Breastfeeding nerve pain
Vasospasm and breastfeeding - symptoms, causes, management
beginning of content5-minute read
Listen
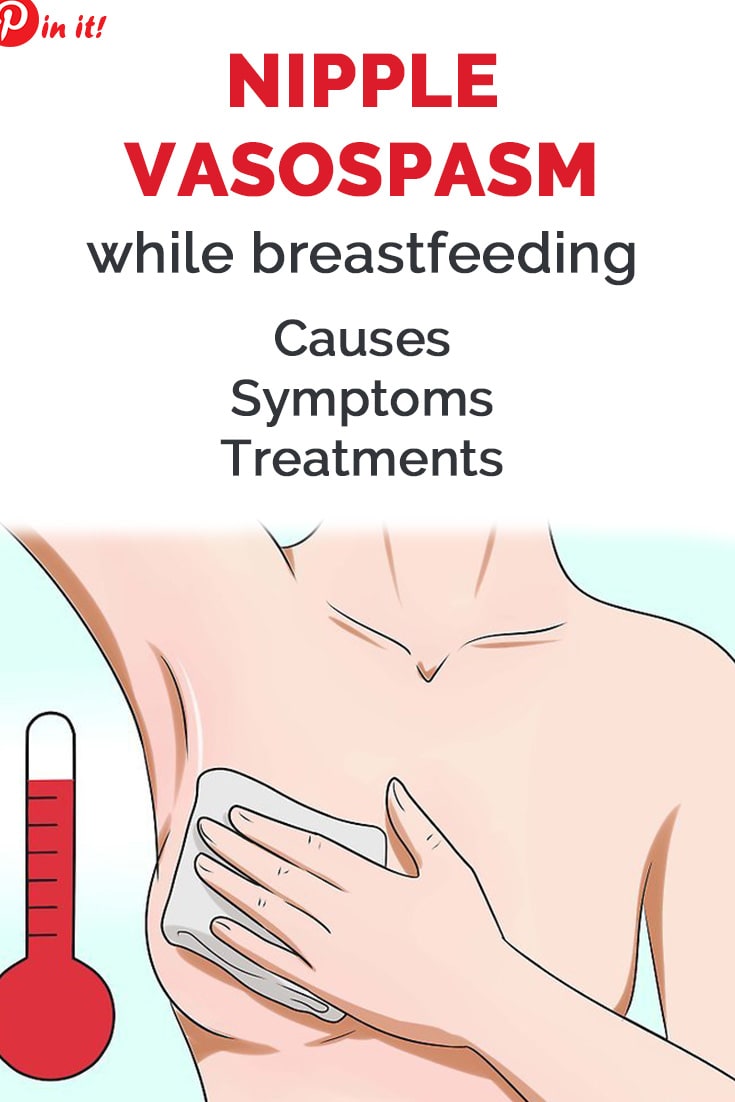
What is nipple vasospasm?
Vasospasm is what happens when the blood vessels supplying the nipple go into spasm and reduce the blood flow to the nipple. This affects the flow of milk from the nipple.
It is common to feel intense pain if this happens, particularly if the weather is cold. While any of the body's blood vessels can be affected by vasospasm, it can be a particularly painful condition for breastfeeding mothers.
Nipple vasospasm can occur:
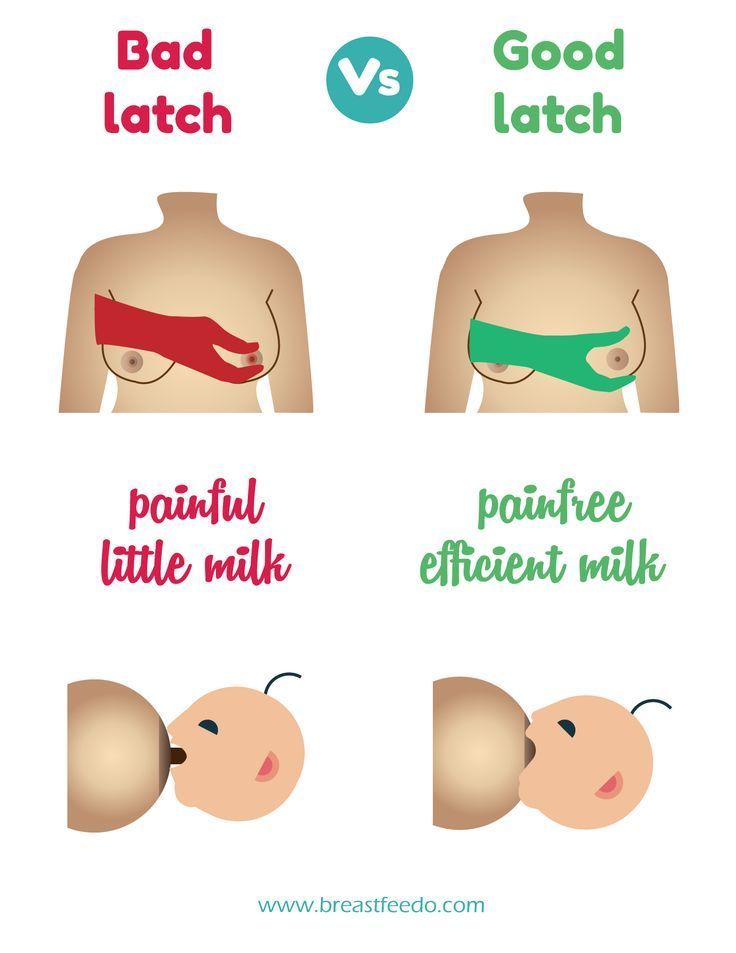
- In response to nipple trauma if the baby is not well attached to the breast.
- It can also happen due to Raynaud’s phenomenon, more commonly called ‘Raynauds’ (see below). This is when vasospasm occurs randomly and is unrelated to breastfeeds.
