2 week rash
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up, including moisturising regularly.
You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
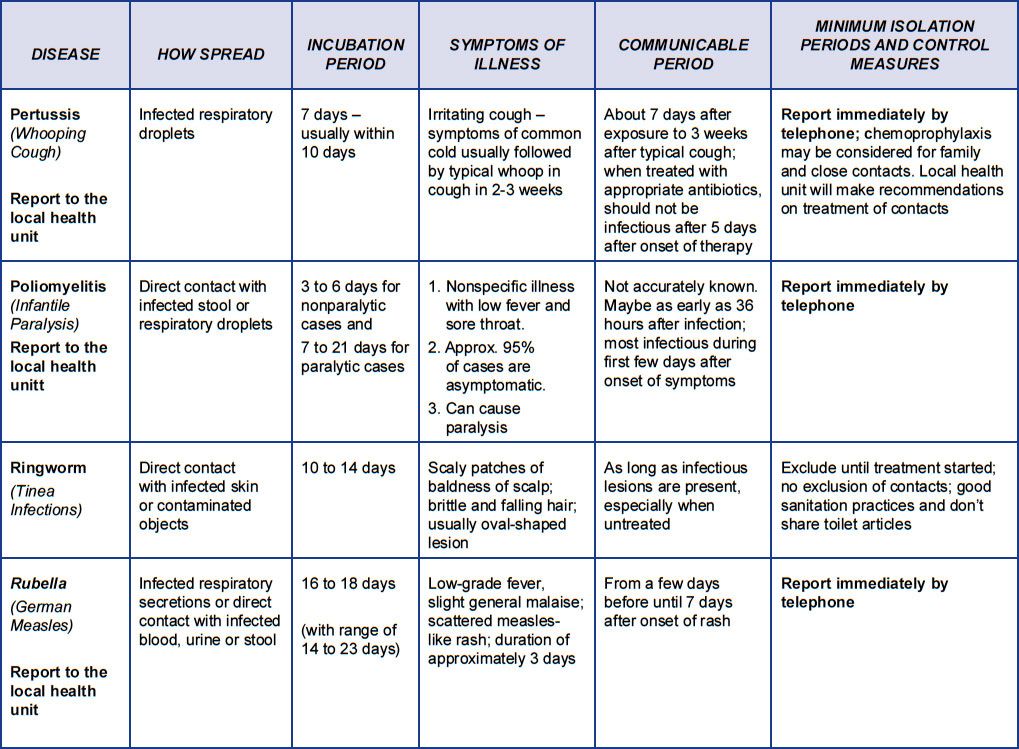
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.
Hives (urticaria)
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.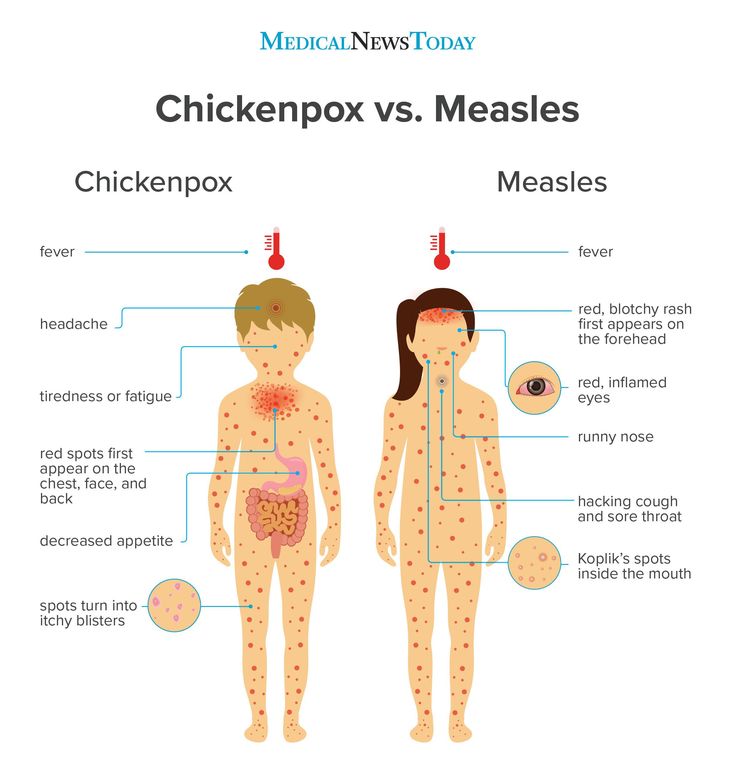
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Newborn Rashes and Birthmarks
Is this your child's symptom?
- Normal skin rashes and birthmark questions about newborns
Newborn Rashes - Topics Covered
If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice.
- Acne. Small red bumps on the face (onset 2-4 weeks).
- Drooling or Spit-Up Rash. Rash around the mouth and on the chin (onset anytime).
- Erythema Toxicum. Red blotches with small white "pimple" in the center (onset 2-3 days).
