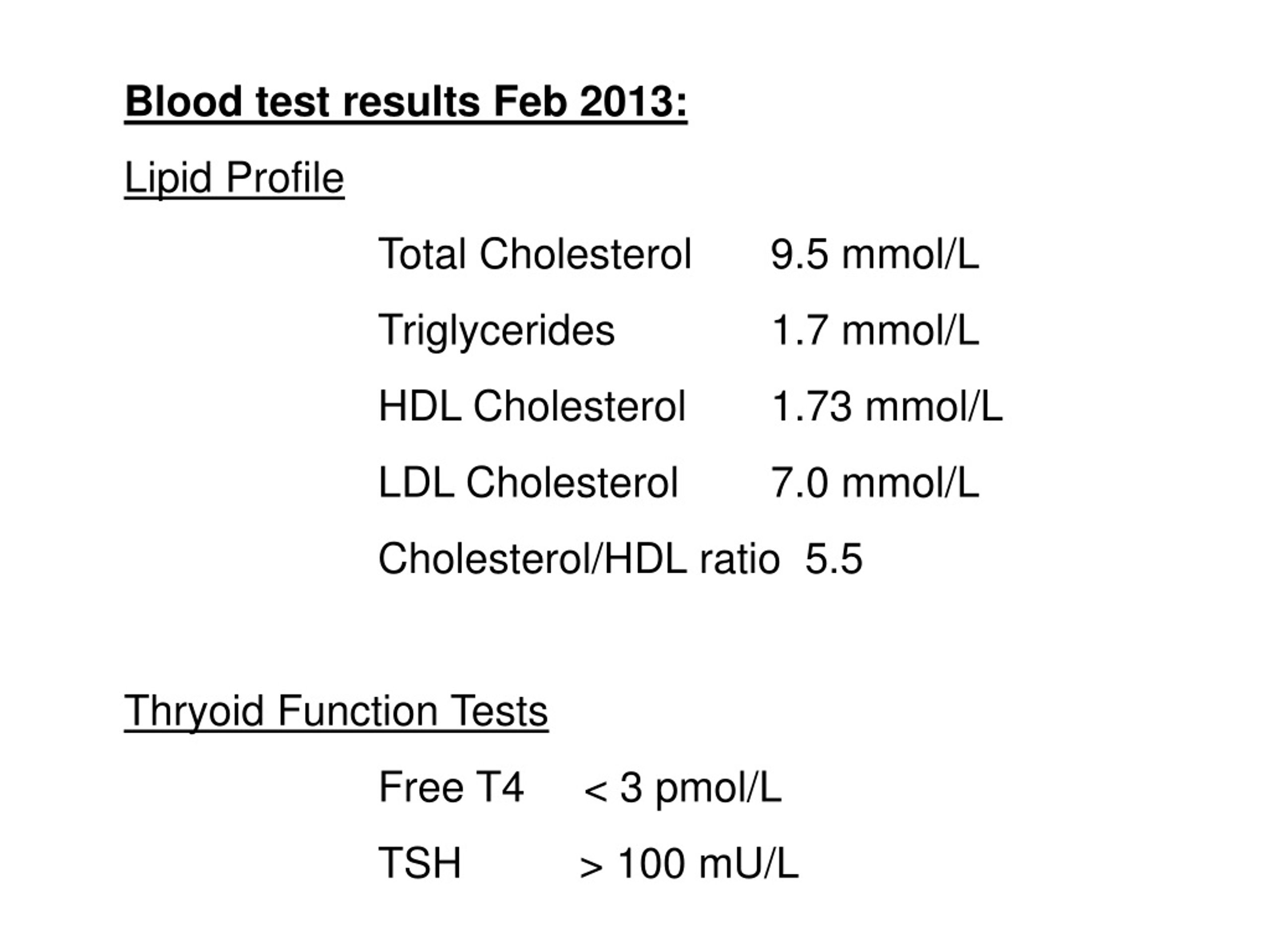
10 week blood test
Prenatal Genetic Screening Tests | ACOG
Amniocentesis: A procedure in which amniotic fluid and cells are taken from the uterus for testing. The procedure uses a needle to withdraw fluid and cells from the sac that holds the fetus.
Aneuploidy: Having an abnormal number of chromosomes. Types include trisomy, in which there is an extra chromosome, or monosomy, in which a chromosome is missing. Aneuploidy can affect any chromosome, including the sex chromosomes. Down syndrome (trisomy 21) is a common aneuploidy. Others are Patau syndrome (trisomy 13) and Edwards syndrome (trisomy 18).
Carrier Screening: A test done on a person without signs or symptoms to find out whether he or she carries a gene for a genetic disorder.
Cell-Free DNA: DNA from the placenta that moves freely in a pregnant woman’s blood. Analysis of this DNA can be done as a noninvasive prenatal screening test.
Cells: The smallest units of a structure in the body. Cells are the building blocks for all parts of the body.
Chorionic Villus Sampling (CVS): A procedure in which a small sample of cells is taken from the placenta and tested.
Chromosomes: Structures that are located inside each cell in the body. They contain the genes that determine a person’s physical makeup.
Cystic Fibrosis (CF): An inherited disorder that causes problems with breathing and digestion.
Diagnostic Tests: Tests that look for a disease or cause of a disease.
DNA: The genetic material that is passed down from parent to child. DNA is packaged in structures called chromosomes.
