Epidural needle for pregnancy
Epidural block - pregnancy: MedlinePlus Medical Encyclopedia
An epidural block is a numbing medicine given by injection (shot) in the back. It numbs or causes a loss of feeling in the lower half of your body. This lessens the pain of contractions during childbirth. An epidural block may also be used to reduce pain during surgery on the lower extremities. This article focuses on epidural blocks during childbirth.
The block or shot is given into an area over your lower back or spine.
- You may be asked to lie on your side, or you may sit up.
- Either way, you will be asked to pull your stomach inward and hunch your back outward.
Your health care provider will wash the area of your back and inject a little medicine to numb the spot where the epidural needle is placed:
- The provider inserts a needle into your lower back.
- The needle is placed into a small space outside your spinal cord.
- A small soft tube (catheter) is placed into your back, next to your spine.
- The needle is removed.
The numbing medicine is given through the tube for as long as it is needed.
In most cases, you will receive a low dose because it is safer for you and baby. Once the medicine takes effect (10 to 20 minutes), you should feel better. You may still feel some back or rectal pressure during contractions.
You may shiver after an epidural, but this is common. Many women shiver during labor even without an epidural.
Many studies have shown that an epidural is a safe way to manage pain during childbirth. While rare, there are some risks.
Your blood pressure may drop for a short while. This might cause the baby's heart rate to slow down.
- To avoid this, you will receive fluids through an intravenous (IV) line to help keep your blood pressure stable.
- If your blood pressure shows a drop, you may need to lie on your side to keep the blood moving throughout your body.
- Your provider may also give you medicine to raise your blood pressure.

An epidural block may change or alter labor and delivery.
- If you are very numb from the block, you may have a harder time bearing down to push your baby through the birth canal.
- Contractions may lessen or slow down for a little while, but labor will still move along as it should. In some cases, it may even go faster. If your labor slows down, your doctor can give you medicine to speed up your contractions. It is best to wait until you are in active labor to have the epidural placed.
Other rare side effects are:
- You may get a headache after your epidural but this is rare.
- Medicine could enter your spinal fluid. For a short while, it could make you feel dizzy, or you might have a hard time breathing. You could also have a seizure. This is also rare.
There are 2 types:
- "Walking" epidural block. This type of epidural will lessen your pain, but you will still be able to move your legs. Most women are not really able to walk around, but they can move their legs.

- Combined spinal epidural block. This combines both a spinal and epidural block. It provides pain relief much faster. The combined block is used when women are in very active labor and want relief right away.
Delivery - epidural; Labor - epidural
- Epidural - series
Hawkins JL, Bucklin BA. Obstetric anesthesia. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 16.
Nathan N, Wong CA. Spinal, epidural, and caudal anesthesia: anatomy, physiology, and technique. In: Chestnut DH, Wong CA, Tsen LC, et al, eds. Chestnut's Obstetric Anesthesia: Principles and Practice. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 12.
Sharpe EE, Arendt KW. Anesthesia for obstetrics. In: Gropper MA, ed. Miller's Anesthesia. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 62.
Updated by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Browse the Encyclopedia
Epidural | Pregnancy Birth and Baby
beginning of content3-minute read
Listen
An epidural is a type of pain relief for women in labour or who are having a caesarean section.
What is an epidural?
An epidural is a procedure that injects a local anaesthetic in to the space around the spinal nerves in your lower back.
This anaesthetic usually blocks the pain from labour contractions and during the birth very effectively. With an epidural you can usually move and can push your baby out when you need to.
An epidural is usually done by an anaesthetist.
The procedure
Before an epidural, you will usually have a drip for fluids put into your arm.
You can sit up and bend forward over a pillow, or lie on your side curled up into a ball. This makes it easier for the needle to be inserted into the right place. You will be asked to stay still.
Your lower back will be washed with cold antiseptic. A small amount of local anaesthetic will be injected into the skin of your lower back. A needle will be inserted between the bones of your spine into the space around your spinal nerves. Your anaesthetist will insert the epidural needle when your contraction stops, so it is important that you tell them when you have a contraction.