- Skin Injury from Birth Process. From forceps, scalp electrode or birth canal (present at birth).
- Milia. Tiny white bumps on the nose and cheeks (present at birth).
- Mongolian Spots. Bluish-green birthmark, often on buttock (present at birth).
- Stork Bites (Pink Birthmarks). On back of neck or bridge of nose (present at birth).
- Strawberry Hemangiomas. Raised red birthmarks (onset 2-4 weeks).
- Port-wine Stains. Dark red or purple flat birthmarks (present at birth).
Newborn Face Rashes: Most Common Ones
- Erythema Toxicum 50% (onset day 2 or 3)
- Milia 40% (present at birth)
- Baby Acne 30% (onset week 2 to 4)
- Drooling or Spit-up Rash (common and onset any time)
- Heat Rash (common and onset any time)
Heat Rash
- Many newborn rashes that have no clear cause are heat rashes.

- Heat rashes are a pink blotchy area with tiny bumps.
- They mainly occur on the face, neck and chest.
- During hot weather, most temporary newborn rashes are heat rashes.
- Cause: blocked off sweat glands. The openings are so tiny in newborns, that any irritation can block them. Examples are getting any ointment on the skin, friction from clothing or being overheated. Being held against the mother's skin while nursing causes many face rashes.
Herpes Simplex: Serious Newborn Rash
- Appearance. Several water blisters or pimples grouped in a cluster. They look like the cold sores (fever blisters) that adults get on their lip. After several days, they crust over.
- Location. Just one part of the body, usually the scalp or face.
- Redness. The base can be pink. The pinkness does not extend beyond the cluster of vesicles.
- Onset. Within the first 2 weeks of life.

- Importance. Early treatment with anti-viral drugs can prevent serious problems. If you think your newborn's rash looks like herpes, call your child's doctor now.
- Imitator. Although herpes can be confused with erythema toxicum, they look very different.
When to Call for Newborn Rashes and Birthmarks
Call 911 Now
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Purple or blood-colored spots or dots not present at birth
- Tiny blisters (little bumps that contain clear fluid)
- Pimples (little bumps that contain pus). Exception: looks like erythema toxicum which occurs in half of newborns.
- Skin looks infected (such as spreading redness, sores or pus)
- Rash is painful to touch
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Mild newborn rash, but cause is not clear
- You have other questions or concerns
Self Care at Home
- Normal newborn rashes or birthmarks
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
- Virtual Urgent Care
Care Advice for Newborn Rashes and Birthmarks
- Acne:
- More than 30 percent of newborns develop baby acne of the face. Acne consists of small red bumps.
- This baby acne begins at 2 to 4 weeks of age. It lasts until 4 to 6 months of age.
- The cause appears to be the transfer of maternal hormones just prior to birth.
- Since it goes away on its own, no treatment is needed. Baby oil or ointments make it worse.
- Drooling or Spit-up Rash:
- Many babies have a rash on the chin or cheeks that comes and goes. This is often due to contact with food. It's more common after starting baby foods. In newborns, it can also be from stomach acid that has been spit up. Prolonged contact with spit-up during sleep can cause the rash to get worse.
- Other temporary rashes on the face are heat rashes. These can occur in areas held against the mother's skin during nursing. Heat rashes are more common in the summertime.
- Rinse the face with water after all feedings or spitting up. During hot weather, change the baby's position more often. Also, put a cool wet washcloth on the rash. Do this for 10 minutes.
- Erythema Toxicum:
- More than 50 percent of babies get a rash called erythema toxicum.
 It starts on the second or third day of life.
It starts on the second or third day of life. - It's a harmless baby rash that doesn't need to be seen.
- The rash is made up red blotches. They are ½ inch to 1 inch (1 to 2.5 cm). The blotches have a small white or yellow "pimple" in the center.
- They look like insect bites, but are not. Red blotches are the main feature.
- They can be numerous, keep occurring, and look terrible. They can occur anywhere on the body surface, except the palms and soles.
- Their cause is unknown, but they are not an infection.
- They go away by 1-2 weeks of age.
- No treatment is needed. Ointments or baby oil make it worse.
- More than 50 percent of babies get a rash called erythema toxicum.
- Skin Injury from Forceps, Scalp Electrode or Birth Canal:
- The pressure of a forceps on the skin can leave marks. You may see bruises or scrapes anywhere on the head or face.
- During birth, skin overlying bony prominences can become damaged. You might see this on the sides of the skull bone. This is from pressure from the birth canal.
 Even without a forceps delivery, you may see bruises or scrapes.
Even without a forceps delivery, you may see bruises or scrapes. - Scalp electrodes can also cause scalp scrapes and scabs.
- The bruises and scrapes will be noted at birth. They will be more noticeable by day 2. They heal over or go away by 1 - 2 weeks of age.
- A fat tissue injury won't appear until day 5 to 10. Look for a firm coin-shaped lump. It will be under the skin and sometimes with a scab. This lump may take 3 or 4 weeks to go away.
