Prevention spina bifida
Spina bifida - Symptoms and causes
Overview
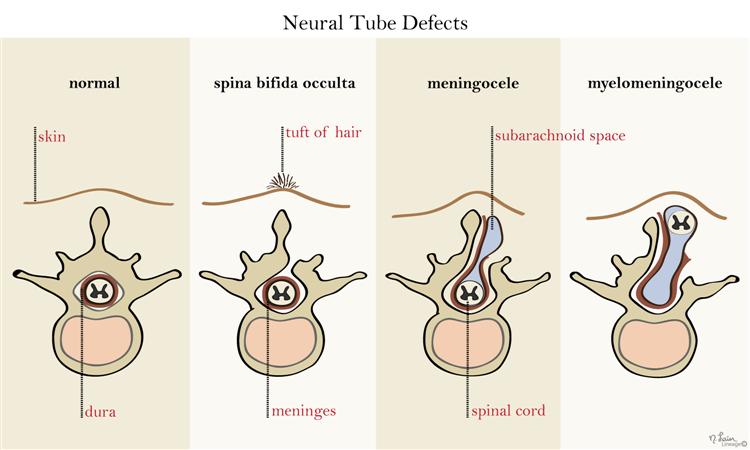
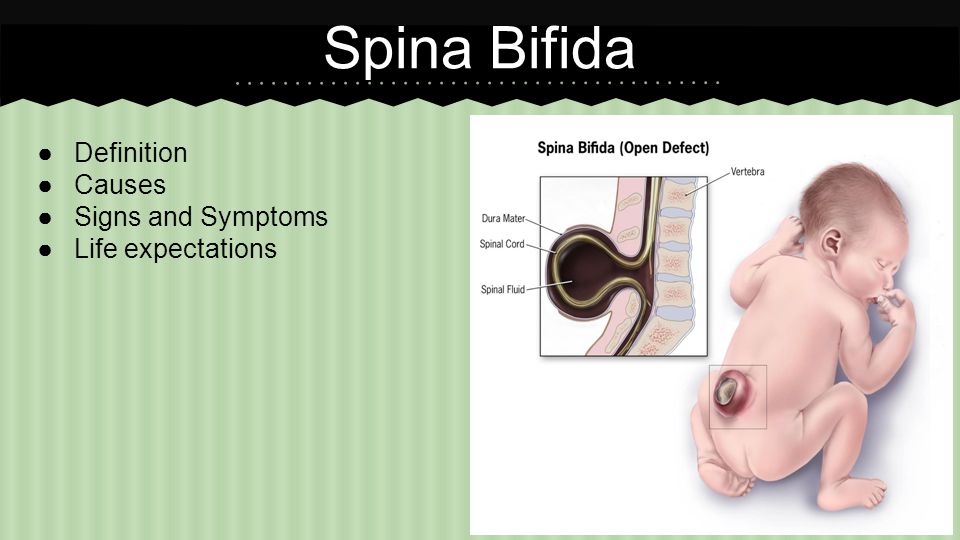
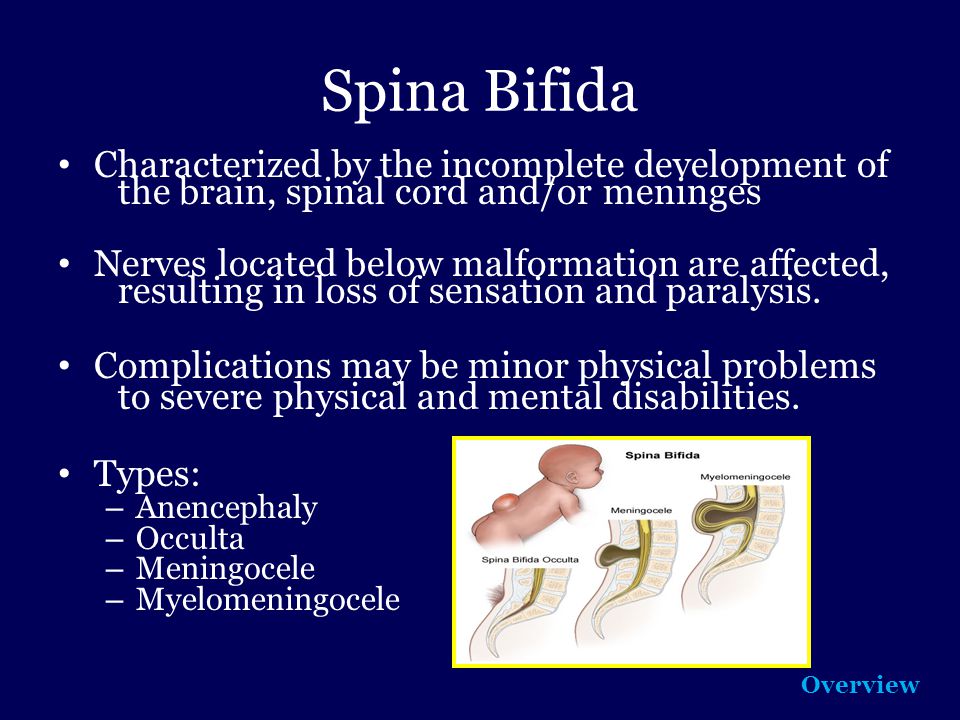
Spina bifida is a birth defect that occurs when the spine and spinal cord don't form properly. It's a type of neural tube defect. The neural tube is the structure in a developing embryo that eventually becomes the baby's brain, spinal cord and the tissues that enclose them.
Typically, the neural tube forms early in pregnancy and it closes by the 28th day after conception. In babies with spina bifida, a portion of the neural tube doesn't close or develop properly, causing problems in the spinal cord and in the bones of the spine.
Spina bifida can range from mild to severe, depending on the type of defect, size, location and complications. When necessary, early treatment for spina bifida involves surgery — although such treatment doesn't always completely resolve the problem.
Types
Spina bifida (myelomeningocele)
Spina bifida (myelomeningocele)
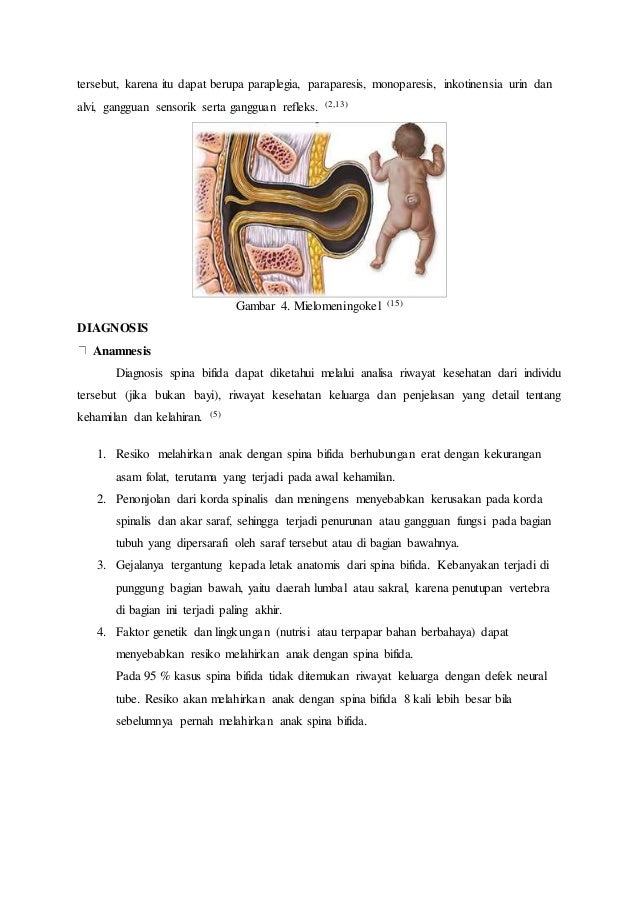
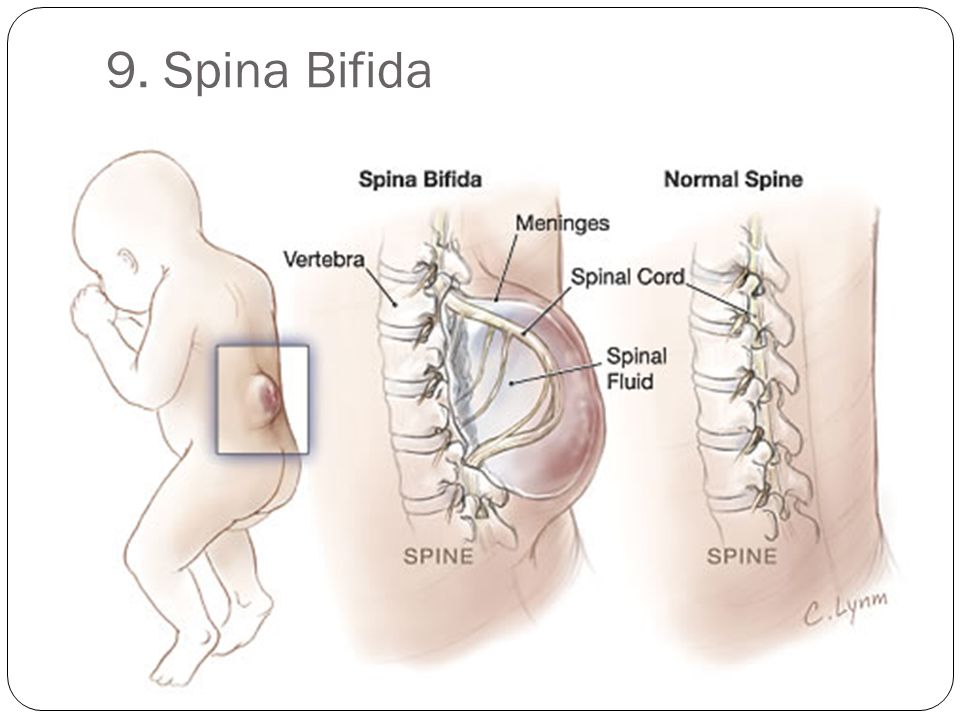
Myelomeningocele is a severe type of spina bifida in which the membranes and the spinal nerves protrude at birth, forming a sac on the baby's back. The exposed nervous system may become infected, so prompt surgery is needed after birth.