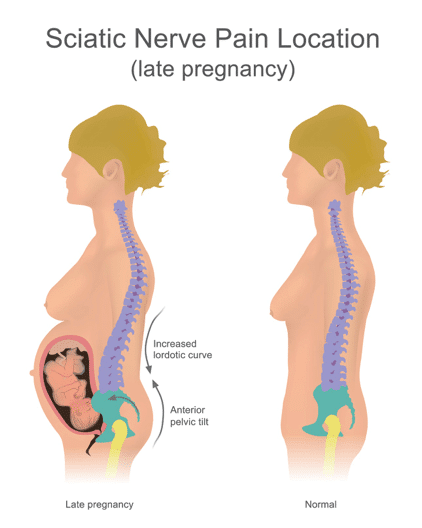
Some women are more likely to have nipple vasospasm, particularly those who tend to have cold fingers and feet and who may already believe they have poor circulation. Sometimes women first experience nipple vasospasm during their pregnancy.
Women who are below average weight for their height are also at greater risk. Cigarette smoking can make vasospasm worse because nicotine constricts the blood vessels.
What does vasospasm with breastfeeding feel like?
Women with vasospasm commonly describe it as an intense, throbbing, burning type of pain in their nipples. When the blood vessels in the nipples are affected by vasospasm, pain can be felt before, during or after breastfeeds. The pain can last for a few seconds or longer. Some women experience vasospasm when they ‘let down’ or their milk ejection reflex has been activated.
What does vasospasm look like?
The nipple or the tip of the nipple can appear white, or blanched during vasospasm. The colour of the nipple can also change as the blood returns to the vessels and tissues. This can mean there’s a change from white to purple, blue or red as the nipples return to their normal colour.
This can mean there’s a change from white to purple, blue or red as the nipples return to their normal colour.
What is Raynaud’s phenomenon?
Raynaud’s phenomenon, more commonly called ‘Raynauds’ occurs when vasospasm happens randomly and is unrelated to breastfeeds. Vasospasm symptoms can also occur in the fingers and toes in response to cold.
Raynauds is caused by a temporary interruption to normal blood flow in the small blood vessels in the extremities. This is why the fingers and toes, nose, lips and ears are often the most vulnerable body parts being affected.
If you have Raynauds when you are pregnant, you may also experience nipple vasospasm when you are breastfeeding.
How do I know if I have vasospasm?
Breastfeeding should not be painful or uncomfortable. It is common in the early days of breastfeeding for mothers to experience some nipple sensitivity as their body adjusts tp feeding. Women with nipple vasospasm may continue to experience pain when breastfeeding, even when their baby is attached properly and sucking well.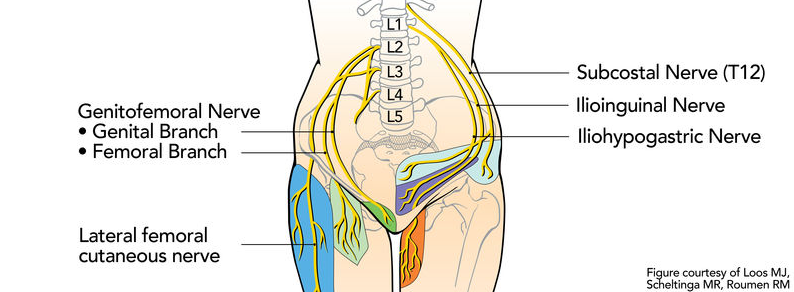
How can vasospasm be treated or managed?
You can manage the effects of nipple vasospasm by reducing your exposure to the air or cold. This will help your blood vessels to stay dilated and avoid becoming restricted. You can make your own decisions about comfort when deciding how many layers of clothing you need to wear. Ideally, you should use light layers which you can take off easily if you feel you’re overheating.
There are other strategies you can try too — for example:
- Apply warmth with a compress or heat pack straight after breastfeeding.
- Use breast warmers made from a reflective material since this can be soothing. Check with your pharmacist to see the options that are available.
- Try massaging olive oil onto your nipples after feeding but without exposing your breast to cold air.
- Try avoiding caffeine — some women report that avoiding this is helpful.
- Avoid exposing your nipples to cold air and wear more layers of clothing to avoid getting cold.

You should also check to make sure your baby is well attached when they are breastfeeding, and that you don’t have any nipple trauma or thrush.
Do supplements help for nipple vasospasm?
Some women find that taking supplements is very helpful in alleviating the symptoms of vasospasm. Before taking any medication or supplements, however, it’s important you speak with a healthcare professional or your pharmacist.
- Fish oil capsules or evening primrose oil (gamma linoleic) may help to improve blood vessel relaxation.
- Magnesium tablets can help to relax the blood vessels.
- Prescription medication may be beneficial — speak with your doctor for more information.
Where can I go for help and advice?
For more help with nipple vasospasm and breastfeeding, speak with:
- your midwife or child health nurse.
- a lactation consultant.
- Australian Breastfeeding Association — Helpline 1800 mum 2 mum, 1800 686 268.

- Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse.
Sources:
ACT Health (Nipple Vasospasm), The Royal Women's Hospital Victoria (Herbal medicines & breastfeeding), The Royal Women's Hospital Victoria (Nipple vasospasm), Australian Breastfeeding Association (Vasospasm)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2021
Back To Top
Related pages
- Diet and medication while breastfeeding
- Breastfeeding your baby
- Mixed feeding
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Some features, tools or interaction may not work correctly.
Nipple Vasospasm and Breastfeeding - Breastfeeding Support
A vasospasm is a sudden narrowing (or constriction) of blood vessels. If the blood vessels in the nipple have a vasospasm this can cause nipple pain and sometimes deeper breast pain. A breastfeeding baby can trigger a nipple vasospasm if they are not attached (latched) to the breast comfortably ie with a big mouthful of breast tissue as well as the nipple. A nipple vasospasm can also be connected with Raynaud’s phenomenon (a condition affecting blood supply). This article looks at the symptoms, causes and possible treatments for easing nipple vasospasm.