- For any breaks in the skin, apply an antibiotic ointment (such as Polysporin). No prescription is needed. Use 3 times per day until healed.
- Call Your Doctor If:
- It becomes tender to the touch
- Becomes soft in the center
- Starts to looks infected
- Milia:
- Milia are tiny white bumps that occur on the face. The nose and cheeks are most often involved. Milia can also be seen on the forehead and chin.
- Milia occur in 40 percent of newborn babies. Present at birth.
- Milia are many in number. They occur equally on both sides of the face.
- Although they look like pimples, they are much smaller (pinhead size). They are not infected.
- They do not look like water blisters.
- They are blocked-off skin pores. They will open up.
- Milia will go away by 1 to 2 months of age.
- No treatment is needed. Ointments or creams can make them worse.
- Mongolian Spots:
- A Mongolian spot is a normal bluish-green or bluish-gray flat birthmark. They occur in over 90 percent of Native American, Asian, Hispanic, and African American babies. They are also seen in 10 percent of Caucasians, especially those of Mediterranean descent.
- They are present at birth.
- They occur most commonly over the back and buttocks. However, they can be present on any part of the body.
- They vary greatly in size and shape.
- They do not indicate illness or any disease.
- Most fade away by 2 or 3 years of age.
 A trace may last into adult life.
A trace may last into adult life.
- Stork Bites (Pink Birthmarks):
- Flat pink birthmarks that occur over the bridge of the nose or the eyelids. You can also find them on the back of the neck ("stork bites"). The ones in front are often referred to as "an angel's kiss".
- They occur in more than 50 percent of newborns. They are present at birth.
- All the birthmarks on the bridge of the nose and eyelids clear completely. Those on the eyelids clear by 1 year of age. Those on the bridge of the nose may last for a few more years. Those on the forehead from the nose up to the hairline usually last into adulthood. Laser treatment during infancy should be considered. Most birthmarks on the nape of the neck also clear. But, 25 percent can last into adult life.
- Strawberry Hemangiomas:
- Strawberry hemangiomas are red birthmarks that are raised or increasing in size.
- Onset usually between 2-4 weeks of age.
 Most often, start after 3 weeks of age. Sometimes (although rare), they don't appear until the second month of life.
Most often, start after 3 weeks of age. Sometimes (although rare), they don't appear until the second month of life. - They become larger for 1 year. Then, they fade away over 6 to 8 years without any treatment.
- They run a small risk of bleeding with trauma. Any bleeding should stop with 10 minutes of direct pressure.
- Discuss with your child's doctor on the next regular visit. Call sooner if you are concerned.
- Port-Wine Stain Birthmarks:
- Present at birth in 1 out of 200 newborns
- Deeper in color (dark red or purple) than stork bites (salmon patches)
- Flat, smooth surface
- Natural course: Do not fade or disappear like stork bites. May become darker.
- Grow with the child, but cover the same area
- Treatment: May refer to dermatologist for laser treatments early in infancy
- Call Your Doctor If:
- Your baby starts to look or act abnormal in any way
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 02/25/2023
Last Revised: 12/30/2022
Copyright 2000-2023. Schmitt Pediatric Guidelines LLC.
Dermatoses of pregnancy
Cost: from 1500 rubles
Sign up
Pregnancy is a wonderful time for any woman, especially when it is a planned and desired event in the life of a couple. Unfortunately, due to various circumstances, pregnancy does not always occur naturally - in such cases, modern medicine offers various procedures for assisted reproductive technologies. This makes the woman's attitude to such a natural process even more reverent. And here, often, our skin can present surprises. A number of skin conditions can worsen during pregnancy. However, traditionally prescribed drugs have limitations for use in such a situation. And here it is important that the specialist has experience in treating such situations.
And here it is important that the specialist has experience in treating such situations.
Our Clinic is unique in some way, since many years of experience in managing women with skin diseases during pregnancy is not only the head doctor, who has been a consultant at the D.O. Ott, but also other specialists who are employees of the Department of Skin Diseases of the First Medical University. Academician I.P. Pavlov.
Now let's try to explain the causes and identify the most common skin diseases during pregnancy.
During pregnancy, the main cause of skin lesions is considered to be changes in the immune system of the pregnant woman. Pathological processes can be manifested by an exacerbation of chronic skin diseases or the appearance of specific pregnancy-associated dermatosis, the so-called "pregnancy dermatosis".
Changes on the skin are very diverse both in manifestations and in the mechanisms of development. Conventionally, they can be divided into 3 groups:
I.
 Pregnancy stigmas:
Pregnancy stigmas: Chloasma is the most famous of them. As a development mechanism, various functional endocrine-metabolic changes during pregnancy are assumed. It appears as brownish spots of indefinite outlines, often symmetrical, on the skin of the cheeks, forehead, chin, neck without subjective sensations. Chloasma can occur at different gestational ages, intensifying as it develops and disappearing without a trace shortly after childbirth. But with subsequent pregnancies, chloasma occurs again. Exposure to sunlight enhances the severity of spots.
