Do placenta move during pregnancy
Placenta previa: MedlinePlus Medical Encyclopedia
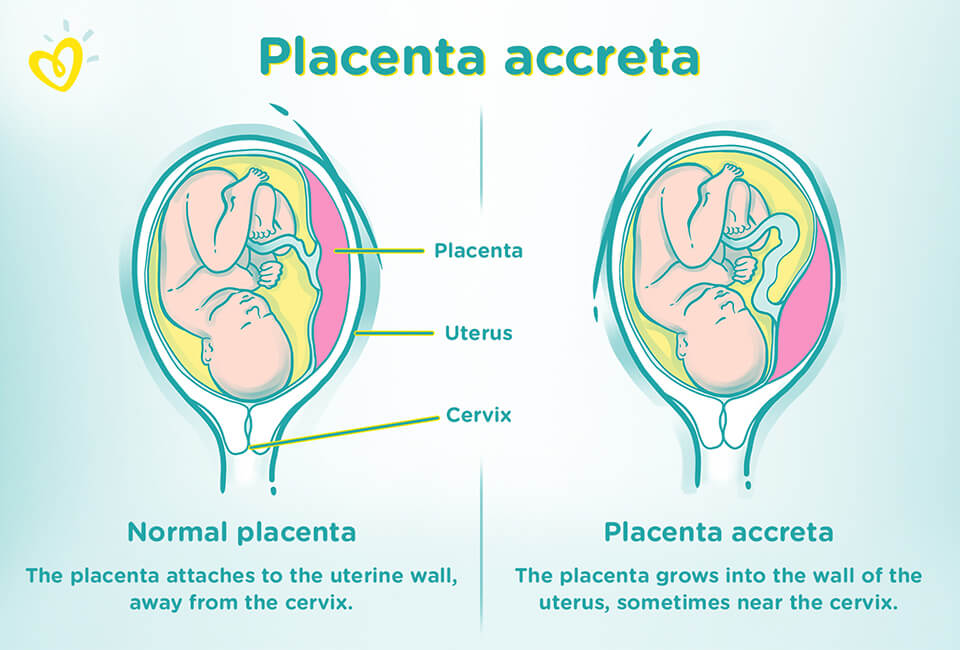
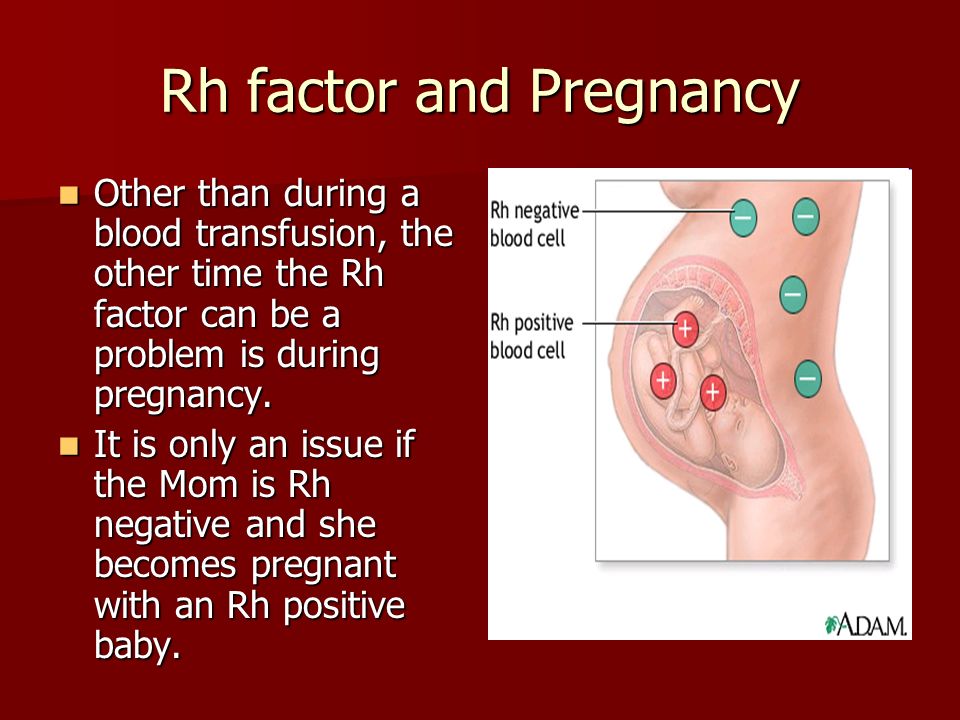
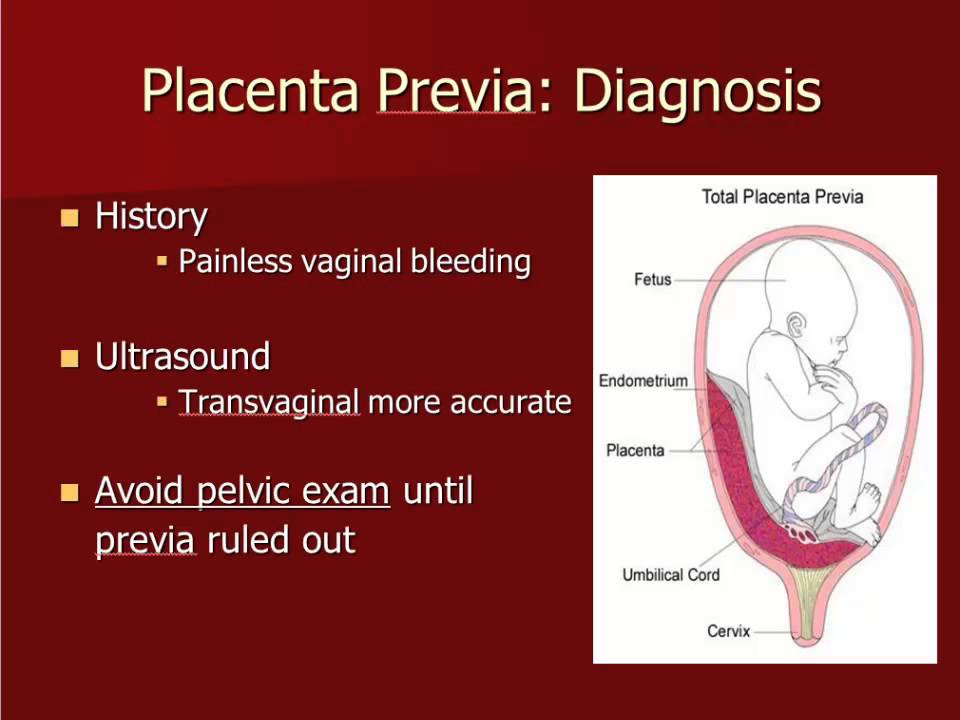
Placenta previa is a problem of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening to the cervix.
The placenta grows during pregnancy and feeds the developing baby. The cervix is the opening to the birth canal.
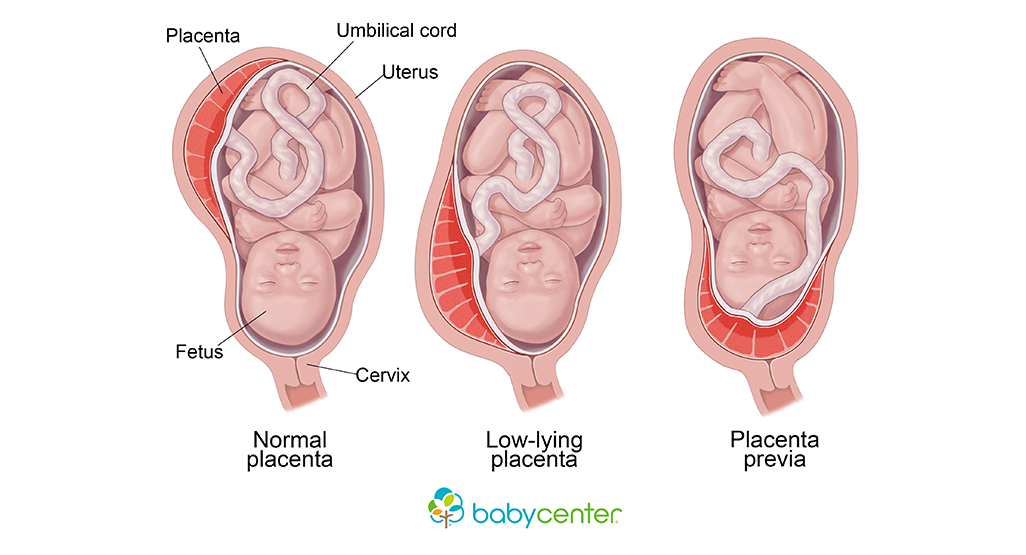
During pregnancy, the placenta moves as the womb stretches and grows. It is very common for the placenta to be low in the womb in early pregnancy. But as the pregnancy continues, the placenta moves to the top of the womb. By the third trimester, the placenta should be near the top of the womb, so the cervix is open for delivery.
Sometimes, the placenta partly or completely covers the cervix. This is called a placenta previa.
There are different forms of placenta previa:
- Marginal: The placenta is next to the cervix but does not cover the opening.
