How to make an infant poop when constipated
Symptoms, Treatment and When to Call a Doctor
Nationwide Children’s Hospital
Constipation (con-sta-PA-shun) in infants can worry parents. Most of the time, your baby is not really constipated. They may not have developed a routine for pooping yet. Some babies do not develop a bowel movement (BM) pattern for a while.
An infant’s BM pattern can change if their diet changes, like switching from breastmilk to formula, starting solid foods, or drinking less formula than usual. If your baby’s stool (poop) is not soft or easily passed, then they may be constipated.
In rare cases, constipation may be caused by a lack of nerves going to the intestines or by a problem with the way the intestine formed at birth. Your baby can be tested for these conditions if your health care provider feels it is needed.
Signs of Constipation
- less stools than their usual pattern
- straining more than normal to have a bowel movement
- a change in how the stool looks from soft and mushy to:
- small, hard pebbles, or like a large, round golf ball
- loose and watery
- abdomen (belly) bloated or swollen with gas
- painful cramps
Treatment
- If your baby is not eating baby food yet, you may give 1 to 2 ounces of 100% fruit juice (pear, prune, cherry, or apple) once a day.
Stop the juice if their stools become too loose.
- If they are old enough to eat baby foods, feed them pureed pears, peaches, or prunes instead of giving them juice.
- If your baby eats cereal, it may help to give oatmeal, wheat, or barley cereal. Rice cereal can cause constipation in some children.
- Sometimes giving your baby a warm bath to relax them or exercising their legs, like riding a bicycle, will help stimulate the bowels to move (Picture 1).
- If it has been a few days since your baby has pooped and the juice or pureed food has not worked, then you can try a glycerin suppository. Place your baby on their back. Gently push the suppository into their anus (bottom). Suppositories are meant for occasional use.
- Contact your baby’s health care provider before giving them laxatives, baby mineral oil, or enemas to treat constipation.
Medical Therapy
Your child’s health care provider may order the following treatments:
- Give your child medication.
- Check your child’s temperature using a digital, rectal thermometer. Put a small amount of petroleum jelly (Vaseline®) on its tip before inserting into the rectum. Taking a rectal temperature may stimulate the baby to pass stool.
When to Call the Health Care Provider
Call the health care provider if any of the following occurs:
- Your baby is irritable and seems to be having stomach pain. Infants will pull their legs up to their stomach and cry when they are in pain.
- Your baby has constipation and develops vomiting, and their belly looks like it is bloated or filled with gas.
- You see blood in their stool.
- Their constipation does not get better with treatment.
If you have any questions or concerns, call your baby’s health care provider.
Constipation: Infant (PDF), Spanish (PDF), Somali (PDF), Arabic (PDF), Nepali (PDF)
HH-I-14 ©Copyright 1984, Revised 2022, Nationwide Children’s Hospital
You Might Also Be Interested In
Blog
Pelvic Floor Physical Therapy: How It Can Help
Podcast
PediaCast 503 Your Childs Stomach Part 1
Blog
Senna-Based Laxatives for Kids’ Constipation: Are They Safe?
Baby constipation: Top 7 home remedies
Babies often go a long time between bowel movements. Most of the time, it is normal for a baby to go days or even more than a week without a bowel movement. However, a baby may sometimes be constipated and need a little help.
Most of the time, it is normal for a baby to go days or even more than a week without a bowel movement. However, a baby may sometimes be constipated and need a little help.
If a baby is constipated, a pediatrician may recommend using home remedies as a first-line treatment for baby constipation.
Home remedies for constipation in a baby include:
1. Exercise
Moving a baby’s legs can help relieve constipation.
As with adults, exercise and movement tend to stimulate a baby’s bowels.
However, as babies may not be walking or even crawling yet, a parent or caregiver may want to help them exercise to relieve constipation.
The parent or caregiver can gently move the baby’s legs while they are lying on their back to mimic the motion of riding a bicycle. Doing this may help the bowels function and relieve constipation.
2. A warm bath
Giving a baby a warm bath can relax their abdominal muscles and help them stop straining. It can also relieve some of the discomfort relating to constipation.
3. Dietary changes
Certain dietary changes may help constipation, but these will vary depending on the baby’s age and diet.
While breastfeeding a baby, a woman could eliminate certain foods, such as dairy, from her diet. It may take some trial and error to identify the dietary changes that help, and it is quite possible that changes in the diet will have no effect on the baby’s constipation.
For formula-fed babies, a parent or caregiver may want to try a different kind of formula. It is best not to switch to a gentle or dairy-free formula without consulting a pediatrician first. If one change does not make a difference, continuing to try different formulas is unlikely to help.
If an infant is eating solid foods, parents or caregivers should look to introduce foods that are good sources of fiber.
Many fruits and vegetables can help stimulate the bowels because of their higher fiber content. Good food choices for babies with constipation include:
- skinless apples
- broccoli
- whole grains, such as oatmeal or whole-grain bread or pasta
- peaches
- pears
- plums
4.
 Hydration
HydrationYoung infants do not typically need supplemental liquids as they get their hydration from breast milk or formula.
However, babies that are constipated may benefit from a small amount of extra liquid.
Pediatricians sometimes recommend adding a small amount of water or, occasionally, fruit juice, to the baby’s diet when they are over 2–4 months old and are constipated.
5. Massage
There are several ways to massage a baby’s stomach to relieve constipation. These include:
- Using the fingertip to make circular motions on the stomach in a clockwise pattern.
- Walking the fingers around the naval in a clockwise pattern.
- Holding the baby’s knees and feet together and gently pushing the feet toward the belly.
- Stroking from the rib cage down past the belly button with the edge of a finger.
6. Fruit juice
A small amount of pure apple juice can help soften stool.
After a baby reaches 2–4 months of age, they can have a small amount of fruit juice, such as 100-percent prune or apple juice. This juice may help treat constipation.
This juice may help treat constipation.
Experts may recommend starting with about 2–4 ounces of fruit juice. The sugar in the juice is hard to digest. As a result, more liquid enters the intestines, which helps soften and break up the stool.
However, a parent or caregiver should not give fruit juice to a baby for the first time without consulting their pediatrician.
7. Taking a rectal temperature
When a baby is constipated, taking the baby’s rectal temperature with a clean, lubricated thermometer may help them pass stool.
It is important not to use this method very often, as it can make constipation worse. The baby may start not wanting to pass a bowel movement without help, or they may begin to associate having a bowel movement with discomfort, leading them to fuss or cry more during the process.
Anyone who feels as though they often need to use this method to help the baby have a bowel movement should talk to the baby’s doctor.
As infants may go for extended periods without a bowel movement, it can be hard to tell if they are constipated. Signs that indicate constipation in a baby include:
Signs that indicate constipation in a baby include:
- infrequent stools that are not soft in consistency
- clay-like stool consistency
- hard pellets of stool
- long periods of straining or crying while trying to have a bowel movement
- streaks of red blood in the stool
- lack of appetite
- a hard belly
Signs of constipation in babies vary depending on their age and diet. A normal bowel movement before a baby begins eating solid food should be very soft, almost like the consistency of peanut butter or even looser.
