When can you do amniocentesis
Amniocentesis - NHS
Amniocentesis is a test you may be offered during pregnancy to check if your baby has a genetic or chromosomal condition, such as Down's syndrome, Edwards' syndrome or Patau's syndrome.
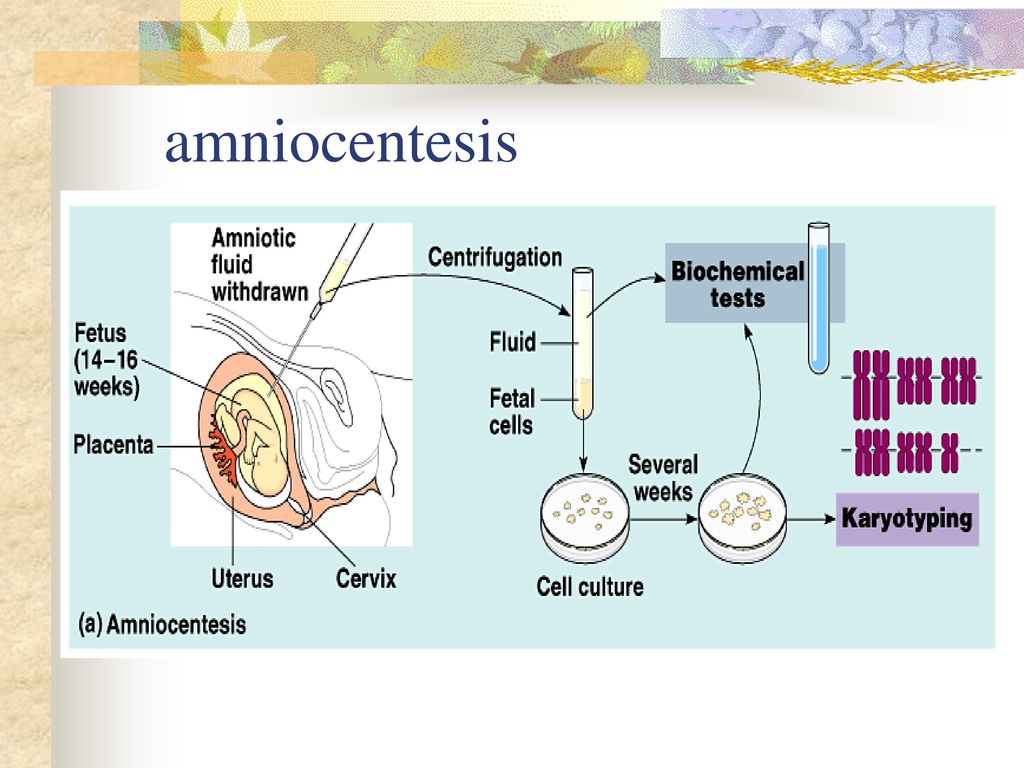
It involves removing and testing a small sample of cells from amniotic fluid, the fluid that surrounds the baby in the womb (uterus).
When amniocentesis is offered
Amniocentesis is not offered to all pregnant women. It's only offered if there's a higher chance your baby could have a genetic condition.
This could be because:
- an antenatal screening test has suggested your baby may be born with a condition, such as Down's syndrome, Edwards' syndrome or Patau's syndrome
- you have had a previous pregnancy that was affected by a genetic condition
- you have a family history of a genetic condition, such as sickle cell disease, thalassaemia, cystic fibrosis or muscular dystrophy
It's important to remember that you do not have to have amniocentesis if it's offered. It's up to you to decide whether you want it.
A midwife or doctor will speak to you about what the test involves and let you know what the possible benefits and risks are to help you make a decision.
Find out about why amniocentesis is offered and deciding whether to have it
How amniocentesis is performed
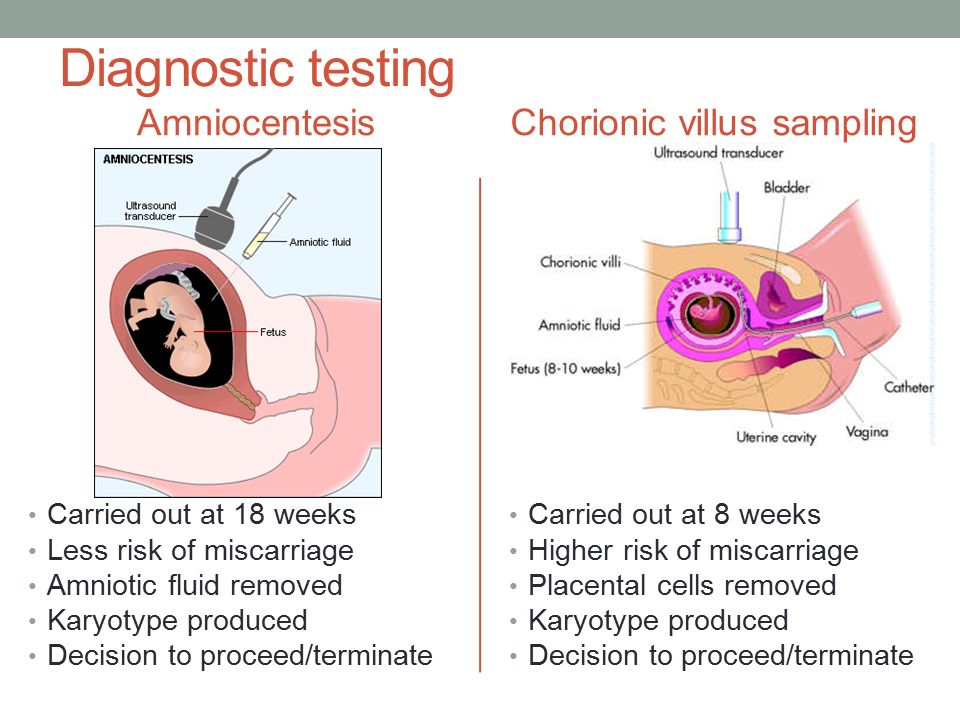
Amniocentesis is usually carried out between the 15th and 20th weeks of pregnancy, but you can have it later if necessary.
It can be performed earlier, but this may increase the risk of complications of amniocentesis and is usually avoided.