- Partial: The placenta covers part of the cervical opening.
- Complete: The placenta covers all of the cervical opening.
Placenta previa occurs in 1 out of 200 pregnancies. It is more common in women who have:
- An abnormally shaped uterus
- Had many pregnancies in the past
- Had multiple pregnancies, such as twins or triplets
- Scarring on the lining of the uterus due to a history of surgery, C-section, or abortion
- In vitro fertilization
Women who smoke, use cocaine, or have their children at an older age may also have an increased risk.
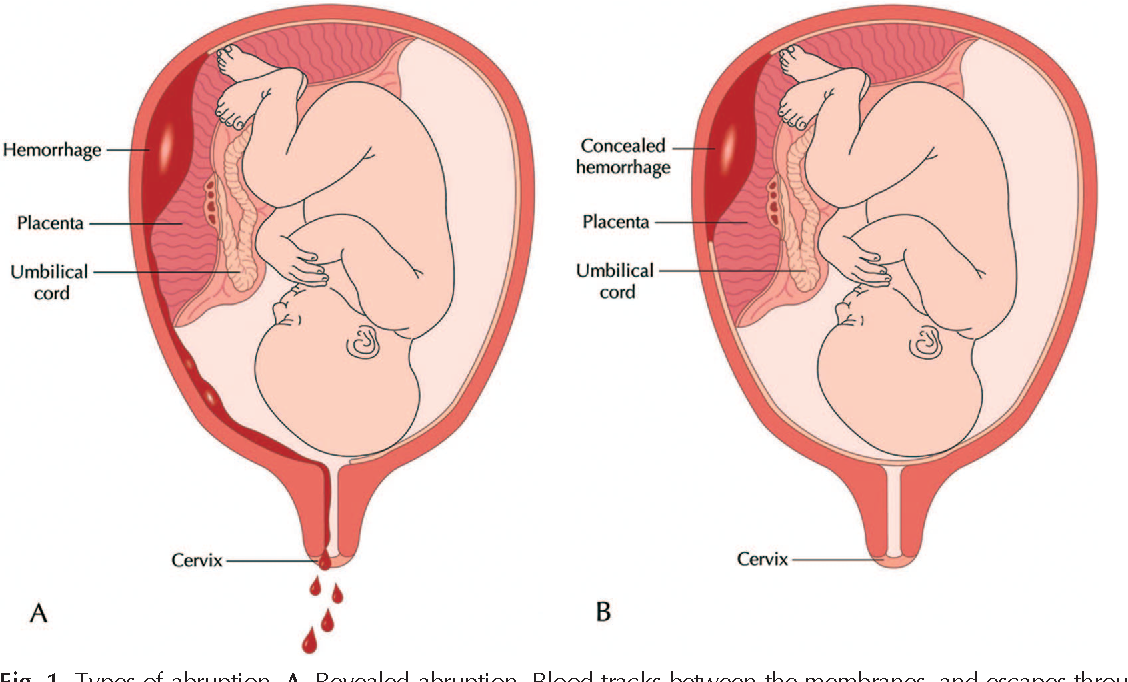
The main symptom of placenta previa is sudden bleeding from the vagina. Some women also have cramps. The bleeding often starts near the end of the second trimester or beginning of the third trimester.
Bleeding may be severe and life threatening. It may stop on its own but can start again days or weeks later.
Labor sometimes starts within several days of the heavy bleeding. Sometimes, bleeding may not occur until after labor starts.
Your health care provider can diagnose this condition with a pregnancy ultrasound.
Your provider will carefully consider the risk of bleeding against early delivery of your baby. After 36 weeks, delivery of the baby may be the best treatment.
Nearly all women with placenta previa need a C-section. If the placenta covers all or part of the cervix, a vaginal delivery can cause severe bleeding. This can be deadly to both the mother and baby.
If the placenta is near or covering part of the cervix, your provider may recommend:
- Reducing your activities
- Bed rest
- Pelvic rest, which means no sex, no tampons, and no douching
Nothing should be placed in the vagina.
You may need to stay in the hospital so your health care team can closely monitor you and your baby.
Other treatments you may receive:
- Blood transfusions
- Medicines to prevent early labor
- Medicines to help pregnancy continue to at least 36 weeks
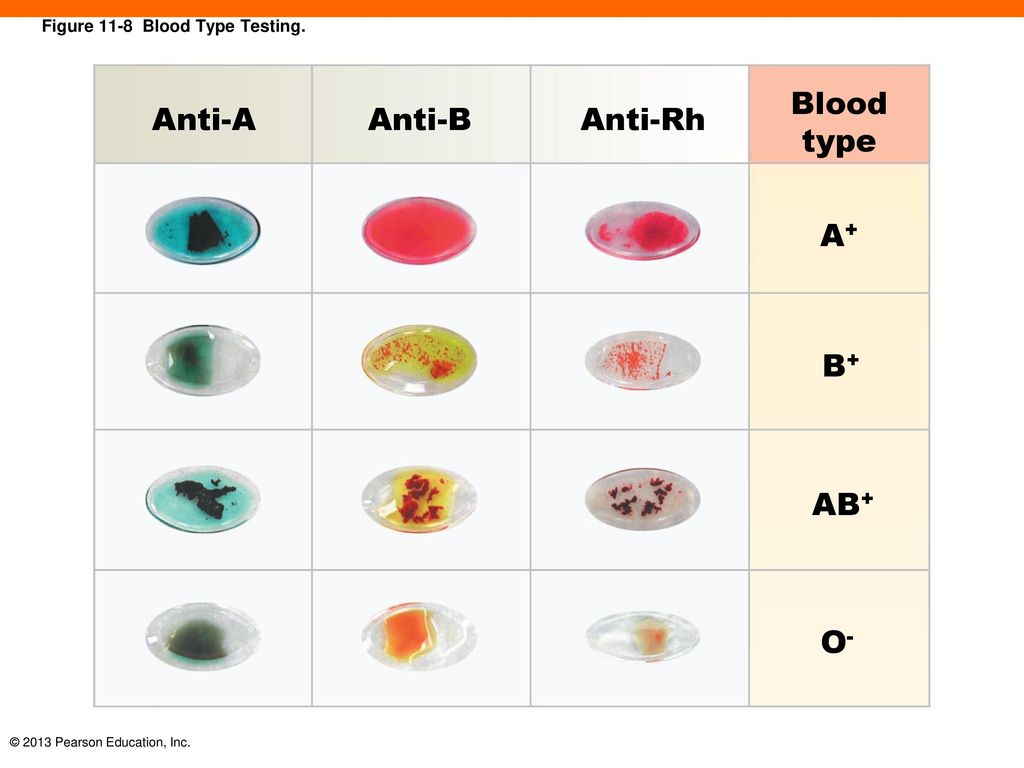
- Shot of special medicine called Rhogam if your blood type is Rh-negative
- Steroid shots to help the baby's lungs mature
An emergency C-section may be done if the bleeding is heavy and cannot be controlled.
The biggest risk is severe bleeding that can be life threatening to the mother and baby. If you have severe bleeding, your baby may need to be delivered early, before major organs, such as the lungs, have developed.
For most women who receive regular prenatal care, this condition is diagnosed before symptoms appear. This helps the provider and mother take steps to minimize risks from this condition.
Contact your provider if you have vaginal bleeding during pregnancy. Placenta previa can be dangerous to both you and your baby.
Vaginal bleeding - placenta previa; Pregnancy - placenta previa
- Cesarean section
- Ultrasound in pregnancy
- Anatomy of a normal placenta
- Placenta previa
- Placenta
- Ultrasound, normal fetus - arms and legs
- Ultrasound, normal relaxed placenta
- Ultrasound, color - normal umbilical cord
- Placenta
Francois KE, Foley MR.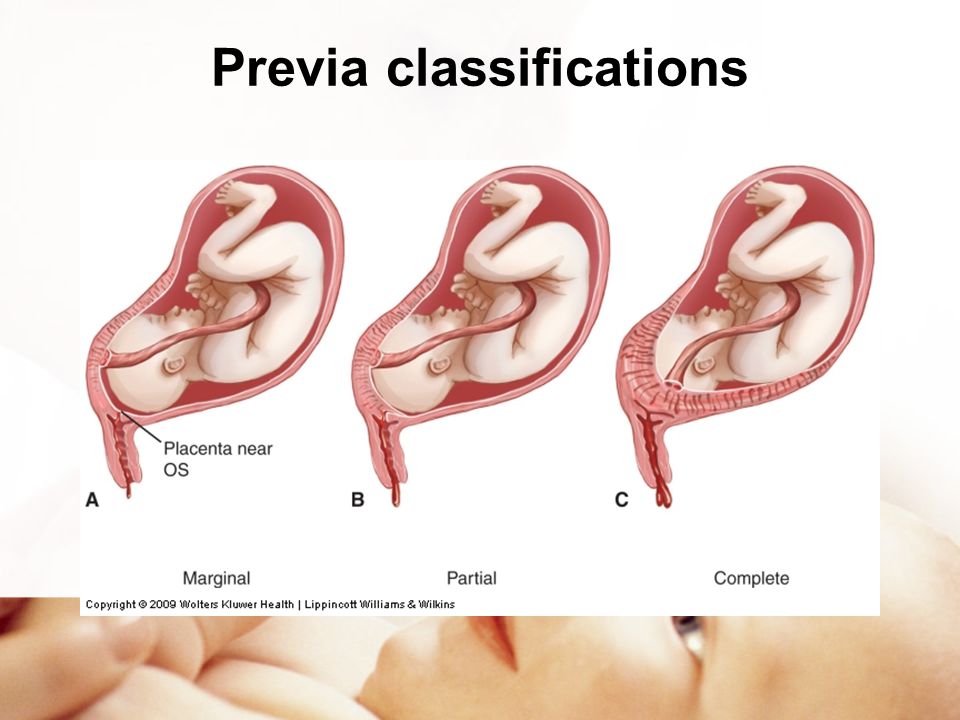 Antepartum and postpartum hemorrhage. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
Antepartum and postpartum hemorrhage. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
Hull AD, Resnik R, Silver RM. Placenta previa and accreta, vasa previa, subchorionic hemorrhage, and abruptio placentae. In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 46.
