Yeast infection common in early pregnancy
Yeast Infections During Pregnancy - American Pregnancy Association
Yeast infections during pregnancy are more common than any other time in a woman’s life, especially during the second trimester of pregnancy. You may be noticing an increase in the amount of thin, white, odd smelling discharge. This is common and a normal symptom in the second trimester.
If you think you may be experiencing a yeast infection, the following information will prepare you to discuss the possibility with your doctor. Though yeast infections have no major negative effect on pregnancy, they are often more difficult to control during pregnancy, causing significant discomfort for you. Don’t wait to seek treatment!
What is a yeast infection?
Yeast infection occurs when the normal levels of acid and yeast in the vagina are out of balance, which allows the yeast to overgrow causing an uncomfortable, but not serious, a condition called a yeast infection.
If you have never been diagnosed or treated by a physician for a yeast infection and have some of the symptoms, you should see your physician first for accurate diagnosis and treatment. Other infections have similar symptoms, so you want to make sure that you are treating the infection correctly. There are also treatments that are not appropriate during pregnancy.
What causes yeast infections during pregnancy?
A yeast infection can be caused by one or more of the following:
- Hormonal changes that come with pregnancy or before your period
- Taking hormones or birth control pills
- Taking antibiotics or steroids
- High blood sugar, as in diabetes
- Vaginal intercourse
- Douching
- Blood or semen
Why are yeast infections more common during pregnancy?
Your body is going through so many changes right now, and it is difficult for your body to keep up with the chemical changes in the vagina. There is more sugar in vaginal secretions on which the yeast can feed, causing an imbalance which results in too much yeast.
What are the symptoms of yeast infections?
The symptoms of a yeast infection may include one or more of the following:
- Discharge that is usually white/tan in color, similar to cottage cheese and may smell like yeast/bread
- Other discharge may be greenish or yellowish, also similar to cottage cheese and may smell like yeast/bread
- An increase in discharge
- Redness, itching, or irritation of the lips of the vagina
- Burning sensation during urination or intercourse
What else could I be experiencing?
If you are experiencing symptoms similar to a yeast infection, but a physician has ruled this diagnosis out, you may have one of the following:
- Sexually Transmitted Diseases (STDs) like Chlamydia, Gonorrhea, & Trichomoniasis
- A vaginal infection called bacterial vaginosis
How do I know for sure if I have a yeast infection?
At your doctor’s office or medical clinic, a clinician will use a simple, painless swab to remove the discharge or vaginal secretions and examine it through a microscope.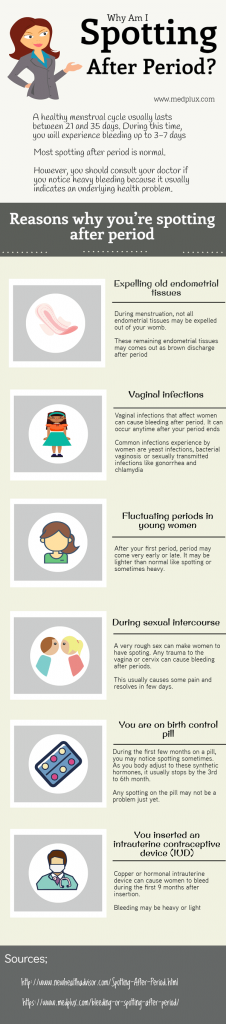 Usually, upon a simple examination of the vagina, a physician can diagnose a yeast infection. In rare cases, the culture may be sent to a lab.
Usually, upon a simple examination of the vagina, a physician can diagnose a yeast infection. In rare cases, the culture may be sent to a lab.
How are yeast infections treated during pregnancy?
During pregnancy, physicians recommend vaginal creams and suppositories only. The oral medication, Diflucan (a single-dose medication), has not been proven safe during pregnancy and lactation. Not all vaginal creams and suppositories are okay to use during pregnancy, so it is best to consult your doctor or pharmacist to get the right one. If left untreated, yeast infections can pass to your baby’s mouth during delivery. This is called “thrush” and is effectively treated with Nystatin.
It may take 10-14 days to find relief or completely clear up the infection while you are pregnant. After the infection has cleared up and any sores have healed, it may be helpful to use a starch-free drying powder, or Nystatin powder to prevent a recurring infection.
How can I prevent a yeast infection or recurring yeast infections?
Most yeast infections can usually be avoided by doing the following:
- Wear loose, breathable cotton clothing and cotton underwear.

- After regular, thorough washing (using unscented, hypoallergenic or gentle soap), use your blow dryer on a low, cool setting to help dry the outside of your genital area.
- Always wipe from front to back after using the restroom.
- Shower immediately after you swim. Change out of your swimsuit, workout clothes, or other damp clothes as soon as possible.
- Do NOT:
- douche
- use feminine hygiene sprays
- use sanitary pads and tampons that contain deodorant
- take a bubble bath/use scented soaps
- use colored or perfumed toilet paper
- Include yogurt with “lactobacillus acidophilus” in your diet.
- Limit sugar intake, as sugar promotes the growth of yeast.
- Get plenty of rest to make it easier for your body to fight infections.
When should I contact my doctor?
If you are experiencing the symptoms described in this article, call your doctor now. Yeast infections have similar symptoms of other infections, such as STDs.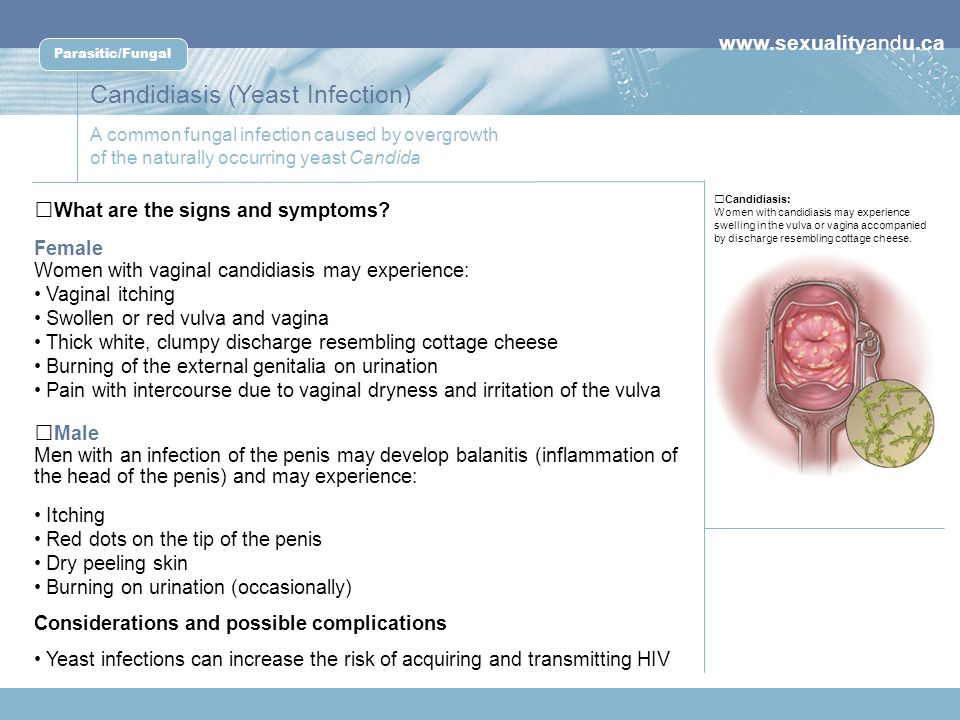 Proper diagnosis every time you experience these symptoms is vital for the most effective, immediate treatment, or your condition may worsen/not go away.
Proper diagnosis every time you experience these symptoms is vital for the most effective, immediate treatment, or your condition may worsen/not go away.
If you see no improvement within three days, or if symptoms worsen or come back after treatment, you should contact your healthcare provider again.
Want to Know More?