Nipple vasospasm and breastfeeding
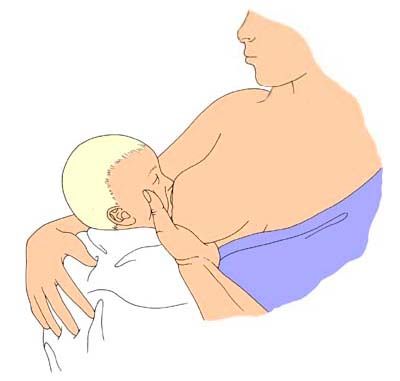
If a nipple is flattened or compressed because a baby is pinching the nipple during a breastfeed, this may trigger a nipple vasospasm. The nipple may look pointed or slanted like the top of a new lipstick straight after a feed and, since the blood vessels in the nipple are narrowed, less blood can flow and the nipple can temporarily turn white. When the blood flows back to the nipple after each breastfeed, mothers may feel a painful burning or throbbing sensation.
When the blood flows back to the nipple after each breastfeed, mothers may feel a painful burning or throbbing sensation.
What are the symptoms of nipple vasospasm?
Symptoms of nipple vasospasm include:
- Painful nipples—the pain is often described as burning, stabbing or itching and may be felt a short time after breastfeeding and/or in between feeds.
- Sore nipples—nipple vasospasm is associated with misshapen nipples and sore nipples or previously damaged nipples that are healing.1
- White nipples—nipple tips may look white (blanched) after a feed or mothers may notice other colour changes in their nipples e.g. blue or dark red (also associated with Raynaud’s Phenomenon—see below)
- Deep breast pain—some mothers may feel deep breast pain or shooting pains deep in the breast sometimes referred to as Mammary Constriction Syndrome.
- Cold temperatures and stress may worsen the pain or trigger it.
Not vasospasm? Other causes of pain
There are many causes of sore nipples or pain during breastfeeding and for a complete overview see Causes of Sore Nipples and Why Does Breastfeeding Hurt? Vasospasm symptoms such as burning pain and soreness can be very similar to those of a bacterial infection (e.g. a Staph infection) or a fungal infection (e.g. thrush). Note that a misdiagnosis of thrush and resulting unnecessary prescription medication, may make vasospasm symptoms worse.2
What causes nipple vasospasm?
There are a number of risk factors that seem to make nipple vasospasm more likely:
- A shallow latch. In breastfeeding mothers, the main trigger for nipple vasospasm is likely to be a poor latch (the way a baby attaches to the breast).
 If a baby breastfeeds with mostly only the nipple in their mouth and not a good deep mouthful of breast tissue as well, this is often called a shallow latch. In a shallow latch the nipple is more likely to get pinched between baby’s tongue and the roof of their mouth and trigger the vasospasm. Some babies also learn that pinching the nipples is a good way to slow the milk flow in a fast let-down.
If a baby breastfeeds with mostly only the nipple in their mouth and not a good deep mouthful of breast tissue as well, this is often called a shallow latch. In a shallow latch the nipple is more likely to get pinched between baby’s tongue and the roof of their mouth and trigger the vasospasm. Some babies also learn that pinching the nipples is a good way to slow the milk flow in a fast let-down. - Sore nipples. Sore nipples, damaged or cracked nipples, and nipples that are healing are associated with poor positioning at the breast and are risk factors for vasospasm (Thomas, 2013).
- Cold temperatures. Exposure to cold temperatures and climates, or the sudden drop in temperature when a baby lets go of the nipple is a risk factor for a nipple vasospasm.3
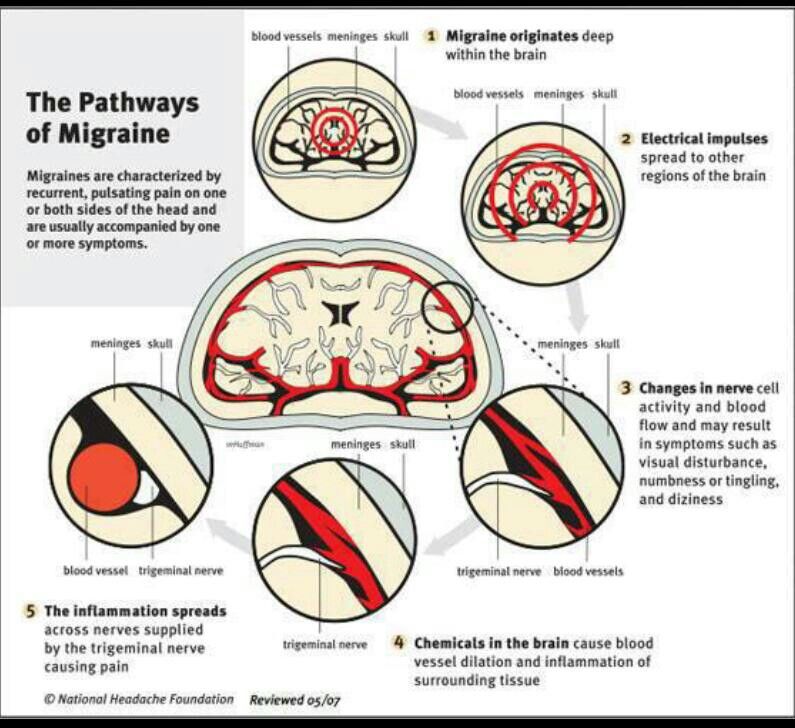
- Severe stress. Severe emotional stress is a risk factor for nipple vasospasm and a history of migraines may be a risk factor (Goldfarb, 2019).