A small soft plastic tube will be inserted and the needle will be removed. That tube delivers the anaesthetic that will numb your pain.
It usually takes between 5 and 30 minutes for your pain to be relieved by the epidural.
You usually only have an epidural during the first stage of labour — but it can be given at any stage of labour.
Advantages and disadvantages of an epidural
Epidurals are available at most hospitals but not in birth centres or for home births.
The advantages of an epidural are:
- it is usually very effective
- it is generally very safe
- you can often still move around in bed and push when you need to
- if you have a long labour, it allows you to sleep and recover your strength
- if you're having a caesarean, you can stay awake and your partner can be there
The disadvantages of an epidural are:
- for medical reasons, not everyone can have an epidural
- you might need to have fluids given to you through a tube in your arm, and will need to have your blood pressure monitored
- you might lose feeling in your bladder and need a catheter (tube) in your bladder to help you pass urine
- you might lose feeling in your legs for a few hours
- it might slow down the second stage of labour
- you might not be able to push and need help to give birth
- your baby will need to be closely monitored during your labour
Whether you have an epidural or not makes no difference to the chance of you having a caesarean section.
Risks and side effects
An epidural is effective and fairly safe. But there are some risks.
- Some women feel cold or itchy.
- A small number of women get little or no pain relief.
- Some women get weakness in the legs; it wears off after a few hours.
- There is an increased risk of needing forceps or a vacuum to help with the birth.
- Some women develop a bad headache 24 to 48 hours after an epidural.
- There is a small chance of developing a skin infection.
- Very rarely a few women get permanent nerve damage.
What to discuss with your doctor or midwife
You can check:
- if you can have an epidural at your chosen hospital or birth centre
- what their epidural procedures are
- the type of pain relief that might suit you best
Sources:
Australia and New Zealand College of Anaesthetists (Epidurals and childbirth), Government of Western Australia Department of Health (Epidurals for childbirth), Mater Mothers' Hospital (Epidural), They Royal Women's Hospital (Epidural information), Royal Australian College of Obstetricians and Gynaecologists (Pain relief in labour and childbirth), Queensland Health (Epidural analgesia in labour - clinical guidelines)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: January 2020
Back To Top
Related pages
- TENS (Transcutaneous electrical nerve stimulation)
- Gas (Entonox)
- Non-medical pain relief during labour
- Pain relief during labour
- Making a birth plan
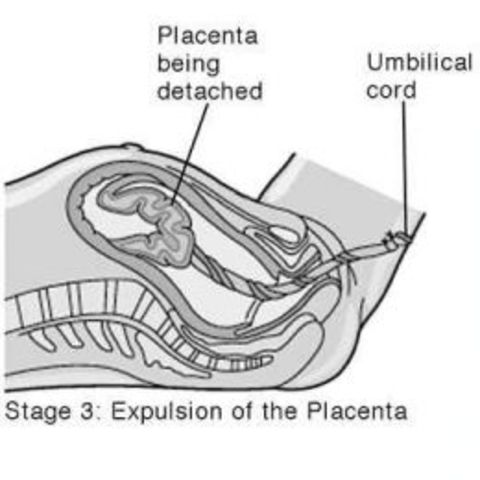
- Giving birth - stages of labour
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.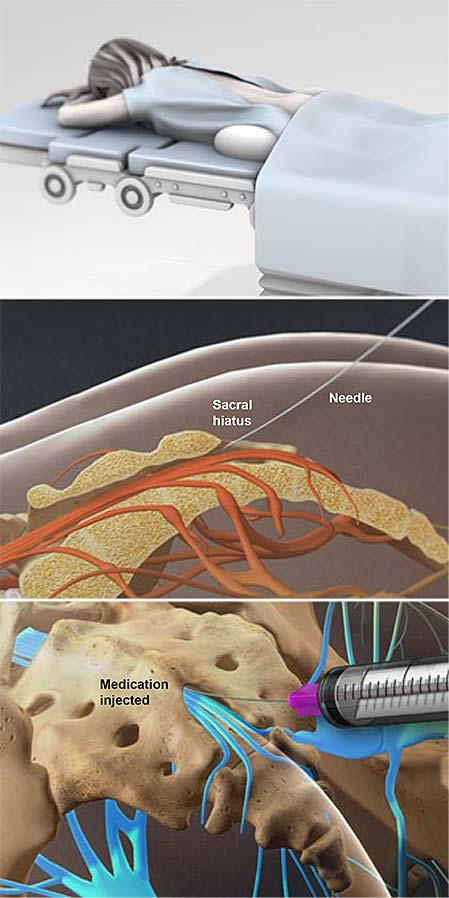
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Not Found (#404)
Paracelsus Medical Center
Page not found.
