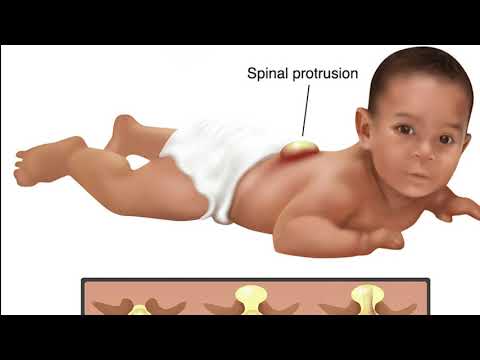
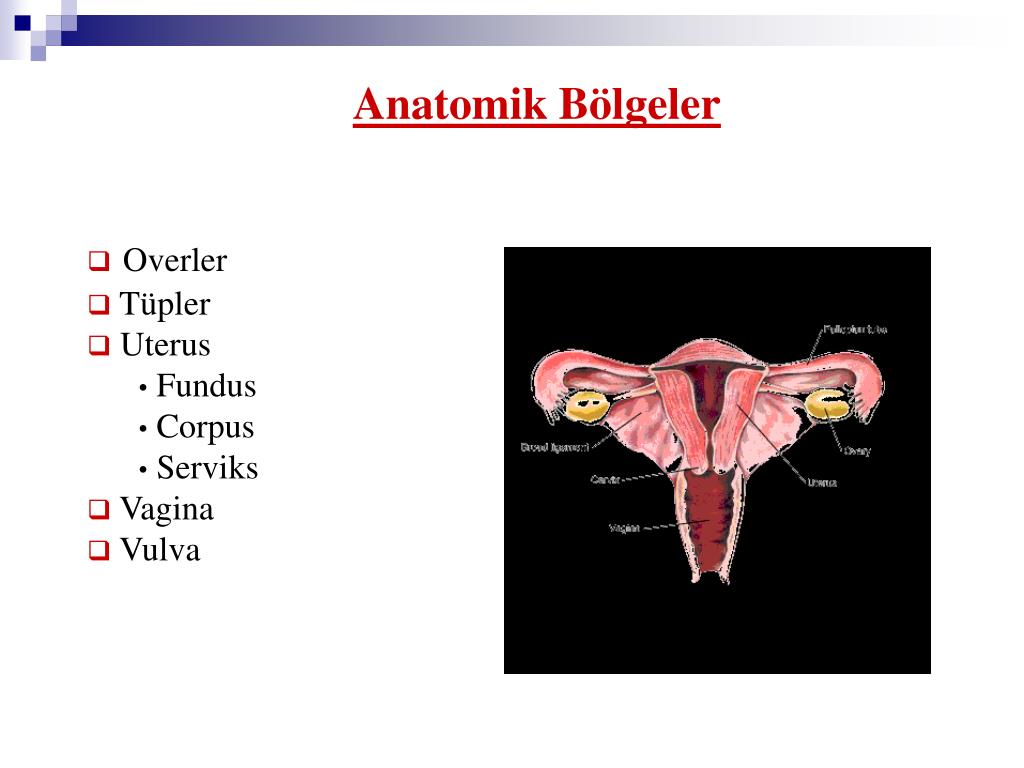
What is the fundus of uterus
fallopian tube | Anatomy & Function
uterus
See all media
- Key People:
- Gabriel Fallopius
- Related Topics:
- Rubin’s test isthmus of the fallopian tube ampulla tubae uterinae fimbria of the fallopian tube infundibulum
See all related content →
fallopian tube, also called oviduct or uterine tube, either of a pair of long narrow ducts located in the human female abdominal cavity that transport male sperm cells to the egg, provide a suitable environment for fertilization, and transport the egg from the ovary, where it is produced, to the central channel (lumen) of the uterus.
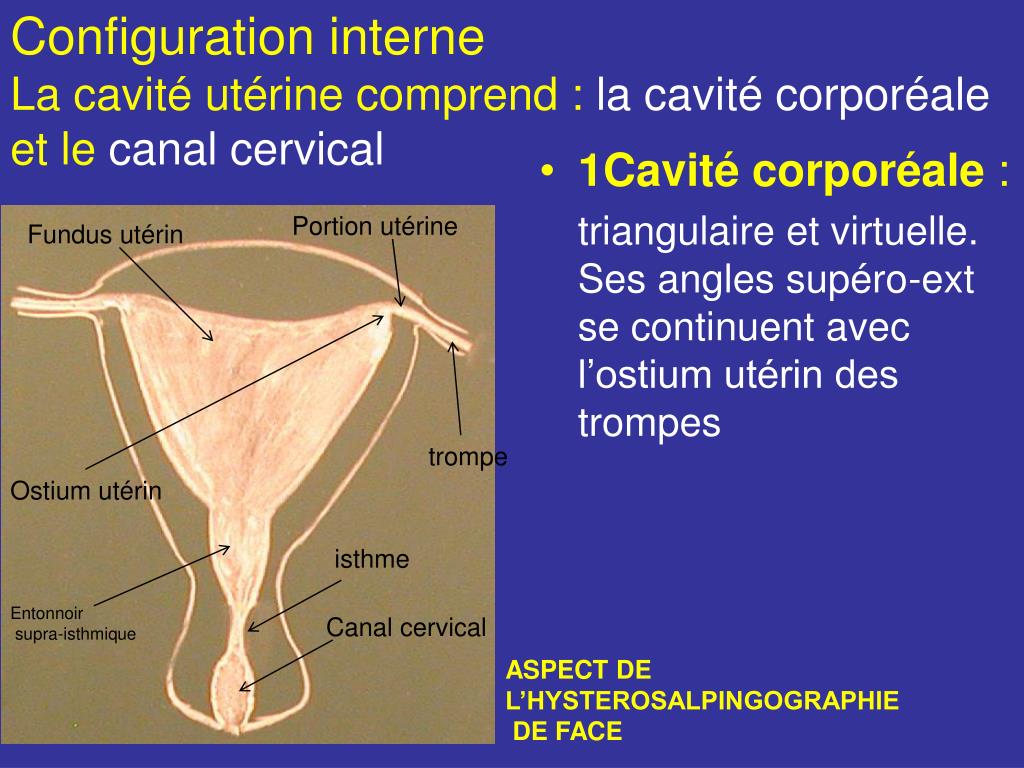
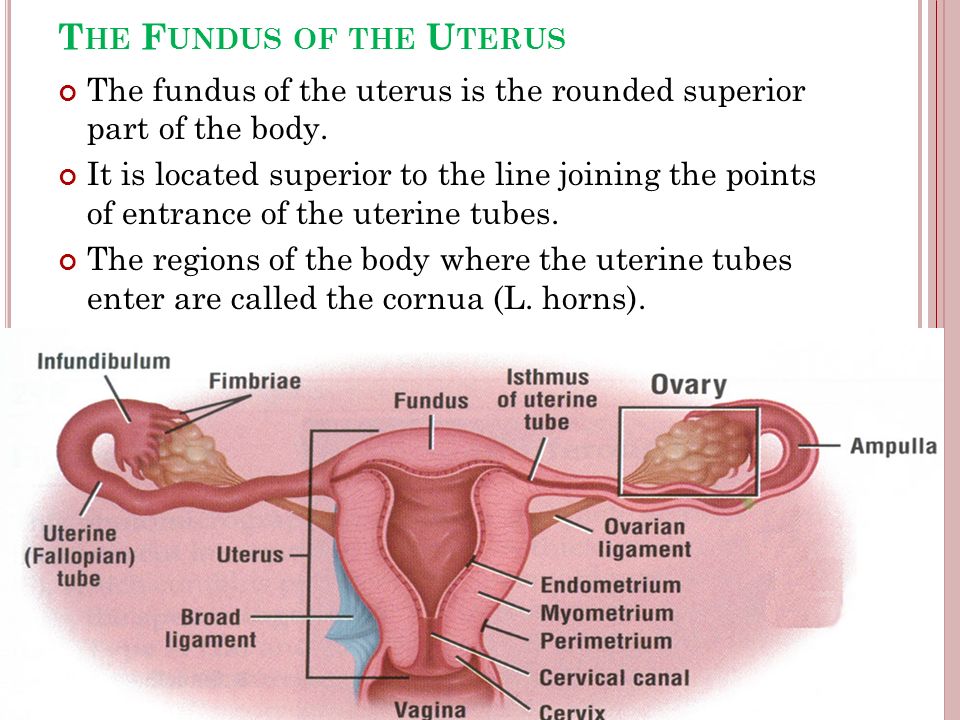
Each fallopian tube is 10–13 cm (4–5 inches) long and 0.5–1.2 cm (0.2–0.6 inch) in diameter. The channel of the tube is lined with a layer of mucous membrane that has many folds and papillae—small cone-shaped projections of tissue. Over the mucous membrane are three layers of muscle tissue; the innermost layer has spirally arranged fibres, the middle layer has circular fibres, and the outermost sheath has longitudinal fibres that end in many fingerlike branches (fimbriae) near the ovaries, forming a funnel-shaped depository called the infundibulum. The infundibulum catches and channels the released eggs; it is the wide distal (outermost) portion of each fallopian tube. The endings of the fimbriae extend over the ovary; they contract close to the ovary’s surface during ovulation in order to guide the free egg. Leading from the infundibulum is the long central portion of the fallopian tube called the ampulla. The isthmus is a small region, only about 2 cm (0.8 inch) long, that connects the ampulla and infundibulum to the uterus. The final region of the fallopian tube, known as the intramural, or uterine, part, is located in the top portion (fundus) of the uterus; it is a narrow tube continuous with the isthmus, and it leads through the thick uterine wall to the uterine cavity, where fertilized eggs normally attach and develop.
 The channel of the intramural duct is the narrowest part of the fallopian tube.