- Pregnancy Nutrition
- Medication and Pregnancy
Compiled using information from the following sources:
1. American Academy of Family Physicians
https://familydoctor.org
1. Mayo Clinic Complete Book of Pregnancy & Babys First Year. Johnson, Robert V., M.D., et al, Ch. 11.
Answers to 6 burning questions about yeast infection during pregnancy | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
September 20, 2022
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
D. Obstetrics and Gynecology
Vaginal candidiasis, also known as a yeast infection, can be a real pain. The itching, burning, and discharge can be especially worrisome during pregnancy.
In most cases, though, vaginal yeast infections and most treatment options pose minimal risk to the patient or pregnancy.
After bacterial vaginal infections, yeast infections are the second most common cause of vaginal inflammation, and 75% of women will have at least one in their lifetime. Common symptoms can include redness, itching, or irritation on the external genital area (vulva), an increase in white or tan vaginal discharge, and a burning sensation during urination or intercourse.
There are a range of over-the-counter and prescription treatments, and an Ob/Gyn or gynecologist can help you choose the safest, most effective option during pregnancy.
I’ve invited Meredith McClure, M.D., a UT Southwestern gynecologist, to answer the top questions pregnant and breastfeeding patients ask about yeast infection treatment and prevention.
Meredith McClure, M.D.Q: How common are yeast infections during pregnancy?
A: Studies have found that 20%-30% of women develop a yeast infection during pregnancy. An increase in the hormone estrogen creates a more hospitable climate for yeast to colonize the vagina because it binds to the protein factor H on the surface of the cells that cause vulvovaginal candidiasis.
Some women are more likely to develop yeast infections due to their genetics. Mutations of several genes can interfere with the immune system’s ability to defend against candida yeast, resulting in recurring infections for some people. This inherited predisposition is called familial candidiasis.
This inherited predisposition is called familial candidiasis.
Q: Can a yeast infection harm my pregnancy?
A: No. A yeast infection won’t affect your developing baby – that’s why we don’t treat yeast infections that don’t have symptoms. However, most symptomatic yeast infections get worse when left untreated. This means more itching, redness, and inflammation. If the skin becomes cracked or torn from repeated scratching, a skin infection can result. In rare cases, an untreated yeast infection can lead to fatigue, oral thrush, or digestive problems.
Q: Do yeast infections appear throughout pregnancy?
A: Yeast infections can occur any time, but they are most common during the second trimester. Talk with your doctor if you notice signs of a yeast infection while pregnant, even if you have had one before. Some more serious infections have similar symptoms, so your doctor will perform a simple fungal culture swap in the office to check for the presence of yeast.
Q: What treatment options are available?
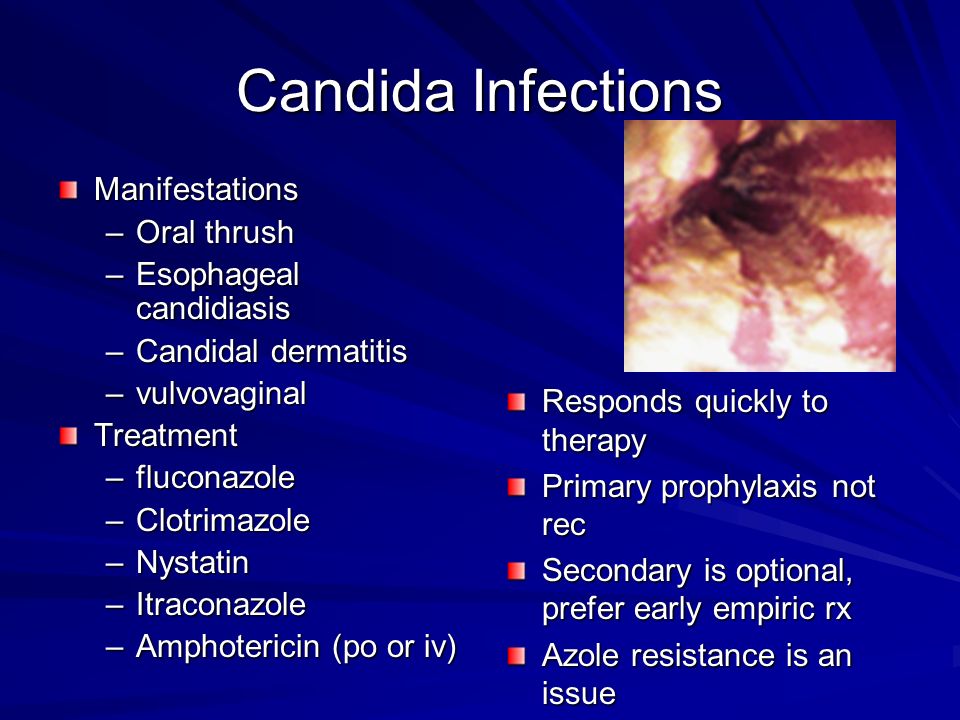
Talk with your doctor about the safest and most effective options for treating yeast infections during pregnancy.A: Topical creams or vaginal suppositories are the recommended yeast infection treatment options during pregnancy or while breastfeeding. Over-the-counter medications such as Miconazole, Clotrimazole, and Terconazole have been shown to eliminate a yeast infection safely and effectively. They are usually applied for three to seven days. It is important to finish the entire course of medication to prevent the infection from coming back. Studies have demonstrated these medications are safe to use during pregnancy.
The oral medication Diflucan (fluconazole) is not recommended for most patients during pregnancy. Though taking a single pill is simpler, quicker, and less messy, some studies suggest fluconazole carries a slightly increased risk of miscarriage, birth defects, or stillbirth, especially at high doses taken over long periods of time.
While the increase is small – approximately 12 incidents per 10,000 births – the convenience of single-pill treatment might not outweigh the risk. However, in the event you have already taken or need to take fluconazole while pregnant, the additional risk at a normal dose is unlikely to pose any problems for your baby.
Q: Are yeast infection treatments safe while breastfeeding?
A: Yeast infections are less common among breastfeeding patients because estrogen levels drop dramatically in the postpartum period, making it hard for yeast to thrive. But if they occur, fluconazole may be taken by women who are breastfeeding as the levels secreted into breast milk are small.
It is possible for a breastfeeding mother and baby to pass thrush, a fungal infection that typically grows in the mouth and throat, back and forth between nipple and mouth. If that happens, both must be treated to stop the infection. Thrush is usually minor and is often caused by the same fungus – and treated with a 7- to 14-day course of the same antifungal medicines – as a yeast infection in the vagina.
Q: What steps can reduce the risk of yeast infection?
A: During pregnancy and otherwise, take the following precautions:
- Wipe front to back after using the toilet.
- Avoid using scented tampons, pads, and pantyliners.
- Change tampons, pads, and pantyliners often.
- Avoid very hot baths and hot tubs.
- Wear underwear with a cotton lining to promote airflow.
- Do not douche, which removes healthy vaginal bacteria that prevent infection.
- Wear loose fitting clothing.
- Manage your blood sugar if you have diabetes or gestational diabetes.
- Remove wet workout clothes and swimsuits as soon as possible after activities.
If you’re pregnant and notice signs of a yeast infection, discuss treatment options with your doctor so you can eliminate these disruptive symptoms. To request an appointment, call 214-645-8300 or request online.
More in: Your Pregnancy Matters
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.
 D.
D.
September 27, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
Your Pregnancy Matters
- Patricia Santiago-Munoz, M.
 D.
D.
August 23, 2022
Mental Health; Your Pregnancy Matters
August 11, 2022
Your Pregnancy Matters
- Emily Adhikari, M.D.
August 2, 2022
Your Pregnancy Matters
- Abey Eapen, M.
 D., Ph.D.
D., Ph.D.
July 26, 2022
More Articles
symptoms, treatment (1st, 2nd, 3rd trimesters)
Did you know that every third woman in the world suffers from candidiasis? At the same time, thrush occurs three times more often in pregnant women. Let's take a look at the causes of thrush together, and also talk about the main symptoms and methods of treating thrush at different stages of pregnancy.