- Medical conditions. An existing history of autoimmune disease eg lupus, rheumatoid arthritis, thyroid dysfunction, scleroderma, or previous diagnosis of Raynaud’s syndrome increases the likelihood of nipple vasospasm.4
- Cigarette smoking. Exposure to cigarette smoke, second-hand smoke or nicotine can be triggers for nipple vasospasm (Goldfarb, 2013).5
- Medications. Certain medications including fluconazole (prescribed for thrush), some decongestants, or birth control medication are risk factors for nipple vasospasm (Goldfarb, 2019; Breastfeeding Network, 2019) also beta-blockers, or vasoconstrictor medications which narrow blood vessels (Douglas, Vol 18: 1–29 2022).
- Caffeine may be a trigger for vasospasm (Goldfarb, 2019; Breastfeeding Network, 2019) however Douglas says there is no clear evidence linking caffeine intake to secondary Raynaud’s syndrome (vasospasm without existing Raynaud’s) (Douglas, Vol 18: 1–29 2022).
How can I avoid vasospasm symptoms?
Minimising the risk factors can work very well to help prevent symptoms of nipple vasospasm, namely:
- Get help with positioning from an International Board Certified Lactation Consultant so that your baby’s latch is not triggering vasospasm. A poorly latched baby, an ineffective suck or the baby clamping on the nipple can all cause nipple blanching. Babies with high muscle tone or those with tummy ache (e.g. from a food allergy) may seem to “bite” at the breast and can cause a nipple vasospasm. A baby needs to attach to the breast deeply with a big mouthful of breast as well as the nipple. See Breastfeeding Positioning for Newborns, Latching Tips and Why Does Breastfeeding Hurt? for more information and see your breastfeeding specialist for one to one help.
- Check pumping equipment. A poorly fitted pump flange could cause nipple damage and vasospasm symptoms, conversely pumping with a well fitted pump may offer relief to symptoms compared to breastfeeding for some women until they can get help with positioning.

- Keep warm; breastfeed in a warm room and cover the nipple as soon as a breastfeed ends. Don’t leave nipples to air dry as they will get colder that way. Keep breastpads dry, some mothers use woollen or fleecy breastpads for warmth. Try to avoid sudden temperature changes.6
- Avoid latching a baby while the nipple is having a vasospasm, as this may cause damage to the nipple, try warming the breast and repeatedly squeezing the nipple to help blood flow back into this area before latching (Hills, accessed Oct 2022).
- Gentle massage. Try massaging the nipples with warm olive oil after a breastfeed to stop a nipple vasospasm.78 Repeatedly squeezing the nipple during a vasospasm helps blood flow return to the nipple and can improve recovery time.
 9
9 - Rule out a bacterial infection or thrush—check with your health professional that you don’t have any other causes of burning pain and sore nipples.
- Avoid potential triggers: cigarette smoke and smoking, nicotine, caffeine, or any medications that promote vasoconstriction e.g. some decongestants10 and avoid stress where possible.
- Keep active with aerobic exercise.
Raynaud’s phenomenon
Raynaud’s is a disorder of the tiny blood vessels of the extremities which reduces blood flow. Cold temperatures or strong emotions cause the blood vessels in the extremities to go into spasms, which may cause pain, numbness, throbbing and tingling. Some women who have Raynaud’s in the fingers and toes may find they get Raynaud’s of the nipple when they breastfeed. This might be because breastfeeding affords lots of opportunities for nipples to get cold e.g. just before and after latching. Painful breastfeeding can also be stressful. Raynaud’s is often misdiagnosed as thrush or a poor latch .11
This might be because breastfeeding affords lots of opportunities for nipples to get cold e.g. just before and after latching. Painful breastfeeding can also be stressful. Raynaud’s is often misdiagnosed as thrush or a poor latch .11
Diagnosis of Raynaud’s
Raynaud’s symptoms affecting the nipple may be difficult to distinguish from nipple vasospasm caused by a poor latch:
- Symptoms can be triggered by cold and may still occur in spite of a good latch.
- Colour changes of the nipples e.g. from white to blue to red/purple may be seen with lighter skin tones.
- Raynaud’s may be linked with a history of migraines or a history of poor circulation 12.
- May be associated with previous breast surgery and nipple damage1314
Treatments for nipple vasospasm
In addition to using the above ideas to avoid getting vasospasm symptoms, there are a number of treatment options for nipple vasospasm that still persists after a poor latch has been corrected and other infections ruled out. Treatments options are discussed in the following patient information handout from the Goldfarb Breastfeeding Clinic and include pain relief, dietary supplements (calcium, magnesium and vitamin B6), omega fatty acids and prescription medication:
Excerpt from
Nipple Vasospasm Patient Handout, Herzl Family Practice Centre, Goldfarb Breastfeeding Clinic, 2019
- The use of Advil™ or Motrin™ (ibuprofen) and/or Tylenol™ (acetaminophen) may be very useful to treat the pain of nipple vasospasm. These medications are safe during breastfeeding.
- Your health professional may suggest high doses of calcium and magnesium, and vitamin B6.
Please consult your health professionals for doses specific to your case.
- Omega fatty acids may also help. Evening primrose oil (up to 12 capsules a day) and fish oil capsules are rich sources of omega fatty acids.
- Nifedipine (Adalat™) […] normally used for high blood pressure, can also be used for nipple vasospasm, and is safe for breastfeeding mothers and infants.
Nifedipine
Refer to the full Goldfarb article online for precautions regarding nifedipine and share this with your health care professional. The Breastfeeding Network discusses doses and side effects of nifedipine in their fact sheet Raynaud’s Phenomenon in Breastfeeding Mothers and for more places to find information about the safety of nifedipine online see Medications and Breastfeeding. Always discuss medications or medicinal doses of supplements with your health care provider.