The channel of the intramural duct is the narrowest part of the fallopian tube.
Britannica Quiz
Human Body: Fact or Fiction?
How deep is your body of knowledge about the inner workings of humans? Test it with this quiz.
The mucous membrane lining the fallopian tube gives off secretions that help to transport the sperm and the egg and to keep them alive. The major constituents of the fluid are calcium, sodium, chloride, glucose (a sugar), proteins, bicarbonates, and lactic acid. The bicarbonates and lactic acid are vital to the sperm’s use of oxygen, and they also help the egg to develop once it is fertilized. Glucose is a nutrient for the egg and sperm, whereas the rest of the chemicals provide an appropriate environment for fertilization to occur.
Besides the cells that secrete fluids, the mucous membrane contains cells that have fine hairlike structures called cilia; the cilia help to move the egg and sperm through the fallopian tubes. Sperm deposited in the female reproductive tract usually reach the infundibulum within a few hours.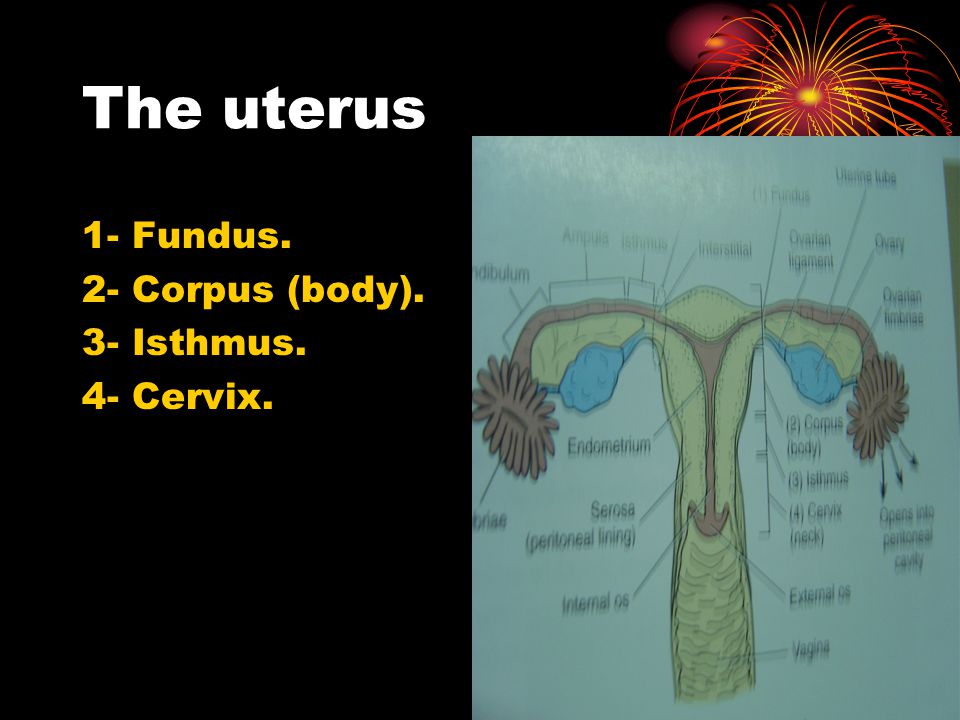 The egg, whether fertilized or not, takes three to four days to reach the uterine cavity. The swaying motions of the cilia and the rhythmic muscular contractions (peristaltic waves) of the fallopian tube’s wall work together while moving the egg or sperm.
The egg, whether fertilized or not, takes three to four days to reach the uterine cavity. The swaying motions of the cilia and the rhythmic muscular contractions (peristaltic waves) of the fallopian tube’s wall work together while moving the egg or sperm.
Abnormalities of or damage to the fallopian tubes can affect a woman’s fertility. If the tubes are blocked or damaged, for example, sperm are unable to reach the egg, or the fertilized egg may be prevented from traveling to the uterus. Abnormalities in fallopian tube anatomy and function have various causes, including pelvic infection (e.g., pelvic inflammatory disease), endometriosis, and congenital defects.
The Editors of Encyclopaedia Britannica This article was most recently revised and updated by Kara Rogers.
What is the Uterine Fundus?