Pregnancy melanosis - skin changes in the form of hyperpigmentation in the nipples, genitals, white line of the abdomen, also without subjective sensations or inflammation. After childbirth, these disorders disappear. Chloasma and melanosis usually do not require special treatment and spontaneously regress after delivery.
II. Skin diseases that are relatively often registered during pregnancy:
This group includes a variety of skin changes and diseases that often accompany pregnancy, as well as some common dermatoses, the course of which usually worsens during gestation. The main mechanism is a change in hormonal ratios in the body of a pregnant woman. This, in turn, affects the functionality of the immune and nervous systems, the state of the gastrointestinal tract, kidneys, cardiovascular activity, water-salt metabolism, etc.
The main mechanism is a change in hormonal ratios in the body of a pregnant woman. This, in turn, affects the functionality of the immune and nervous systems, the state of the gastrointestinal tract, kidneys, cardiovascular activity, water-salt metabolism, etc.
This group includes: hyperhidrosis
- hypertrichosis
- palmoplantar telangiectasias
- erythema of the palms
- alopecia - hair loss
- onychodystrophy - changes in the nail plates
Most of these and other conditions, as a rule, disappear after childbirth. Their treatment, if necessary, is symptomatic.
The course and severity of symptoms of other skin diseases also change during pregnancy. These primarily include eczema, atopic dermatitis, psoriasis, lichen planus, acne, Dühring's herpetiformis. During pregnancy, they often worsen, and exacerbations are usually more pronounced, more severe than before gestation. Sometimes, on the contrary, during pregnancy, a remission occurs, which continues until childbirth, after which another exacerbation occurs. Correction of exacerbations of these dermatoses during pregnancy is very difficult. Many medicines used under normal conditions affect the development of the fetus. Therefore, external symptomatic therapy becomes the leading method.
Correction of exacerbations of these dermatoses during pregnancy is very difficult. Many medicines used under normal conditions affect the development of the fetus. Therefore, external symptomatic therapy becomes the leading method.
III. Actually dermatoses of pregnant women
The four skin diseases characteristic of pregnancy, gestational pemphigoid, polymorphic dermatosis of pregnancy, atopic dermatitis of pregnancy, and cholestasis of pregnancy can be distinguished by clinical presentation, histopathology, risk of fetal complications. Only gestational pemphigoid and intrahepatic cholestasis of pregnancy are associated with significant risk to the fetus. Because all of these dermatoses are characterized by pruritus, careful evaluation of any pruritic pregnancies is necessary.
Pregnancy pemphigoid , formerly known as herpes gestationis, is the rarest of the skin disorders of pregnancy and is an autoimmune disease. Clinically, it manifests itself in the form of papules and plaques, transforming into vesiculobullous elements, localized in the umbilical region with spread to the chest, back and limbs. Pemphigoid usually resolves spontaneously within a few months after delivery. As a rule, there is a recurrence of dermatosis during subsequent pregnancies with an earlier onset of dermatosis and greater severity compared to the previous pregnancy. Treatment should be aimed at reducing itching and blistering. In mild cases, topical corticosteroids and antihistamines are effective. In severe pemphigoid, it is advisable to use systemic corticosteroids.
Pemphigoid usually resolves spontaneously within a few months after delivery. As a rule, there is a recurrence of dermatosis during subsequent pregnancies with an earlier onset of dermatosis and greater severity compared to the previous pregnancy. Treatment should be aimed at reducing itching and blistering. In mild cases, topical corticosteroids and antihistamines are effective. In severe pemphigoid, it is advisable to use systemic corticosteroids.
Polymorphic dermatosis of pregnancy (PEP) is a benign, pruritic inflammatory disease. It usually occurs at the end of the third trimester or immediately after delivery in the first pregnancy. Urticarial papules and plaques appear first on the abdomen and, unlike gestational pemphigoid, do not affect the umbilical region. The rash usually spreads to the thighs and buttocks, and can rarely be widespread. Eruptions with clear boundaries regress spontaneously within 4-6 weeks without treatment. Treatment for PEP is based on symptomatic relief with topical corticosteroids and antihistamines. If the rash becomes generalized, a short course of systemic corticosteroids may be used.
If the rash becomes generalized, a short course of systemic corticosteroids may be used.
Atopic dermatitis of pregnancy (AEP) is the most common skin disorder in pregnancy. AEP is a benign disease characterized by an pruritic eczematous or papular rash. Two-thirds of AEP cases are characterized by eczematous skin changes localized to atopic areas of the body such as the neck and flexor surfaces of the extremities. The remaining cases are characterized by a papular rash in the abdomen and extremities. Lesions usually respond well to treatment and resolve spontaneously after delivery. However, AEP is more likely to recur in subsequent pregnancies. Dermatosis does not significantly affect the fetus, but there is an increased risk of developing atopic dermatitis in an infant.