Hard baby stool prior to solid food is the most obvious indication of constipation in babies.
At first, breastfed babies may pass stool often since breast milk is easy to digest. However, once a baby is between 3 and 6 weeks old, they may only pass a large, soft stool once a week and sometimes even less.
Formula-fed babies tend to pass stool more frequently than breastfed babies. Most formula-fed babies will have a bowel movement at least once a day or every other day. However, some formula-fed babies may go longer between bowel movements without being constipated.
However, some formula-fed babies may go longer between bowel movements without being constipated.
Once a parent introduces solid food to a baby’s diet, a baby may be more likely to experience constipation. A baby may also be more likely to become constipated if a parent or caregiver introduces cow’s milk (other than formula) to their diet.
Share on PinterestA doctor should assess a baby with ongoing constipation.
It is advisable to call a pediatrician if a baby has not passed a stool after a day or two and there are other signs present, such as:
- blood in the stool
- the baby seems to be irritable
- the baby appears to have abdominal pain
- there is no improvement in the baby’s constipation after taking steps to treat it
Treatment typically starts with home remedies. If home remedies do not work, a doctor may examine the baby and, in rare cases, prescribe medications, such as:
- laxatives
- enemas
- suppositories
People should never give these medications to a baby unless a doctor prescribes them.
Constipation can lead to discomfort and irritability in a baby. People can try several at-home methods to help alleviate constipation.
If symptoms do not improve, it is best to speak to the infant’s pediatrician for additional strategies.
Read the article in Spanish.
Constipation in children. Prevention. Diet therapy
home
Articles
Health
Sabitova Vasily Ilyasovna Gastroenterologist
06/21/2019
Constipation is widespread among both adults and children (5-30% depending on the diagnostic criteria). Symptoms become chronic in more than 30% of patients, not only cause discomfort and pain to the child himself, but also disrupt the quality of life of his family.
CONSTIPATION - a condition manifested by an increase in the intervals between bowel movements (compared to the individual norm) or systematically slow, difficult and / or insufficient bowel movements. Constipation also includes stools with “gruel”, but after defecation was absent for up to 3 days.
Constipation also includes stools with “gruel”, but after defecation was absent for up to 3 days.
Constipation can be related to functional or organic causes (abnormalities, inflammation). In children, 90-95% of constipation is functional. The peak incidence of functional constipation falls on 2-4 years, when they begin to accustom the child to the potty / toilet.
Main causes of functional constipation
- Pain
- Fever
- Dehydration
- Wrong diet of a nursing mother
- Insufficient drinking regime of a child with artificial feeding
- Insufficient drinking regimen of a breast-fed child with the introduction of complementary foods
- Early transition of the child to artificial feeding
- Fast transition of the baby from one mixture to another (less than 7 days)
- Irrational nutrition of the child (for a long time the child receives food with a large amount of proteins, fats and insufficient dietary fiber, abuse of drinks containing a large amount of astringents - tea, coffee, cocoa)
- Excessive use of baby hygiene products or the development of an allergic reaction of the skin of the perianal area
- Consequences of perinatal injuries of the nervous system
- Rickets, vitamin D deficiency
- Anemia
- Impaired thyroid function (deficiency - hypothyroidism)
- Food allergy, especially cow's milk protein allergy
- Forced potty training, period of adaptation to new conditions (nursery, kindergarten)
- Physical inactivity - a sedentary lifestyle
- Mental trauma or stress
- Systematic suppression of the urge to empty the bowels, associated, for example, with the beginning of attending a kindergarten, school, etc.

- Taking certain drugs
- Constipation in family members
Frequency of defecation in children of different ages
| Age | Number of bowel movements per week | Number of bowel movements per day |
| 0 – 3 months breastfeeding artificial feeding | 5 - 40 5 - 20 | 2.9 2.0 |
| 6 - 12 months | 5 - 28 | 1.8 |
| 1 - 3 years | 4-21 | 1.4 |
| 4 years and older | 3 - 14 | 1.0 |
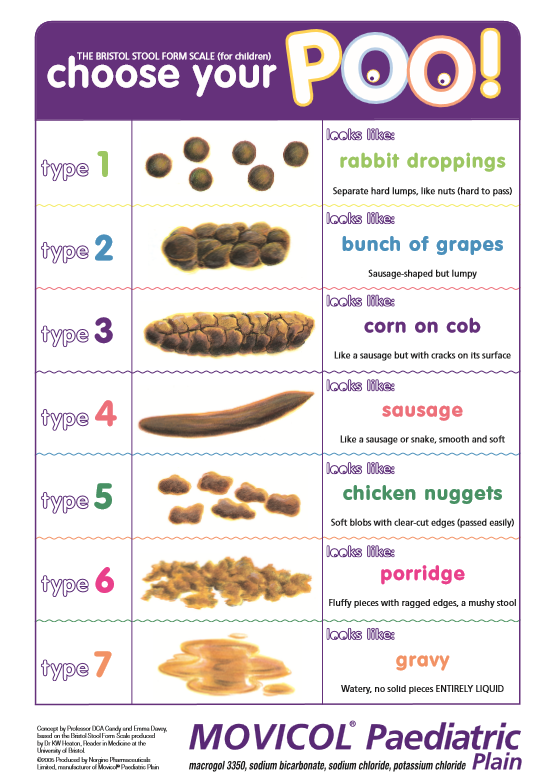
In addition to the frequency of the chair, you should pay attention to its nature. For a more objective assessment, the “Bristol fecal shape scale” is convenient, since it is the shape of the feces, and not the frequency of the stool, that is more consistent with the time of intestinal transit.
Bristol stool chart
In accordance with this scale, 3 and 4 form of feces is regarded as normal, and 1 and 2 indicate delayed transit (constipation). Quite often, in practice, there are situations when a child has a bowel movement frequency within the normal range, but the stool is dense, fragmented, in a meager amount. These signs indicate incomplete emptying of the bowels and are considered as manifestations of constipation.
The consistency of the stool in newborns and infants should be mushy. From 6 months to 1.5 - 2 years, feces can be both formalized and mushy. From the age of two, the chair must be decorated.