The above error occurred while the Web server was processing your request.
Please contact us if you think this is a server error. thank you.
Please wait, download may take time
Loading...
Do you know which doctor you want to see
You know the service you want to sign up for
Service selection
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
The choice of a specialist
Service selected:
Choosing a specialist service
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
Address selection:
st. Vikulova, 33, building 2 st. Bolshakova, d. 68
Date selection:
Time of receipt:
Password
Password
Register Can't login? account activation
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for password recovery
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for reactivating your account
Your application has been accepted, our specialists will answer your question as soon as possible!
Telephone
Comment
Dear patients!
Multidisciplinary Clinic and Maternity Hospital "Paracelsus" informs you, according to the Letter of the Ministry of Finance of the Russian Federation to the Federal Tax Service dated March 25, 2022. N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
Joint order of the Ministry of Taxation of Russia and the Ministry of Health of Russia of July 25, 2001 N 289 / BG-3-04 / 256 (hereinafter - the order of July 25, 2001) approved the form of the Certificate of payment for medical services for submission to the tax authorities of the Russian Federation (hereinafter - the Certificate payment for medical services).
This certificate certifies the fact of receiving a medical service and its payment through the cash desk of a healthcare institution at the expense of the taxpayer.
Thus, if the taxpayer submits to the tax authority a Certificate of payment for medical services, the taxpayer's failure to submit the relevant contract for the provision of medical services and (or) documents confirming payment cannot be grounds for refusing to provide such a deduction.
The amounts are based on payment data. Therefore, checks, an agreement and a clinic license are not needed to make a deduction.
Sample certificate attached.
Help Sample
Your application has been accepted, our specialists will contact you shortly!
Telephone
Comment
Epidural analgesia in childbirth - GBUZ VO "REGIONAL PERINATAL CENTER"
The use of epidural analgesia during childbirth is becoming popular because of the convenience it provides. An epidural block reduces sensation in the lower parts of the body, but does not affect consciousness. The stage of labor at which an epidural is used may differ from patient to patient. If you need an epidural, your obstetrician and anesthesiologist will need to evaluate you and your baby, history of past anesthesias, and the progress of your labor. The most frequently asked questions when performing epidural analgesia in labor are:
An epidural block reduces sensation in the lower parts of the body, but does not affect consciousness. The stage of labor at which an epidural is used may differ from patient to patient. If you need an epidural, your obstetrician and anesthesiologist will need to evaluate you and your baby, history of past anesthesias, and the progress of your labor. The most frequently asked questions when performing epidural analgesia in labor are:
When is epidural analgesia performed?
The time to start epidural analgesia is determined by the obstetrician and anesthesiologist, depending on the needs of the mother and baby during labor.
How is an epidural block performed?
Epidural lumbar anesthesia is performed in the lower back with the patient sitting or lying on her side. Anesthesia is performed below the level where the spinal cord ends.
Before performing the block, the skin is treated with an antiseptic solution. The anesthesiologist then performs local anesthesia of the skin at the puncture site. After that, a special needle is inserted into the epidural space of the spine, slightly short of the spinal space. An epidural catheter, which is a thin, flexible tube, is inserted through the needle. Sometimes the catheter can touch a nerve, causing a shooting sensation in the leg.