Down Syndrome (Trisomy 21): A genetic disorder that causes abnormal features of the face and body, medical problems such as heart defects, and mental disability. Most cases of Down syndrome are caused by an extra chromosome 21 (trisomy 21).
Edwards Syndrome (Trisomy 18): A genetic condition that causes serious problems. It causes a small head, heart defects, and deafness.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Genes: Segments of DNA that contain instructions for the development of a person’s physical traits and control of the processes in the body. The gene is the basic unit of heredity and can be passed from parent to child.
Genetic Counselor: A health care professional with special training in genetics who can provide expert advice about genetic disorders and prenatal testing.
Genetic Disorders: Disorders caused by a change in genes or chromosomes.
Inherited Disorders: Disorders caused by a change in a gene that can be passed from parents to children.
Monosomy: A condition in which there is a missing chromosome.
Mutations: Changes in genes that can be passed from parent to child.
Neural Tube Defects (NTDs): Birth defects that result from a problem in development of the brain, spinal cord, or their coverings.
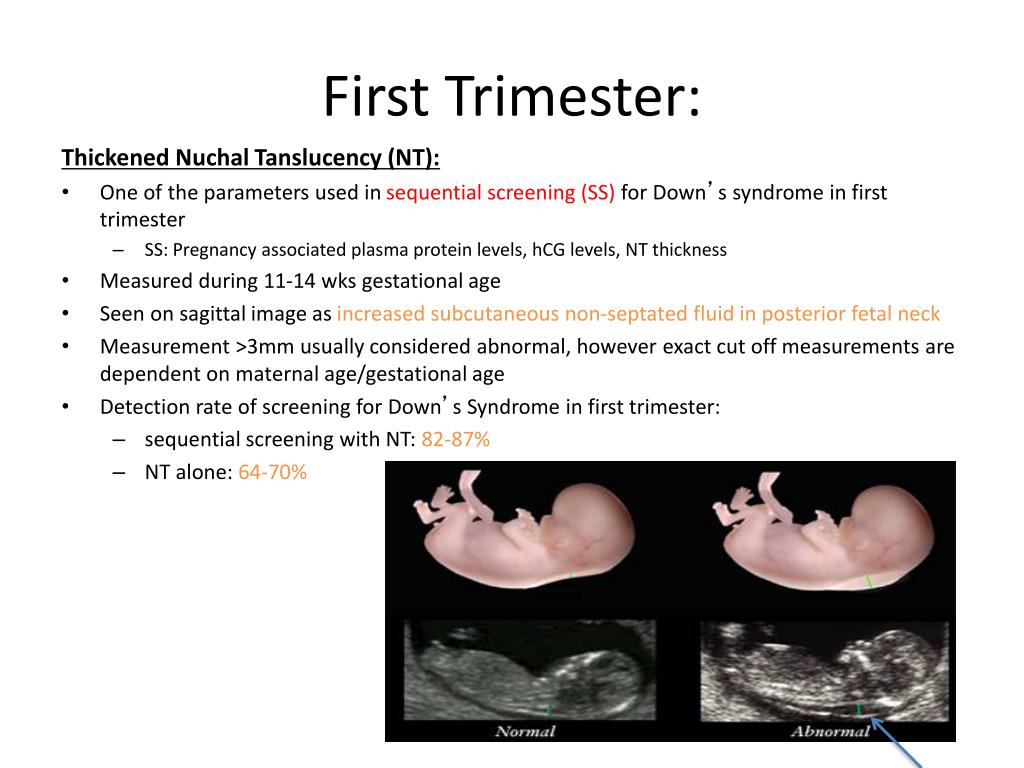
Nuchal Translucency Screening: A test to screen for certain birth defects, such as Down syndrome, Edwards syndrome, or heart defects. The screening uses ultrasound to measure fluid at the back of the fetus’s neck.
Obstetrician: A doctor who cares for women during pregnancy and their labor.
Patau Syndrome (Trisomy 13): A genetic condition that causes serious problems. It involves the heart and brain, cleft lip and palate, and extra fingers and toes.
Placenta: An organ that provides nutrients to and takes waste away from the fetus.
Screening Tests: Tests that look for possible signs of disease in people who do not have signs or symptoms.
Sex Chromosomes: The chromosomes that determine a person’s sex. In humans, there are two sex chromosomes, X and Y. Females have two X chromosomes and males have an X and a Y chromosome.
Sickle Cell Disease: An inherited disorder in which red blood cells have a crescent shape, which causes chronic anemia and episodes of pain.
Tay–Sachs Disease: An inherited disorder that causes mental disability, blindness, seizures, and death, usually by age 5.
Trimester: A 3-month time in pregnancy. It can be first, second, or third.
Trisomy: A condition in which there is an extra chromosome.
Ultrasound Exams: Tests in which sound waves are used to examine inner parts of the body. During pregnancy, ultrasound can be used to check the fetus.
First trimester tests during pregnancy
Written by WebMD Editorial Contributors
Routine tests help keep close tabs on you and your baby. That’s why it’s so important to keep all your prenatal appointments. Screening tests can spot potential problems early.
That’s why it’s so important to keep all your prenatal appointments. Screening tests can spot potential problems early.
These tests usually include:
History and physical exam. During your first or second prenatal visit, you’ll answer a lot of questions about your health and family history. This information helps the doctor know whether you have any specific risks to address, such as an inherited genetic disorder. You will also have a physical exam. Your doctor will calculate your due date based on the date of your last menstrual period.