Signs and symptoms of constipation
- abdominal pain, often bursting, aching, sometimes colicky
- bloating
- change in the shape and consistency of the stool
- excessive flatulence
- unpleasant smell of flatus and stool
- may have pain during bowel movements
- straining during bowel movements
- there may be blood in the stool - on the surface of the feces or in the form of traces on a napkin (indicates an anal fissure)
If you do not eliminate constipation and do not establish bowel movements, then there is a risk of coprostasis (formation of fecal stones) and fecal intoxication:
- loss of appetite
- lack of energy
- general malaise
- depression, irritability
- nausea, vomiting
- skin symptoms - dryness, rash, peeling
- fecal incontinence, stool spotting
- urinary retention and incontinence due to pressure from a crowded bowel on the bladder
- bleeding from fissures, hemorrhoids
The treatment of constipation involves the following goals:
1. Normalization of stool consistency (soft, painless stools)
Normalization of stool consistency (soft, painless stools)
2. Regularity of bowel movements (prevention of re-accumulation of feces)
The treatment of constipation is a sequential, complex, individual process and consists of several stages:
- child and parent education
- correction of nutrition and drinking regimen
- elimination of existing coprostasis with the help of medications
- maintenance therapy
It is necessary to exclude factors that provoke and contribute to constipation (normalization of motor and nutritional regimen, discontinuation of medications that can cause constipation, identification of a food allergen, exclusion or confirmation of neuromuscular disease, celiac disease, etc.).
Lifestyle normalization includes:
- development of a conditioned reflex
- active lifestyle
- gymnastics
- light abdominal massage training
- for small children - laying out on the stomach, bending the legs to the stomach.
Education is the first step in the treatment of functional constipation. It must be remembered that episodes of fecal smearing and encopresis (fecal incontinence) are not arbitrary and should not be blamed on the child, who may already be frightened and disoriented. In some cases, when the intra-family situation is difficult, the help of a family psychologist may be needed.
It is important to understand that the treatment of functional constipation can be lengthy, based on trust, partnership and requires patience. Modern laxatives that are legal in children will not make the intestines “lazy”, will not cause “addiction”, they enter the bloodstream in minimal amounts or are not absorbed at all and are safe for long-term use.
Correction of the behavior of a child with constipation is based on the development of a routine of visiting the toilet, in order to achieve regular defecation. Defecation should be every time at the same time. The urge to defecate is based on the gastrocecal reflex, which manifests itself in the morning 1 hour after eating. A child with constipation needs to spend 3-10 minutes in the toilet (depending on age). It is necessary to plant the child on a potty or offer to visit the toilet after each meal.
A child with constipation needs to spend 3-10 minutes in the toilet (depending on age). It is necessary to plant the child on a potty or offer to visit the toilet after each meal.
A prerequisite for effective defecation is to provide a good support for the legs (a low bench on which the child can put his feet), which helps to increase intra-abdominal pressure.
If the defecation is not successful, the child should never be punished and vice versa. The daily frequency of bowel movements can be noted in a diary, which can be analyzed at a scheduled visit to the doctor.
Treatment of constipation should begin with lifestyle changes, which include dietary modification, drinking regimen and physical activity.
Calculation of fluid volume for healthy children
Children under the age of 1 year should drink at least 100 ml of water per day.
For healthy children weighing 10 to 20 kg the water requirement is calculated using the formula:
100 ml (volume of water for children under 1 year old) + 50 ml per kg for body weight over 10 kg.
For example, with a mass of 12 kg: 100 ml + 2 x 50 ml = 200 ml.
A child weighing 20 kg should drink water: 100 ml + 50 x 10 = 600 ml
For children weighing over 20 kg the following formula is suggested for calculation:
600 ml (volume of water for a child weighing 20 kg) + 20 ml for each kg over 20 kg.
For children over 3-5 years old you can use the calculation of the amount of water: 30ml / kg of weight
Principles of diet therapy for constipation:
- satisfaction of physical needs for nutrients and energy
- exclusion of excessive consumption of proteins and fats, which can inhibit intestinal motility
- enrichment of the diet with dietary fiber
- normalization of intestinal microflora with pro- and prebiotics
If the child is breastfed, then the mother's nutrition is corrected (restriction of products that promote gas formation). With artificial feeding, special mixtures are shown. For constipation associated with an allergy to cow's milk protein, therapeutic mixtures are prescribed if the child is bottle-fed. If the child is breastfed, cow's milk and products based on it are completely excluded from the mother's diet.
For constipation associated with an allergy to cow's milk protein, therapeutic mixtures are prescribed if the child is bottle-fed. If the child is breastfed, cow's milk and products based on it are completely excluded from the mother's diet.
After the introduction of “thick” complementary foods, boiled water is necessary for all children, regardless of the type of feeding.
For older children, it is recommended to eat foods rich in vegetable fibers. It is not recommended to “smear food”, puree, “snacks”, “eating on the go”. Food should be crumbly, meat / poultry / fish - “piece”. A “bulk” breakfast is required to stimulate the “gastrocecal reflex”.
The main source of coarse-fiber vegetable fiber, containing a large amount of dietary fiber, is cereal bran, rye bread, as well as a number of vegetables and fruits. According to the principles of evidence-based medicine, a statistically significant increase in stool frequency and improvement in its consistency was demonstrated with the use of fiber compared with placebo.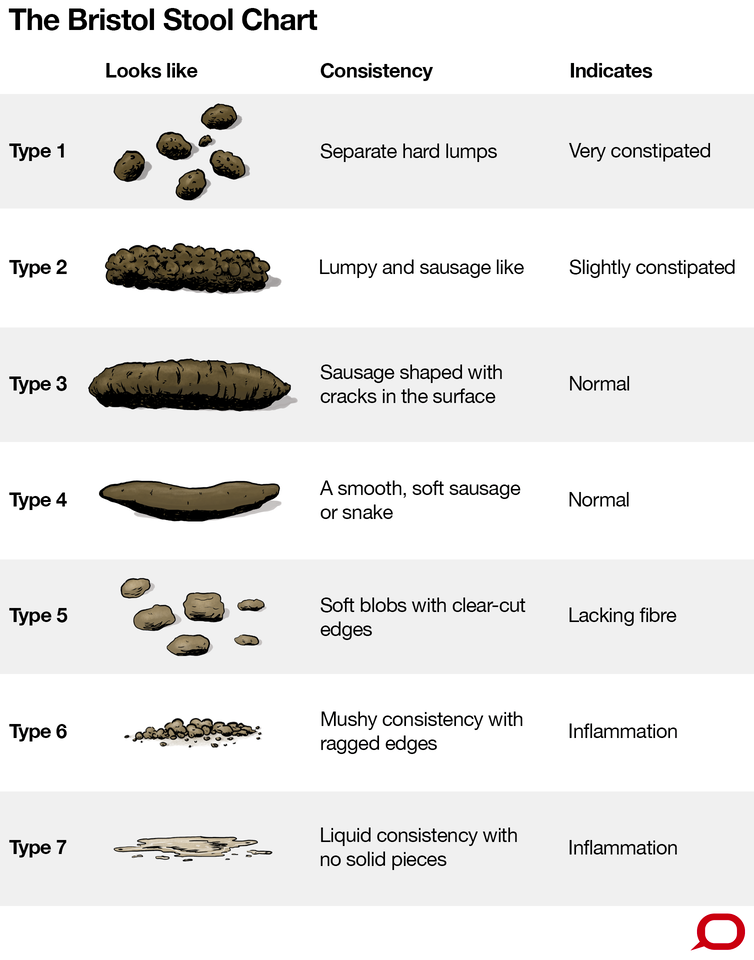
Bran, as the main source of vegetable fiber, is recommended to be added to the second and third courses, after pouring boiling water over it and settling for 20 minutes. Bran can also be used in between meals, drinking plenty of fluids. For school-age children, the total amount of fluid when taking bran should be at least 1.5-2 liters per day, otherwise they mainly act as sorbents, absorbing fluid from the intestines, thereby increasing constipation. The dose is selected individually, it is recommended to start with 1 teaspoon 2-3 times a day, with a gradual increase to 40 g per day. When the effect is achieved, the dose is reduced and limited to one dose.