Lyudmila Starichenko
doctor of the highest qualification category,
head doctor of the Clinic of Innovative Technologies
work experience 41 years
learn more on the website
Causes of thrush
Signs and symptoms of thrush in pregnant women
Treatment of thrush in pregnant women
What to avoid when treating thrush?
Why is thrush dangerous during pregnancy?
What if it doesn't go away?
Prevention
Causes of thrush
Thrush or vulvovaginal candidiasis is a common disease of the vaginal mucosa. The main reason for its appearance is a fungal infection.
The main reason for its appearance is a fungal infection.
Pregnant women are at particular risk. After all, in this position, the patient has a natural decrease in immunity, which can even lead to a decrease in local immunity. As a result, the inevitable growth of opportunistic microorganisms occurs. Among them are yeast-like fungi that cause candidiasis. Changes in the hormonal background, namely, an increase in the level of female sex hormones, can also affect the increased growth of yeast-like fungi. This is especially true for patients who have pregnancy complications.
Read more about the causes of candidiasis in our material.
learn more
Signs and symptoms of thrush in pregnancy
The signs and symptoms of thrush in pregnancy are no different from the usual symptoms of thrush. They differ only in what particular organ is affected by thrush.
So, for example, with urogenital candidiasis, the most characteristic symptoms are discharge from the genital tract, itching, burning in the genital area and its intensification during sleep and water procedures.
Treatment of thrush in pregnant women
All medications during pregnancy must be selected by a doctor. Self-treatment is out of the question here, because by wrong actions a woman can harm not only herself, but also her child!
As a rule, only local therapy is prescribed during pregnancy at any time.
First trimester
In the first trimester, use Natamycin 100 mg intravaginally for 6 days. The drug refuses fungicidal and antifungal action.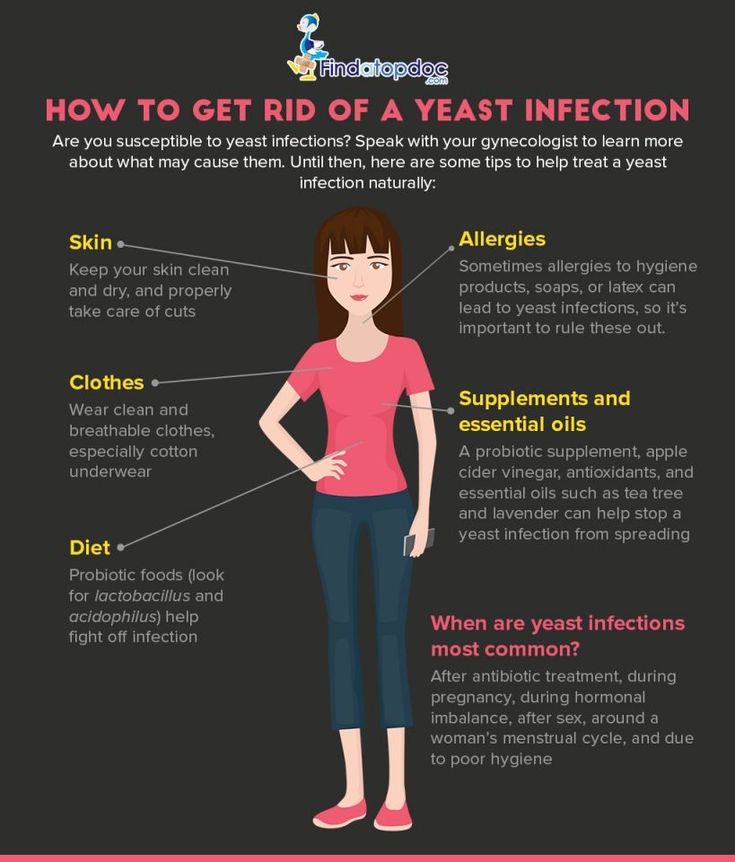 Thanks to the active substance, it binds to the sterols of the cell membrane of the fungus and disrupts its permeability. This leads to the destruction of the fungal cell as a result of damage or rupture of the membrane.
Thanks to the active substance, it binds to the sterols of the cell membrane of the fungus and disrupts its permeability. This leads to the destruction of the fungal cell as a result of damage or rupture of the membrane.
Natamycin is active against most yeast-like fungi, and especially against fungi of the genus Candida. The advantage of this drug is that it does not have a systemic effect and is not absorbed into the gastrointestinal tract, acting only locally on the damaged mucous membrane. Of the possible side effects with topical application - only irritation and burning sensation at the site of application.
Second and third trimesters
In the II and III trimester, Sertoconazole 300 mg is used intravaginally once. This drug has a powerful antifungal effect by increasing the permeability of the cell membrane, which leads to the destruction of the cells of the opportunistic fungus.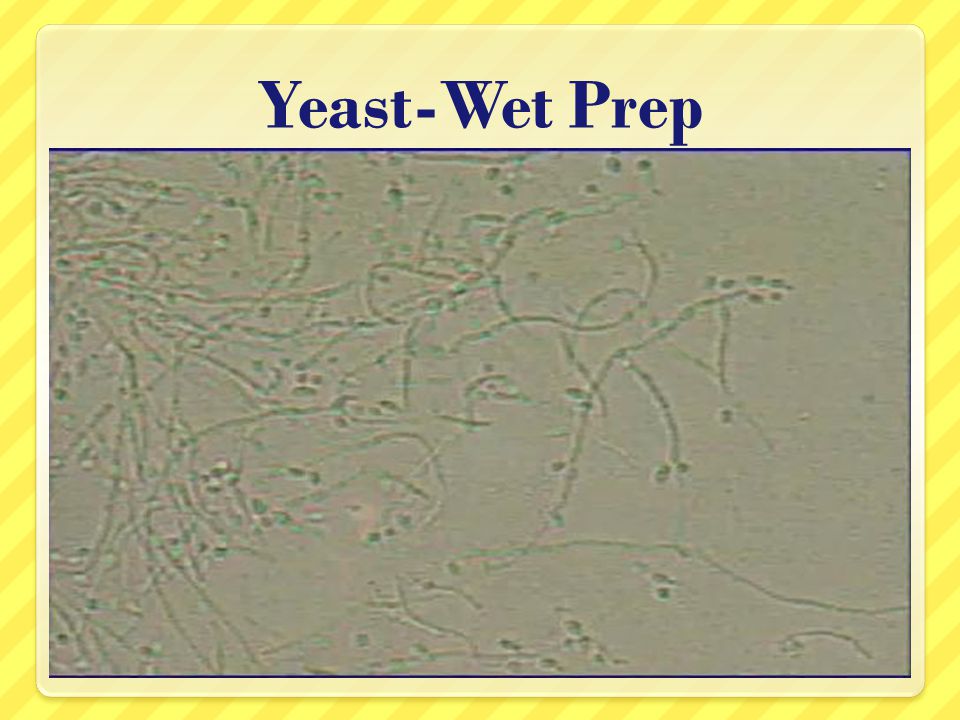 Side effects do not differ from the previous drug. Of the side effects at the site of application of Sertoconazole, itching and burning may occur, which will pass on their own.
Side effects do not differ from the previous drug. Of the side effects at the site of application of Sertoconazole, itching and burning may occur, which will pass on their own.
Followed by Econazole 150 mg intravaginally for 3 days. The drug has a local antifungal and antibacterial effect. It stops the biosynthesis of ergosterol and other sterols that regulate the permeability of the fungal cell wall. With intravaginal administration, patients did not experience pregnancy complications or other undesirable effects of therapy on reproduction. Local reactions are possible: rash, burning, irritation, itching, redness and dryness of the skin.
The last stage of treatment is Clotrimazole 100 mg intravaginally for 6-10 days. The drug belongs to a broad spectrum antifungal agent. It is applied topically only by the intravaginal method. Clotrimazole inhibits the growth and division of microorganisms.
