What are congenital disorders
What is a congenital disorder?
What is a congenital disorder? | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is a congenital disorder?
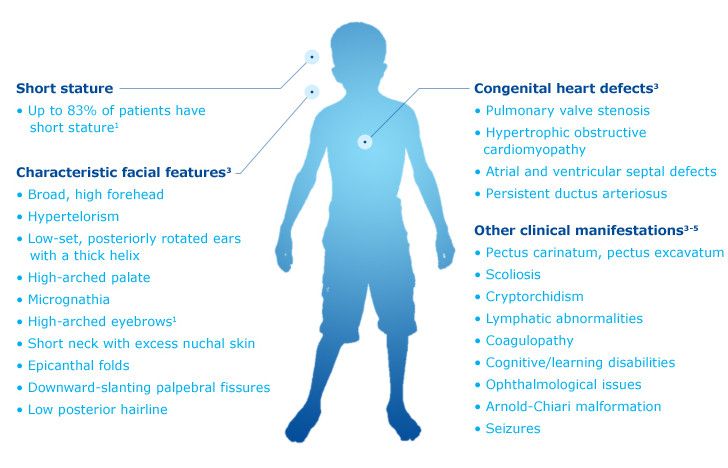
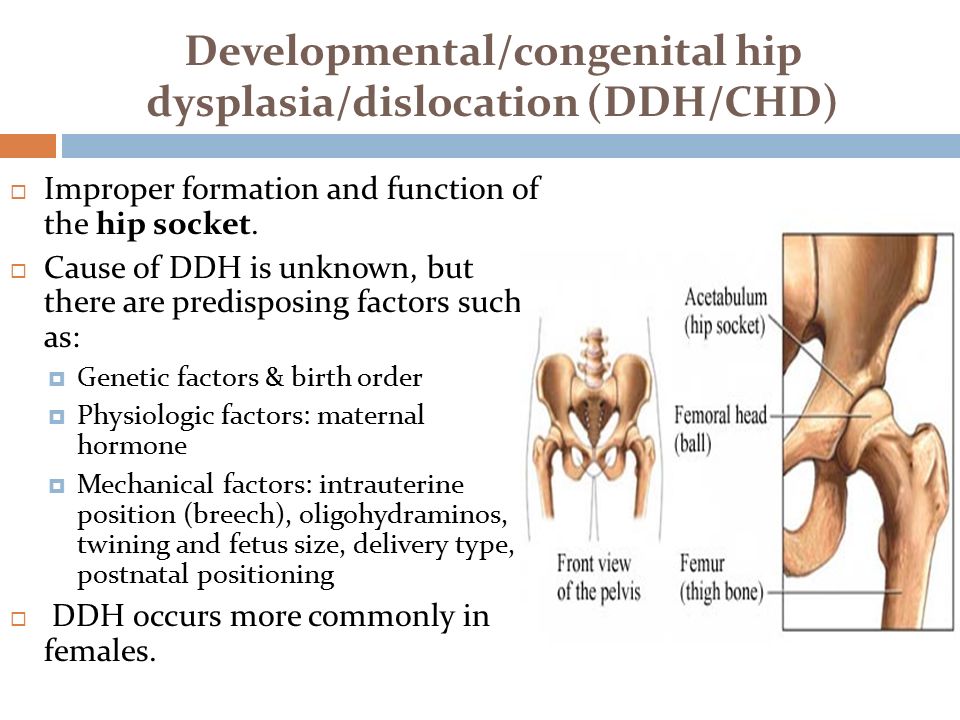
A congenital disorder is a condition that is present from birth. Congenital disorders can be inherited or caused by environmental factors. Their impact on a child’s health and development isn’t always severe, and sometimes it can be quite mild. However, a child with a congenital disorder may experience a disability or health problems throughout life.
It’s natural to be concerned about congenital disorders if you’re pregnant or planning a pregnancy, especially if your family has a history of a particular disorder. It’s possible to test for some, but not all disorders during pregnancy, and there are also things you can do to reduce the chances of your baby being born with a congenital disorder.
What are the most common congenital disorders?
Some common congenital disorders are:
- cleft lip and cleft palate — usually diagnosed during routine scans in pregnancy
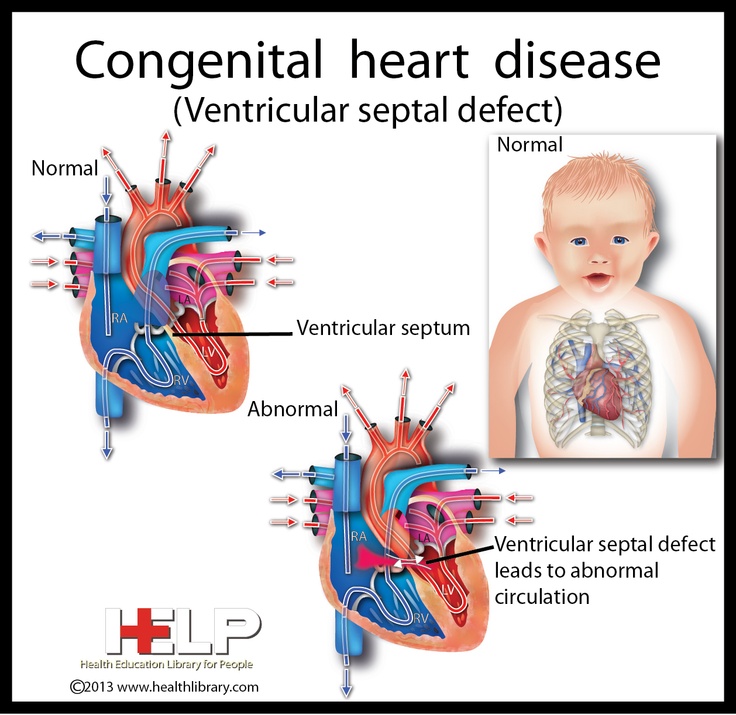
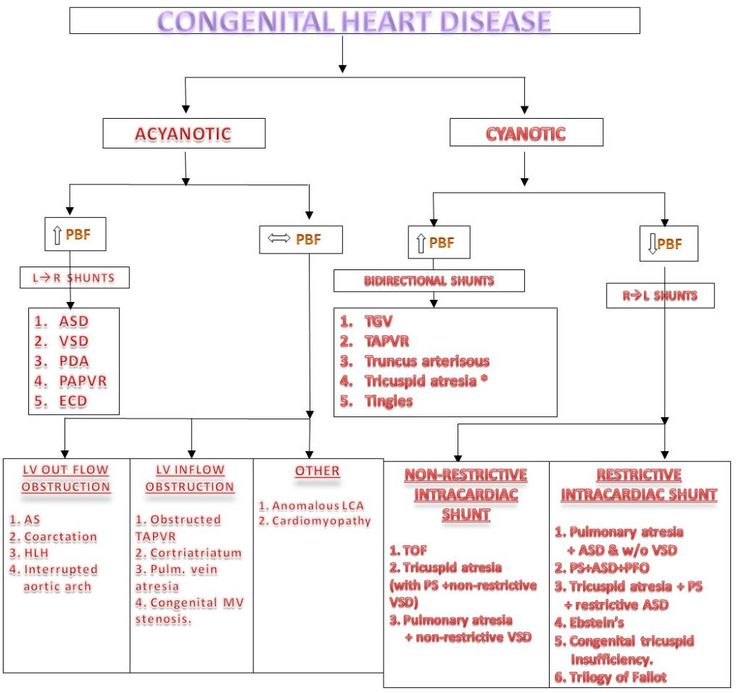
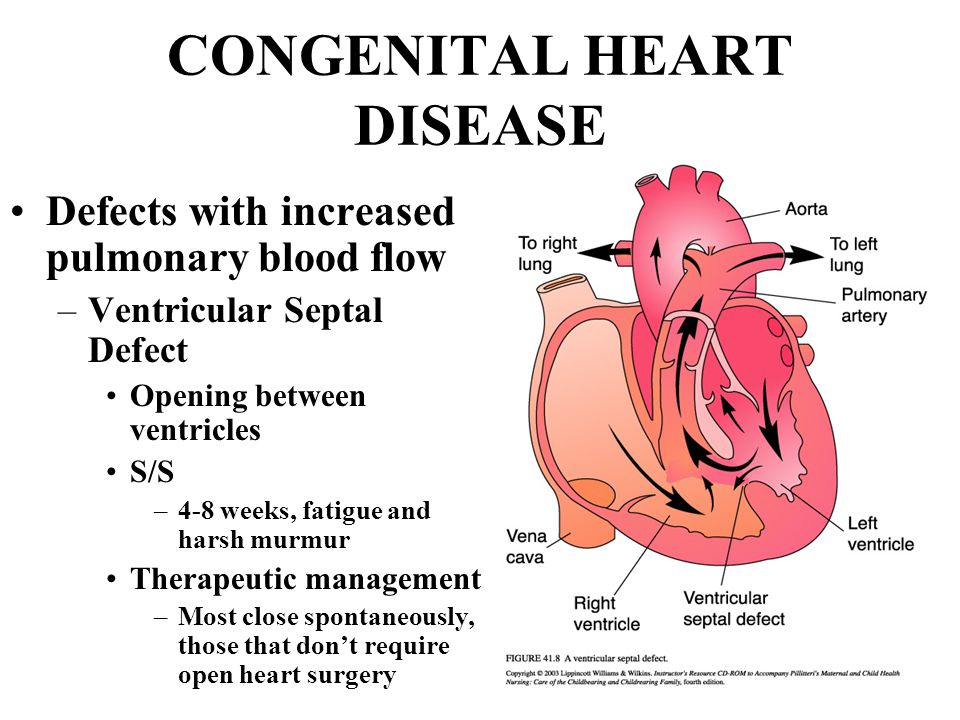
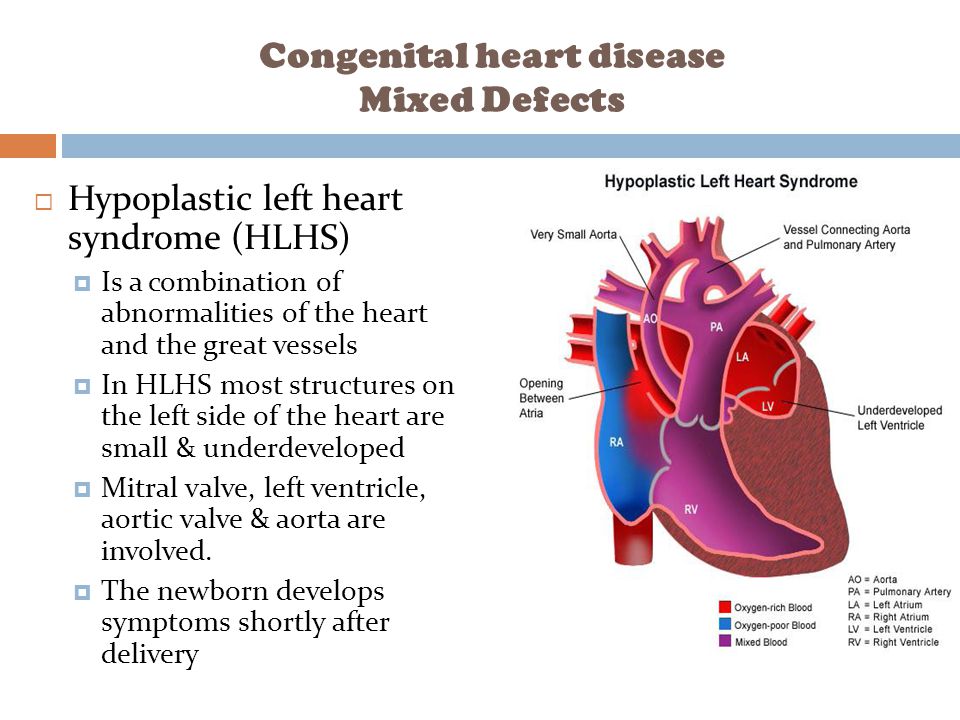
- congenital heart disease — including a hole in the heart, a valve problem or a problem with the blood vessels. These are usually diagnosed during routine scans in pregnancy or during newborn screening.
