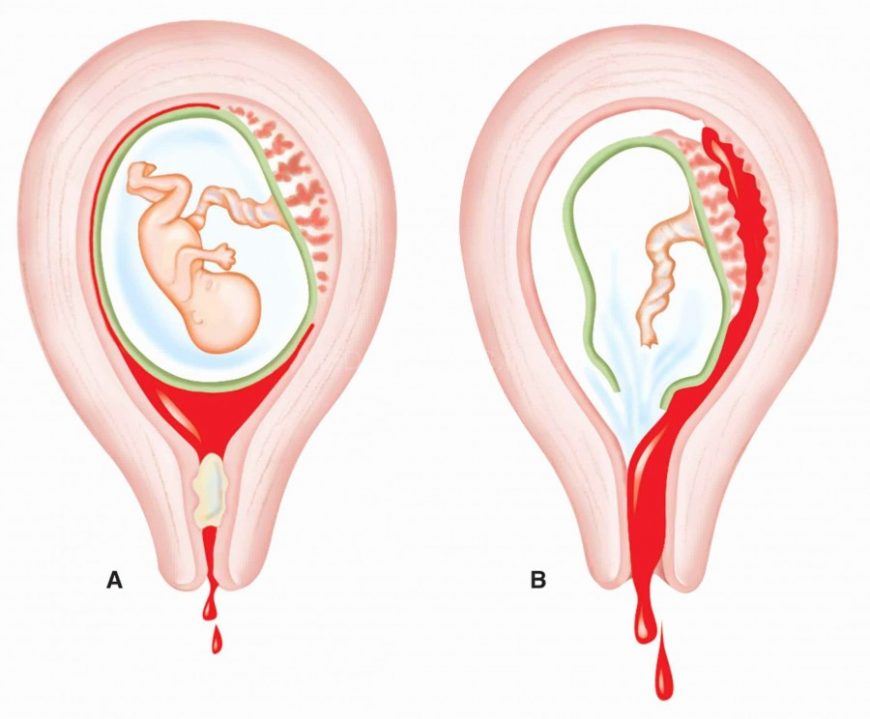
What Are the Different Types of Miscarriage?
A miscarriage, or “spontaneous abortion,” refers to the loss of a pregnancy before 20 weeks and occurs in 15 to 20 percent of all pregnancies. Most miscarriages occur during the first trimester but can also occur later on in the pregnancy.
Different types of miscarriages can occur at different stages of your pregnancy. The symptoms and treatments will depend on the type of miscarriage. Learn more about the different stages, signs and symptoms of, and treatment for miscarriage:
Chemical Pregnancy
A chemical pregnancy is a very early miscarriage which can occur before you even learn that you’re pregnant. As pregnancy tests have become more sensitive and more common, an increased number of chemical pregnancies have been diagnosed.
Chemical pregnancy is most likely the result of chromosomal abnormalities in the fertilized egg. An egg is fertilized, but is non-viable shortly after implantation, and is never visible on ultrasound.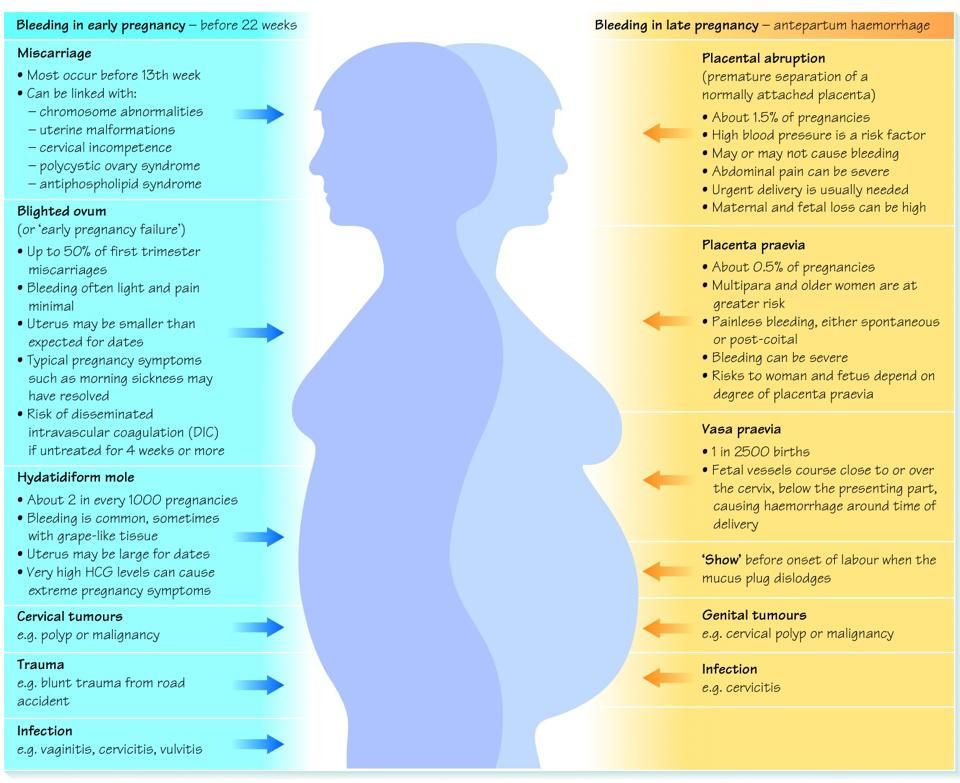
Signs and Symptoms: There may be no signs of a chemical pregnancy. Most women simply begin to bleed around the time of their next period, though their period may arrive a few days late or be slightly heavier.