Reviewed by
Dr.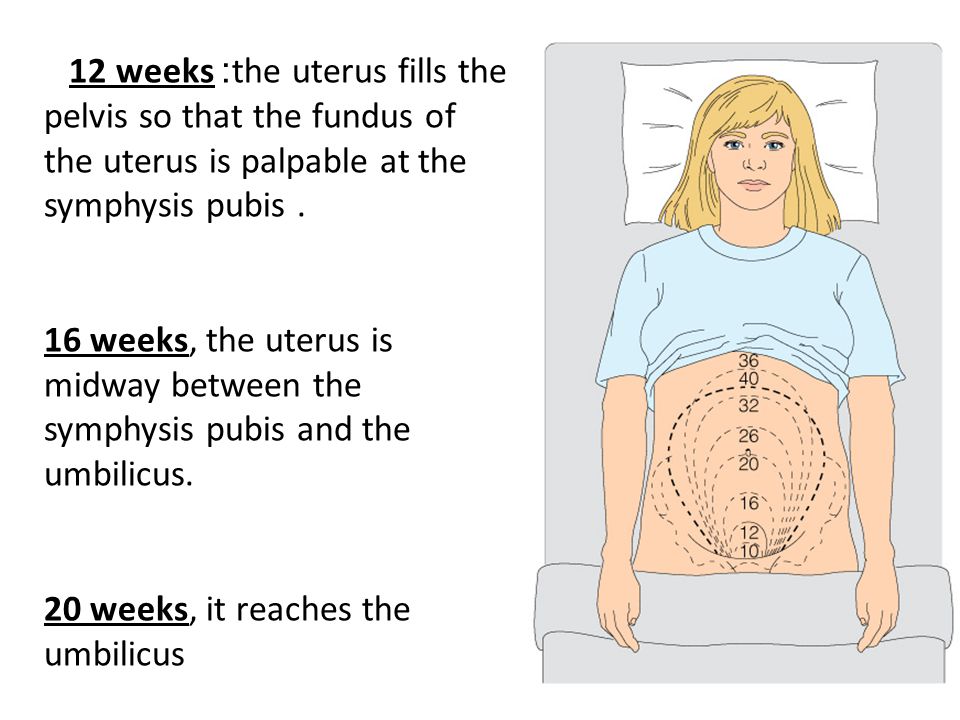 Huma Rasheed, MBBS
Huma Rasheed, MBBS| Last updated: April 28, 2020
What Does Uterine Fundus Mean?
The uterine fundus is the dome-shaped uppermost, rounded part of the uterus. The shape and competency of the uterine fundus are assessed when a woman is unable to conceive because uterine fibroids can interfere with the implantation of the embryo within the uterus.
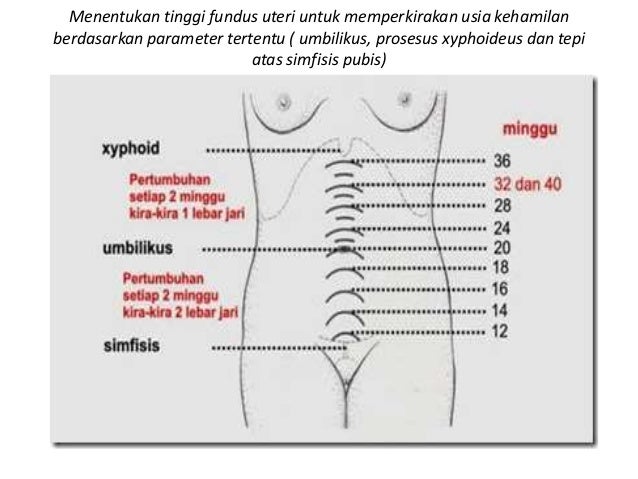
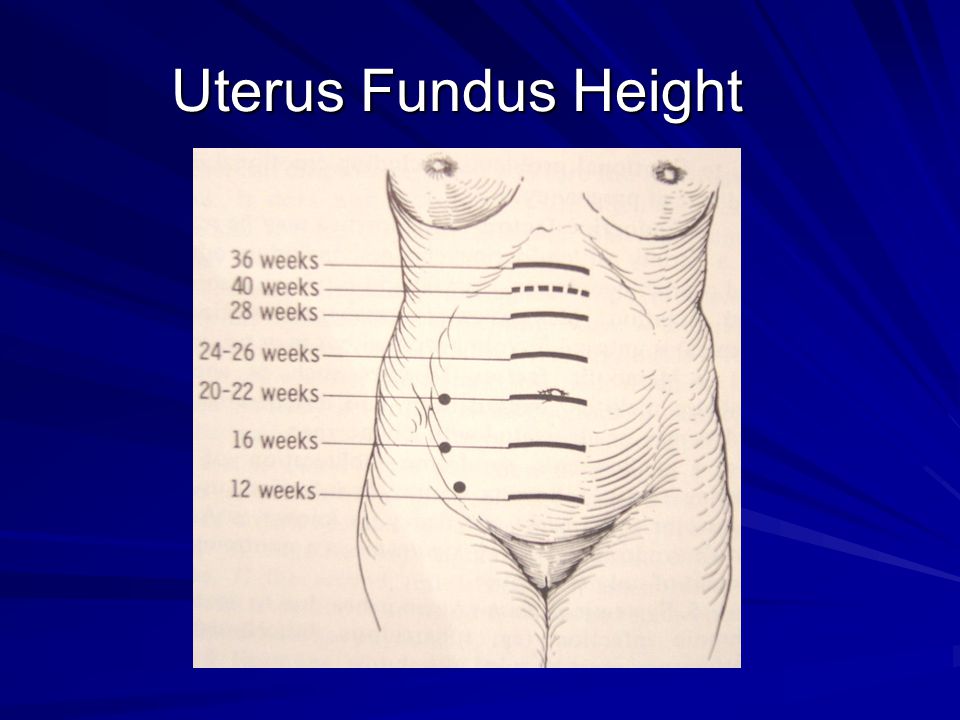
The fundal height is also used to determine the progression of pregnancy.
FertilitySmarts Explains Uterine Fundus
The uterine fundus is important for the following reasons:
Fibroids
The fundas can become occupied by uterine tumors called fibroids that develop from the muscular layer of the uterine wall.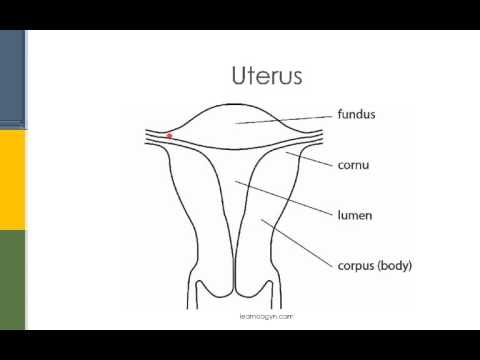 Massive tumors cause the uterine fundus to enlarge, displacing it from its normal position.
Massive tumors cause the uterine fundus to enlarge, displacing it from its normal position.