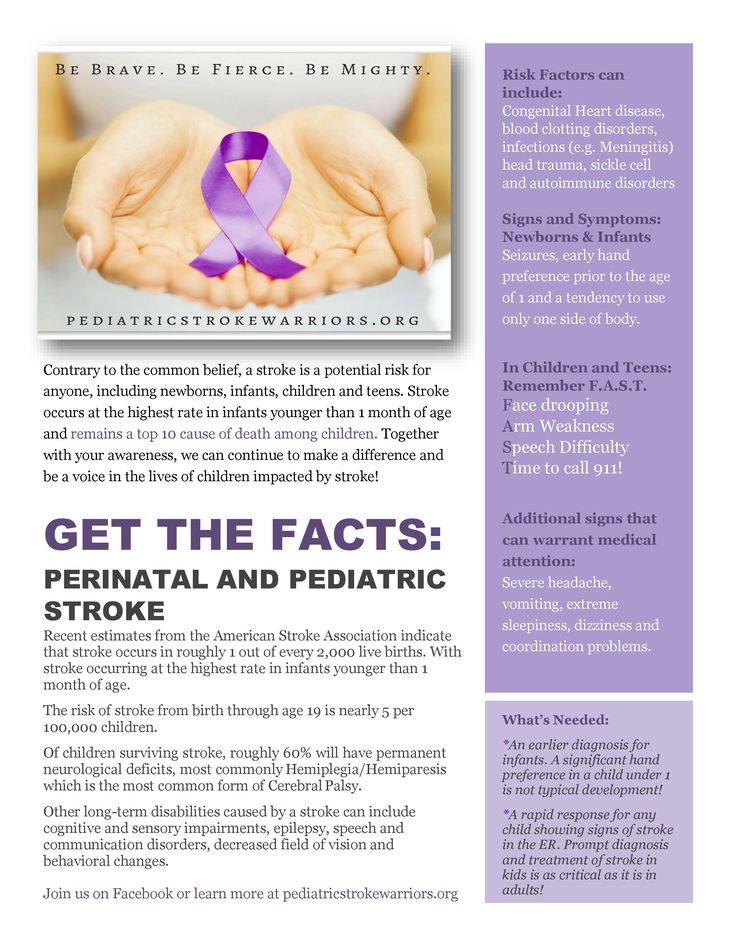
- cerebral palsy — usually diagnosed in the first few years of life
- Fragile X syndrome — may be diagnosed through genetic testing during pregnancy or in the first few years of life
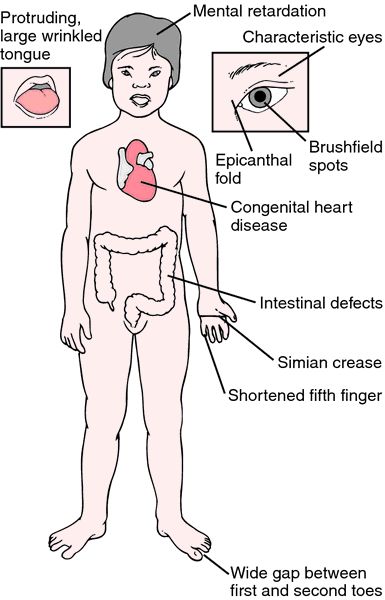
- Down syndrome (Trisomy 21) — usually diagnosed through genetic during pregnancy
- spina bifida — usually diagnosed during routine scans in pregnancy
- cystic fibrosis — usually diagnosed during newborn screening
What tests for congenital disorders are available in pregnancy?
Testing for some congenital disorders, such as Down syndrome, can be performed using a blood test from 10 weeks of pregnancy onwards.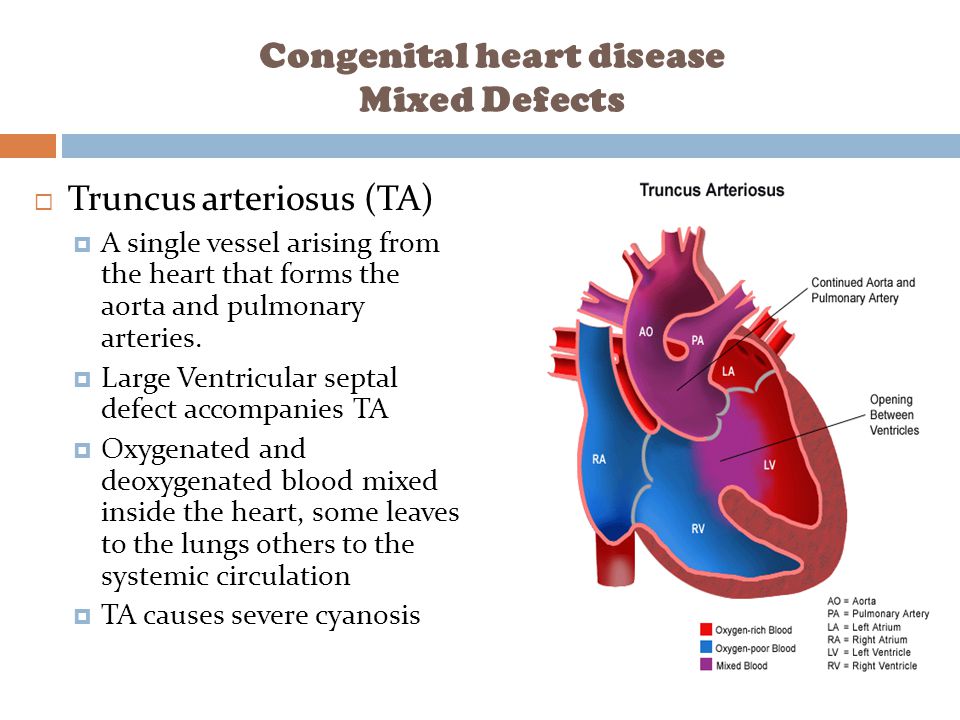 Although many parents choose to have tests during pregnancy, it is not compulsory. Some parents choose not to have tests.
Although many parents choose to have tests during pregnancy, it is not compulsory. Some parents choose not to have tests.
Screening tests are designed to identify babies who may be at increased risk of a congenital disorder. If a screening test does not rule out your baby having a congenital disorder, the next step is to have a diagnostic test.
Diagnostic tests, such as ultrasound scans, blood tests and sometimes urine tests, aim to identify babies who have a congenital disorder and to find out what that disorder is.
However, it is not possible to test for all congenital disorders during pregnancy, and testing is not perfect.
