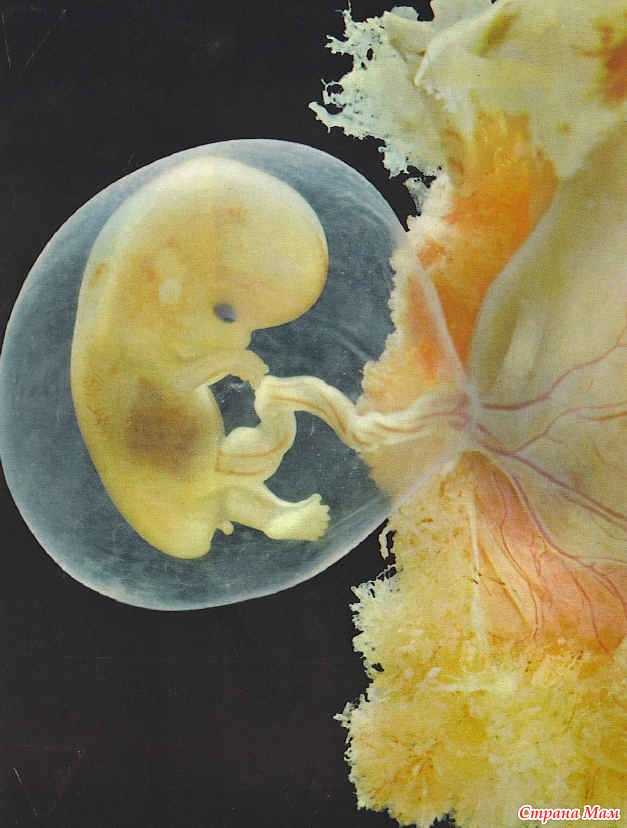
Fetus at first trimester
Stages of Fetal Development - First Trimester
Stages of Fetal Development - First TrimesterStages of Fetal Development - First Trimester
One - 13 Weeks
| FERTILIZATION Biologically speaking, fertilization (or conception) is the beginning of human development. Fertilization normally occurs within several hours of ovulation (some authors report up to 24 hours) when a man's sperm combines with a woman's egg | |
| WEEK 2
| |
| WEEK 4
| |
| WEEK 6
| |
| WEEK 8
| |
| WEEK 10
| |
| WEEK 12
| |
First trimester | Pregnancy Birth and Baby
First trimester | Pregnancy Birth and Baby beginning of content5-minute read
Listen
From the moment you get the news that you are pregnant, you will probably be filled with a rush of emotions – and most likely a flood of questions too. While the first trimester of pregnancy is filled with a host of changes for you and for your baby, many will be invisible to the outside world. Read on to find out what happens to your body and how to stay healthy.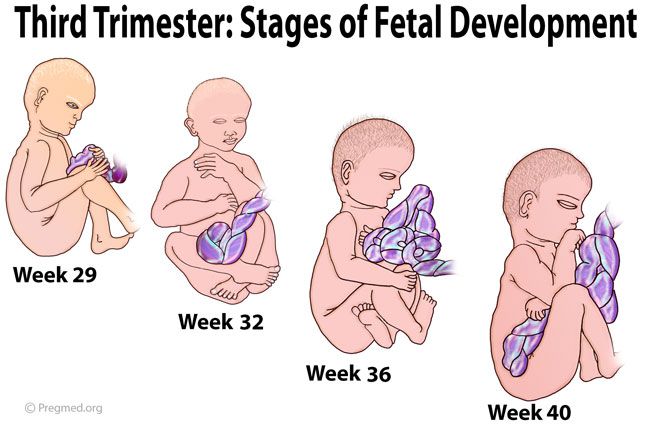
What is the first trimester?
A full-term pregnancy lasts around 9 months, and most people (including your doctors and midwives) will break this up into 3 ‘trimesters’. Although you are pregnant from the moment of conception – when a male sperm fertilises your ovum (egg) – the first trimester of pregnancy is counted from the first day of your last period through to week 12. This is because most women who conceive naturally won’t know the date of conception.
Trimesters are a helpful way to think about pregnancy because the changes that happen to you and your baby fall into the 3 broad categories of early, middle and late pregnancy, called first, second and third trimesters.
What happens to your body?
For some women, the first trimester is characterised by nausea (often called ‘morning sickness’, although it can occur at any time of day). But remember that every pregnancy is different and while some women have food cravings, others experience food aversions, and some have no change in appetite at all.
Other changes in the first trimester include changes to your breasts as they become tender, larger and heavier, while your uterus will grow and put pressure on your bladder so that you need to urinate more often.
Your emotions
You might feel a range of emotions during your first trimester. Hormone changes may make you feel moody or irritable, and tiredness is common in the early months. These feelings are normal, so discuss how you feel with you partner or with a close friend. If you feel down or anxious, speak with your doctor or midwife.
What happens to the baby?
Through the first trimester, your baby goes from being a fertilised ovum to a fetus of about 6cm in length at 12 weeks. By the end of the first trimester, your baby’s heart is starting to beat, and the brain, stomach and intestines are developing. There are little bumps known as 'buds' where arms and legs are starting to grow.