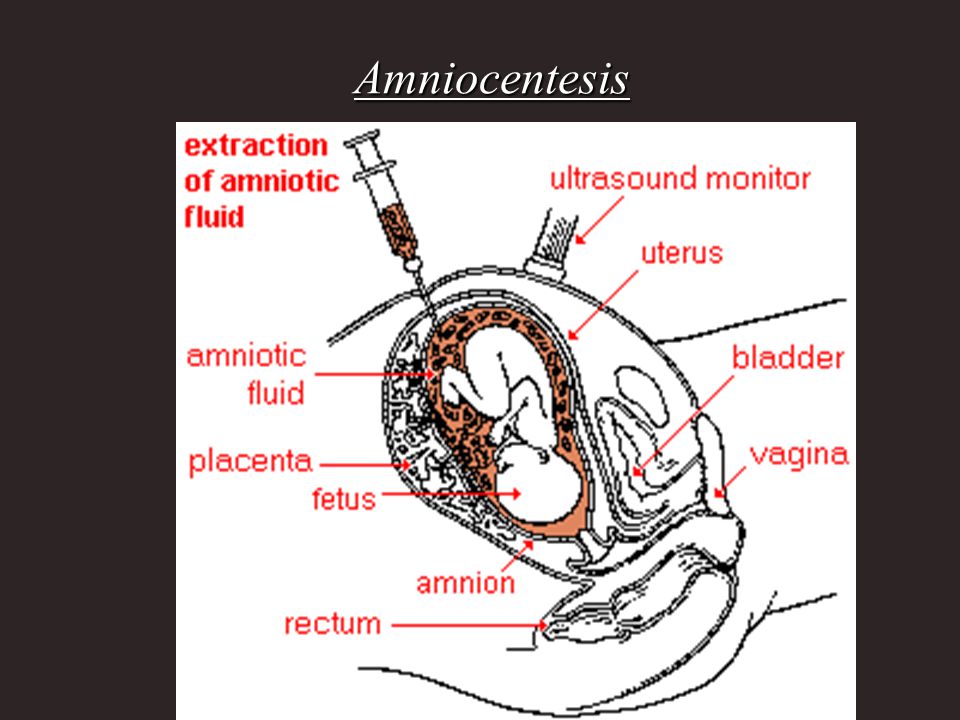
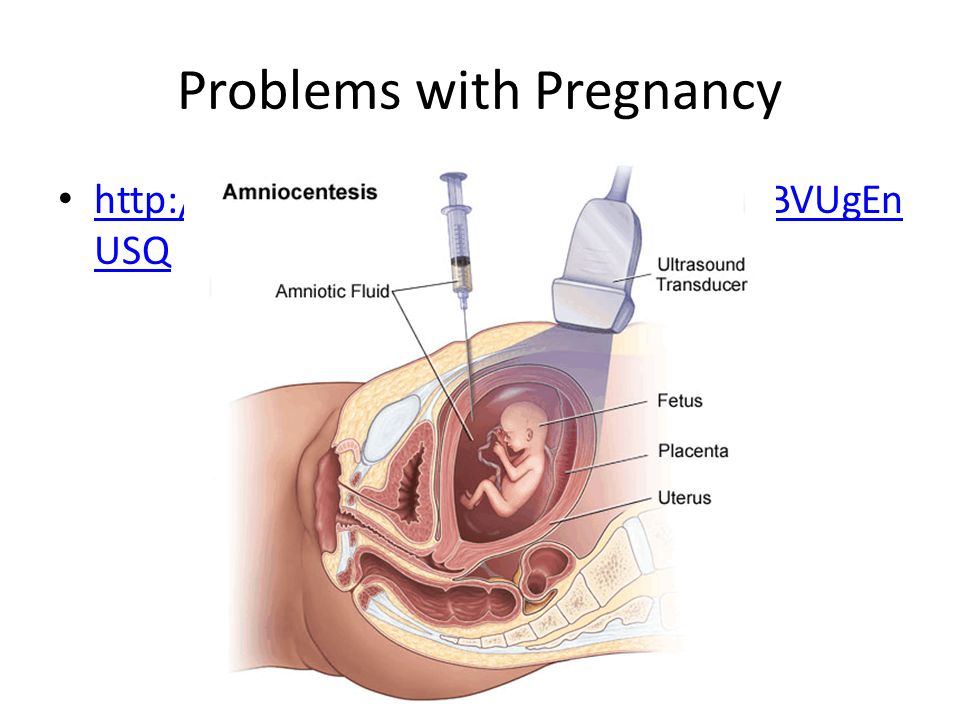
During the test, a long, thin needle is inserted through your abdominal wall, guided by an ultrasound image.
The needle is passed into the amniotic sac that surrounds your baby and a small sample of amniotic fluid is removed for analysis.
The test itself usually takes about 10 minutes, although the whole consultation may take about 30 minutes.
Amniocentesis is usually described as being uncomfortable rather than painful.
Some women describe experiencing a pain similar to period pain or feeling pressure when the needle is taken out.
Find out more about what happens during amniocentesis
Getting your results
The first results of the test should be available within 3 working days and will tell you whether Down's syndrome, Edwards' syndrome or Patau's syndrome has been discovered.
If rarer conditions are also being tested for, it can take 3 weeks or more for the results to come back.
If your test shows that your baby has a genetic or chromosomal condition, the implications will be fully discussed with you.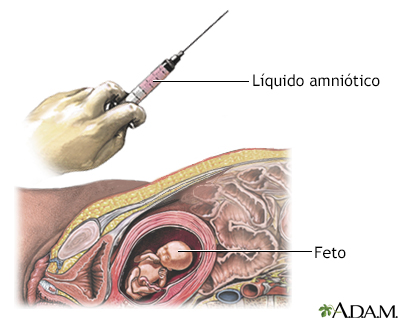
There's no cure for most of the conditions amniocentesis finds, so you'll need to consider your options carefully.
You may choose to continue with your pregnancy, while gathering information about the condition so you're fully prepared.
Find out more about having a baby that might be born with a condition
Or you may consider ending your pregnancy (having a termination).
Find out more about the results of amniocentesis
What are the risks of amniocentesis?
Before you decide to have amniocentesis, the risks and possible complications will be discussed with you.
One of the main risks associated with amniocentesis is miscarriage, which is the loss of the pregnancy in the first 23 weeks.
This is estimated to occur in up to 1 out of every 200 women who have amniocentesis.
There are also some other risks, such as infection or needing to have the procedure again because it was not possible to accurately test the first sample.
The risk of amniocentesis causing complications is higher if it's carried out before the 15th week of pregnancy, which is why the test is only done after this point.
Find out more about the possible complications of amniocentesis
What are the alternatives?
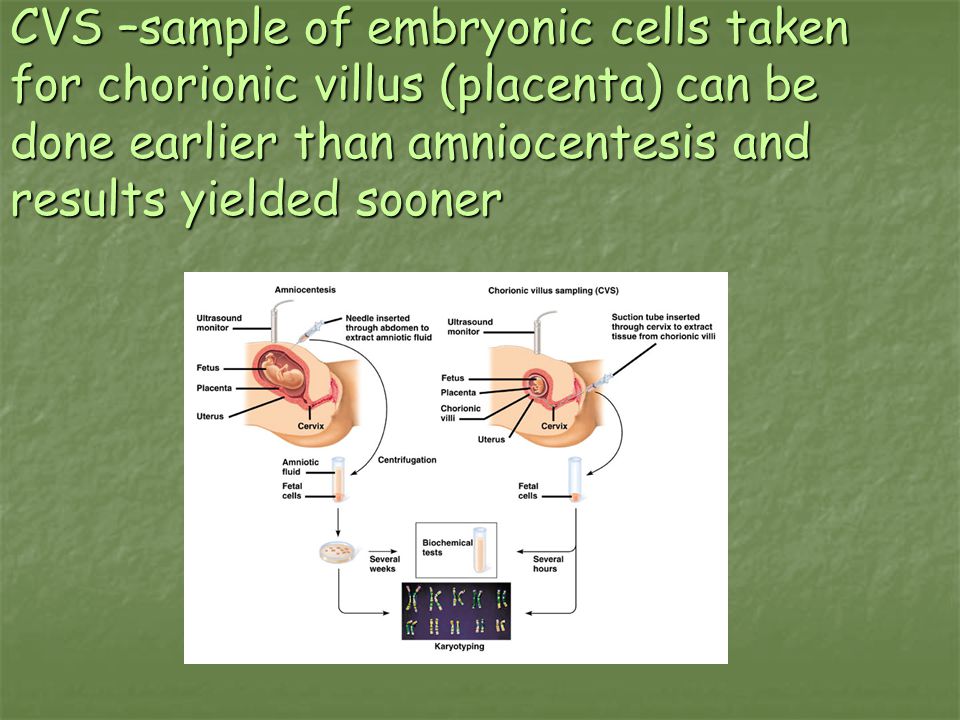
An alternative to amniocentesis is a test called chorionic villus sampling (CVS).
This is where a small sample of cells from the placenta, the organ that links the mother's blood supply with her baby's, is removed for testing.
It's usually carried out between the 11th and 14th weeks of pregnancy, although it can be performed later than this if necessary.
With CVS, the risk of miscarriage is similar to the risk of miscarriage for amniocentesis (up to 1 out of every 200).
As the test can be carried out earlier, you'll have more time to consider the results.
If you're offered tests to look for a genetic or chromosomal condition in your baby, a specialist involved in carrying out the test will be able to discuss the different options with you and help you make a decision.
Page last reviewed: 12 October 2022
Next review due: 12 October 2025
Amniocentesis - Mayo Clinic
Overview
Amniocentesis
Amniocentesis
Amniocentesis is a test done during pregnancy. During amniocentesis, an ultrasound wand (transducer) is used to show a baby's position in the uterus on a monitor. A sample of amniotic fluid, which contains fetal cells and chemicals produced by the baby, is then taken for testing.
Amniocentesis is done to remove amniotic fluid and cells from the uterus for testing or treatment. Amniotic fluid surrounds and protects a baby during pregnancy.