Fundal Height
Fundal height is used to estimate fetal growth and development during pregnancy. It is measured by placing a measuring tape or fingers between the top of the woman's uterus to the top of the joint of the pubic bone. It is typically recorded on every prenatal visit. The fundal height loses its accuracy as the pregnancy approaches term. A shorter or longer than normal height may indicate issues with the developing fetus.
Shorter height may be due to one of the following reasons:
- Incorrect estimation of the due date of pregnancy as determined by the first day of the last menstrual period (LMP). This can occur when the woman does not remember the first day of the last LMP
- Too little fluid in the amniotic sac (oligohydramnios)
- Fetal descent to the pelvis, which usually occurs two to four weeks prior to delivery
- Restriction of the growth of the fetus while in the uterus
- A small fetus
On the other hand, a larger height may be secondary to one of the following factors:
- Pregnant with twins or multiples
- Error in the calculated due date of pregnancy
- A diabetic mother with a large fetus
- Too much fluid in the amniotic sac (polyhydramnios)
- Birth weight greater than the 90th percentile at birth
- Breech baby
- Abnormal fertilized egg or enlargement of tissue from the placenta as seen in molar pregnancy
Share this Term
Related Terms
- Last Menstrual Period
Term Sources
FertilitySmarts uses high-quality sources to support the facts within our content including peer-reviewed studies, academic
research institutions, professional organizations, and governmental organizations.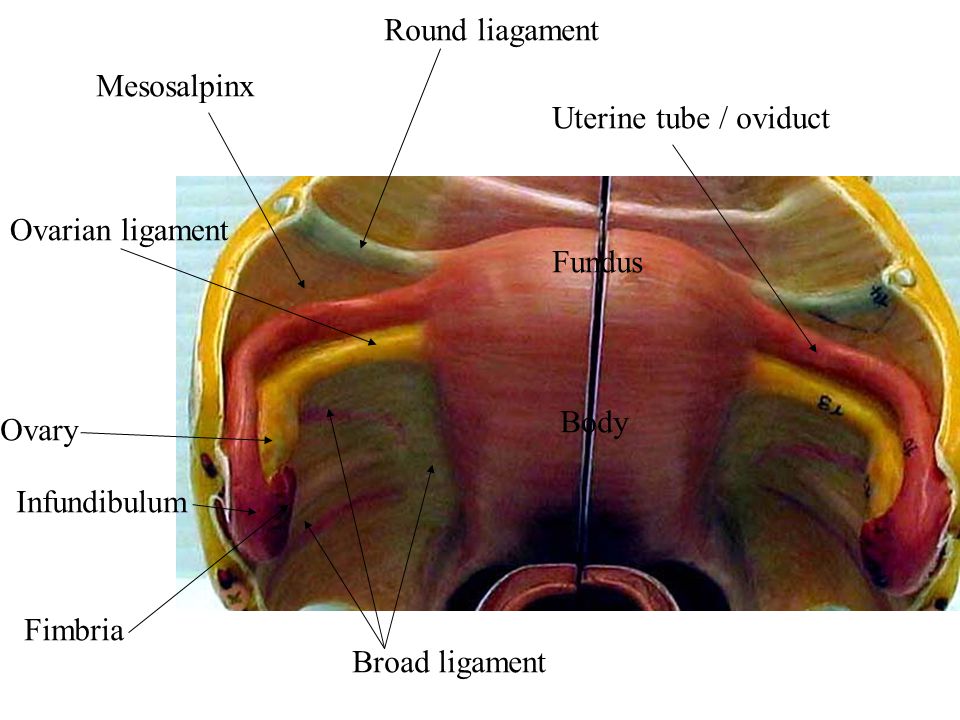
-
McKnight K.
Evaluation of Infertility, Ovulation Induction and Assisted Reproduction.
(2016).
https://www.ncbi.nlm.nih.gov/books/NBK279018/
-
Tobah YB.
What's the significance of a fundal height measurement?.
(2020).
https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-answers/fundal-height/faq-20057962
Related Reading
- Understanding Polycystic Ovary Syndrome
- Implantation Bleeding
- 14 Onesies that Celebrate IVF Babies
- IVF Pregnancy Announcements
- Fertility Podcasts
- Relatable Words After a Miscarriage
Tags
Uterine IssuesPregnancyHealthFemale Reproductive SystemUterusFibroids and Polyps
Trending Articles
Treatment
From Eggs to Blastocysts: Understanding IVF Attrition
Health
Implantation Calendar: What is Happening During the Two Week Wait?
Treatment
5 Things Your Embryologist Wants You To Know About Your IVF Procedure
Treatment
Embryo and Blastocyst Grading - How Does it Work?
WMD norm by weeks of pregnancy: measurement rules
- What is called the height of the fundus of the uterus (VDM)?
- Why measure WMD by week of pregnancy?
- How are the circumference of the abdomen and UMD related?
- When do they start evaluating WDM?
- Rules for measuring WDM and coolant
- What is the rate of WDM and coolant by weeks of pregnancy?
- Correspondence of WDM and coolant during pregnancy by weeks.
Contents:
During pregnancy, every woman visits an obstetrician-gynecologist regularly. At the reception, complaints, general condition, tests are assessed, as well as a number of indicators are measured that indirectly characterize the baby. In particular, important parameters include: the height of the uterine fundus (VDM), abdominal circumference (AC), fetal heartbeat.
What is called the height of the fundus of the uterus (VDM)?
The uterus is a female organ that becomes a cozy home for the unborn baby. The body of the uterus tapers downward and passes into a rounded part - the cervix, and the upper convex part of the uterus is called the fundus. This whole structure resembles a bag or a ball tied at the bottom, in which the fetus grows and develops.
