Milk let down feeling
Let-down reflex | Pregnancy Birth and Baby
Let-down reflex | Pregnancy Birth and Baby beginning of content3-minute read
Listen
The let-down reflex is an important part of breastfeeding that starts milk flowing when your baby feeds. Each woman feels it differently, and some may not feel it at all. It can be affected by stress, pain and tiredness but once feeding is established, it requires little or no thought.
What is the let-down reflex?
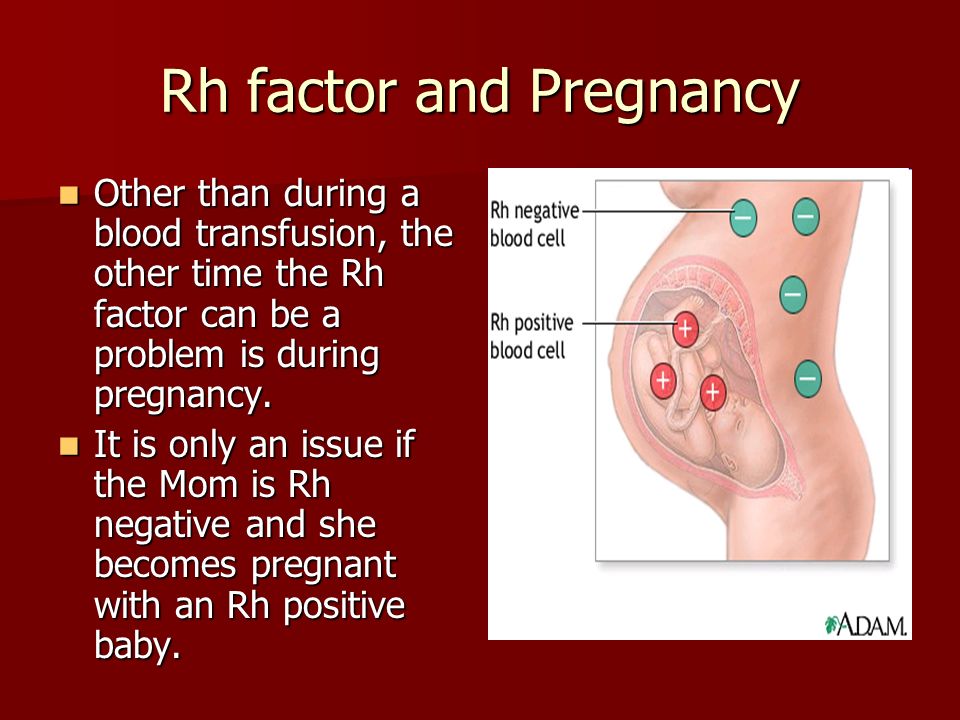
The let-down reflex is what makes breastmilk flow. When your baby sucks at the breast, tiny nerves are stimulated. This causes two hormones – prolactin and oxytocin – to be released into your bloodstream. Prolactin helps make the milk, while oxytocin causes the breast to push out the milk. Milk is then released or let down through the nipple.
Some women feel the let-down reflex as a tingling sensation in the breasts or a feeling of fullness, although others don’t feel anything in the breast.
Most women notice a change in their baby’s sucking pattern as the milk begins to flow, from small, shallow sucks to stronger, slower sucks.
Some women also notice, while feeding or expressing from one breast, that milk drips from the other.
Your let-down reflex needs to be established and maintained to ensure a good supply of milk. This reflex requires no thought, unless you are having problems with breastfeeding.
When does it occur?
The let-down reflex occurs:
- in response to your baby sucking at the breast
- hearing, seeing or thinking about your baby
- using a breast pump, hand expressing or touching your breasts or nipples
- looking at a picture of your baby
- hearing your baby (or another baby) cry
The let-down reflex generally occurs 2 or 3 times a feed. Most women only feel the first, if at all. This reflex is not always consistent, particularly early on, but after a few weeks of regular breastfeeding or expressing, it becomes an automatic response.