Chorionic villus sampling (CVS)
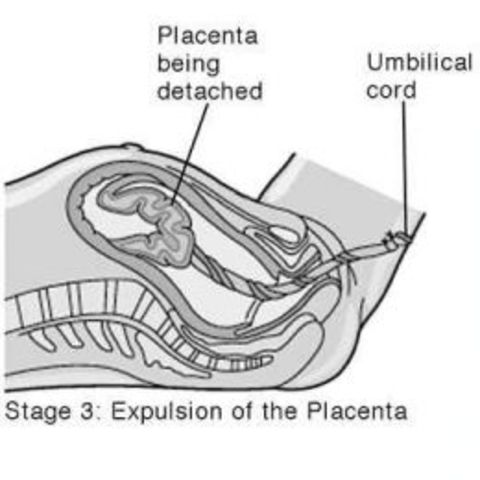
Chorionic villus sampling, or CVS, is usually performed between 10 and 13 weeks of pregnancy if screening tests show your baby may have a congenital disorder. CVS can be used to diagnose babies with Down syndrome or other genetic conditions. You would be given a local anaesthetic and a doctor would use a needle to collect a small sample of cells from your placenta, which is then sent for testing.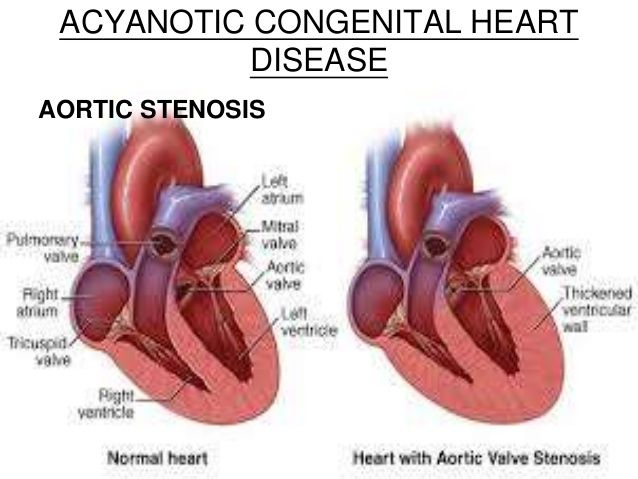
Amniocentesis
This test is done after 15 weeks of pregnancy and may be done instead of, or as well as CVS. It can provide a definite answer as to whether your baby has Down syndrome or another congenital disorder.
Amniocentesis involves taking a small amount of fluid from around your baby, using a needle and after a local anaesthetic, which is then sent for testing.
There is a very small risk of miscarriage with both CVS and amniocentesis.
Can congenital disorders be prevented?
If you have a personal or family history of certain congenital disorders, you can have genetic tests before you become pregnant. You may wish to meet with a genetic counsellor to discuss your family history, the likelihood your baby will have any congenital disorders, and possibly to arrange to have genetic testing.
If you are having in vitro fertilisation (IVF) treatment, your embryo can be tested at 2 to 4 days old, before it is implanted into your uterus.
Other things you can do to try to prevent congenital disorders include:
- eating a healthy diet with enough vitamins and minerals, in particular folic acid, during the reproductive years
- taking folic acid supplements before you become pregnant and for the first trimester of pregnancy
- avoiding alcohol, smoking and other drugs because these can harm the fetus
- controlling diabetes and gestational diabetes
- avoiding exposure to chemicals in your environment, such as pesticides or lead
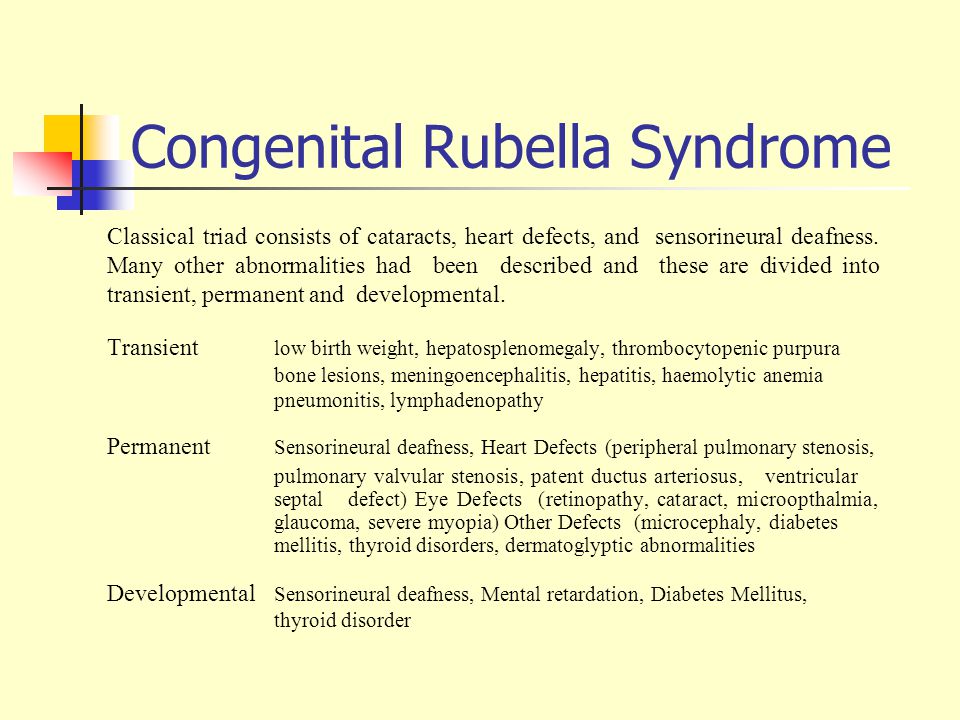
- being vaccinated, especially against rubella
Newborn testing and assessment
A paediatrician and other health professionals examine your baby in the first few days of life to check for hearing problems, heart conditions, and blood, metabolism and hormone disorders. This is called newborn screening. Early detection of such problems can often prevent them from becoming more serious physical, intellectual, visual or hearing disabilities.
This is called newborn screening. Early detection of such problems can often prevent them from becoming more serious physical, intellectual, visual or hearing disabilities.
Sources:
Raising Children Network (Tests in pregnancy), Raising Children Network (Newborn screening), Raising Children Network (Antenatal tests: chromosomal abnormalities and other conditions), Raising Children Network (Congenital heart disease), World Health Organization (Congenital anomalies), The Royal Children's Hospital Melbourne (Cleft lip and palate), Cerebral Palsy Alliance (Signs and symptoms of Cerebral Palsy), Fragile X Association of Australia (Testing and screening for Fragile X), NSW Health Centre for Genetics Education (Screening tests during pregnancy), Sydney Children's Hospitals Network (Spina bifida)Learn more here about the development and quality assurance of healthdirect content.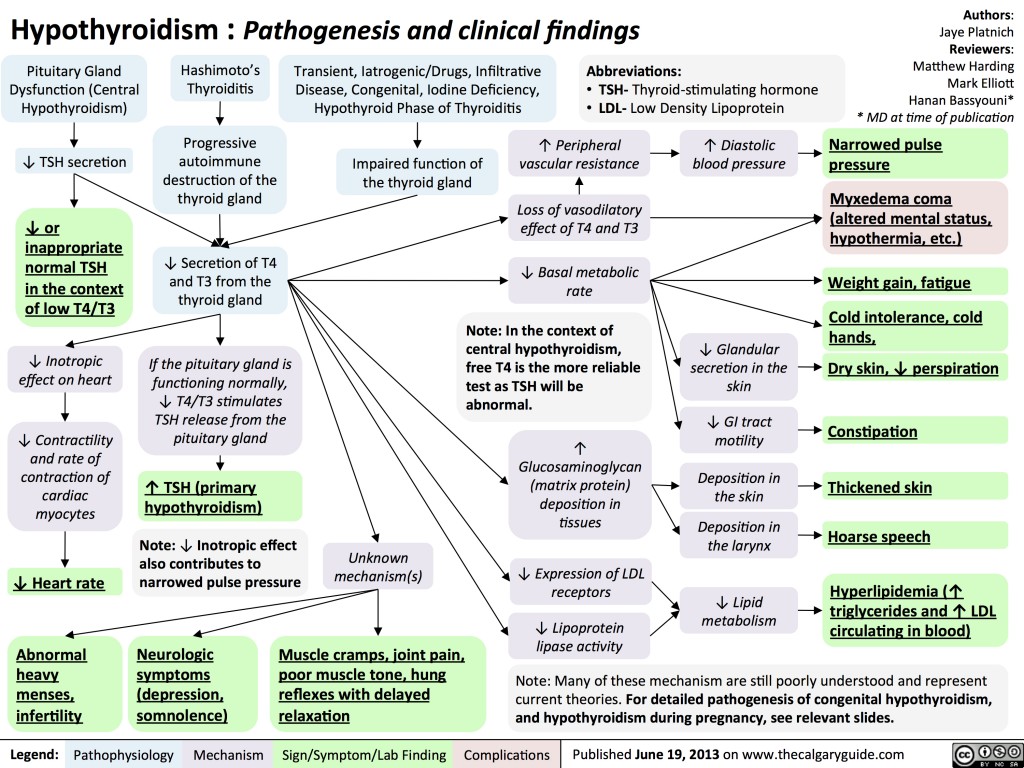
Last reviewed: June 2021
Back To Top
Related pages
- Disability and parenting support
- Early childhood intervention
- What is a childhood disability?