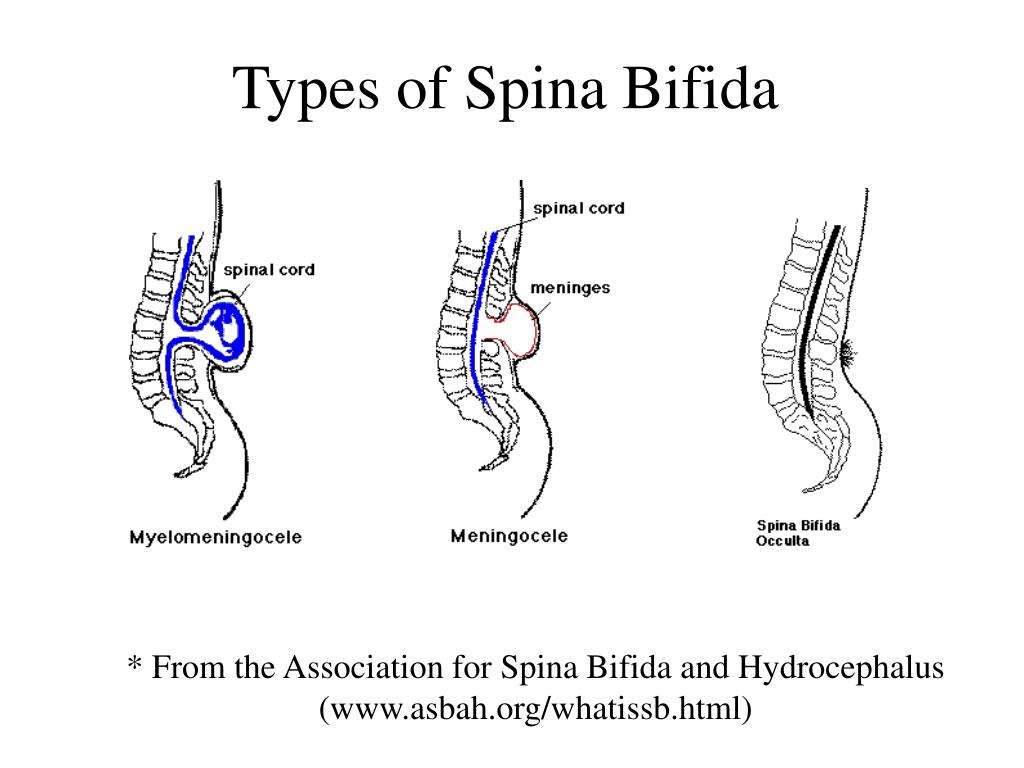
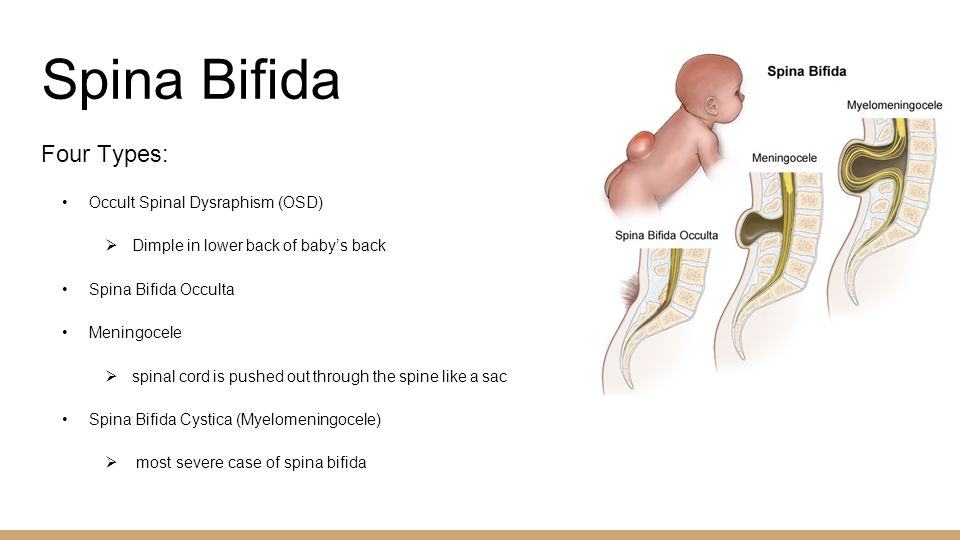
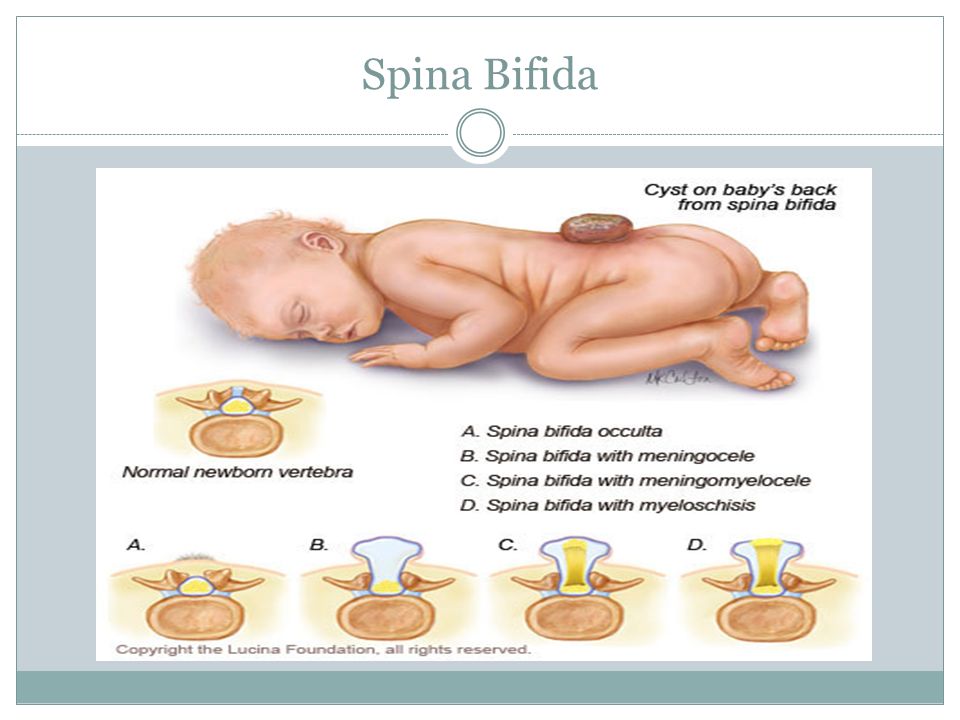
Spina bifida can occur in different types: spina bifida occulta, myelomeningocele (my-uh-lo-muh-NING-go-seel) or the very rare type meningocele (muh-NING-go-seel).
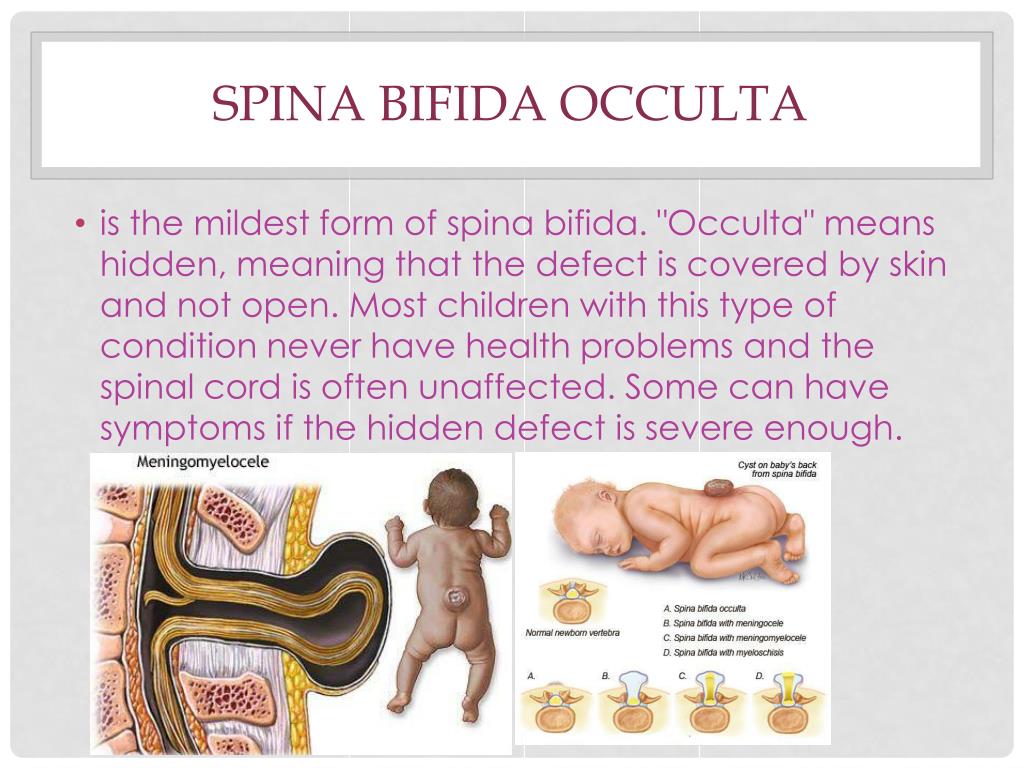
Spina bifida occulta
Occulta means hidden. It's the mildest and most common type. Spina bifida occulta results in a small separation or gap in one or more of the bones of the spine (vertebrae). Many people who have spina bifida occulta don't even know it, unless the condition is discovered during an imaging test done for unrelated reasons.