Henn MC, Lall MD. Complications of pregnancy. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 173.
Updated by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Placenta Previa
Placenta previa occurs when the placenta covers the opening of the cervix during the last months of pregnancy. This condition can cause severe bleeding before or during labor.
This condition can cause severe bleeding before or during labor.
The placenta develops in a pregnant person’s uterus during pregnancy. This sac-like organ provides the developing baby with food and oxygen. It also removes waste products from the baby’s blood. The placenta is also referred to as “afterbirth” because it exits the body after the baby is born.
During pregnancy, the uterus stretches and grows. It’s normal for the placenta to be low in the uterus in early pregnancy. As the pregnancy continues and the uterus stretches, the part of the uterine the placenta was stuck to moves, usually away from the cervical opening.
By the third trimester, the placenta should be near the top of the womb. This position allows the cervix, or the entrance to the womb at the bottom of the uterus, a clear path for delivery.
If the placenta attaches instead to the lower part of the uterus, it can cover part or all of the internal opening or “os” of the cervix. When the placenta covers the cervical os during the last months of pregnancy, the condition is known as placenta previa.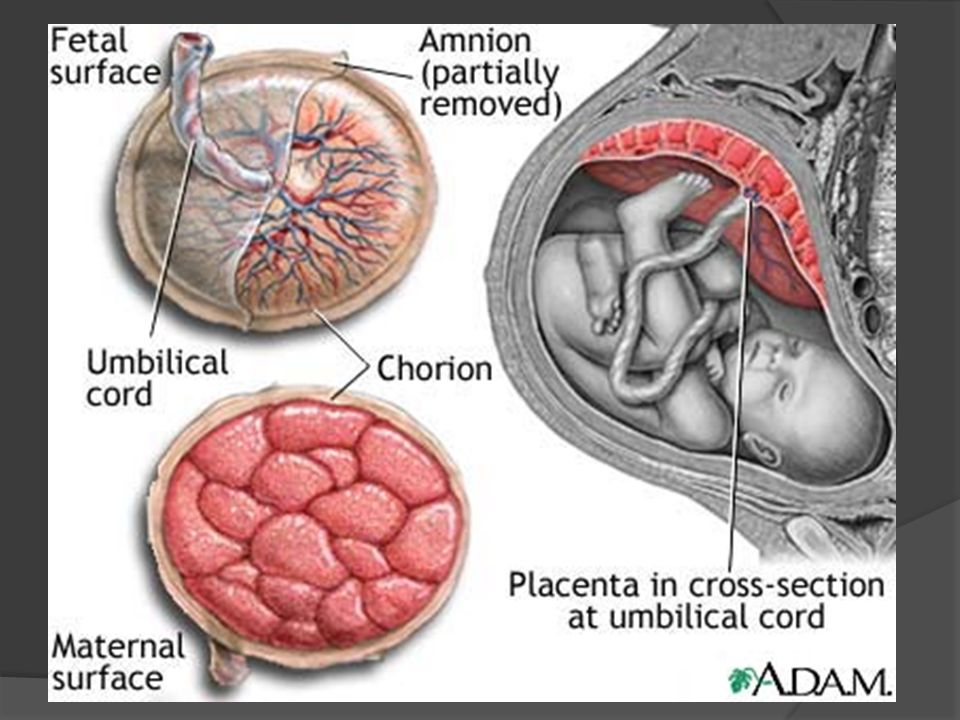
Most pregnant people with placenta previa will require pelvic rest. This typically includes abstaining from having sexual intercourse, limiting any procedures like an obstetrical check for dilation, and possibly restricting any exercises that may strain the pelvic floor.
The main symptom of placenta previa is sudden light to heavy bleeding from the vagina. Any bleeding can be representative of problems with the placenta and needs investigation by a physician. Specific symptoms may include:
- cramps or sharp pains
- bleeding that starts, stops, and begins again days or weeks later
- bleeding after intercourse
- bleeding during the second half of pregnancy
Risk factors for the development of placenta previa include:
- unusual position of the baby, including breech (buttocks first) or transverse (lying horizontally across the womb)
- previous surgeries that involve the uterus: cesarean delivery, surgery to remove uterine fibroids, dilation and curettage (D&C)
- pregnant with twins or other multiples
- prior miscarriage
- large placenta
- abnormally shaped uterus
- having already given birth to one child
- prior diagnosis of placenta previa
Pregnant people who are smokers, who are older than 35, or who are of Asian descent are also at higher risk of developing placenta previa.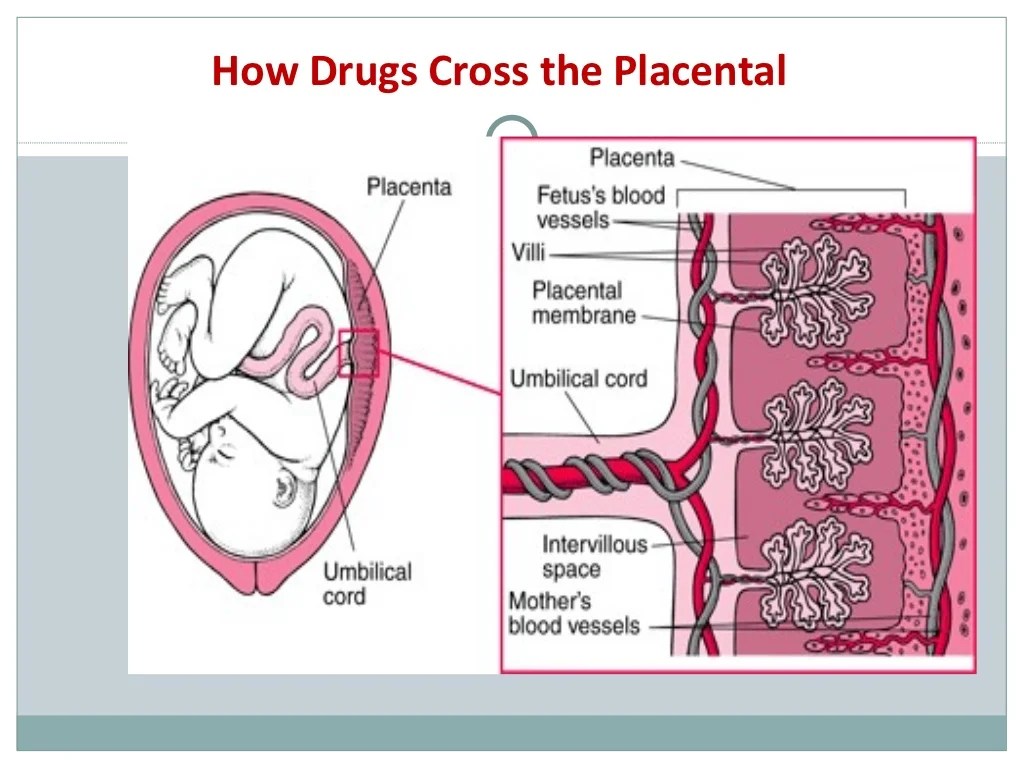
Usually, the first signs of placenta previa will show up during the routine 20-week ultrasound. These initial signs are not necessarily a cause for worry, since the placenta is often lower in the uterus during the early part of a pregnancy.
The placenta usually corrects itself. According to the Royal College of Obstetricians and Gynaecologists, only 10 percent of people with low-lying placenta at 20 weeks will have a low-lying placenta at their next ultrasound. Only .5 percent will have placenta previa at the end of their pregnancy.
If you experience any bleeding in the second half of your pregnancy, doctors will monitor the position of the placenta using one of these preferred methods:
- Transvaginal ultrasound. Your doctor places a probe inside the vagina to provide an inside view of your vaginal canal and cervix. This is the preferred and most accurate method for determining placenta previa.
- Transabdominal ultrasound. A healthcare technician places gel on your abdomen and moves a handheld unit called a transducer around your abdomen to view the pelvic organs.
 The sound waves make a picture on a TV-like screen.