Most women only feel the first, if at all. This reflex is not always consistent, particularly early on, but after a few weeks of regular breastfeeding or expressing, it becomes an automatic response.
The let-down reflex can also occur with other stimulation of the breast, such as by your partner.
Strategies to encourage the reflex
The let-down reflex can be affected by stress, pain and tiredness. There are many things to try if you are experiencing difficulty.
- Ensure that your baby is correctly attached to the breast. A well-attached baby will drain a breast better.
- Feed or express in a familiar and comfortable environment.
- Try different methods to help you to relax: calming music, a warm shower or a warm washer on the breast, some slow deep breathing, or a neck and shoulder massage.
- Gently hand express and massage your breast before commencing the feed.
- Look at and think about your baby.
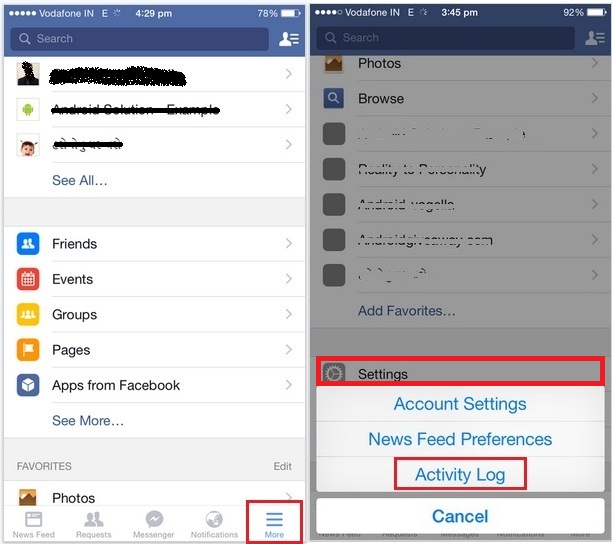
- If you are away from your baby, try looking at your baby’s photo.

- Always have a glass of water nearby.
Milk let-down can be quite forceful, particularly at the beginning of a feed. This fast flow of milk can upset your baby, but it might not mean you have oversupply. It can be managed through expressing before a feed, reclining slightly and burping your baby after the first few minutes. If you continue to have problems, seek advice.
How to deal with unexpected let-down
Until you and your baby fine-tune breastfeeding, many sensations and thoughts can trigger your let-down reflex. Leaking breasts can be embarrassing, but should stop once breastfeeding is fully established.
In the meantime you can feed regularly, apply firm pressure to your breasts when you feel the first sensation of let-down, use breast pads and wear clothing that disguises milk stains.
If you need help and advice:
- Pregnancy Birth and Baby on 1800 882 436
- your maternal child health nurse
- a lactation consultant (your maternity hospital might be able to help)
- Australian Breastfeeding Association on 1800 686 268
Sources:
Australian Breastfeeding Association (Breastfeeding - naturally : the Australian Breastfeeding Association's guide to breastfeeding - from birth to weaning), Australian Breastfeeding Association (Let-down reflex)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2021
Back To Top
Related pages
- Breastfeeding your baby
- How to increase breast milk supply
- Oversupply of breastmilk
Need more information?
Breastfeeding challenges - Ngala
Sometimes breastfeeding can be challenging
Read more on Ngala website
Breast refusal and baby biting breast | Raising Children Network
Breast refusal or baby biting breast are common breastfeeding issues. These issues might resolve themselves, or your child and family health nurse can help.
Read more on raisingchildren.net.au website
Breastfeeding - expressing breastmilk - Better Health Channel
Expressing breast milk by hand is a cheap and convenient method.
Read more on Better Health Channel website
Breast feeding your baby - MyDr.com.au
Breast milk has long been known as the ideal food for babies and infants. Major health organisations recommend that women breast feed their babies exclusively until they are 6 months old, and continue breast feeding, along with solids, until they are 12 months old or more. Breast milk has many benefits.
Read more on myDr website
Expressing and storing breast milk
This page includes information about expressing, storing, cleaning equipment, transporting and preparing expressed breastmilk for your baby.