The mechanism of action of the drug is associated with a change in the permeability of cell membranes.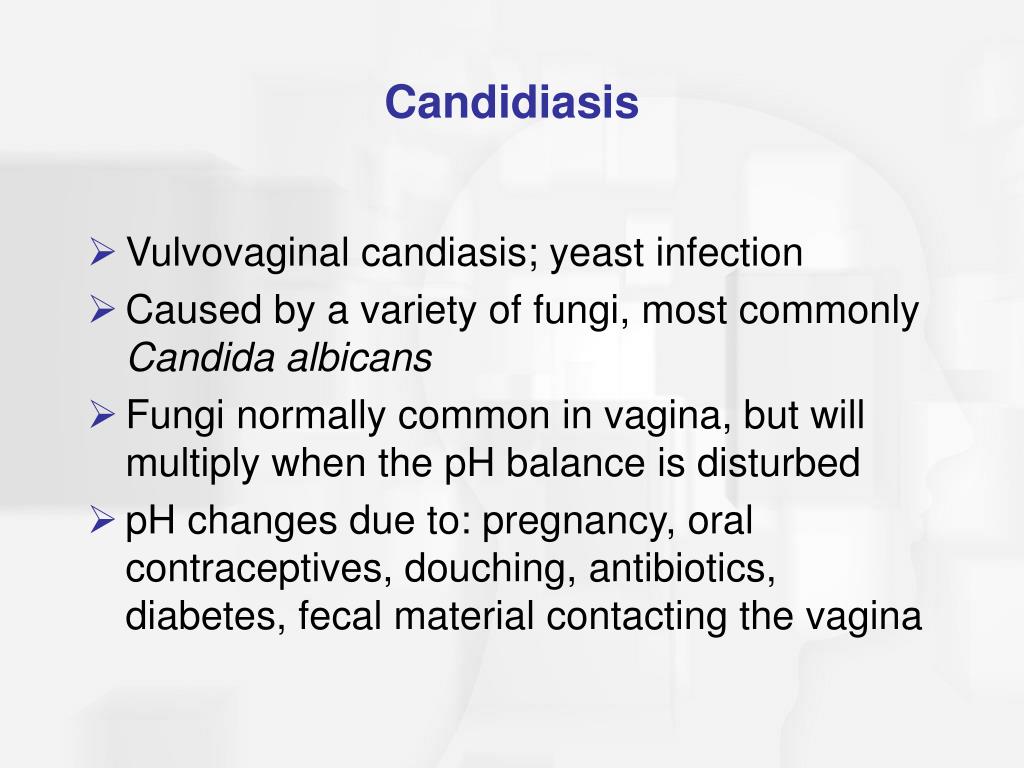 It inhibits the synthesis of proteins, fats, damages nucleic acids in fungal cells and accelerates the excretion of potassium. Very rarely, but sometimes there are yeast-like fungi that may be immune to the drug. In general, reviews of the drug are extremely positive, however, some patients may experience side effects that Clotrimazole has in abundance.
It inhibits the synthesis of proteins, fats, damages nucleic acids in fungal cells and accelerates the excretion of potassium. Very rarely, but sometimes there are yeast-like fungi that may be immune to the drug. In general, reviews of the drug are extremely positive, however, some patients may experience side effects that Clotrimazole has in abundance.
In addition, when treating candidiasis, it is recommended to follow a diet. About what foods can be consumed, and which are better not worth it, read our material.
Folk methods
It should be said that the doctor with whom we consulted does not advise the use of folk remedies for thrush, as they are simply not able to help with this disease. But on the Internet, some means are indicated. Among them: douching and tar soap, soda and chamomile, potassium permanganate and sea buckthorn oil.
For more information on how to use these folk remedies, look in our material.
However, we want to remind you once again that none of the folk remedies is a panacea for thrush. Alternative recipes can reduce the intensity of unpleasant symptoms, but can not cure candidiasis. Therefore, we recommend that you seek professional medical help without fail and do not self-medicate.
find out how to get diagnosed
What to avoid when treating thrush?
First of all, do not self-medicate. This advice is especially relevant during pregnancy. Not all drugs are compatible with pregnancy, and which of them can or cannot be taken - only the attending physician can decide!
As we said above, during pregnancy, only local therapy is prescribed. Ignorance of these features can adversely affect the fetus.
Ignorance of these features can adversely affect the fetus.
Why is thrush dangerous during pregnancy?
Thrush is dangerous during pregnancy. At this time, the development of an ascending infection with intrauterine infection of the fetus and a newborn with the development of intrauterine infection is possible.
Do not start this disease. This is fraught not only with unpleasant symptoms, but also with consequences for the body. Candidiasis carries the following complications: systemic damage to the pelvic organs, a significant decrease in the quality of life, constant discomfort, dysbiotic disorders of the microflora of the intestinal tract. During pregnancy, the effects may intensify.
What to do if it doesn't go away?
Unfortunately, thrush can easily develop from an active to a chronic form. This happens for a number of reasons. For example, hormonal disruptions and other health-related causes, which abound during pregnancy, can lead to the reappearance of candidiasis. In addition, a decrease in immunity, fatigue, and even climate change can provoke a relapse.
This happens for a number of reasons. For example, hormonal disruptions and other health-related causes, which abound during pregnancy, can lead to the reappearance of candidiasis. In addition, a decrease in immunity, fatigue, and even climate change can provoke a relapse.
If candidiasis does not go away during pregnancy or returns, you should not fight it yourself according to the prepared scheme from the last time. The patient needs to contact the attending physician again to select the most effective drugs.
This is especially true for pregnant women. Drugs used outside of pregnancy can not only not help, but also harm.
Prevention
How to avoid the unpleasant symptoms and consequences of thrush? It is not so difficult to do this if you strictly follow the basic rules of prevention and hygiene. Among them - the selection of comfortable underwear, personal hygiene, the rejection of scented pads and, of course, maintaining the immune system. The last point is, in principle, relevant for pregnant women.
Among them - the selection of comfortable underwear, personal hygiene, the rejection of scented pads and, of course, maintaining the immune system. The last point is, in principle, relevant for pregnant women.
Conclusion
During pregnancy, a woman has a natural decrease in immunity, which may, unfortunately, lead to thrush. And if you do not start a fight with it in time, then the disease can be transmitted to the child. However, with timely treatment and elimination of the factors that cause the disease, it is possible to forget about this disease once and for all. The main thing is not to start thrush to a chronic form. Only a medical specialist will be able to individually select for you a treatment that will cope with the disease.
If you still have questions, you can ask them to the specialists of the Innovative Technology Clinic.