Blighted Ovum
Also known as anembryonic pregnancy, blighted ovum occurs very early in pregnancy, often before you even know you are pregnant. A fertilized egg attaches to the uterine wall, but an embryo does not develop.
Signs and Symptoms: You may feel signs of pregnancy, but when your doctor performs an ultrasound, he or she finds an empty gestational sac or cannot confirm a heartbeat.
You may miscarry the pregnancy or schedule a dilation and curettage (D&C) procedure, in which the cervix is opened, and the pregnancy is gently curetted, or removed, from the uterus.
Missed Miscarriage
A missed miscarriage, or a missed abortion, occurs when a fetus implants, but fails to develop.
The body does not expel the pregnancy tissue.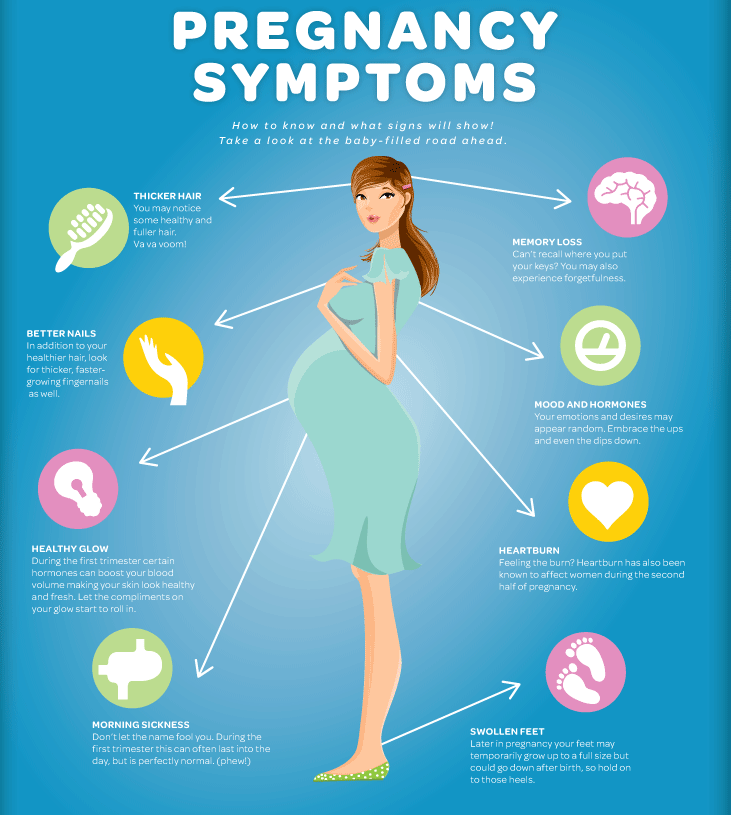
Signs and Symptoms: You may continue to feel signs of pregnancy if the placenta still releases hormones. Or, you may notice signs of pregnancy fade. Some women may experience some vaginal discharge and cramping, but many have no symptoms of miscarriage.
Sometimes the body will dispel the fetal tissue, but other times, a D&C procedure is necessary.
Threatened Miscarriage
A threatened miscarriage refers to vaginal bleeding that occurs during the first 20 weeks of pregnancy. It does not necessarily mean your pregnancy will end in a miscarriage — around half of threatened miscarriages result in a live birth.
Signs and Symptoms: Other symptoms of threatened miscarriage include lower back pain and abdominal cramps. If you have experienced unexplained bleeding during pregnancy, your doctor will want to perform an examination.
Cervix Dilation: In a threatened miscarriage, the cervix will remain closed. However, if an examination reveals the cervix has opened, a miscarriage is much more likely.
Inevitable Miscarriage
Inevitable miscarriage refers to unexplained vaginal bleeding and abdominal pain during early pregnancy.
Signs and Symptoms: Bleeding is heavier than with a threatened miscarriage and abdominal cramps more severe. Unlike threatened miscarriage, an inevitable miscarriage is also accompanied by dilation of the cervical canal. The open cervix is a sign that the body is in the process of miscarrying the pregnancy.
Incomplete Abortion
An incomplete abortion, which is also called an incomplete miscarriage, happens when some—but not all—of the pregnancy tissue is passed.
Signs and Symptoms: It is often accompanied by heavy vaginal bleeding and intense abdominal pain. The cervix will be open, and some remaining pregnancy tissue will be found in the uterus during an examination.
Complete Miscarriage
A complete miscarriage, also called a complete abortion, refers to a miscarriage in which all of the pregnancy tissue is expelled from the uterus.
Signs & Symptoms: A complete miscarriage is characterized by heavy vaginal bleeding, severe abdominal pain, and passage of pregnancy tissue. With a complete miscarriage, the bleeding and pain should subside quickly. Complete miscarriages can be confirmed through an ultrasound.