The location of the bottom is determined by hands through the abdomen. This becomes possible when the pregnant uterus, in which the baby grows, increases in size and occupies not only the pelvic area, but also the abdominal cavity.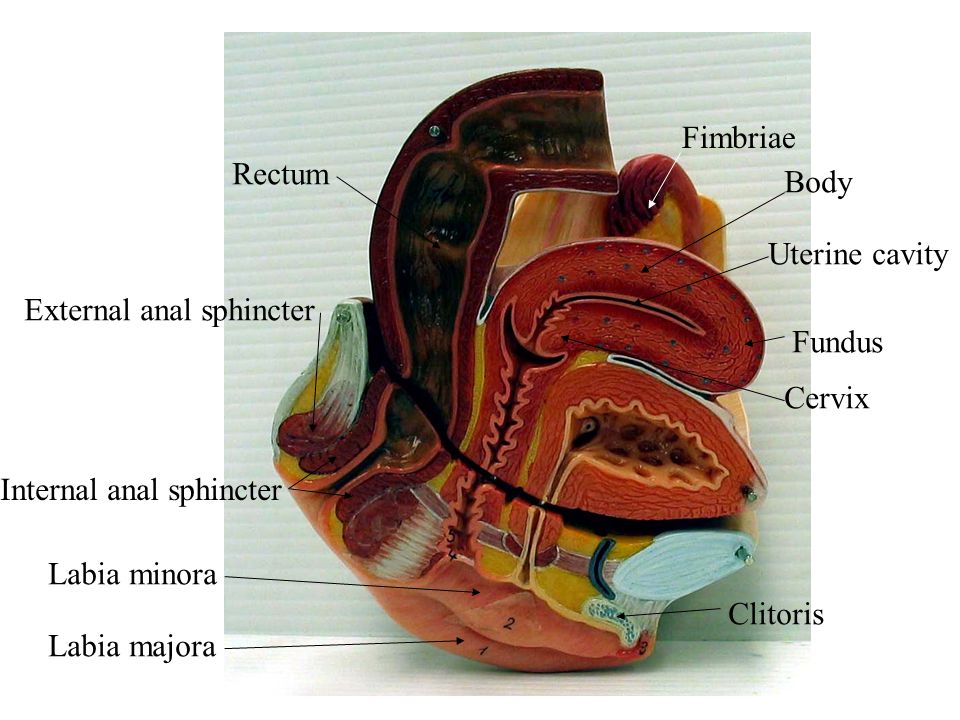
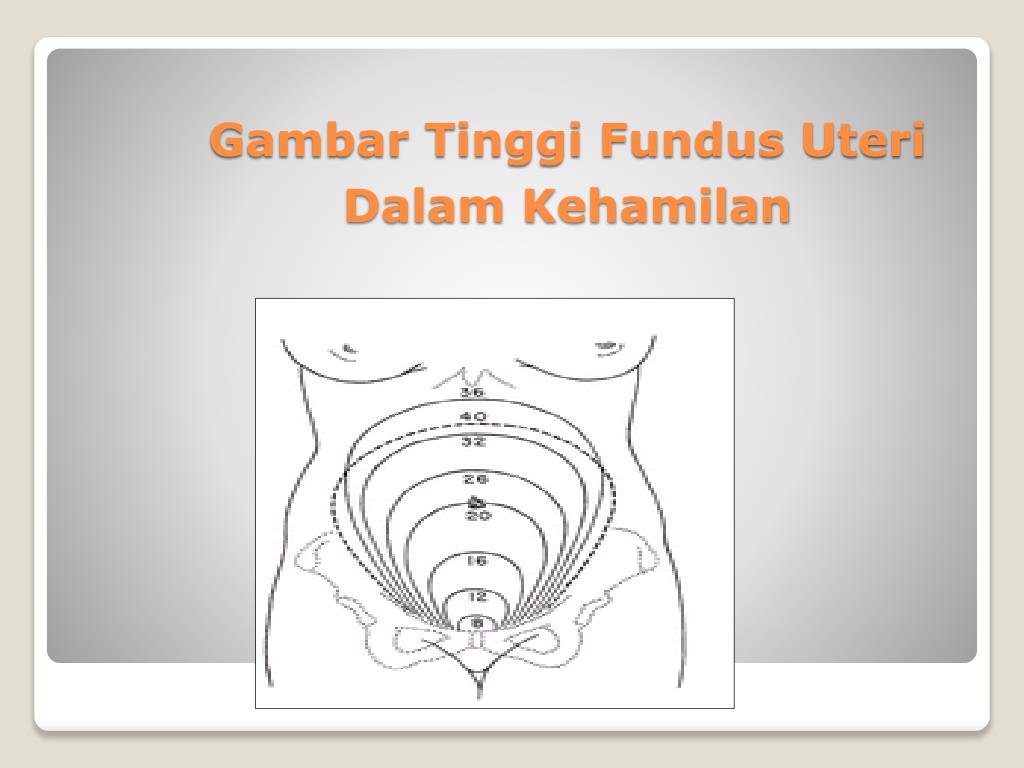
The fundal height (FH) is the distance between the pubic symphysis and the fundus of the uterus, the highest point of the organ.
Why measure WMD by week of pregnancy?
The height of the fundus of the uterus is an indicator by which the doctor may suspect a disturbed course of pregnancy, abnormalities in the development of the fetus, as well as maternal pathology.
At each visit, the obstetrician-gynecologist fills in a summary table of data - a gravidogram, which reflects the dynamics of the course of pregnancy. The measured values, including the height of the uterine fundus, are recorded in the form of graphs. This allows you to visually track the growth and build a WDM curve during pregnancy by weeks.
Fundal height is measured for:
-
determination of compliance with the gestational age;
-
assessment of the term of the baby;
-
calculation of the estimated weight of the fetus.
Thus, using a centimeter tape, the doctor gives a preliminary assessment of the growth and intrauterine development of the fetus, and can also diagnose multiple pregnancies and suggest the presence of complications such as polyhydramnios or oligohydramnios.
How are the circumference of the abdomen and UMD related?
To calculate the estimated fetal weight, in addition to VMD, the doctor will need another important indicator - abdominal circumference or coolant.
Abdominal circumference is measured with a centimeter tape at the level of the navel.
If the indicator exceeds 100, this makes it possible to suspect polyhydramnios, multiple pregnancy, large fetus, incorrect position of the baby.
In order to calculate the estimated weight of the fetus, use the formula:
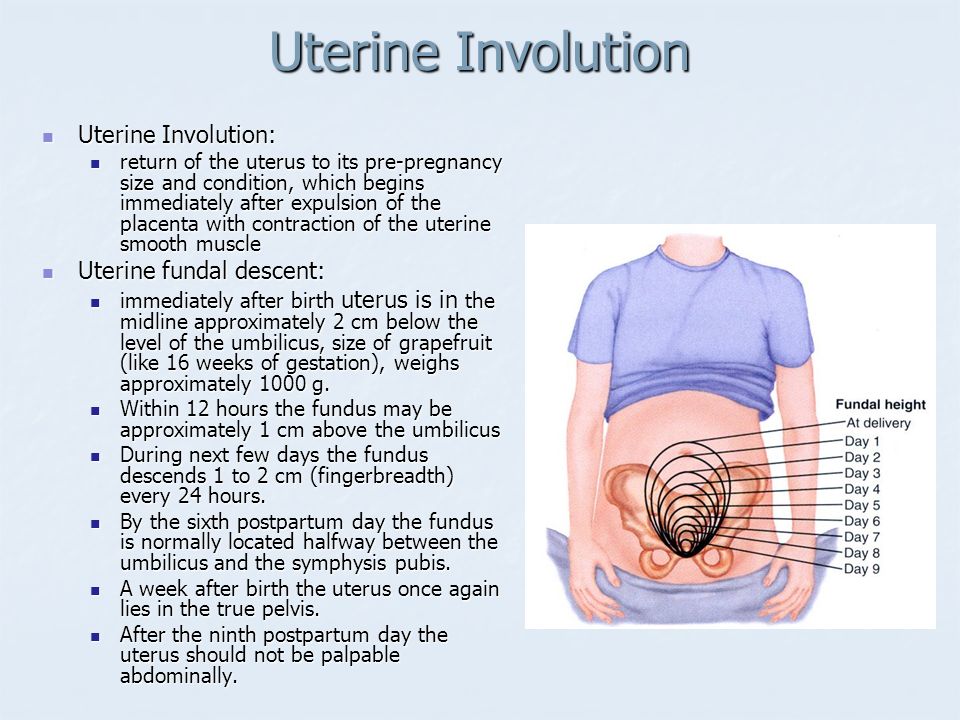
When does WYD begin to be assessed?