What can be expected from the doctor and midwife?
Your antenatal (pregnancy) health checks might be with your GP, a midwife or an obstetrician, depending on where you will give birth. During your first antenatal health check, you will probably have your pregnancy confirmed with a urine or blood test. These are more reliable than home pregnancy tests. First trimester antenatal health checks usually happen every 4 to 6 weeks, but this can vary, based on your health and how your baby develops.
During your first antenatal health check, you will probably have your pregnancy confirmed with a urine or blood test. These are more reliable than home pregnancy tests. First trimester antenatal health checks usually happen every 4 to 6 weeks, but this can vary, based on your health and how your baby develops.
Many women are offered an ultrasound scan at around 12 weeks – you might hear the baby’s heartbeat at this scan. This ultrasound will also show if you are having a multiple birth (e.g. twins) and can help estimate the baby’s size and due date, as well as check for some health conditions.
Other health checks during the first trimester include:
- urine tests to detect urinary infections, a common but manageable condition that if left untreated can trigger pre-term labour
- blood tests to check your blood type (particularly Rh status), iron levels, blood sugars (for gestational diabetes), rubella (German measles) immunity, and other infections such as HIV, hepatitis B and syphilis
- general maternal health and wellbeing checks, including a discussion of concerns you might have about your pregnancy or general health, and a medication review (including natural or alternative medicines) to check for safety during pregnancy
How to stay healthy
Staying healthy is doubly important during pregnancy.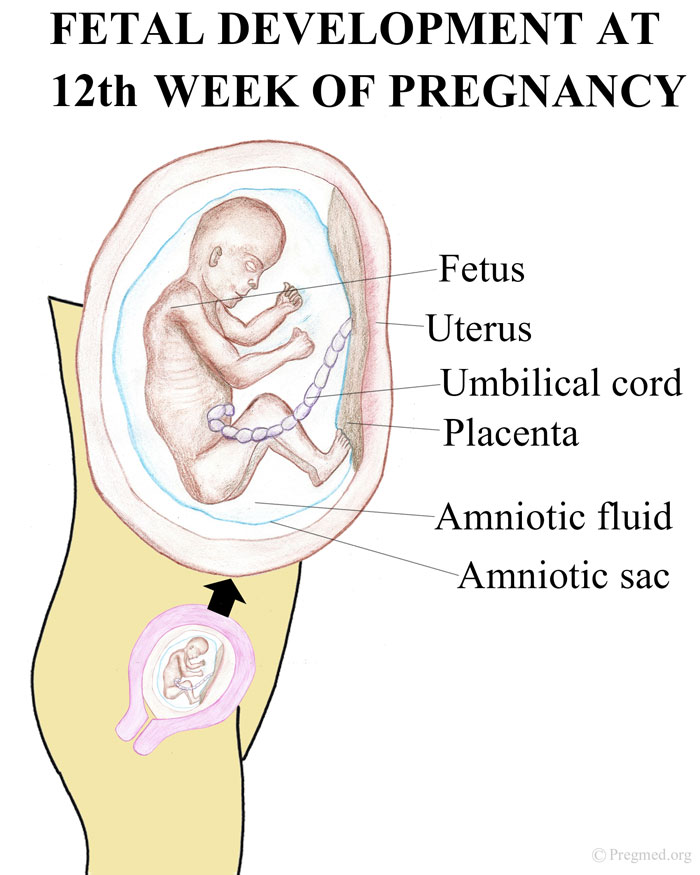 If you are a smoker, this is a great time to quit – speak with your doctor or pharmacist for support.
If you are a smoker, this is a great time to quit – speak with your doctor or pharmacist for support.
It is safest not to drink any alcohol while you are pregnant, since even low-level drinking, particularly in the first trimester of pregnancy, can have long-term negative effects on your baby.
Try to eat a variety of nutritious foods during pregnancy since this will help meet your baby’s nutritional requirements, as well as your own. While the amount of food you need to eat during your first trimester won’t increase by much, you will need more of some nutrients. Most women will also need folic acid and iodine supplements because it's difficult to get enough of these from food alone.
It’s important to keep up regular physical activity during your pregnancy because of the many benefits both for you and your baby. If you experience any discomfort or complications, speak to your doctor or midwife.
Things to consider in the first trimester
- Book your antenatal appointments for the whole trimester – they are important for tracking your health and your baby’s growth.

- Get support – ask your partner, a friend or a family member to go with you to health checks.
- Are your vaccinations up to date? Immunisation is important, and several vaccines are funded for pregnant women under the National Immunisation Program. Speak to your doctor for guidance.
- Your doctor or midwife can help you access a range of support services, not just for medical concerns - for example, if you feel you are at risk of violence or you are feeling vulnerable during your pregnancy.
Your pregnancy journey
Follow your pregnancy week-by-week to find out how your baby is growing and what is happening to your body.