Dr. Alan Copperman is a board-certified reproductive endocrinologist and infertility specialist with a long history of success in treating infertility and applying fertility preservation technologies. He serves as Medical Director of Progyny, a leading fertility benefits management company, and co-founded and serves as Medical Director of RMA of New York, one of the largest and most prestigious IVF centers in the country. Dr. Copperman is also the Vice Chairman and Director of Infertility for the Icahn School of Medicine at Mount Sinai, and Chief Medical Officer of Sema4, a health information company. Dr. Copperman has been named to New York magazine’s list of Best Doctors 17 years in a row.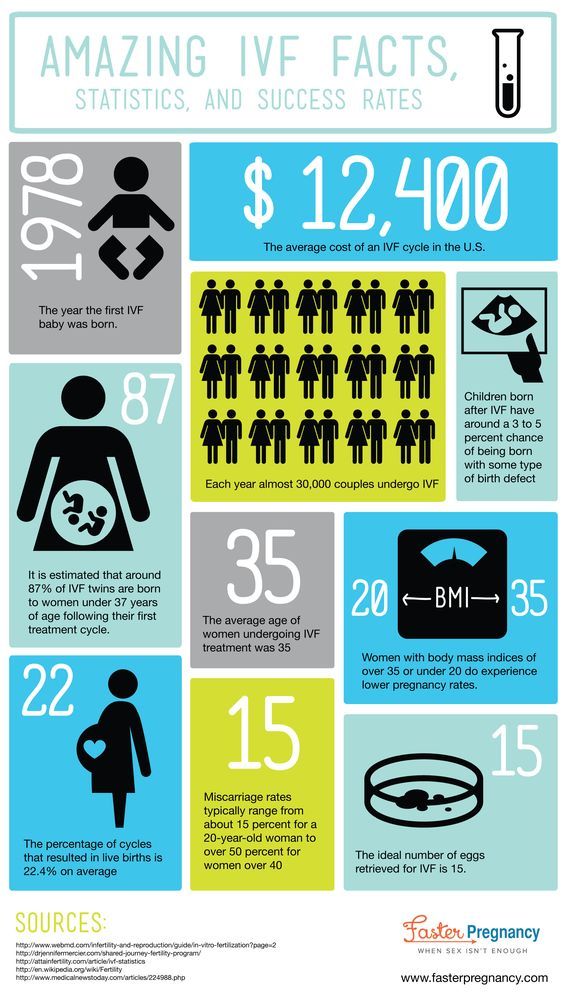 He has been recognized by his peers and patient advocacy organizations for his commitment to patient-focused and data-driven care. He has published more than 100 original manuscripts and book chapters on reproductive medicine and has co-authored over 300 scientific abstracts on infertility, in vitro fertilization, egg freezing, ovum donation, and reproductive genetics.
He has been recognized by his peers and patient advocacy organizations for his commitment to patient-focused and data-driven care. He has published more than 100 original manuscripts and book chapters on reproductive medicine and has co-authored over 300 scientific abstracts on infertility, in vitro fertilization, egg freezing, ovum donation, and reproductive genetics.
Miscarriage
Miscarriage is a spontaneous premature termination of pregnancy for a period of less than 20 weeks, that is, during the period when the embryo or fetus cannot yet survive on its own outside the female body. This is the most common complication of the first trimester of pregnancy.
Approximately 10-20% of all pregnancies end in miscarriage. Most often, spontaneous abortion occurs in the first 12 weeks. In some cases, the pregnancy is terminated before the woman even knows about its existence.
The risk of miscarriage increases with age: in women younger than 35 years old it is 15%, from 35 to 45 years old - 20-35%, over 45 years old - more than 50%. Women who have had a miscarriage in the past have an increased risk of spontaneous abortion. However, if a woman is healthy and re-pregnancy occurs 2-3 months after a spontaneous abortion, then it most often ends safely.
Women who have had a miscarriage in the past have an increased risk of spontaneous abortion. However, if a woman is healthy and re-pregnancy occurs 2-3 months after a spontaneous abortion, then it most often ends safely.
If a woman experiences three or more spontaneous abortions, then this condition is called recurrent miscarriage. It is diagnosed in approximately 1% of women who have had a spontaneous abortion. Identification of the immediate cause of recurrent miscarriage and appropriate treatment allows most patients to subsequently become pregnant and give birth to a healthy child.
Russian synonyms
Spontaneous abortion, spontaneous abortion.
Synonyms English
Miscarriage, early miscarriage, recurrent miscarriage, spontaneous abortion.
Symptoms
Symptoms of miscarriage can be both almost imperceptible and pronounced. The duration of manifestations can also vary. In some cases, the main symptoms are preceded by a period of non-specific manifestations: there may be weight loss, weakness, back pain, bloody or mucous discharge from the genitals.
In some cases, the main symptoms are preceded by a period of non-specific manifestations: there may be weight loss, weakness, back pain, bloody or mucous discharge from the genitals.
The main symptoms of miscarriage are:
- bleeding from the genitals;
- abdominal pain;
- contractions.
Other complications of pregnancy, such as ectopic pregnancy, may have similar symptoms. Therefore, in case of any violations, it is necessary to consult a doctor as soon as possible to identify the cause of the pathology and timely treatment.
General information about the disease
Miscarriage occurs quite often, and in many cases it is impossible to determine the cause of this pathology. There are several groups of factors that can lead to spontaneous abortion.
- Chromosomal disorders in embryonic cells. Chromosomes are cellular structures that contain genetic information. Chromosomal abnormalities incompatible with life cause spontaneous abortion in the early stages of pregnancy.