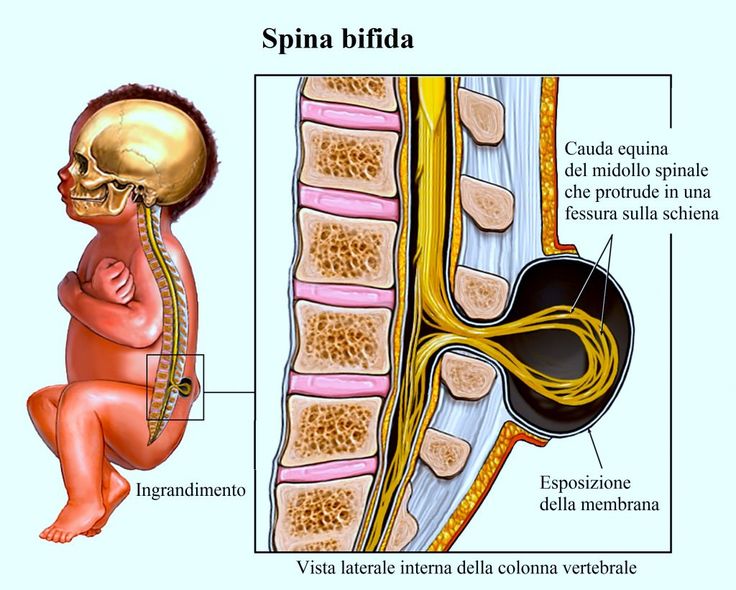
Myelomeningocele
Also known as open spina bifida, myelomeningocele is the most severe type. The spinal canal is open along several vertebrae in the lower or middle back. The membranes and spinal nerves push through this opening at birth, forming a sac on the baby's back, typically exposing tissues and nerves. This makes the baby prone to life-threatening infections and may also cause paralysis and bladder and bowel dysfunction.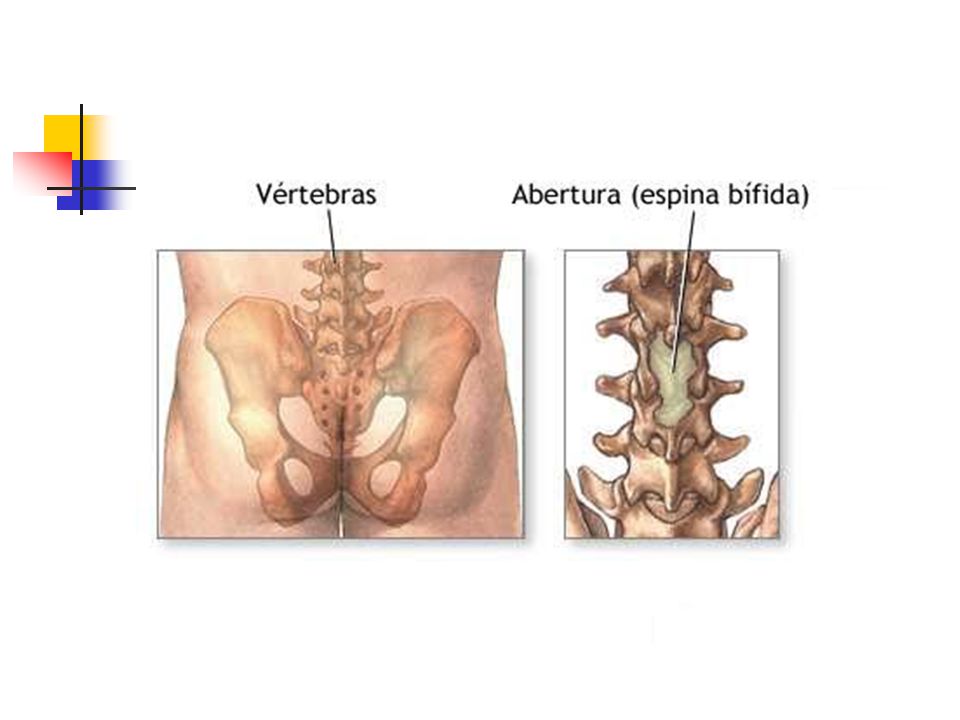
Meningocele
This rare type of spina bifida is characterized by a sac of spinal fluid bulging through an opening in the spine. No nerves are affected in this type, and the spinal cord isn't in the fluid sac. Babies with meningocele may have some minor problems with functioning, including those affecting the bladder and bowels.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Signs and symptoms of spina bifida vary by type and severity, and also between individuals.
- Spina bifida occulta. Typically, there aren't any signs or symptoms because the spinal nerves aren't involved. But you can sometimes see signs on the newborn's skin above the spinal problem, including a tuft of hair, a small dimple or a birthmark. Sometimes, these skin marks can be signs of an underlying spinal cord issue that can be discovered with MRI or spinal ultrasound in a newborn.
- Meningocele. This type may cause problems with bladder and bowel function.
- Myelomeningocele. In this severe type of spina bifida:
- The spinal canal remains open along several vertebrae in the lower or middle back
- Both the membranes and the spinal cord or nerves protrude at birth, forming a sac
- Tissues and nerves usually are exposed, though sometimes skin covers the sac
When to see a doctor
Typically, myelomeningocele is diagnosed before or right after birth, when medical care is available. Children diagnosed with this condition should be followed by a specialized team of health care providers throughout their lives. Families should be educated on the different complications to watch for.
Children with spina bifida occulta typically don't have any symptoms or complications, so usually only routine pediatric care is needed.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.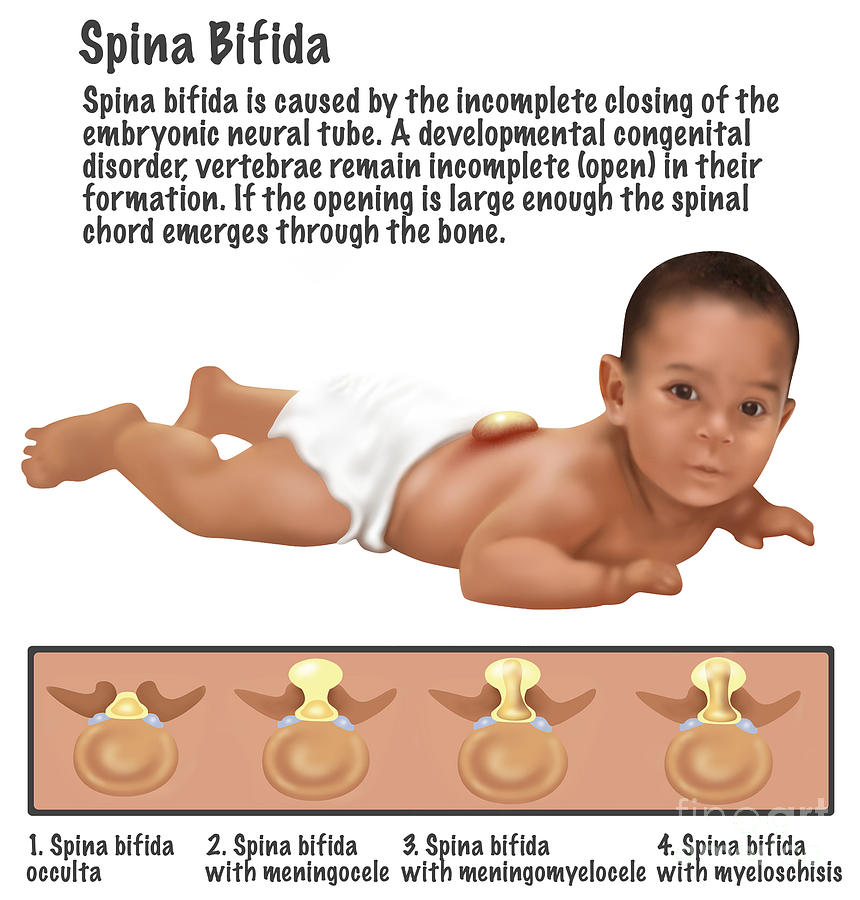
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
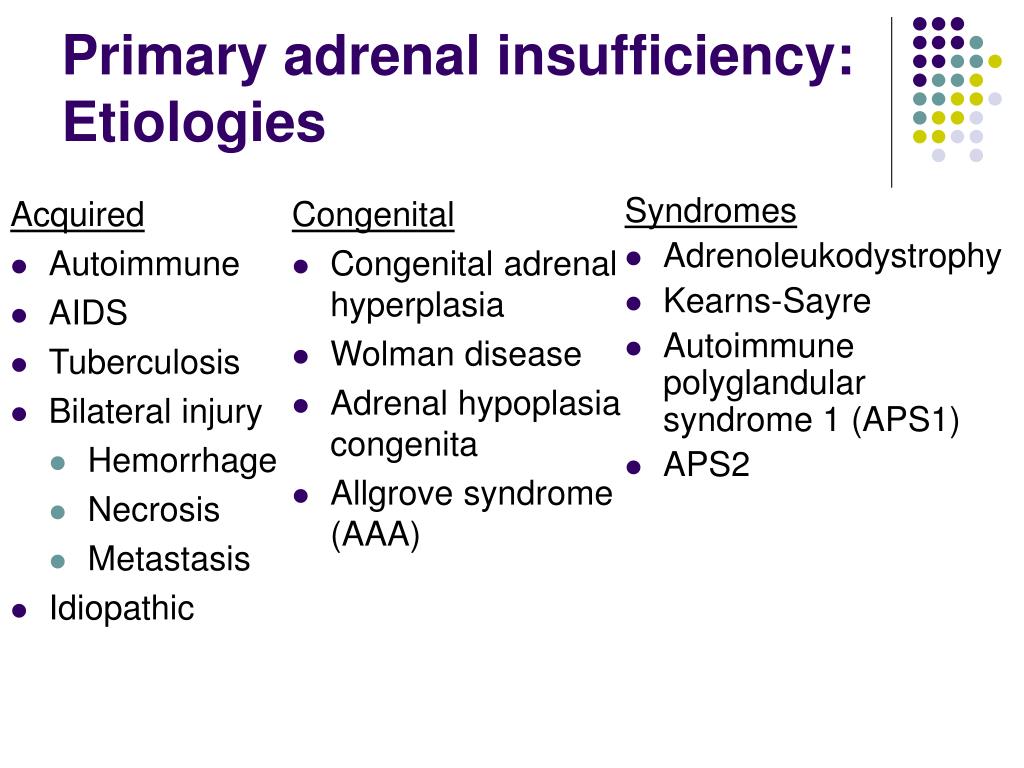
Doctors aren't certain what causes spina bifida. It's thought to result from a combination of genetic, nutritional and environmental risk factors, such as a family history of neural tube defects and folate (vitamin B-9) deficiency.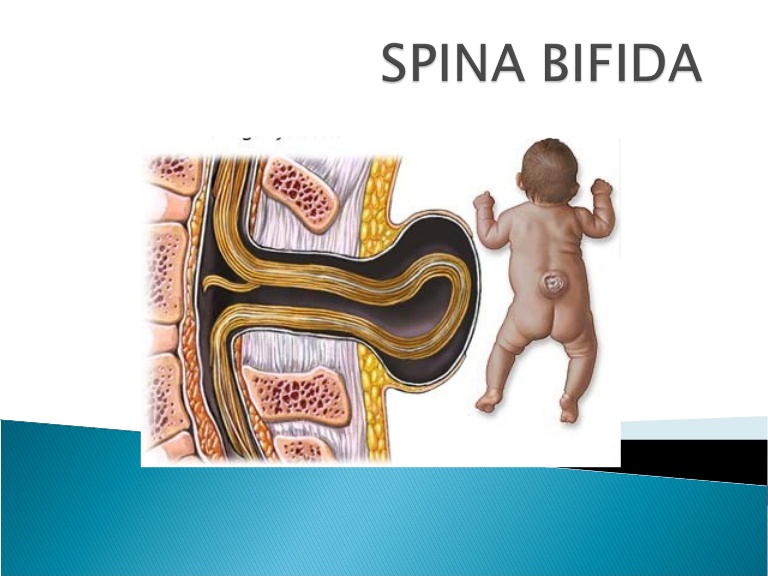
Risk factors
Spina bifida is more common among white people and Hispanics, and females are affected more often than males. Although doctors and researchers don't know for sure why spina bifida occurs, they have identified some risk factors:
- Folate deficiency. Folate, the natural form of vitamin B-9, is important to the development of a healthy baby. The synthetic form, found in supplements and fortified foods, is called folic acid. A folate deficiency increases the risk of spina bifida and other neural tube defects.