- Your feelings about your child's disability
- Disability rights for children
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.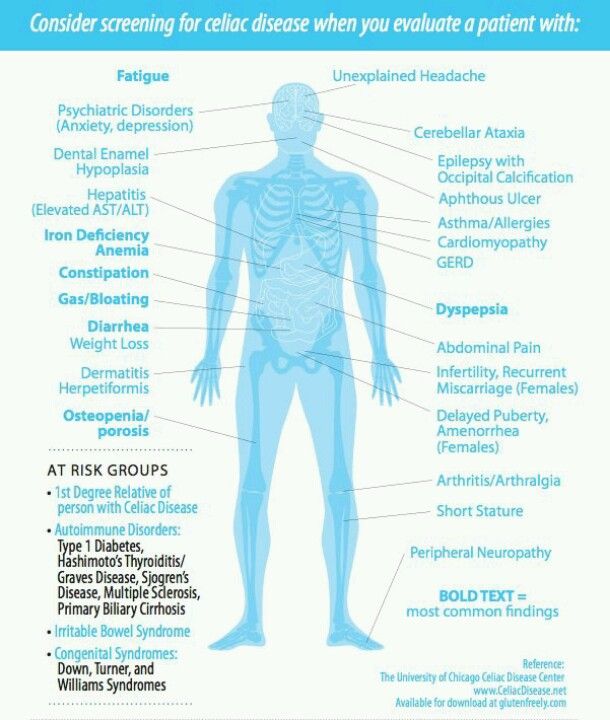
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Congenital anomalies
Congenital anomalies- All topics »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Resources »
- Fact sheets
- Facts in pictures
- Multimedia
- Publications
- Questions & answers
- Tools and toolkits
- Popular »
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Monkeypox
- All countries »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Regions »
- Africa
- Americas
- South-East Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- WHO in countries »
- Statistics
- Cooperation strategies
- Ukraine emergency
- All news »
- News releases
- Statements
- Campaigns
- Commentaries
- Events
- Feature stories
- Speeches
- Spotlights
- Newsletters
- Photo library
- Media distribution list
- Headlines »
- Focus on »
- Afghanistan crisis
- COVID-19 pandemic
- Northern Ethiopia crisis
- Syria crisis
- Ukraine emergency
- Monkeypox outbreak
- Greater Horn of Africa crisis
- Latest »
- Disease Outbreak News
- Travel advice
- Situation reports
- Weekly Epidemiological Record
- WHO in emergencies »
- Surveillance
- Research
- Funding
- Partners
- Operations
- Independent Oversight and Advisory Committee
- Data at WHO »
- Global Health Estimates
- Health SDGs
- Mortality Database
- Data collections
- Dashboards »
- COVID-19 Dashboard
- Triple Billion Dashboard
- Health Inequality Monitor
- Highlights »
- Global Health Observatory
- SCORE
- Insights and visualizations
- Data collection tools
- Reports »
- World Health Statistics 2022
- COVID excess deaths
- DDI IN FOCUS: 2022
- About WHO »
- People
- Teams
- Structure
- Partnerships and collaboration
- Collaborating centres
- Networks, committees and advisory groups
- Transformation
- Our Work »
- General Programme of Work
- WHO Academy
- Activities
- Initiatives
- Funding »
- Investment case
- WHO Foundation
- Accountability »
- Audit
- Budget
- Financial statements
- Programme Budget Portal
- Results Report
- Governance »
- World Health Assembly
- Executive Board
- Election of Director-General
- Governing Bodies website
- Home/
- Health topics/
- Congenital anomalies
UNICEF/Noorani
Newborn baby in Timor-Leste
© Credits
Fact sheets
Guidelines
Databases
WHO resolutions
WHO teams
- Newborn Health Unit
- Maternal, Newborn, Child and Adolescent Health and Ageing
- Nutrition and Food Safety
- Sensory Functions, Disability and Rehabilitation
- Sexual and Reproductive Health
Publications
All →A wide range of causes of congenital anomalies means that a portfolio of prevention approaches is needed including prevention of sexually transmitted infections,. ..
..
Congenital anomalies, also known as birth defects, are structural or functional abnormalities, including metabolic disorders, that are present from birth....
Survive and thrive: transforming care for every small and sick newborn maps out a pathway towards 2030. It is built upon epidemiology, historical trends,...
Since the publication of the WHO Guidelines for the management of sexually transmitted infections in 2003, changes in the epidemiology of STIs...
The goal of this course is to provide participants with the foundational skills needed to begin the development, implementation and ongoing improvement...
This guideline provides global, evidence-informed recommendations on blood folate concentrations in women of reproductive age for the prevention of neural...
A wide range of causes of congenital anomalies means that a portfolio of prevention approaches is needed including prevention of sexually transmitted infections,...
Feature stories
All →Resources
Toolkit for Health Needs Assessment in Congenital Disorders
International Clearinghouse for Birth Defects Surveillance and Research
Measles & Rubella Initiative
Related health topics
Class XVII.
 Congenital anomalies (malformations), deformities and chromosomal disorders (Q00-Q99)
Congenital anomalies (malformations), deformities and chromosomal disorders (Q00-Q99)
Order of the Ministry of Health of the Russian Federation of November 7,
2012 No. 614n "On approval of the standard for specialized medical care at
acute nephritic syndrome, recurrent and persistent hematuria,
chronic nephritic syndrome, other specified syndromes
congenital malformations not elsewhere classified"
(Registered with the Ministry of Justice of the Russian Federation on January 23, 2013, No. 26679)
Age category: adults, children
Gender: any
Phase: any
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 14,
Nosological units
ICD code X
N00 Acute nephritic syndrome
N02 Recurrent and persistent hematuria
N03 Chronic nephritic syndrome
Q87. 8 Other specified congenital malformation syndromes, not elsewhere classified
8 Other specified congenital malformation syndromes, not elsewhere classified
in other headings
Order of the Ministry of Health of the Russian Federation dated November 7,
2012 No. 652n "On approval of the standard for specialized medical care for children with congenital anomalies of the nervous system"
(Registered with the Ministry of Justice of the Russian Federation on February 15, 2013, No. 27133)
Age category: children
Gender: any
Phase: any
Stage: any
Complication: regardless of complications
Type of medical care: specialized medical care
Condition of rendering: stationary
Form of medical care: planned
Average treatment time (number of days): 14
ICD code X
Nosological units
Q01 Encephalocele
Q01.1 Nasal frontal encephalocele
Q03 Congenital hydrocephalus
Q03.0 Congenital malformation of aqueduct of Sylvian
Q03.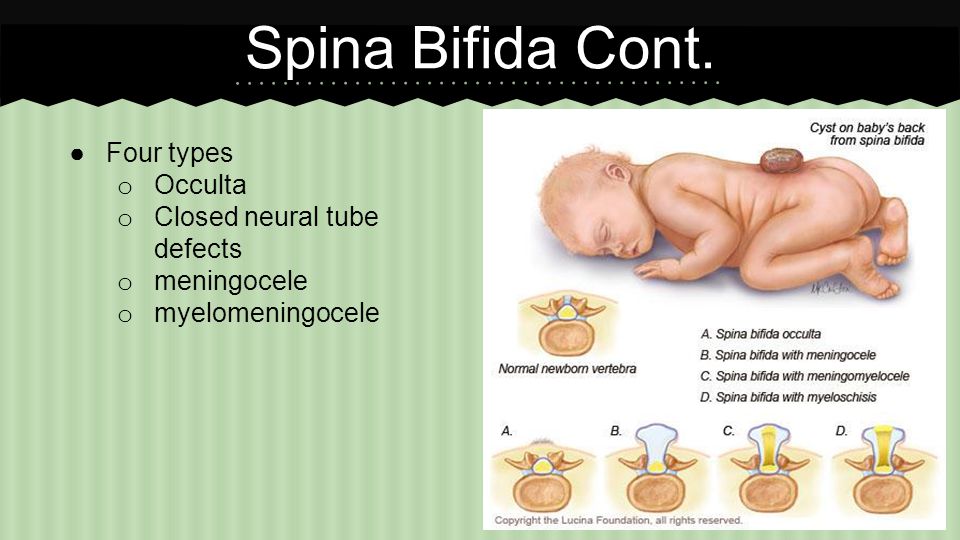 1 Atresia of foramina of Magendie and Luschka
1 Atresia of foramina of Magendie and Luschka
Q03.8 Other congenital hydrocephalus
Q05 Spina bifida [incomplete occlusion of spinal canal]
Q05.0 Spina bifida in cervical region with hydrocephalus
Q07 Other congenital malformations of the spinal cord
Q07.0 Arnold-Chiari syndrome
Q76 Congenital malformations (malformations) of the spine and cavities of the chest
Q76.0 Spina bifida occulta
Order of the Ministry of Health of the Russian Federation dated November 7,
2012 No. 653n "On approval of the standard for specialized medical care at
degenerative diseases of the spine and spinal cord"
(Registered with the Ministry of Justice of the Russian Federation on January 25, 2013, No. 26717)
Age category: adults
Gender: any
Phase: any
Stage: in the presence of neurological disorders
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 10
ICD code X
Nosological units
M43. 1 Spondylolisthesis
1 Spondylolisthesis
M48.0 Spinal stenosis
M50 Cervical intervertebral disc disease
M51 Damage to intervertebral discs of other departments
Q76.4 Other congenital malformations of the spine not associated with scoliosis
T91.1 Sequelae of vertebral fracture
Order of the Ministry of Health of the Russian Federation dated November 9,
2012 No. 725n "On approval of the standard of primary health care for children with premature puberty, including secondary genesis"
(Registered with the Ministry of Justice of the Russian Federation on February 13, 2013, No. 27056)
Age category: children
Gender: any
Phase: any