Website: https://3dkit.ru/
Phone: +7 (963) 380-10-31 +7 (865) 257-76-05
. Dovatortsev, 53 B
Author: Ekaterina Vlasova
Photo: Anastasia Ryazhskaya
Yeast Infection - All You Need to Know
Definition
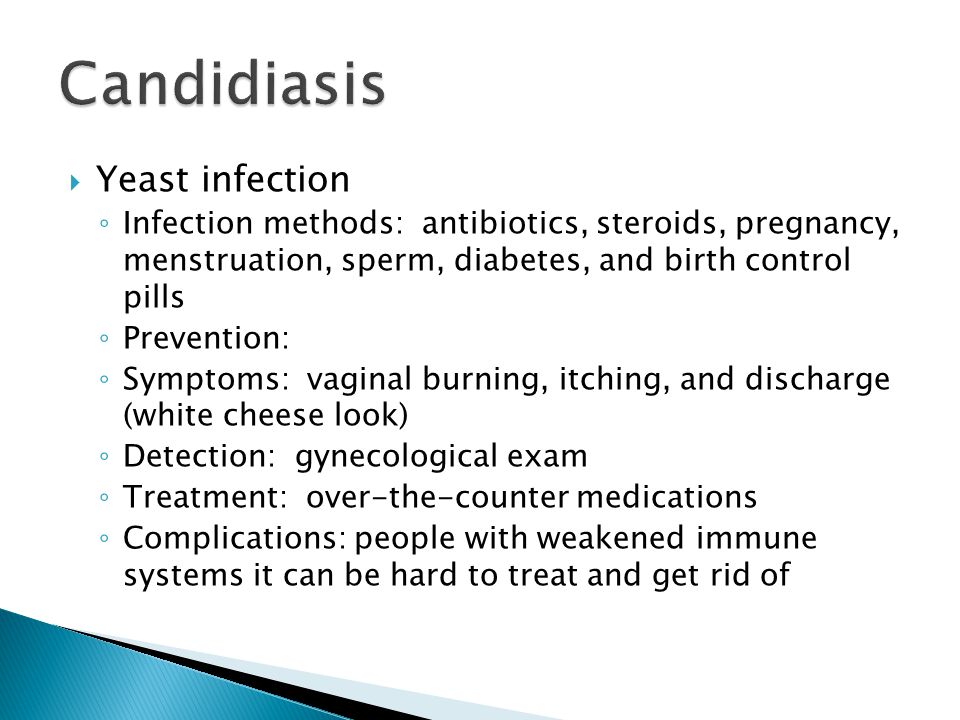
A yeast infection is commonly called candidiasis. This is a widespread infection caused by the yeast Candida Albicans. Fungal infections are common in warm, moist areas of the body, including the mouth, intestines, vagina, throat, and moist areas of the skin.
Candida usually causes no problems and can live inside the body. Normally, the body's immune system is actively working to balance the growth of fungi. If the immune system changes, you can get candidiasis. When Candida gets out of control, you may experience a number of problems. Thrush occurs due to the abundance of fungi in the mouth. If it forms in the vagina, it is called a vaginal yeast infection.
Thrush occurs due to the abundance of fungi in the mouth. If it forms in the vagina, it is called a vaginal yeast infection.
Candidiasis is more likely to occur as a secondary infection in immunocompromised people. Candidiasis, moniliosis and thrush are synonymous with candidiasis. These organisms can be found in the mouth, gastrointestinal tract, genitals, and other parts of the body.
Fungi become pathogenic only under certain conditions. They can affect the oral cavity, vaginal area, penis, and other parts of the body. Thrush is the name of a type of candidiasis that affects the oral cavity. Oral candidiasis can be pseudomembranous, erythematous, and chronic hyperplastic.
Candidiasis is common in chronically ill people and newborns. It most often appears as white, soft, slightly raised plaques on the tongue and oral mucosa. The plaques look like cottage cheese and are composed of matted masses of fungal hyphae, desquamated epithelium, necrotic debris, keratin, leukocytes, fibrin, and bacteria.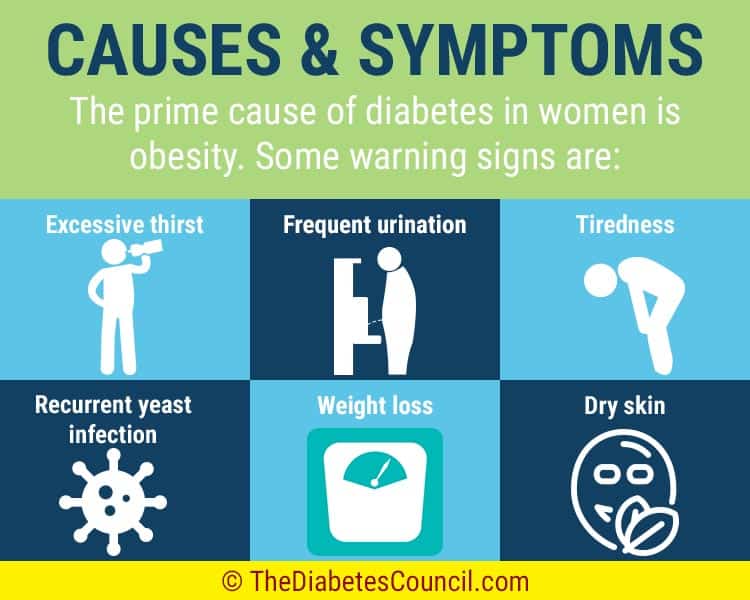 When the white plaque is removed, an erythematous area remains.
When the white plaque is removed, an erythematous area remains.
Antibiotic pain in the mouth is another name for erythematous candidiasis. This occurs after the use of broad-spectrum antibiotics or corticosteroids. Lesions present as persistently painful erythematous patches on the tongue, as well as atrophy of the central papillae. When the palate is involved and erythema occurs as a result of contact with the tongue, this is called kissing injury.
Candidiasis leukoplakia, also known as chronic hyperplastic candidiasis, is characterized by hard, white, persistent plaques on the lips, tongue, and buccal mucosa. These plaques may be uniform or nodular and may persist for years. This may be a precancerous condition.
Epidemiology of thrush
Candidiasis is more common in the elderly and children. Thrush affects approximately 37% of newborns in the United States during the first few months of their lives. Oral candidiasis is more common in children who use inhaled steroids.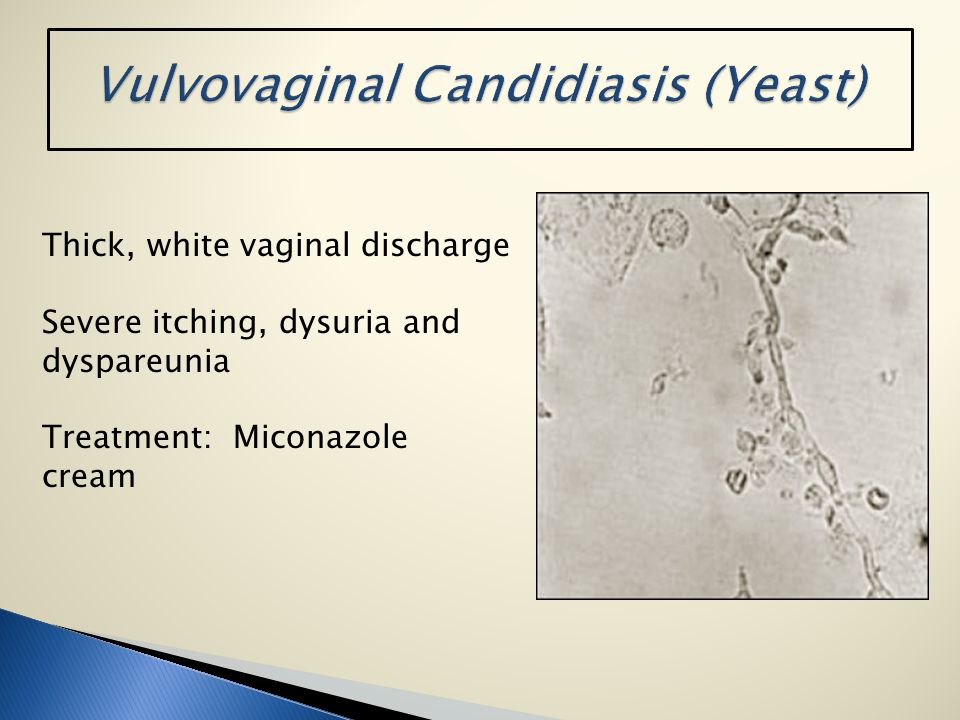 Quite common in pregnant women. Thrush can be an early sign of HIV infection. Thrush occurs worldwide and is more common in those who are malnourished. Thrush affects both men and women.
Quite common in pregnant women. Thrush can be an early sign of HIV infection. Thrush occurs worldwide and is more common in those who are malnourished. Thrush affects both men and women.
How does a yeast infection occur?
Yeast infections can occur for a number of reasons. As a result of fluctuations in hormones in some women, they appear during the menstrual cycle or during pregnancy. Some birth control pills can also make you more likely to develop a yeast infection.