 More than half of the cases of miscarriage in the first trimester is associated with them. The risk of genetic abnormalities increases in proportion to the age of the mother.
More than half of the cases of miscarriage in the first trimester is associated with them. The risk of genetic abnormalities increases in proportion to the age of the mother. - Maternal pathology. Most often, maternal illness leads to miscarriage between the 12th and 20th week of pregnancy. Allocate:
- Chronic maternal diseases: diabetes mellitus, thyroid disease, severe urinary and cardiovascular disorders, autoimmune diseases (antiphospholipid syndrome, systemic lupus erythematosus), blood clotting disorders (factor Leiden deficiency), as well as certain chromosomal abnormalities in the mother's body.
- Acute illness of the mother: severe trauma, burns, infections, in particular cytomegalovirus infection, mycoplasma, as well as severe emotional stress.
- Diseases and disorders of the structure of the genital organs of a woman: pathology of the structure of the uterus, cervical insufficiency, uterine fibromyoma. This group also includes anomalies in the structure and position of the placenta, as well as multiple pregnancy, which also increases the risk of miscarriage.
- Use of alcohol, psychoactive substances by a woman.
In the normal course of pregnancy in a healthy woman, moderate physical activity and sex cannot cause miscarriage. However, in some cases, in order to maintain pregnancy, the doctor may advise the patient to limit physical activity and stop sexual intercourse for a while.
There are the following types of miscarriage:
- Threatened spontaneous abortion. This term is used for any bleeding from the uterine cavity in the first half of pregnancy. At the same time, the external cervical os is closed and there are signs of the vital activity of the embryo.
- Inevitable abortion. It is diagnosed if bleeding from the uterine cavity is accompanied by the opening of the cervix, but the fetus and placenta are still in the uterine cavity.
- Incomplete abortion. A condition in which parts of the embryo or placenta are still in the uterine cavity.
- Complete abortion.
 With a complete abortion, all components of the fetus, placenta, membranes are completely expelled from the uterine cavity.
With a complete abortion, all components of the fetus, placenta, membranes are completely expelled from the uterine cavity. - Frozen pregnancy. A condition in which intrauterine fetal death occurs, but neither the fetus nor the placenta is expelled from the uterine cavity.
Who is at risk?
- Women over 35
- Women who have had a spontaneous abortion in the past
- Women with chronic diseases
- Women with acute infectious pathology, injuries, exhaustion, exposed to ionizing radiation
- Women who smoke and use alcohol and/or drugs
- Women with multiple pregnancies
Diagnosis
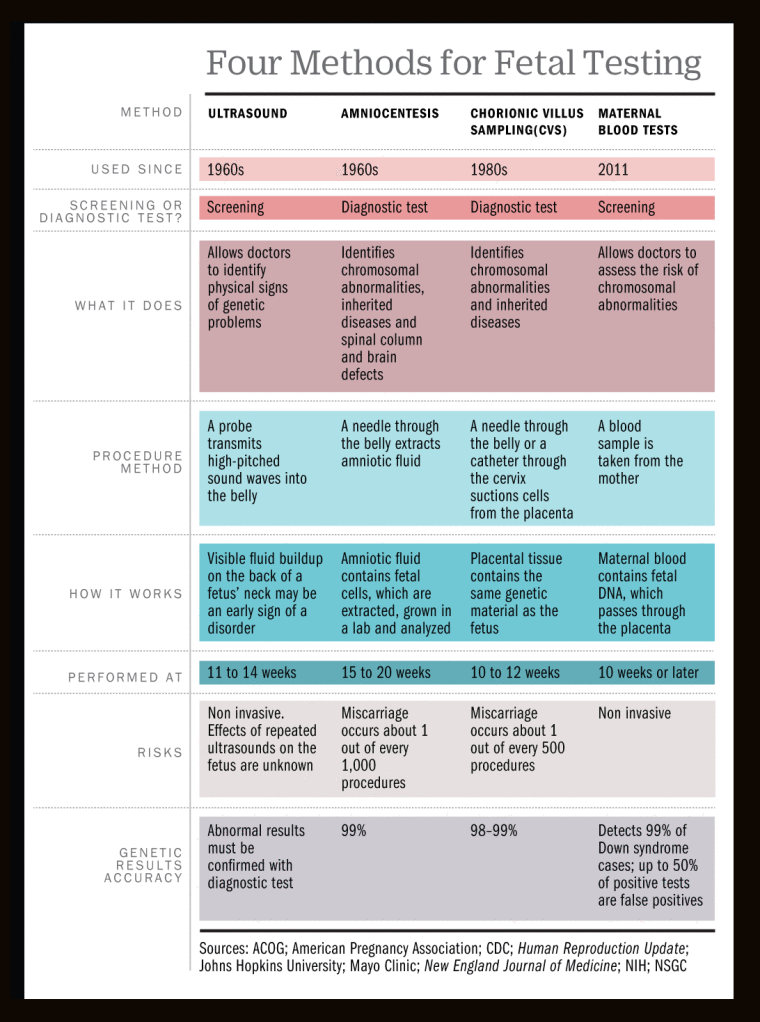
If a spontaneous abortion is suspected, the doctor first of all performs a gynecological examination and ultrasound examination of the pelvic organs, which allows assessing the condition of the uterus, its cervix, the presence of elements of the fetus and placenta in its cavity. Sometimes, to monitor the course of pregnancy, as well as to identify the causes of miscarriage, a number of additional laboratory and instrumental studies may be required.