Stage: chronic
Complications: regardless of complications
Type of medical care: primary health care
Conditions of provision: outpatient
Form of medical care: planned
Average treatment time (number of days): 365
ICD code X
Nosological units
D27 Benign neoplasm of ovary
D29 Benign neoplasms of the male genital organs
D29.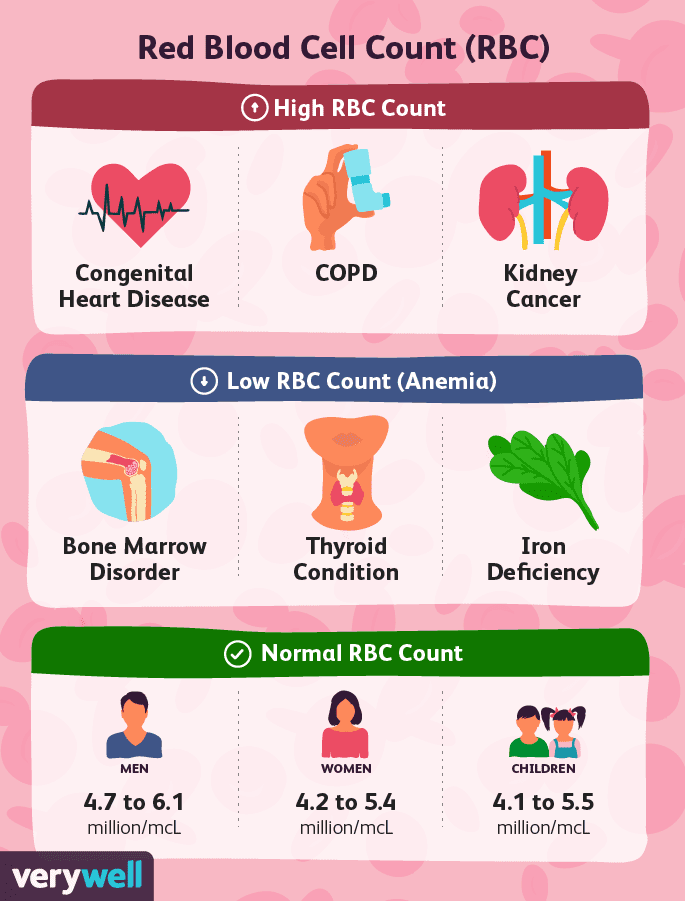 2 Testis
2 Testis
D35 Benign neoplasms of other and unspecified endocrine glands
D35.0 Adrenal
E03.9 Hypothyroidism, unspecified
E22.8 Other conditions of pituitary hyperfunction
E22.9 Hyperfunction of the pituitary gland, unspecified
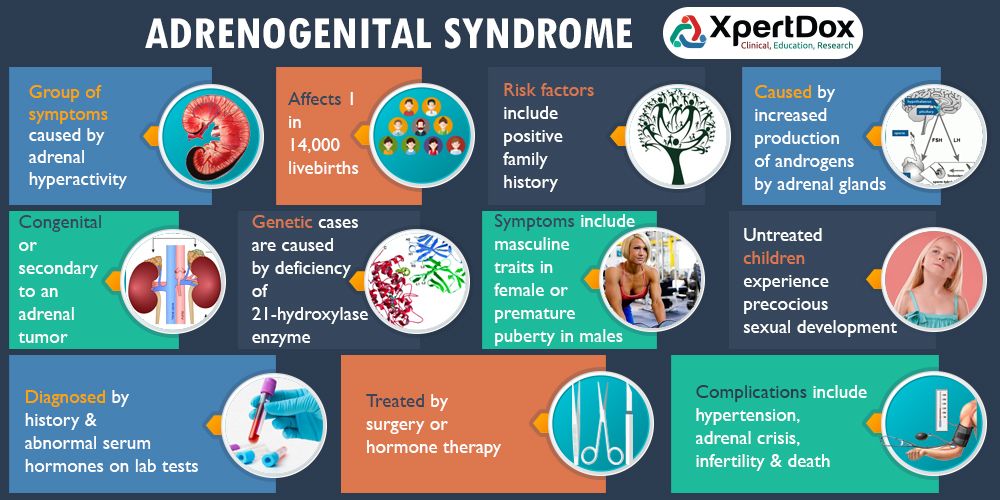
E25 Adrenogenital disorders
E25.9 Androgenital disorder, unspecified
E27.0 Other types of hypersecretion of the adrenal cortex
E28.0 Excess estrogen
E29.0 Testicular hyperfunction
E29.9 Testicular dysfunction, unspecified
E30.1 Precocious puberty
E30.8 Other disorders of puberty
E30.9 Disorder of puberty, unspecified
Q78.1 Polyostotic fibrous dysplasia
Order of the Ministry of Health of the Russian Federation dated November 9,
2012 No. 748n "On approval of the standard for specialized medical care
women with hypogonadism"
(Registered with the Ministry of Justice of the Russian Federation on January 21, 2013, No.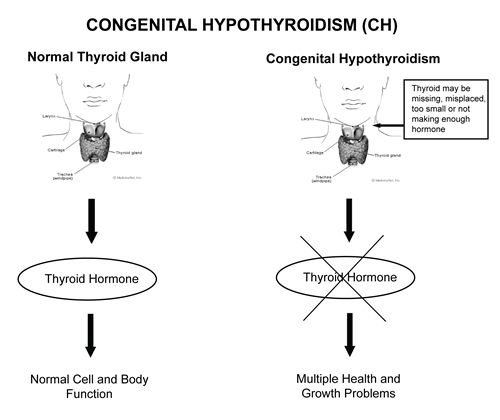 26623)
26623)
Age category: adults
Gender: female
Phase: any
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient, day hospital
Form of medical care: planned
Average treatment time (number of days): 10
ICD code X
Nosological units
E22.1 Hyperprolactinemia
E23.0 Hypopituitarism
E28.3 Primary ovarian failure
E30.0 Delayed puberty
E89.3 Hypopituitarism following medical procedures
E89.4 Ovarian dysfunction following medical procedures
Q50 Congenital anomalies [malformations] of ovaries, fallopian tubes
and wide ligaments
Q96 Turner syndrome
Order of the Ministry of Health of the Russian Federation dated November 9,
2012 No. 852n "On approval of the standard for specialized medical care for children with disorders of sex formation"
(Registered with the Ministry of Justice of the Russian Federation on February 15, 2013, No. 27124)
27124)
Age category: children
Gender: any
Phase: chronic
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient, day hospital
Form of medical care: planned
Average treatment time (number of days): 21
ICD code X
Nosological units
D27 Benign neoplasm of ovary
D35 Benign neoplasm of other and unspecified endocrine glands
D35.0 Adrenal
D39 Neoplasms of uncertain or unknown nature of the female genital
organs
D39.1 Ovary
E25 Adrenogenital disorders
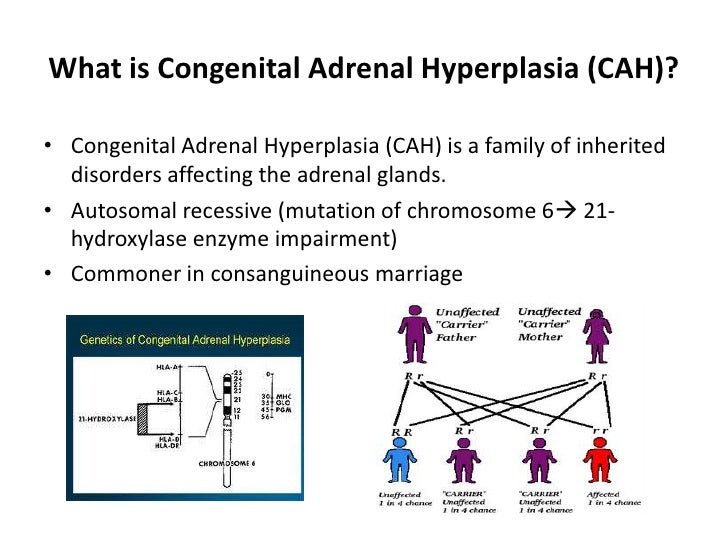
E25.0 Congenital adrenogenital disorders associated with enzyme deficiency
E25.8 Other adrenogenital disorders
E25.9 Adrenogenital disorder, unspecified
E28.3 Primary ovarian failure
E28.8 Other types of ovarian dysfunction
E28.9 Ovarian dysfunction, unspecified
E29.1 Testicular hypofunction
E29. 8 Other types of testicular dysfunction
8 Other types of testicular dysfunction
E29.9 Testicular dysfunction, unspecified
E34.5 Androgen resistance syndrome
Q55.1 Hypoplasia of testis and scrotum
Q55.6 Other congenital malformations of penis
Q55.8 Other specified congenital malformations of male genital organs
Q55.9 Congenital malformation of male genital organs, unspecified
Q56 Sexual uncertainty and pseudohermaphroditism
Q56.0 Hermaphroditism, not elsewhere classified
Q56.1 Male pseudohermaphroditism, not elsewhere classified
Q56.2 Female pseudohermaphroditism, not elsewhere classified
Q56.3 Pseudohermaphroditism, unspecified
Q56.4 Uncertainty of sex, unspecified
Q97.3 Woman with 46,XY karyotype
Q97.8 Other specified abnormal sex chromosomes, female phenotype
Q98.8 Other specified sex chromosome abnormalities, male phenotype
Q99.0 Mosaic [chimera] 46,XX/46,XY
Q99.1 46,XX true hermaphrodite
Q99.8 Other specified chromosomal abnormalities
Order of the Ministry of Health of the Russian Federation dated November 9,
2012 No. 857n "On approval of the standard for primary health care for children with stunted growth"
857n "On approval of the standard for primary health care for children with stunted growth"
(Registered with the Ministry of Justice of the Russian Federation on February 18, 2013, No. 27166)
Age category: children
Gender: any
Phase: chronic
Stage: any
Complications: regardless of complications
Type of medical care: primary health care
Conditions for the provision of medical care: outpatient
Form of medical care: planned
Average treatment time (number of days): 365
ICD code X
Nosological units
E34.3 Short stature [dwarfism], not elsewhere classified
E89.8 Other endocrine and metabolic disorders following medical treatment
procedures
Q77.8 Other osteochondrodysplasia with growth defects of long bones and vertebrae
pillar
Q77.9 Osteochondrodysplasia with growth defects of tubular bones and spinal column
unspecified
Q87.1 Congenital malformation syndromes presenting predominantly with dwarfism
Q96 Turner syndrome
Q96. 0 Karyotype 45, X
0 Karyotype 45, X
Q96.1 Karyotype 46, X iso (Xq)
Q96.2 Karyotype 46, X with abnormal sex chromosome, except iso (Xq)
Q96.3 Mosaic 45, X/46, XX or XY
Q96.4 Mosaicism 45,X/other cell line(s) with abnormal sex chromosome
Q96.8 Other variants of Turner syndrome
Q96.9 Turner syndrome, unspecified
Order of the Ministry of Health of the Russian Federation of November 9 glaucoma (Registered with the Ministry of Justice of the Russian Federation on January 31, 2013 No. 26761) Age category: adults Order of the Ministry of Health of the Russian Federation dated December 20 (Registered with the Ministry of Justice of the Russian Federation on February 19, 2013, No. 27191) Age category: children Order of the Ministry of Health of the Russian Federation dated December 20 (Registered in the Ministry of Justice of the Russian Federation 19February 2013, No. 27188) Age category: adults, children Order of the Ministry of Health of the Russian Federation of December 24, (Registered in the Ministry of Justice of the Russian Federation on March 26, 2013, No. 27892) Age category: children Order of the Ministry of Health of the Russian Federation of December 24, (Registered with the Ministry of Justice of the Russian Federation on March 5, 2013, No. 27477) Age category: children Order of the Ministry of Health of the Russian Federation of December 28 (Registered with the Ministry of Justice of the Russian Federation on March 13, 2013, No. 27645) Age category: children Order of the Ministry of Health of the Russian Federation dated December 28 (Registered with the Ministry of Justice of the Russian Federation on March 11, 2013, No. 27607) Age category: adults Order of the Ministry of Health of the Russian Federation dated December 28 (Registered with the Ministry of Justice of the Russian Federation on February 28, 2013, No. 27400) Age category: adults Order of the Ministry of Health of the Russian Federation dated December 28 (Registered with the Ministry of Justice of the Russian Federation on February 28, 2013, No. 27398) Age category: adults, children Order of the Ministry of Health of the Russian Federation of December 29, (Registered with the Ministry of Justice of the Russian Federation on March 22, 2013, No. 27845) Age category: adults, children Order of