Read more on WA Health website
Expressing breastmilk & storing breastmilk | Raising Children Network
You can express breastmilk by hand, or with a manual or an electric pump. Store expressed breastmilk in special bags or containers in the fridge or freezer.
Store expressed breastmilk in special bags or containers in the fridge or freezer.
Read more on raisingchildren.net.au website
Mastitis, blocked duct & breast abscess | Raising Children Network
If you think you have a blocked milk duct, you can treat it at home to start with. If you think you have mastitis or a breast abscess, see your GP as soon as possible.
Read more on raisingchildren.net.au website
Weaning at 6 Months | Tresillian
Babies start weaning when they begin consuming foods other than breastmilk. For advice on weaning check out Tresillian's tip page.
Read more on Tresillian website
Frequently asked questions about alcohol and pregnancy | FASD Hub
We've answered some common questions about alcohol use during pregnancy and breastfeeding, and about living with fetal alcohol spectrum disorder (FASD).
Read more on FASD Hub Australia website
Breastfeeding challenges - Ngala
Many new mothers experience breastfeeding challenges
Read more on Ngala website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What You Should Know About Your Let Down Reflex
Written by WebMD Editorial Contributors
In this Article
- How Does the Let Down Reflex Work?
- What Are Signs of a Good Let Down?
- Complications of the Let Down Reflex
When your baby first latches on to nurse, they don’t actually get much milk at first. Instead, their suckling sends a message to your body to release the milk stored in your breasts. The strength and timing of the let down reflex, also called the milk ejection reflex, varies from mother to mother.
Instead, their suckling sends a message to your body to release the milk stored in your breasts. The strength and timing of the let down reflex, also called the milk ejection reflex, varies from mother to mother.
How Does the Let Down Reflex Work?
If milk came out of your breasts instantly when your baby latched on, you’d probably leak constantly. Instead, your breasts store the milk until it’s needed. Most often, your let down reflex is triggered by a particular suckling motion your baby makes to stimulate milk production.
The let down reflex is a physiological response to your baby’s sucking. They stimulate small nerves in the nipple, which causes prolactin and oxytocin to produce milk and let down milk, respectively. The reflex is often accompanied by a tingling sensation in the nipple, but not all women experience that.
If you pay attention to your baby’s nursing patterns, at first their suckling will be faster and shallower to stimulate the release of milk. Once your milk lets down and your baby is drinking, their suckles will be deeper and longer. If they nurse longer and need more milk, they may adjust how they suck to stimulate more milk flow.
Once your milk lets down and your baby is drinking, their suckles will be deeper and longer. If they nurse longer and need more milk, they may adjust how they suck to stimulate more milk flow.
Other let down triggers. Since your brain is wired to care for a newborn, other things may trigger the let down reflex. If your baby cries, or if you hear any baby cry, your milk may let down in response. If you go too long without nursing and your breasts get too full, your let down reflex may trigger to relieve the pressure.
Strong emotions may also trigger a let down of milk. If you are feeling intensely stressed, angry, or sad, your body may take that as a sign that you need to nurse your baby or release milk to alleviate pressure.
If your milk is not letting down, you can physically stimulate the nipple to allow let down. Try gently rolling your hand down your breast toward the nipple, then massage gently. It can also help to relax and think about your baby.
What Are Signs of a Good Let Down?
Breastfeeding is wonderful for your baby, but it is often full of doubts and questions. Are you producing enough milk? Are you doing it right? This extends to the let down reflex, too. You may wonder if your let down is strong enough or too strong.
Here are signs of a healthy, functioning let down response:
Uterine cramps. You may notice that your uterus cramps during a let down in the days following birth. This is natural and nothing to be concerned about. As with menstrual cramps, for some the cramps are mild and barely noticeable, while for others the contractions can be more painful.
Change in sucking pattern. You may notice a change in your baby’s sucking pattern during a nursing session. Their suckle will go from being short and fast to long and slow once milk lets down. If they need more milk, their sucking may change again to encourage another let down.