Candida (yeast) is a form of fungus that can survive almost anywhere. It is normally present in the body; however, the immune system prevents it from spreading out of reach. Thus, infection occurs as most of the yeast multiplies inside the vagina.
Thrush can occur due to an imbalance in the natural balance between yeast and bacteria in the vagina. For example, antibiotics used to treat any bacterial infection can also kill lactobacilli. These are beneficial bacteria found in the vagina that inhibit the growth of yeast.
Fungal infections may be exacerbated by conditions that compromise the immune system, including sexually transmitted diseases. Women with diabetes who do not control their blood sugar are also at greater risk. This is due to the fact that elevated sugar levels stimulate the growth of yeast.
Yeast infections can sometimes also occur on the scrotum and penis, although this is less common. They can cause inflammation and redness around the penis or scrotum.
Generally, yeast infections are not STDs. They are not contagious and cannot be transmitted during sexual intercourse. However, intercourse can sometimes lead to fungal infections. This is because the body can react negatively to someone else's natural genital yeast or bacteria, causing the yeast to develop.
Risk factors for yeast infection
The following factors may increase your chances of getting a yeast infection;
Use of antibiotics. Yeast infections are common in women who take antibiotics frequently. Broad-spectrum antibiotics that kill all bacteria often kill the good bacteria in the vagina, leading to yeast overgrowth.
Broad-spectrum antibiotics that kill all bacteria often kill the good bacteria in the vagina, leading to yeast overgrowth.
High estrogen levels. In most cases, yeast infections are more common in women with higher estrogen levels. This includes pregnant women or women taking high doses of birth control or estrogen hormones.
Uncontrolled diabetes. Most women with poorly controlled blood sugar levels are more prone to yeast infections than women with well controlled blood sugar levels.
Immune system dysfunction: Women with weakened immune systems, including those due to corticosteroid injections and HIV infection, are most likely to develop yeast infections.
Types of yeast infections
Thrush (oropharyngeal candidiasis):
Thrush is an infection that occurs when Candida is spread in the throat and mouth. It is more common in the elderly, newborns, and people with weakened immune systems.
Oral candidiasis is a fungus that affects the oral mucosa and is one of the most common fungal infections. These ulcers are caused by the yeast Candida albicans. Candida albicans is a common component of the normal oral microbiota, with 30 to 50 percent of people carrying the fungus. With the age of the patient, the frequency of carriage increases. Candida albicans is found on the lips in 60% of patients over 60 with dentures.
In addition, adults are more likely to get thrush if they;
- Under treatment for cancer
- Taking medications such as corticosteroids or broad-spectrum antibiotics.
- Have diabetes
- Wearing dentures
Thrush may not cause any symptoms in the early stages. However, as the infection worsens, you may develop one or more of the following signs and symptoms;
- White or yellow bumps around the tongue, cheeks, lips, tonsils or gums
- If the bumps of the yeast infection are scraped off, you may have some bleeding.
- Burning and sore mouth
- Cotton sensation in the mouth
- Cracked and dry skin around the corners of the mouth
- Problems with swallowing
- Having an unpleasant taste in the mouth
- Loss of taste
In some cases, thrush can also affect the esophagus, although this is rare. A similar fungus associated with oral thrush can also cause a yeast infection in another part of the body.
Yeast infection is contagious to people who are at increased risk. This includes people with compromised body immune systems or who use certain medications. The infection is rarely transmitted through kissing or other intimate contact in healthy people. In most cases, thrush is not contagious, but it can still spread.
If you are afraid of contracting thrush from an infected person, refrain from contact with his saliva. When you are in close proximity to a person with thrush, it is recommended that you wash your hands as often as possible.
- Difference between "oral yeast infection" and "strep" infection.
A bacterial infection of the throat causes soreness and inflammation of the throat. Oral candidiasis is an opportunistic oral infection that often co-occurs with staphylococcus or streptococcus bacteria.
- Oral Yeast Infection and Simple Tongue Ulcer
Ulcers are painful sores that develop in the inside of the mouth. Ulcers are caused by stress, minor trauma to the inside of the mouth, sour fruits and vegetables, and hot, spicy foods.
Genital yeast infection or genital candidiasis:
Approximately 3 out of every four adult women will develop a yeast infection at any point in their lives. This happens if there is so much yeast growing in the vagina. Genital yeast infections can also occur in men, but are much less common.
Thrush usually occurs when the vaginal balance changes. Diabetes, pregnancy, use of certain medications, spermicides, lubricants, or a weakened immune system can contribute to this. Sometimes the infection can be passed from one person to another during sexual intercourse.
Diabetes, pregnancy, use of certain medications, spermicides, lubricants, or a weakened immune system can contribute to this. Sometimes the infection can be passed from one person to another during sexual intercourse.
A vaginal or genital yeast infection can be associated with numerous signs and symptoms:
- Itching sensation in the vaginal and vulvar area.
- White and thick cheesy vaginal discharge.
- Swelling of the vulva and vagina.
- Small cracks and tiny cuts in the skin around the vulva due to looseness of the skin.
- Burning sensation in thrush, especially when urinating
- In some cases, pain during intercourse may be associated with a vaginal yeast infection.
Invasive candidiasis:
Candida yeast can spread to the heart, eyes, blood, bones and brain if it enters the bloodstream. This can happen through medical instruments or devices, resulting in a severe fatal infection.
This usually occurs in patients who have been hospitalized or live in a medical facility such as a nursing home. You are more likely to have invasive candidiasis, especially if you have a weakened immune system, diabetes, kidney disease, or are taking antibiotics.
You are more likely to have invasive candidiasis, especially if you have a weakened immune system, diabetes, kidney disease, or are taking antibiotics.
Fever and chills are some of the signs and symptoms of invasive candidiasis. Although a person with this infection is likely to develop another disease, it can be difficult to diagnose.
Diaper rash due to yeast infection:
Diaper rash usually occurs when a wet or dirty diaper is left on the baby for an extended period of time. When a child's skin becomes irritated, infection becomes more likely. If the diaper rash persists, examine the child and check for reddened perineal skin. Also check for raised red borders on sores. If this is the case, ask the pediatrician to examine the child for candidiasis.
In general, the best way to avoid candidiasis and diaper rash is to keep your baby's bottom clean and dry at all times.
Yeast infection symptoms
Intense itching and irritation in the vagina and vulva, burning sensation when urinating, which can be mistaken for a urinary tract infection. Vaginal discomfort or pain, a dry, erythematous rash, and a thick, white, cheesy discharge are all symptoms of vulvovaginitis.
Vaginal discomfort or pain, a dry, erythematous rash, and a thick, white, cheesy discharge are all symptoms of vulvovaginitis.
Candida can also cause thrush, which is characterized by a white or yellow rash on the tongue and mucous membranes of the mouth, and redness and cracking pain around the corners of the mouth. In this case, it spreads into the oropharynx, causing discomfort when swallowing. Infants, the elderly, and people with weakened immune systems are all susceptible to candidiasis. Fever, chills, hypotension, and confusion are all symptoms of systemic candidemia.
Candidal infection of the larynx is rare. Women suffer the most. They often express dysphoria. It is closely related to gastric reflux or a history of inhaled corticosteroid use. The presence of leukoplastic lesions can lead to damage to the glottis.
Diagnosis of thrush
To effectively diagnose a yeast infection, a gynecologist or other healthcare professional may;
- Ask about your general medical history .
 This usually includes getting the necessary information about previous yeast infections and any STIs.
This usually includes getting the necessary information about previous yeast infections and any STIs. - Gynecological examination. During the diagnosis, the doctor will evaluate the external genitalia for signs of a yeast infection. After that, he or she may insert a device known as a speculum into the vagina to examine the cervix and vagina. The cervix is the lower and narrower region of the uterus.
- Examination of vaginal discharge. If necessary, the doctor may take a sample of vaginal secretions to analyze the types of fungus, which will further provoke infection. Determining the types of fungus allows a doctor to prescribe appropriate forms of treatment for recurrent yeast infections.