In the first trimester of pregnancy, the uterus is completely located in the pelvic cavity.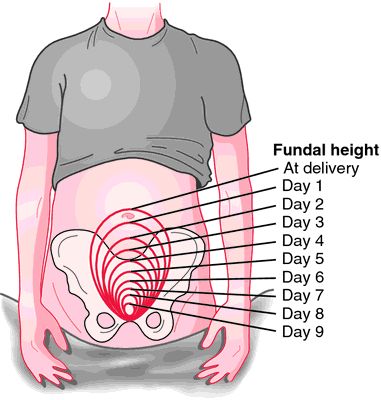 Growth picks up after the 16th week. As a rule, at this time, a rounded tummy becomes noticeable in a woman.
Growth picks up after the 16th week. As a rule, at this time, a rounded tummy becomes noticeable in a woman.
The increase in the size of the uterus at this stage is due not only to the growing fetus, but also to the growth of smooth muscle fibers. It becomes crowded in the small pelvis. The uterus rises, begins to partially occupy the abdominal cavity, and the bottom is selected and begins to support the diaphragm.
According to the clinical guidelines of the Ministry of Health of the Russian Federation 2020 "Normal pregnancy", an obstetrician-gynecologist at each visit of a pregnant woman after 20 weeks is required to measure the VMS and OB. The data is recorded in a gravidogram to track the dynamics. This is how the VDM norms look like by weeks of pregnancy:
The abscissa shows the gestational age, the ordinate shows the values of VMD for these weeks of pregnancy in centimeters. Normal WDM indicators are determined within the limits from 10th to 9th0th percentile.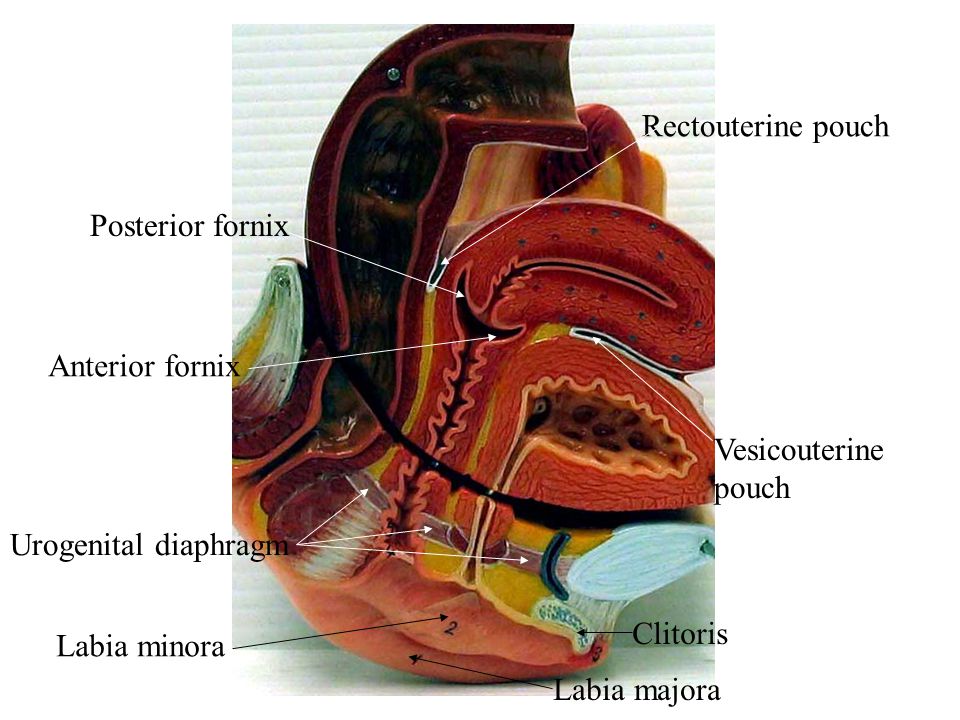
If the gravidogram shows that the graph rises or falls below the designated corridor, this is a reason for additional diagnostic procedures. A pregnant woman needs an assessment of the intrauterine development of the baby, as well as measuring the amount of amniotic fluid using ultrasound.
Particular attention is paid to AMD in the third trimester. If the doctor notes a discrepancy between the values and the gestational age, then it is necessary to exclude late-manifesting malformations of the baby, and also measure the estimated weight to identify a large or underweight fetus. To do this, at the 30-34th week, the patient is also sent for an ultrasound examination.
Rules for measuring WDM and coolant
-
Empty the bladder before measurement.
-
A woman lies on a hard couch on her back, and her legs are slightly bent at the knees.
-
The doctor stands to the left of the pregnant woman and feels her stomach.
-
The beginning of the tape is placed in the middle of the upper edge of the pubic joint and held with one hand.
-
The fundus of the uterus is fixed with the edge of the palm of the second hand.
-
The measuring tape is pulled along the midline of the abdomen to the above point.
-
Measure the distance from the edge of the pubis to the protruding fundus of the uterus.
Conditions for measuring coolant are the same as for WMD by weeks of pregnancy. Anatomical landmarks: the level of the navel is in front, and the upper corner of the sacral rhombus is behind. A centimeter tape is placed at the indicated points on the abdomen and lumbar region, after which the measured value is recorded.
What is the norm of WMD and coolant by weeks of pregnancy?
From the 20th week, when the measurement of the fundal height becomes clinically significant, the numbers conditionally correspond to the gestational age.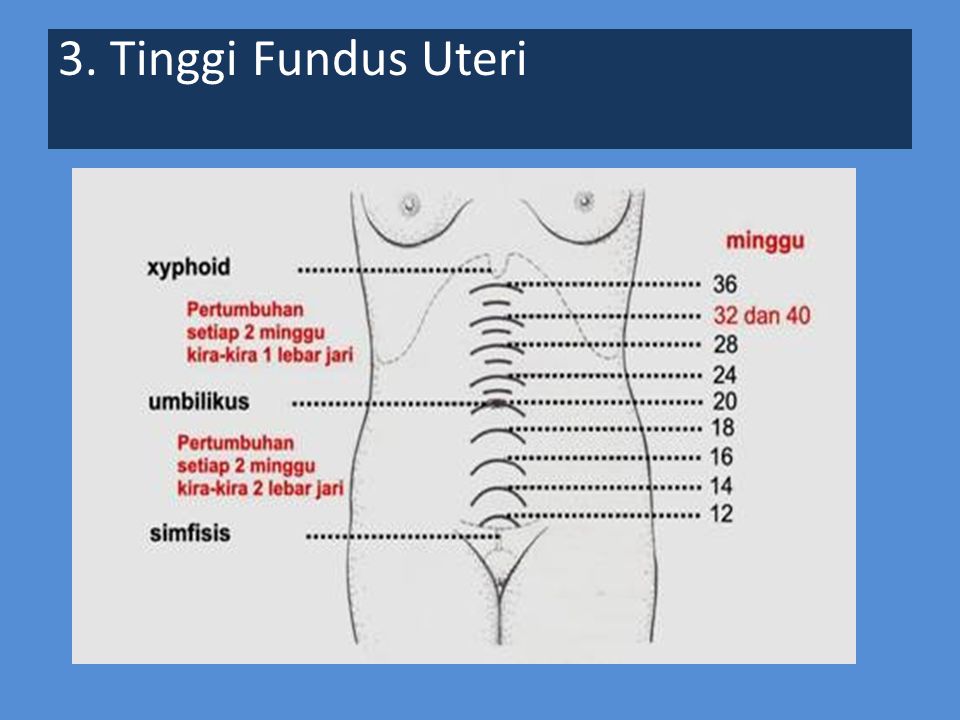 The norms vary within 3-4 centimeters.