the Ministry of Health of the Russian Federation of December 29, (Registered with the Ministry of Justice of the Russian Federation on February 13, 2013, No. Age category: adults, children Order of the Ministry of Health of the Russian Federation of December 29, (Registered with the Ministry of Justice of the Russian Federation on March 7, 2013, No. 27559) Age category: adults, children Order of the Ministry of Health of the Russian Federation of December 29, (Registered with the Ministry of Justice of the Russian Federation on February 26, 2013, No. 27351) Age category: children Order of the Ministry of Health of the Russian Federation dated 29December (Registered with the Ministry of Justice of the Russian Federation on March 25, 2013, No. 27862) Age category: children Order of the Ministry of Health of the Russian Federation of December 29, (Registered with the Ministry of Justice of the Russian Federation on March 5, 2013, No. 27485) Age category: adults Categories: order; standards; ICD X. \n \n \n \nCongenital malformations are also referred to as congenital malformations, congenital disorders, or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life. \n \n \nApproximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known. \n \n \nAlthough low income may be an indirect determinant, malformations are more likely to occur in families and countries with insufficient resources. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development. \n \n \nIncest (consanguinity) increases the incidence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins . Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.\n \n \n \nMaternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries. \n \n \nDeficiencies in iodine, folate, obesity, or conditions such as diabetes mellitus are associated with some malformations. \n \n \nMaternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of developing the fetus or a newborn baby with birth defects. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition. \n \n \nPregnancy and conception preventive health care and prenatal care can reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures: \n \n \n \nPre-conception (pre-conception) and near conception (per-conception) health care includes basic reproductive health care as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below. \n \n \n \nIn countries with adequate health services, structural congenital malformations can be corrected with pediatric surgery and children with functional problems such as thalassemia (inherited by recessive blood disease), sickle cell disorders, and congenital hypothyroidism. \n \n \nIn 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs. \n \nThe Global Strategy for Women's and Children's Health, announced in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in implementing efficient and cost-effective action to promote newborn and child health.\n \n \nWHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy on salt fortification in foods folic acid at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts. \n \nThe International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit, international organization in official relations with WHO. \n \nThe WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual seminars on surveillance and prevention of birth defects and preterm birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs. \n \nThe GAVI Alliance, partnered with WHO, is helping developing countries to increase the control and elimination of rubella and congenital rubella syndrome through immunization. \n \nWHO is developing normative tools, including guidelines and a global plan of action to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers. \n \n \nThe WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school). \n ","datePublished":"2022-02-28T22:52:00.0000000+00:00","image":"https://cdn.who.int/media/images/default -source/imported/preterm-birth-mother-jpg.jpg?sfvrsn=c5c1adf1_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo": {"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified ":"2022-02-28T22:52:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/congenital-anomalies", "@context":"http://schema.org","@type":"Article"}; Malformations and preterm birth are major causes of childhood death, chronic disease and disability in many countries. In 2010, the World Health Assembly adopted a resolution calling on all Member States to promote primary prevention and health promotion for children with developmental disabilities through: Congenital malformations are also referred to as congenital malformations, congenital disorders or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life. Approximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known. While low income may be an indirect determinant, malformations are more likely to occur in under-resourced families and countries. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development. Incest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins. Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations. Maternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries. Deficiency of iodine, folic acid salts, obesity, or conditions such as diabetes mellitus are associated with some malformations. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. Maternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of birth defects in the fetus or newborn. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition. Preventive health care during pregnancy and conception, as well as antenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures: Medical care before conception (in the preconception period) and around the time of conception (in the periconceptional period) includes basic reproductive health care, as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below. In countries with adequate health services, structural birth defects can be corrected with pediatric surgery and timely treatment can be provided for children with functional problems such as thalassemia (a recessive blood disorder), sickle cell disorders, and congenital hypothyroidism. In 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs. The Global Strategy for Women's and Children's Health, launched in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in achieving effective and cost-effective action to improve newborn health and children. WHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy for folic acid fortification at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts. The International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit international organization in official relations with WHO. This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects. The WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual workshops on surveillance and prevention of birth defects and premature birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs. The GAVI Alliance, with WHO among its partners, is helping developing countries to accelerate the control and elimination of rubella and congenital rubella syndrome through immunization. WHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers. The WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).