Amniocentesis can provide useful information about a baby's health. But it's important to know the risks of amniocentesis — and be prepared for the results.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Obstetricks
Why it's done
Amniocentesis can be done for a number of reasons:
- Genetic testing. Genetic amniocentesis involves taking a sample of amniotic fluid and testing the DNA from the cells for diagnosis of certain conditions, such as Down syndrome. This might follow another screening test that showed a high risk of the condition.
- Diagnosis of fetal infection. Occasionally, amniocentesis is used to look for infection or other illness in the baby.
- Treatment. Amniocentesis might be done to drain amniotic fluid from the uterus if too much has built up — a condition called polyhydramnios.
- Fetal lung testing.
 If delivery is planned sooner than 39 weeks, amniotic fluid might be tested to help find out whether a baby's lungs are mature enough for birth. This is rarely done.
If delivery is planned sooner than 39 weeks, amniotic fluid might be tested to help find out whether a baby's lungs are mature enough for birth. This is rarely done.
Genetic amniocentesis
Genetic amniocentesis can provide information about the baby's genes. Generally, genetic amniocentesis is offered when the test results might affect how to manage the pregnancy.
Genetic amniocentesis is usually done between weeks 14 and 20 of pregnancy. Amniocentesis done before week 14 of pregnancy might lead to more complications.
Reasons to consider genetic amniocentesis include:
- Having positive results from a prenatal screening test. If the results of a screening test — such as the first-trimester screen or prenatal cell-free DNA screening — show high risk or are worrisome, amniocentesis might confirm or rule out a diagnosis.
- Having an earlier pregnancy affected by a genetic condition. A health care provider might suggest amniocentesis to look for that condition.

- Being 35 or older. Babies born to people 35 and older have a higher risk of chromosomal conditions, such as Down syndrome. A health care provider might suggest amniocentesis to rule out these conditions if prenatal cell-free DNA screening is positive.
- Having a family history of a genetic condition, or if the parents are carriers of a genetic condition. Besides identifying Down syndrome, amniocentesis can be used to diagnose other genetic conditions, such as cystic fibrosis.
- Having unusual ultrasound findings. A health care provider might recommend amniocentesis to diagnose or rule out genetic conditions associated with unusual ultrasound findings.
More Information
- Prenatal testing: Quick guide to common tests
- Cleft lip and cleft palate
- Congenital adrenal hyperplasia
- Cytomegalovirus (CMV) infection
- Down syndrome
- Hunter syndrome
- Incompetent cervix
- Spina bifida
- Thalassemia
- Toxoplasmosis
- Triple X syndrome
- Turner syndrome
Request an Appointment at Mayo Clinic
Risks
Amniocentesis carries risks, which occur in approximately 1 in 900 tests.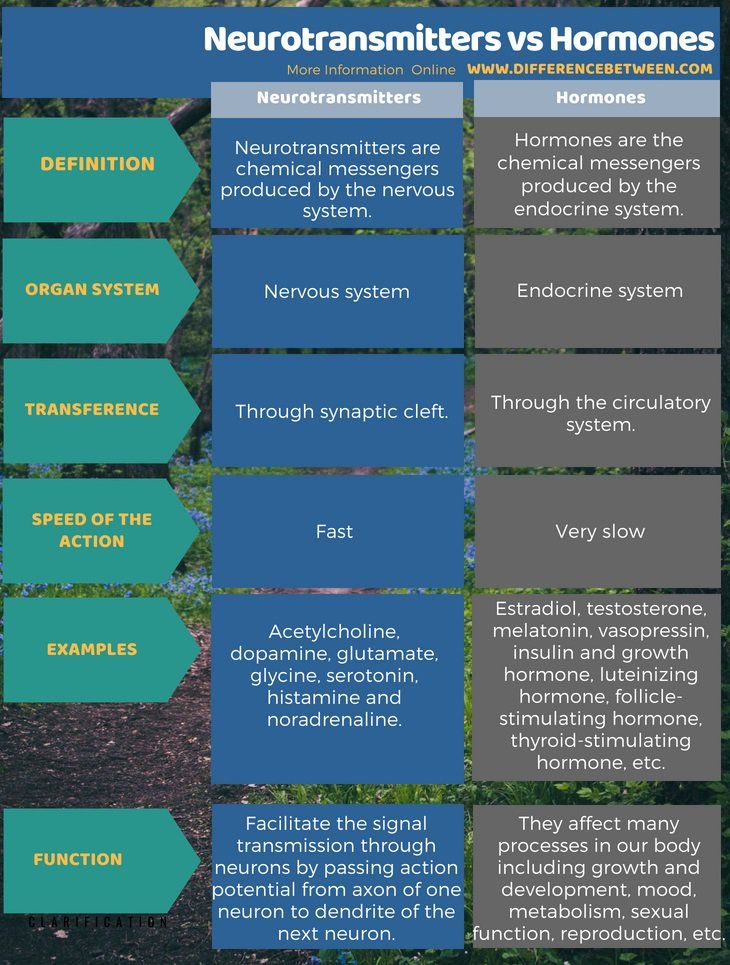 They include:
They include:
- Leaking amniotic fluid. Rarely, amniotic fluid leaks through the vagina after amniocentesis. In most cases, the amount of fluid lost is small and stops within one week with no effect on the pregnancy.
- Miscarriage. Second-trimester amniocentesis carries a slight risk of miscarriage — about 0.1% to 0.3% when done by a skilled person using ultrasound. Research suggests that the risk of pregnancy loss is higher for amniocentesis done before 15 weeks of pregnancy.
- Needle injury. During amniocentesis, the baby might move an arm or leg into the path of the needle. Serious needle injuries are rare.
- Rh sensitization. Rarely, amniocentesis might cause the baby's blood cells to enter the pregnant person's bloodstream. Those with Rh negative blood who haven't developed antibodies to Rh positive blood are given an injection of a blood product, Rh immune globulin, after amniocentesis.
 This prevents the body from making Rh antibodies that can cross the placenta and damage the baby's red blood cells.
This prevents the body from making Rh antibodies that can cross the placenta and damage the baby's red blood cells. - Infection. Very rarely, amniocentesis might trigger a uterine infection.
- Infection transmission. Someone who has an infection — such as hepatitis C, toxoplasmosis or HIV/AIDS — might transfer it to the baby during amniocentesis.
Remember, genetic amniocentesis is usually offered to pregnant people for whom the test results might greatly affect how they manage the pregnancy. The decision to have genetic amniocentesis is yours. Your health care provider or genetic counselor can give you information to help you decide.
How you prepare
Your health care provider will explain the procedure and ask you to sign a consent form. Consider asking someone to accompany you to the appointment for emotional support or to drive you home afterward.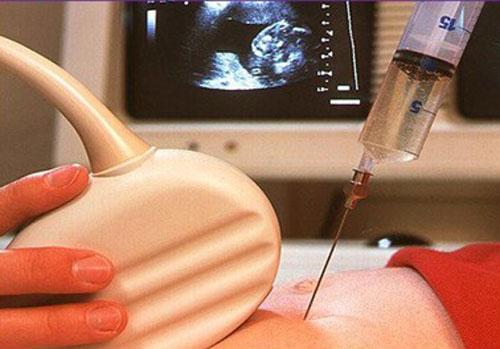
What you can expect
Amniocentesis is usually done in an outpatient obstetric center or a health care provider's office.