Pelvic exam and Pap smear.Prenatal testing during the first trimester begins with a pelvic exam and Pap smear to check the health of your cervical cells. This testing screens for cervical cancer and for certain sexually transmitted diseases (STDs).
Blood tests. During one of your first visits, your doctor or midwife will identify your blood type and Rh (rhesus) factor, screen for anemia, check for immunity to rubella (German measles), and test for hepatitis B, syphilis, and HIV and other STDs.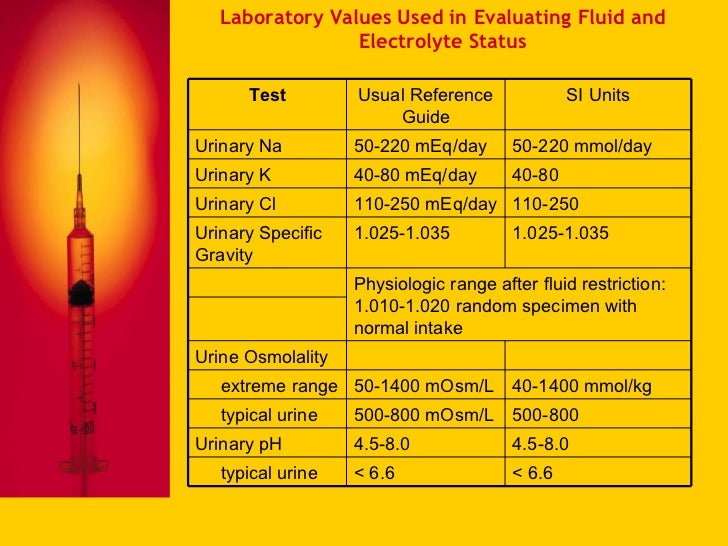
Depending on racial, ethnic, or family background, you may be offered tests and genetic counseling to assess risks for diseases such as Tay-Sachs, cystic fibrosis, and sickle cell anemia (if these weren't done at a preconception visit). Testing for some of these diseases can also be done with saliva.
You might be tested for exposure to diseases such as toxoplasmosis and varicella (the virus that causes chickenpox. Your health care provider may also want to check your levels of hCG, a hormone secreted by the placenta, and progesterone, a hormone that helps maintain the pregnancy.
Urine tests. You will also be asked early on for a urine sample so that your doctor or midwife can look for signs of kidney infection and, if necessary, can confirm your pregnancy by measuring the hCG level. (A blood hCG test to confirm pregnancy may be used instead.) Urine samples will be collected regularly to spot glucose (a sign of diabetes) and protein, which could show preeclampsia, a pregnancy-induced disease marked by high blood pressure.
In the later part of the first trimester you will be offered genetic testing. Some people feel like these tests may cause them undue stress, and they prefer to make sure the baby is genetically normal after delivery. Others want all the testing they can get, realizing that these tests sometimes are not 100% accurate. Talk with your doctor or with a genetic counselor about the pros and the cons before you decide. There are different genetic testing options that involve blood tests alone or with an ultrasound that involve no risk to the fetus. If these noninvasive tests are abnormal, you might have further tests.
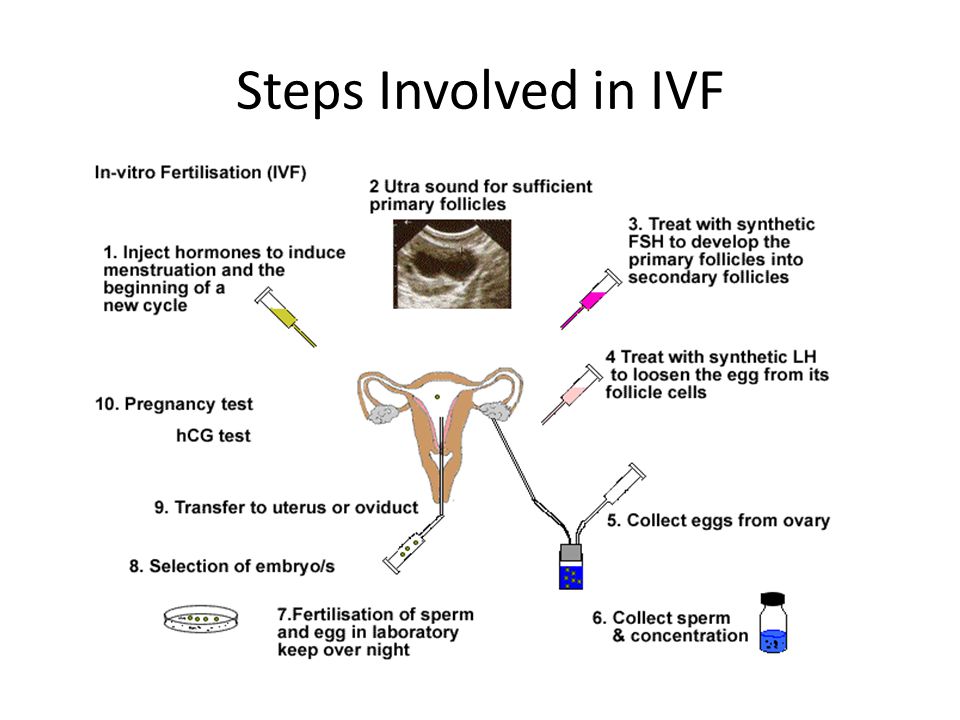
One first semester genetic test combines a blood test with an ultrasound to screen for Down syndrome. It may be available between 11 and 14 weeks of pregnancy. The results of a blood test that measures hCG and PAPP-A (pregnancy-associated plasma protein A) in maternal blood are used with an ultrasound measurement of the skin at the back of the fetus’ neck (called nuchal translucency). The procedure may be able to spot many Down syndrome cases and other genetic conditions. However, as with all screening methods, a more invasive diagnostic technique like CVS is used if results are positive.