Sometimes, to monitor the course of pregnancy, as well as to identify the causes of miscarriage, a number of additional laboratory and instrumental studies may be required.
Laboratory diagnostics
- Complete blood count with leukocyte formula, erythrocyte sedimentation rate (ESR). These indicators allow you to assess the general condition of the patient, identify signs of anemia, infection and other diseases that affect the normal course of pregnancy.
- Urinalysis with microscopy, serum creatinine, serum urea. These studies allow you to evaluate the functioning of the urinary system and identify kidney diseases that can cause spontaneous abortion.
- Hemostasiology studies that assess the activity of the blood coagulation and anticoagulation system, identify diseases that increase the risk of miscarriage:
- D-dimer
- Activated partial thromboplastin time (APTT)
- Coagulogram No. 1 (prothrombin (according to Quick), INR)
- Fibrinogen
- Examination of liver functions.
 Allows you to identify signs of acute or chronic liver pathology:
Allows you to identify signs of acute or chronic liver pathology: - Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Total protein in serum
- Bilirubin total
- Bilirubin direct
- Plasma glucose. An increase in blood glucose levels can be a sign of diabetes, one of the main risk factors for miscarriage.
- Thyroid stimulating hormone (TSH). Allows you to evaluate the activity of the thyroid gland and signs of endocrine diseases that affect the course of pregnancy.
- Diagnosis of infectious diseases. The level of various types of antibodies to certain infections is determined:
- HIV 1, 2 Ag/Ab Combo (determination of antibodies to HIV types 1 and 2 and p24 antigen)
- anti-HCV, antibodies, express, ultra sensitive
- HBsAg, ultra sensitive
- Treponema pallidum, antibodies, hypersensitive
- Toxoplasma gondii, IgM
- Toxoplasma gondii, IgG (quantitative)
- Rubella Virus, IgM
- Rubella Virus, IgG (quantitative)
- Cytomegalovirus, IgM (quantitative)
- Cytomegalovirus, IgG
- Herpes Simplex Virus 1/2, IgM
- Herpes Simplex Virus 1/2, IgG
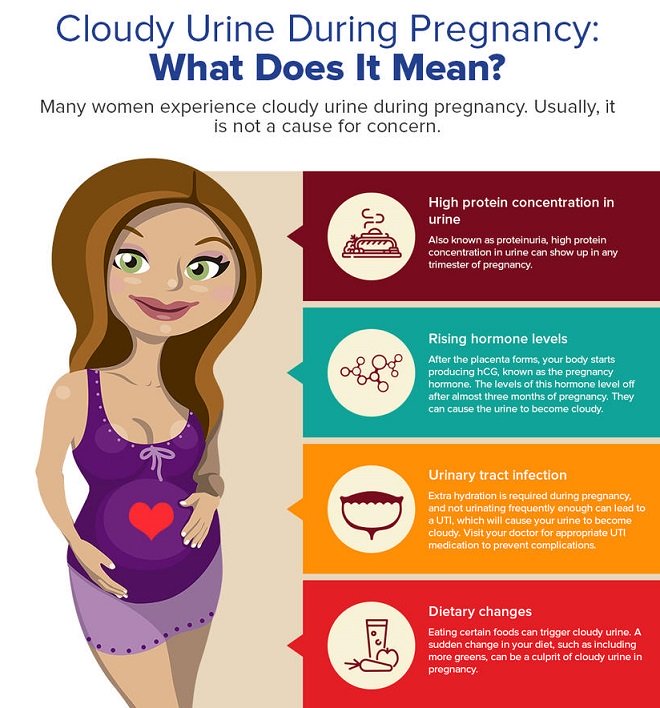
- Beta subunit of human chorionic gonadotropin (beta hCG).
 It is a glycoprotein synthesized by the placenta. A decrease in the level of beta-hCG, which does not correspond to the gestational age, makes it possible to suspect a pathology.
It is a glycoprotein synthesized by the placenta. A decrease in the level of beta-hCG, which does not correspond to the gestational age, makes it possible to suspect a pathology. - Diagnosis of antiphospholipid syndrome, which can cause miscarriage:
- Antiphospholipid IgG
- Antiphospholipid IgM
- Genetic research. Allow to identify chromosomal abnormalities in the mother, which can cause abnormal gametogenesis and, as a result, genetic abnormalities of the fetus that are incompatible with life. It is also possible to identify a genetic predisposition to early habitual pregnancy loss.
Instrumental methods of examination
Visual examination of the pelvic organs assesses the condition of the uterus, reveals anomalies in its structure, pathology of the reproductive system, establishes the presence or absence of elements of the placenta and embryo in the uterine cavity.
- Pelvic ultrasound
- Hysteroscopy
- Laparoscopy
Treatment
Treatment depends on the type of spontaneous abortion, the condition of the woman. With a complete spontaneous abortion, when there are no elements of the fetus and placenta in the uterus, additional intervention is usually not required. In case of incomplete abortion, it is necessary to remove all elements of the membranes, embryo and placenta from the uterine cavity. For this, curettage or, in some cases, drug treatment can be carried out.