Intrahepatic cholestasis of pregnancy (ICP) - characterized by itching with acute onset, which often begins on the palms and soles, and then generalizes. The skin has mostly secondary lesions such as excoriations but may also have papules. In 10%, jaundice develops due to concomitant extrahepatic cholestasis. After giving birth, itching goes away within a few weeks. There is a risk of recurrence in subsequent pregnancies. Diagnosis of ICP is important because there is a risk of complications for both mother and fetus.
The skin has mostly secondary lesions such as excoriations but may also have papules. In 10%, jaundice develops due to concomitant extrahepatic cholestasis. After giving birth, itching goes away within a few weeks. There is a risk of recurrence in subsequent pregnancies. Diagnosis of ICP is important because there is a risk of complications for both mother and fetus.
Treatment is aimed at normalizing the level of bile acids in the blood serum in order to reduce the risk to the fetus and to control symptoms in the mother. Treatment with ursodeoxycholic acid (UDCA) is recommended. Other drugs that reduce itching may be used, such as antihistamines, dexamethasone. Treatment of pregnant women with dermatoses is very difficult, especially in the first trimester of pregnancy. If dermatosis is detected in a pregnant woman, it is necessary to jointly manage it by a dermatologist, an obstetrician-gynecologist. Treatment of dermatoses in pregnant women requires a differentiated approach to therapy, taking into account the duration of pregnancy, exacerbation of the disease and the prevalence of the process.
The clinic has sufficient laboratory facilities and all the necessary equipment for the diagnosis and treatment of conditions such as pregnancy dermatosis.
Rashes in newborns | clinic blog Nashe Vremya
The rash is localized on the face, head, in the oral and nasal cavities, as well as any part of the body. When combing, abrasions and erosion occur, a secondary infection may join.
A rash in a baby does not appear on its own, most often it is a sign of pathological processes in the body, although sometimes it is also a consequence of physiological conditions. Usually accompanied by additional symptoms - fever, sleep disturbance and appetite, joint and muscle pain, nausea, vomiting, weakness.
The rash may look different. First, primary elements are formed:
- pustules - small vesicles with purulent contents
- papules - prominent firm nodules
- bullae blisters raised above the skin
- vesicles - small vesicles up to 5 mm containing exudate
- maculae - flat red spots
- plaques vesicles fused together
- petechiae - subcutaneous hemorrhages caused by capillary injury
- hemorrhages - subcutaneous hemorrhages caused by high permeability of vessel walls
After a while, secondary elements can form on the affected areas:
- hyperpigmentation or depigmentation skin discoloration
- desquamation - scaling of dying epidermis
- erosions - superficial lesions arising from the opening of a vesicle or abscess
- abrasions - violations of the integrity of the skin when scratching
- crusts - formations in place of burst pustules and vesicles
- lichenification - thickening of the skin with enhancement of its pattern
Most rashes are harmless and go away either on their own or with minor interventions. A baby is born with thin and sensitive skin, which tends to react sharply to any stimuli. Because of this, acne, peeling, redness appear. Despite the fact that usually skin manifestations are physiological and disappear on their own, some of them still require a mandatory examination and follow-up by a doctor.
A baby is born with thin and sensitive skin, which tends to react sharply to any stimuli. Because of this, acne, peeling, redness appear. Despite the fact that usually skin manifestations are physiological and disappear on their own, some of them still require a mandatory examination and follow-up by a doctor.
Reasons for appearance
The causes of skin changes and lesions are physiological conditions, various diseases, allergic reactions and physical irritants.
Physiological states
At birth, the baby is covered with primordial lubrication, which protects the skin from pathogenic microorganisms. In the hospital, it is not completely removed so that the skin adapts to the environment. But later, external conditions begin to act on it, causing various reactions that pass over time and are not dangerous for the baby.
A few minutes after childbirth, the color of the skin changes - it becomes bright pink or reddish. This is due to the fact that the air pressure is lower than the pressure of the aquatic environment in which the newborn has been for a long time, blood begins to flow to the skin, changing its color. When the vessels return to normal, it will become the usual pink color. This takes about 2 weeks, premature babies a little more - up to 3 weeks.
When the vessels return to normal, it will become the usual pink color. This takes about 2 weeks, premature babies a little more - up to 3 weeks.
At first, the baby's skin may look like marble due to pink-purple spots. This is how the vessels react to cold, so marbling is usually noticeable when dressing or swaddling until the child is protected by clothes. If the marble spots are uniform and disappear when the baby is warmed, then there is no cause for concern. However, if something worries you, it is better to consult a doctor for advice so as not to miss heart or lung diseases, when marbling is a symptom of oxygen starvation.
On days 2-3, the baby's skin begins to peel off due to the transition to a dry environment after the womb. The degree of peeling is different, in post-term children it is more pronounced. It goes away in a few days. If cracks occur during peeling, you need to use special tools - emollients. However, if the skin bursts and is very desquamated, you need to see a doctor to exclude ichthyosis, hyperkeratosis and other pathologies.