The procedure may be able to spot many Down syndrome cases and other genetic conditions. However, as with all screening methods, a more invasive diagnostic technique like CVS is used if results are positive.
Noninvasive prenatal testing (NIPT). This cell-free fetal DNA test can be done as early as after 10 weeks of pregnancy. The test uses a blood sample to measure the relative amount of free fetal DNA in a mother's blood. It's thought that the test can detect 99% of all Down syndrome pregnancies. It also tests for some other chromosomal abnormalities.
Chorionic villus sampling (CVS). If you're 35 or older, have a family history of certain diseases, or have had a positive result on noninvasive genetic tests, you will be offered this invasive test, usually between 10 and 12 weeks of pregnancy. CVS can detect many genetic defects, such as Down syndrome, sickle cell anemia, cystic fibrosis, hemophilia, and muscular dystrophy. The procedure involves threading a tiny catheter through your cervix or inserting a needle into your abdomen to get a tissue sample from the placenta. The procedure carries a 1% risk of inducing miscarriage and is about 98% accurate in ruling out certain chromosomal birth defects. But, in contrast to amniocentesis, it does not help in detecting neural tube disorders, such as spina bifida and anencephaly, or abdominal wall defects.
The procedure carries a 1% risk of inducing miscarriage and is about 98% accurate in ruling out certain chromosomal birth defects. But, in contrast to amniocentesis, it does not help in detecting neural tube disorders, such as spina bifida and anencephaly, or abdominal wall defects.
Be sure to discuss all of your testing options with your doctor so that together you can decide on the ones that will be best for you.
If you’re expecting twins, it’s a high-risk pregnancy. For this reason, your doctor will want to watch you and your babies closely. You'll have all the routine tests, but expect to have some of them earlier and more often.
Your doctor may suggest that you see a perinatologist, also called a maternal fetal medicine specialist. These doctors are obstetricians who specialize in high-risk pregnancies. They may work with your regular obstetrician to manage your pregnancy and order tests.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Citizens | Ministry of Health of the Kaliningrad Region
| Gestational age | Analyzes | Events (registration, medical examinations, doctor visit schedule) |
| Up to 12 weeks | Early registration in the antenatal clinic Taking medications: folic acid throughout the first trimester, no more than 400 mcg / day; potassium iodide 200-250 mcg/day (in the absence of thyroid disease) | |
| At first appearance | An obstetrician-gynecologist collects anamnesis, conducts a general physical examination of the respiratory, circulatory, digestive, urinary system, mammary glands, anthropometry (measurement of height, body weight, determination of body mass index), measurement of the size of the pelvis, examination of the cervix in the mirrors, bimanual vaginal study | |
| Not later than 7-10 days after the initial visit to the antenatal clinic | Inspections and consultations: - general practitioner; - a dentist; - an otolaryngologist; - an ophthalmologist; - other medical specialists - according to indications, taking into account concomitant pathology | |
| First trimester (up to 13 weeks) (and at first visit) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol. 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, to the herpes simplex virus (HSV), to cytomegalovirus (CMV), determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of the main blood groups (A, B, 0) and Rh-affiliation. In Rh-negative women: a) examination of the father of the child for group and Rh-affiliation. 7. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 8. Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida. 9. PCR chlamydial infection, PCR gonococcal infection, PCR mycoplasma infection, PCR trichomoniasis. | Visiting an obstetrician-gynecologist every 3-4 weeks (with the physiological course of pregnancy). Electrocardiography (hereinafter - ECG) as prescribed by a general practitioner (cardiologist). Up to 13 weeks of pregnancy are accepted: - folic acid no more than 400 mcg / day; - potassium iodide 200-250 mcg / day (in the absence of thyroid disease) |
| 1 time per month (up to 28 weeks) | Blood test for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 11-14 weeks | Biochemical screening for serum marker levels: - pregnancy-associated plasma protein A (PAPP-A), - free beta subunit of human chorionic gonadotropin (hereinafter - beta-CG) | In the office of prenatal diagnostics, an ultrasound examination (hereinafter referred to as ultrasound) of the pelvic organs is performed. According to the results of complex prenatal diagnostics, a conclusion of a geneticist is issued. |
| After 14 weeks - once | Culture of midstream urine | To exclude asymptomatic bacteriuria (the presence of bacterial colonies of more than 105 in 1 ml of an average portion of urine, determined by a culture method without clinical symptoms) to all pregnant women. |
| In the second trimester (14-26 weeks) | General (clinical) analysis of blood and urine. | Visiting an obstetrician-gynecologist every 2-3 weeks (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), uterine tone, palpation of the fetus, auscultation of the fetus with a stethoscope. Potassium iodide 200-250 mcg/day |