Your feelings. Moms often report that they feel very relaxed and even sleepy when their milk lets down. This is a side effect of the oxytocin released during let down. You may also feel suddenly thirsty, which is your body’s way of preparing to replace the milk being removed during a nursing session.
Moms often report that they feel very relaxed and even sleepy when their milk lets down. This is a side effect of the oxytocin released during let down. You may also feel suddenly thirsty, which is your body’s way of preparing to replace the milk being removed during a nursing session.
Complications of the Let Down Reflex
Oversupply milk ejection reflex. A powerful let down is often accompanied by an oversupply of milk, sometimes called oversupply milk ejection reflex (O-MER). When your let down happens, you may notice that your baby sputters, coughs, and even chokes on your milk. Your baby may bite down to slow the milk flow. You may leak when not nursing or notice that your baby has more frequent but short feedings if you have an oversupply.
If this happens, keep a bib or cloth handy to catch your milk when it first lets down so that your baby doesn’t choke. After a moment when the let down slows, you can try latching your baby again. You can also restrict your milk flow by squeezing your areola during breastfeeding.
Talk to your doctor about safe ways to decrease your oversupply so that your let down is less strong.
Dysphoric milk ejection reflex. In some women, breastfeeding can create a negative physiological response, leading to negative emotions like guilt, anxiety, depression, and sadness. It is usually an isolated response that occurs only when you first let down your milk and into the first few minutes of breastfeeding. This is called dysphoric milk ejection reflex (D-MER) and is different from postpartum depression.
There is still more research needed on the causes and effects of D-MER. Talk to your doctor if you are struggling with negative emotions during breastfeeding.
Weak let down. You may have a weak let down if your baby seems frustrated while nursing. They may not be getting enough milk, or they may not be getting milk as fast as they want it. Using a breast pump can supplement less successful nursing sessions.
When pumping, look at photos and videos of your baby to try and encourage a let down. And just as you do when breastfeeding, try to relax. Take deep breaths and think about your little one, letting go of any stress.
And just as you do when breastfeeding, try to relax. Take deep breaths and think about your little one, letting go of any stress.
Signs of lack of milk | Improving lactation
Many mothers are concerned about insufficient milk production, but it is not always easy to find out if milk is really low. Read our article to understand if this is true and what can be done about it.
Share this information
“Do I have enough milk?” - a question that is often asked by young mothers. If your baby is healthy and growing well, there is no reason to worry. However, if you are still worried about milk production, it is best to consult a specialist as soon as possible. If everything is in order, he will be able to calm you down. In addition, you will not needlessly feed the baby formula, because of which milk production can really decrease.
Causes of insufficient milk supply
Some mothers do not produce enough breast milk for medical reasons, which include: approximately three days after birth). 1
1
If you have any of the conditions listed, contact your lactation consultant or healthcare provider.
How milk is produced
With the advent of milk, the breast begins to work on the principle of supply and demand. Each time after it is emptied, whether it is feeding the baby or pumping, even more milk will be produced.
This is why milk production may be reduced if you give formula to your baby - your body will not get the signal to produce more milk because it will remain.
The way your baby eats also affects milk production. The more often and better he sucks the breast, the bigger it will be. If your baby eats only a small portion at one feeding, it is necessary to express milk regularly to maintain the level of its production. Read more about this below.
Signs that the baby is not getting enough milk
Although low milk production is rare, the baby may have difficulty feeding in the first few weeks, but for other reasons. You may not be feeding him often enough or for enough time, especially if you're trying to stick to a specific schedule. The baby may not latch on properly, or it may have features that make it difficult to take in milk.
The following signs indicate that the baby is not getting enough milk:
- Poor weight gain. In the first few days of life, newborns normally lose 5 to 7%, and sometimes even up to 10%, of their birth weight. However, after that, they should gain at least 20–30 g per day and regain their birth weight by 10–14 days.
 5,6,7 If your baby has lost 10% or more of their weight in the early days, or has not started gaining weight by 5-6 days, you should contact your doctor immediately.