With a complete spontaneous abortion, when there are no elements of the fetus and placenta in the uterus, additional intervention is usually not required. In case of incomplete abortion, it is necessary to remove all elements of the membranes, embryo and placenta from the uterine cavity. For this, curettage or, in some cases, drug treatment can be carried out.
If there is a threat of miscarriage and the preservation of signs of fetal vital activity, it is necessary to try to save the pregnancy. Depending on the severity of the condition, a woman may be admitted to a hospital or treated on an outpatient basis. The treatment regimen is selected by the doctor individually, depending on the cause of miscarriage, gestational age, the patient's condition and other factors.
Prevention
Prevention of miscarriage includes both parental care before conception and following certain recommendations after pregnancy. To reduce the risk of pregnancy termination, a pregnant woman should:
- give up alcohol, smoking, limit or stop drinking coffee and caffeinated drinks;
- regularly undergo preventive examinations;
- refrain from extreme sports that could result in serious injury;
- avoid ionizing radiation, contact with sources of infection.

Recommended tests
- CBC
- Leukocyte formula
- Erythrocyte sedimentation rate (ESR)
- Urinalysis with microscopy
- D-dimer
- Activated partial thromboplastin time (APTT)
- Coagulogram No. 1 (prothrombin (quick), INR)
- Fibrinogen
- Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Plasma glucose
- Serum creatinine
- Serum urea
- Total protein in serum
- Bilirubin total
- Bilirubin direct
- HIV 1, 2 Ag/Ab Combo (determination of antibodies to HIV types 1 and 2 and p24 antigen)
- anti-HCV, antibodies, express, ultra sensitive
- HBsAg, ultra sensitive
- Treponema pallidum, antibodies, hypersensitive
- Toxoplasma gondii, IgM
- Toxoplasma gondii, IgG (quantitative)
- Rubella Virus, IgM
- Rubella Virus, IgG (quantitative)
- Cytomegalovirus, IgM
- Cytomegalovirus, IgG
- Herpes Simplex Virus 1/2, IgM
- Herpes Simplex Virus 1/2, IgG
- Thyroid Stimulating Hormone (TSH)
- Pregnancy - I trimester
- Beta subunit of human chorionic gonadotropin (beta hCG)
- Antiphospholipid IgG
- Antiphospholipid IgM
- Predisposition to early habitual pregnancy loss
- Predisposition to early habitual pregnancy loss (extended)
Miscarriage, The role of IVF and PGD in prevention
Miscarriage is a spontaneous abortion that occurs at any time up to 22 weeks, later - miscarriage is classified as preterm birth. The percentage of pregnant women who, for one reason or another, experience non-embroidery fluctuates between 10-25%.
The percentage of pregnant women who, for one reason or another, experience non-embroidery fluctuates between 10-25%.
Successfully performed infertility treatment, unfortunately, does not always result in the birth of a child. The termination of a long-awaited pregnancy becomes a real tragedy for a married couple and for their doctor.
The reasons for early termination of pregnancy are often unknown, although chromosomal abnormalities are usually implied. If a woman has had a miscarriage in the second trimester or two or more in the first trimester, tests are recommended to help determine the cause.
Make an appointment
Most cases of miscarriage are observed in women who have been treated for infertility, including IVF. However, the IVF procedure itself cannot in any way be the cause of a miscarriage.
Causes of miscarriage:
Chromosomal problems
Up to 70% of all miscarriages occurring in the first trimester are due to abnormalities of the somatic chromosomes in the fetus. Most fetal chromosomal abnormalities result from the involvement of a defective egg or sperm in fertilization.
Most fetal chromosomal abnormalities result from the involvement of a defective egg or sperm in fertilization.
In such cases, the resulting embryo has a chromosomal abnormality, which leads to an undeveloped pregnancy. Chromosomal abnormalities increase with age.
Women over 35 have a higher risk of miscarriage than younger women. Recent studies show that a father's age over 40 also increases the risk of miscarriage.
Pathology of the uterus
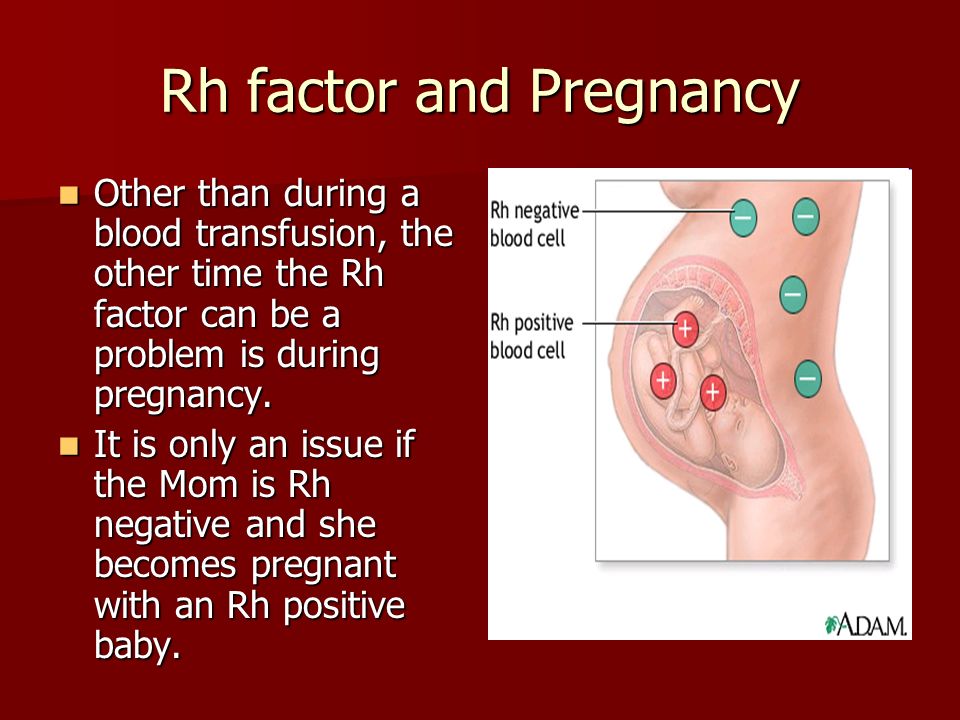
In 10-15% of cases, uterine anomalies (congenital malformations, septa in the uterine cavity, fibroids, adenomyosis, cicatricial postoperative changes) are the cause of miscarriage, both in the first and second trimesters.