Treatment tips from Dr Jack Newman
Jack Newman, a Canadian paediatrician and breastfeeding expert, has a protocol for treating vasospasm; see Vasospasm on his website.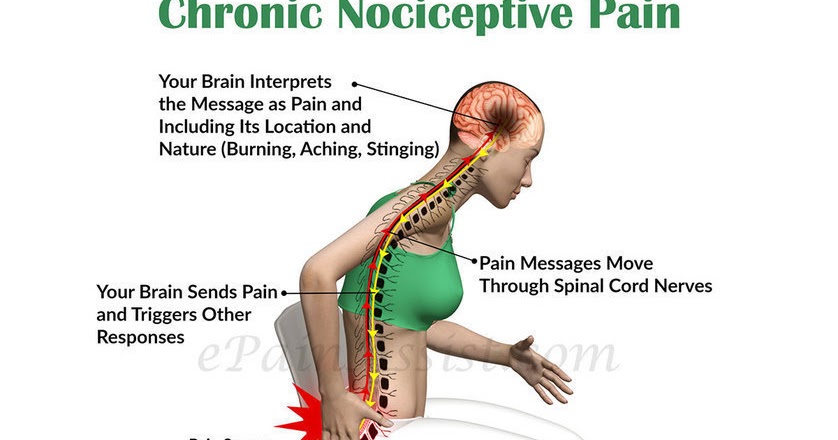 In addition to a discussion of certain vitamin and mineral supplements (also referred to in the patient handout quoted above), Dr Newman advocates:
In addition to a discussion of certain vitamin and mineral supplements (also referred to in the patient handout quoted above), Dr Newman advocates:
- All Purpose Nipple Ointment (APNO), a topical cream with antibacterial, antifungal and anti-inflammatory ingredients to help with soreness.
- Massaging olive oil into the nipples as an alternative to APNO.
- Pectoral muscle massage see Mammary Constriction Syndrome.
Complementary medicine
Scleroderma and Raynaud’s UK (SRUD) discuss natural and over the counter complementary medicine for scleroderma and Raynaud’s in Natural Therapies. They discuss doses of vitamin C, vitamin E, gamolenic acid (GLA), ginkgo bilboa and ginger and more. The latest recommendations on the compatibility of many supplements while breastfeeding can be checked online at e-Lactancia or LactMed and should always be discussed with your health professional.
Excerpt from
Natural Therapies, Scleroderma and Raynaud’s UK (SRUD), 2022 [accessed 20 October 2022]
- Gingko Biloba Up to 240mg daily in three doses.
Some people find that this produces a significant reduction in their Raynaud’s symptoms.
- Ginger 2000mg–4000mg daily.
The Breastfeeding Network fact sheet for Raynaud’s adds that it may be helpful to include ginger in the mother’s diet e.g. drink ginger tea, or even add a spoonful of ground ginger to bath water.
Summary
Nipple vasospasm is a narrowing of blood vessels in the nipple. It can be triggered by a baby breastfeeding in a shallow latch and can cause burning, stabbing or itching pain in the nipples after a breastfeed. Nipple vasospasm can also be associated with Raynaud’s phenomenon and can also cause Mammary Constriction Syndrome or deep breast pain. Treatment involves improving a baby’s latch and positioning at the breast, and avoiding the triggers of nipple vasospasm. Some medications and natural remedies may help symptoms.
Footnotes & References
-
Thomas. The problem with yeast. Too much diagnosis.
 Too little data. Adapted from Dr Jen’s Guide to Breastfeeding p98. 2012 [accessed 21 October 2022]
Too little data. Adapted from Dr Jen’s Guide to Breastfeeding p98. 2012 [accessed 21 October 2022] -
Nipple Vasospasm Patient Handout, Herzl Family Practice Centre, Goldfarb Breastfeeding Clinic, 2019
-
Nipple Vasospasm Patient Handout, Herzl Family Practice Centre, Goldfarb Breastfeeding Clinic, 2019
-
Douglas. Re-thinking lactation-related nipple pain and damage. Women’s Health Volume 18: 1–29 2022
-
Raynaud’s Phenomenon in Breastfeeding Mothers, Breastfeeding Network, 2019
-
Hills. Raynaud’s of the Nipple: Help for Pregnant & Breastfeeding Moms. Raynauds.org [accessed 20 October 2022]
-
Raynaud’s Phenomenon in Breastfeeding Mothers, Breastfeeding Network, 2019
-
Newman. Vasospasm. 2019
-
Raynaud’s Information.
 Summerwarmth.co.nz [accessed 20 October 2022]
Summerwarmth.co.nz [accessed 20 October 2022] -
Raynaud’s Syndrome, Breastfeeding Network, 2019
-
Anderson et al, Raynaud’s Phenomenon of the Nipple: A Treatable Cause of Painful Breastfeeding, Pediatrics, 2004
-
Raynaud’s Phenomenon in Breastfeeding Mothers, Breastfeeding Network, 2019
-
Anderson et al, Raynaud’s Phenomenon of the Nipple: A Treatable Cause of Painful Breastfeeding, Pediatrics, 2004
-
Hills. Raynaud’s of the Nipple: Help for Pregnant & Breastfeeding Moms. Raynauds.org [accessed 20 October 2022]
Neuralgia of the thoracic region (intercostal neuralgia) - LLC "Quality of Life"
Neuralgia of the thoracic spine, or intercostal neuralgia is a disease in which nerve endings are compressed by muscles, ribs, intervertebral discs. This leads to the development of pain, mostly paroxysmal. Pathology usually occurs against the background of other neurological disorders of the musculoskeletal system.
Pathology usually occurs against the background of other neurological disorders of the musculoskeletal system.
CAUSES OF CHEST PAIN
- 1. Pain in the chest, not associated with pathologies of the intervertebral discs and intercostal nerves. They are caused by a bruise, frequent hypothermia, prolonged stay in a tense uncomfortable position, and posture disorders. As a rule, they pass within 2 weeks.