The sound waves make a picture on a TV-like screen. - MRI (magnetic resonance imaging). This imaging scan will help clearly determine the placenta’s location.
Doctors will decide how to treat your placenta previa based on:
- the amount of bleeding
- the month of your pregnancy
- the baby’s health
- the position of the placenta and the baby
The amount of bleeding is a doctor’s main consideration when deciding how to treat the condition.
Minimal to no bleedingFor cases of placenta previa with minimal or no bleeding, your doctor will likely suggest pelvic rest. This means refraining from putting anything into your vagina during pregnancy in order to prevent medical complications.
You’ll also be asked to avoid sex and likely exercise as well. If bleeding occurs during this time, you should seek medical care as soon as possible.
Heavy bleedingIn the case of heavy bleeding, your doctor will advise scheduling a cesarean delivery as soon as it’s safe to deliver — preferably after 36 weeks. If the C-section needs to be scheduled sooner, your baby may be given corticosteroid injections to speed up their lung growth.
If the C-section needs to be scheduled sooner, your baby may be given corticosteroid injections to speed up their lung growth.
In the case of uncontrolled bleeding, an emergency cesarean delivery will have to be performed.
During labor, the cervix will open to allow the baby to move into the vaginal canal for birth. If the placenta is in front of the cervix, it will begin to separate as the cervix opens, causing internal bleeding.
This can necessitate an emergency C-section, even if the baby is premature, as the pregnant person could bleed to death if no action is taken. Vaginal birth also poses too many risks for the pregnant person, who could experience severe hemorrhaging during labor, delivery, or after the first few hours of delivery.
A placenta previa diagnosis can be alarming for people who are expecting a baby. Here are some ideas for how to cope with your condition and how to prepare yourself for delivery.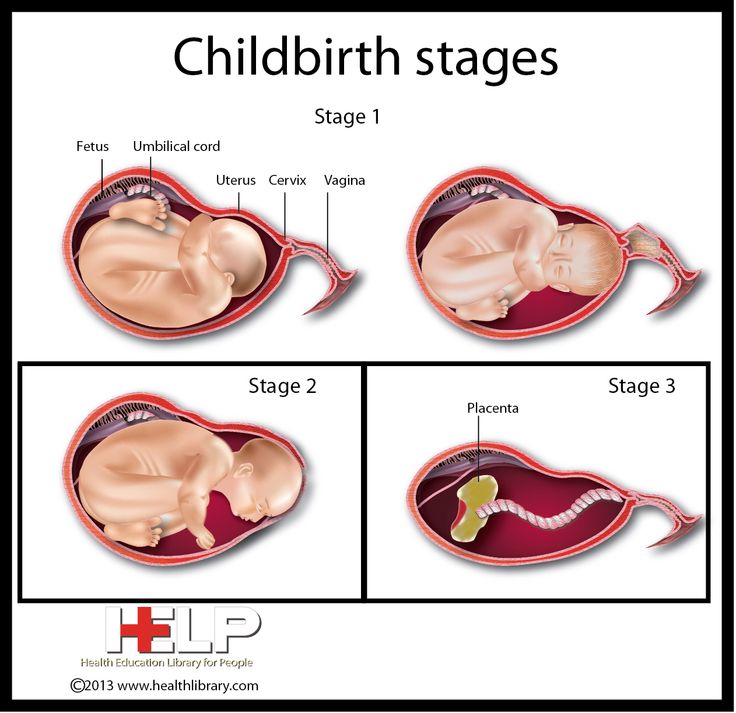
Get educated. The more you know, the more you’ll know what to expect. Get in contact with other people who have been through placenta previa births.
Be prepared for your cesarean delivery. Depending on the type of your placenta previa, you might not be able to have a vaginal birth. It’s good to remember the ultimate goal — the health of you and your baby.
Rest. Pelvic rest is important while you are experiencing this condition. Additionally you should not engage in any strenuous activity or heavy lifting. You can use the time wisely by catching up on small projects, such as:
- putting together a photo album
- writing letters
- reading about your upcoming lifestyle change
Pamper yourself. Indulge in small pleasures, such as:
- buying a new pair of comfortable pajamas
- reading a good book
- watching your favorite TV program
- keeping a gratitude journal
Be sure to rely on your circle of friends and family for conversation and support.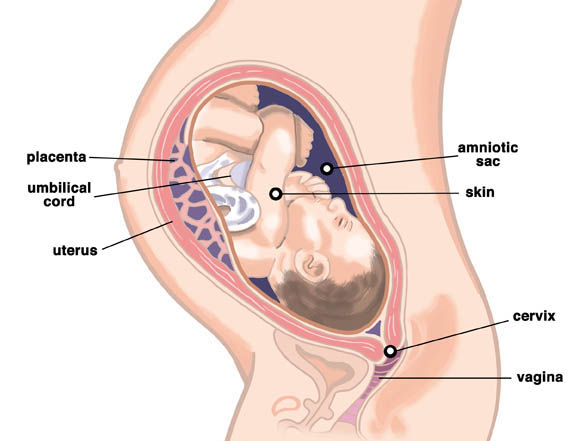
Fetal movement during pregnancy | When the first movements appear
Pregnancy
Article
5/5 1 reviews
The feeling of the first fetal movements is one of the most exciting experiences during pregnancy. The movements of the crumbs help to fully feel the presence of a small life inside and make sure that everything is in order with the crumbs. After all, the movement of the baby in the stomach is also an important marker that allows you to assess his condition at different stages of pregnancy.
6 min. for reading Feb. 17, 2022
When do the first movements appear?
The baby begins to move very early in the womb - at 7-8 weeks of gestation. But the first movement of the fetus goes unnoticed, since during this period it is very tiny, a little larger than a marigold.
The first tangible movements of the child, as a rule, appear in the second trimester - between 16 and 22 weeks of pregnancy, when the baby has already grown and grown stronger. The week in which the movement is felt depends on many factors:
- First or second child. During the first pregnancy, the movements of the baby become noticeable closer to the 20-22nd week. If the pregnancy is the second or third, the movements begin to be felt on average at 18 weeks or even earlier, because the woman already knows what sensations to expect.
- Placenta placement. If the placenta is closer to the back wall of the uterus, then the woman may feel movements later, if to the front - earlier.
- The physique of the expectant mother. Sometimes physique plays a role: fragile girls can feel the first tremors 2 weeks earlier.
- Lifestyle. In the midst of the working day, in noise or shaking, fetal movement is easy to miss. It is more likely to feel the first movement of the crumbs in a calm position, sitting or lying down.
In what part of the abdomen do you feel the first movements? Usually timid first movements are felt in the lower abdomen. At first, it is easy to confuse them with other internal processes, such as rumbling and bouts of hunger. But the baby grows and the movements become more intense, more diverse and “travel” along the tummy along with the tumbling baby.
Features of fetal movements at different stages of pregnancy
The nature and frequency of movements of the child change as he grows and develops. At first they are weak and irregular, but then the activity increases, and the movements become stronger and more intense.
Let's take a closer look at how the baby moves at different times and how the mother feels it.
First trimester
Toward the end of the first trimester, the baby begins to make its first movements, as light as the fluttering of a butterfly. But it is still very small, so in most cases the movements go unnoticed.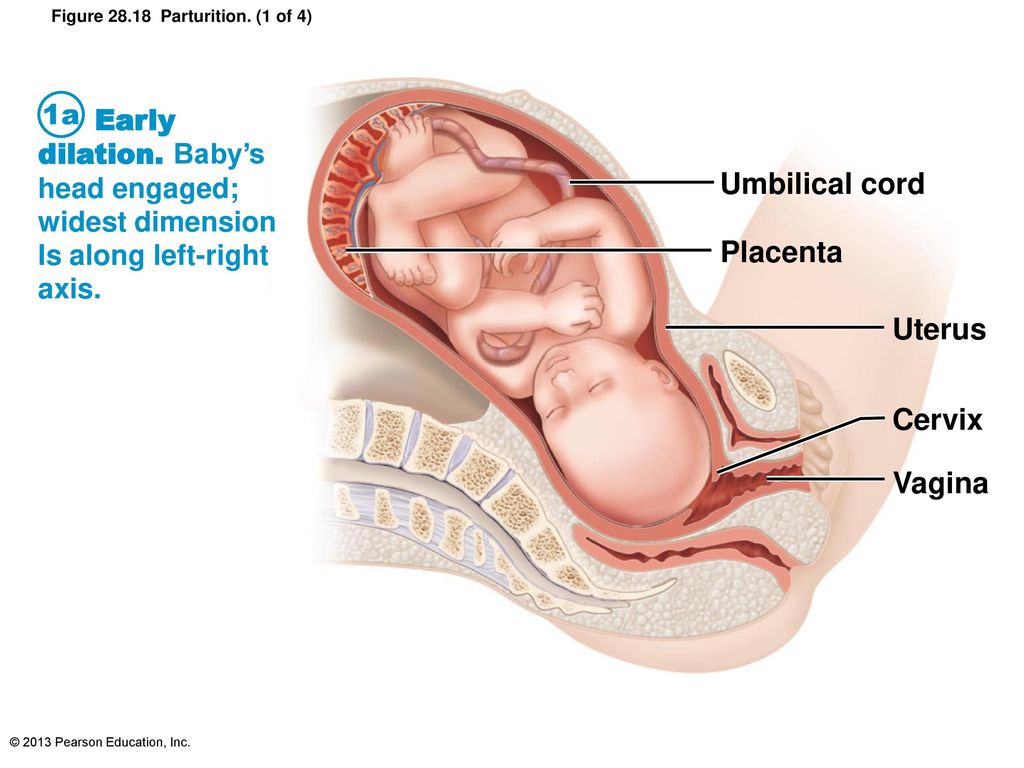 The maximum that can be felt is a light, light, barely noticeable flutter in the lower abdomen or something resembling bubbles.