- Family history of neural tube defects. Couples who've had one child with a neural tube defect have a slightly higher chance of having another baby with the same defect. That risk increases if two previous children have been affected by the condition. In addition, women who were born with a neural tube defect have a greater chance of giving birth to a child with spina bifida than someone who doesn't have a neural tube defect.
 However, most babies with spina bifida are born to parents with no known family history of the condition.
However, most babies with spina bifida are born to parents with no known family history of the condition. - Some medications. For example, anti-seizure medications, such as valproic acid seem to cause neural tube defects when taken during pregnancy. This might happen because they interfere with the body's ability to use folate and folic acid.
- Diabetes. Women with diabetes who don't have well-controlled blood sugar have a higher risk of having a baby with spina bifida.
- Obesity. Pre-pregnancy obesity is associated with an increased risk of neural tube birth defects, including spina bifida.
- Increased body temperature. Some evidence suggests that increased body temperature (hyperthermia) in the early weeks of pregnancy may increase the risk of spina bifida. Increases in core body temperature, due to fever or use of a sauna or hot tub, have been associated with a slightly increased risk of spina bifida.

If you have known risk factors for spina bifida, talk with your doctor to determine if you need a larger dose or prescription dose of folic acid, even before a pregnancy begins.
If you take medications, tell your doctor. If you plan ahead, some medications can be adjusted to diminish the potential risk of spina bifida.
Complications
Spina bifida may cause minimal symptoms or minor physical problems. But severe spina bifida can lead to more significant physical conditions. Severity is affected by:
- The size and location of the neural tube defect
- Whether skin covers the affected area
- Which spinal nerves come out of the affected area of the spinal cord
This list of possible complications may seem overwhelming, but not all children with spina bifida get all of these complications. Many of these complications can be treated.
- Walking and mobility problems. The nerves that control the leg muscles don't work properly below the area of the spina bifida defect.
 This can cause muscle weakness of the legs and sometimes paralysis. Whether a child can walk typically depends on where the defect is, its size, and the care received before and after birth.
This can cause muscle weakness of the legs and sometimes paralysis. Whether a child can walk typically depends on where the defect is, its size, and the care received before and after birth. - Orthopedic complications. Children with myelomeningocele can have a variety of problems in the legs and spine because of weak muscles in the legs and back. The types of problems depend on the location of the defect. Possible problems include orthopedic issues such as:
- Curved spine (scoliosis)
- Abnormal growth
- Dislocation of the hip
- Bone and joint deformities
- Muscle contractures
- Bowel and bladder problems. Nerves that supply the bladder and bowels usually don't work properly when children have myelomeningocele. This is because the nerves that supply the bowel and bladder come from the lowest level of the spinal cord.
- Accumulation of fluid in the brain (hydrocephalus).
 Babies born with myelomeningocele commonly experience accumulation of fluid in the brain, a condition known as hydrocephalus.
Babies born with myelomeningocele commonly experience accumulation of fluid in the brain, a condition known as hydrocephalus. - Shunt malfunction. Shunts placed in the brain to treat hydrocephalus can stop working or become infected. Warning signs may vary. Some of the warning signs of a shunt that isn't working include:
- Headaches
- Vomiting
- Sleepiness
- Irritability
- Swelling or redness along the shunt
- Confusion
- Changes in the eyes (fixed downward gaze)
- Trouble feeding
- Seizures
- Chiari malformation type II. Chiari malformation (kee-AH-ree mal-for-MAY-shun) type 2 is a common problem with the brain in children who have the myelomeningocele type of spina bifida. The brainstem is the lowest part of the brain above the spinal cord. In Chiari malformation type 2, the brainstem is elongated and positioned lower than usual.
 This can cause problems with breathing and swallowing. Rarely, compression on this area of the brain occurs and surgery is needed to relieve the pressure.
This can cause problems with breathing and swallowing. Rarely, compression on this area of the brain occurs and surgery is needed to relieve the pressure. - Infection in the tissues surrounding the brain (meningitis). Some babies with myelomeningocele may develop meningitis, an infection in the tissues surrounding the brain. This potentially life-threatening infection may cause brain injury.
- Tethered spinal cord. Tethered spinal cord results when the spinal nerves bind to the scar where the defect was closed surgically. The spinal cord is less able to grow as the child grows. This progressive tethering can cause loss of muscle function to the legs, bowel or bladder. Surgery can limit the degree of disability.
- Sleep-disordered breathing. Both children and adults with spina bifida, particularly myelomeningocele, may have sleep apnea or other sleep disorders. Assessment for a sleep disorder in those with myelomeningocele helps detect sleep-disordered breathing, such as sleep apnea, which warrants treatment to improve health and quality of life.
- Skin problems. Children with spina bifida may get wounds on their feet, legs, buttocks or back. They can't feel when they get a blister or sore. Sores or blisters can turn into deep wounds or foot infections that are hard to treat. Children with myelomeningocele have a higher risk of wound problems in casts.
- Latex allergy. Children with spina bifida have a higher risk of latex allergy, an allergic reaction to natural rubber or latex products. Latex allergy may cause rash, sneezing, itching, watery eyes and a runny nose. It can also cause anaphylaxis, a potentially life-threatening condition in which swelling of the face and airways can make breathing difficult. So it's best to use latex-free gloves and equipment at delivery time and when caring for a child with spina bifida.
- Other complications. More problems may arise as children with spina bifida get older, such as urinary tract infections, gastrointestinal (GI) disorders and depression.
 Children with myelomeningocele may develop learning disorders, such as problems paying attention, and difficulty learning reading and math.
Children with myelomeningocele may develop learning disorders, such as problems paying attention, and difficulty learning reading and math.
Prevention
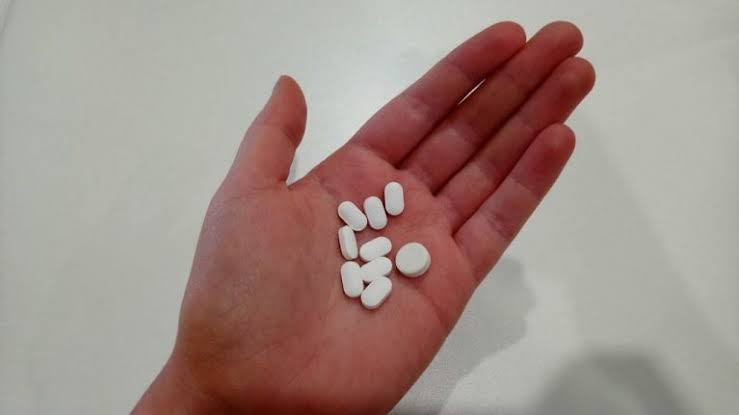
Folic acid, taken in supplement form starting at least one month before conception and continuing through the first trimester of pregnancy, greatly reduces the risk of spina bifida and other neural tube defects.
Get folic acid first
Having enough folic acid in your system by the early weeks of pregnancy is critical to prevent spina bifida. Because many women don't discover that they're pregnant until this time, experts recommend that all women of childbearing age take a daily supplement of 400 micrograms (mcg) of folic acid.
Several foods are fortified with 400 mcg of folic acid per serving, including:
- Enriched bread
- Pasta
- Rice
- Some breakfast cereals
Folic acid may be listed on food packages as folate, which is the natural form of folic acid found in foods.
Planning pregnancy
Adult women who are planning pregnancy or who could become pregnant should be advised to get 400 to 800 mcg of folic acid a day.
Your body doesn't absorb folate as easily as it absorbs synthetic folic acid, and most people don't get the recommended amount of folate through diet alone, so vitamin supplements are necessary to prevent spina bifida. And it's possible that folic acid will also help reduce the risk of other birth defects, including cleft lip, cleft palate and some congenital heart defects.
It's also a good idea to eat a healthy diet, including foods rich in folate or enriched with folic acid. This vitamin is present naturally in many foods, including:
- Beans and peas
- Citrus fruits and juices
- Egg yolks
- Milk
- Avocados
- Dark green vegetables, such as broccoli and spinach
When higher doses are needed
If you have spina bifida or if you've previously given birth to a child with spina bifida, you'll need extra folic acid before you become pregnant. If you're taking anti-seizure medications or you have diabetes, you may also benefit from a higher dose of this B vitamin. Check with your doctor before taking additional folic acid supplements.
If you're taking anti-seizure medications or you have diabetes, you may also benefit from a higher dose of this B vitamin. Check with your doctor before taking additional folic acid supplements.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
What is Spina Bifida? Resources and Prevention
Spina Bifida is the most common permanently disabling birth defect that is associated with life. Approximately 166,000 individuals in the United States have Spina Bifida.
It’s a type of neural tube defect (NTD) that occurs when a baby’s neural tube fails to develop or close properly – the literal meaning for Spina Bifida is “split spine.” Typically occurring within the first 28 days of pregnancy while the neural tube is forming, Spina Bifida often occurs before a woman knows she is pregnant.
Commonly referred to as the “snowflake condition” of birth defects because no two cases are the same, Spina Bifida can range from mild to severe. The severity depends on everything from the size of the opening to the location on the spine.
The severity depends on everything from the size of the opening to the location on the spine.
What Causes Spina Bifida?
No one knows for sure. Doctors and scientists believe that a complex mix of both genetic and environmental factors act together to cause the condition. Are you an expectant parent? Click here for resources and information that might be of benefit to you.
Can Spina Bifida Be Detected Before Birth?
Yes. There are three tests, but, it is important to remember that no medical test is perfect and the results are not always 100 percent accurate. Spina Bifida can be detected in utero by one of the following tests:
- A blood test during the 16th to 18th weeks of pregnancy. This is called the alpha-fetoprotein (AFP screening test). This test is higher in about 75–80 percent of women who have a fetus with Spina Bifida.
- An ultrasound of the fetus. This is also called a sonogram and can show signs of Spina Bifida such as the open spine.

- A test where a small amount of the fluid from the womb is taken through a thin needle. This is called maternal amniocentesis and can be used to look at protein levels.