Yeast Infection Treatment
Yeast infection treatment usually depends on the type and nature of the infection, whether it is complex or uncomplicated.
For a less complex yeast infection, treatment includes two approaches including oral therapy and topical vaginal treatment. A short course of vaginal therapy is usually appropriate for treating an uncomplicated yeast infection.
A short course of vaginal therapy is usually appropriate for treating an uncomplicated yeast infection.
Alternative medicine for yeast infection or over-the-counter yeast infection medications include butoconazole (ginazol-1), clotrimazole (gynelothrimine), miconazole (monistat 3), and terconazole (terazol 3). In addition, clotrimazole, monistat 3 and terciflunomide can be purchased online.
The effectiveness of oral and topical therapy is the same, although oral preparations are more expensive. Fluconazole should not be given during the first trimester of pregnancy. Fluconazole is taken on days 1, 4, and 7 for recurrent vaginal candida infection, and then monthly for six months.
Oral thrush can similarly be treated with oral lozenges as a replacement dosage form. Oral or intravenous antifungals such as caspofungin, fluconazole, and amphotericin B are used to treat systemic candidiasis.
In the case of fungal stomatitis, the patient should stop using a denture for at least two weeks and apply topical antifungal drugs. Loss of vertical dimension of the jaw causes angular cheilitis. As a result, when the infection subsides, it is necessary to fabricate a new denture with suitable vertical dimensions. Probiotics may be used as an adjunct in the treatment of oral thrush.
Loss of vertical dimension of the jaw causes angular cheilitis. As a result, when the infection subsides, it is necessary to fabricate a new denture with suitable vertical dimensions. Probiotics may be used as an adjunct in the treatment of oral thrush.
Complex yeast infection:
Treatment of complex yeast infection will require long-term vaginal treatment or multi-dose oral formulas. Maintenance medications may be recommended. Such drugs are used daily to prevent the recurrence of the disease.
Long-term vaginal therapy consists of 7-14 days of complex treatment using tablets, vaginal cream, thrush suppositories or ointment. Instead of direct vaginal treatment, two or three oral doses of fluconazole can sometimes be given. When symptoms are severe, a doctor may recommend topical steroids for a few days to relieve symptoms until antifungal treatment is effective.
Before taking antifungals, check to see if fungal infections are causing symptoms. This is because overuse of antifungal medications can increase the chance of yeast resistance. This means that drugs can no longer function in the body in the way that they will in the future.
This is because overuse of antifungal medications can increase the chance of yeast resistance. This means that drugs can no longer function in the body in the way that they will in the future.
When maintenance prescriptions are needed, they should be started after completion of one of the above forms of treatment. This may be weekly oral fluconazole therapy for six months or weekly vaginal therapy with clotrimazole.
If your partner is showing symptoms of a yeast infection, they should also be treated. In this case, it is often recommended to use a condom.
Yeast Infection Prevention
Although there is no sure way to avoid a Candida infection, there are certain things you can do to reduce your chance of getting a vaginal yeast infection. In most cases, women at risk are strongly advised to:
- Refrain from douching
- Avoid using feminine deodorants, tampons, or deodorant pads.
- Wear underwear made from cotton or other natural fabrics.
- Wear slightly loose and fitted trousers and skirts.
- Wash underwear at high temperatures
- Refrain from wearing tight underwear or tights
- Eat a balanced, varied diet
- Change wet clothing, such as bathing suits, as soon as possible.
- Avoid hot tubs and hot tubs if possible.
Health care providers may recommend oral or intravaginal probiotics for women with more than three infections per year. Also, if you notice or suspect any symptoms and signs of a yeast infection, talk to your doctor right away about a proper diagnosis.
Differential
Pustular psoriasis, subcorneal pustulosis, and acute generalized basal pustulosis can all cause a spongy rash. To exclude the fungal etiology of psoriasis, certain dyes should be applied.
Impetigo is also spongy. Gram stain can be used to detect bacterial colonies in impetigo, although GMS and PAS stains do not stain fungal forms.
Tinea cruris and corporis are known for their spongy shape. Without developing candida yeast, special staining reveals septate hyphae. Sometimes it can be difficult to tell the difference. Candida infiltrates the keratinized epithelium, while dermatophytosis more often affects the stratum corneum.
Without developing candida yeast, special staining reveals septate hyphae. Sometimes it can be difficult to tell the difference. Candida infiltrates the keratinized epithelium, while dermatophytosis more often affects the stratum corneum.
It is difficult for an otolaryngologist to make a correct diagnosis of laryngeal candidiasis, a high degree of alertness is required. Patients with predisposed characteristics who present with a suspected lesion should include the disease in the differential diagnosis.
Prognosis
Although the most common candidal infections are localized, vaginal and skin infections are also common. As a result, antifungal drugs can be used to treat them, resulting in complete recovery and excellent prognosis and outcomes. Candida infection, if left untreated, can spread to other organs and cause systemic disease.
The extent and location of the Candida infection, the general health of the victim, and the timing of diagnosis and treatment all play a role in the long-term prognosis of systemic candidiasis.
Nearly a third of patients with candidaemia develop septic shock as a result of host characteristics, including age and source of infection, rather than virulence characteristics of the organisms.
Complications of yeast infections
Complications of a yeast infection can occur in the following cases:
- If you have extreme signs and symptoms, including widespread redness, itching, and swelling that cause cracks, tears, and sores.
- Four or more episodes of yeast infections within one year
- Infection due to less common forms of fungus.
- Pregnancy
- Compromised body immune system due to certain medications or health conditions such as HIV infection.
- Uncontrolled diabetes
Is thrush contagious?
Although yeast infections are not classified as sexually transmitted infections (STIs), they are still contagious. Thrush can be transmitted through oral and vaginal sex. Also, a yeast infection is spread through sex toys or kissing someone who has oral candidiasis.
Also, a yeast infection is spread through sex toys or kissing someone who has oral candidiasis.
A baby may develop a fungal diaper rash during childbirth if the mother had vaginal thrush during childbirth. Also, if you have a Candida overgrowth around your breast area, you can pass the disease to your baby by mouth while breastfeeding.
Although a yeast infection can be passed from one person to another, it is not contagious like other diseases. Therefore, you will not get an infection through the air or from sharing a shower with someone who has it.
Yeast infections in men
Yeast infections in men can develop and affect the penis. When this happens, the condition is called a penile yeast infection. Candida is in all organs, not only in women. Yeast infection can result from overgrowth of this fungus. Due to moisture and skin folds, the groin area is particularly vulnerable to Candida overgrowth.
Yeast infections in women
Yeast infections in women are common. According to studies, three out of four women may have more than two vaginal yeast infections in their lifetime. Despite their widespread occurrence, it is extremely important to treat vaginal yeast infections as soon as possible. You will not only be able to relieve unpleasant symptoms, but you will also be able to minimize the possibility of the spread of the disease in the body.
According to studies, three out of four women may have more than two vaginal yeast infections in their lifetime. Despite their widespread occurrence, it is extremely important to treat vaginal yeast infections as soon as possible. You will not only be able to relieve unpleasant symptoms, but you will also be able to minimize the possibility of the spread of the disease in the body.
Yeast infections in children
Yeast infections are usually associated with vaginal infections, but they can also affect children. Diaper rash is the most common yeast infection in children. However, not all diaper rash is caused by yeast overgrowth.
Sometimes your baby's skin becomes excessively red and blotchy around the diaper or groin area, even after diaper rash cream is applied. With this, you will be able to determine if the disorder is more than a typical diaper rash. In other cases, a yeast infection may also occur in other skin folds, including under the armpits.
Your child's pediatrician will likely recommend a topical antifungal cream to fight fungal skin infections. If a child has oral candidiasis or a yeast infection in the mouth, oral treatment may be needed. While a yeast infection rash in children is usually harmless, it can be more serious if left untreated.