5,6,7 If your baby has lost 10% or more of their weight in the early days, or has not started gaining weight by 5-6 days, you should contact your doctor immediately. - Not enough wet and soiled diapers. A good indicator of whether a baby is getting enough milk is the number of diapers used per day. Check out our article detailing the norm for wet and soiled diapers in Breastfeeding Your Newborn: What to Expect in the First Week. Seek medical advice if something bothers you or you notice that the number of soiled diapers has begun to decrease.
- Dehydration. If your baby has dark urine, dry mouth or jaundice (yellowing of the skin or eyes), or baby is lethargic, has lost appetite, and may be dehydrated. 6 Dehydration can be caused by fever, diarrhoea, vomiting or overheating. If you notice any of these symptoms, seek medical attention as soon as possible.
Misconceptions about lack of milk
Newborns usually eat very frequently, about 10-12 times a day or every two hours. This does not mean that they do not have enough milk. Keep in mind that breastfeeding is also about comfort, so it's hard to tell how much milk a baby eats at each feed as the amount can vary.
This does not mean that they do not have enough milk. Keep in mind that breastfeeding is also about comfort, so it's hard to tell how much milk a baby eats at each feed as the amount can vary.
You have enough milk even if:
- the child wants to eat often;
- the child does not want to be laid down;
- the child wakes up at night;
- feeding is fast;
- feeding takes a long time;
- after feeding, the child takes another bottle;
- Your breasts are softer than in the first weeks;
- milk does not leak or has stopped leaking;
- You cannot express much milk;
- You have small breasts.
What to do about insufficient milk production
If you suspect that your baby is not getting enough milk, contact a lactation consultant or your doctor. He will determine if you have enough milk and check how the baby is latch-on and if he is getting enough milk. He may also suggest changing the feeding position or the way the baby is attached to the breast to make it easier.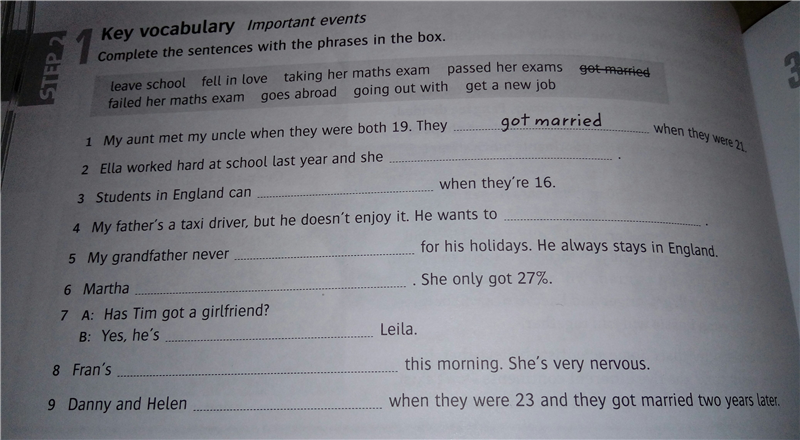
Also try holding your baby close to you more often to increase skin-to-skin contact before and during feedings. This stimulates the production of the hormone oxytocin, which promotes milk flow. Use relaxation techniques, such as listening to your favorite soothing music, to reduce anxiety that can negatively impact milk production. 8
With proper support, most under-lactating mothers can breastfeed their babies at least partially, and some manage to normalize production.
If your baby is unable to get enough milk directly from the breast (perhaps because he was born prematurely or has special needs), you need to express milk to support his production. Your doctor may prescribe you special drugs that stimulate lactation.
If you are unable to express enough milk, you will need to supplement your baby with donor milk or formula. This should also take place under the supervision of a physician. The Supplemental Nursing System (SNS)* is a great way to help your baby get all the milk he needs at the breast.
How to increase your milk production with a breast pump
If you need to increase your milk production in the first five days after giving birth, you can use a dual electronic breast pump with lactation start technology, such as the Medela Symphony**. Such a breast pump imitates the sucking of the breast by a child and helps to increase milk production in the future. 9
After your milk comes in, double pumping allows you to get more milk in less time. 10 This method helps to better empty the breast, which also improves lactation.