The American Academy of Pediatrics (2009) recommends a fiber intake of 0.5 g/kg/day (maximum 35 g/day) for all children. Fiber intake below the minimum recommended value has been shown to be a risk factor for chronic constipation in children.
However, long-term intake of a large amount of plant fibers due to fermentation by intestinal microflora is naturally accompanied by bloating and flatulence.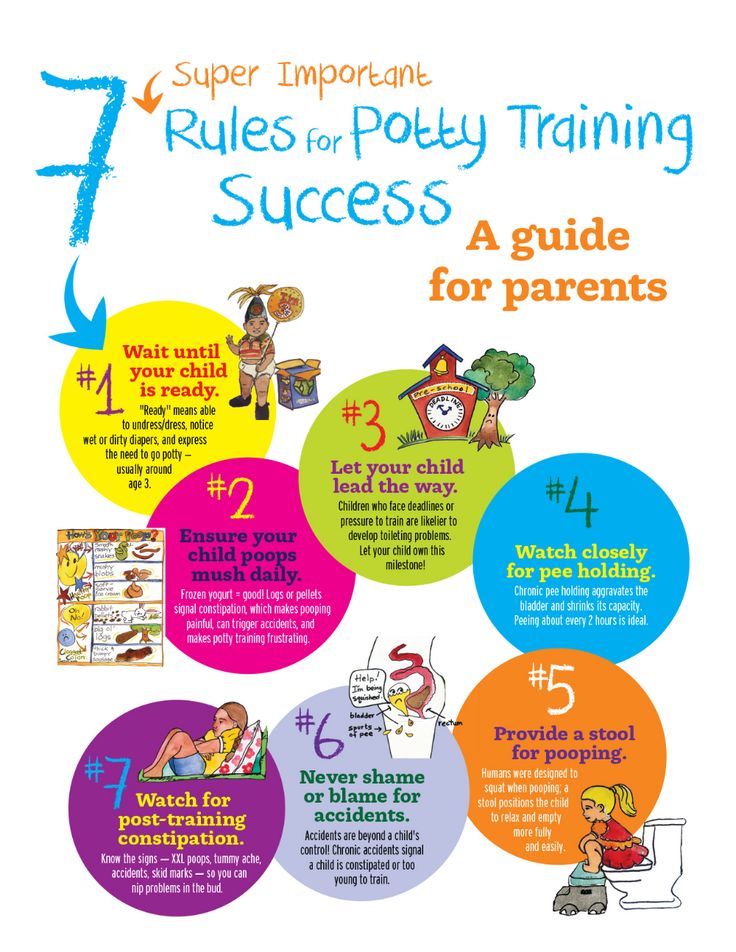
Children with constipation are shown to take cool liquids on an empty stomach (drinking and mineral water, juice, compotes, kvass), to enhance the laxative effect, it is possible to add honey, xylitol or sorbitol. It is very beneficial for bowel function to increase the intake of juices containing sorbitol/sorbitol, such as juice from plums, pears, apricots, peaches and apples,
With “sluggish” bowel function (hypomotor constipation), cool mineral water of medium and high mineralization is used, such as Essentuki 17, Batalinskaya, Arzni, Donat Magnesium, etc.; with spastic constipation (hypermotor constipation, stool form more often type 1) - warm and low mineralization (Essentuki 4). Calculation of mineral water - 3-5 ml / kg per day.
It is necessary to limit milk in its pure form and in dishes, as flatulence may occur with the appearance or intensification of abdominal pain. It is better to replace whole milk with sour-milk products - kefir, acidophilus, yogurt, yogurt, etc.
The diet of children with constipation includes dishes rich in vegetable fiber - salads from fresh vegetables, greens 2-3 times a day, baked apples, stewed vegetables, diluted vegetable and fruit juices with pulp. Food is cooked mostly unground, steamed or boiled in water.
It is preferable to take raw vegetables and fruits (in the absence of contraindications). Especially recommended are tomatoes, zucchini, pumpkin, carrots, beets, lettuce, cauliflower, apples. Dried fruits (prunes, dried apricots, figs) are given in soaked form and as part of cooked dishes. White cabbage, young green beans, green peas are allowed with good tolerance. Parsley, dill, celery are good to add to various dishes and salads.
If after reading the article you still have questions or you do not understand how to apply the recommendations in your particular case, we invite you and your child to be examined by a pediatric gastroenterologist at the DDC. For the convenience of parents, you can make an appointment with a pediatric gastroenterologist at the Children's Diagnostic Center on a weekday and on Saturdays.
We will be happy to help!
Who gets a tan, who gets a blow!
If a child has a fever, what should I do?
Return to the list
How to deal with constipation in a child?
08/15/17
Guide to parents on a problem that is very common in children with autism
Source: Autism Speaks
The child includes:
- Very very hard and dense stool.
- Pain and difficulty in emptying the bowels.
- The child has a bowel movement three times a week or less.
Talk to your child's doctor to find out if your child is constipated.
What causes constipation in children with autism?
1. Holding a stool
Some children try to hold a stool and ignore the urge to have a bowel movement. This can happen for various reasons, for example:
- Fear of the toilet.
- Reluctance to use the toilet outside the home.
- Unwillingness to interrupt the game.
- Fear of pain during bowel movements.
2. Toilet training
Children may resist and hold stool when toilet training is attempted. This can become a habit that is difficult to break later on.
3. Nutrition problems
- Lack of fiber found in fruits, vegetables and whole grains.
- Dairy products, if the child is allergic to cow's milk or consumes too much dairy products.
- Insufficient intake of water and other beverages, especially when ill.
- Changes in appetite or diet due to illness of the child.
4. Stress and changes in daily routine.
Travel, weather changes, and stress can all affect bowel function.
5. Medications
Some medications, such as antacids, antidepressants, and some attention-deficit/hyperactivity disorder medications, can cause stools that are too hard.
6. Associated medical problems.
Constipation is common in children who have movement problems, including decreased muscle tone and cerebral palsy. Also, constipation is possible in case of hypersensitivity to gluten or casein.
Acute constipation and encopresis
Acute constipation
Some (but not all) children with chronic constipation may have this problem. Acute constipation can be caused by too much hard stool in the colon. As a result, the child cannot have a bowel movement for several days. Acute constipation is diagnosed by a doctor by palpation of the abdomen or by X-ray. Acute constipation is often accompanied by loss of appetite and lethargy. After a bowel movement, the child feels better and the symptoms decrease.