The maximum that can be felt is a light, light, barely noticeable flutter in the lower abdomen or something resembling bubbles.
Second trimester
At 16 weeks pregnant, some women begin to feel the baby move. Someone describes them as the flutter of small wings or the movement of a fish wagging its tail, while someone describes them as twitching of a vein pulsating inside or blows of a small hammer.
By 20 weeks, most pregnant women already feel the baby's light movements. At week 24, they become more pronounced and intense, sometimes accompanied by a slight twitch during hiccups. By the end of the second trimester, active fetal movement begins - the child somersaults and pushes more and more clearly, more often and stronger.
Third trimester
At 28 weeks, the baby moves up to 30 times an hour, and some of his kicks and pokes can be so strong that the mother takes her breath away. During this period, obstetricians recommend starting to count the movements of the child. The nature of the activity helps the doctor understand what is happening with the baby and how he is developing.
The nature of the activity helps the doctor understand what is happening with the baby and how he is developing.
At this stage of development, the baby develops a certain pattern of sleep and wakefulness. Peak activity tends to occur in the evening and at night—between 9:00 PM and 01:00 AM—just when mom is trying to sleep. This surge is due to changes in blood sugar levels. In addition, the movements of the baby can react to touch, bright light, loud noises or an uncomfortable posture of the mother.
Your baby's activity continues to increase until 32 weeks. But after that, the grown-up child becomes more and more crowded in the fetal sac and the number of movements is reduced.
Tip
If you want your baby to make itself felt and move around, eat something sweet and lie on your side. An increase in blood glucose will cheer up the baby and he will begin to push.
Due to lack of space, fetal movements before childbirth become slower and more and more constrained.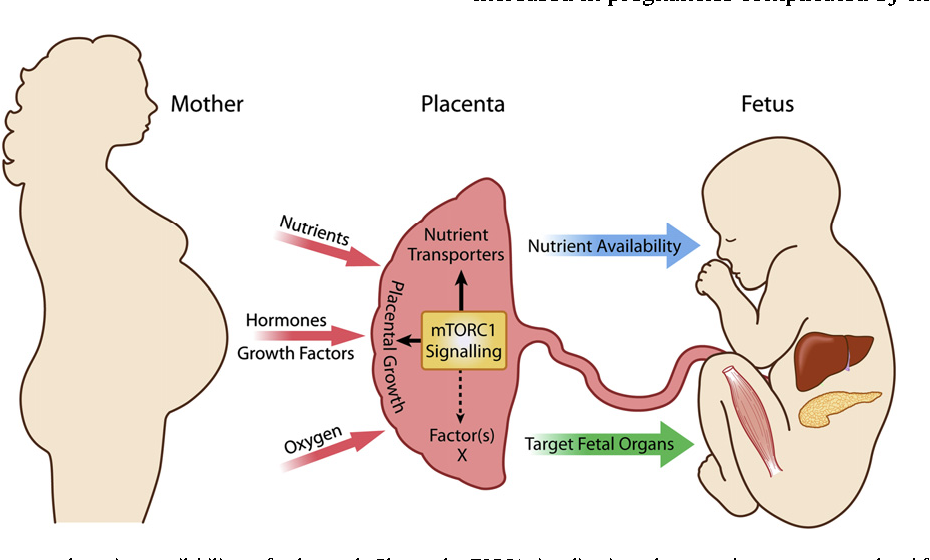 However, the baby should continue to move regularly throughout the day.
However, the baby should continue to move regularly throughout the day.
Important!
If your child's activity changes dramatically for unexplained reasons: he calms down or vice versa - the movements are too intensified and more frequent - tell your doctor as soon as possible. A change in the motor activity of the fetus may be a symptom of a violation of its condition and necessarily requires additional examination.
How to correctly calculate fetal movements?
Starting from the 28th week of pregnancy, the child's physical activity should be monitored every day. Until this time, the movements of the baby are not so noticeable, so the calculation will be uninformative.
So, how many movements should be per day? And how to count them correctly?
To determine the characteristics of the child's activity at home, use a special test of fetal movement by D. Pearson - "Count to ten". To do this, you need to mark in a special table every tenth movement of the baby from 9:00 to 21:00.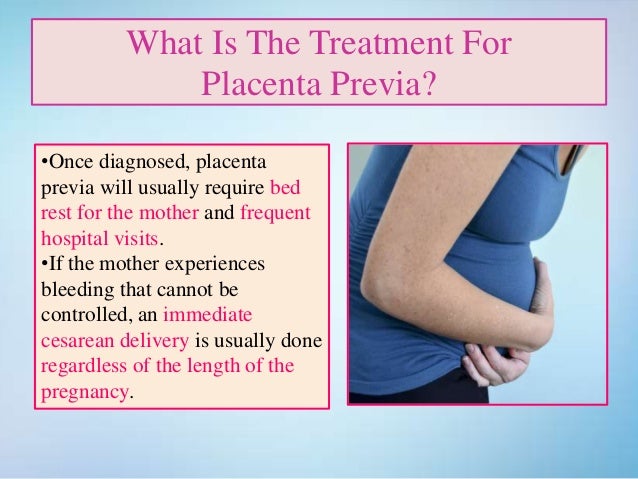 If the child develops normally, then in 12 hours you will count at least 10 movements.
If the child develops normally, then in 12 hours you will count at least 10 movements.
Important!
Not every push is considered a movement, but a series of movements (from the start of pushes to a pause).
After the 10th movement, write down the time and start counting the next day. And if the baby moves much less or does not make itself felt within 12 hours, contact your doctor as soon as possible!
In addition to the Pearson test, there is another way to count the child's movements. Choose an hour during which you will count movements every day. It is very important to do it at the same time. Focus on the baby's movements and see how long it takes the baby to complete 10 kicks. If you counted 10 shocks in an hour, you can be calm - everything is in order.
If you still don't get 10 pushes within an hour, try eating, changing your position, and then try counting the number of pushes again.
Advice
Keep a diary of your movements to record all changes. You can write everything in a notebook, or you can use a special mobile application that will help you track and record movements.
You can write everything in a notebook, or you can use a special mobile application that will help you track and record movements.
What should alert the future mother?
Be sure to contact your gynecologist if:
- You are past 22 weeks and you still don't feel your baby move. Perhaps you just did not notice them, but you need to make sure that the pregnancy is proceeding normally.
- Tracking the activity of the child, you notice that for more than 12 hours there is no movement at all or they have become significantly less during the day.
- For several hours in a row, the baby behaves too actively, the intensity of the shocks has changed so much that it hurts you because of his movements.
- A sharp change in the nature and frequency of movements is monitored, although there are no apparent reasons for this. This may indicate a violation of the condition of the fetus, its heartbeat, or an infection.
Advice
In the third trimester of pregnancy it is not recommended to sleep on your back. In this position, the vena cava can be clamped, which provides the baby with oxygen.
In this position, the vena cava can be clamped, which provides the baby with oxygen.
See also: Cord entanglement: causes and consequences for the baby
To make sure that everything is fine with the baby, the doctor may perform several examinations, such as auscultation, cardiotocography (CTG) and Doppler ultrasound.
Auscultation is a method of assessing the condition of the baby by the sounds that he makes in the womb. The doctor listens to the tone and rhythm of the heartbeat, different noises, monitors their sequence and duration.
CTG (cardiotocography) is an ultrasound examination of the fetus. But unlike conventional ultrasound, during CTG, the tone of the uterus, the heartbeat and the movements of the baby are recorded. Based on the results of this study, the doctor can determine how comfortable the child feels, check the work of his heart and the level of development. If there are deviations in CTG, the specialist may recommend an assessment of the fetal blood flow - dopplerometry.
If indicated, your doctor can choose the right treatment, recommend that the mother rest and get more rest, or even prescribe bed rest.
But do not immediately panic if the child is suspiciously quiet for an hour or two. Perhaps right now he is sleeping or preparing for an imminent meeting with his parents. There are also children who rest all day and become active only in the late afternoon. Just be attentive to yourself, your feelings and do not forget to take good care of your baby.
Related articles:
How does the baby behave before birth?
How does a woman's diet affect fetal development?