Babies can develop seborrheic dermatitis, which forms in areas with strong sebum production. Appears as yellow scales on the head and behind the ears, less often in the axillary and inguinal folds. The second name for seborrheic dermatitis is "milk crusts". Usually pass without treatment, do not cause itching and do not cause discomfort, although it does not look aesthetically pleasing. To speed up the healing process, you can use baby oil and comb out the scales with a soft baby comb. Sometimes antifungal and anti-inflammatory creams may be needed.
For physiological reasons, various rashes can occur - toxic erythema, neonatal acne, milia. This is normal, because the delicate skin of the baby adapts to new living conditions. A rash in a baby appears due to an increased content of hormones, activation of the sebaceous glands and blockage of the follicles.
Physical influences (overheating, cold, friction)
Baby's skin is sensitive not only to the natural environment, but also to various mechanical influences and irritants. For example, overheating can cause prickly heat, contact with saliva can cause contact dermatitis, and a diaper can cause diaper dermatitis.
For example, overheating can cause prickly heat, contact with saliva can cause contact dermatitis, and a diaper can cause diaper dermatitis.
Infections
Infections that can cause rashes are viral, bacterial, or fungal. In this case, other symptoms are usually present - fever, intoxication, pain. See a doctor as soon as possible if the baby refuses to eat, the rash is accompanied by high fever, pus, severe swelling or redness of the skin. Hemorrhages in the form of red-blue blots, which do not disappear when pressed (test with a glass), require special attention.
Allergy
A rash in newborns can also appear upon contact with an allergen. Allergy can be food, contact, drug, cold, etc. Its symptoms are manifested by rashes, itching, urticaria, Quincke's edema, runny nose, cough, bronchospasm and intestinal disorders (diarrhea, constipation, flatulence, colic). Anaphylaxis is life-threatening and requires an immediate emergency call.
Also, a rash in newborns is caused by autoimmune diseases, vascular and other pathologies of the body, but this happens extremely rarely.
Types of rashes
Types of rash in newborns depend on its cause and are divided into physiological and pathological , and the latter - into infectious, allergic and mechanical .
Physiological
Neonatal acne (neonatal pustulosis)
In the 3rd week of life, 20% of newborns may develop teenage acne. They occur under the influence of hormones and look like pustules with a red border. The rash on the body of the baby is usually localized on the face, sometimes spreads to the scalp, less often to the collar zone. It is not dangerous and goes away on its own in 1-3 months.
With neonatal acne, the skin needs to be properly cleansed and moisturized, and may sometimes require the use of medicated creams. It is absolutely impossible to squeeze pimples and cauterize with alcohol-containing solutions. If the rash in the baby is abundant and leads to secondary infection, you should definitely see a doctor. Acne can drag on for a month or more, then it is considered infantile. If more than six months do not pass, the risk of developing acne in adolescence increases.
If more than six months do not pass, the risk of developing acne in adolescence increases.
Milia
50% of babies develop small yellow or white nodules 1-2 mm in size, called milia or milia. These are cysts of the sebaceous glands that do not require removal. They spread to the face, head, chest and disappear in about a month.
Toxic erythema
This is a benign rash in a newborn child, resulting from the influence of the external environment on delicate skin. Develops by 2-3 days of life in 70% of babies in the form of small red rashes on the face, limbs, trunk. First, small dots appear, which later merge into spots with a 1-2 mm tubercle in the center. Toxic erythema is not dangerous and disappears within a week, sometimes 2-3 weeks. If something worries you, it is better to consult a doctor to rule out infections.
Pathological
Viral eruptions
Chickenpox
It starts with a few blisters and spreads throughout the body, including the scalp and mucous membranes. First, red spots appear, and then turn into bubbles. Then they burst and form crusts that cause itching and bother the baby. The rashes last 5-10 days.
Measles
A highly contagious disease characterized by a small raspberry-red rash that first appears in the mouth, then spreads to the whole body. Affected skin becomes rough, later scaly patches remain for 1–2 weeks. Develops against the background of high temperature.
Rubella
Small pink-red spots appear on the head, and then all over the body, which last 2-4 days, and then disappear. Other symptoms are sore throat, nasal congestion, high fever.
Herpes
A rash in newborns occurs in the form of blisters on the lips and in the oral cavity, which disappears in 1-2 weeks.
Infectious mononucleosis
With infectious mononucleosis, densely spaced pink spots of about 10–15 mm appear. Other symptoms are high fever, swollen lymph nodes, sore throat.
Roseola
First, the temperature rises, after its normalization, small light pink dots appear. It goes away on its own and does not require treatment.
Coxsackie syndrome
Bubble rashes appear on the palms, feet and in the oral cavity. Additional symptoms are fever, vomiting.
Erythema infectiosum (fifth disease)
This is a common viral infection among newborns, which is manifested by a red rash on the cheeks and is accompanied by fever. It resolves on its own in a few days and does not require treatment.