Sources:
NSW Health (Having a baby), Royal Women's Hospital (Pregnancy and birth), Raising Children Network (Pregnancy week-by-week), Women's and Children's Health Network (The first 3 months of pregnancy: the first trimester), Better Health Channel (Pregnancy - prenatal tests)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Related pages
- Pregnancy week-by-week
- Third trimester
- Second trimester
Need more information?
Pregnancy at week 7
Your baby is now about 1cm long and if you haven’t seen your doctor yet, now is a good time to start your antenatal care.
Read more on Pregnancy, Birth & Baby website
Antenatal care during your pregnancy
You receive antenatal care from your GP, midwife or obstetrician. You’ll be offered tests and scans and your health and your baby’s will be checked.
Read more on Pregnancy, Birth & Baby website
Men’s feelings in early pregnancy | Raising Children Network
In early pregnancy, it’s normal for men to feel uninterested or just ‘not into it’. Read more about men’s feelings during pregnancy in our Dads Guide.
Read more about men’s feelings during pregnancy in our Dads Guide.
Read more on raisingchildren.net.au website
Week by week pregnancy- antenatal care at 7 weeks pregnant
Your doctor can look at your foetus’s features to determine how old they are – find out how. You need to talk to your doctor if you experience very severe morning sickness as you may not be getting all the nutrients you and your baby need or early pregnancy spotting (spot bleeding) as you may be at risk of miscarriage.
Read more on Parenthub website
Routine antenatal tests
During pregnancy, you'll be offered a range of tests, including blood tests and ultrasound scans. Each test can tell you something about you and your baby’s health.
Read more on Pregnancy, Birth & Baby website
Pregnancy care for migrant and refugee women | Australian Government Department of Health and Aged Care
While many migrant and refugee women experience healthy pregnancies, issues associated with resettlement can contribute to poorer perinatal outcomes than those experienced by women in general.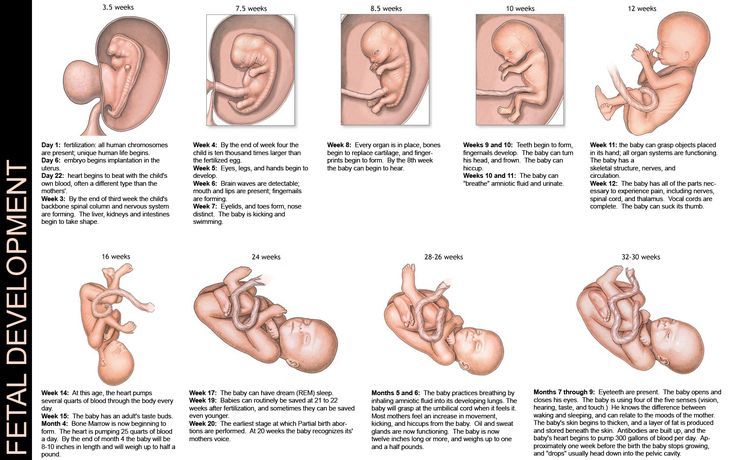
Read more on Department of Health and Aged Care website
Second trimester
During the second trimester, your baby’s organs will develop and they will start to hear sounds. Any morning sickness will likely ease off around this time.
Read more on Pregnancy, Birth & Baby website
Third trimester
The third trimester is the last 3 months of your pregnancy – an exciting time, but with some discomforts too. Learn more about what to expect before the birth.
Read more on Pregnancy, Birth & Baby website
The challenges and benefits of antenatal tests for aboriginal mothers | Know Pathology Know Healthcare
For many pregnant Aboriginal and Torres Strait Islander women poor health and social disadvantage contribute to poorer perinatal outcomes than those of non-Indigenous women.
Read more on Know Pathology Know Healthcare website
A guide to blood tests in pregnancy | Know Pathology Know Healthcare
The following guide outlines the different pathology tests available throughout each trimester, and the purpose of your prenatal blood tests.
Read more on Know Pathology Know Healthcare website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
1st trimester of pregnancy: what happens to the fetus
1st trimester of pregnancy: what happens to the fetus - Private maternity hospital Ekaterininskaya Clinics1st trimester: 1st-12th weeks
The gestational age is calculated from the first day of the last menstruation, since it is difficult to determine the exact day of conception. Since conception usually occurs in the middle of the menstrual cycle, you are not actually pregnant during the first two weeks, but this period is counted as the beginning of pregnancy.
Since conception usually occurs in the middle of the menstrual cycle, you are not actually pregnant during the first two weeks, but this period is counted as the beginning of pregnancy.
As soon as the fertilization of the egg takes place around the 3rd week, the hormones begin to produce changes in your body little by little. As a result, you may experience some of the following symptoms:
- Morning sickness. As a result of rising levels of hormones characteristic of pregnancy, up to 80% of women in the 1st trimester experience morning sickness with symptoms such as nausea and vomiting. The idea that such malaise is observed only in the morning is a common misconception. In fact, symptoms can appear at any time of the day or night. Up to 1 in 5 women experience morning sickness in the 2nd trimester of pregnancy and can sometimes persist throughout pregnancy.