Gender: any
Phase: with normal, moderately elevated or high intraocular pressure
Stage: any
Complications: no complications, cataract
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned, emergency
Average treatment time (number of days): 8
ICD code X
Nosological units
H26.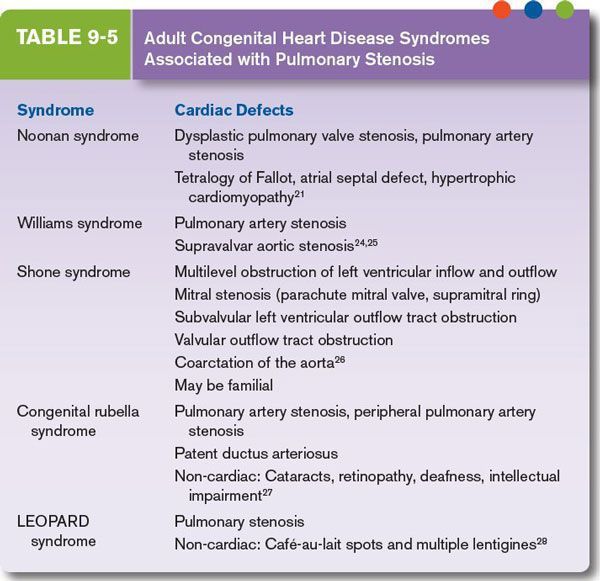 2 Complicated cataract
2 Complicated cataract
H40.0 Suspected glaucoma
H40.1 Primary open-angle glaucoma
H40.2 Primary angle-closure glaucoma
H40.3 Glaucoma, secondary, post-traumatic
H40.4 Glaucoma secondary to inflammatory eye disease
H40.5 Glaucoma secondary to other diseases of the eye
H40.6 Glaucoma, secondary, drug-induced
H40.8 Other glaucoma
H40.9 Glaucoma, unspecified
H42.0 Glaucoma in diseases of the endocrine system, eating disorders and disorders
metabolism
Q15.0 Congenital glaucoma
2012 No. 1074n "On approval of the standard for specialized medical care for children with delayed sexual development"
Gender: female
Phase: any
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 21
ICD code X
Nosological units
E23. 0 Hypopituitarism
0 Hypopituitarism
E28.3 Primary ovarian failure
E30.0 Delayed puberty
E89.3 Hypopituitarism following medical procedures
Q50.0 Congenital absence of ovary
Q56.0 Hermaphroditism, not elsewhere classified
Q87.1 Syndromes of congenital malformations presenting predominantly with dwarfism
Q96 Turner syndrome
Q97.3 Woman with 46,XY karyotype
Q99.0 Mosaic [chimera] 46,XX/46,XY
Q99.1 46,XX true hermaphrodite
2012 No. 1076n "On approval of the standard for specialized medical care at
rough rigid scoliotic deformity of the spine"
Gender: any
Phase: progressive; non-progressive
Stage: rigid scoliotic deformity over 110 degrees
Complications: no complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 60
ICD code X
Nosological units
Q76. 3 Congenital scoliosis due to malformation of bone
3 Congenital scoliosis due to malformation of bone
Q77.9 Osteochondrodysplasia with growth defects of tubular bones and spinal column
unspecified
M41.1 Juvenile idiopathic scoliosis
M41.2 Other idiopathic scoliosis
M41.3 Thoracogenic scoliosis
M41.4 Neuromuscular scoliosis
M41.5 Other secondary scoliosis
2012 No. 1422n "On approval of the standard for primary health care for children with delayed sexual development"
Gender: female
Phase: light; moderate
Stage: remission; subacute course
Complications: no complications
Type of medical care: primary health care
Conditions for the provision of medical care: outpatient
Form of medical care: planned
Average treatment time (number of days): 14
ICD code X
Nosological units
E30. 0 Delayed puberty
0 Delayed puberty
E23.0 Hypopituitarism
E89.3 Hypopituitarism following medical procedures
E28.3 Primary ovarian failure
Q50.0 Congenital absence of ovary
Q96 Turner syndrome
Q99.0 Mosaic [chimera] 46,XX/46,XY
Q97.3 Female with 46,XY karyotype
Q99.1 46,XX true hermaphrodite
Q56.0 Hermaphroditism, not elsewhere classified
2012 No. 1561n "On approval of the standard for specialized medical care for children with precocious puberty"
Gender: any
Phase: any
Stage: chronic
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient; day hospital
Form of medical care: planned
Average treatment time (number of days): 14,
ICD code X
Nosological units
C56 Malignant neoplasm of ovary
C62 Malignant neoplasm of testis
C74. 0 Adrenal cortex
0 Adrenal cortex
D27 Benign neoplasm of ovary
D29.2 Testicles
D35.0 Adrenal
E03.9 Hypothyroidism, unspecified
E22.8 Other conditions of pituitary hyperfunction
E25 Adrenogenital disorders
E25.9 Adrenogenital disorder, unspecified
E27.0 Other types of hypersecretion of the adrenal cortex
E28.0 Excess estrogen
E28.1 Androgen excess
E29.0 Testicular hyperfunction
E29.9 Testicular dysfunction, unspecified
E30.1 Precocious puberty
E30.8 Other disorders of puberty
E30.9 Disorder of puberty, unspecified
E35.8 Disorders of other endocrine glands in diseases classified elsewhere
headings
Q78.1 Polyostotic fibrous dysplasia
Y42.4 Oral contraceptives
Y42.5 Other estrogens and progestogens
Y42.7 Androgens and their anabolic analogues
Y42.8 Other and unspecified hormones and their synthetic substitutes
Y42.9 Other and unspecified hormone antagonists
2012 No. 1595n "On approval of the standard for specialized medical care for children with congenital anomalies (malformations) and posterior diseases
1595n "On approval of the standard for specialized medical care for children with congenital anomalies (malformations) and posterior diseases
eye segment"
Gender: any
Phase: any
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 11
ICD code X
Nosological units
Q14.0 Congenital malformation of the vitreous body
Q14.1 Congenital retinal anomaly
Q14.3 Congenital malformation of choroid
Q14.2 Congenital malformation of optic disc
Q14.9 Congenital malformation of posterior segment of eye, unspecified
2012 No. 1614n "On approval of the standard for primary health care at
1614n "On approval of the standard for primary health care at
congenital ichthyosis"
Gender: any
Phase: any
Stage: any
Complications: regardless of complications
Type of medical care: primary health care
Conditions for the provision of medical care: outpatient
Form of medical care: planned
Average treatment time (number of days): 30
ICD code X
Nosological units
Q80.0 Ichthyosis simplex
2012 No. 1615n "On approval of the standard for specialized medical care at
congenital ichthyosis"
Gender: any
Phase: any
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 18