Molluscum contagiosum
Appears as a cluster of white-pink bubbles with curdled contents inside. It is usually localized on the face, neck, eyelids, trunk and extremities.
Bacterial rashes
Scarlet fever
With scarlet fever, numerous red dots appear in the folds of the skin, on the abdomen and on the sides of the body, accompanied by itching and flaking. A distinctive feature is that there are no rashes in the nasolabial triangle. Passes in 3-7 days. Additional symptoms are severe sore throat, crimson tongue.
Meningitis
Terrible disease, accompanied by a rash in the form of hemorrhages caused by rupture of capillaries, which do not go away and do not turn pale when pressed. Additional symptoms are headache, vomiting, pain in the extremities, stiff neck. The disease develops rapidly and can be deadly. If you suspect meningitis, you need to urgently call an ambulance.
Impetigo (streptoderma)
Accompanied by large blisters with purulent contents. Treatment is with topical or systemic antibiotics.
Fungal eruptions
Caused by contact with a fungal infection, they are divided into keratomycosis (damage to the stratum corneum of the epidermis) and dermatophytosis (damage to the skin, hair and nails). Usually appear as red rings on any part of the body. Transmitted from sick animals and people.
Rashes caused by parasites
Scabies
It manifests itself in the form of pairwise located points between the fingers, in the inguinal folds, on the knees and elbows. Accompanied by severe itching and disturb the baby. The reason is the scabies mite. Special creams are usually prescribed, and all family members should be treated.
Allergic rashes
Urticaria
This is an acute allergic reaction in which raised red blisters quickly appear, similar to a nettle burn. It develops suddenly upon contact with an allergen, accompanied by severe itching. It has an acute and chronic character. Occurs with the use of food proteins, viral infections, insect bites and the use of drugs. In severe cases, it is accompanied by Quincke's edema, which requires an ambulance call.
Atopic dermatitis
This is a genetically determined disease associated with a defect in the skin barrier. It is important to note that allergy is not the cause of its occurrence, but rather a consequence. Only in 30% of cases, atopic dermatitis is combined with food allergies. The rash in the baby is localized on the face, buttocks, torso, extensor surfaces of the limbs. It is manifested by redness and peeling, accompanied by itching. Exacerbation is provoked by various triggers - stress, infections, sweat, histamine liberator products, tobacco smoke, animal hair.
For treatment, special creams are used that restore the barrier function - emollients. They need to be used daily, plentifully lubricating the skin. In severe cases, hormonal ointments are prescribed.
Pseudo-allergic
A pseudo-allergic reaction looks like an allergic reaction, but in fact it is not, since its development does not have an immune mechanism. The reasons are an increased content of histamine in foods, the ability of foods to stimulate its release from mast cells, increased absorption of histamine due to gastrointestinal pathologies. Histamine liberators include strawberries, chocolate, cocoa, citrus fruits, cheeses, preservatives, colorants and flavor enhancers. In a breastfed newborn, they arise due to the use of these products by the mother. Treatment consists of a tolerable dose, skin care, and sometimes antihistamines.
Mechanical eruptions
Prickly heat
Appears in the form of small red spots when overheated. It may also look like nodules or vesicles, appears in the folds of the skin, on the face, head, trunk, limbs. The occurrence of prickly heat contributes to an increase in body temperature, overheating due to too warm clothes, the use of things made of dense fabric. Lasts from several hours to several days, air baths speed up the healing process.
To prevent prickly heat, do not wrap the baby while walking, dress according to the principle - plus one layer of clothing relative to an adult. During wakefulness, periodically undress the baby for air baths. If prickly heat has already appeared, choose looser clothes, bathe without soap and protect from overheating.
Contact dermatitis
This is skin damage due to prolonged exposure to various irritants - saliva, fruit and vegetable juices, detergents. In newborns, saliva often causes dermatitis near the mouth and on the neck. Passes when the irritant is eliminated, anti-inflammatory creams are sometimes prescribed.
Diaper dermatitis
Prototype contact dermatitis, only appears under a diaper. The cause is both overheating and contact with urine, sweat and feces. A rash in a baby occurs on the thighs, abdomen, buttocks in the form of red spots, bumps and peeling.
Treatment is carried out according to the abbreviation ABCDE (air, barrier, cleansing, diaper, education) - air, barrier, cleansing, diaper, education. With diaper dermatitis, you need to change diapers every 2-3 hours, arrange air baths when changing clothes, dry the skin thoroughly after bathing, and also lubricate with diaper cream. Sometimes local hormonal agents are used.
How to tell a rash from an allergy
An allergic reaction develops when an allergen enters the body. The immune system rushes to the defense, while blood vessels dilate, the skin turns red and inflamed, rashes appear, and edema may develop. If there was no contact with the allergen, then the rash is most likely not allergic.
It is also worth distinguishing an allergic rash in an infant from an infectious one. With an allergy, it occurs suddenly, with an infection in stages - first it is localized in one place, and then it appears in another, it has clear boundaries of lesions. An infectious rash is contagious, so if one of the family members has it, then it is not an allergy. Viral or bacterial infections are often accompanied by fever, allergies are not. With an allergic rash, there is almost always severe itching, swelling, rhinitis, conjunctivitis may appear.