If you experience morning sickness, avoid foods that make you sick, eat little and often, avoid fatty and spicy foods, drink more water.
 If you experience severe symptoms or symptoms that bother you, see your doctor.
If you experience severe symptoms or symptoms that bother you, see your doctor. - Breast changes. The mammary glands will begin to increase in size, soreness may appear. The nipples will increase in size, become darker and more protruding.
- Fatigue. High levels of the hormone progesterone can make you feel tired and sleepy. Rest as often as possible in a horizontal position with your legs up and eat as well as possible, which is not easy if you are experiencing morning sickness!
- Increased emotionality. A higher level of emotionality, manifested as a result of an increase in hormone levels, is normal. Understanding and patience on the part of your partner and loved ones is very important here.
- Food likes and dislikes. You may find yourself intolerant of one food and addicted to another. This is usually not a problem, unless you feel like eating weird foods like chalk.
 If you are concerned about the situation, contact your doctor.
If you are concerned about the situation, contact your doctor. - Frequent urination. As your fluid levels increase and your uterus puts pressure on your bladder, you will become more likely to visit the toilet. Go to the toilet as soon as you feel the need - this minimizes the pressure on the bladder.
- Feeling of dizziness. Sometimes you may feel a little dizzy (this is due to hormonal changes). Try not to stay on your feet for a long time and slowly rise from a sitting or lying position. If you experience severe dizziness, contact your doctor immediately.
- Heartburn and constipation. Your digestive system will slow down to give you more time to digest your food. This can lead to heartburn and constipation. To help manage heartburn, try to eat small meals at regular intervals and avoid fried or spicy foods and carbonated drinks. Constipation is helped by eating a diet rich in fiber, maintaining physical activity and drinking plenty of water.

1st trimester milestones
- Approximately 7 days after fertilization, the embryo implants in the uterine wall. The placenta, umbilical cord and amniotic sac will begin to form to provide nourishment and protection to the embryo.
- By the end of the first 12 weeks of pregnancy, the uterus is palpable through the wall of the abdomen, the abdomen will begin to grow.
Child development in the 1st trimester of pregnancy
By the end of the 1st trimester:
- All the main organs of the baby are formed, the circulatory system works.
- The development of the sexual organs has begun.
- Fingers are formed on the hands and feet, nails have appeared.
- Facial features have formed.
- The length of the baby's body is about 6 cm from the head to the lower part of the body, he is already recognizable. The baby moves in the amniotic sac, but you don't feel it move yet.
Clinic mobile app
You can make an appointment with a doctor, get tests
and much more...
Fill out the form to make an appointment or order a call back
I agree with personal data processing policy and user agreement I also give my consent to the processing of personal data.
Sign up for a consultation
I agree with personal data processing policy and user agreement I also give my consent to the processing of personal data.
By continuing to use rd.clinic23.ru, you agree to the use of cookies. How to ban the use of certain cookies can be found in Politics
Pregnancy management, 1st trimester - basic studies.
It is necessary to register for pregnancy, as this allows timely diagnosis of:
- Pathologies of fetal development;
- Chronic medical conditions in the mother that may affect the course and outcome of pregnancy;
- Acute pathologies in the mother during pregnancy, affecting the growth and development of the fetus and the health of the mother.

Pregnancy is a complex restructuring of the body, diseases in the mother are not always known if the examination before conception is not passed.
What happens to the body during the 1st trimester of pregnancy
1st trimester is counted from conception to 12 weeks of pregnancy.