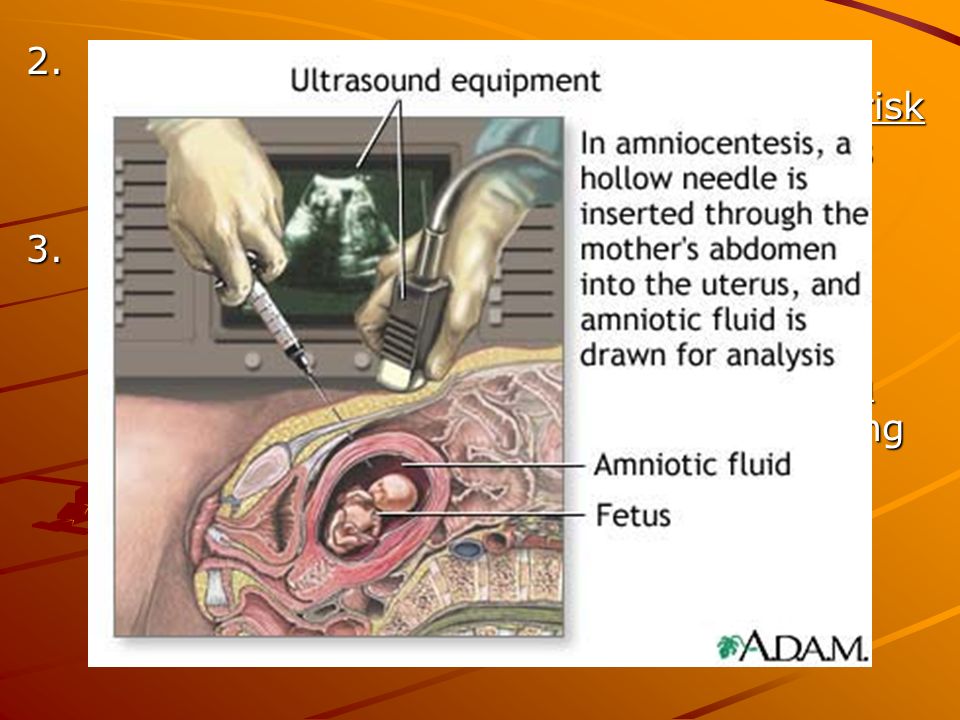
During the procedure
First, a health care provider will use ultrasound to pinpoint where the baby is in the uterus. You'll lie on your back on an exam table with your belly showing. Your health care provider will apply a gel to your belly and then use a small device known as an ultrasound transducer to show your baby's position on a monitor.
Next, your health care provider will clean your abdomen. A numbing medication generally isn't used. Most people report only mild soreness during the procedure.
Guided by ultrasound, your health care provider will insert a thin, hollow needle through your stomach wall and into the uterus. A small amount of amniotic fluid is drawn into a syringe. The needle is then removed.
You need to lie still while the needle is put in and the amniotic fluid is taken out. You might feel a sting when the needle enters your skin.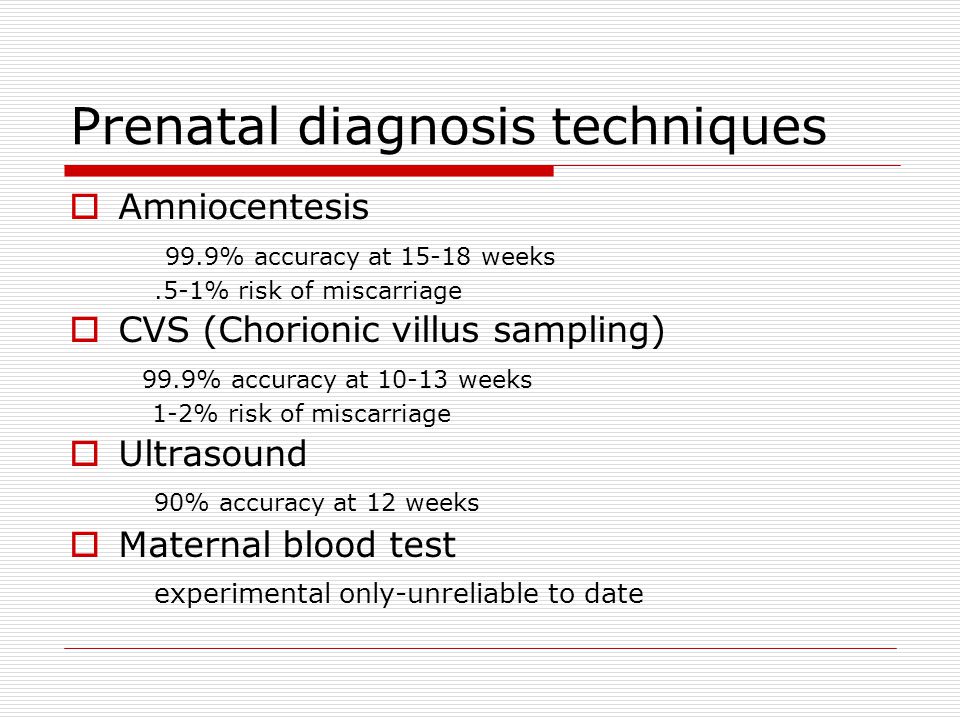 You might feel cramping when the needle enters your uterus.
You might feel cramping when the needle enters your uterus.
After the procedure
After amniocentesis, your health care provider will continue using the ultrasound to monitor your baby's heart rate. You might have cramping or mild pelvic pain after an amniocentesis.
You can return to your regular activities after the test.
The sample of amniotic fluid will be looked at in a lab. Some results might be available within a few days. Other results might take several weeks.
Contact your health care provider if you have:
- Bleeding or loss of amniotic fluid through the vagina
- Severe uterine cramping that lasts more than a few hours
- Fever
- Redness where the needle was inserted
- Fetal activity that is different than usual or no fetal movement
Results
Your health care provider or a genetic counselor will help you understand your amniocentesis results.
For genetic amniocentesis, test results can rule out or diagnose some genetic conditions, such as Down syndrome.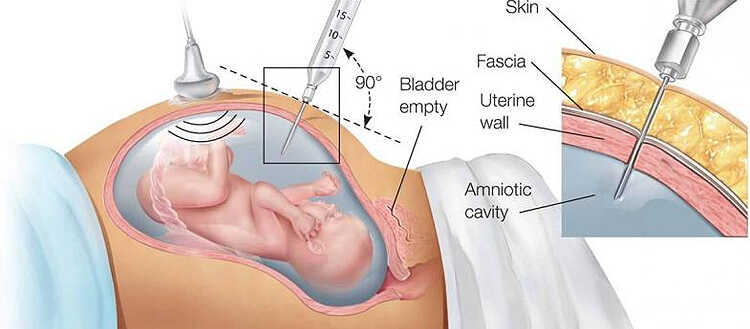 Amniocentesis can't identify all genetic conditions and birth defects.
Amniocentesis can't identify all genetic conditions and birth defects.
If amniocentesis suggests that your baby has a genetic or chromosomal condition that can't be treated, you might face hard decisions. Seek support from your health care team and your loved ones.
By Mayo Clinic Staff
Related
Products & Services
What is amniocentesis, indications and procedure
What is amniocentesis?
Amniocentesis is a specific amniotic fluid test. A study is carried out by puncturing the abdomen, the embryonic membrane in order to obtain a sample of the amniotic fluid containing fetal cells. According to the results of studies of the amniotic fluid, the doctor can determine the presence or absence of genetic diseases in the unborn child. Amniocentesis in Kyiv is successfully performed at the IPF Family Planning Institute.
Depending on the indications, several types of amniotic fluid tests are carried out:
- hormonal analysis, determines the composition and amount of available hormones;
- cytological - studies the cells and particles of the fetus contained in the amniotic fluid in order to detect chromosomal abnormalities;
- immunological - "tell" about possible violations of the emerging immunity;
- biochemical analysis will show the composition and properties of amniotic fluid;
- analysis for general indicators will determine the color, transparency of the liquid, its amount.
The amniocentesis procedure can be performed at the IPF clinic. Sign up for a consultation by going to at the link in contacts.
At what stage of pregnancy can amniocentesis be done?
The study of amniotic fluid is carried out not earlier than the 14th week of pregnancy. Why? Until this time, there are not enough cells in the amniotic fluid to obtain reliable analysis results.
14 weeks of pregnancy is the earliest period at which doctors can perform an amniocentesis: at this time, it is already possible to study the chromosome set of the embryo and make sure that there are no/presence of anomalies, the most common of which is Down syndrome.