Isthmic-cervical insufficiency (weakness of the muscular ring of the cervix) can lead to miscarriage, usually between 16 and 18 weeks of pregnancy.
Hormonal causes
If the body produces too much or too little of certain hormones, the risk of miscarriage increases. Hyperandrogenism, luteal phase deficiency, hypo- and hyperthyroidism, hyperprolactemia, diabetes mellitus can cause abortion.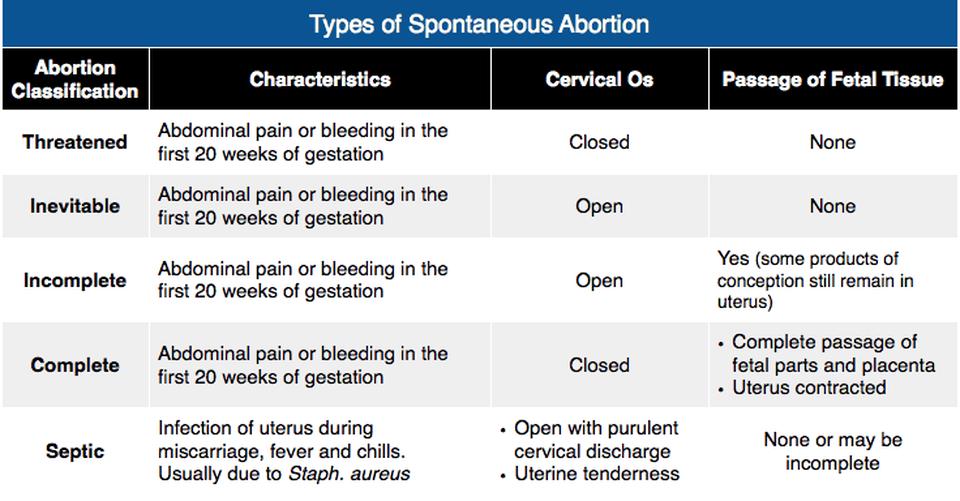
Autoimmune problems
While everyone's body makes proteins called antibodies to fight infections, some people's bodies produce antibodies (autoantibodies) that can attack the body's own tissues, causing a range of health problems.
They can cause infertility or miscarriage.
Certain types of autoantibodies (such as anticardiolipin or lupus anticoagulant) cause blood clots that can block the blood supply to the uterus. Mutations in the blood coagulation system can also be the cause of recurrent miscarriage.
Infections and other factors
Termination of pregnancy due to an inflammatory process is caused by the penetration of infectious agents from the mother's body through the placenta to the fetus. The infection is most dangerous during pregnancy.
The presence of microorganisms in the mother may be asymptomatic or accompanied by characteristic signs of an inflammatory disease. Bacteria (gram-negative and gram-positive cocci, listeria, treponema and mycobacteria), protozoa (toxoplasma, plasmodia) and viruses can enter the fetus from the mother.
Spouses should also discuss the possible impact of chemicals in their workplace with their doctor.
A woman is not advised to try to conceive until she is physically and emotionally ready for it and has completed all the tests recommended to determine the cause of the miscarriage.
From a medical point of view, conception is safe from the moment of passing at least one menstrual cycle (unless investigations or treatment of the causes of previous miscarriage are performed). However, it may take a much longer time before a woman is emotionally ready for pregnancy. Fortunately, the vast majority of women who have had one or two miscarriages successfully carry on with their next pregnancy.
For difficult cases, there are special treatments available using Preimplantation Genetic Diagnosis (PGD). PGD allows for genetic testing of the embryo before it is transferred into the uterine cavity. This technique is carried out as part of the IVF program and allows you to transfer into the uterine cavity only "healthy" embryos that do not have certain genetic diseases.
They can not only lead to miscarriage, but also provoke infertility.
When can I get pregnant after a miscarriage?
A woman is not recommended to try to conceive until she is physically and emotionally ready and has completed all the tests recommended to determine the cause of the miscarriage.
From a medical point of view, conception is safe from the moment of passing at least one menstrual cycle (unless investigations or treatment of the causes of previous miscarriage are performed).
However, it may take a much longer time before a woman is emotionally ready for pregnancy. Fortunately, the vast majority of women who have experienced one or two miscarriages do not suffer from infertility and successfully carry their next pregnancy to term.