Although every mother is different, it is often recommended to express milk immediately or one hour after a feed. This may seem strange, since it is usually easier to express milk from a full breast. However, the pumping session should be seen as an "investment in tomorrow."
You will probably only be able to express a little milk at first, but don't be discouraged - if you express regularly, your milk supply will increase. Try to empty your breasts - by putting your baby to your breast or expressing milk - 8 to 12 times a day, including one nightly session, when your levels of prolactin (the hormone responsible for producing milk) are highest. The more often you empty your chest, the better. After two to three days of regular pumping, you will notice a significant increase in milk production. For tips on how to get more milk with every pump, see Tips for Using a Breast Pump.
Try to empty your breasts - by putting your baby to your breast or expressing milk - 8 to 12 times a day, including one nightly session, when your levels of prolactin (the hormone responsible for producing milk) are highest. The more often you empty your chest, the better. After two to three days of regular pumping, you will notice a significant increase in milk production. For tips on how to get more milk with every pump, see Tips for Using a Breast Pump.
Pumping with massage to get more milk
If your baby is not lating at all or you are not yet able to express enough milk for him, a technique called “massage pumping” may be helpful. It helps mothers increase the amount of milk they get in one pumping session. 11.12 The whole process takes about 25-30 minutes. Remember that the better you empty your breast, the faster milk is produced in it.
A few simple steps are required:
- Massage your breasts.
- Perform a double pump while wearing a special bustier top that allows you to keep your hands free.
- While expressing, squeeze the chest with all fingers for a few seconds. Release and repeat. Squeeze both breasts until the milk flows in a thin stream.
- Massage the chest again.
- Express milk manually or with a single breast pump, squeezing each breast in turn to empty them as completely as possible.
When your baby starts to gain weight and milk production increases, you can switch to exclusive breastfeeding.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. 9 E et al . Breastfeeding in polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2008;87(5):531-535. - Wanky, I. et al., "Breastfeeding in the setting of polycystic ovaries." Akta Obstet Ginecol Scand. 2008;87(5):531-535.
Acta Obstet Gynecol Scand. 2008;87(5):531-535. - Wanky, I. et al., "Breastfeeding in the setting of polycystic ovaries." Akta Obstet Ginecol Scand. 2008;87(5):531-535.
3 Neifert MR et al. Lactation failure due to insufficient glandular development of the breast. Pediatrics. 1985;76(5):823-828. - Neifert M.R. et al., "Inability to Lactate Due to Deficiency of Glandular Breast Tissue". Pediatrix (Pediatrics). 1985;76(5):823-828.
4 Neifert M et al. The influence of breast surgery, breast appearance, and pregnancy-induced breast changes on lactation sufficiency as measured by infant weight gain. Birth. 1990;17(1):31-38. - Neifert M. et al., "Influence of breast surgery, breast appearance, and pregnancy-induced breast changes on milk supply as measured by weighing the baby." Bers. 1990;17(1):31-38.
5 C Tawia S, McGuire L. Early weight loss and weight gain in healthy, full-term, exclusively-breastfed infants. Breastfeed Rev . 2014;22(1):31-42. - S. Tavia S., McGuire L., "Natural Weight Loss and Gain in Healthy, Exclusively Breastfed Full-Term Infants." Brestfeed Rev (Breastfeeding Review). 2014;22(1):31-42.
Breastfeed Rev . 2014;22(1):31-42. - S. Tavia S., McGuire L., "Natural Weight Loss and Gain in Healthy, Exclusively Breastfed Full-Term Infants." Brestfeed Rev (Breastfeeding Review). 2014;22(1):31-42.