Next, the needle is removed and the catheter is attached to the back. Subsequent injections will no longer require a second puncture, but are made through a catheter. An epidurally administered local anesthetic is thought to provide an epidural block by bathing the spinal nerves.
How soon does an epidural block occur and how long does it last?
The start of the block is gradual and slow. Pain relief usually develops 10-20 minutes after epidural administration and may be continued until the end of labor as additional doses of drugs can be administered through the epidural catheter. After delivery, the catheter is removed and after a few hours your sensations return to normal.
How does an epidural block feel?
With a significant reduction in pain, there may be a feeling of pressure during contractions and vaginal examination by an obstetrician. There may be transient numbness, weakness, and heaviness in the legs.
Do I need to stay in bed after an epidural?
Usually, during analgesia, you are warned not to get out of bed and lie on your back for more than 10 minutes during labor. However, it is believed that maintaining the vertical position of the body contributes to the favorable course of childbirth. There is a type of epidural analgesia that allows you to sit and walk. This type of analgesia is called "walking epidural" or ambulatory, mobile epidural.
Does epidural analgesia affect the child?
Studies show that epidural analgesia is safe for mother and child.
Will an epidural block slow down labor?
In some patients, during the action of epidural analgesia, contractions may weaken for a short time. Most patients note that epidural analgesia helps them relax, while at the same time, uterine contractility improves.
Will the ability to push remain?
Epidural analgesia will allow you to relax and maintain strength during the longest part of labor - when the cervix opens. In the pushing period of childbirth, if properly applied, it will not affect the attempts and even make them more pleasant.
What are the possible side effects of epidural analgesia?
Rarely, even with careful monitoring and precautions by the anesthetist, complications or side effects may occur. The most common complications are arterial hypotension and headache. More severe complications are a toxic reaction to local anesthetics, respiratory arrest, and neurological disorders. They are extremely rare.
Lowering blood pressure. You will receive intravenous fluids to prevent this complication. In addition, during delivery, you usually need to lie on your side, and after delivery, you need to stay in bed until the block wears off.
Headache occurs infrequently, in about 0.7-1.4% of cases. Maintaining the required position during the puncture helps to prevent its occurrence. When a headache occurs, simple measures are usually effective: bed rest, fluids, and pain medications. If pain persists, additional treatment may be required.
Chills is a common reaction during childbirth, but may also occur during anesthesia. Warming helps a lot.
Itchy skin is mild in most cases, but if it becomes unbearable, it can be cured by the administration of drugs.
Difficulty breathing Very rarely anesthesia can affect the intercostal muscles and make breathing difficult. In this case, the condition of the woman in labor will facilitate the administration of oxygen.
Reactions to local anesthetics are rare but can be serious. During pregnancy, the veins passing through the epidural space dilate, and therefore there is a risk of intravascular injection. In order to avoid unwanted reactions, the anesthesiologist initially administers a test dose of the drug and asks the woman in labor to pay attention to the possibility of dizziness, metallic taste, palpitations or numbness.
Insufficient anesthesia. Sometimes the action of the anesthetic is "mosaic" or one-sided. The anesthetist may change your position in bed or pull up your epidural catheter. Rarely, repeat epidural anesthesia may be required.
The anesthesia anesthetist evaluates your condition and takes precautions during the procedure. You can discuss with him the possibilities of pain relief and your concerns about it.
When should epidurals not be used?
Contraindications to the use of epidural anesthesia are:
- bleeding disorders or the use of anticoagulants,
- generalized infection or infection at the puncture site,
- bleeding,
- patient refusal,
- severe neurological disease,
- heart disease with fixed cardiac output.
The Department of Anesthesiology and Intensive Care provides labor pain relief using epidural analgesia to all patients who need this pain relief. When performing analgesia, modern disposable sets for epidural blockade made in Germany, anesthetic Naropin made in Great Britain are used.