The fertilization of the egg occurs directly in the abdominal cavity. After fertilization, the egg is in the abdominal cavity and is actively split into smaller cells and becomes like a raspberry or mulberry, such an embryo is called a morula. Then it is captured by the villi of the fallopian tubes and moves into the uterine cavity. On the 7th day, the embryo is attached to the wall of the uterus. The fetal egg begins to form, consisting of amniotic fluid and the yolk sac, from which the embryo will form. At 7-8 weeks, the fetal bladder and placenta form from the fetal egg. From 8 to 12 weeks, the placenta is finally formed (in the future it only develops), it becomes visible on ultrasound.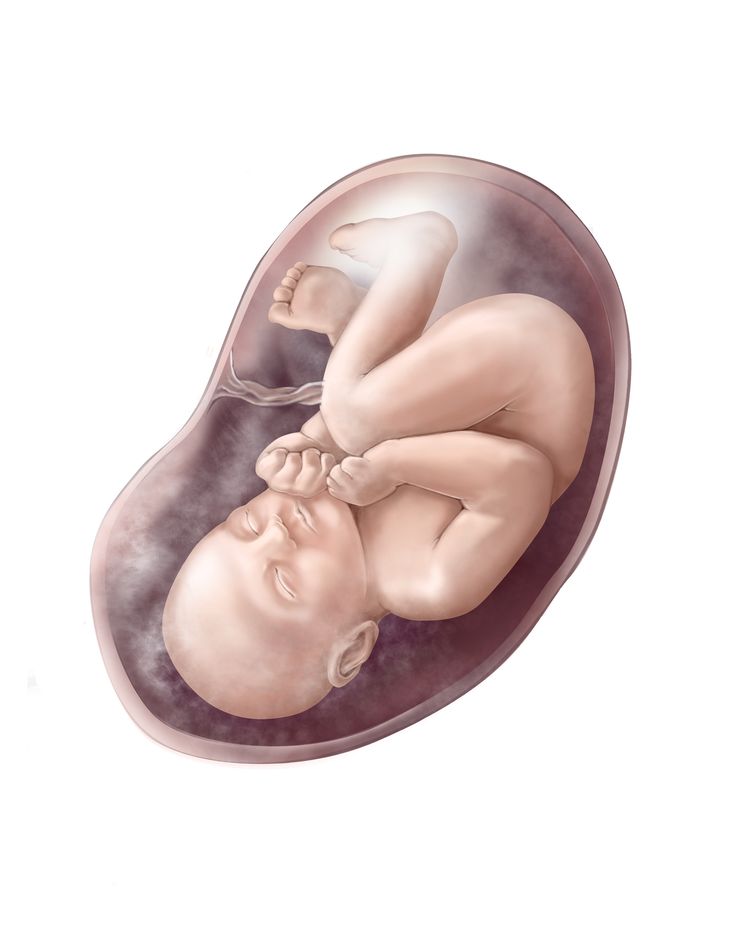 At 12 weeks, the fetus looks like a full-fledged baby about 9 in size.cm, he has formed limbs, head and main internal organs.
At 12 weeks, the fetus looks like a full-fledged baby about 9 in size.cm, he has formed limbs, head and main internal organs.
Mother's changes. Ideally, a woman does not feel pregnancy in any way. The only sign is an increase in the mammary glands, due to the development of glandular tissue under the action of hormones. The stomach practically does not increase.
During pregnancy, many women experience so-called "toxicosis" - nausea and/or vomiting. This is due to an increase in the level of estrogen (in particular progesterone) and hCG (chronic gonadotropin). Moreover, these symptoms can complicate the life of a pregnant woman, not only in the morning, but at any time of the day. Sometimes nausea or vomiting may persist throughout pregnancy.
There is such a formidable complication as excessive (uncontrolled) vomiting of pregnant women, which leads to maternal dehydration, electrolyte imbalance, liver and kidney dysfunction and encephalopathy, requiring hospitalization and treatment in a hospital.
It is best to eat according to your appetite. Food should not cause negative reactions, eat in small portions, pay attention to what kind of food provokes nausea and try not to eat it for a while, listen to your body, usually a woman herself feels what she would like to eat. Do not forget that food should not only be desirable and tasty, but also healthy. It would be ideal to eat according to the Harvard Healthy Eating Plate method, when ½ of the volume of the plate is occupied by vegetables, ¼ proteins (including plant origin), ¼ complex carbohydrates (grains, potatoes, cereals, etc.).
Your body will also begin to change. And the first thing you will feel will be engorgement and an increase in the sensitivity of the mammary glands, the nipples will swell a little and increase in size. It is important to wear comfortable, comfortable underwear and clothing to minimize discomfort. Sometimes there is pain in the nipples, your gynecologist may recommend ointments for this case.
We all remember that a pregnant woman becomes more vulnerable, whiny and sometimes even capricious. It is also associated with rising estrogen levels and requires patience and understanding on the part of family and partner. A calm atmosphere at home and, if possible, at work is important. You can connect such relaxation methods as walking, listening to your favorite music, aromatherapy in the absence of reactions to smells. Think about what could bring back your balance and calmness?
The main pregnancy hormone, progesterone, causes fluid retention in the body. In parallel with this, the growing uterus squeezes the bladder and there are frequent urges to urinate. This is normal, it is important to plan your day so that you always have the opportunity to visit the toilet.
Progesterone also reduces the tone of blood vessels, which can lead to dizziness. You can minimize these discomforts by changing the position of the body smoothly, do not get up and do not sit down abruptly. Another reason for frequent dizziness can be a decrease in the level of magnesium in the blood, your doctor will help you figure it out.
Another reason for frequent dizziness can be a decrease in the level of magnesium in the blood, your doctor will help you figure it out.
Pregnant women often have an increased need for sleep, which is explained by the same action of hormones, as well as the need for additional rest for the body, because there is a lot of work to bear, give birth and then feed the baby.
Under the action of progesterone, the smooth muscles of the whole organism (uterus, intestines, blood vessels, bile ducts and pancreatic ducts, etc.) relax, the work of internal organs slows down, which in turn leads to constipation and heartburn. In addition to medication correction (prescribed by a doctor), fractional meals in small portions, foods rich in fiber (our favorite vegetables), sufficient fluid intake, feasible physical activity (exercise therapy, walking, swimming, yoga, Pilates, etc.) help
Unfortunately, sometimes pregnancy is overshadowed by pathology, let's talk about the most common problems of the first trimester of pregnancy.