Encoprese
This problem occurs in some (but not all) constipated children. Encopresis means that during constipation, the child has loose stools. This is a common problem.
Encopresis can develop if a child holds a stool for so long that it becomes difficult for him to have a bowel movement. The stool becomes larger and drier. Due to the retention of large stools, the intestinal muscles get tired and relax. After the muscles relax, loose stools can seep into the underwear.
The child does not feel that this is happening and cannot control loose stools. This usually happens several times a day, causing the underwear to become dirty. Sometimes encopresis is confused with diarrhea, but the child does not actually have diarrhea because most of the stool in the intestines remains solid.
Many children with encopresis experience loss of appetite and decreased interest in daily activities. After a bowel movement, the child feels better and these symptoms decrease.
Treatment of constipation
There are three main approaches to the treatment of constipation.
Talk to your child's doctor about which type of treatment is best for you:
1. Dietary changes
Dietary changes
- Increasing the amount of fiber in your diet will make bowel movements easier.
- Increasing fluid intake , especially water and juice, helps soften stools and reduces the chance of constipation.
2. Behavioral changes
- Regular exercise . Physical activity improves the functioning of the abdominal muscles, which facilitates bowel movements. Regular exercise, including walking, jumping rope, ball games, cycling and swimming, can help with constipation.
- Bowel training in the toilet . It is important that the child knows how to use the toilet at the first urge. The best way to teach this is through planned and extended "sit-downs" where the child is rewarded for simply sitting on the toilet for extended periods of time.
3. Medications
Children often need medication to have regular bowel movements. These can be:
These can be:
- Preparations for daily use.
- Single-dose preparations that "cleanse" the intestines in case of severe difficulty with emptying.
Increasing fiber in the child's diet
A diet high in fiber promotes regular bowel movements and prevents constipation. Fiber is a substance that the body cannot digest. There are two types of fiber - soluble and insoluble. Soluble fiber promotes the entry of water into the intestines. Insoluble fiber facilitates the passage of stool through the intestines. Both types of fiber are needed to prevent constipation.
Fiber is an important part of a healthy diet. A lot of fiber is found in foods such as fruits, vegetables, whole grains, legumes, nuts, and seeds. They also contain a lot of protein, vitamins and minerals. A diet high in these foods is the best way to get enough fiber.
Where to find fiber
When shopping for food, you can check the nutritional information of the product, including the fiber level. Good choices are foods that contain at least 2 grams of fiber per serving.
Good choices are foods that contain at least 2 grams of fiber per serving.
When shopping, look for products that contain whole grains, whole grain flour, and oatmeal. Perhaps there are options for your child's favorite foods with whole grains, that is, higher fiber content. For example, whole-grain cheese crackers, whole-grain wheat flour bread, and high-fiber cereals may be suitable for you.
Recommended Fiber Intakes
- Ages 1 to 3: 19 grams per day (for boys and girls).
- Ages 4 to 8: 25 grams per day (for boys and girls).
- Ages 9 to 13: 31 grams per day for boys and 26 grams per day for girls.
Examples of high fiber foods
- White beans: 9.5 grams per 1/2 cup.
- Oatmeal: 8.8 grams per 1/2 cup.
- Red beans: 8.2 grams per 1/2 cup.
- Beans: 7.5 grams per 1/2 cup.
- Pear (with skin): 4.3 grams per small pear.
- Raspberries: 4.0 grams per 1/2 cup.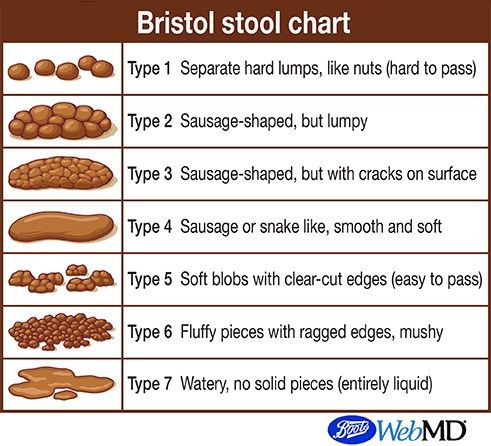
- Baked potatoes (with skin): 3.8 grams per piece.
- Almonds: 3.3 grams per 30 grams.
- Apple (with skin): 3.3 grams per piece.
- Banana: 3.1 grams for one medium-sized piece.
- Orange: 3.1 grams per medium sized piece.
- Peanut butter: 3.0 grams per 2 tablespoons.
- Broccoli: 2.8 grams per 1/2 cup.
- Green peas: 2.5 grams per 1/2 cup.
- Avocado: 2.3 grams per 1/2 cup.
- Corn: 1.6 grams per 1/2 cup.
- Strawberries: 1.5 grams per 1/2 cup.
- Wild rice: 1.5 grams per 1/2 cup.
- Raisins: 1.4 grams per 1/2 cup.
- Popcorn: 1.2 grams per 1 cup.
Increasing fiber and fluids in the child's diet
It is advisable to offer children foods rich in fiber from an early age so that their use becomes a lifelong habit.
If your child is currently constipated, it is important to increase fiber levels very gradually over 2-3 weeks. Increasing too much fiber in the diet may worsen constipation or cause gas, abdominal pain and diarrhea.
Increasing too much fiber in the diet may worsen constipation or cause gas, abdominal pain and diarrhea.
Increasing fiber will only be effective if the child also starts drinking more fluids. Make sure your child not only starts eating more fiber, but also starts drinking more water and juice.
How to Increase Fiber Without Child Resistance
Children with autism often resist change, especially dietary changes. Parents need to be patient and try different approaches, for example:
- Switch to crackers and whole grain pasta.
- Try whole grain bread and pizza. Many types of whole-grain bread do not differ in appearance from ordinary white bread.
- Offer your child whole grain muesli or popcorn as a snack.
— Offer the child dried fruit as a sweet treat (prunes, dried apricots, raisins).
- Try to make cocktails from frozen fruits or berries based on juice or milk.
- Offer your child carrot, bell pepper, or celery sticks that can be dipped in peanut butter, hummus, or salad dressing.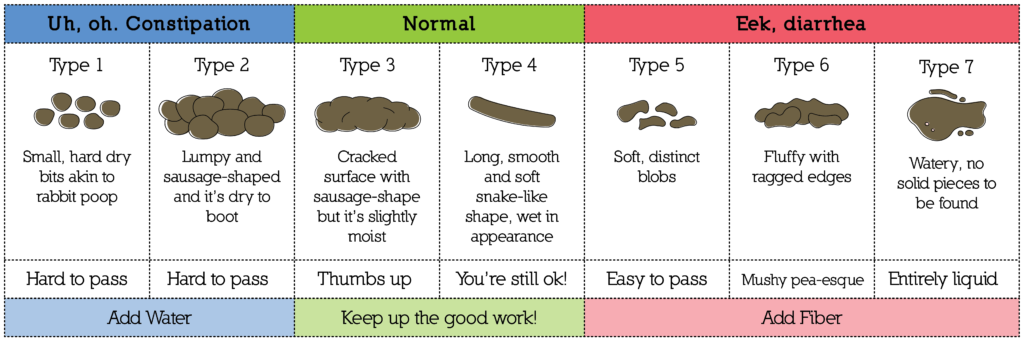
— Add shredded vegetables or mashed vegetables to your child's favorite foods, such as pasta or pizza.