The terms of the research procedure are from 16 to 22 weeks, and since the results of the analysis do not come immediately, they are ready in a few weeks, it is better to do it at 16-17 weeks, in case of disappointing results, it is possible to terminate the pregnancy before 20 -and a weekly period.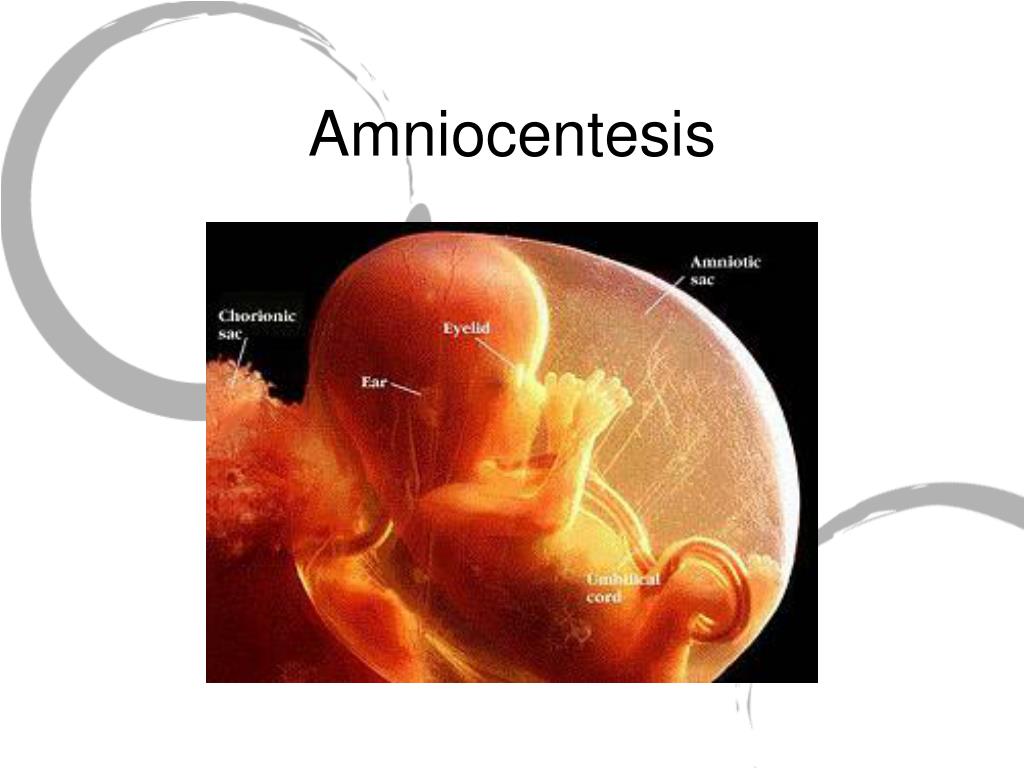
Indications and contraindications for analysis
Indications for analysis
When a woman finds out she is pregnant, she goes to an obstetrician-gynecologist. At the appointment, the doctor collects an anamnesis, prescribes a list of tests, taking into account the duration of pregnancy.
If, at the time of data collection or the results of tests performed, the gynecologist doubts the normal course of pregnancy, the health of the fetus and its healthy development, he may suggest an amniocentesis to the pregnant woman.
What factors may warrant a procedure?
- Age. A doctor may suggest an amniocentesis procedure for a pregnant woman over 35 years of age.
- Burdened heredity. If during the collection of anamnesis it was found that there are genetic diseases in the family of the pregnant woman and her husband, as well as from relatives.
- The woman had a baby with a chromosome abnormality in a previous pregnancy.
- Ultrasound examination raised suspicions regarding the absence of anomalies.
- The results of screening tests showed possible disorders that require invasive intervention to clarify. Invasive intervention is also used in case of necessary surgical treatment of the fetus, as well as in the presence of medical indications for abortion.
Contraindications for amniocentesis
The main contraindication for amniocentesis is the threat of miscarriage.
Do not perform the procedure under the following circumstances:
- placental abruption;
- the presence of urogenital infections;
- the presence of acute inflammatory processes in the body of a woman;
- tumor-like neoplasms of the muscular layers of the uterus of large sizes;
- exacerbations of chronic diseases.
Poor blood clotting, abnormal development of the uterus, location of the placenta on the anterior wall of the uterus can be an obstacle to the analysis.
If a woman fears complications, she may refuse the procedure, but she must clearly understand what the consequences of such a decision may be.
Amniocentesis methods and process
Two methods of amniocentesis are known to doctors today:
- The first method is called the Free Hand Method.
The procedure is carried out under ultrasound control, it is with the help of an ultrasound probe that the insertion site of the puncture needle is specified.
To avoid the risk of possible complications and the threat of miscarriage, the needle injection site is chosen where the placenta is absent or, if this is not possible, in the place where the placental wall is as thin as possible.
- The second method is the “Puncture Adapter Method”.
The second method differs from the first one in that the puncture needle is fixed on the ultrasound probe, and then a trajectory is drawn along which the needle will go.
The main plus of this method is the possibility of visual visibility of the needle and its trajectory during the entire course of the procedure.
However, this method requires experience and certain professional skills from the doctor.
How long does an amniocentesis procedure take and how painful is it?
In terms of time, the procedure will take about 5 minutes, including preparation. Puncture of the abdomen with a puncture needle - 1 minute. The next step in amniocentesis is amniotic fluid sampling. The next 2 hours after the operation, the pregnant woman should be in the hospital under the supervision of doctors.
Patients do not feel any severe pain during amniocentesis, the procedure is similar to a regular injection. A slight movement in the lower abdomen can be felt at the time of amniotic fluid sampling.
Many pregnant women, driven by a sense of fear, ask for pain relief. Yes, local anesthesia can be used, but doctors have noticed that anesthetic injections cause more discomfort than the amniocentesis procedure itself, and therefore gynecologists recommend women not to do anesthesia.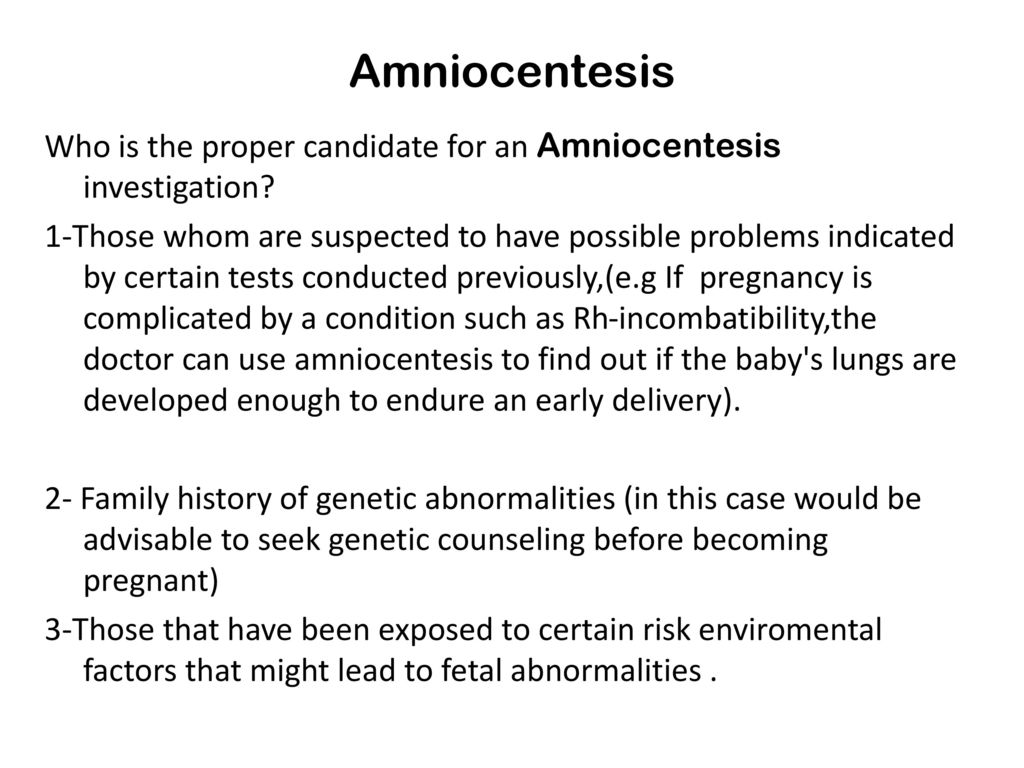
Most women agree, because it is better to endure one injection instead of two.
How is the amniocentesis procedure performed?
The procedure takes place in an office equipped with an ultrasound machine. The gynecologist invites the pregnant woman to lie down and expose her belly. The puncture site on the abdomen is treated with an antiseptic - iodine or alcohol. The next step - the doctor, using an ultrasound machine, determines the most successful place for a puncture: the point of insertion of the needle should be away from the baby and from the placenta.