The most common problems of the 1st trimester of pregnancy
Bleeding : due to lack of progesterone, there is a spasm and relaxation of the muscles of the uterus and, accordingly, detachment of the ovum and bleeding (in severe cases - miscarriage). Also, with hypothyroidism, there is a violation of the implantation of the fetal egg, which also leads to bleeding.
Thrombosis . During pregnancy, blood clotting increases (this is normal - the body is preparing for blood loss). To prevent thrombosis of the veins of the lower extremities, it is necessary to stop taking oral contraceptives 6 months before the start of pregnancy planning, and during the onset of pregnancy, maintain sufficient physical activity (long walks, swimming) and be observed by a doctor. If you experience pain, swelling, "cyanosis" in the lower extremities, you should immediately consult a doctor.
Developmental anomalies and genetic pathologies .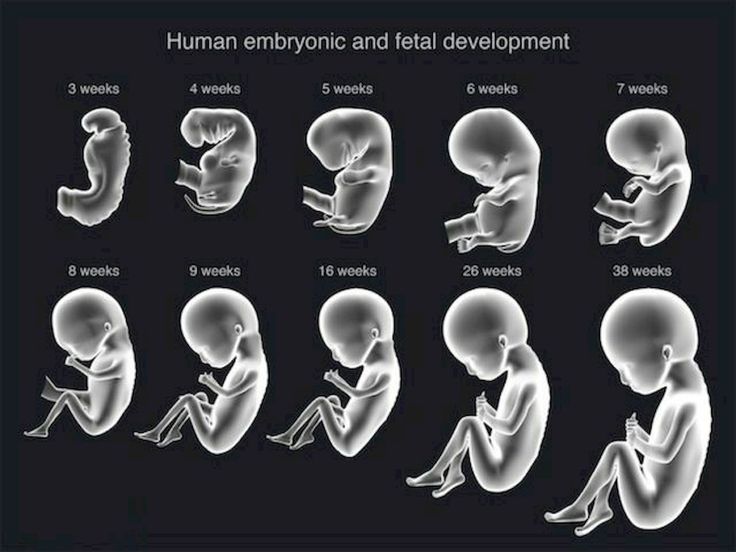 In the 1st trimester, abnormalities in the development of the fetus most often develop and manifest, which can occur as a result of ionizing radiation, infectious diseases suffered during pregnancy (rubella, influenza, etc.), taking drugs prohibited during pregnancy (fluoroquinolones, macrolides, tetracyclines, tranquilizers , etc.), genetic pathologies and hereditary diseases.
In the 1st trimester, abnormalities in the development of the fetus most often develop and manifest, which can occur as a result of ionizing radiation, infectious diseases suffered during pregnancy (rubella, influenza, etc.), taking drugs prohibited during pregnancy (fluoroquinolones, macrolides, tetracyclines, tranquilizers , etc.), genetic pathologies and hereditary diseases.
Anemia . More often it happens due to iron deficiency, tk. the fetus consumes a huge amount of it, taking away iron stores from the mother, less often due to bleeding. B12 and folic deficiency anemias also occur, also associated with increased consumption and insufficient intake by the mother. Anemia is a dangerous chronic lack of oxygen, causing fetal growth retardation syndrome. In severe cases, it can lead to fetal death.
During pregnancy chronic diseases may worsen . This is due to the fact that the fertilized egg already carries a part of DNA alien to the mother.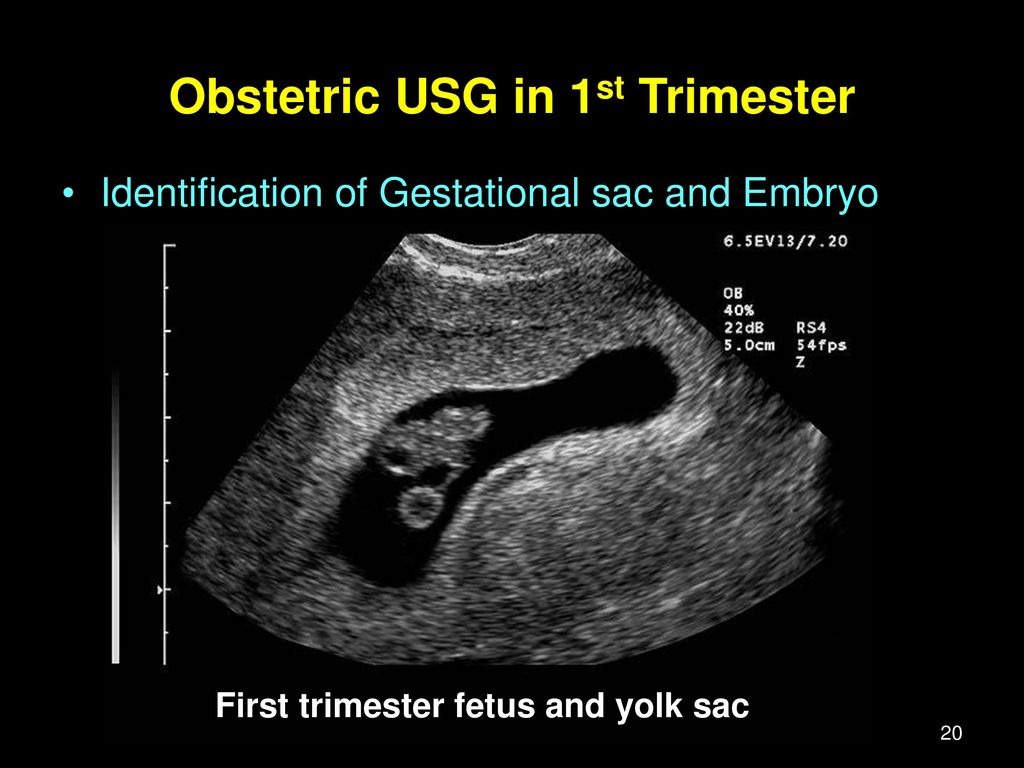 To prevent egg rejection, the mother's body suppresses its immunity throughout pregnancy, which affects the body as a whole. Therefore, all diseases not identified at the stage of preparation for pregnancy should be detected and cured. This applies mainly to infectious diseases. For example, exacerbation of chronic pyelonephritis, or herpes virus infection.