The norms vary within 3-4 centimeters.
Compliance with WMD and coolant during pregnancy by weeks.
According to the table, at 36–39 weeks of gestation, AMD is fixed. And by the 40th week it goes down. This is due to physiological processes.
By 36 weeks, the uterus tends to support the diaphragm. It has nowhere to grow further, which means that the maximum peak of WDM is determined. After the 38th week, the fetal head begins to gradually move into the pelvic cavity. The woman notes that the tummy has dropped, and it becomes easier for her to breathe, as the diaphragm gets a little freedom of movement.
The expectant mother should know by what indicators the doctor judges her condition. But deviations from the norm do not always indicate a pathological process. Therefore, it is not worth measuring WDM at home. The assessment of indicators is carried out only by an obstetrician-gynecologist, taking into account such factors as genetics, height, weight, pelvic parameters, number and location of fetuses.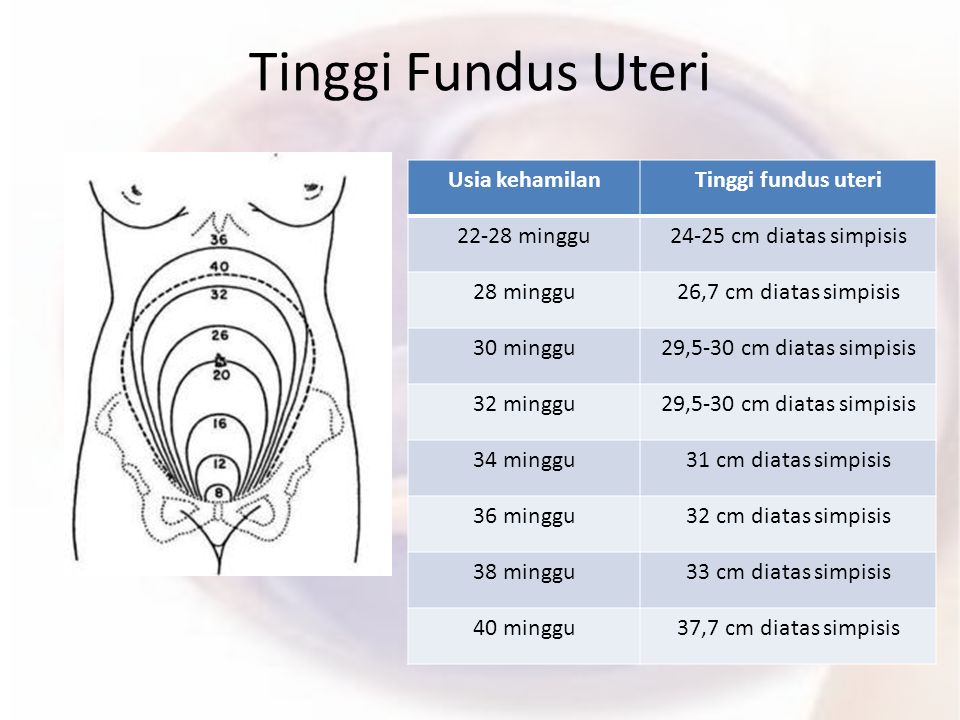
Sources:
-
Clinical recommendations of the Ministry of Health of the Russian Federation "Normal pregnancy", 2020
-
Antenatal Care. Routine care for the Healthy Pregnant Woman. NICE&NCCWCH, RCOG Press 2008.
-
Maruotti GM, Saccone G, Martinelli P. Third trimester ultrasound soft-tissue measurements accurately predicts macrosomia. J Matern Fetal Neonatal Med. 2017 Apr;30(8):972-6.
-
Caradeux J, Martinez-Portilla RJ, Peguero A, Sotiriadis A, Figueras F. Diagnostic performance of third-trimester ultrasound for the prediction of late-onset fetal growth restriction: a systematic review and meta-analysis. Am J Obstet Gynecol. 2019 Jan 8.
-
Obstetrics: national guide / ed. G.M. Savelieva, G.T. Sukhikh, V.N. Serova, V.E. Radzinsky.
 — 2nd ed. — M.: GEOTAR-Media, 2018
— 2nd ed. — M.: GEOTAR-Media, 2018
| Author: pediatrician Ekaterina Koshelnikova |
Fundal pressure during the second stage of labor to improve maternal and fetal outcomes
What is the problem?
The second stage of labor is the period of pushing that begins when the cervix is fully dilated (up to 10 cm) and ends with the birth of the baby. stage. Pressure on the fundus of the uterus by pushing the mother's abdomen toward the birth canal is often used to promote spontaneous vaginal delivery, shorten the duration of the second period, and reduce the need for instrumental delivery (with forceps or vacuum) or caesarean section. This is especially true in conditions of limited resources in which the possibilities of operative delivery are limited or absent.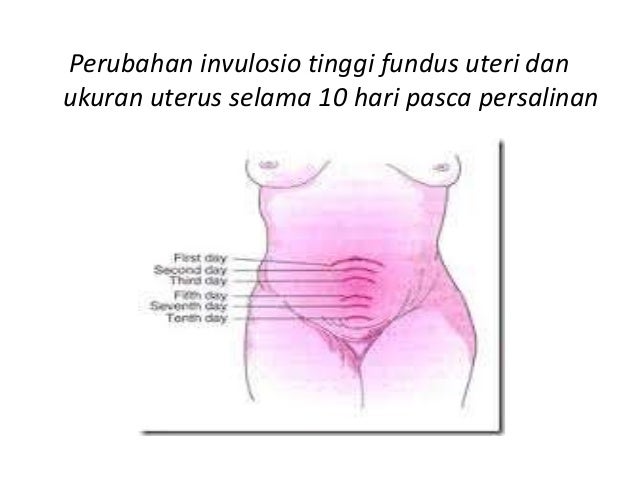 Hand pressure can be applied each time the uterus contracts. Alternatively, an inflatable brace can be used to apply pressure during contractions.
Hand pressure can be applied each time the uterus contracts. Alternatively, an inflatable brace can be used to apply pressure during contractions.
This review aimed to find out if the pressure on the fundus of the uterus during labor during the second stage of labor assists in vaginal delivery and causes any negative consequences for the woman or her unborn child.