When looking for a good point, the gynecologist may ask the pregnant woman to turn on one side, then on the other - it all depends on the position of the fetus in the uterus and the location of the placenta.
That's it, a good point has been found: the doctor inserts a thin puncture needle, pierces the skin of the abdomen and enters the membrane surrounding the amniotic fluid. The sampling of amniotic fluid is carried out under ultrasound control - about 2 tablespoons are taken for analysis. Future babies do not feel a lack of amniotic fluid, and soon its amount is replenished.
Future babies do not feel a lack of amniotic fluid, and soon its amount is replenished.
What if I am Rh negative and the baby's father is Rh positive?
If a pregnant woman has a negative Rh factor, and the father of the child has a positive Rh factor, then after the amniocentesis procedure, the pregnant woman is given a special drug that prevents the immune conflict between the body of the mother and the unborn child.
What happens after the amniocentesis?
After the amniotic fluid collection procedure, the specialist will show the baby on the screen of the ultrasound machine, and the woman herself will be able to make sure that nothing happened to the baby.
A few hours after the procedure, the doctor observes the patient, then the pregnant woman can go home. The rest of the day is recommended to be spent in peace, it is advisable for a working woman to take a day off. 2-3 days after the procedure, gynecologists advise not to lift weights, refrain from sex, air travel is not recommended in the next few days.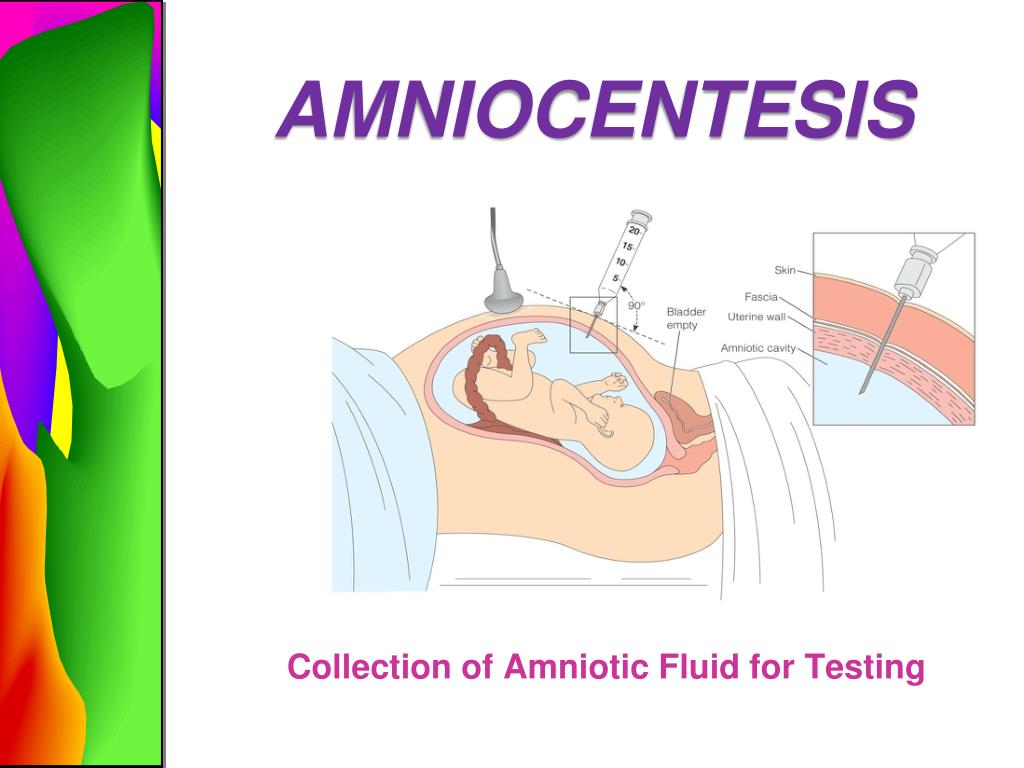
One to two days after the amniocentesis, the woman may experience mild abdominal cramps. There is no cause for concern - this is normal after the procedure.
It is urgent to consult a gynecologist if:
- spasms become pronounced, intensify and become frequent;
- bleeding from the vagina;
- profuse watery discharge began to stand out.
Amniocentesis - how to take the test results?
The test results are within the normal range, they say that your baby is all right - the chromosome set of the unborn child is formed normally, there are no signs of a neural tube defect. The test is quite accurate and informative, but, nevertheless, it should be remembered that no one will give a 100% guarantee about the birth of an absolutely healthy child.
If the test showed that the fetus has congenital malformations, the development takes place with pathologies - a pregnant woman and her husband will have to make a very difficult decision.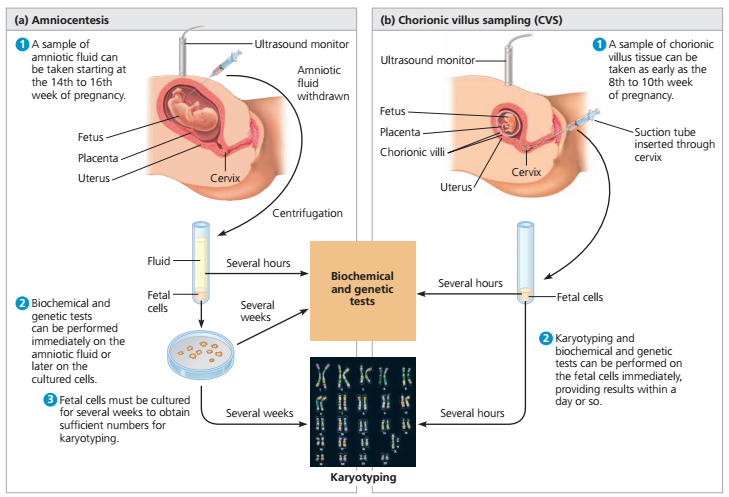 In some cases, the decision depends on various facts - on the type of defect, the partner's reaction to unpleasant news, the woman's personal reaction to what happened.
In some cases, the decision depends on various facts - on the type of defect, the partner's reaction to unpleasant news, the woman's personal reaction to what happened.
Naturally, many women have questions:
- Should I continue this pregnancy?
If a fetus is found to have a serious defect, some women undergo a medical abortion. Others decide to have a baby with a defect.
- Where is the best place to give birth?
If the fetus is found to have a defect that requires surgical intervention at birth, childbirth should only take place in specialized clinics where doctors know how to act, where to provide such services - not new.
For a baby with a disability, which is better: natural delivery or caesarean section?
The results of the amniocentesis will show whether a caesarean section is needed and whether the baby is ready for delivery.
Amniocentesis - is there a similar test?
Chorionic villus sampling may be an alternative to amniocentesis in the first trimester of pregnancy.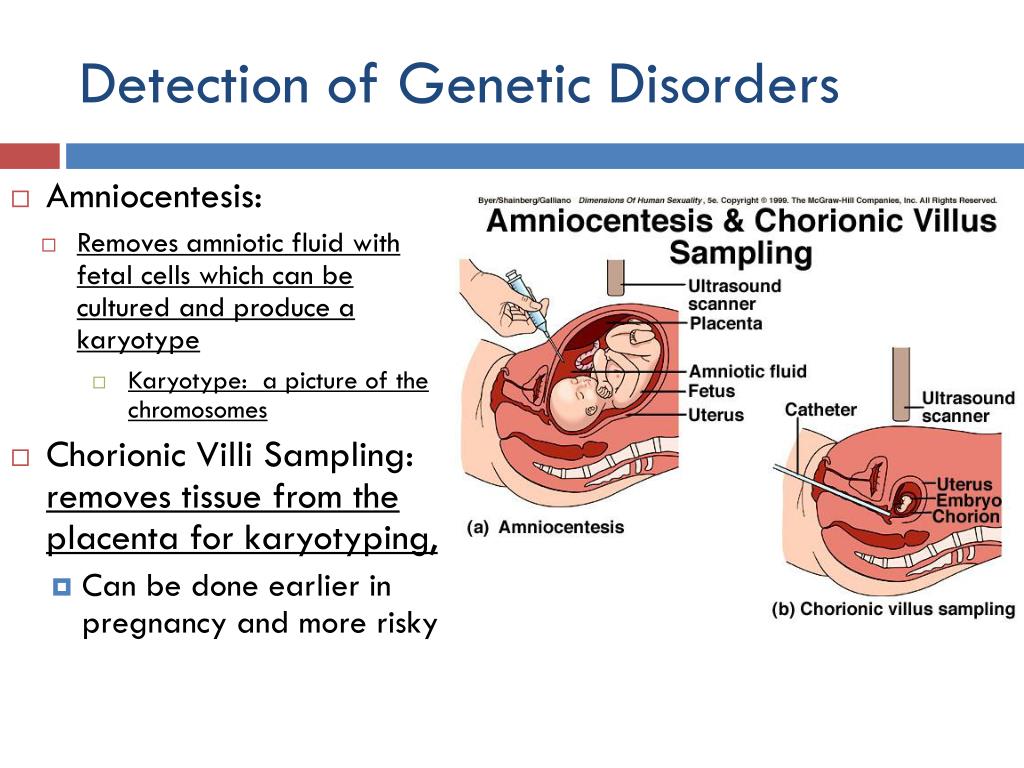 With the help of this test, the presence / absence of Down syndrome and other genetic diseases in the future baby can be detected in early pregnancy. But, this test does not detect neural tube defects.