Material approved by doctor Oksana Negrich
Last reviews
Average customer rating
1 customer ratings
Snapshot of community ratings
- 5 1
- 4 0
- 3 0
- 2 0
- 1 0
when the first movement normally occurs during the first, second, third pregnancies, mother's feelings
The first movement of a child is a long-awaited and exciting event.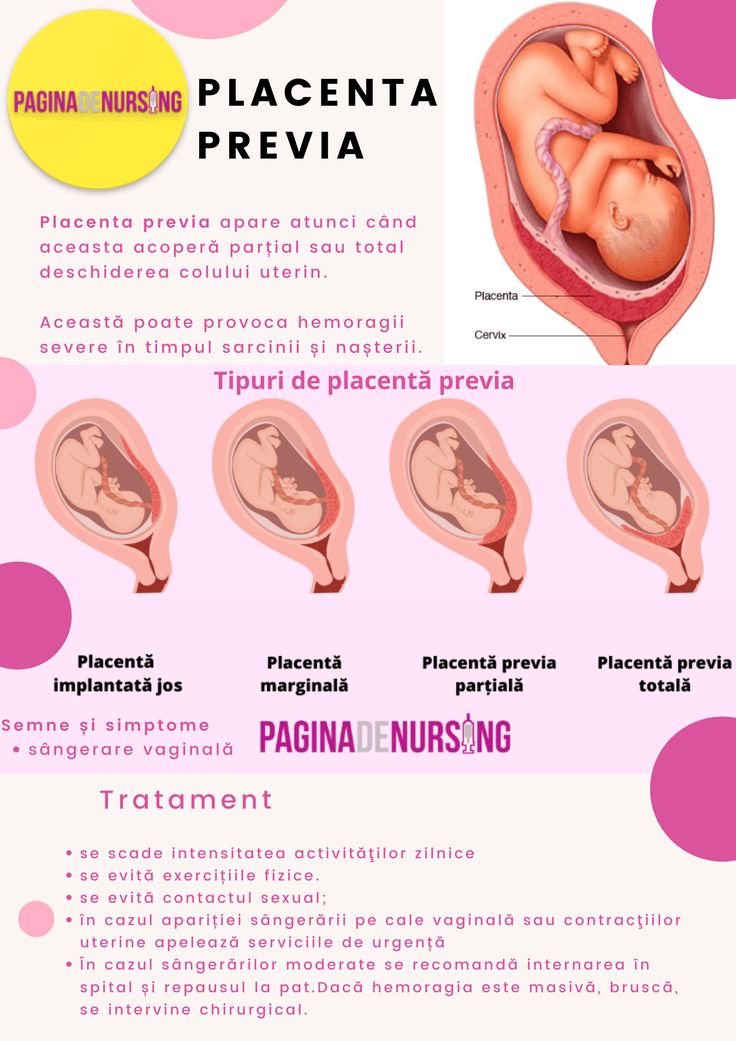 Each mother feels it in her own way, so for a woman carrying her first child, no one can describe exactly what she will feel. Someone perceives the beginning of the baby's movement as light jolts, someone - as a gurgling or fluttering of a butterfly. At the same time, the movement of the child during the second and subsequent pregnancies may be completely different from the first time.
Each mother feels it in her own way, so for a woman carrying her first child, no one can describe exactly what she will feel. Someone perceives the beginning of the baby's movement as light jolts, someone - as a gurgling or fluttering of a butterfly. At the same time, the movement of the child during the second and subsequent pregnancies may be completely different from the first time.
But while the mother is experiencing all these exciting sensations, the baby is busy with serious business. By moving his legs and arms, the child develops muscles and joints, tendons are formed. These "workouts" are not in vain compared with water aerobics.
By the way a child moves, one can judge his health. But only a specialist can correctly interpret fetal motility. Therefore, you should not worry ahead of time if the nature of fetal movements during pregnancy has changed. At the same time, it would not hurt the expectant mother to know what affects the behavior of the baby in her womb, when he begins to be active, and what changes may be the reason for going to the doctor. We will tell about this.
But only a specialist can correctly interpret fetal motility. Therefore, you should not worry ahead of time if the nature of fetal movements during pregnancy has changed. At the same time, it would not hurt the expectant mother to know what affects the behavior of the baby in her womb, when he begins to be active, and what changes may be the reason for going to the doctor. We will tell about this.
What you need to know about fetal movements during pregnancy
For a mother, the movement of a child in the womb is contact, communication with him. For the doctor - a source of information. By the nature of the movements, it is possible to determine how the child feels, where his head and legs are, and to calculate the pre-term of delivery.
| When a woman feels the first fetal movement | Normal from 18-22 weeks of pregnancy |
| How movements change over time | Intensity increases |
| How many movements should be normal | At least 10 movements in 12 hours from the second half of pregnancy (calculation by the most common method - Pearson) |
| in the navel, depending on the position of the child |
When the first movement of the fetus normally occurs
Usually the fetus itself begins to move already at 7-8 weeks of pregnancy - these are spontaneous muscle contractions, the woman does not feel them.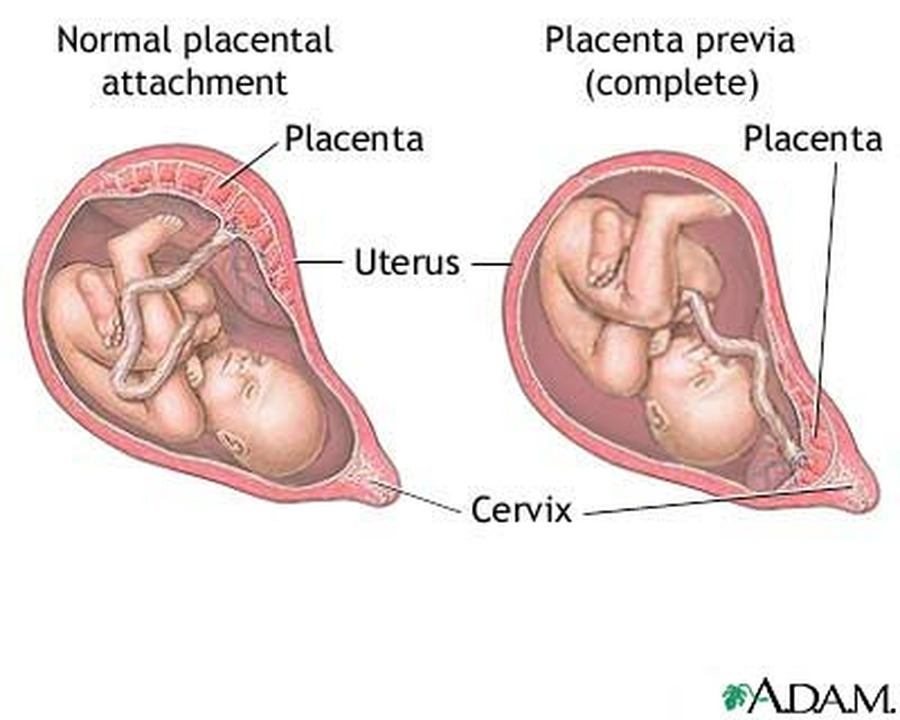 At the 12-14th week, the child is already quite actively moving his legs and arms, somersaults and swims in the uterine cavity like in a pool. But he is still so small that he practically does not come into contact with the walls of the uterus, and his mother can only see his movements on an ultrasound. But by the 16th week, she may well feel them. Women who are overweight or active, and those who work a lot, tend to feel movements later than slender women and those who live in a measured rhythm.
At the 12-14th week, the child is already quite actively moving his legs and arms, somersaults and swims in the uterine cavity like in a pool. But he is still so small that he practically does not come into contact with the walls of the uterus, and his mother can only see his movements on an ultrasound. But by the 16th week, she may well feel them. Women who are overweight or active, and those who work a lot, tend to feel movements later than slender women and those who live in a measured rhythm.
Normally, a mother can feel her baby's movements as early as the 18th week. However, there may be differences between primiparas and women who have given birth before.
During the first pregnancy
When carrying her first child, a woman begins to feel his movements at about 20 weeks. Usually a little later than those who are not pregnant for the first time.