Types of Spina Bifida
The three most common types of Spina Bifida are:
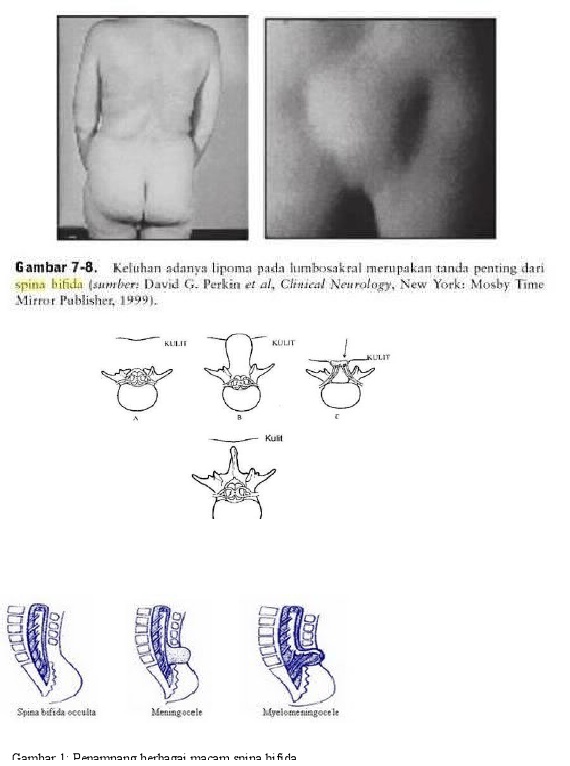
Spina Bifida Occulta
It is often called “hidden Spina Bifida” because about 15 percent of healthy people have it and do not know it. Spina Bifida Occulta (SBO) usually does not cause harm, and has no visible signs. The spinal cord and nerves are usually fine. People find out they have it after having an X-ray of their back. It is considered an incidental finding because the X-Ray is normally done for other reasons. However, in a small group of people with SBO, pain and neurological symptoms may occur. Tethered cord can be an insidious complication that requires investigation by a neurosurgeon.
Meningocele
Meningocele causes part of the spinal cord to come through the spine like a sac that is pushed out.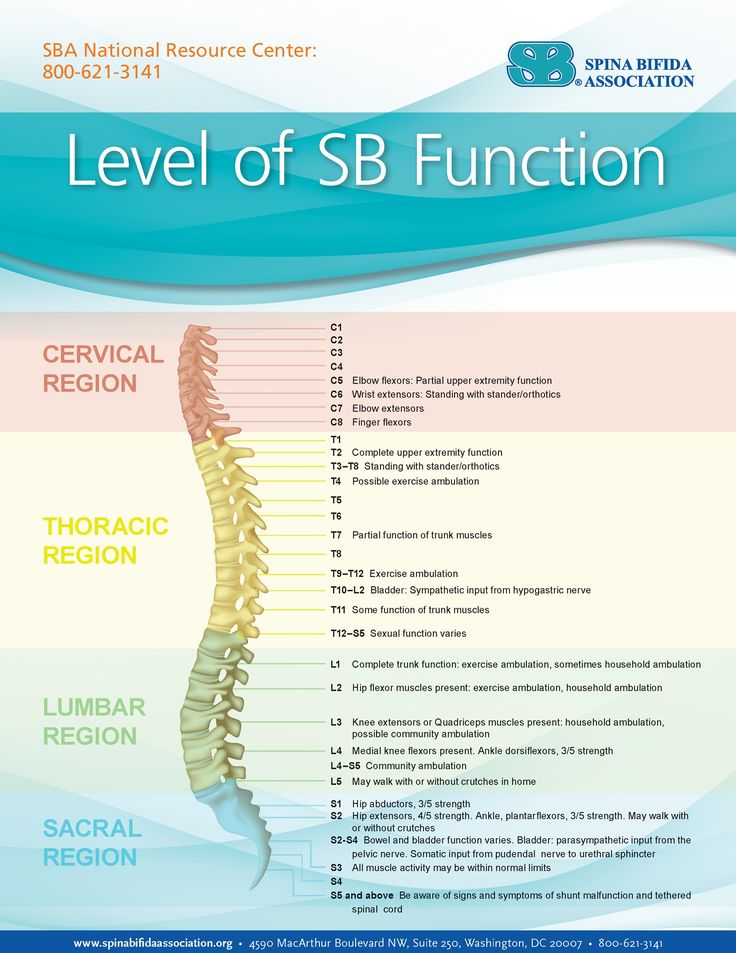 Nerve fluid is in the sac, and there is usually no nerve damage. Individuals with this condition may have minor disabilities.
Nerve fluid is in the sac, and there is usually no nerve damage. Individuals with this condition may have minor disabilities.
Myelomeningocele (Meningomyelocele), also called Spina Bifida Cystica
This is the most severe form of Spina Bifida. It happens when parts of the spinal cord and nerves come through the open part of the spine. It causes nerve damage and other disabilities. Seventy to ninety percent of children with this condition also have too much fluid on their brains. This happens because fluid that protects the brain and spinal cord is unable to drain like it should. The fluid builds up, causing pressure and swelling. Without treatment, a person’s head grows too big, and may have brain damage. Children who do not have Spina Bifida can also have this problem, so parents need to check with a doctor.
Other variations of Spina Bifida include:
How is Spina Bifida treated?
Treatment for Spina Bifida depends on the severity of the condition. Below are the ways in which Spina Bifida is treated before or shortly after birth.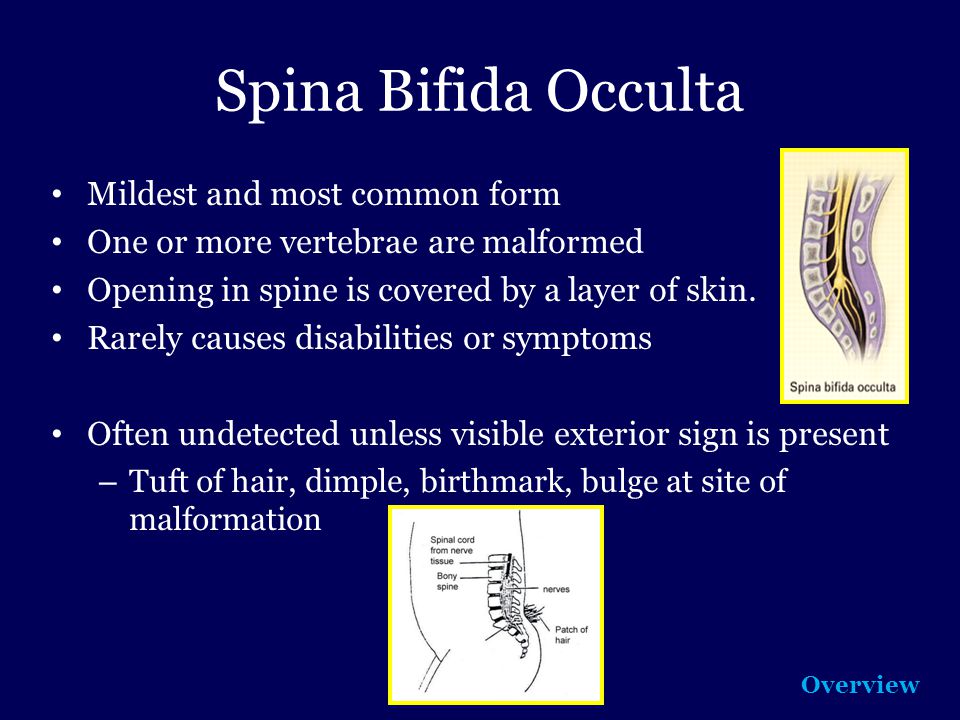
-
-
- A child with Meningomyelocele usually is operated on within two to three days of birth. This prevents infections and helps save the spinal cord from more damage.
- A child with Meningocele usually is treated with surgery, and more often than not, the child is not paralyzed. Most children with this condition grow up without complications, but they should be checked by a doctor because they could have other serious problems, too.
- A child with OSD should see a surgeon. Most experts think that surgery is needed early to keep nerves and the brain from becoming more damaged as the child grows.
- Spina Bifida Occulta typically does not require treatment.
-
Prevention
While there is no known cause, it has been shown that women who are old enough to have babies should take folic acid before and during the first three months of pregnancy. Because half of the pregnancies in the United States are unplanned, the Spina Bifida Association asks women to take a vitamin with 400 mcg (0. 4 mg) of folic acid each day during the years of their lives when they are possibly able to have children.
4 mg) of folic acid each day during the years of their lives when they are possibly able to have children.
Additionally, women who have a child or sibling with Spina Bifida, have had an affected pregnancy, or have Spina Bifida themselves should take 4000 mcg (4.0 mg) of folic acid for one to three months before and during the first three months of pregnancy. Research shows the likelihood of having a second baby with Spina Bifida is about three percent. It’s important to know that neural tube defects like Spina Bifida are not entirely understood, and Spina Bifida is not something that is caused by the actions of the parents. It is recommended that adults with Spina Bifida and couples who already have a child with Spina Bifida talk with their OB-GYN or genetic counselor about their risk factors and ways to reduce the risk.
Resources
Seeking additional information? Contact our National Resource Center at [email protected].
Spina bifida (spina bifida) - treatment, symptoms, causes, diagnosis
Spina bifida (spina bifida) is a complex congenital defect in the development of the spinal cord and spine. This is a type of open neural tube defect in which there is an abnormal development of the back of the spine, the spinal cord, the surrounding nerves, and/or the fluid-filled sac that surrounds the spinal cord.
This is a type of open neural tube defect in which there is an abnormal development of the back of the spine, the spinal cord, the surrounding nerves, and/or the fluid-filled sac that surrounds the spinal cord.
Spina bifida (back bifida) is an incurable, life-long condition that affects the neuromuscular and musculoskeletal systems.
This defect varies by type and ranges from moderate to severe.
Children with this defect may need corsets as the body grows, and in severe cases, a wheelchair.
Treatment is mainly aimed at slowing down the deformity and maintaining motor activity.