With the help of this test, the presence / absence of Down syndrome and other genetic diseases in the future baby can be detected in early pregnancy. But, this test does not detect neural tube defects.
Modern research has confirmed that both amniocentesis and chorionic villus sampling cause the same percentage of miscarriages.
Even if the procedures are carried out by experienced graduates, spontaneous abortions occur in 400 cases - 1.
Other studies show an increased risk of 2 or even 4 miscarriages per 400 cases. These statistics are in medical centers where specialists are less professional, where such procedures are not often performed, especially chorionic villus biopsy.
IPF specialists are highly qualified, and therefore the risk of spontaneous miscarriage after procedures in our clinic is minimal.
Amniocentesis - possible risk during test
In most cases, the amniocentesis procedure is quite safe. The reaction of women to the results of a test, which can show that the fetus has a congenital pathology, an inherited disease, or Down's syndrome, is more unpredictable than the possible risks of the procedure. But, nevertheless, certain risks exist:
But, nevertheless, certain risks exist:
- If an inexperienced specialist undertakes the procedure, he can prick the mother or fetus with a needle. To reduce this risk, ultrasound is used to accurately guide the puncture needle. It happens that during the procedure the placenta is pierced, but it is quickly restored.
- There is a risk of infection in the amniotic sac - this happens 1 in 1000 cases.
- Miscarriages. According to statistics, when amniocentesis is performed by experienced specialists, the risk of spontaneous abortion is 1 in 400 cases. Sometimes miscarriages after the procedure are not related to the procedure itself, the problem may lie in the course of pregnancy or in the fetus itself.
- If the procedure is carried out before the 15th week, there is a risk of developing clubfoot in the unborn child.
- There is a risk that maternal and fetal blood will mix during amniocentesis. This fact can cause concern only when the mother and fetus have different Rh factors (the mother has a negative Rh factor) and there is a possibility of Rh sensitization, that is, an increased sensitivity of the body to the effects of various factors.
 To avoid such a risk, a woman is given a special vaccine after the procedure that prevents this risk.
To avoid such a risk, a woman is given a special vaccine after the procedure that prevents this risk.
norm, examination, analysis, determination - to be submitted to the DNAOM laboratory
An accompanying document is sent to the laboratory along with the biomaterial (a referral from a doctor indicating the patient's data, clinical data, grounds for the study) - form No. 6.
Cytogenetic study (karyotype) of amniotic fluid ) to detect serious hereditary diseases, malformations, genetic diseases and chromosomal abnormalities in a child.
Amniocentesis
During an amniocentesis, the doctor removes a small amount of amniotic fluid (amniotic fluid) using a long, thin needle inserted through the skin of the abdomen. The amniotic fluid obtained by amniocentesis is then sent to the laboratory.
Timing of amniocentesis
Amniocentesis is performed at the 16th week of pregnancy.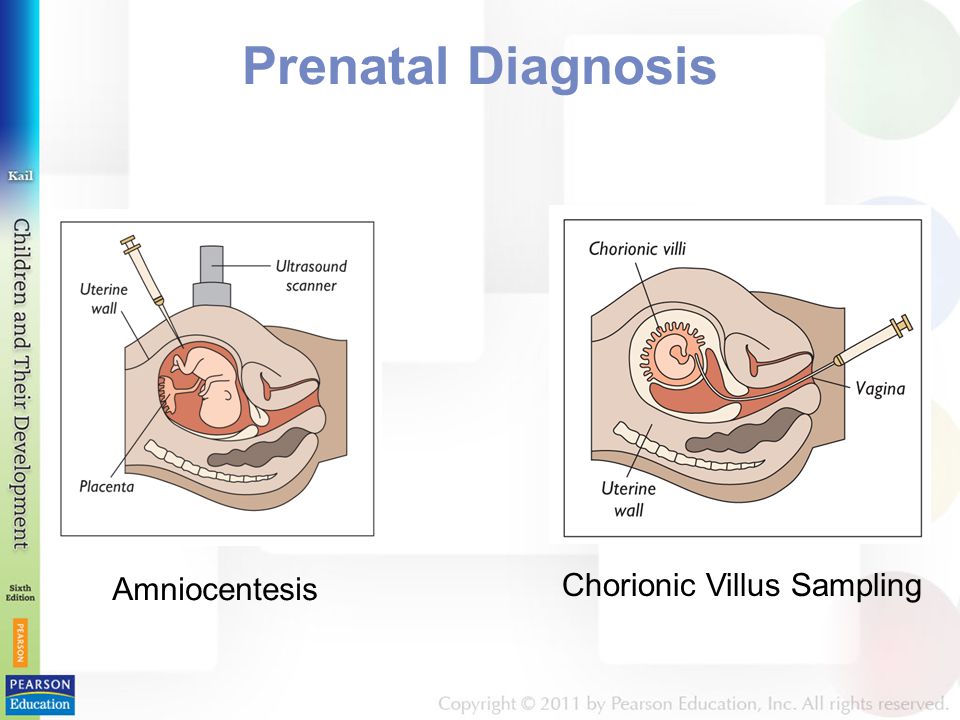 Earlier dates (13–15 weeks) are also acceptable with careful observance of security measures. It is important to remember that during amniocentesis there is an invasion of the internal processes of growth and development of the unborn child. Therefore, amniocentesis is not recommended for every pregnant woman.
Earlier dates (13–15 weeks) are also acceptable with careful observance of security measures. It is important to remember that during amniocentesis there is an invasion of the internal processes of growth and development of the unborn child. Therefore, amniocentesis is not recommended for every pregnant woman.
Cytogenetic examination (karyotype) of amniotic fluid allows to detect a deviation in the number of chromosomes (aneuploidy), to diagnose Down syndrome (chromosome 21), and any excess or deficiency of whole chromosomes. The test also allows you to find rare additions or deficiencies in the chromosome.
Amniocentesis can detect the following diseases:
- Hereditary diseases.
- Malformations (heart defects, cleft lip, etc.).
- Chromosomal disorders such as Down syndrome and Edwards syndrome.
- Spina bifida.
- Causes of early unexplained miscarriages.
- Infections (toxoplasmosis, cytomegalovirus, rubella, bacterial infections).
Indications for amniocentesis
Since amniocentesis is an invasive procedure, it is prescribed strictly according to indications:
- Detection of congenital and hereditary diseases (study of the karyotype of the obtained cells, determination of the number of chromosomes and their structure).
- Adverse screening results (abnormalities on ultrasound, in the biochemical analysis of blood - "triple" or "double" test).
- The need for the introduction of drugs into the fetal bladder for early termination of pregnancy.
- The age of the woman (at 35 years of age or older, the risk of having a child with chromosomal abnormalities increases).
- Amnioreduction (removal of excess amniotic fluid in case of polyhydramnios).
- Fetal monitoring (determining the degree of maturity of the lungs, the production of surfactant (a substance that prevents the lungs from collapsing on a breath), the severity of fetal hemolytic disease).
- Definition of intrauterine infections.