- 2 . Facet syndrome - develops as a result of inflammation and degenerative processes in the intervertebral joints.
- 3. Intercostal neuralgia - pinching or irritation of the intercostal nerves.
There are many other possible causes of chest pain: angina pectoris, infectious diseases (for example, herpes zoster), thoracic osteochondrosis, intervertebral hernia, aortic aneurysm, malignant tumors of the lungs and pleura, esophagus, pancreas diseases, breast surgery cell.
SYMPTOMS OF THORACIC NERALGIA
- 1 . Most often, the pain is severe, but it can also manifest itself in the form of some discomfort.
- 2 . Increases after a change in body position (tilts, turns), as well as during coughing or sneezing.
- 3 . It manifests itself as a constant or paroxysmal.
- 4 . Sensations burning, stabbing, pressing.
- 5 . Duration - from 1-2 hours to several days or more.
- 6. Even a slight touch to the intercostal spaces or paravertebral points makes the pain unbearable.
- 7 . Irradiation is observed in the arm, back, neck, front of the chest on the left. It is this symptom that often leads to a false interpretation of the cause of the disease, as it resembles a heart attack.
- 8 . The skin along the strangulated nerve changes sensitivity.
 There is paresthesia (distorted sensation) in the form of burning, crawling, tingling. Sometimes a person complains of numbness in the affected area.
There is paresthesia (distorted sensation) in the form of burning, crawling, tingling. Sometimes a person complains of numbness in the affected area. - 9 . The attack is often accompanied by sweating, blanching, cramps in the muscle fibers. The last symptom is caused by impaired blood flow in this area and irritation. The local temperature drops and the area of the body becomes cool.
All of the above symptoms can occur at the same time. But it happens that only one or two signs appear. The degree of their severity depends on the sensitivity threshold and other individual characteristics.
Other diseases that cause chest pain have their own characteristic symptoms. In order to understand them correctly and establish an accurate diagnosis, the doctor asks the patient in detail, carefully examines
VARIETIES OF INTERCOSTAL NAURALGIA
- 1. Left hand . Often confused with cardiac pathologies, which complicates treatment and threatens with complications.
 The pain is localized in the left side of the body, but can radiate to the right. Accompanied by a change in heart rate. If discomfort increases with a change in the position of the body, you should immediately consult a doctor for diagnosis.
The pain is localized in the left side of the body, but can radiate to the right. Accompanied by a change in heart rate. If discomfort increases with a change in the position of the body, you should immediately consult a doctor for diagnosis. - 2 . Right hand . Symptoms practically do not differ from the left-sided, except for the localization of sensations.
- 3. Double sided . It is characterized by girdle pain throughout the upper body, which limits the mobility of the body.
HOW TO DIFFERENTIATE INTERCOSTAL NEURALGIA FROM HEART PAIN
You need to know that not all pain in the chest area is associated with the heart. So you don't have to be scared right away. The diagnosis is made only by a doctor. If you have a pain in your chest, this is a significant reason to see a doctor. The doctor will deal with the cause of the pain. In addition, neuralgia also needs to be treated.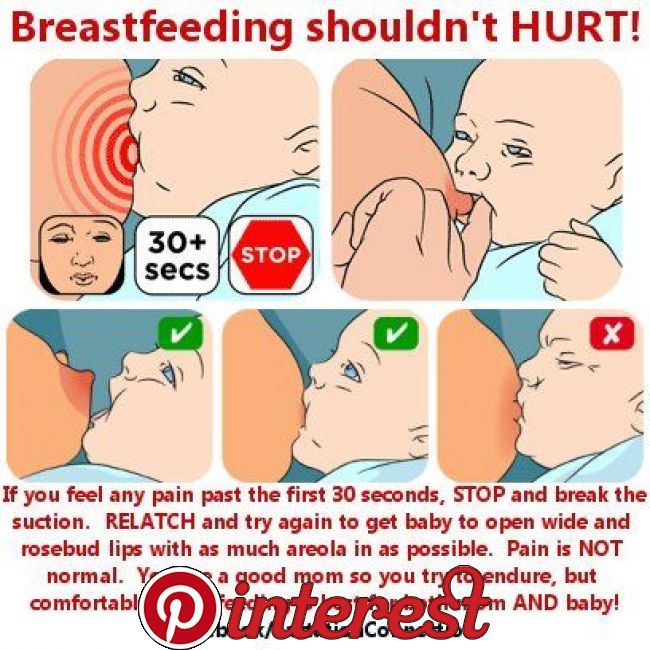
Intercostal neuralgia most often occurs in the elderly, but it also occurs at a young age (at risk are people who lead a sedentary lifestyle, as well as swimming). In children, intercostal neuralgia can occur, as a rule, during a period of intensive growth.
A characteristic sign of intercostal neuralgia is severe pain along the affected nerve. The pain may come in fits or be constant. As a rule, the pain becomes more intense with inhalation, exhalation, as well as any movement that affects the chest. If you press on the area between the ribs, where the causative nerve passes, the pain intensifies. In this case, the entire nerve is felt; pain can radiate to the arm, neck, shoulder, lower back. Along the course of the affected nerve, numbness and blanching of the skin may be observed.
Thus, if with pain in the chest area there is a dependence on a change in body position, there is no shortness of breath (a typical symptom of cardiac pathology), the pain increases with palpation, then, most likely, it is neuralgia.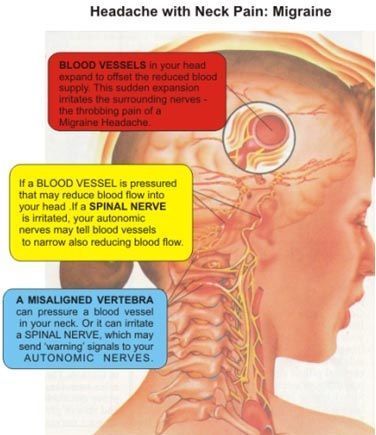 You can also focus on the effectiveness of the drugs taken: heart drugs do not help with neuralgia, but sedatives can reduce pain.