- Make funny faces or figures out of slices of fruits and vegetables.
- Invite the child to dip fruit slices in nut butter or his favorite kind of yogurt.
- Bake cookies, muffins or pies with whole wheat flour.
Increasing fluid intake
Sufficient water is essential for maintaining a healthy body. It is found in both foods and drinks. As you increase the amount of fiber in your diet, you also need to increase your fluid intake.
How much liquid do you need?
- Follow your thirst. The amount of water a child needs varies depending on physical activity and what the child eats. Therefore, it is very important to monitor the signs of thirst in a child.
- When a child drinks enough water, his urine becomes clear, light yellow in color. Dark, tea-colored urine usually means your child needs to drink more.
Fluid types
1. Water: the best source of fluid.
2. 100% juice: good for health, but should be limited.
- 120-180 ml per day for children under 6 years old
- 240-360 ml per day for children over 6 years old
- Some juices (pear, apple, plum) contain sugars that act as a natural laxative and may help with constipation.
3. Milk:
- An important part of a child's nutrition.
— Excessive consumption of milk can lead to constipation.
- Desirable rate for milk: 480-720 ml per day (2-3 cups).
4. Sports drinks and drinks with electrolytes:
- They often have added sugar.
- Not the best choice for children.
- Check with your doctor before giving these drinks to your child.
5. Fruit drinks, soft drinks:
- They usually have added sugar.
- Not the best choice for children.
- It is better to save them for special occasions, such as holidays, you should not give them to the child regularly.
Fluids and constipation
It is very important to increase fluid intake at the same time as increasing fiber. Fluid helps soften stools and make bowel movements easier.
- Some juices (pear, apple, plum) are natural laxatives.
— It is advisable to give the child a lot to drink between meals, this contributes to regular bowel movements.
- Drinks with a lot of sugar, caffeine or "fortified with vitamins" can increase constipation.
Tips for increasing fluid intake
— Encourage your child to drink water between meals, on a full stomach the child may drink too little.
- Offer your child fruits with a high water content, such as grapes, oranges, or watermelon, as snacks and treats.
— Keep a bottle or cup of water handy so your child can always have a drink. Add some citrus juice to your water to make it taste better. Or try adding some other drink to the water.
- Lead by example.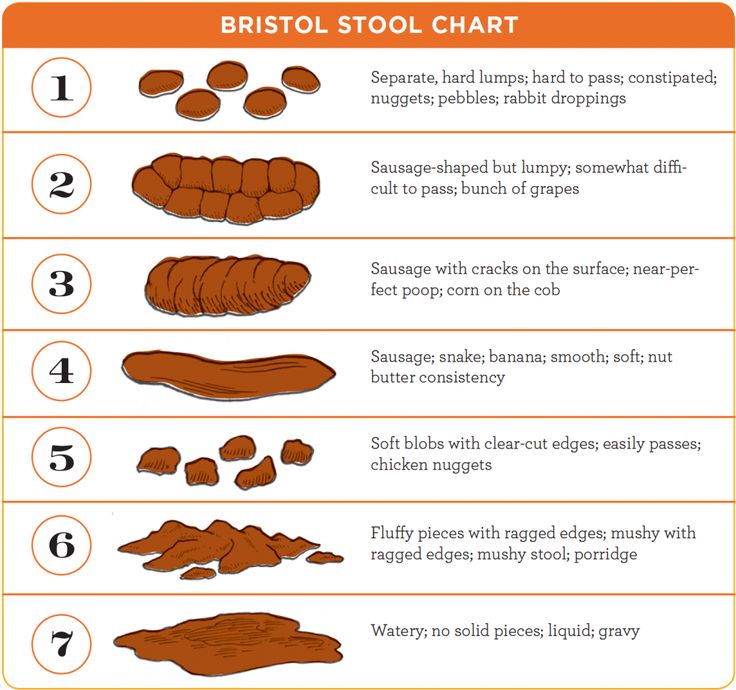 Children are more likely to drink water when they see their parents or siblings drinking water.
Children are more likely to drink water when they see their parents or siblings drinking water.
Toilet training
In case of constipation, it is very important to teach the child to use the toilet as soon as he feels the first urge. The easiest way to teach this is with a daily period of time when the child sits on the toilet for a long time. When a child gets used to sitting on the toilet for a long time, it will be easier for him to relax the muscles that hold the stool. With daily toilet seating time, your child will become less likely to hold a stool. When the child stops holding the stool, the intestines return to normal size and become more sensitive.
How to teach your child to sit on the toilet for a long time every day
1. Be patient with yourself and with your child. Learning a new skill, especially this skill, is never easy.
2. Start by teaching your child to sit on the toilet, even if he does not defecate:
- Start with 1-2 minutes.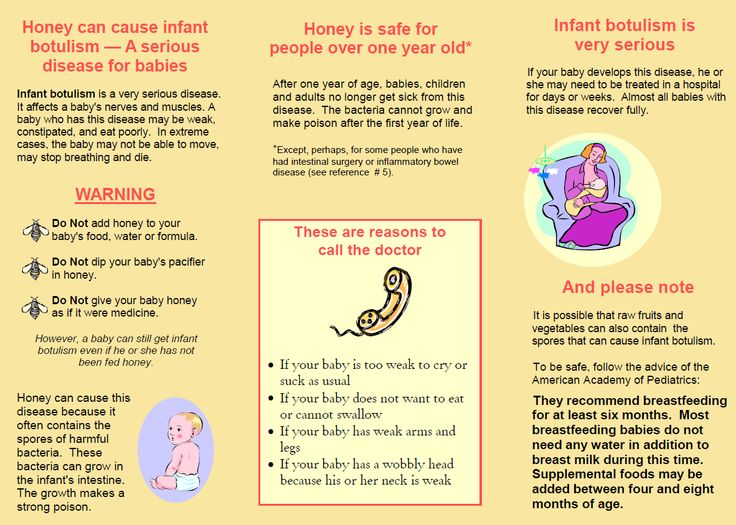 Very slowly increase the time to 10-12 minutes.
Very slowly increase the time to 10-12 minutes.
- Use a visual timer to let your child know how long to sit.
- Offer the child some quiet activity while he sits on the toilet. For example, reading a book, drawing, playing a handheld computer game, listening to music or audio books.
- Try to save the child's favorite pastime for sitting on the toilet and do not offer it at other times.