The defect may occur along the entire length of the spine and may present as part of the spinal cord and surrounding tissues protruding outward rather than inward. Approximately 85 percent of defects occur in the lower back and 15 percent in the neck and thoracic region. Surgically, it is possible to restore the integrity of the spinal column, but nerve damage cannot be restored, and if they are pronounced, then patients have various degrees of paresis of the lower extremities.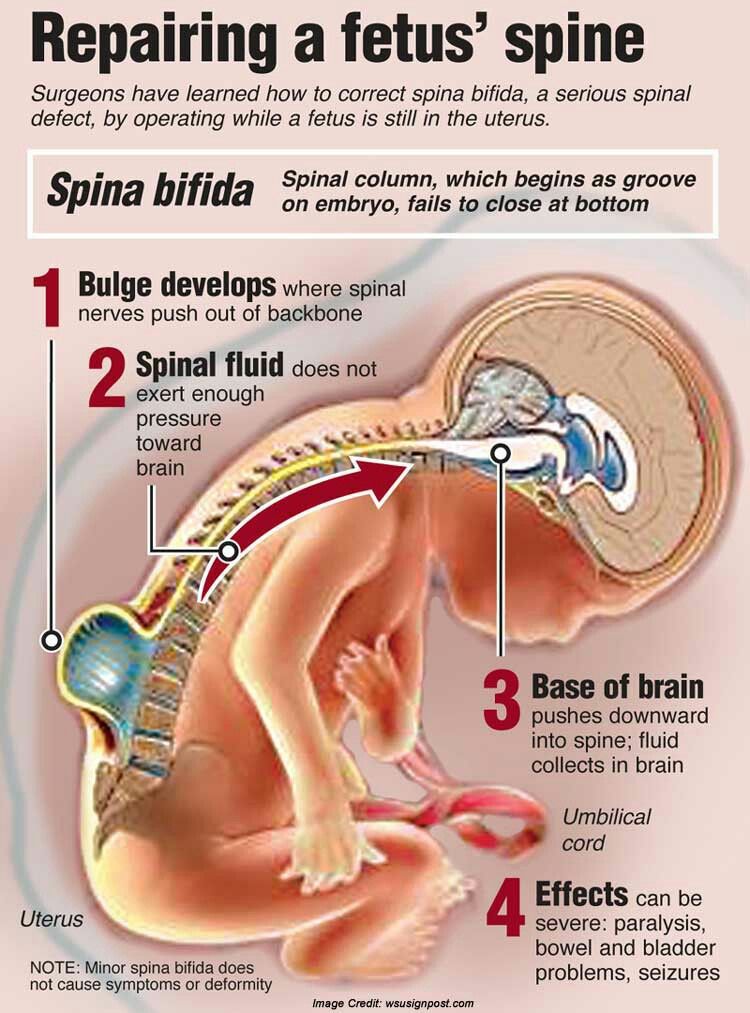 The higher the defect on the spinal column, the more severe the nerve damage and movement disorders (paresis and paralysis).
The higher the defect on the spinal column, the more severe the nerve damage and movement disorders (paresis and paralysis).
According to studies, this developmental anomaly occurs in 7 cases per 10,000 newborns. There are several types of spina bifida that have varying degrees of severity.
- Latent spina bifida (spina bifida occulta) - the most moderate form, in which there are no obvious signs of malformation and changes in the skin. In this form, at least one vertebra changes, but the nerves and spinal cord do not bulge. A child at birth may have a spot or depression in the area of the anomaly. And usually, the baby will not have symptoms. With this form of anomaly (as well as with others), there may be an anomaly in the development of the spinal cord, characterized by attachment of the spinal cord to the spine to the end of the lumbar region, when normally the spinal cord ends at the level of the first lumbar vertebrae and sags freely without attachment to the spine.

- Meningocele is a moderate (and the most common) anomaly in which the spinal canal is not properly closed and the meninges (membranes that cover the spinal cord) bulge outside the bony structures of the spinal canal, but the spinal cord itself remains intact. The cystic mass is covered with skin. Most children with meningocele have normal limb function, but may have partial paresis or abnormalities of the bladder or bowel. With this anomaly, there is often underdevelopment of the spinal cord. Almost all patients with this anomaly require surgery to close the defect and free the spinal cord.
- Lipomeningocele is an anomaly in which fatty tissue is attached to the spinal cord and puts pressure on it. Children with this form of anomaly may not have severe nerve damage, but bladder and bowel function may be impaired. In these cases, surgical treatment is also often used.
- Myelomeningocele: the most severe common form and associated with spina bifida. The spinal canal is not closed, and the bulging mass consists of the meninges, pathologically altered spinal cord, and nerves.
 In addition, in this area the skin is also underdeveloped. In children with this form of spinal cord splitting, paresis below the defect and dysfunction of the pelvic organs are observed in whole or in part. In addition, nerve damage and other pathologies are observed.
In addition, in this area the skin is also underdeveloped. In children with this form of spinal cord splitting, paresis below the defect and dysfunction of the pelvic organs are observed in whole or in part. In addition, nerve damage and other pathologies are observed.
Symptoms
The symptoms of spina bifida vary greatly, depending on the form and severity of the individual child. For example, at birth:
- In latent splitting (spina bifida occulta), there may be no obvious signs or symptoms—only a small spot, depression, or birthmark.
- With a meningocele, there will be a sac-like protrusion that will be located on the back in the spinal region.
- With myelomeningocele, there will also be a protrusion, but with altered skin, there will be a release of nerves and spinal cord.
In severe spina bifida with localization in the lumbar spine, the following symptoms may occur: paralysis of the lower extremities, dysfunction of the bladder, intestines. In addition, these patients usually have other developmental anomalies:
In addition, these patients usually have other developmental anomalies:
- Hydrocephalus occurs in 75 percent of myelomeningocele cases and this condition requires operative endoscopic treatment in order to restore normal CSF flow or a shunt to drain excess fluid from the brain.
- Chiari anomaly (displacement of the brain into the upper cervical vertebrae) can cause pressure on the brainstem, which can manifest as impaired speech, swallowing, and motor disorders in the limbs.
- Underdevelopment of the spinal cord Orthopedic problems including scoliosis, kyphosis, hip dysplasia (congenital dislocation), combined deformities, clubfoot, etc.
- Precocious puberty (especially in girls with spina bifida and hydrocephalus).
- depression and other neurotic conditions
- obesity
- dermatological problems
- developmental anomalies of the urinary tract.
- heart disease
- vision problems
Diagnosis
Diagnosis may be performed during pregnancy to evaluate the fetus for spina bifida.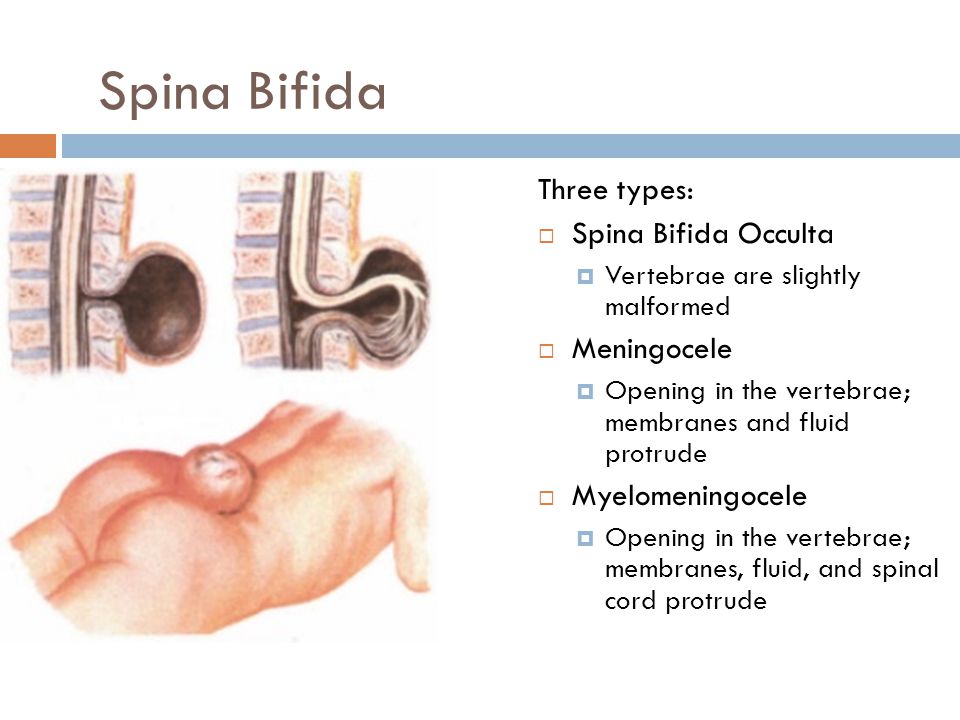 These include:
These include:
- Amniocentesis: A procedure in which a long, thin needle is inserted through the mother's abdomen into the amniotic sac to remove a small amount of amniotic fluid for examination. The fluid is analyzed to determine the presence or absence of an open neural tube defect. Although the analysis is very reliable, it does not allow diagnosing small or closed defects.
- Prenatal ultrasound: this technique, being absolutely harmless, allows you to non-invasively assess the condition and visualize the internal organs, vessels, tissues of the fetus. Sometimes it is possible to diagnose not only spina bifida, but also other anomalies.
- Blood tests: It is recommended that blood tests be performed between 15 and 20 weeks of gestation for all women who have not previously had a child with an open neural tube defect and who have no family history of the condition. A blood test for alpha-fetoprotein and other biochemical parameters can determine how high the risk of developing spinal anomalies is.
- At birth, severe cases of spina bifida are evident by the presence of a fluid-filled sac bulging on the back of the newborn. Visual indicators of mild forms (spina occulta) may be a hairy patch on the skin or a depression along the spine. Unusual weakness or lack of coordination in the lower extremities also suggests spina bifida. In children and adults, this anomaly is often diagnosed during routine studies or, if necessary, to differentiate neurological symptoms using instrumental research methods (MRI, CT, radiography).
Causes
During pregnancy, the human brain and spinal column begin to form as a flat sheet of cells that folds into a tube called the neural tube. If all or part of the neural tube fails to close, then the open area is called an open neural tube defect. An open neural tube is open in 80 percent of cases, and is covered by bone or skin in 20 percent of cases. The cause of spina bifida (spina bifida and other defects) remains unknown, but is most likely the result of a combination of genetic, nutritional, and environmental factors, such as:
- maternal dietary deficiency of folic acid (vitamin B) during pregnancy (sufficient folic acid intake during pregnancy may reduce the risk of this anomaly).
- maternal uncontrolled diabetes
- Certain medicines (antibiotics, anticonvulsants).
- A genetic factor is usually only relevant in 10 percent of cases.
- Mother's age
- What kind of births on the account (firstborns are more at risk).
- Socioeconomic status (children born in lower socioeconomic families are at higher risk).
- ethnicity
- obesity or excessive consumption of alcohol by a pregnant woman
- When exposed to pregnant hyperthermia in the early stages (sauna, jacuzzi).
Treatment
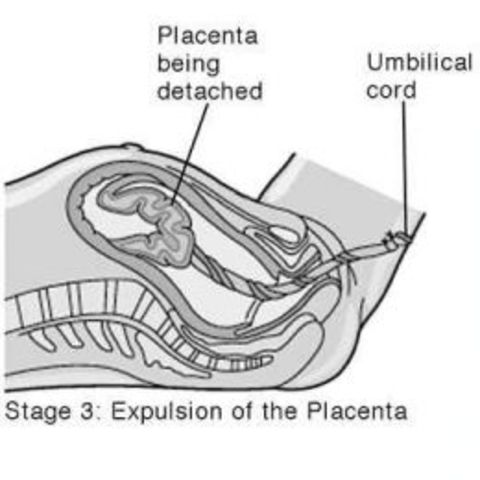
Spina bifida can be treated immediately after birth. If this defect is diagnosed prenatally, then a caesarean section is recommended in order to reduce possible damage to the spinal cord during the passage of the birth canal. Newborns with meningocele or myelomeningocele are recommended to have surgery within 24 hours of birth. With such an operation, the bone defect is closed and it is possible to preserve the function of the intact part of the spinal cord. Unfortunately, surgical treatment cannot restore the function of damaged nerves as they are irreversible.