| 1 time per month (up to 28 weeks) | Blood for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 16-18 weeks | Blood test for estriol, alpha-fetoprotein, beta-hCG | Only at late turnout unless biochemical screening for serum marker levels at 11-14 weeks |
| 18-21 weeks | The second screening ultrasound of the fetus is performed in the antenatal clinic | |
| In the third trimester (27-40 weeks) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol). 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 7. | A visit to an obstetrician-gynecologist every 2 weeks, after 36 weeks - weekly (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, VDM, uterine tone, fetal palpation, auscultation of the fetus with a stethoscope. Potassium iodide 200-250 mcg/day |
| 24-28 weeks | Oral glucose tolerance test (OGTT) | |
| 28-30weeks | In Rh-negative women with Rh-positive blood of the child's father and the absence of Rh antibodies in the mother's blood | Administration of human immunoglobulin antirhesus RHO[D] |
| 30 weeks | A certificate of incapacity for work is issued for maternity leave | |
| 30-34 weeks | The third screening ultrasound of the fetus with dopplerometry in the antenatal clinic. - general practitioner; - a dentist. | |
| After 32 weeks | At each visit to the doctor of the antenatal clinic, in addition to determining the circumference of the abdomen, the height of the uterine fundus (hereinafter referred to as VDM), uterine tone, determine the position of the fetus, the presenting part, the doctor auscultates the fetus with a stethoscope. | |
| After 33 weeks | Cardiotocography (hereinafter referred to as CTG) of the fetus is performed | |
| Throughout pregnancy | In antenatal clinics there are schools for pregnant women, which are attended by expectant mothers along with fathers. In the process of learning, there is an acquaintance with the changes in the body of a woman during physiological pregnancy, acquaintance with the process of childbirth, the correct behavior in childbirth, the basics of breastfeeding. | |
| Over 37 weeks | Hospitalization with the onset of labor. According to indications - planned antenatal hospitalization. | |
| 41 weeks | Planned hospitalization for delivery | |
| No later than 72 hours after delivery | All women with an Rh-negative blood group who gave birth to a child with a positive Rh-belonging, or a child whose Rh-belonging is not possible to determine, regardless of their compatibility according to the AB0 system | Re-introduction of human immunoglobulin anti-rhesus RHO[D] |
| postpartum period | 1. Early breastfeeding 2. Recommendations for breastfeeding. 3. Consultation of medical specialists on concomitant extragenital disease (if indicated). 4. Toilet of the external genital organs. 5. Dry processing of seams (if any). 6. Removal of external non-absorbable sutures (if any) on the 5th day. 7. Early discharge. | |
| Daily postpartum | 1. Examination by an obstetrician-gynecologist; 2. Inspection and palpation of the mammary glands. | |
| 3 days after birth | Ultrasound of the pelvic organs | |
| After delivery by caesarean section | 1. Complete blood count, general urinalysis. 2. Biochemistry of blood (according to indications). | Ultrasound of the pelvic organs |
Normal blood count during pregnancy. Hemoglobin, platelets, hematocrit, erythrocytes and leukocytes during pregnancy. Clinical blood test during pregnancy. Hematological changes during pregnancy.
A normal pregnancy is characterized by significant changes in almost all organs and systems to adapt to the requirements of the fetoplacental complex, including changes in blood tests during pregnancy.
Pregnancy blood test norms: article summary
- Significant hematological changes during pregnancy are physiological anemia, neutrophilia, moderate thrombocytopenia, increased blood clotting factors and decreased fibrinolysis.
- By 6-12 weeks of gestation, plasma volume increases by approximately 10-15%. The fastest rate of increase in plasma volume occurs between 30 and 34 weeks of gestation, after which plasma volume changes little.
- Red blood cell count begins to increase at 8-10 weeks of gestation and by the end of pregnancy increases by 20-30% (250-450 ml) of the normal level for non-pregnant women by the end of pregnancy A significant increase in plasma volume relative to the increase in hemoglobin and red blood cell volume leads to moderate decrease in hemoglobin levels (physiological anemia of pregnancy), which is observed in healthy pregnant women.
- Pregnant women may have a slightly lower platelet count than healthy non-pregnant women.
- The neutrophil count begins to rise in the second month of pregnancy and stabilizes in the second or third trimester, at which time the white blood cell count. The absolute number of lymphocytes does not change.
- The level of some blood clotting factors changes during pregnancy.
This article describes the hematological changes that occur during pregnancy, the most important of which are:
- Increased plasma volume and decreased hematocrit
- Physiological anemia, low hemoglobin
- Elevated white blood cells during pregnancy
- Neutrophilia
- Moderate thrombocytopenia
- Increased procoagulant factors
- Fibrinolysis reduction
Tests mentioned in the article
How to take blood tests and get a 5% discount? Go to the CIR laboratories online store!