One of the explanations is that the tone of the anterior wall of the abdomen is higher in the primipara.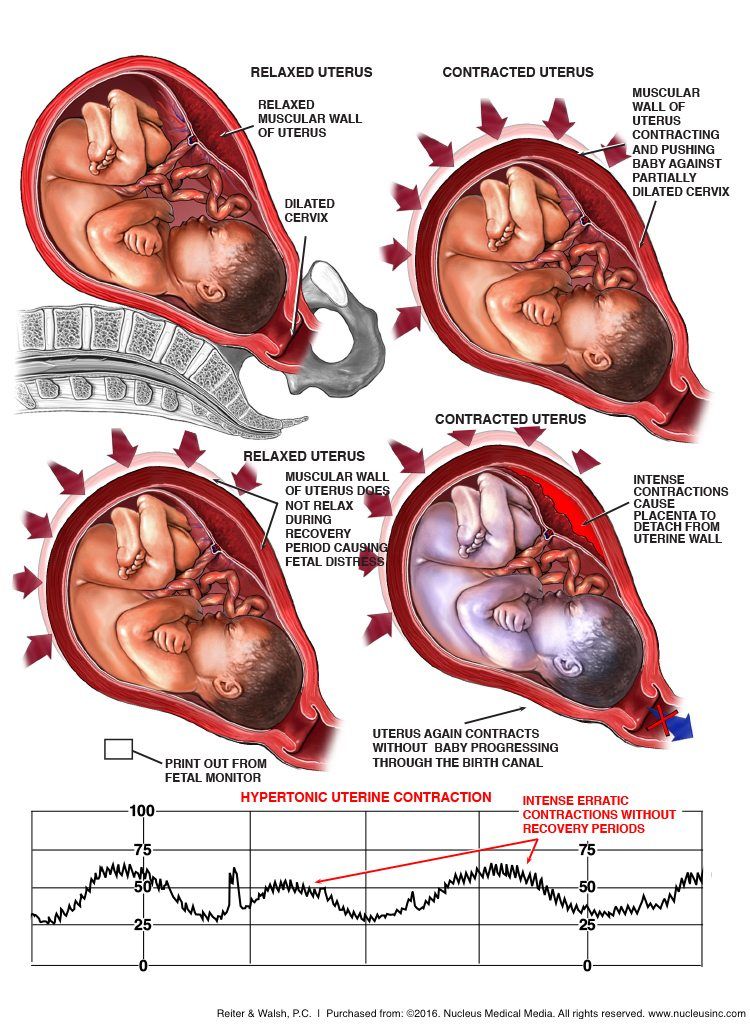 Another - due to inexperience, a woman may not attach any importance to the first movements at all and take them, for example, for "something with the intestines." Especially if the expectant mother is active, works a lot and she has no time to constantly listen to what is happening inside.
Another - due to inexperience, a woman may not attach any importance to the first movements at all and take them, for example, for "something with the intestines." Especially if the expectant mother is active, works a lot and she has no time to constantly listen to what is happening inside.
During the second pregnancy
It is believed that during the second pregnancy a woman may feel fetal movements a couple of weeks earlier than during the first. She is already experienced enough to understand that “butterfly fluttering” or “bubbles” in her stomach is a signal that the baby has reached out to her mother.
During the third pregnancy
The beginning of the baby's movement during the third pregnancy can be felt by a woman from the 16th to the 24th week. The walls of the uterus become more elastic and slightly thinner, so the nerve receptors of the peritoneum are more sensitive to the movements of the baby.
During the fourth and subsequent pregnancies
After each pregnancy, a woman has more experience and knowledge. She can already recognize the gentle and timid first movements of her child much earlier. Some mothers of many children can hear this cherished “knock-knock” of their fourth, fifth or sixth child as early as the 14th week.
She can already recognize the gentle and timid first movements of her child much earlier. Some mothers of many children can hear this cherished “knock-knock” of their fourth, fifth or sixth child as early as the 14th week.
How does mother feel?
Perception of movements is very individual. Especially the very first ones. They are compared with the “gurgling” of bubbles, fluttering butterflies, light tickling, “murmuring” in the stomach. All of them are at first quiet and unobtrusive. The longer the period, the more actively and persistently the child declares himself with tangible shocks. Closer to childbirth, he can already decently kick and even hurt his mother.
The frequency of the baby's movements in the womb depends on its position in the uterus, the characteristics of the woman's body, her mood and other factors. But the pregnant woman does not feel all the movements of the fetus. Meanwhile, on the 20th week there are already about 200 of them per day, and on the 28-32nd week - up to 600!
On average, after 28 weeks, the frequency of perceptible fetal movements is from 4 to 8 per hour. But at this time, the child already has cycles of sleep and wakefulness. The baby can sleep for several hours in a row, calming down for this time.
But at this time, the child already has cycles of sleep and wakefulness. The baby can sleep for several hours in a row, calming down for this time.
There are several general methods for assessing fetal movements.
- Pearson method
A pregnant woman counts fetal movements in 12 hours, and writes down the time of each 10th movement in a table. If there are less than 10 such records in 12 hours, then the activity of the fetus is low, and in order to understand the reasons, one should consult a doctor (1).
- Sadowski method
The woman lies on her left side and counts all fetal movements, even the smallest ones. If the child feels well, the mother will count at least 10 movements per hour. If there are fewer movements, you need to lie down for another hour or two and continue counting. If in two hours there were less than 10 movements, you should consult a doctor.
How the nature of movements changes during the entire period of pregnancy
A baby begins to move in the womb much earlier than the mother feels it - at a period of 7-8 weeks.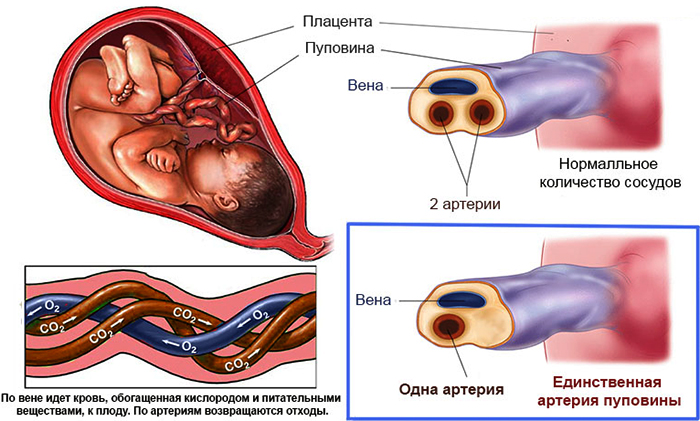 We are talking about the movements that she can feel.
We are talking about the movements that she can feel.
The very first - at 18-20 weeks - gentle and light, wavy or pulsating. But the baby is growing, the nature of the movements is changing. It moves most actively during the period from the 24th to the 32nd week of pregnancy. It can tumble, roll over, wiggle, rotate along its axis. Sometimes these movements of his can be traced along the mother's stomach, into which he rests from the inside with his heel, then his knee, then his hand.
By the 30th week, the fairly grown fetus assumes a permanent posture, bending its head and pressing its arms and legs to the body. He has little space for movements, but they are much more noticeable for mom, and sometimes even painful.
Fetal movements become smoother, more limited after 34-36 weeks. By stirring, the baby responds to a change in the position of the mother's body. After 38 weeks, when the abdomen droops, the fetus also moves lower and becomes calmer, as if saving energy for childbirth.
Doctors' comments about movements during pregnancy
Shared her opinion Maria Filatova, obstetrician-gynecologist, gynecologist-endocrinologist at the Chaika clinic :
— During pregnancy, women can be very worried and tend to overestimate the slightest changes in the nature of the baby's movements. This is fine. It is better to go to the doctor as soon as you suspect something is wrong (albeit several times), but make sure that your baby is doing well and stop worrying than not to come at all.
Regular fetal movements indicate a successful pregnancy. But the number of movements that is considered normal is a rather conditional indicator. It is most important for a woman to know about the individual nature of her child's movements. Reducing or changing the movements is what you need to pay attention to. If the movements become more rare and weak, it is urgent to contact an obstetrician-gynecologist.
Be sure to see a doctor if:
- fetal movements are not felt after 22 weeks of pregnancy;
- there were no movements during the day or they became significantly less within 12 hours;
- the movements became too active, to the point of pain, their character and frequency changed dramatically for no apparent reason.
Some drugs (such as strong painkillers or sedatives) can enter the fetal circulation and reduce the amount of fetal movement. Alcohol and smoking can also affect your child's movements. Often, expectant mothers note an increase in fetal activity after they have eaten sweets and against the background of their stress.
Comments Victoria Fisyuk, obstetrician-gynecologist at the SM-Clinic Reproductive Health Center:
— According to obstetric books, it is believed that fetal movements begin to be felt in a primigravida from 20 weeks, in a multi-pregnant woman - from 18 weeks. But at a doctor's appointment, pregnant women sometimes say that they feel movements from 16 and even from 14 weeks, and there is no reason not to believe them.