You can also focus on the effectiveness of the drugs taken: heart drugs do not help with neuralgia, but sedatives can reduce pain.
However, in any case, you need to see a doctor for diagnosis and prescriptions.
DIAGNOSTIC METHODS OF INTERCOSTAL NEURALGIA
If you suspect intercostal neuralgia, you should contact a neurologist.
In most cases, the diagnosis is established on the basis of the patient's complaints, medical history and examination of the patient directly at the appointment. The doctor pays attention to the patient's posture: in an effort to reduce pain by reducing pressure on the affected nerve, the patient tilts the body in the opposite direction. The intercostal spaces are palpated in the area of pain localization. There is a loss of sensitivity and blanching of the skin.
Sometimes instrumental and laboratory diagnostics may be required.
In the medical center "Quality of Life" a doctor of the highest category sees a neurologist.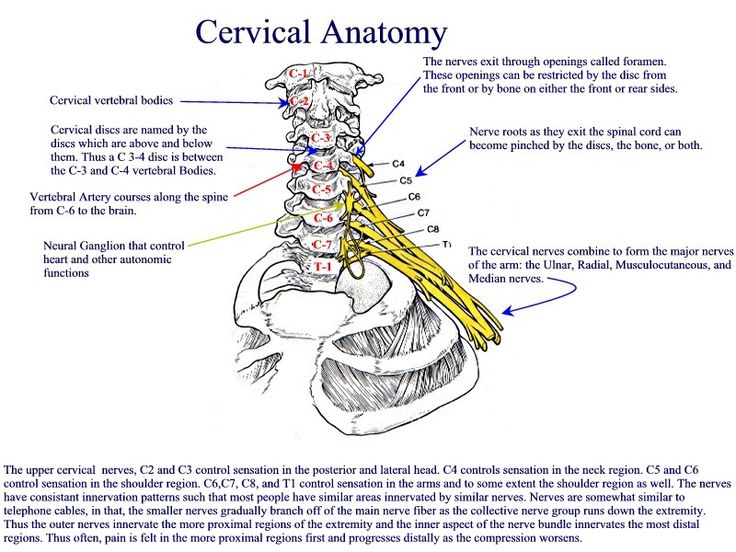 Provides assistance to patients with diseases of the central and peripheral nervous system, and also provides treatment using modern methods.
Provides assistance to patients with diseases of the central and peripheral nervous system, and also provides treatment using modern methods.
Cost of consultation 1100 rub
There are contraindications. Specialist consultation is required.
Pinched nerve in the thoracic region
Pinched nerves in the thoracic region - a condition in which the vertebrae or spinal discs compress the nerve endings. As a result, a person feels pain of varying intensity, which can radiate to different parts of the body. Often, patients come to the doctor with complaints of aching pain. They may be accompanied by difficulty when trying to lie down on the bed, as the process is accompanied by sharp shooting pains. Unpleasant signs in some cases are accompanied by numbness of the limbs.
Pinched nerves of the thoracic region are accompanied by pains of varying intensity. The nature of the discomfort depends on the type of the affected nerve.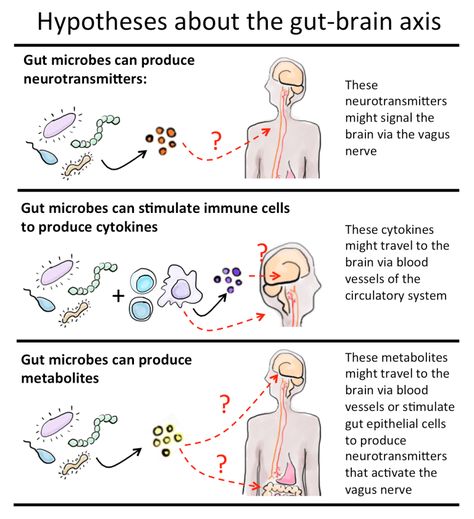 He can answer:
He can answer:
- for sensitivity;
- physical activity;
- vegetative functions.
People who have been suffering from manifestations of osteochondrosis and neuralgia for several years know well what acute, burning pains are, which do not allow them to do everyday activities and reduce the quality of life in general. Unfortunately, it is not easy to stop the pain of nerve root compression, traditional anesthetics rarely help to cope with the task.
Some people, when faced with nerve damage in the spinal column, confuse signs of pathology with symptoms of heart disease, since the manifestations of pathologies are similar.
Pinched nerves: the main causes
Damage to the nerve roots of the thoracic region does not occur at one moment - it is a long process preceded by:
- age-related changes - this process affects all organs and systems, including the spine: over time, the spinal column lends itself to degenerative-dystrophic changes;
- injury, eg rib fractures, spinal contusions;
- violation of posture - scoliosis and other problems must be eliminated, otherwise complications are possible: herniated discs with pinched nerves of the thoracic region;
- long-term and heavy load on the segments of the thoracic region;
- minimization of segment stability due to ankylosing spondylitis;
- problems of a genetic nature;
- excess body weight;
- sedentary lifestyle.
Also, the causes of the pathology are osteochondrosis of the thoracic and cervical regions, disc protrusion, displacement of segments, arthritis, deformity of the spinal column, oncological diseases.
Pathogenesis - what experts say
Doctors believe that the pathogenesis of pinched nerves in the thoracic spine is no different from the process of pinching any other nerves. A negative state occurs due to disorders of nerve conduction due to effects on nerve fibers - deterioration of local metabolic processes, which causes ischemic neuropathy.