6 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
7 World Health Organization. [Internet]. Neonatal Care . 2012;12(2):112-119 - Keith D.R. et al., "Effects of listening to music on the amount, fat content, composition and calorie content of breast milk in mothers of premature and seriously ill children. " Adv Neonatal Care. 2012;12(2):112-119
" Adv Neonatal Care. 2012;12(2):112-119
9 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J. Perinatol. 2012;32(2):103-10. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants." J Perinatol (Journal of Perinatology). 2012;32(2):103-10.
10 Prime DK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression.Breastfeed Med . 2012;7(6):442-447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
11 Stanford University School of Medicine [Internet]. Stanford, CA, USA: Maximizing Milk Production with Hands-On Pumping; 2017. [ Accessed 04/30/2018]. - Stanford University School of Medicine [Internet]. Stanford, CA, USA: "Increased milk production from hand expression"; 2017. [Page accessed 04/30/2018].
Stanford, CA, USA: Maximizing Milk Production with Hands-On Pumping; 2017. [ Accessed 04/30/2018]. - Stanford University School of Medicine [Internet]. Stanford, CA, USA: "Increased milk production from hand expression"; 2017. [Page accessed 04/30/2018].
12 Morton J et al. Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. J. Perinatol. 2009;29(11):757-764. - Morton J. et al., "Manual pumping combined with an electric breast pump increases breast milk production in mothers of preterm infants." J Perinatol (Journal of Perinatology). 2009;29(11):757.
Read instructions before use. Consult a specialist about possible contraindications.
*RU No. FSZ 2010/07352 dated 07/19/10
** RU No. FCZ 2010/06525 dated 17/03/2021
myths about breast and breastfeeding
myth:
Reality:
MIF:
Breastfeeding with small breasts or inverted nipples is not possible.
REALITY:
The size of the breast does not matter, what is important is the maturity of the mammary glands, which are finally prepared for feeding during pregnancy. The shape of the nipple can create problems at the beginning of feeding, but over time these features get used to and the difficulties are overcome.
MYTH:
Failure to feed the first child precludes breastfeeding.
REALITY:
Much of the failure to feed is due to the correct sucking technique of the baby. Usually, women have more milk after their second pregnancy, and if the baby suckles well, everything may be fine.
MYTH:
A woman can always determine breast fullness by her feelings, there is no milk in soft breasts.
REALITY:
The feeling of fullness in the breasts always disappears in the normal way in the second or third month of feeding, the breasts become "empty" and decrease in size. This does not mean that there is not enough milk. Just in case, you can track how much the baby gains weight per week. If he adds well, at least 150 grams per week, there is no reason to worry.
If he adds well, at least 150 grams per week, there is no reason to worry.
MYTH:
Breast milk can be controlled by pumping.
REALITY:
Normal breastfeeding does not require pumping at all. It is absolutely not suitable for self-control, because the child always stimulates the breast more than any device.
MYTH:
In hot weather, give your baby water.
REALITY:
In the first six months of life, a baby does not need anything but breast milk, and he does not need water. Breast milk always contains a sufficient amount of liquid that is well absorbed by the baby. If it is hot, the baby will usually ask for the breast more often, thereby covering the increased need for fluids. Giving your baby extra drinks all the time can interfere with the flow of breastfeeding because the baby's stomach simply won't fit the right amount of breast milk. If the child is offered additional drinks for a long time, this can lead to a decrease in the baby's appetite.
MYTH:
The quantity and quality of breast milk can be improved by eating (halvah) or drinking (milk tea).
REALITY:
The quality of breast milk is practically independent of the mother's diet. All the components necessary for the child - water, proteins, carbohydrates and fats - are present in breast milk even when the mother's nutrition is limited. Only the content of water-soluble vitamins (vitamin C and B vitamins) is directly dependent on the mother's diet. Therefore, vegan mothers should make sure that they are getting enough vitamins D and B12, iron, calcium and zinc during breastfeeding. The amount of breast milk directly depends on the needs of the child, and only as much breast milk is produced as needed at the moment. The baby should ask for the breast at least eight times a day and gain an average of 600-800 grams in weight every month. In this case, everything is in order with his food. More frequent feedings increase the amount and fat content of milk.