Previously, when it was not possible to assess the condition of the fetus with the help of instrumental methods of research, they paid attention and attached great importance to precisely the movements of the fetus, their nature and quantity.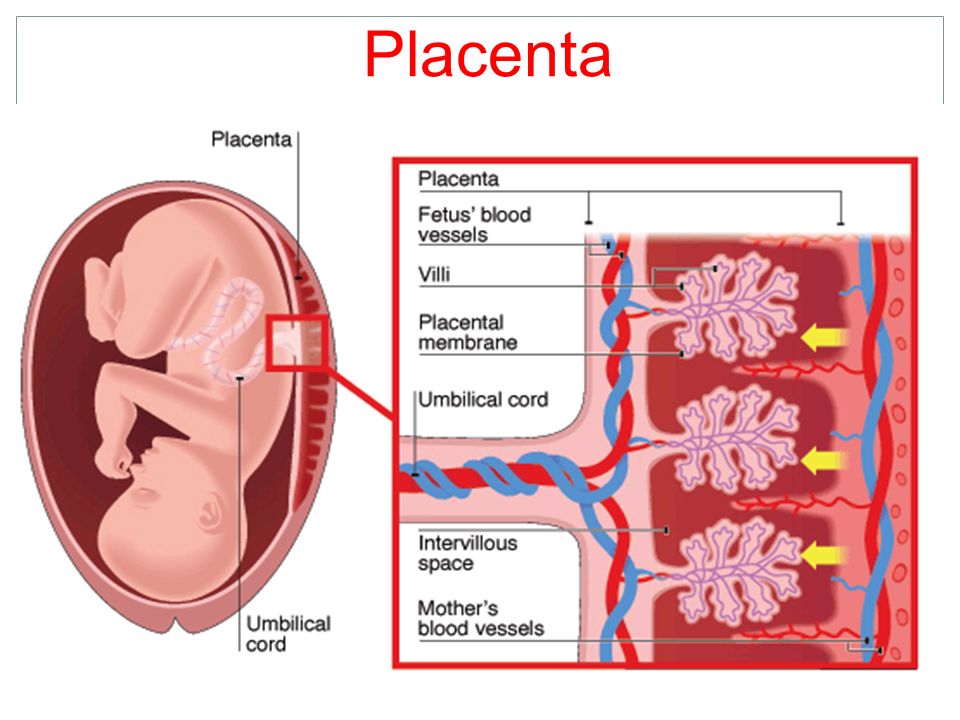 Focused on counting movements per hour, per 12 hours. But in my opinion, it was an assessment as such of the life of the fetus and nothing more. The fetus is already a person who lives his own life, he sleeps, rests, moves. Oddly enough, weather conditions influence him: when it rains or snows outside, he can just sleep all day. Sometimes his behavior may depend on the nutrition of his mother. If she hasn’t eaten for a long time, he can calm down, after eating for some time activity increases significantly, and a little later the fetus can sleep, which sometimes we, adults, want after a hearty dinner.
Focused on counting movements per hour, per 12 hours. But in my opinion, it was an assessment as such of the life of the fetus and nothing more. The fetus is already a person who lives his own life, he sleeps, rests, moves. Oddly enough, weather conditions influence him: when it rains or snows outside, he can just sleep all day. Sometimes his behavior may depend on the nutrition of his mother. If she hasn’t eaten for a long time, he can calm down, after eating for some time activity increases significantly, and a little later the fetus can sleep, which sometimes we, adults, want after a hearty dinner.
With an excess of sugar, the fetus will be less active. If the mother is unwell, for example, due to a viral infection, the fetus may also suffer a little from this.
Any attempt to adequately assess the vital activity of the fetus is not an easy task. But thanks to modern types of research: fetal ultrasound with Doppler, just Doppler, CTG, which is usually performed after 32 weeks, you can make the right conclusion.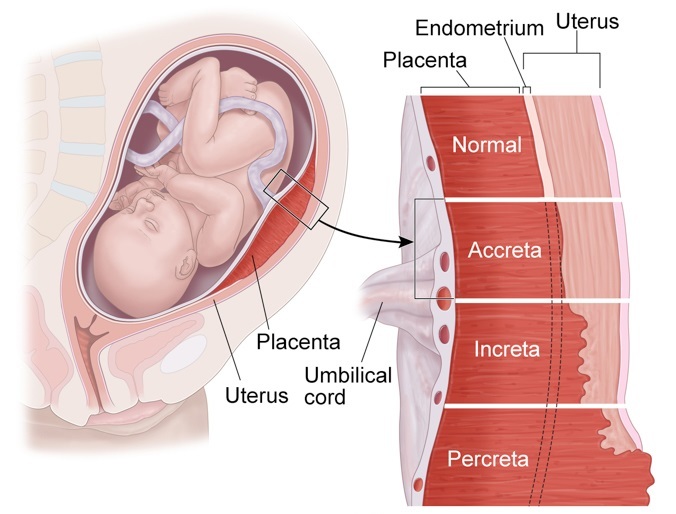
Sometimes a mother can come just in time for CTG, for example, in the afternoon, that is, when the fetus is sleeping. And in order not to get an incorrect result, we sometimes offer a woman to eat a chocolate bar or just move around, change position, turn to the other side. In the future, we recommend that you come to CTG during the hours of the greatest activity of the fetus.
If the assessment is low, a conclusion is given on suspicion of fetal hypoxia and, as a rule, the pregnant woman is sent to a hospital, where, thanks to monitoring, the condition of the fetus is assessed and sometimes a decision is made on delivery without waiting for the full term in the interests of the unborn child. Therefore, at the slightest suspicion of the mother that the fetus is "somehow not moving like that", you should immediately consult an obstetrician-gynecologist who will help relieve anxiety in order to continue to carry the pregnancy calmly.
Frequently asked questions and answers
Obstetrician-gynecologist Maria Filatova answers frequently asked questions from readers.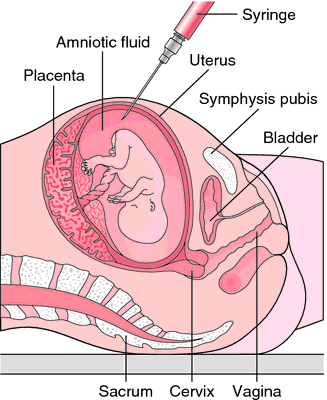
In what cases should the movement intervals be counted?
In situations where there are violations of the fetal-placental blood flow on ultrasound or abnormalities on CTG, a fetal movement test becomes mandatory for the expectant mother. But any woman can use it during pregnancy.
Usually start testing at 28 weeks using the Pearson method (see What is the normal frequency of movement). From 9.00 to 21.00 every tenth movement of the baby is recorded in a special table.
With normal development, at least 10 movements can be counted in 12 hours. If the tenth movement was at 14-15 hours, and the next day by this time the baby did not move even 5 times, then you should consult a doctor. Perhaps there is a violation of placental blood flow and fetal hypoxia (2).
What to do if the movements seem too active or, on the contrary, too weak?
Seek medical attention. Both too active movements and too weak ones can speak of hypoxia.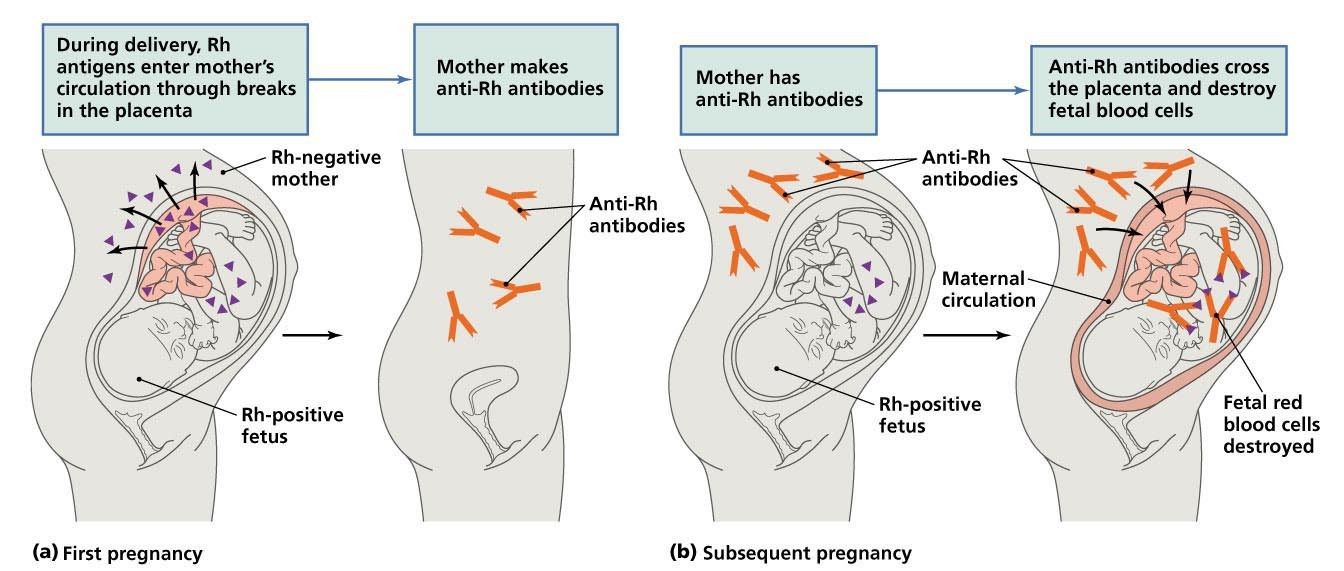 Some anatomical and physiological features of the mother can also affect her perception of the intensity of movements. For example, thin women will feel more intense movements (3).
Some anatomical and physiological features of the mother can also affect her perception of the intensity of movements. For example, thin women will feel more intense movements (3).
If the placenta (afterbirth) is in the anterior part of the uterus (womb), the woman may feel less able to move. If the baby is closer to the uterus with his back than with his hands, then the movements may also be felt less intensely.
In any case, whatever the cause of weak movements, it is better to go to the doctor and make sure that everything is in order with the baby.
Where do you feel movement in the abdomen?
If the baby's head is down, the main movements will be felt near the navel. If at the bottom of his legs, then the motor activity will shift to the lower abdomen.
By the nature of the movements, it is possible to determine in which direction the child's face is turned. If to the back of the mother, then the movements occur in the depths of the abdomen, if to the stomach, the movements are directed outward.