Unfortunately, surgical treatment cannot restore the function of damaged nerves as they are irreversible.
Currently, there are clinics that perform prenatal surgery to close the defect, but the techniques have not yet found wide application. The main task of treatment, both in a non-severe form and in the postoperative period, is to preserve the functions of both the musculoskeletal system and the functions of the bladder and intestines. If necessary, orthoses, therapeutic exercises, physiotherapy are used.
In cases where spina bifida is detected by chance during X-ray (MRI, CT) examination, measures must be taken to reduce the risk of spinal cord injury in the area of the spine where this defect exists.
Operative treatment in adults is used only in the presence of complications. Basically, treatment in adults is aimed only at preventing possible complications (exercise therapy, physiotherapy, wearing a corset).
What is fetal spina bifida
What should be done to diagnose the causes of spina bifida in a fetus? To solve this problem, the first step for the patient is to make an appointment with an obstetrician-gynecologist.
After the initial examination, the doctor may prescribe additional examinations using:
- ultrasound examination
- ultrasound scan of the brain
- computed tomography of the brain or magnetic resonance imaging of the brain
- ultrasound scan of the bladder
- ultrasound scan of the kidneys.
Spina bifida is a birth defect in which the baby's spine and spinal cord do not develop properly in the womb, causing damage to the spinal column. This pathology of the spine is a type of neural tube defect - the structure that eventually transforms into the brain and spinal cord. The neural tube begins to form early in pregnancy and closes about 4 weeks after conception. In spina bifida, part of the neural tube does not develop or close, resulting in defects in the spinal cord and vertebrae.
Causes of spina bifida
The exact cause of spina bifida is not known, but a number of factors can increase a child's risk of developing the condition.
Folic acid deficiency
Folic acid (also known as vitamin B9) is found naturally in some foods such as broccoli, peas, brown rice, breakfast cereals. All pregnant women, as well as those planning a pregnancy, are recommended to take a mandatory folic acid preparation. It is estimated that taking this vitamin before conception and during pregnancy can prevent up to 7 out of 10 neural tube defects. It is not clear how folic acid helps reduce the risk of spina bifida, but it is likely necessary for important biochemical reactions in the body.
Family history
The presence of neural tube defects in close relatives increases the chances of having a child with spina bifida. Also, if parents previously had a child with this defect, the chances of having other sick children also increase.
Medical factors
Taking certain medications during pregnancy is associated with an increased risk of having a baby with a spina bifida or other birth defects.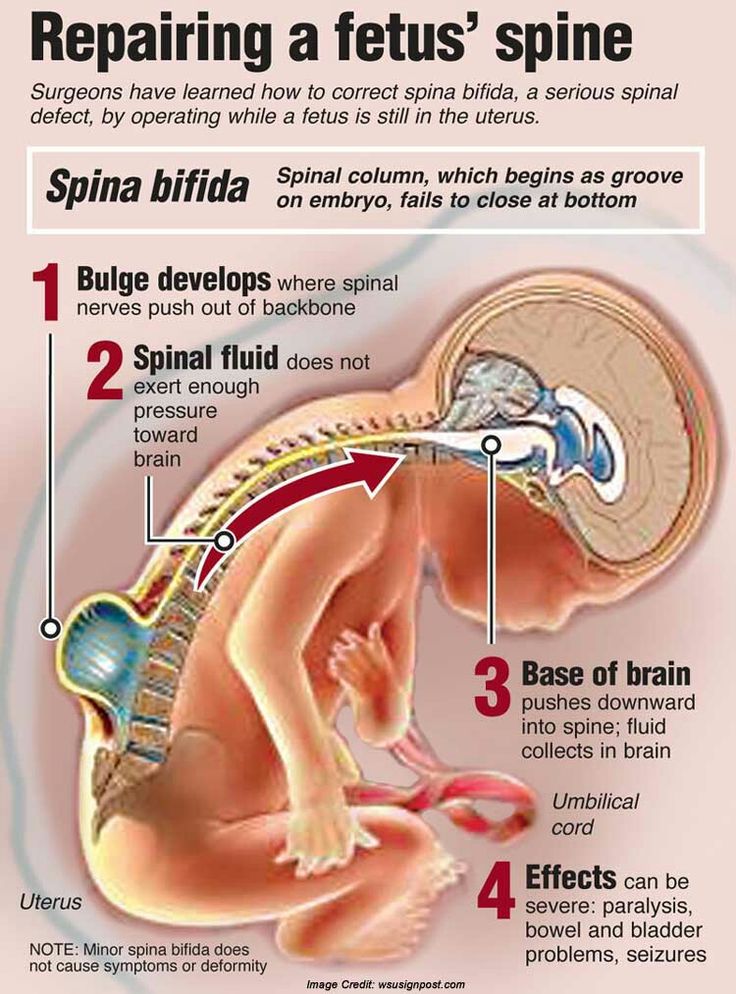 Valproate and carbamazepine are the drugs most commonly associated with spina bifida. They are often used to treat epilepsy and certain mental illnesses such as bipolar disorder. Doctors will try to avoid prescribing these drugs if there is a possibility that a woman may become pregnant while taking them, but they may still be needed if other alternative methods are ineffective. In this case, the specialist will reduce the dose and prescribe folic acid supplements in a large dose.
Valproate and carbamazepine are the drugs most commonly associated with spina bifida. They are often used to treat epilepsy and certain mental illnesses such as bipolar disorder. Doctors will try to avoid prescribing these drugs if there is a possibility that a woman may become pregnant while taking them, but they may still be needed if other alternative methods are ineffective. In this case, the specialist will reduce the dose and prescribe folic acid supplements in a large dose.
Genetic factors
It is very common for a child to have spina bifida in combination with some genetic diseases such as Patau syndrome, Edwards syndrome or Down syndrome.
Other risk factors
Other risk factors for spina bifida include:
obesity - obese women are more likely to have a child with spina bifida than women of average weight; Diabetes - Women with diabetes may have an increased risk of the defect in their children.
Types of spina bifida
There are several different types of spina bifida:
- myelomeningocele is the most severe form of spina bifida, where a child's spinal canal remains open for several vertebrae, allowing the spinal cord and protective membranes around it to bulge out and form a hernial sac ;
- meningocele is another serious type of spina bifida in which the protective membranes of the spinal cord protrude outward through the spine, with the spinal cord usually developing normally;
- spina bifida occulta is the most common and mildest form of spina bifida, in which one or more vertebrae are malformed but the gap in the spine is very small; this type of disease usually does not cause serious problems.
Spina bifida symptoms
Spina bifida can cause a wide range of symptoms, including movement problems, bladder and bowel problems, and hydrocephalus.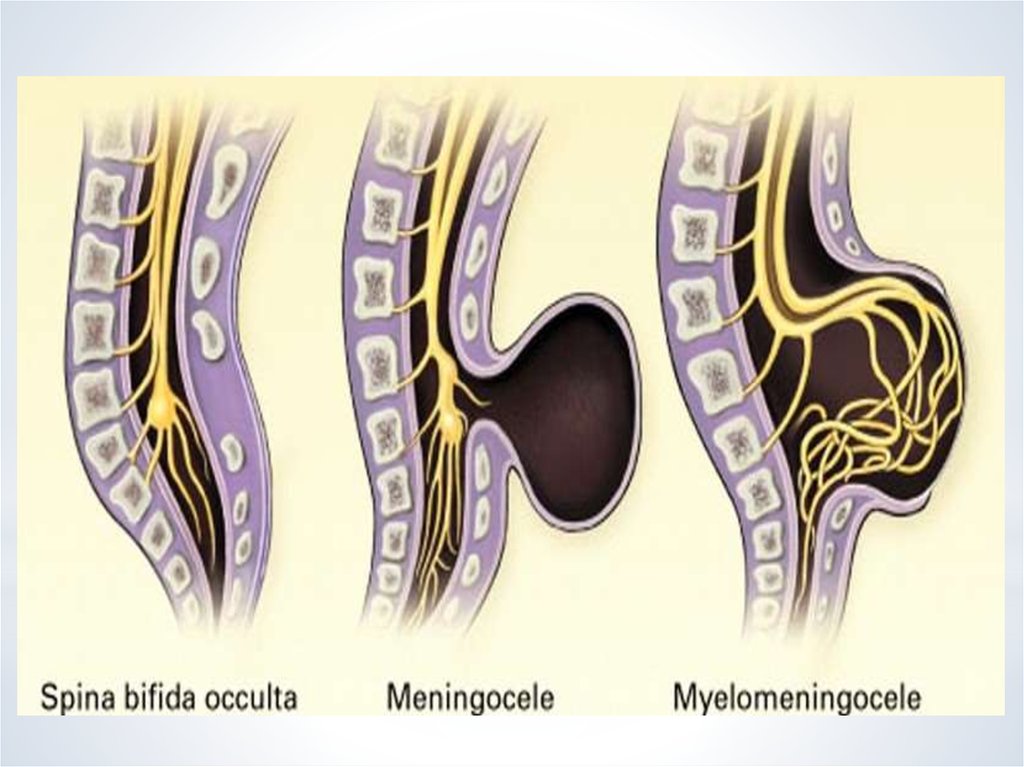 The severity of the symptoms of this anomaly varies significantly, largely depending on the location of the cleft in the spine. An upper spinal defect is more likely to cause leg paralysis and difficulty with mobility than a cleft in the middle or base of the spinal column.
The severity of the symptoms of this anomaly varies significantly, largely depending on the location of the cleft in the spine. An upper spinal defect is more likely to cause leg paralysis and difficulty with mobility than a cleft in the middle or base of the spinal column.
Movement problems
Most children with spina bifida have weakness or paralysis in the lower extremities. They may need to use ankle supports or crutches to get around, or in severe cases they may need a wheelchair. Paralysis can also cause other related problems. For example, if the leg muscles are not used regularly, they can become very weak (atrophy). Muscles support bones, so muscle weakness can in turn cause dislocation or deformity of joints, bone fractures, bone deformity, and abnormal curvature of the spine.
Bladder problems
Many patients with spina bifida have problems urinating. This is caused by improper formation of the nerves that control the bladder and can lead to:
- urinary incontinence;
- urinary tract infections;
- hydronephrosis - when one or both kidneys increase in size due to the accumulation of urine inside them;
- scarring of the kidneys;
- kidney stones.