Preparation for pregnancy in case of recurrent miscarriage
If there have already been 2 or more cases of spontaneous abortion, preparation is necessary before the next conception of a child. The reproductive specialist will prescribe a series of studies aimed at identifying the cause of miscarriage. Many diagnostic measures are similar to those prescribed for infertility. The woman will have to:
The reproductive specialist will prescribe a series of studies aimed at identifying the cause of miscarriage. Many diagnostic measures are similar to those prescribed for infertility. The woman will have to:
- take blood tests for hormones - to identify the endocrine factor;
- get swabs and blood tests for infections;
- visit a hemostasiologist;
- pass an extended coagulogram;
- get advice from a geneticist;
- undergo instrumental studies to diagnose possible inflammatory diseases of the genital organs and detect uterine factor.
A man should also visit a geneticist, as well as take a spermogram and analysis for sperm DNA fragmentation. It is likely that it is the male germ cells that carry defective genetic material. It can cause both infertility and miscarriage.
The choice of investigations in a woman largely depends on the trimester in which the miscarriage occurs. So, in the first trimester, the endocrine factor becomes the cause of miscarriage much more often, so the most important are the studies of the level of hormones in the blood.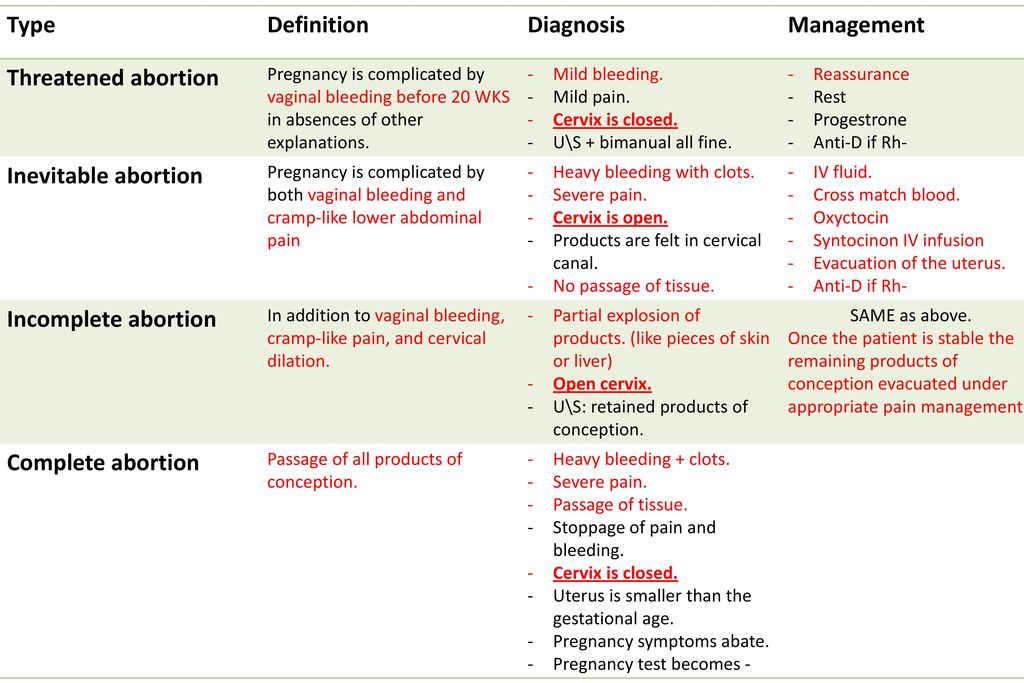 In the second trimester, disorders in the hemostasis system or uterine factor (isthmic-cervical insufficiency) often come to the fore.
In the second trimester, disorders in the hemostasis system or uterine factor (isthmic-cervical insufficiency) often come to the fore.
Further preparation for pregnancy may include:
- hormonal correction;
- treatment of inflammatory diseases of the pelvic organs;
- elimination of violations in the hemostasis system;
- surgical treatment if there is a uterine miscarriage factor;
- IVF with PGD in case of suspicion of a genetic factor.
What can a woman do to prevent miscarriage?
Episodes of abortion do not always indicate a pathological process. It is likely that the examination will not reveal violations, and then the next pregnancy will end in childbirth.
In order to increase the chances of success, you need to:
- undergo a medical examination in a timely manner;
- eliminate heavy physical exertion;
- normalize sleep and wakefulness;
- avoid alcohol and smoking;
- avoid crowded places in order to prevent SARS infection;
- monitor the state of somatic health;
- avoid stress.
The greatest risk of miscarriage is present in the first trimester of pregnancy (80% of all spontaneous abortions). Therefore, it is during this period that a woman should more carefully monitor her health, lifestyle, daily routine.
The role of IVF and PGD in the prevention of miscarriage
IVF is the most effective method to overcome infertility. As part of this procedure, preimplantation genetic diagnosis can be performed. The essence of the method is to study one of the cells of the embryo to identify chromosomal and gene mutations. They are the most common cause of habitual miscarriage.
The risk group includes women over 35 years of age, as well as patients with relatives with genetic pathologies, working in hazardous industries, having bad habits.
IVF with PGD is recommended in cases where a woman has several episodes of spontaneous abortion, and the cause of this phenomenon cannot be determined. This procedure may also be recommended by a geneticist based on the results of an examination of a married couple.