To prevent egg rejection, the mother's body suppresses its immunity throughout pregnancy, which affects the body as a whole. Therefore, all diseases not identified at the stage of preparation for pregnancy should be detected and cured. This applies mainly to infectious diseases. For example, exacerbation of chronic pyelonephritis, or herpes virus infection.
Also during pregnancy there is a sharp restructuring of the hormonal background , which, in turn, affects somatic (non-infectious) diseases. For example, due to thickening of bile and compression of the gallbladder by the uterus, chronic cholecystitis may be exacerbated. As the fetus develops, the islets of Langerhans (cells that produce insulin in the pancreas) sometimes don't develop fast enough and the baby begins to consume the mother's insulin. If the mother has diabetes or impaired glucose tolerance (including hidden ones), both the child and the mother lack insulin, which leads to tissue damage to both the child and the mother (early aging of the placenta, fetal growth retardation, premature birth, polyhydramnios, increased blood pressure in a pregnant woman, the formation of a large fetus, the risk of injury to a woman and a child during childbirth, and the most formidable complication is intrauterine fetal death).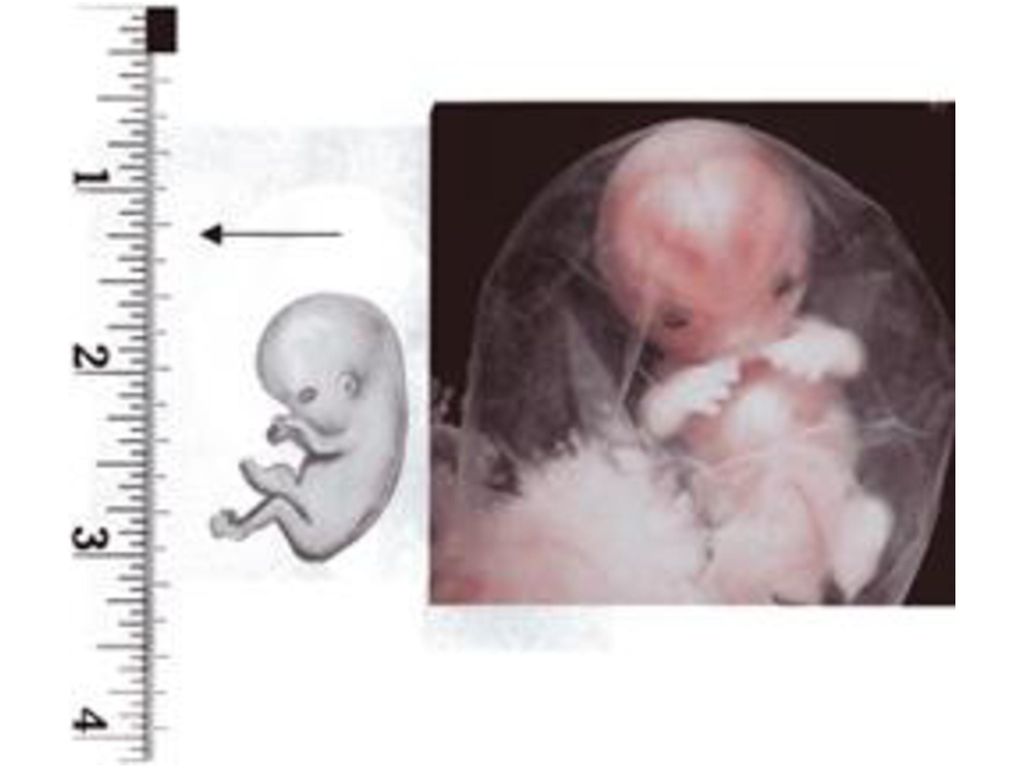
In addition, the fetal liver does not yet function as a detoxification organ, and all the decay products produced by the child must be processed by the mother's liver. 2% of pregnant women develop benign cholestatic hepatosis of pregnancy - violation of the formation and outflow of bile, which causes: effects on cells and bile ducts
1st trimester tests
Compulsory tests
Urinalysis . Needed to assess kidney function and determine the risk of eclampsia, a dangerous condition that develops during pregnancy, as well as to exclude asymptomatic bacteriuria.