If a child has oral candidiasis or a yeast infection in the mouth, oral treatment may be needed. While a yeast infection rash in children is usually harmless, it can be more serious if left untreated.
Thrush and intercourse
Fungal infection is not sexually transmitted. However, infection is possible after sexual intercourse. On the other hand, other factors can upset the balance of Candida in the vagina. The bacteria can be transmitted through vaginal intercourse, fingers, and sex toys.
Another risk is vaginal intercourse with a partner who has a penile yeast infection. A man can also get a penile yeast infection from a partner with a vaginal yeast infection. In addition, bacteria in the mouth, vaginal area, and also in the penis area can be destroyed by oral sex.
It is also likely that a yeast infection after sex is not associated with other symptoms. Sexual intercourse is just one of the major risk factors for a yeast infection.
Fungal infection and urinary tract infection (UTI)
UTI is one of the most common infections affecting most women.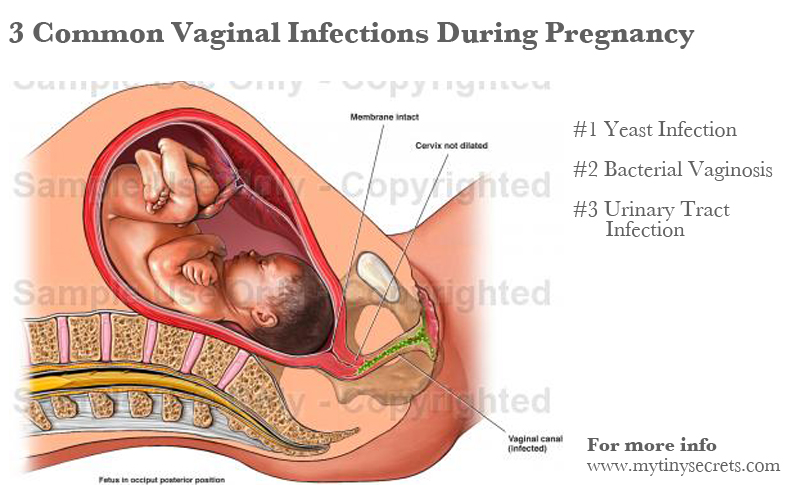 While it is possible to get one or both diseases at the same time, yeast infections and UTIs are two different diseases.
While it is possible to get one or both diseases at the same time, yeast infections and UTIs are two different diseases.
A urinary tract infection is a bacterial infection that develops in the urinary system. The urethra, bladder and kidneys are part of this complex structure. UTIs can also occur due to a variety of factors, including sexual intercourse, STIs, and lack of regular urination.
Signs and symptoms of a UTI are different from those of a yeast infection. As long as there is no visible discharge from a yeast infection, you may notice a small trace of blood in your urine. In addition to regular urination, a UTI can cause pain in the pelvis as well as in the abdomen.
A UTI can cause serious kidney problems if left untreated. Antibiotics must be obtained from a physician. Also, ask your doctor about the differences between a yeast infection and a urinary tract infection.
How do you tell a "yeast infection" from a "chlamydia" infection?
Yeast infections cause thick, white, cottage cheese-like discharge, while chlamydia can cause white, green, or yellow discharge.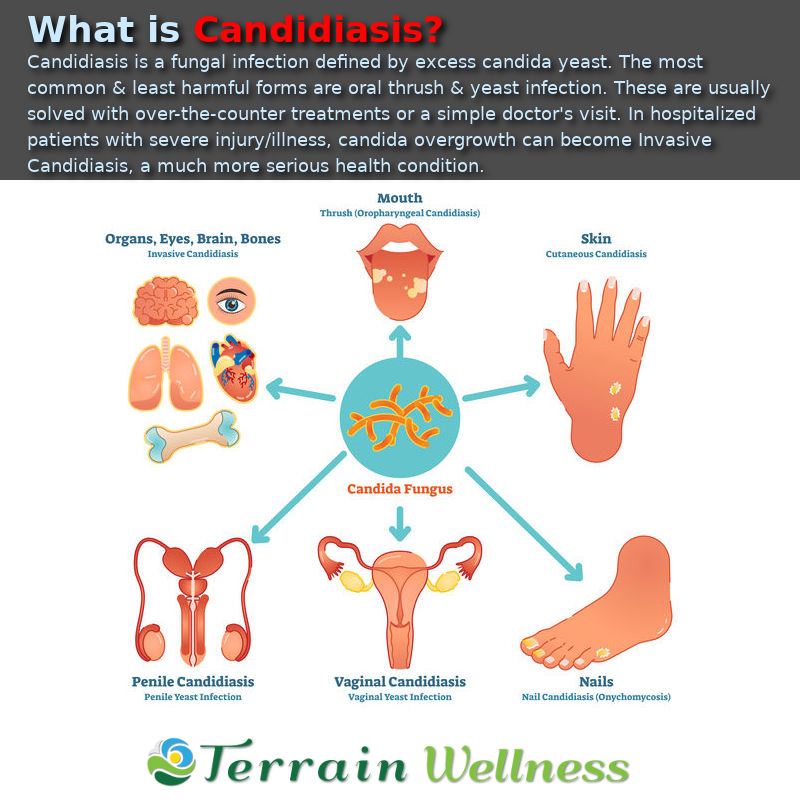 Gonorrhea discharge is white or green.
Gonorrhea discharge is white or green.
Thrush and menstrual periods
Having a yeast infection and menstruating at the same time can seem like a disaster. This, however, is rare. Yeast infections are common in women in the last days before menstruation.
Hormonal fluctuations are believed to be the cause of thrush before menstruation. This creates an imbalance of good bacteria in the vagina.
If you have white or yellow discharge about a week before your cycle, it may not always be due to a yeast infection. What matters is whether you already have these telltale signs, including redness, itching, or burning.
Although it may be uncomfortable, early treatment can clear up the yeast infection before your next period. Check with your doctor if signs of a yeast infection persist after a cycle is completed. You may also notice them if you continue to get thrush every month before your period.
Yeast infection during pregnancy
Due to the hormonal changes that occur during pregnancy, yeast infections are normal. If you are pregnant and think you have a yeast infection, you should consult your doctor and get a proper diagnosis.
If you are pregnant and think you have a yeast infection, you should consult your doctor and get a proper diagnosis.
Thrush during pregnancy is not treated in the same way as in non-pregnant women. Because of the potential risk of birth defects in the fetus, you will not be able to use oral antifungals. Doctors often recommend using topical antifungals during pregnancy.
Although yeast infections will not harm the baby, Candida can be passed at birth. Therefore, as a result of this, the child may develop diaper rash or stomatitis. Therefore, it is very important to treat a yeast infection as soon as possible during pregnancy to avoid complications.
Intestinal yeast infection
In immunocompromised individuals, fungal infections are one of the leading causes of morbidity and mortality. Invasive fungal infections, especially of the gastrointestinal tract, have become more common as the number of immunocompromised people has grown.
Mushroom growth in the intestines is also possible. As a result, candida may appear in your stool. When patients develop symptoms of colon inflammation, especially if they are immunosuppressed, doctors should be aware of the possibility of this fungal disease.
As a result, candida may appear in your stool. When patients develop symptoms of colon inflammation, especially if they are immunosuppressed, doctors should be aware of the possibility of this fungal disease.
Yeast Infection Diet
It is possible that the foods you eat are contributing to the development of a yeast infection. Sugar is the favorite of yeast. Avoiding the foods listed below (sometimes called the Candida diet) will help you control the development of yeast in your body:
- White flour and rice
- Foods or drinks fermented with yeast
- Products consisting of simple sugars
While avoiding certain foods can help you avoid a yeast infection, sticking to this diet can be difficult. Fortunately, you may not need to completely avoid these foods to reduce the frequency or severity of yeast infections. It may be helpful to simply reduce the amount of these foods.
It may also be helpful to increase your intake of healthy proteins and fats, as well as low starch fruits and vegetables.