- Praise your child even for small progress.
- Never force a child to sit on the toilet and never force him to sit on it unless you are working with a behavior specialist to help you do it safely.
3. Choose a time for your child to use the toilet.
- Making toilet use a regular part of a child's daily routine will help develop a normal bowel habit.
— Children with autism often like routine. Making toilet seating a part of the daily routine will reduce the risk of child resistance.
- Try using a visual timetable with pictures, one of the items being toilet time.
— If your child is most likely to have a bowel movement at some time of the day, try to schedule toilet seating for that time.
— Morning is the best time for most people, but it may not be suitable for a child who will be rushed to kindergarten or school in the morning.
- For some children, the best time is after coming home from school or kindergarten.
4. Make sure your child is comfortable.
- Choose the toilet seat or potty that is most comfortable for your child.
— Use a child seat for the toilet if the normal seat is too big for the child.
- Use the footrest if the child's feet do not touch the floor.
How to teach a bowel movement in the toilet
1. Make sure your child sits on the toilet for long periods 1-2 times each day.
2. Teach your child that "poop goes down the toilet" by emptying dirty diapers or underwear.
3. Try to time your child to sit on the toilet when you think your child is most likely to have a stool.
4. Try to stimulate the gastrocolic reflex before sitting on the toilet. This reflex occurs after eating or drinking and allows the bowel muscles to expel stool after eating. To stimulate this reflex, try to get your child to eat or snack, and drink a warm drink before sitting on the toilet.
5. Watch for possible signs in the child's behavior. If you notice that he wants to use the toilet, then take him there. Signs may include:
- Changes in facial expressions.
- Attempts to go to a quiet part of the house.
- Muscular tension.
Positive reinforcement
- Start with rewards for your child just sitting on the toilet.
- When the child begins to empty his bowels on the toilet, start rewarding him for it.
- Small rewards that the child receives immediately after the desired behavior work best.
- Give rewards less frequently over time.
Try not to use food as a reward. Instead, you can reward your child with:
- Sing your favorite song with your child.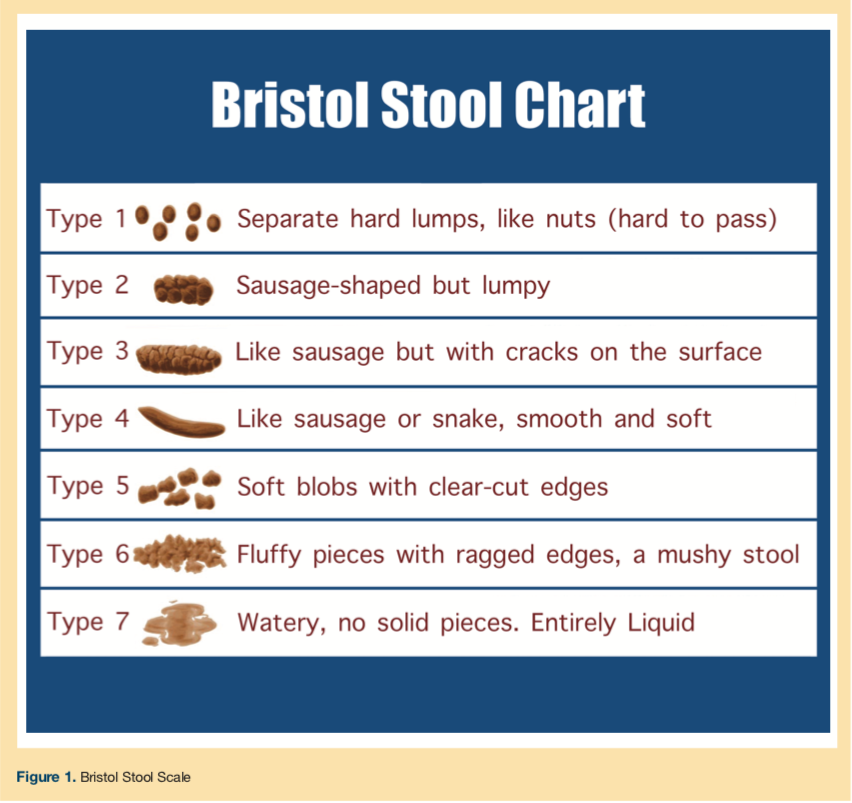
- Hugs, tickling, verbal praise.
- Favorite game with a child.
- Stickers that will allow the child to track their progress.
- Time for your favorite pastime.
- Tokens (in the form of stickers, stars or other items) that can then be exchanged for very large rewards, such as a trip to the cinema or to the park.
Many children with autism have special interests. They can be used when planning rewards. For example, if a child is interested in cars, then as a reward, he can look at car magazines. If a child loves trains, then he can receive stickers with trains as a reward.
Positive rewards lead to the desired changes in behavior much faster than any punishment or criticism.
If the child is dirty
- Say something like "I noticed that you are dirty" or "Please change."
- Help the child to do this as needed.
— Do not scold the child or draw attention to what has happened.
If the child does not want to sit on the toilet
- Try to get the child as close to the toilet as possible when he begins to have a bowel movement. If the child does it in diapers while standing, then try to have him do it while standing in the toilet.
If the child does it in diapers while standing, then try to have him do it while standing in the toilet.
- When the child has defecated in the diaper, throw the contents of the diaper down the toilet in front of the child.
- Teach your child to sit on the toilet with their clothes down. Give your child a toy that can keep him busy for a while.
- Over time, move on to having the child sit on the toilet with the lid up but wearing a diaper.
- When the baby is comfortable sitting on the toilet with the lid up, cut a hole in the diaper and enlarge it over time. Try to have the child sit on the toilet in a diaper while having a bowel movement.
Specialist help
Very often it is difficult for a family to change what happens at home. Toilet training can be a very complex behavioral problem. Some families need additional specialist support. Signs that the family needs more help include:
- The child becomes very upset when taken to the toilet.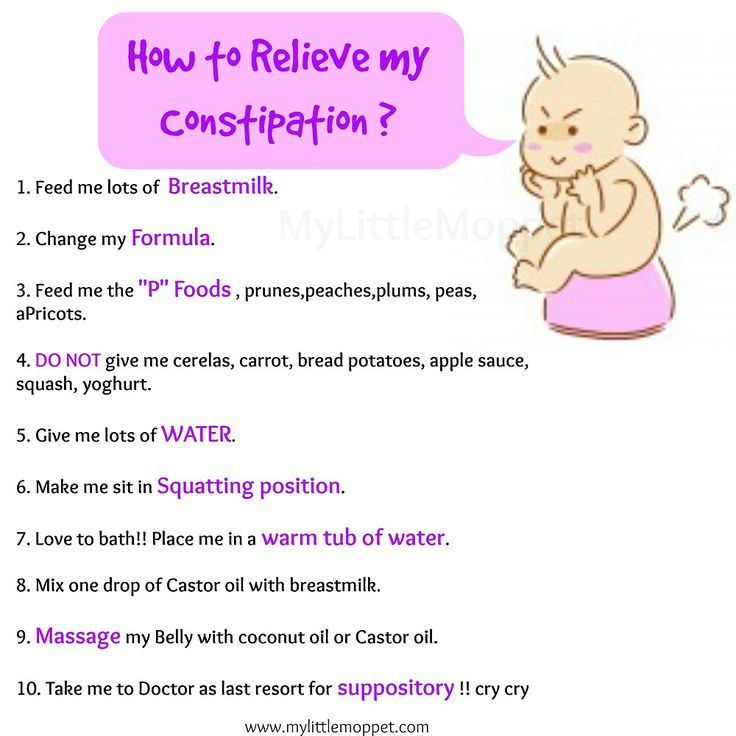
- Child holds stool longer and longer.