Bowel problems
The nerves that run through the spinal cord also control bowel movements and the sphincter muscles that keep feces in the bowel. Many people with spina bifida have little or no control of the sphincter muscles. Bowel incontinence often leads to periods of constipation followed by episodes of diarrhea.
Hydrocephalus
Some children with spina bifida have hydrocephalus, an accumulation of excess fluid in the brain that can damage the brain substance and cause further problems. Many patients with hydrocephalus will have normal intelligence, although some will have learning difficulties such as:
- short attention span;
- difficulty in solving problems;
- reading difficulties;
- difficulty understanding spoken language - especially fast conversations between a group of people;
- difficulty organizing events or making detailed plans;
- problems with visual and physical coordination;
- irritability;
- convulsions;
- drowsiness;
- nausea.
In some infants, hydrocephalus causes the lower parts of the brain to move down towards the spinal cord - this is called Arnold-Chiari type 2 malformation.
Other problems
Other problems associated with spina bifida include:
- skin problems - decreased sensation;
- this can make it difficult to determine the location of damage to the skin on the legs in case of burns on the radiator, injuries or infections;
- latex allergy - symptoms can range from a mild allergic reaction (watery eyes and skin rash) to a severe allergic reaction known as anaphylactic shock, which requires immediate medical attention.
Spina Bifida Diagnosis
Spina bifida is often detected during a routine ultrasound scan, which is offered to all pregnant women between 18 and 21 weeks of pregnancy. If a neural tube defect is detected, the woman will be consulted by a medical commission on the possibility of prolonging or terminating the pregnancy.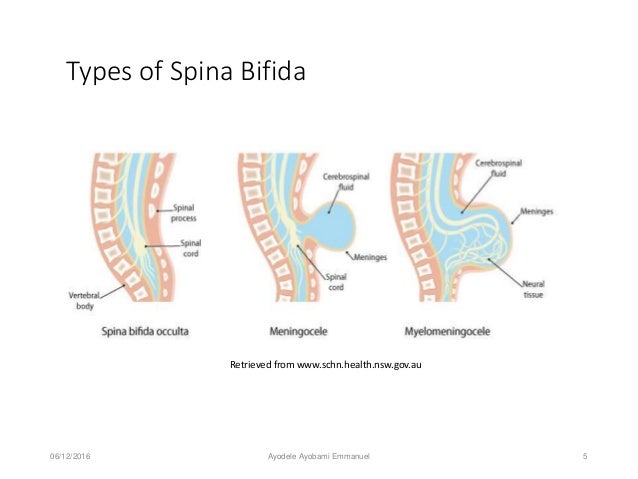
Tests after birth
After the baby is born, a number of additional tests may be done to determine the severity of the condition and choose the most effective treatment. Tests may include:
- monitoring the growth of the child's head and performing an ultrasound scan of the brain;
- ultrasound scan of the bladder
- ultrasound scan of the kidneys;
- assessment of the child's movements for signs of paralysis.
Treatment of spina bifida
Treatment of symptoms or conditions associated with spina bifida includes:
- surgery to close a hole in the spine and treat hydrocephalus;
- methods of treatment that help to facilitate the daily life of the patient;
- mobility aids and equipment;
- treatment of bowel and urinary problems.
With the right treatment and support, many children with spina bifida survive into adulthood.
Primary spinal repair surgery
Babies with a spinal fissure may have tissue and membranes coming out of the hole in the spine, damaging the nerves and can lead to serious infections, so the baby usually has spinal repair surgery within 48 hours of birth.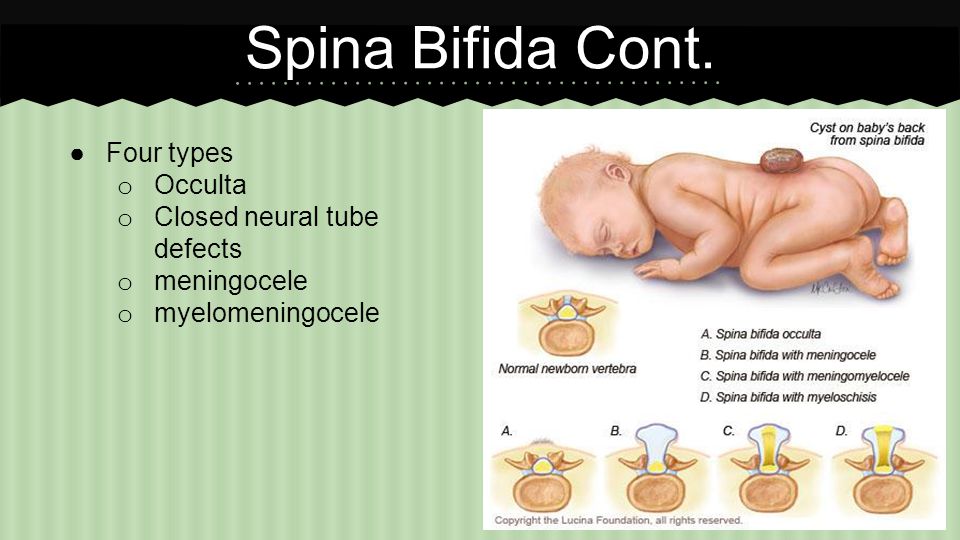 During the operation, the surgeon will return the anatomically correct location of the spinal cord and exposed tissues or nerves, then close the cleft in the spine with muscles and skin. While this will fix the defect, unfortunately it cannot completely fix nerve damage.
During the operation, the surgeon will return the anatomically correct location of the spinal cord and exposed tissues or nerves, then close the cleft in the spine with muscles and skin. While this will fix the defect, unfortunately it cannot completely fix nerve damage.
Treatment of hydrocephalus
To surgically treat hydrocephalus, a surgeon implants a thin tube (shunt) to drain excess fluid from the brain to another part of the body, usually the abdomen. The shunt most often remains in place for the rest of the child's life. Further surgery may be required if:
- the shunt is blocked or infected;
- the child is growing out of the shunt and needs a larger size.
Physiotherapy
Physiotherapy is a method of treatment aimed at helping the patient to move, prevent deformity and stop further weakening of the leg muscles. It may include daily exercise to maintain muscle tone, as well as the wearing of special splints to support the legs.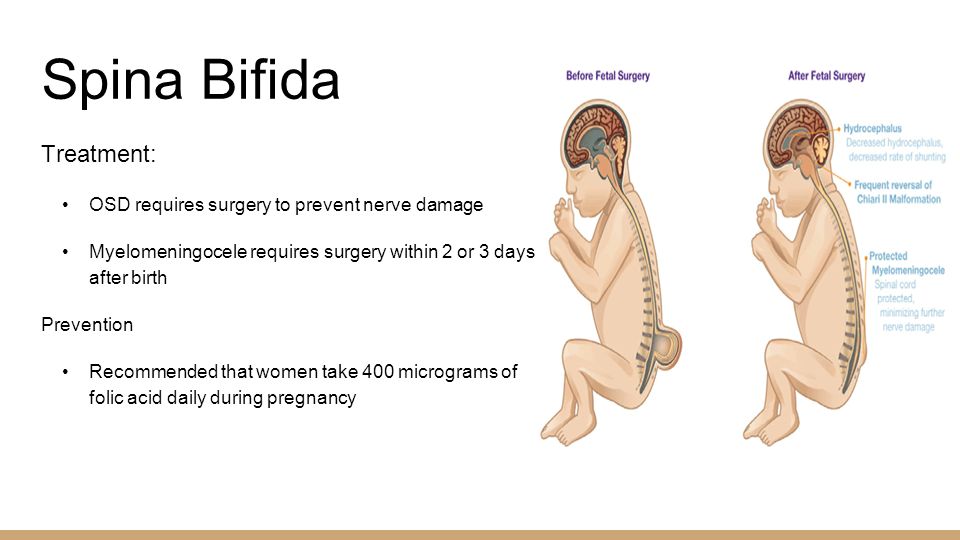
Treatment for bladder problems
Treatment for bladder problems includes:
- antibiotics - sometimes lifelong antibiotics are needed to prevent kidney and urinary tract infections;
- medicines to help relax the bladder so it can store more urine;
- bladder catheterization - using a catheter to remove urine from the bladder several times a day to prevent urinary stasis and infection;
- bladder surgery - may involve enlarging the bladder so it can hold more urine, or connecting the appendix to the bladder and creating an opening in the abdomen to allow the catheter to be inserted more easily.
Treatment of bowel problems
Treatment of bowel problems includes:
- laxatives - medicines to help empty the bowels;
- suppositories and enemas for constipation;
- colostomy - surgery to retract the end of the large intestine through an opening onto the abdomen;
- A stool bag is attached to the opening.
A colostomy may be recommended if other treatments fail.
Prevention of spina bifida with folic acid
The best way to prevent spina bifida is to take folic acid supplements before and during pregnancy. A woman is usually given a 400 mcg folic acid tablet every day during the planning period and up to 12 weeks of pregnancy. A diet rich in foods containing folic acid is also recommended.
Advice for women at increased risk of spina bifida
Women at increased risk of having a baby with spina bifida should be given a higher (5 mg) dose of folic acid.
Share:
Scientific sources:
- Altynnik H.A. The value of ultrasound assessment of the thickness of the nuchal space of the fetus in early pregnancy for prenatal diagnosis of chromosomal abnormalities: Diss. . cand. honey. Sciences. M., 2002.
- Medvedev M.V., Altynnik H.A. On the issue of ultrasound assessment of fetal anatomy in early pregnancy // Prenat.
 Diagn. 2002. V. 1. No. 2. S. 158-159.
Diagn. 2002. V. 1. No. 2. S. 158-159. - Fundamentals of prenatal diagnosis / Ed. Yudina E.V., Medvedeva M.V. M.: RAVUZDPG, Realnoe Vremya, 2002. 184 p.
- Sinitsin, V.E.: Magnetic resonance angiography of today. The level of development and new opportunities / V.E. Sinitsin, E.A. Timonina, O.V. Stukalova // Med. visualization. - 1996. - No. 4. - S. 36-44.
- Turkin A.M. MRI in the diagnosis of the brain. Diss. candidate of medical sciences - M., 1990.-158 p.
Useful information
Hemolytic disease of the fetus
What should be done to diagnose the causes of fetal hemolytic disease (erythroblastosis, Rh incompatibility)? To solve this problem, the first step for the patient is to make an appointment with an obstetrician-gynecologist. After the initial examination, the doctor may prescribe additional examinations: Blood test Checking the child's blood type.
read more +
female infertility
What needs to be done to diagnose and treat female infertility? To solve this problem, the first step for the patient is to make an appointment with a gynecologist.