Symptoms
The main symptom that indicates damage to nerve fibers in the thoracic region is pain of varying intensity in the spine. Other manifestations will also help diagnose pinched nerves, for example, the appearance of a paroxysmal-type pain syndrome in the intercostal muscles. The pains become stronger and radiate to the spine.
In some patients, pinched nerve roots are accompanied by dizziness, loss of consciousness and memory (short-term). When you try to take a deep breath, cough or sneeze, a person experiences increasing pain - the condition worsens. Also, experts say that 95% of patients have high blood pressure, which leads to migraine.
When you try to take a deep breath, cough or sneeze, a person experiences increasing pain - the condition worsens. Also, experts say that 95% of patients have high blood pressure, which leads to migraine.
Patients often observe numbness of the hands - this sign should alert. A person with a pinched nerve in the thoracic or lumbar region feels tired, and even after waking up does not feel a surge of strength, he prefers calm movements to active movements.
When nerve cells are damaged, the pressure in the vessels constantly fluctuates. With slight pressure on the affected area of the body, pain can radiate to the stomach. It is this symptom that can make diagnosis difficult, since pain in the gastrointestinal tract can be confused with an ulcer or gastritis.
Symptoms of pinched spinal nerves resemble those of heart failure. In such cases, the patient takes cardiac medications, but the intensity of the pain does not decrease.
All of the symptoms listed above may indicate a pinched nerve in the thoracic, lumbar, cervical regions. If the patient experiences pain, dizziness and other symptoms, it is recommended to undergo a diagnosis as soon as possible - this is important for effective treatment and rapid relief of the condition.
If the patient experiences pain, dizziness and other symptoms, it is recommended to undergo a diagnosis as soon as possible - this is important for effective treatment and rapid relief of the condition.
What complications and consequences can there be?
How to make a diagnosis
To establish the root cause of the disease, the doctor prescribes several diagnostic measures. If the patient has the main symptoms of the pathology, he is shown special procedures. The doctor individually selects a set of measures, the results of which will help assess the state of health and prescribe effective treatment. Therapy will relieve pain and other manifestations of the disease.
If you have symptoms of pinched nerves in the thoracic region, do not put off a visit to your doctor. This will help you avoid complications and get quality care.
This will help you avoid complications and get quality care.
The complex of diagnostic measures may include:
- clinical urine and blood tests;
- X-ray examination;
- CT and MRI;
- x-ray examination using a contrast agent - the procedure will help determine the location of the problem;
- ultrasound;
- electrocardiogram.
Differential diagnosis
If a patient is diagnosed with cardiovascular pathology, spinal cord cancer, ganglioneuritis, pinched intercostal nerves due to herpes, he is assigned a differential diagnosis.
The technique involves examination of the patient, analysis of the anamnesis, which makes it possible to exclude certain diseases and come to the only correct diagnosis. As part of the differential diagnosis, it is possible to distinguish the existing pathology from others that may have similar symptoms.
How is the treatment of pinched nerves
Patients with cervical osteochondrosis, pinched sciatic nerve due to intervertebral hernia experience severe pain. Therefore, the first task of a medical worker is to select anesthetics that will help relieve pain. The drugs remove muscle spasm, play the role of a blocker, and minimize discomfort. The drug in the treatment of intercostal neuralgia is administered by injection, hormonal and local preparations are prescribed. Be sure to prescribe diuretic medications that help reduce swelling of the pinched nerve. Means that improve nerve conduction are also relevant.
Therefore, the first task of a medical worker is to select anesthetics that will help relieve pain. The drugs remove muscle spasm, play the role of a blocker, and minimize discomfort. The drug in the treatment of intercostal neuralgia is administered by injection, hormonal and local preparations are prescribed. Be sure to prescribe diuretic medications that help reduce swelling of the pinched nerve. Means that improve nerve conduction are also relevant.
In addition to relieving pain, the task of treatment is to have a direct effect on the cause that caused spasm of nerves in the chest, neck muscles, in the lumbar region, etc. Not only drugs, but also massages and manual therapy techniques help reduce joint destruction. Physiotherapy is often prescribed. Showing moderate physical activity. As far as medicines are concerned, patients are shown:
- medicines to normalize blood flow;
- funds responsible for restoring the structure of cartilage;
- medicines containing calcium, vitamin D;
- multivitamin supplemented with a mineral complex.
With cervical osteochondrosis, various types of massage show good results. Moderate physical impact, rubbing in a positive way affects muscle tissue, helps to remove spasms, improve local metabolic processes and improve tissue nutrition.
Some patients suffering from herniated discs require surgery. Such therapy is especially relevant after injuries, if the hernia has reached a large size, stabilization of the spinal column is necessary.
Radiofrequency ablation is prescribed - a modern technique in which a needle is used, through the end of which radiofrequency impulses are passed. Thus, denervation of the affected spinal disc, which is the source of pain, is achieved. If you carry out the procedure with a pinched nerve in the thoracic region, you can minimize or completely remove the pain syndrome.
If you pay attention to the symptoms of spinal pathologies and they interfere with normal life, you should not postpone a visit to the medical center, because ignoring pain and other signs can cause serious complications, including irreversible changes in the structures of the spine.
Which doctor should I contact?
Cervical osteochondrosis, herniated discs are treated by a vertebrologist and an orthopedic traumatologist. Often doctors interact with each other, which allows them to choose effective methods of diagnosis and treatment for the patient.
Prognosis and prevention
Patients with cervical osteochondrosis and other diseases of the spine experience pinched nerves. Not all types of pathology can be prevented, but the risks of pain can be reduced:
- try to watch your posture – you can wear a special corset;
- bring the weight back to normal - obesity contributes to the development of diseases of the spinal column;
- do not hesitate to visit a doctor when the first signs of spinal disease appear.
Prognosis
The effectiveness of the patient's treatment is individual and depends on the localization of the problem, the degree of pinching, the correctness of the diagnosis and the prescribed drugs.