— Constipation progresses in the child.
— Everything connected with the toilet causes tantrums or aggression in the child.
Specialists may include child psychologist, behavioral analyst, pediatrician. Sometimes staff at the child care facility that the child attends can help find the right specialist.
Daily preparations
— May be started immediately if the child does not have acute constipation.
- Taken orally.
- Most effective when taken daily.
Purpose of taking the drug:
- Soft stools and bowel movements every day.
- All stool comes out of the bowels.
Dosage of the drug:
- The initial dose of the drug must be prescribed by a doctor. Sometimes the dosage needs to be varied. Talk to your doctor about this, he will help you change the dosage.
When it is necessary to increase the dosage of the drug:
- Small and hard stools.
- The child does not have a bowel movement every day.
- The child has difficulty emptying the bowels or is in pain.
When to reduce the dosage of the drug:
- Loose stools.
— The child has abdominal pain or cramps.
Duration of drug treatment
— As a rule, the course of treatment lasts at least 6 months.
— After 6 months of daily bowel movements, the doctor may decide to gradually reduce the dosage of the drug.
- If you stop taking the drug before the intestines return to normal, then constipation will begin again.
— It is important to make sure that the child has soft stools every day.
How do drugs to treat constipation work?
There are three types of laxatives. They act differently.
1. Osmotic laxatives. They carry water into the stool to keep it soft. Safe and often given to children. Usually taken every day. Suitable for long term use.
Examples: polyethylene glycol without electrolytes, magnesium hydroxide, magnesium citrate, lactulose, sorbitol.
2. Stimulant laxatives. They promote contractions of the intestinal muscles and promote stool in the intestines. As a rule, they are prescribed for a single dose.
Examples: senna, bisacodyl.
3. Lubricating laxatives. Facilitate the passage of stool through the intestines with an oil base.
Examples: paraffin oil, glycerin suppositories.
Acute constipation medicines
Acute constipation occurs when large masses of hard stool block the intestines. If the doctor thinks that there is a blockage in the intestines, then as a first treatment option, he may prescribe a drug that will "cleanse" the intestines.
Your doctor will work with you to determine the best type of drug. Sometimes drugs that are taken by mouth are best. Sometimes drugs that are injected into the intestines are better suited. This "clearing" usually takes 2-3 days. It is best to spend it on the weekend or on vacation. The child will need to spend 2-3 days near the toilet and use it often.
Sometimes drugs that are injected into the intestines are better suited. This "clearing" usually takes 2-3 days. It is best to spend it on the weekend or on vacation. The child will need to spend 2-3 days near the toilet and use it often.
These drugs can only be prescribed by a doctor. He will tell you how long and how often to take the drug.
Enema procedure
Most cases of constipation in children are treated with drugs taken by mouth. In some cases, children need a drug that is injected into the rectum. Talk to your doctor about what treatment is best for your child. Do not give your child an enema without talking to the doctor first. Below is information about giving an enema, if needed.
How to prepare a child for an enema
- Explain the procedure to the child in a way that they can understand, perhaps with illustrations.
- Let the child look at and touch the enema bottle.
- Touch the tip of the enema to his hand so he knows what it's like.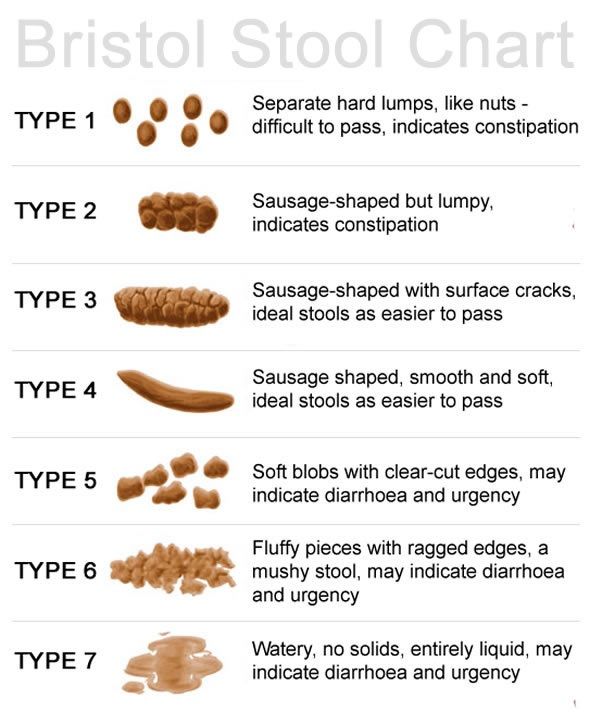
- Help your child practice beforehand how to lie down properly during an enema.
Enema Preparation
— Read the instructions for the enema very carefully. Check out the pictures and instructions in the instructions.
- Make sure the enema is at room temperature.
- Prepare everything you need: an enema bottle; towel on which the child will lie; pillows; music, a favorite toy, or other items to help your child stay calm; wet cleansing wipes.
Decide where you will give the enema. Sometimes it's best to put the baby on a blanket or large towel on the bathroom floor next to the toilet.
- Place towels and/or pillows for your child to lie down comfortably.
- Have another person stand at eye level with the child during the procedure - read to him, sing, talk, play music or otherwise distract him and help him lie still.
How to give an enema
1. Wash your hands.
2. Remove the protective cap from the enema tip. The tip should have a lubricant that makes it easier to administer the enema.
The tip should have a lubricant that makes it easier to administer the enema.
3. Help the child lie on his left side with his knees pressed against his chest.
4. Have your helper talk or sing to your child in an effort to soothe and encourage.
5. Hold the enema in one hand. With your other hand, spread your buttocks until you see the anus.
5. Insert the end of the bottle very carefully into the anus. Don't force it in.
6. Position the end of the enema towards the child's back. The contents of the enema should fall on the intestinal wall, and not on the stool.
7. Squeeze the enema until nearly the entire volume has been delivered.
8. If possible, try to have the child lie down for 15-20 minutes. You can hold on to his buttocks to prevent him from pushing out the contents of the enema too soon.
9. If your child wears diapers, put on a diaper.
10. If the child uses the toilet, then put him on the toilet after 15-20 minutes.