- Fetotherapy (intra-amniotic administration of drugs for the treatment of the fetus).
- Fetosurgery (treatment of the fetus by surgery).
- Birth of a child with a history of hereditary pathology.
- Complicated family history (the spouses have relatives with hereditary diseases or chromosomal abnormalities).
Contraindications
The procedure is contraindicated in the following situations:
- Threatening placental abruption.
- Possibility of termination of pregnancy (threat).
- Malformations of the uterus.
- Tumors of the muscular layer of the uterus.
- Febrile state of a woman.
- Inflammatory diseases in acute form or in the period of exacerbation.
Preparation
Before the procedure, a woman is assigned a routine laboratory examination (KLA, OAM, vaginal smear).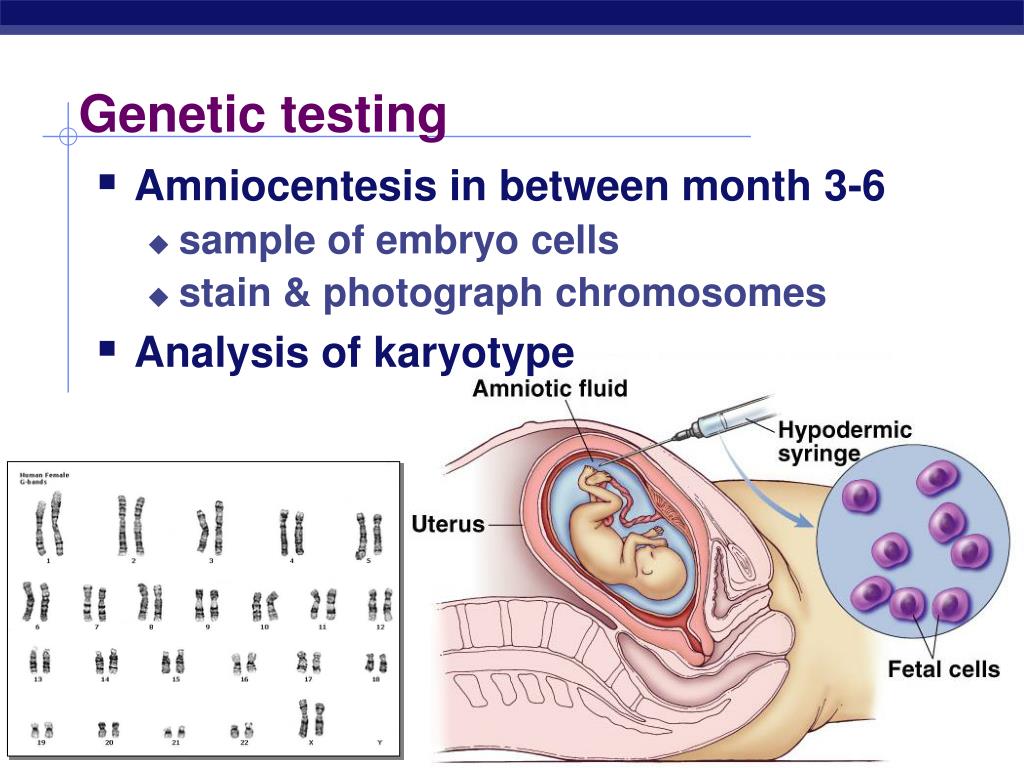 In addition, a mandatory ultrasound is performed on the eve of the procedure to identify the localization of the placenta, the number of fetuses in multiple pregnancies, clarify the gestational age and the amount of amniotic fluid, and identify various anatomical features that can affect the conduct of amniocentesis. Also, before the manipulation, you should not take antiplatelet agents and anticoagulants for 5 days - drugs that thin the blood and reduce its coagulability (aspirin, chimes, heparin).
In addition, a mandatory ultrasound is performed on the eve of the procedure to identify the localization of the placenta, the number of fetuses in multiple pregnancies, clarify the gestational age and the amount of amniotic fluid, and identify various anatomical features that can affect the conduct of amniocentesis. Also, before the manipulation, you should not take antiplatelet agents and anticoagulants for 5 days - drugs that thin the blood and reduce its coagulability (aspirin, chimes, heparin).
If amniotic fluid is collected before 20 weeks, the woman must come to the procedure with a full bladder. At 20 weeks or more, amniocentesis is performed with an empty bladder.
Before the manipulation, the woman is informed about the procedure, possible risks, and she is asked to sign a consent form for the amniocentesis.
Interpretation of results
The accuracy of the study of amniotic fluid and the diagnosis of congenital and hereditary diseases reaches 99%.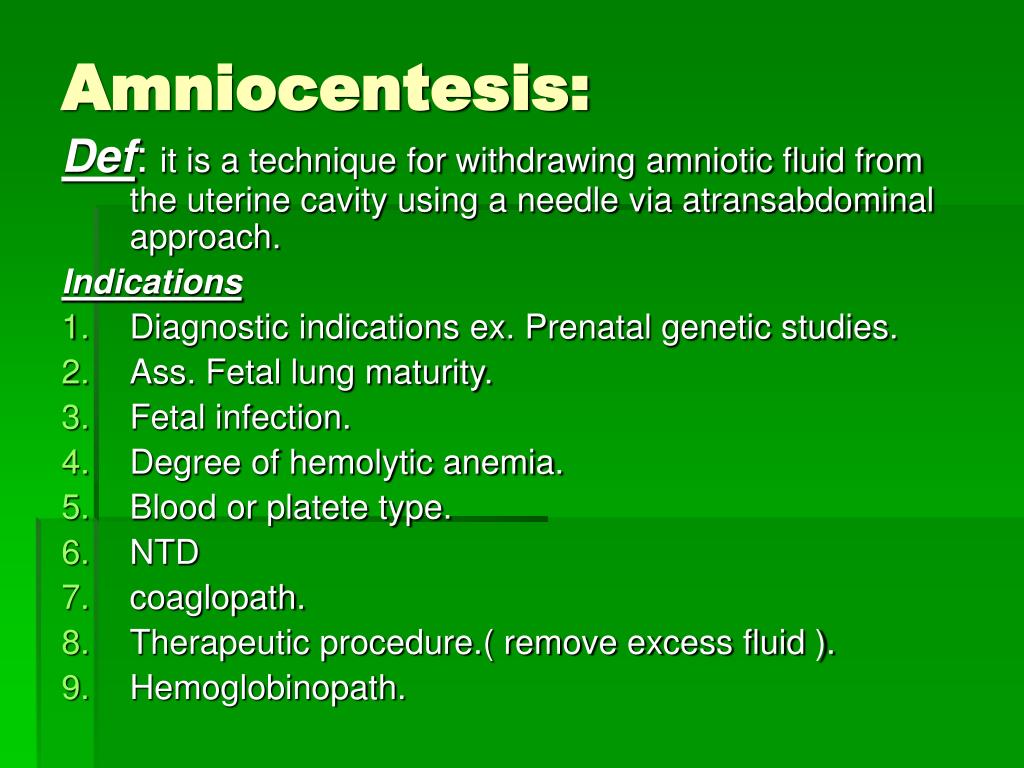 After the amniotic fluid is obtained, it is delivered to the laboratory and fruit cells are isolated from it. These cells are planted on nutrient media to increase their number. Cytogenetic analysis of normal waters shows the content of 23 pairs of normal, without structural abnormalities of chromosomes.
After the amniotic fluid is obtained, it is delivered to the laboratory and fruit cells are isolated from it. These cells are planted on nutrient media to increase their number. Cytogenetic analysis of normal waters shows the content of 23 pairs of normal, without structural abnormalities of chromosomes.
The presence of such chromosomal diseases as Down syndrome, Edwards syndrome, Patau can be determined by the quantity and quality of chromosomes.
Identify/confirm neural tube malformations: anencephaly and spinal hernia.
Cytogenetic analysis of amniotic fluid reveals hereditary diseases (cystic fibrosis, sickle cell anemia), which are not normally present.
Fluid examination also reveals intrauterine infection (herpes, rubella).
Allows you to determine the group and Rh factor of the fetus and gender, which is important for predicting some hereditary diseases linked to the Y-chromosome or X-chromosome (for example, hemophilia).
To determine the severity of fetal hemolytic disease, and decide on the further tactics of pregnancy management.