But still, it is very difficult to establish the cause on your own, so you should consult a doctor for the correct diagnosis and treatment. The doctor may prescribe tests to confirm a particular disease.
What to do if a child has a rash
A rash in a newborn baby can be of different etiologies, in some cases it goes away on its own, and in some it requires treatment. It is especially dangerous to miss formidable diseases such as meningitis or scarlet fever. Since eruptions often occur in greased molds, it is easy to make a mistake.
If simple methods like air baths, using breathable fabrics, frequent diaper changes, using emollients do not help, and even more so if the condition of the newborn worsens - the temperature rises, breathing is difficult, swelling has developed, the baby refuses to eat, urgently seek medical help .
When to see a doctor
In fact, it is better to show any rashes to the doctor. And do it in person, not by photo or video call. The doctor needs not only to examine the rash live, but also to feel, conduct certain tests, and also independently assess the condition of the child. If you find yourself in such a situation, you can contact our specialists.
Pediatricians of the Nashe Vremya clinic work in accordance with the principles of evidence-based medicine. They treat children with great care, carefully and carefully treat babies and are tactful with parents. Here they will not prescribe unnecessary tests, they will not make non-existent diagnoses, they will answer all questions, reassure and prescribe the correct treatment in case it is necessary.
If you want the baby to be examined at home, contact our field service. The pediatrician will arrive on the day of the call, after the examination he will give the necessary recommendations and will observe the baby until he is fully recovered.
We have specialists with extensive experience, as well as great love for their profession and little patients.
Prevention
To prevent rashes, the following measures should be taken:
- take care of the baby's hygiene and wash hands before touching the baby
- monitor the cleanliness of the room, humidify and ventilate in time
- use loose, breathable clothing for the newborn
- avoid overheating and hypothermia of the child
- change diapers more often and take air baths
- limit the amount of contact other people have with the baby
- buy quality toys and baby care products
- if possible, invite a doctor to the house, and not come to the clinic yourself
- avoid contact with allergens
- keep the baby safe from insects
And the most important thing is to vaccinate both the child and others in a timely manner, especially if the child cannot be vaccinated due to age. For example, adults should be vaccinated against influenza or covid.
Methods of treatment
Treatment depends on the cause that caused the damage to the skin. First you need to see a doctor for an accurate diagnosis. Further, depending on the disease, antihistamines, hormonal ointments, emollients, antibiotics, antifungals can be prescribed.
And sometimes a rash in a newborn baby does not need to be treated at all, but just wait. But additional measures may be required - air baths, a comfortable indoor climate, breathable clothing, quality diapers.
Tips for parents
A rash in a baby is not an independent disease or its cause, it is always a symptom. Therefore, it is very important to determine what caused the rash in the baby - allergies, infections, insect bites or mechanical damage.
If the rash is accompanied by fever, the child is lethargic - urgently see a doctor, if hemorrhages appear - immediately call an ambulance! If the rash occurs against the background of the complete health of the child, see the pediatrician in a planned manner.
Terminals
The rash can manifest itself in the form of various elements - from small dots to large blisters and hemorrhages. Types of rash in newborns, as well as their causes, can be completely different:
- physiological - neonatal acne, milia, toxic erythema
- pathological - viral, bacterial, fungal, allergic
- mechanical - prickly heat, contact dermatitis, diaper dermatitis
Therefore, it is important to understand what exactly caused this or that rash in an infant.
Most often, a rash on the body of a baby goes away on its own and does not need treatment, for example, a hormonal rash in a newborn. However, you need to be careful not to miss a serious illness.
It is difficult for parents to figure out the reasons themselves, so it is better to entrust this to a doctor. If the rash is not dangerous, calmly wait until it passes, and if it is the cause of some kind of disease, establish it in time and start treatment.
Sources
1. Kudryavtseva A.V., Atopic dermatitis and food allergy: features of patient management in Russia and other countries (Europe, USA and Japan), School of atopic dermatitis as the basis for successful treatment of children, 2018.
2. Kudryavtseva A.V., Urticaria in children: pathogenetic mechanisms and possibilities of modern therapy, 2017.
3. Revyakina V.A., Urticaria in pediatric practice, 2007.
4. Clinical guidelines: Atopic dermatitis, 2020.
5. Pozdnyakova O.N., Reshetnikova T.B., Bychkov S.G., The structure of the incidence of dermatoses in newborns and infants with a burdened somatic history, 2019.
6. Bokova T.A., Diaper (diaper) dermatitis in a newborn: modern approaches to prevention and treatment, 2019.
7. Gorlanov I.A., Leina L.M., Milyavskaya I.R., Skin of newborns: differential diagnosis of pathological conditions, features of care, 2018.
8. Diagnosis and treatment of seborrheic dermatitis, Gary W Clark et al.