Why is this important?
Prolonged labor can sometimes be dangerous for some women and their babies. Sometimes a woman and an unborn child can be emaciated during childbirth. Many areas have trained professionals to assist with vacuum extraction, forceps, or caesarean section. However, other regions often lack these resources and prolonged labor can be life-threatening. The pressure on the fundus of the uterus can promote labor. It can also increase complications for the baby and mother. This topic is not as deeply studied and it is important to know how this method can affect women and their babies.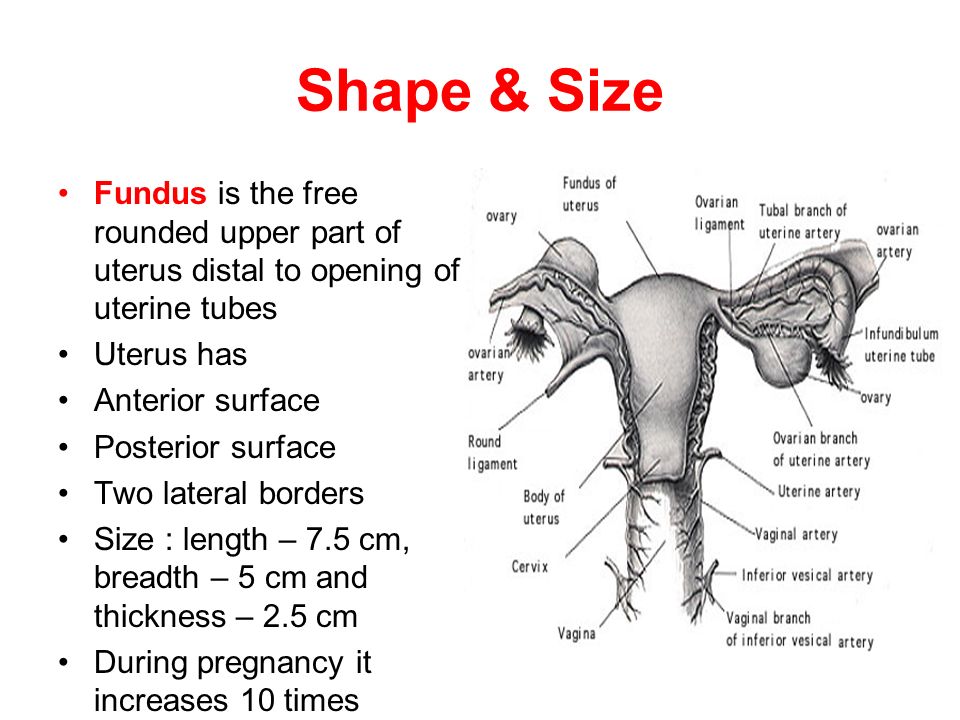
What evidence did we find?
This updated Cochrane review included 9 randomized controlled trials involving 3948 women (search date 30 September 2016). Five studies (involving 3057 women) looked at manual fundus pressure versus no fundus pressure, and four studies (involving 891 women) looked at fundus pressure with an inflatable band.
We found no evidence that manual fundal pressure made a difference in the number of women who gave birth vaginally over time (very low-quality evidence) or who had an instrumental delivery, caesarean section, or vaginal delivery (very low-quality evidence) ). Manual pressure on the fundus of the uterus did not affect the duration of labor (very low-quality evidence). The number of babies who did not deliver well and had low umbilical artery pH or low Apgar scores was the same regardless of whether or not pressure was applied to the mother's fundus (all low-quality evidence). There were no infant deaths in either group.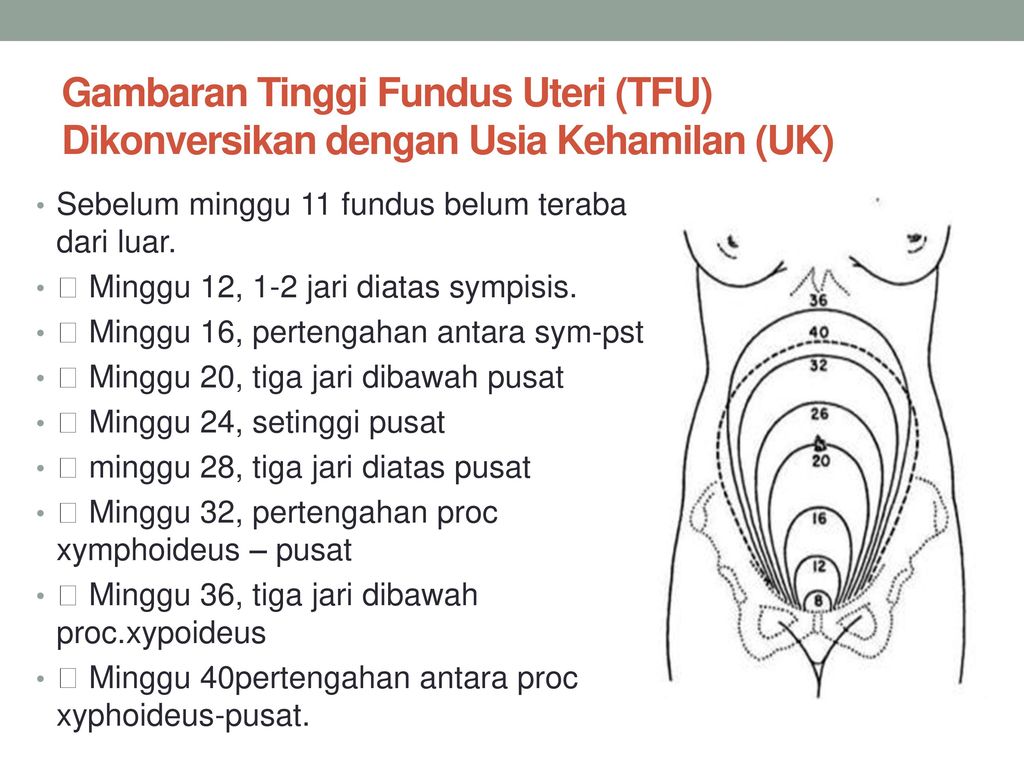 The studies did not report potential serious problems or death in women.
The studies did not report potential serious problems or death in women.
In nulliparous women, fundal pressure with an inflatable band may have resulted in fewer women having an instrumental delivery or a caesarean section (very low-quality evidence), but the evidence was unclear. These women who had an inflatable brace had shorter pushing times than women without an inflatable brace (very low-quality evidence). The inflatable brace made no difference to the number of women who had a caesarean section who delivered babies with low umbilical artery blood pH or a low Apgar score five minutes after birth (very low-quality evidence). None of the studies reported on whether the women gave birth within a certain time frame, the number of babies who died, the potential for serious problems, or the women's deaths. The studies did not use inflatable bandages for women who gave birth again.
What does this mean?
There is insufficient evidence from randomized controlled trials to show whether manual fundal pressure or fundal pressure with an inflatable band are effective ways to reduce labor pressure and prevent operative labor, or whether these methods are safe.