Blood plasma volume
By 6-12 weeks of pregnancy, the volume of blood plasma increases by approximately 10-15%.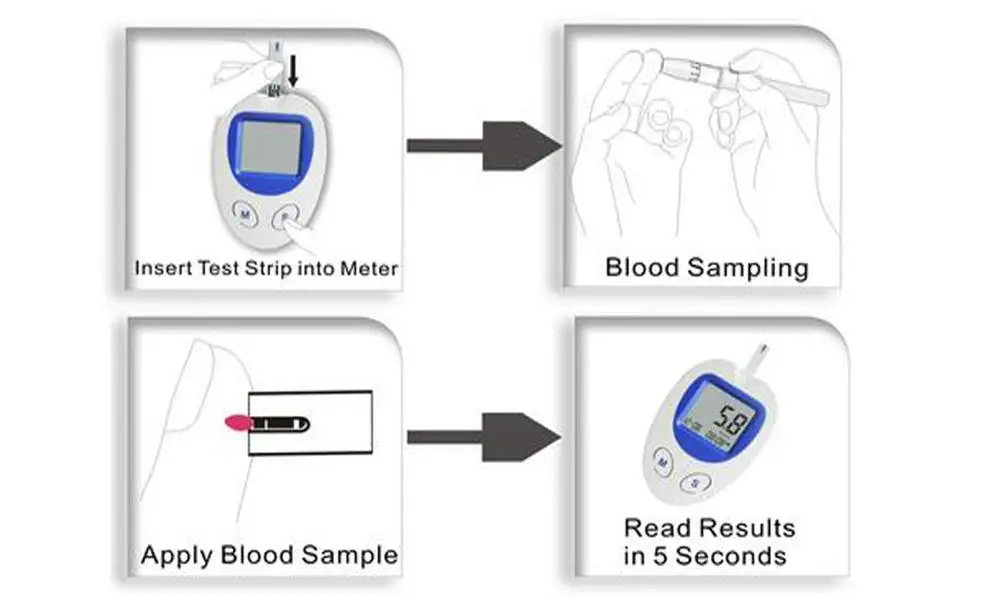 The fastest rate of increase in plasma volume occurs between 30 and 34 weeks of gestation, after which plasma volume changes little. On average, plasma volume increases by 1100-1600 ml per trimester, and as a result, plasma volume during pregnancy increases to 4700-5200 ml, which is 30 to 50% higher than plasma volume in non-pregnant women.
The fastest rate of increase in plasma volume occurs between 30 and 34 weeks of gestation, after which plasma volume changes little. On average, plasma volume increases by 1100-1600 ml per trimester, and as a result, plasma volume during pregnancy increases to 4700-5200 ml, which is 30 to 50% higher than plasma volume in non-pregnant women.
During pregnancy, plasma renin activity tends to increase, while the level of atrial natriuretic peptide decreases slightly. This suggests that the increase in plasma volume is caused by insufficiency of the vascular system, which leads to systemic vasodilation (dilation of blood vessels throughout the body) and an increase in vascular capacity. Since it is the volume of blood plasma that initially increases, its effect on the renal and atrial receptors leads to opposite effects on the hormonal background (a decrease in plasma renin activity and an increase in natriuretic peptide). This hypothesis is also supported by the observation that an increase in sodium intake does not lead to a further increase in plasma volume.
Plasma volume immediately decreases after delivery, but rises again 2-5 days later, possibly due to increased aldosterone secretion occurring at this time. Plasma volume then gradually decreases again: 3 weeks postpartum, it is still elevated by 10-15% of the normal level for non-pregnant women, but usually returns to normal by 6 weeks postpartum.
RBCs in pregnancy, ESR in pregnancy
RBCs begin to increase at 8-10 weeks of gestation and increase by 20-30% (250-450 ml) of normal non-pregnant levels by the end of pregnancy, especially in women taking drugs iron during pregnancy. Among pregnant women who did not take iron supplements, the number of red blood cells may increase by only 15-20%. The lifespan of red blood cells decreases slightly during a normal pregnancy.
The level of erythropoietin during normal pregnancy increases by 50% and its change depends on the presence of pregnancy complications. An increase in plasma erythropoietin leads to an increase in the number of red blood cells, which partially provide for the high metabolic oxygen requirements during pregnancy.
In women who do not take iron supplements, the average volume of red blood cells decreases during pregnancy and in the third trimester averages 80-84 fl. However, in healthy pregnant women and in pregnant women with moderate iron deficiency, the average volume of erythrocytes increases by about 4 fl.
ESR increases during pregnancy, which has no diagnostic value.
Anemia in pregnancy, hemoglobin in pregnancy, hematocrit in pregnancy, low hemoglobin in pregnancy
Decreased hemoglobin in pregnancy
pregnant), which is observed in healthy pregnant women. The biggest difference between the growth rate of blood plasma volume and the number of red blood cells in the maternal circulation is formed during the end of the second, beginning of the third trimester (a decrease in hemoglobin usually occurs at 28-36 weeks of pregnancy). The hemoglobin concentration rises due to the cessation of the increase in plasma volume and the continuation of the increase in the amount of hemoglobin. Conversely, the absence of physiological anemia is a risk factor for stillbirth.
Conversely, the absence of physiological anemia is a risk factor for stillbirth. Anemia in pregnancy
Defining anemia in pregnant women is difficult because it consists of pregnancy-related changes in plasma volume and red blood cell count, physiological differences in hemoglobin concentration between women and men, and the frequency of iron supplementation during pregnancy.
- The Centers for Disease Prevention and Control defined anemia as hemoglobin levels less than 110 g/l (hematocrit less than 33%) in the first and third trimesters and less than 105 g/l (hematocrit less than 32%) in the second trimester.
- WHO defined anemia in pregnancy as a decrease in hemoglobin less than 110 g/l (11 g/dl) or hematocrit less than 6.83 mmol/l or 33%. Severe anemia in pregnancy is determined by a hemoglobin level of less than 70 g/l and needs medical treatment. Very severe anemia is defined as a hemoglobin level of less than 40 g/L and is a medical emergency due to the risk of congestive heart failure.