ICD code X
Nosological units
Q80. 0 Ichthyosis simplex
0 Ichthyosis simplex
2012 No. 1618n "On approval of the standard for specialized medical care at
congenital pulmonary stenosis and other congenital anomalies
pulmonary artery"
Gender: any
Phase: any
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 10
ICD code X
Nosological units
Q25.6 Stenosis of the pulmonary artery
Q25.7 Other congenital malformations of pulmonary artery
2012 No.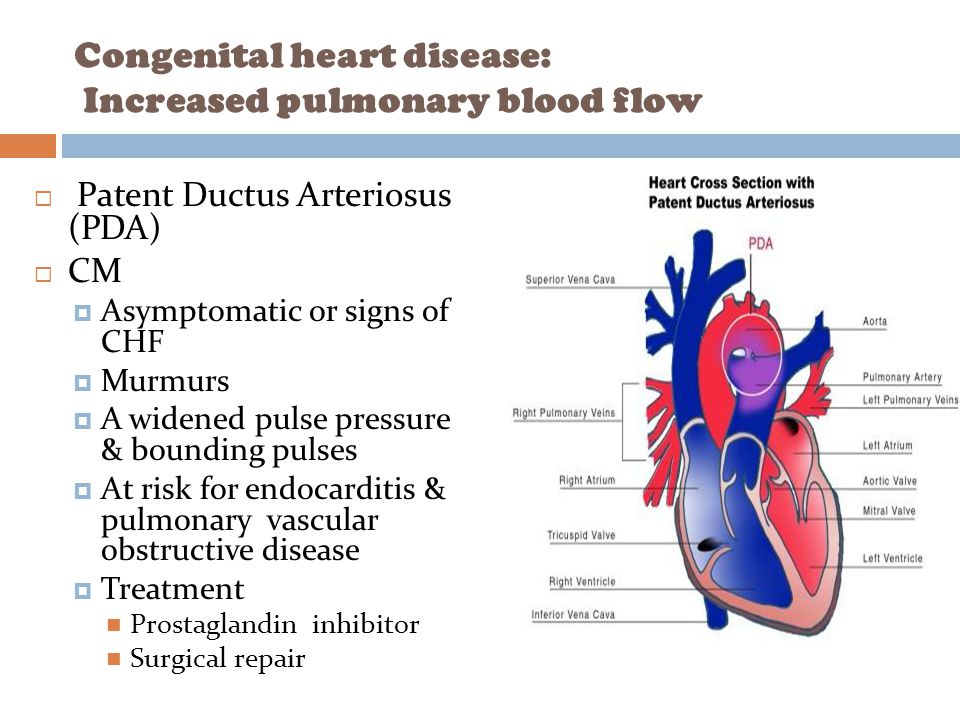 1655n "On approval of the standard for specialized medical care at
1655n "On approval of the standard for specialized medical care at
congenital aortic valve stenosis"
Gender: any
Phase: any
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 10
ICD code X
Nosological units
Q23.0 Congenital aortic valve stenosis
2012 No. 1656n "On approval of the standard for specialized medical care at
congenital anomalies (malformations) of the cardiac septum"  27060)
27060)
Gender: any
Phase: any
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 10
ICD code X
Nosological units
Q21.0 Ventricular septal defect
Q21.1 Atrial septal defect
Q21.2 Atrioventricular septal defect
Q21.4 Septal defect between aorta and pulmonary artery
2012 No. 1657n "On approval of the standard for specialized medical care at
other congenital anomalies (malformations) of the cardiac septum"
Gender: any
Phase: any
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 15
ICD code X
Nosological units
Q21.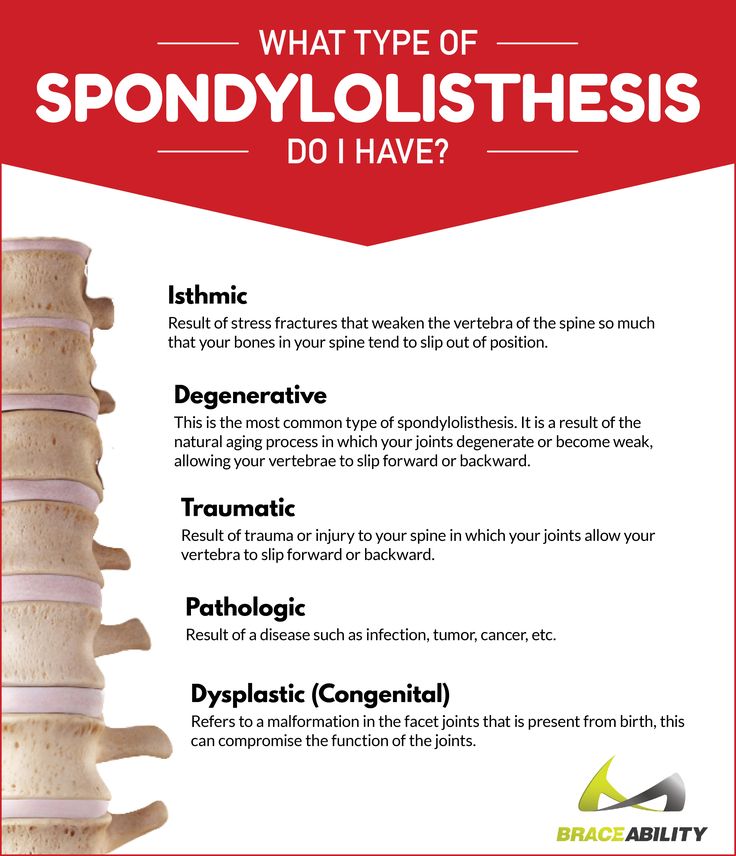 8 Other congenital malformations of cardiac septum
8 Other congenital malformations of cardiac septum
2012 No. 1659n "On approval of the standard for specialized medical care for children with stunted growth"
Gender: any
Phase: chronic
Stage: any
Complications: regardless of complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient; day hospital
Form of medical care: planned
Average treatment time (number of days): 14,
ICD code X
Nosological units
E34.3 Short stature [dwarfism], not elsewhere classified
Q96 Turner syndrome
Q87.1 Congenital malformation syndromes presenting predominantly with dwarfism
Q96. 0 Karyotype 45,X
0 Karyotype 45,X
Q96.1 Karyotype 46,X iso (Xq)
Q96.2 46,X karyotype with abnormal sex chromosome except iso (Xq)
Q96.3 Mosaic 45,X/46,XX or XY
Q96.4 Mosaicism 45,X/other cell line(s) with abnormal sex chromosome
Q96.8 Other variants of Turner syndrome
Q96.9 Turner syndrome, unspecified
Q77.8 Other osteochondrodysplasia with growth defects of tubular bones and vertebral column
Q77.9 Osteochondrodysplasia with growth defects of tubular bones and spinal column
unspecified
2012 No. 1697n "On approval of the standard for specialized medical care for children with tuberous sclerosis"
Gender: any
Phase: any
Stage: any
Complications: no complications
Type of medical care: specialized medical care
Conditions for the provision of medical care: inpatient
Form of medical care: planned
Average treatment time (number of days): 21
ICD code X
Nosological units
Q85.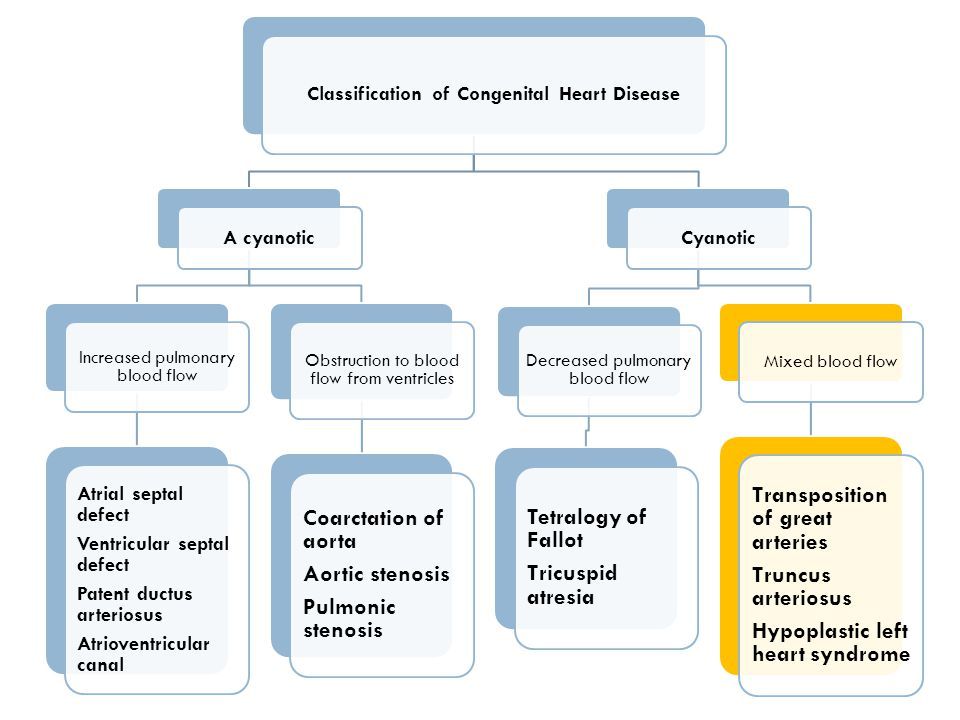 1 Tuberous sclerosis
1 Tuberous sclerosis
2012 No. 1700n "On approval of the standard for primary health care at
glaucoma"
Gender: any
Phase: with normal; moderately elevated or high intraocular pressure
Stage: initial; developed; far gone; terminal
Complications: regardless of complications
Type of care: primary health care
Conditions for the provision of medical care: outpatient
Form of medical care: planned
Average treatment time (number of days): 7
ICD code X
Nosological units
H40.0 Suspected glaucoma
H40.1 Primary open-angle glaucoma
H40.2 Primary angle-closure glaucoma
H40.3 Glaucoma, secondary, post-traumatic
H40.4 Glaucoma secondary to inflammatory disease of the eye
H40. 5 Glaucoma secondary to other diseases of the eye
5 Glaucoma secondary to other diseases of the eye
H40.6 Glaucoma, secondary, drug-induced
H40.8 Other glaucoma
H40.9 Glaucoma, unspecified
H42.0 Glaucoma in diseases of the endocrine system, eating disorders and metabolic disorders
substances
Q15.0 Congenital glaucoma Malformations
Malformations
\n

Definition
Causes and risk factors
Socio-economic factors
 Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations. Genetic factors
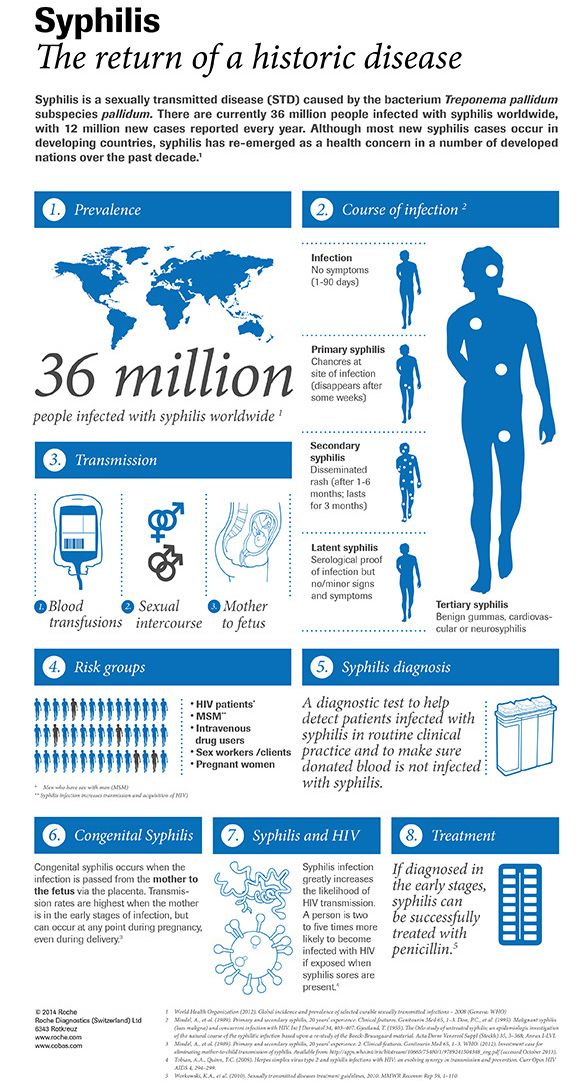
Infections
Maternal nutrition
 For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus. Environmental factors
Prevention
\n
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy.
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. Identification
\n
 In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward.
In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. Treatment and care
WHO activities
 This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects. 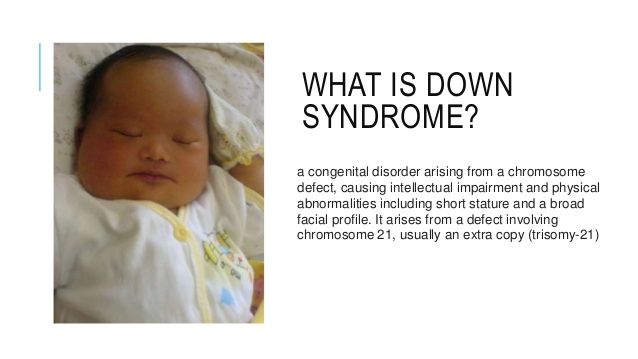
United Nations Convention on the Rights of Persons with Disabilities
Key Facts
Definition
Causes and risk factors
Socio-economic factors
 Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations. Genetic factors
Infections
Maternal nutrition
 In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus. Environmental factors
Prevention

 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy.
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. Detection
 During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy.
During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. Treatment and medical care
WHO activities
UN Convention on the Rights of Persons with Disabilities