Complete blood count . It aims to detect anemia, the risk of thrombosis, and inflammatory reactions.
Blood biochemistry - assessment of liver and kidney function, detection of diabetes mellitus and impaired tolerance (immunity) to glucose.
Coagulogram - detection of pathology of blood coagulation - risk of thrombosis or bleeding.
Therapist – to exclude the pathology of the internal organs, which may prevent or complicate the normal course of pregnancy and the upcoming birth. Most often, diseases such as pyelonephritis, anemia, cholecystitis, gastritis, vegetative dystonia, arterial hypertension are determined.
ECG in the direction of the therapist - detection of pathology of the cardiovascular system. Indirect signs of pericarditis, enlargement of the left ventricle, blockade of the conduction system of the heart.
Examination by an ophthalmologist - to determine the pathology of the organs of vision, incl. assessment of the risk of retinal detachment during childbirth.
ENT - the presence of chronic foci of infection (chronic tonsillitis, pharyngitis, sinusitis) increases the risk of miscarriage in the 1st trimester of pregnancy and the development of rheumatic complications.
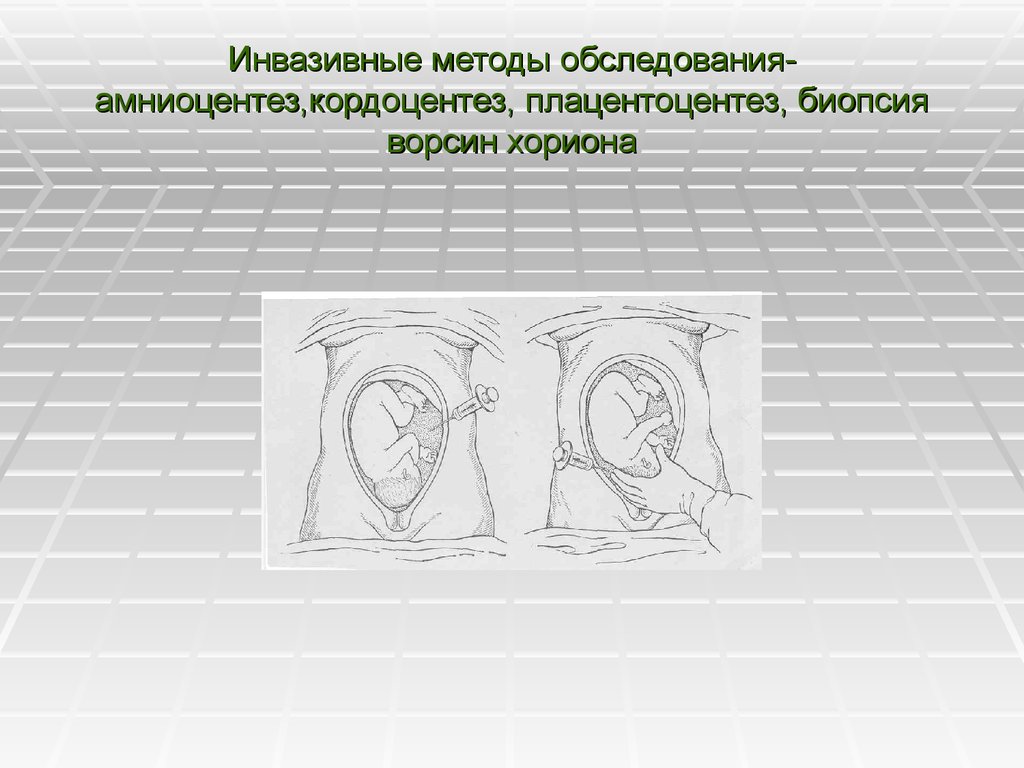
At the period of 11-14 weeks, the first ultrasound screening is carried out to detect abnormalities in the fetus.
Additional tests
When registering, all pregnant women determine the blood type and Rh factor. If the Rh factor is negative, antibodies to the Rh factor in the mother and the blood type, the Rh factor of the father of the child, are determined. Sometimes there is incompatibility in blood types, this can happen if a woman has group I, and a man has any other. Analyzes are carried out once a month, starting from the 8th week of pregnancy. All this is done in order to take the necessary measures in time to prevent hemolytic disease of the newborn.
Anemia is initially diagnosed using a complete blood count and determination of hemoglobin (Hb), mean red cell volume (MCV), and mean red cell hemoglobin (MCH). If there is a decrease or increase in these indicators, the level of ferritin, transferrin, iron, folic acid, B12 is additionally examined.
Sometimes a consultation with a gastroenterologist is necessary to correct gastrointestinal disorders .