Women with hemoglobin values below these levels are considered anemic and should undergo routine tests (CBC with peripheral blood smear evaluation, reticulocyte count, serum iron, ferritin, transferrin). If no abnormalities were detected during the examination, then hemoglobin reduced to a level of 100 g / l can be considered physiological anemia with a wide variety of factors affecting the normal level of hemoglobin in a particular person.
Chronic severe anemia is most common among women in developing countries. A decrease in maternal hemoglobin below 60 g / l leads to a decrease in the volume of amniotic fluid, vasodilation of the cerebral vessels of the fetus and a change in the heart rate of the fetus. It also increases the risk of preterm birth, miscarriage, low birth weight and stillbirth. In addition, severe anemia (hemoglobin less than 70 g/l) increases the risk of maternal death. There is no evidence that anemia increases the risk of congenital malformations of the fetus.
Severe chronic anemia is usually associated with insufficient iron stores (due to insufficient dietary intake or intestinal worm infestations), folate deficiency (due to insufficient intake and chronic hemolytic conditions such as malaria). Thus, prevention of chronic anemia and improvement of pregnancy outcome is possible with the use of nutritional supplements and the use of infection control measures.
Administering blood and packed red cell transfusions (where safe blood transfusion is available) is a reasonable aggressive treatment for severe anemia, especially if there are signs of fetal hypoxia.
Signs of physiological anemia of pregnancy disappear 6 weeks after delivery, when plasma volume returns to normal.
Iron requirement
In a singleton pregnancy, the iron requirement is 1000 mg per pregnancy: approximately 300 mg for the fetus and placenta and approximately 500 mg, if any, to increase hemoglobin. 200 mg is lost through the intestines, urine and skin.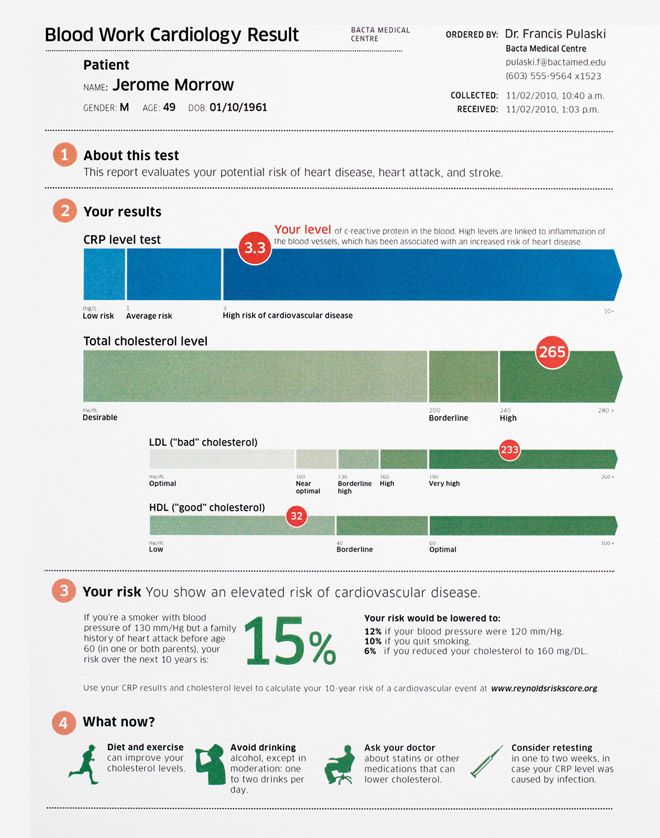 Since most women do not have an adequate supply of iron to meet their needs during pregnancy, iron is usually prescribed as part of a multivitamin, or as a separate element. In general, women taking iron supplements have a 1 g/dL higher hemoglobin concentration than women not taking iron.
Since most women do not have an adequate supply of iron to meet their needs during pregnancy, iron is usually prescribed as part of a multivitamin, or as a separate element. In general, women taking iron supplements have a 1 g/dL higher hemoglobin concentration than women not taking iron.
Folate requirement
The daily folate requirement for non-pregnant women is 50-100 micrograms. An increase in the number of red blood cells during pregnancy leads to an increase in the need for folic acid, which is provided by increasing the dose of folic acid to 400-800 mcg per day, to prevent neural tube defects in the fetus.
Pregnancy platelets
In most cases, the platelet count during an uncomplicated pregnancy remains within the normal range for non-pregnant women, but it is also possible for pregnant women to have a lower platelet count compared to healthy non-pregnant women. The platelet count begins to rise immediately after childbirth and continues to increase for 3-4 weeks until it returns to normal values.
Thrombocytopenia in pregnancy
The most important obstetric change in platelet physiology during pregnancy is thrombocytopenia, which may be associated with pregnancy complications (severe preeclampsia, HELLP syndrome), drug disorders (immune thrombocytopenia) or may be gestational thrombocytopenia.
Gestational or occasional thrombocytopenia is asymptomatic in the third trimester of pregnancy in patients without prior thrombocytopenia. It is not associated with maternal, fetal, or neonatal complications and resolves spontaneously after delivery. 99/l. The white blood cell count drops to the reference range for non-pregnant women by the sixth day after delivery.
Pregnant women may have a small number of myelocytes and metamyelocytes in the peripheral blood. According to some studies, there is an increase in the number of young forms of neutrophils during pregnancy. Lobe bodies (blue staining of cytoplasmic inclusions in granulocytes) are considered normal in pregnant women.
In healthy women during uncomplicated pregnancy, there is no change in the absolute number of lymphocytes and there are no significant changes in the relative number of T- and B-lymphocytes. The number of monocytes usually does not change, the number of basophils may decrease slightly, and the number of eosinophils may increase slightly.
Coagulation factors and inhibitors
During normal pregnancy, the following changes in clotting factor levels occur, leading to physiological hypercoagulation:
- Due to hormonal changes during pregnancy, the activity of total protein S antigen, free protein S antigen and protein S is reduced.
- Activated protein C resistance increases in the second and third trimesters. These changes have been identified in first-generation tests using pure blood plasma (i.e., not lacking factor V), but this test is rarely used clinically and is of only historical interest.
- Fibrinogen and factors II, VII, VIII, X, XII and XIII are increased by 20-200%.

- Von Willebrand factor rises.
- Increased activity of fibrinolysis inhibitors, TAF1, PAI-1 and PAI-2. The level of PAI-1 also increases markedly.
- Levels of antithrombin III, protein C, factor V and factor IX most often remain unchanged or increase slightly.
The end result of these changes is an increase in the tendency to thrombosis, an increase in the likelihood of venous thrombosis during pregnancy and, especially, in the postpartum period. Along with contraction of the myometrium and an increase in the level of decidual tissue factor, hypercoagulability protects the pregnant woman from excessive bleeding during labor and delivery of the placenta.
APTT remains normal during pregnancy, but may decrease slightly. Prothrombin time may be shortened. Bleeding time does not change.
The timing of normalization of blood clotting activity in the postpartum period may vary depending on factors, but everything should return to normal within 6-8 weeks after delivery. The hemostasiogram should not be assessed earlier than 3 months after delivery and after lactation is completed to exclude the influence of pregnancy factors.
The hemostasiogram should not be assessed earlier than 3 months after delivery and after lactation is completed to exclude the influence of pregnancy factors.
The influence of acquired or inherited thrombophilia factors on pregnancy is an area for research.
Postpartum
Hematological changes associated with pregnancy return to normal 6-8 weeks after delivery. The rate and nature of the normalization of changes associated with pregnancy, specific hematological parameters are described above in the section on each parameter.
Hematological complications of pregnancy
- Iron deficiency anemia.
- Thrombocytopenia.
- Neonatal alloimmune thrombocytopenia.
- Acquired hemophilia A.
- Venous thrombosis.
- Rh and non-Rh alloimmunization. For diagnosis, an analysis is carried out for Rh antibodies and anti-group antibodies.
- A manifestation of a previously unrecognized coagulation disorder, such as von Willebrand disease, most commonly manifests in women during pregnancy and childbirth.
 For screening for von Willebrand disease, an assay is given to assess platelet aggregation with ristocetin.
For screening for von Willebrand disease, an assay is given to assess platelet aggregation with ristocetin. - Aplastic anemia.
Other articles in this section
-
ToRCH infections and pregnancy
What are ToRCH infections, what are the dangers of these infections during pregnancy, how and when is the examination performed, how to interpret the results. Perinatal infections account for approximately 2-3% of all congenital fetal anomalies.
-
Pregnancy tests at CIR Laboratories
In our laboratory you can undergo a complete examination upon pregnancy, take tests at any time, and in our clinics you can conclude an agreement on pregnancy management.
-
Online hCG calculator during pregnancy
The hCG calculator is used to calculate the increase in hCG (the difference between two tests taken at different times).
The increase in hCG is important for assessing the development of pregnancy.
 Normally, in the early stages of pregnancy, hCG increases by about 2 times every two days. As the hormone levels increase, the rate of increase decreases.
Normally, in the early stages of pregnancy, hCG increases by about 2 times every two days. As the hormone levels increase, the rate of increase decreases. -
False positive pregnancy test or why hCG is positive but not pregnant?
When can a pregnancy test be positive?
-
The norm of hCG during pregnancy. Table of hCG values by week. Elevated HCG. Low HCG. HCG in ectopic pregnancy. hCG during IVF (hCG after replanting, hCG at 14 dpo).
hCG or beta-hCG or total hCG - human chorionic gonadotropin - a hormone produced during pregnancy. HCG is formed by the placenta, which nourishes the fetus after fertilization and implantation (attachment to the wall of the uterus).
-
Risk assessment of pregnancy complications using prenatal screening
Prenatal screening data allow assessing not only the risks of congenital pathology, but also the risk of other pregnancy complications: intrauterine fetal death, late toxicosis, intrauterine hypoxia, etc.

-
Parvovirus B19 and parvovirus infection: what you need to know when planning and getting pregnant.
What is a parvovirus infection, how is the virus transmitted, who can get sick, what is the danger of the virus during pregnancy, what tests are taken for diagnosis.
-
Pregnancy planning
Obstetrics differs from other specialties in that during the physiological course of pregnancy and childbirth, in principle, it is not part of medicine (the science of treating diseases), but is part of hygiene (the science of maintaining health). Examination during pregnancy planning.
-
1st and 2nd trimester prenatal screening ("double", "triple" and "quadruple" tests)
Prenatal screening are tests performed on pregnant women to identify risk groups for pregnancy complications.
-
Testosterone during pregnancy. Androgens: their formation and metabolism during normal pregnancy.
 General (clinical) blood test.
General (clinical) blood test. 

 General (clinical) blood test.
General (clinical) blood test.  Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.
Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.  Inspections and consultations:
Inspections and consultations: